Stoma Savvy Fraser Health Regional Wound Education Regional






- Slides: 104
Stoma Savvy Fraser Health Regional Wound Education Regional Skin Integrity & Wound Management Steering Committee & Stoma Savvy Education Shared Work Team June 2012 1
Vision MODULE 5 § To enhance the quality of life of clients with Ostomies (colostomy, ileostomy, and/or urostomy) with a person-centered and a team approach Mission § Establish a team approach to identify and to address the needs of clients with ostomies in different settings in a timely manner by: 1. Utilizing the appropriate tools/resources 2. Identifying interdisciplinary team members’ roles Stoma Savvy 2006 Revised: 2012 2
Ice Breaker / Pre-test MODULE 5 Stoma Savvy 2006 Revised: 2012 3
Learning Objectives MODULE 5 § Identify common types of ostomies § Explore basic ostomy management § Discuss psychosocial considerations for the person with a new ostomy § Describe types of peristomal skin problems & their management § Describe stomal complications & their management Stoma Savvy 2006 Revised: 2012 4
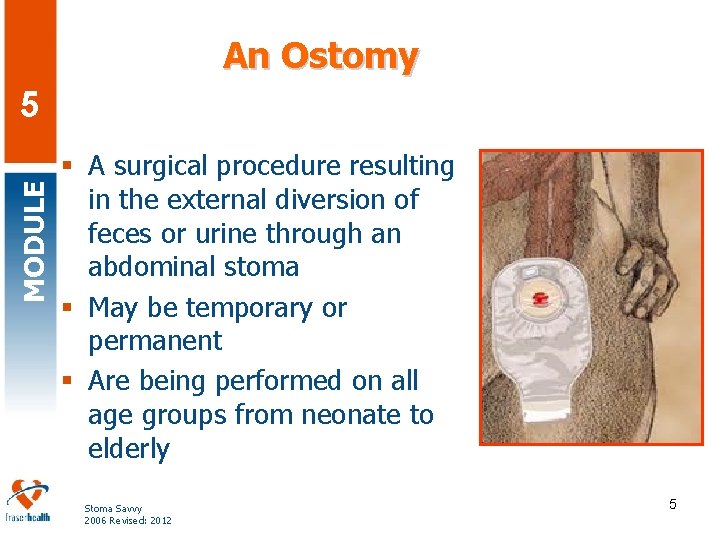
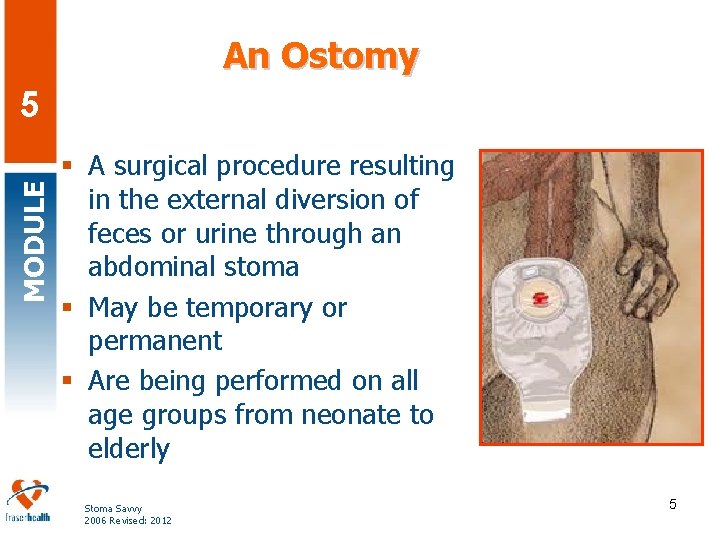
An Ostomy MODULE 5 § A surgical procedure resulting in the external diversion of feces or urine through an abdominal stoma § May be temporary or permanent § Are being performed on all age groups from neonate to elderly Stoma Savvy 2006 Revised: 2012 5
Etiologies for Ostomy MODULE 5 § § § Colorectal cancer (36%) Inflammatory bowel disease (15%) Bladder cancer (12%) Diverticulitis (11%) Necrotizing enterocolitis, congenital anomalies, Hirschsprung’s disease, etc Stoma Savvy 2006 Revised: 2012 6

Interprofessional Team MODULE 5 Client with an Ostomy Recreation staff Physiotherapy Occupational Therapy Social Worker Dietitian Stoma Savvy 2006 Revised: 2012 Physicians/NPs Specialists ET/WOCNs Pharmacist Nurses Care Aides 7
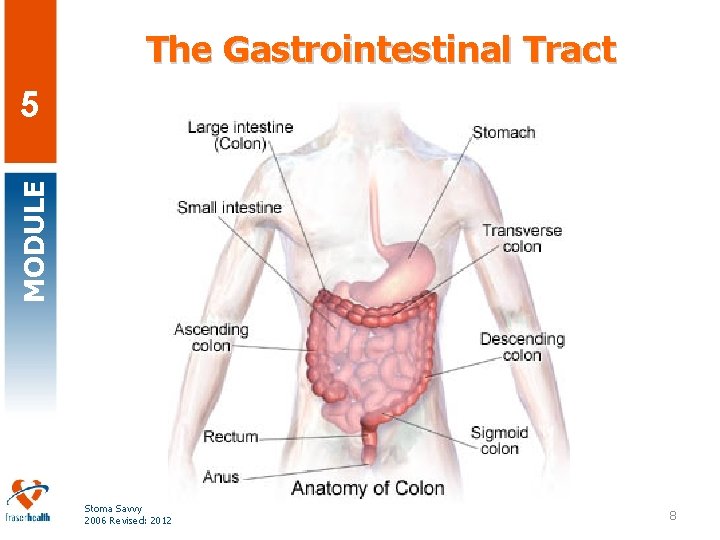
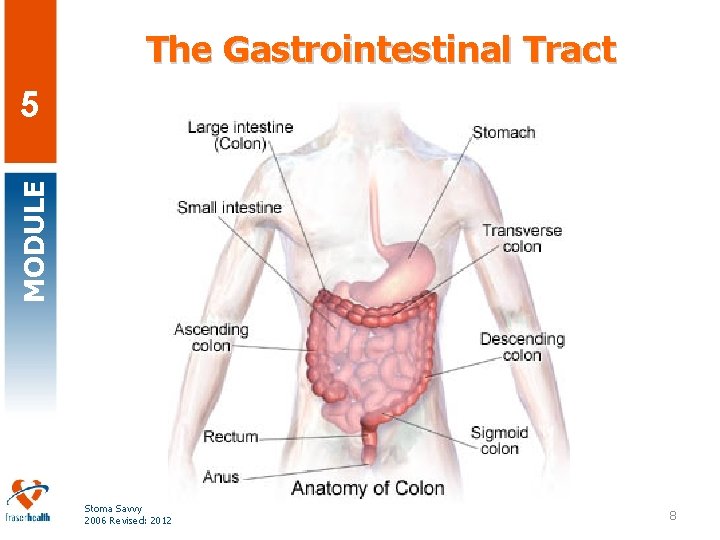
The Gastrointestinal Tract MODULE 5 Stoma Savvy 2006 Revised: 2012 8
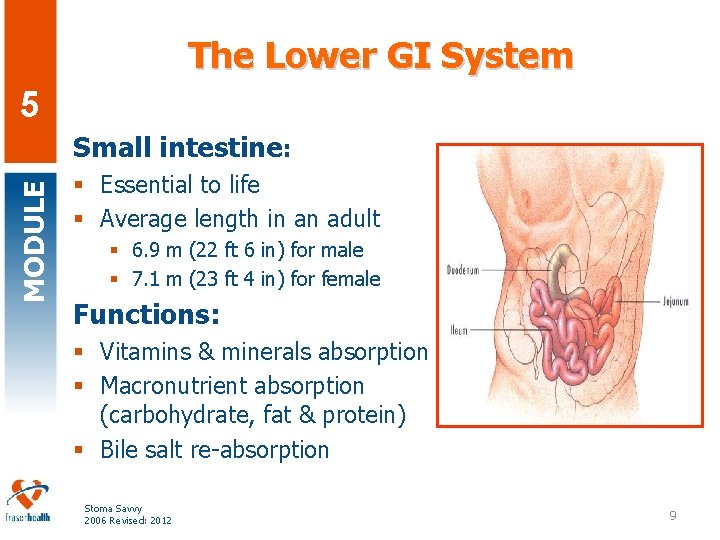
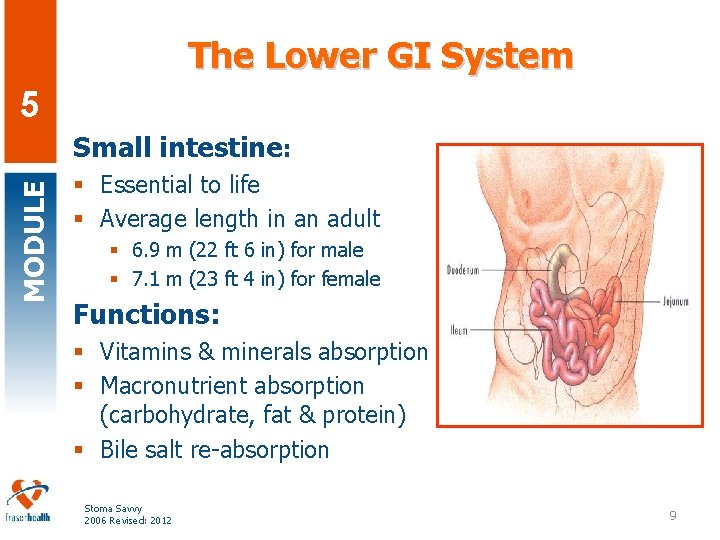
The Lower GI System 5 MODULE Small intestine: § Essential to life § Average length in an adult § 6. 9 m (22 ft 6 in) for male § 7. 1 m (23 ft 4 in) for female Functions: § Vitamins & minerals absorption § Macronutrient absorption (carbohydrate, fat & protein) § Bile salt re-absorption Stoma Savvy 2006 Revised: 2012 9
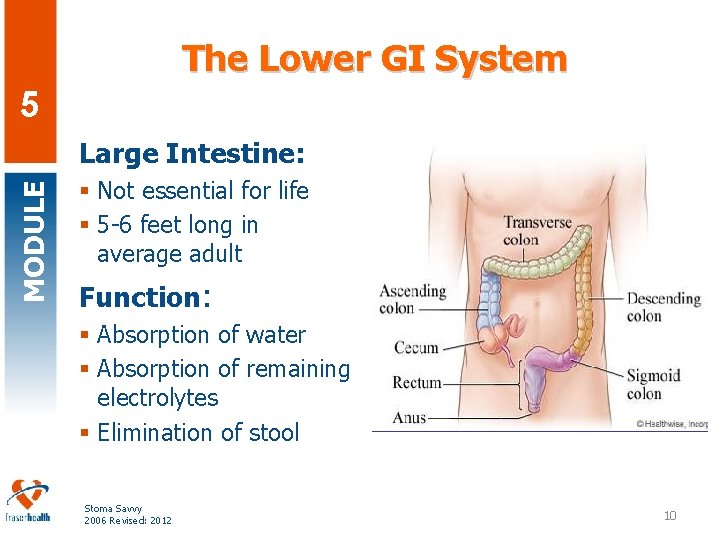
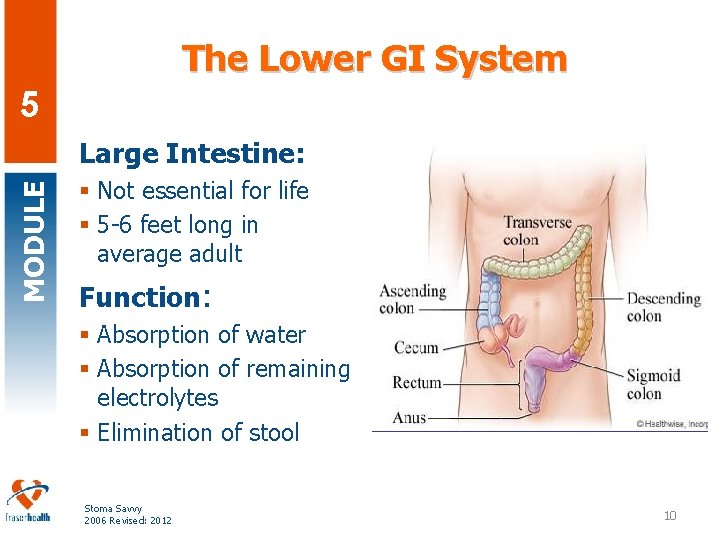
The Lower GI System 5 MODULE Large Intestine: § Not essential for life § 5 -6 feet long in average adult Function: § Absorption of water § Absorption of remaining electrolytes § Elimination of stool Stoma Savvy 2006 Revised: 2012 10
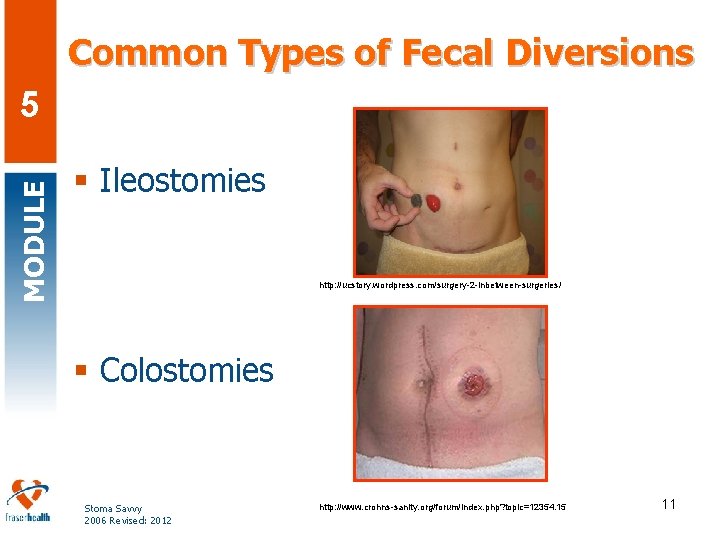
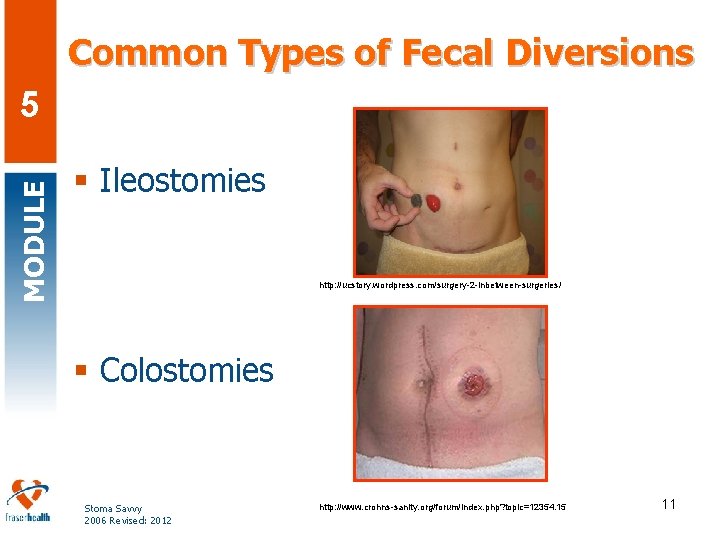
Common Types of Fecal Diversions MODULE 5 § Ileostomies http: //ucstory. wordpress. com/surgery-2 -inbetween-surgeries/ § Colostomies Stoma Savvy 2006 Revised: 2012 http: //www. crohns-sanity. org/forum/index. php? topic=12354. 15 11
Basic Ostomy Management MODULE 5 Goal is to promote client’s independence and quality of life § § Client teaching Can the stoma be reversed and when? When the client can go back to work? What are the specific considerations? Stoma Savvy 2006 Revised: 2012 12
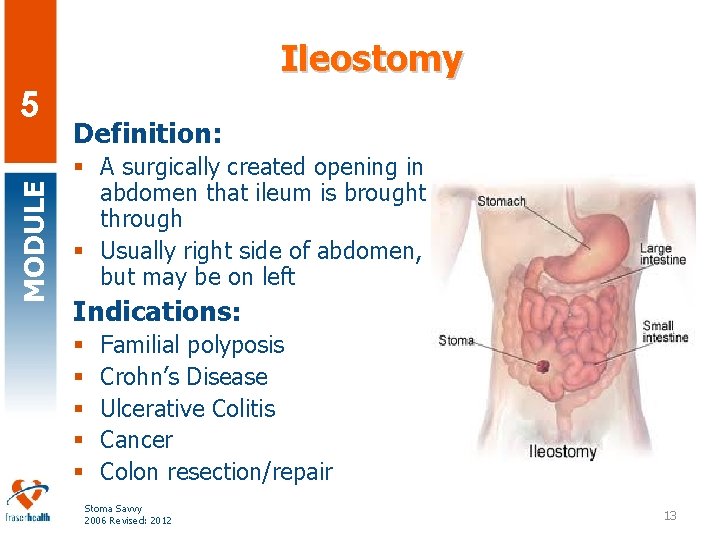
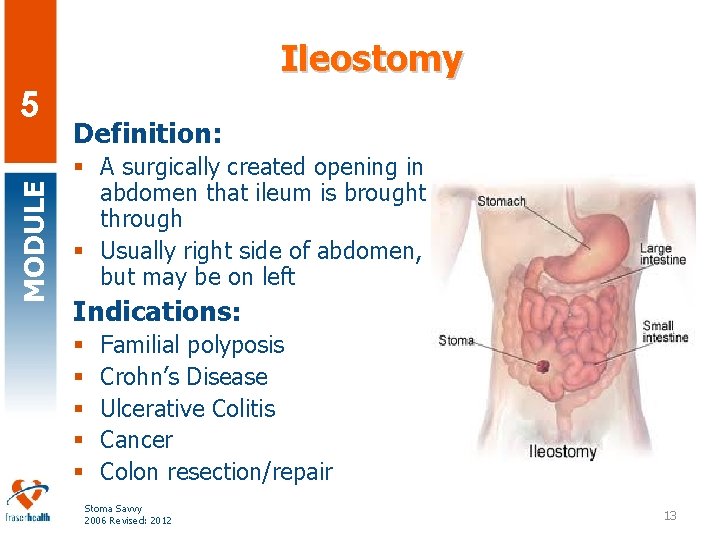
Ileostomy MODULE 5 Definition: § A surgically created opening in abdomen that ileum is brought through § Usually right side of abdomen, but may be on left Indications: § § § Familial polyposis Crohn’s Disease Ulcerative Colitis Cancer Colon resection/repair Stoma Savvy 2006 Revised: 2012 13
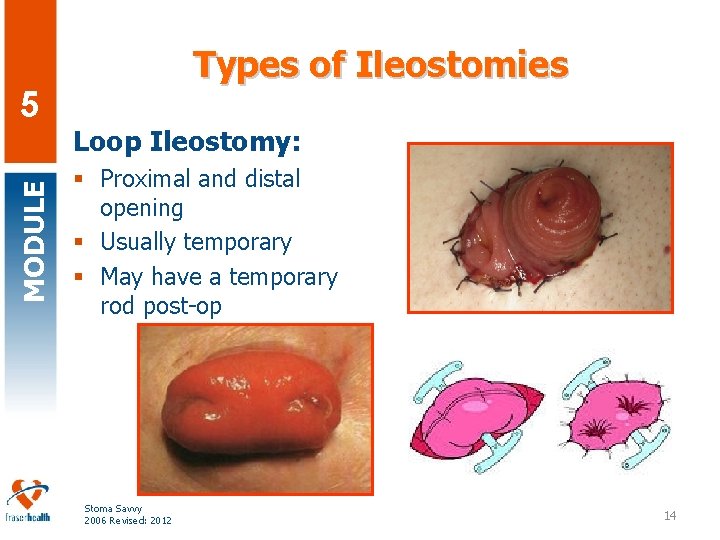
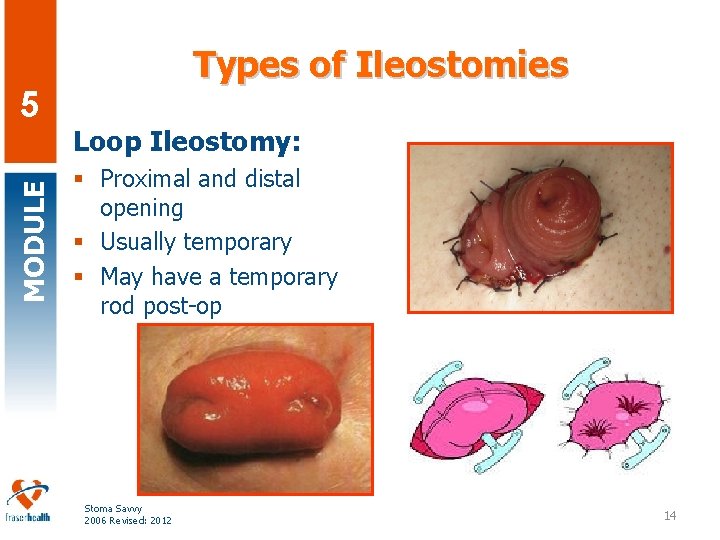
MODULE 5 Types of Ileostomies Loop Ileostomy: § Proximal and distal opening § Usually temporary § May have a temporary rod post-op Stoma Savvy 2006 Revised: 2012 14
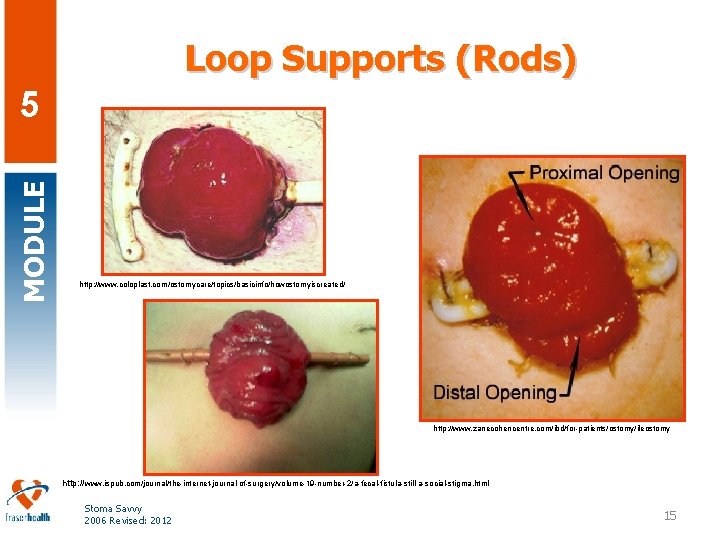
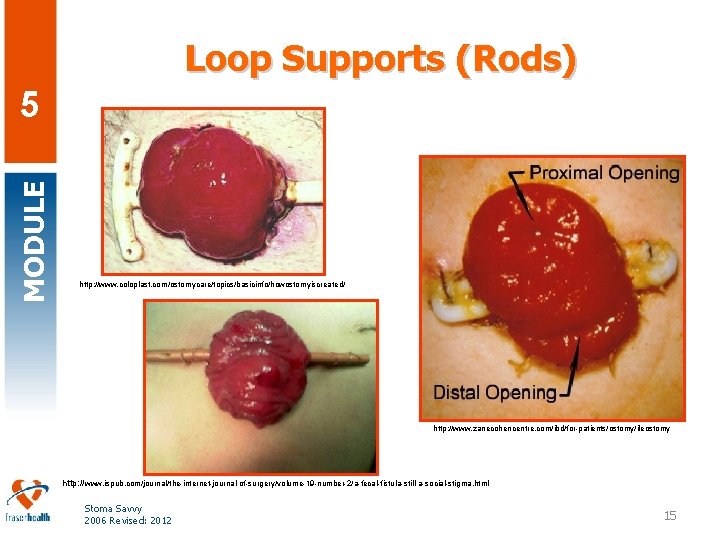
Loop Supports (Rods) MODULE 5 http: //www. coloplast. com/ostomycare/topics/basicinfo/howostomyiscreated/ http: //www. zanecohencentre. com/ibd/for-patients/ostomy/ileostomy http: //www. ispub. com/journal/the-internet-journal-of-surgery/volume-19 -number-2/a-fecal-fistula-still-a-social-stigma. html Stoma Savvy 2006 Revised: 2012 15
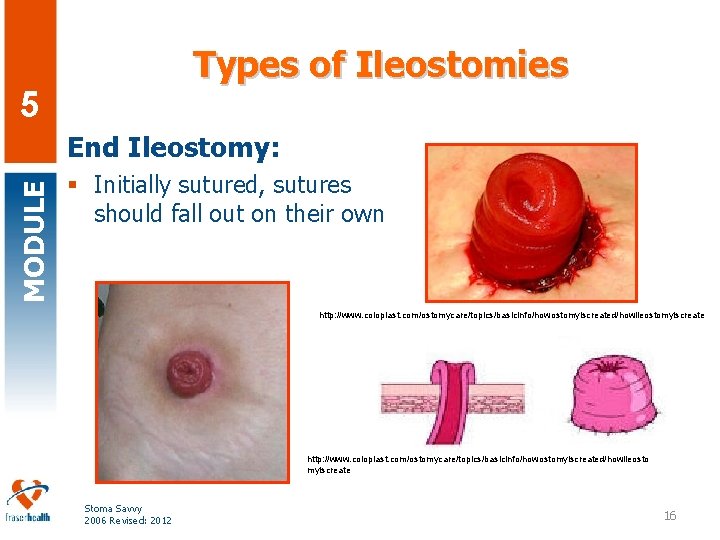
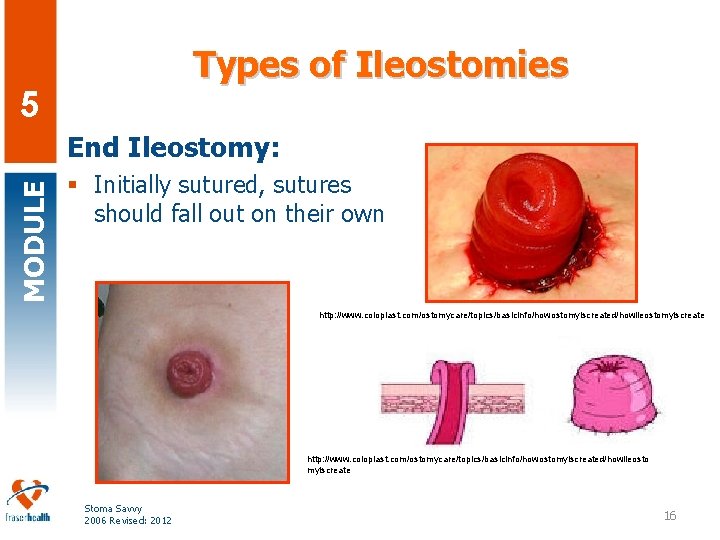
Types of Ileostomies 5 MODULE End Ileostomy: § Initially sutured, sutures should fall out on their own http: //www. coloplast. com/ostomycare/topics/basicinfo/howostomyiscreated/howileostomyiscreate http: //www. coloplast. com/ostomycare/topics/basicinfo/howostomyiscreated/howileosto myiscreate Stoma Savvy 2006 Revised: 2012 16
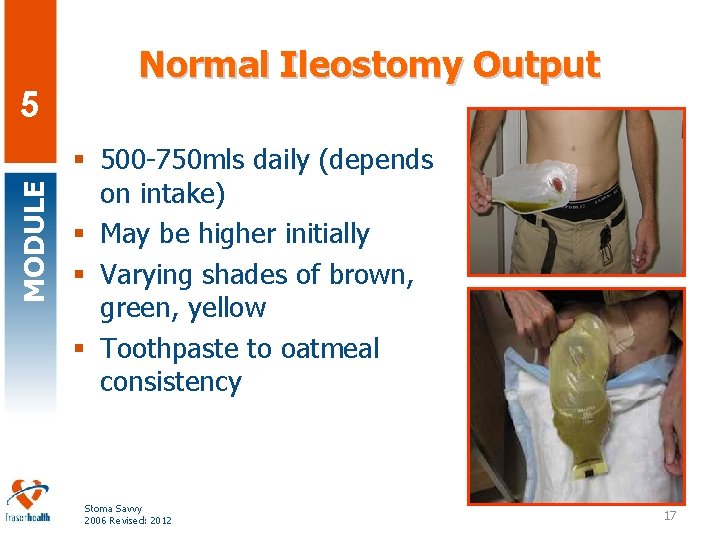
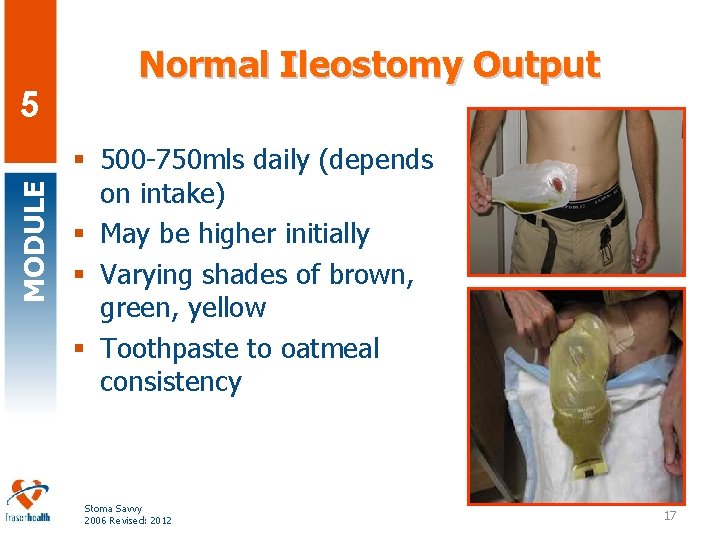
MODULE 5 Normal Ileostomy Output § 500 -750 mls daily (depends on intake) § May be higher initially § Varying shades of brown, green, yellow § Toothpaste to oatmeal consistency Stoma Savvy 2006 Revised: 2012 17
MODULE 5 Ileostomy Bowel Management § Laxatives, suppositories, or enemas are not recommended (RNAO, 2009) § Stool is usually too liquid § Stoma has no sphincter to allow for suppository retention § If stool is too liquid, certain foods and medications may be used to thicken output Stoma Savvy 2006 Revised: 2012 18
MODULE 5 Ileostomy Considerations § Person with an ileostomy will require a “drainable” system that will allow for frequent emptying § Recommend emptying pouch when 1/3 full § May need to empty pouch 4 -6 times daily § They may need to empty through the night Stoma Savvy 2006 Revised: 2012 19
If Pouch is Leaking MODULE 5 Change it! Don’t reinforce it § The enzymes contained in the liquid stool is damaging to the skin § Essential to have peri-stomal skin protected with a properly fitted appliance § Empty the pouch regularly when 1/3 full to protect pouch seal and peristomal skin Stoma Savvy 2006 Revised: 2012 20
5 Diet & Fluid Modifications MODULE Reducing Risk of Blockages: 6 -8 weeks post-op § Avoid high fiber foods After 6 -8 weeks § Re-introduce higher fiber foods in small amounts, one at a time Always § Be sure to chew your food well and smaller, more frequent meals may be better tolerated initially Stoma Savvy 2006 Revised: 2012 21
Diet and Fluid Modifications MODULE 5 § Ileostomy daily fluid loss 500 -750 mls § Intact colon daily fluid loss 100 -200 mls § Hydration: § Drink an extra 2 -3 cups of fluid per day § Pay extra attention to hydration, especially when exercising, hot climate, etc. § Electrolyte Balance: § Oral rehydration solutions as needed as Na+ and K+ losses are increased Stoma Savvy 2006 Revised: 2012 22
Partial/Complete Obstruction MODULE 5 Client education on risk for food blockage Symptoms: § No output or high liquid output in 12 hrs § Cramping § Bloating/nausea Management: § Contact ET/WOCN § Go to Emergency Stoma Savvy 2006 Revised: 2012 23
MODULE 5 Stoma Savvy 2006 Revised: 2012
Ileostomies and Medications MODULE 5 § Changes in medication absorption will occur § Residual pieces of medications in pouch suggest consultation with pharmacist § Medications may result in a change of colour, odour and consistency of feces Stoma Savvy 2006 Revised: 2012 25
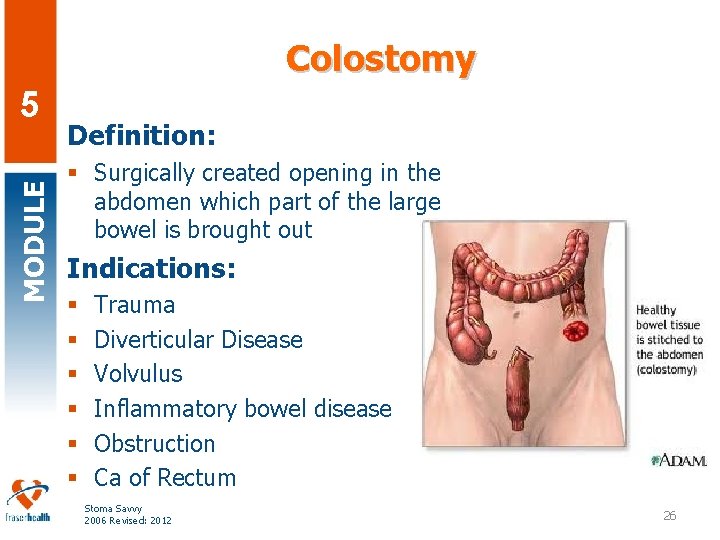
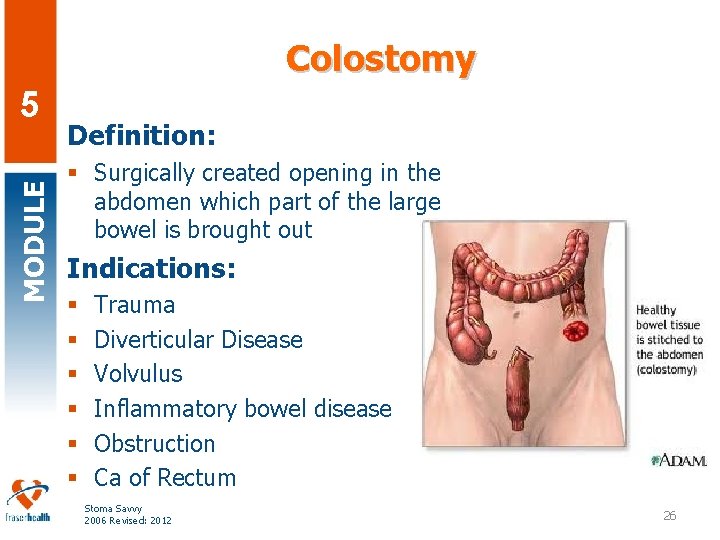
Colostomy MODULE 5 Definition: § Surgically created opening in the abdomen which part of the large bowel is brought out Indications: § § § Trauma Diverticular Disease Volvulus Inflammatory bowel disease Obstruction Ca of Rectum Stoma Savvy 2006 Revised: 2012 26
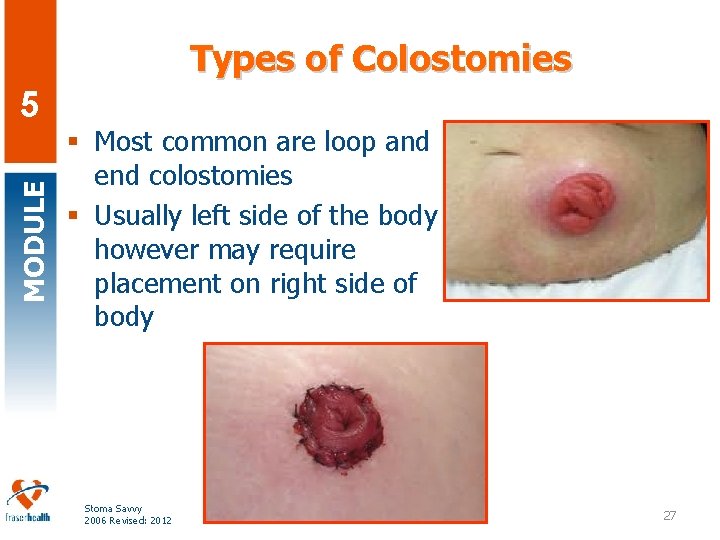
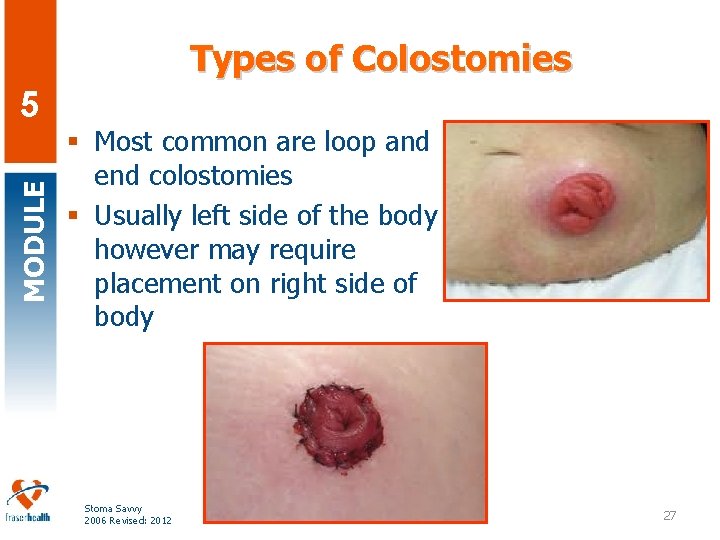
Types of Colostomies MODULE 5 § Most common are loop and end colostomies § Usually left side of the body however may require placement on right side of body Stoma Savvy 2006 Revised: 2012 27
Colostomy Dietary Considerations MODULE 5 § No need for specific dietary changes § Recommend a healthy diet § Adequate fluids, whole grains, fresh fruit and vegetables, milk/milk alternatives and lean meats/meat alternatives Stoma Savvy 2006 Revised: 2012 28
Dietary Considerations MODULE 5 § Some foods may increase gas or odour: § Legumes, broccoli, cauliflower, cabbage, brussel sprouts § If gas is a problem, try avoiding: § Carbonated beverages, drinking through straws, talking while eating and chewing gum § Foods that may help thicken stoma output: § Yogurt, cheese, white bread, potatoes, pasta, bananas, pasta white rice and applesauce. Stoma Savvy 2006 Revised: 2012 29
MODULE 5 Colostomies and Medications § No change in absorption of oral medications § Suppository not recommended § Some medications may constipate or cause diarrhea Stoma Savvy 2006 Revised: 2012 30
MODULE 5 Bowel Care for Colostomies § Persons with a colostomy may experience constipation, a bowel protocol may be required § Stomal enemas are more effective if used with an irrigation cone for fluid retention Stoma Savvy 2006 Revised: 2012 31
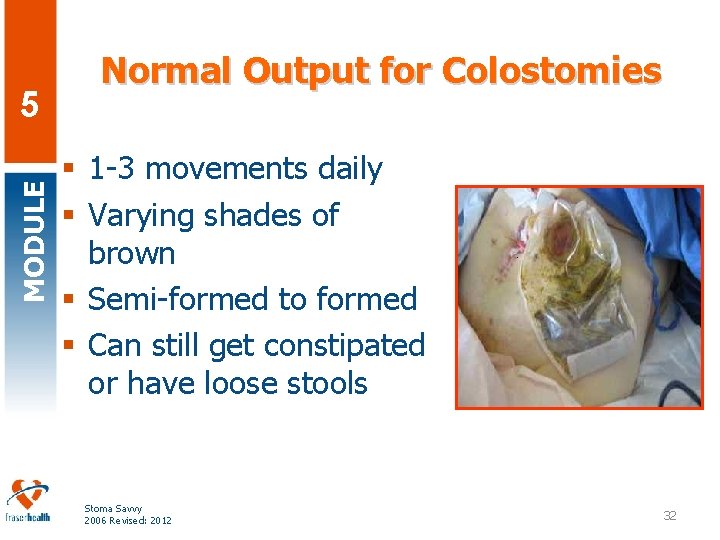
MODULE 5 Normal Output for Colostomies § 1 -3 movements daily § Varying shades of brown § Semi-formed to formed § Can still get constipated or have loose stools Stoma Savvy 2006 Revised: 2012 PHOTOGRAPH REQUIRED 32
Ileostomy/Colostomy Reversal MODULE 5 § Minimum of 3 months after initial surgery § May be longer if chemo or radiation done after surgery § Tests done first to ensure anastamosis is well healed § Length of stay in hospital is usually 3 -5 days § Some diarrhea is normal after reversal. § May require protective barrier cream Stoma Savvy 2006 Revised: 2012 33
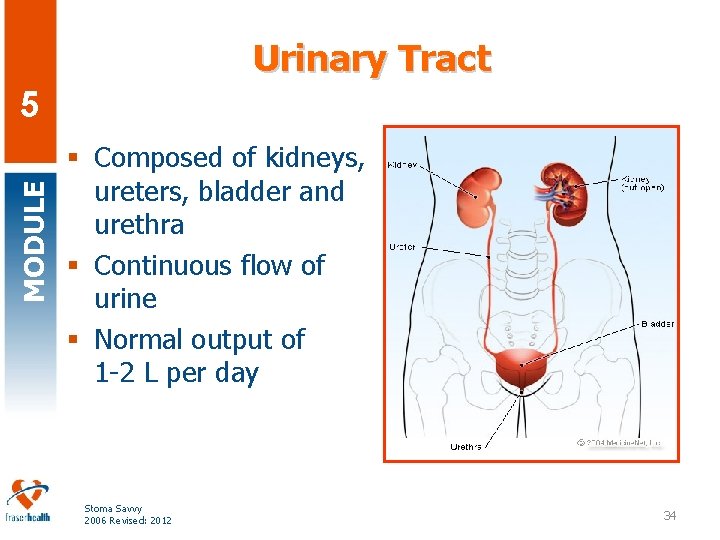
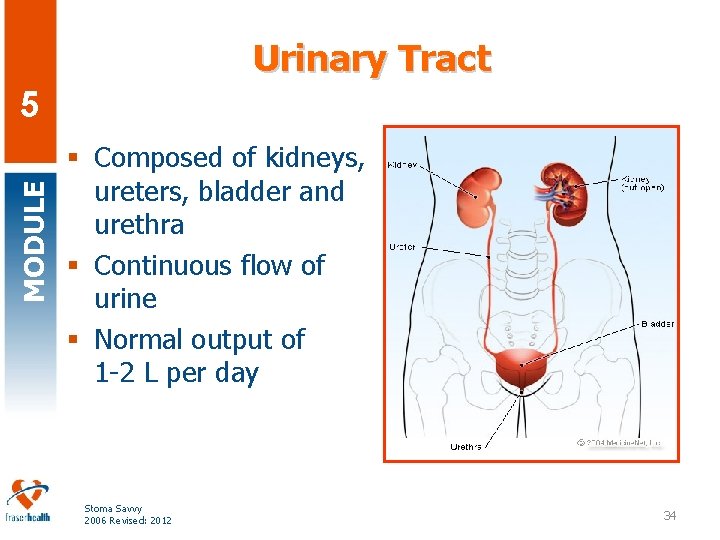
Urinary Tract MODULE 5 § Composed of kidneys, ureters, bladder and urethra § Continuous flow of urine § Normal output of 1 -2 L per day Stoma Savvy 2006 Revised: 2012 34
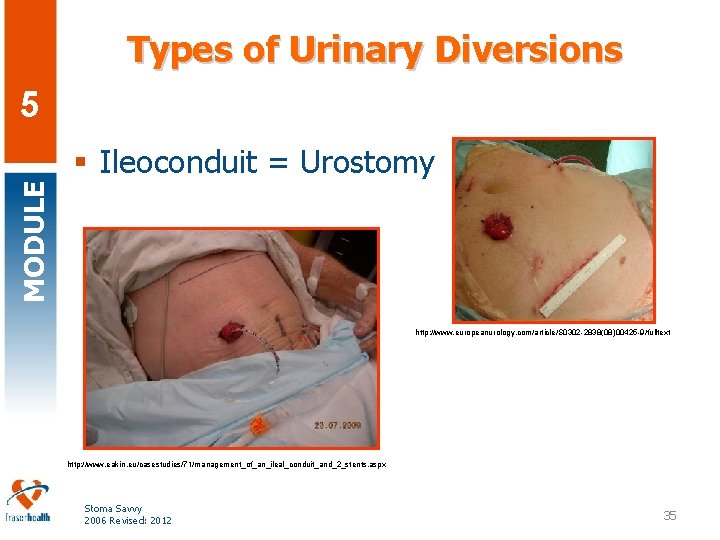
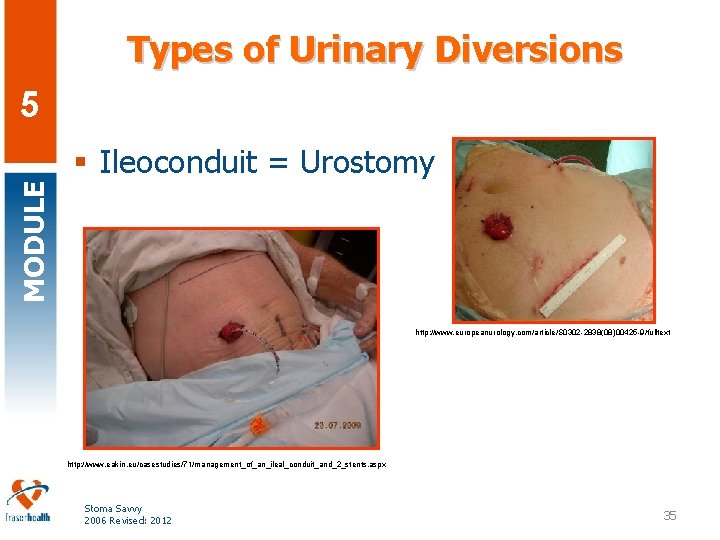
Types of Urinary Diversions 5 MODULE § Ileoconduit = Urostomy http: //www. europeanurology. com/article/S 0302 -2838(08)00425 -9/fulltext http: //www. eakin. eu/casestudies/71/management_of_an_ileal_conduit_and_2_stents. aspx Stoma Savvy 2006 Revised: 2012 35
Reasons for Urinary Diversions MODULE 5 § § § Cancer or tumor of the bladder Injury/trauma Birth defects Chronic UTIs May be elective for incontinence Stoma Savvy 2006 Revised: 2012 36
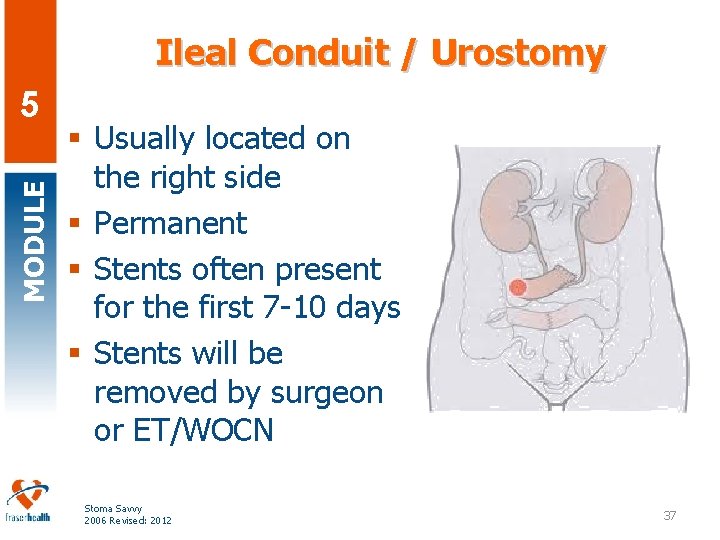
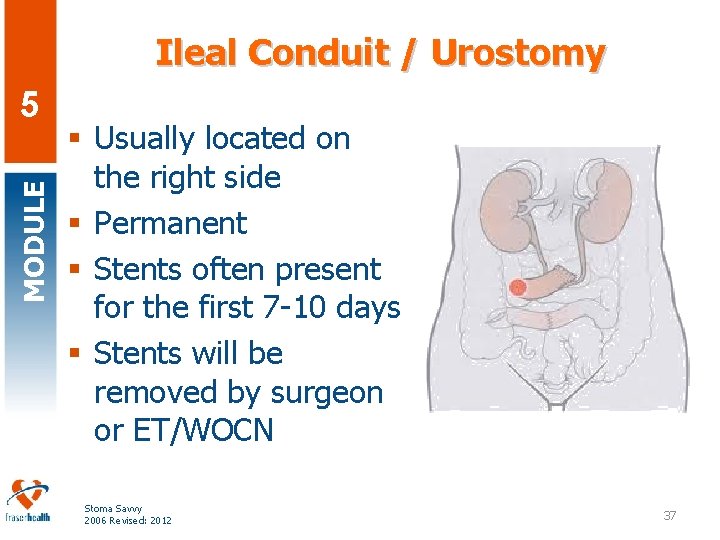
Ileal Conduit / Urostomy MODULE 5 § Usually located on the right side § Permanent § Stents often present for the first 7 -10 days § Stents will be removed by surgeon or ET/WOCN Stoma Savvy 2006 Revised: 2012 37
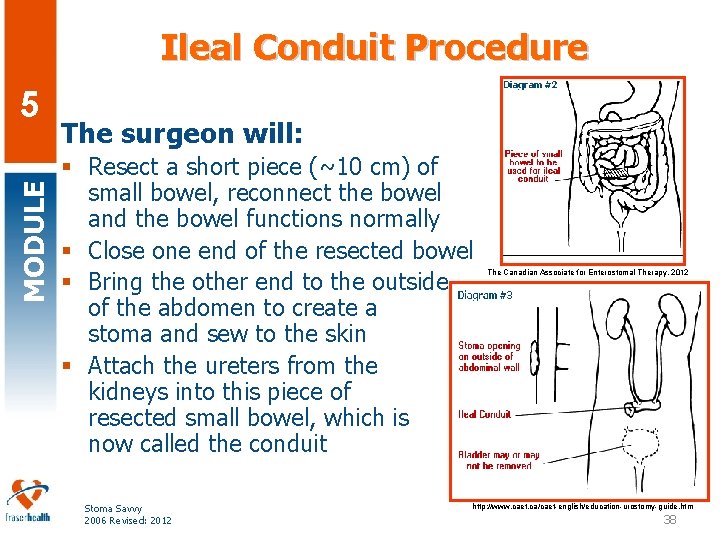
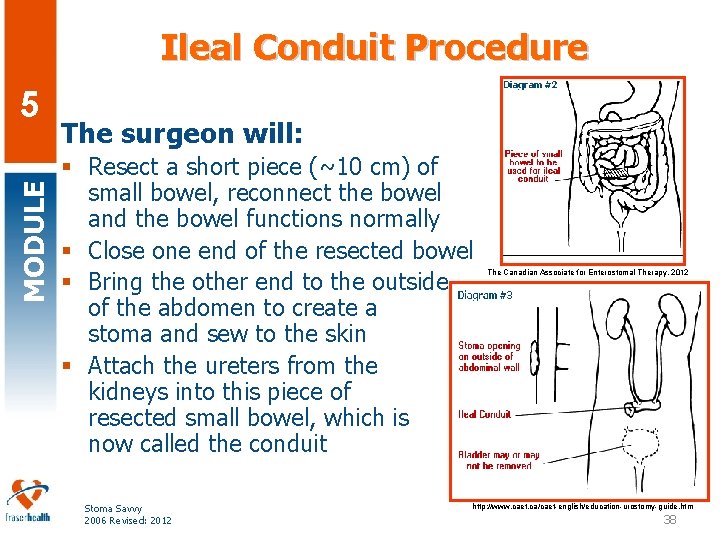
Ileal Conduit Procedure MODULE 5 The surgeon will: § Resect a short piece (~10 cm) of small bowel, reconnect the bowel and the bowel functions normally § Close one end of the resected bowel § Bring the other end to the outside of the abdomen to create a stoma and sew to the skin § Attach the ureters from the kidneys into this piece of resected small bowel, which is now called the conduit Stoma Savvy 2006 Revised: 2012 The Canadian Associate for Enterostomal Therapy, 2012 http: //www. caet. ca/caet-english/education-urostomy-guide. htm 38
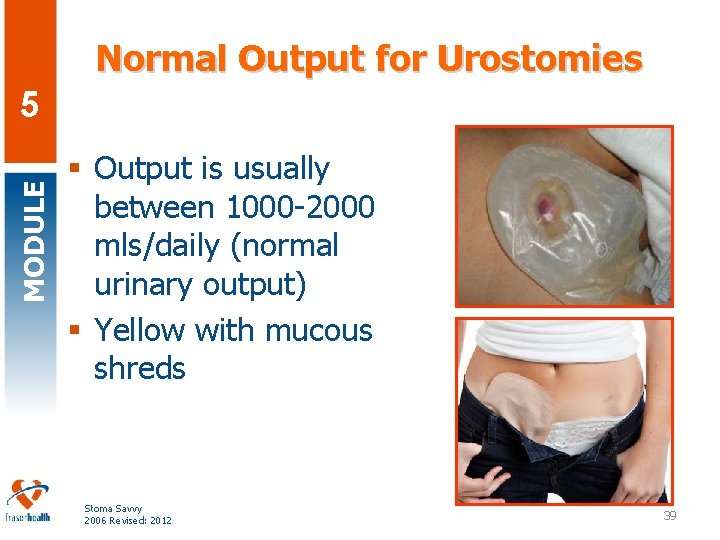
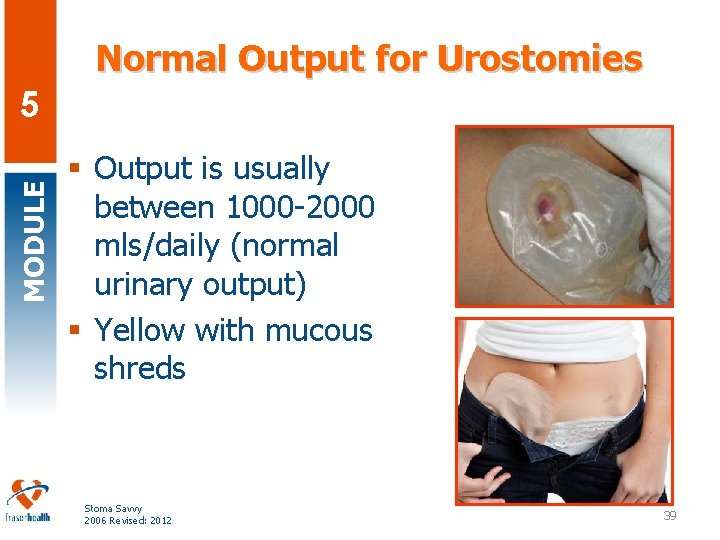
Normal Output for Urostomies MODULE 5 § Output is usually between 1000 -2000 mls/daily (normal urinary output) § Yellow with mucous shreds Stoma Savvy 2006 Revised: 2012 39
Persons with a Urostomy MODULE 5 § Maintain adequate fluid intake for optimal hydration § Monitor for signs and symptoms of urinary tract infection and treat infection promptly § Infection causes urine to become more alkaline which is more damaging Stoma Savvy 2006 Revised: 2012 40
Urostomy Dietary Considerations MODULE 5 § No dietary restrictions § Odour can be increased with certain foods such as asparagus and seafood, and with certain medications § Adequate hydration may help to prevent infections Stoma Savvy 2006 Revised: 2012 41
MODULE 5 Psychosocial Considerations Stoma Savvy 2006 Revised: 2012 42
MODULE Common Concerns for Individuals with New Ostomies… 5 § Will I smell? § How do I shower? § How much are supplies and where do I get them? § Do I always have to wear a pouch? § Questions about sex, exercise, returning to work, travel. Stoma Savvy 2006 Revised: 2012 43
MODULE 5 Stoma Savvy 2006 Revised: 2012

5 MODULE • Coffee Break Stoma Savvy 2006 Revised: 2012
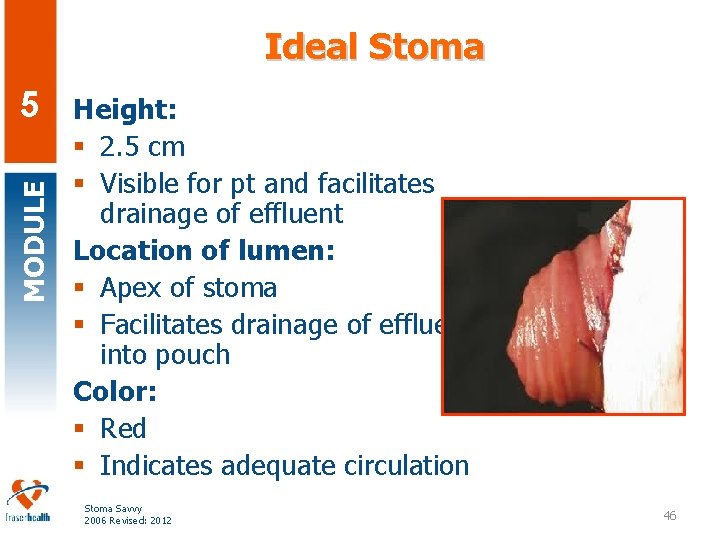
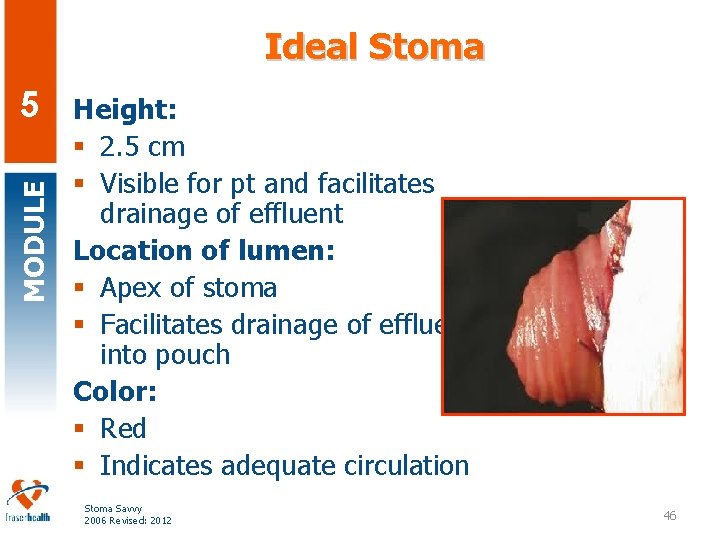
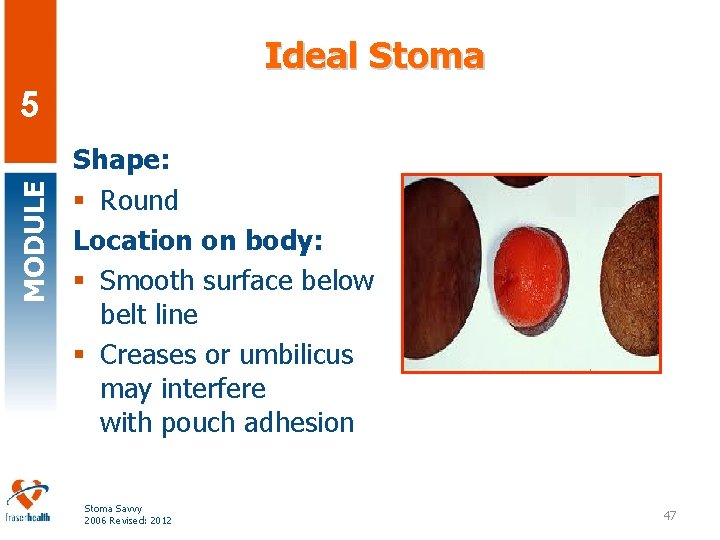
Ideal Stoma MODULE 5 Height: § 2. 5 cm § Visible for pt and facilitates drainage of effluent Location of lumen: § Apex of stoma § Facilitates drainage of effluent into pouch Color: § Red § Indicates adequate circulation Stoma Savvy 2006 Revised: 2012 46
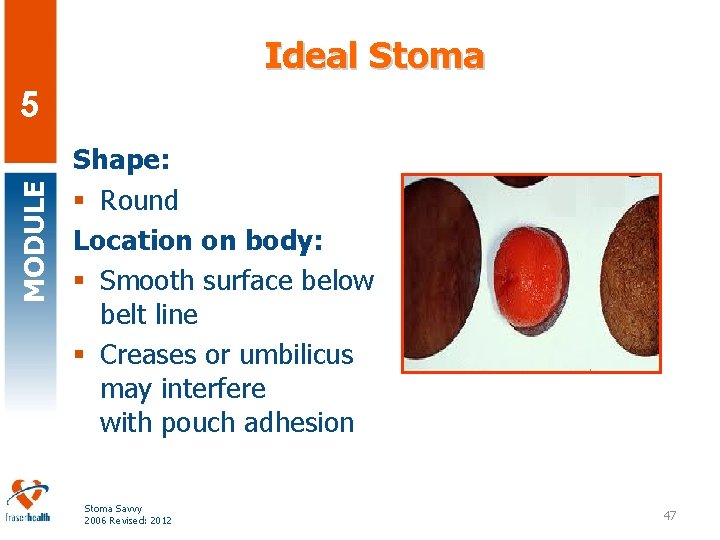
Ideal Stoma MODULE 5 Shape: § Round Location on body: § Smooth surface below belt line § Creases or umbilicus may interfere with pouch adhesion Stoma Savvy 2006 Revised: 2012 47
MODULE Changing An Appliance – What do I Do? 5 Stoma Savvy 2006 Revised: 2012 48
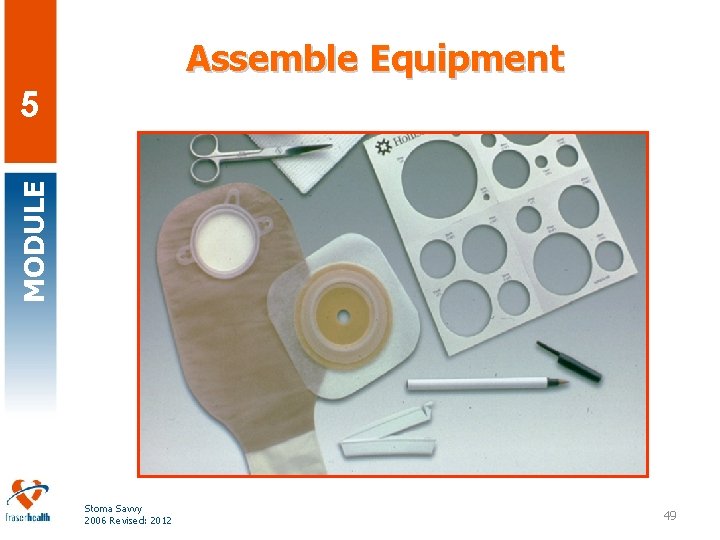
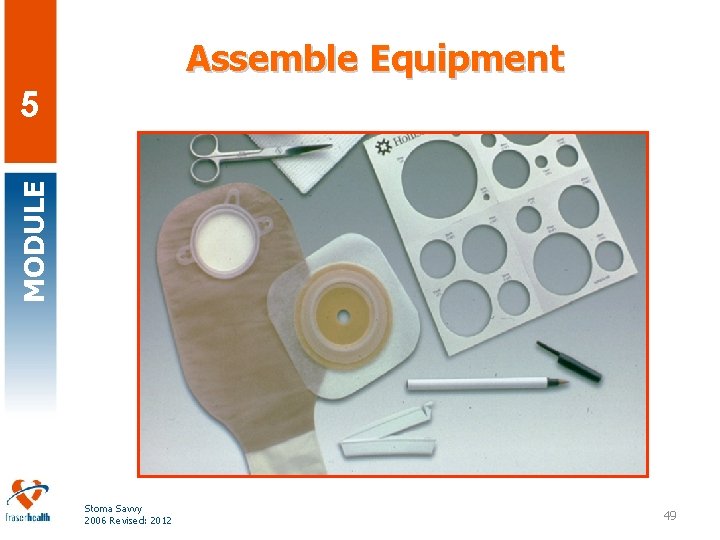
Assemble Equipment MODULE 5 Stoma Savvy 2006 Revised: 2012 49
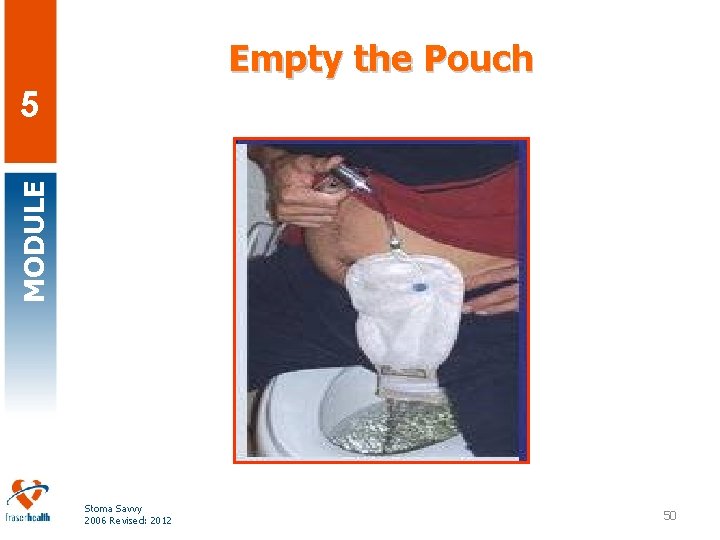
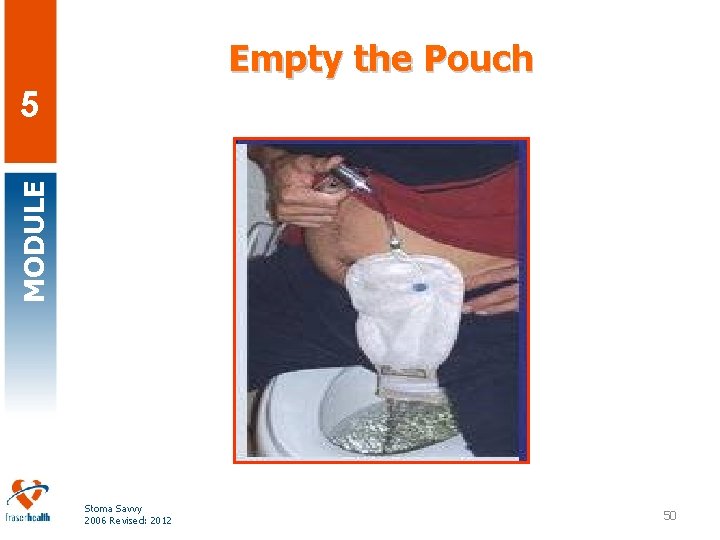
Empty the Pouch MODULE 5 Stoma Savvy 2006 Revised: 2012 50
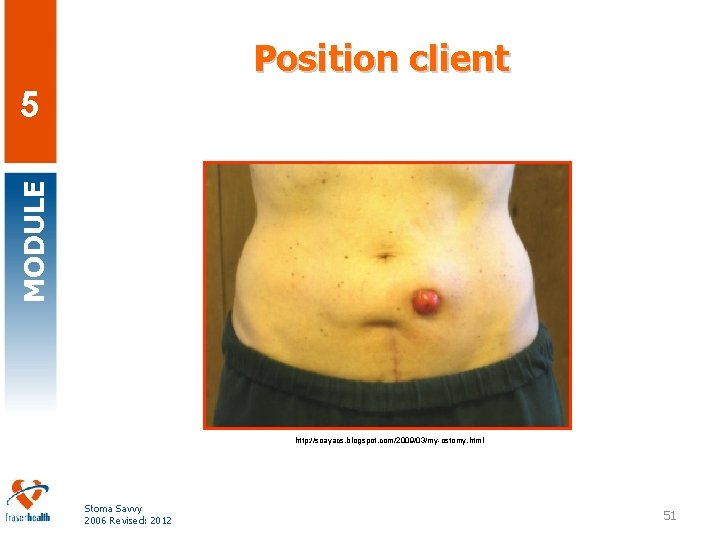
Position client MODULE 5 http: //soayacs. blogspot. com/2009/03/my-ostomy. html Stoma Savvy 2006 Revised: 2012 51

Remove Old Appliance Carefully MODULE 5 Stoma Savvy 2006 Revised: 2012 52
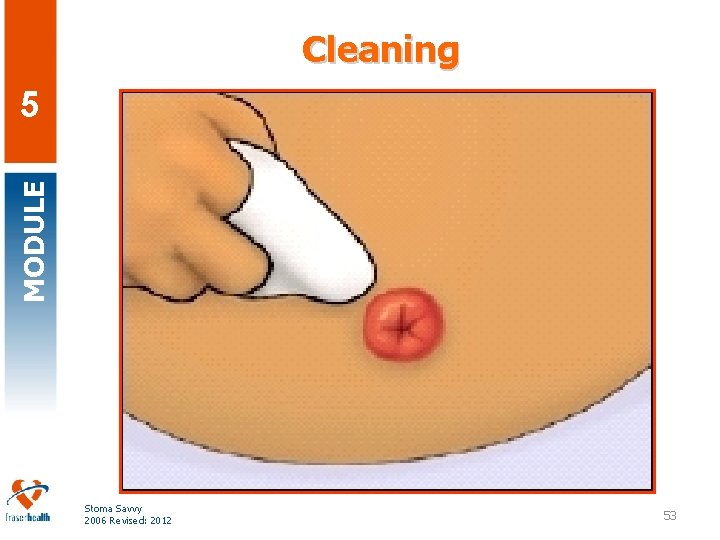
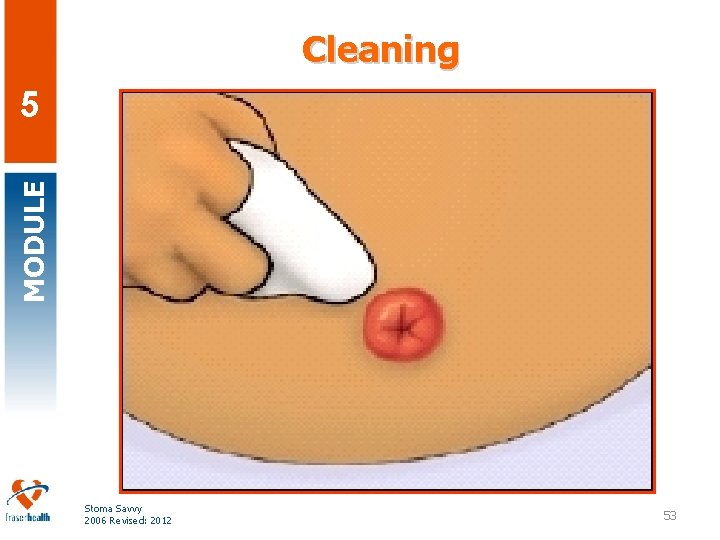
Cleaning MODULE 5 Stoma Savvy 2006 Revised: 2012 53
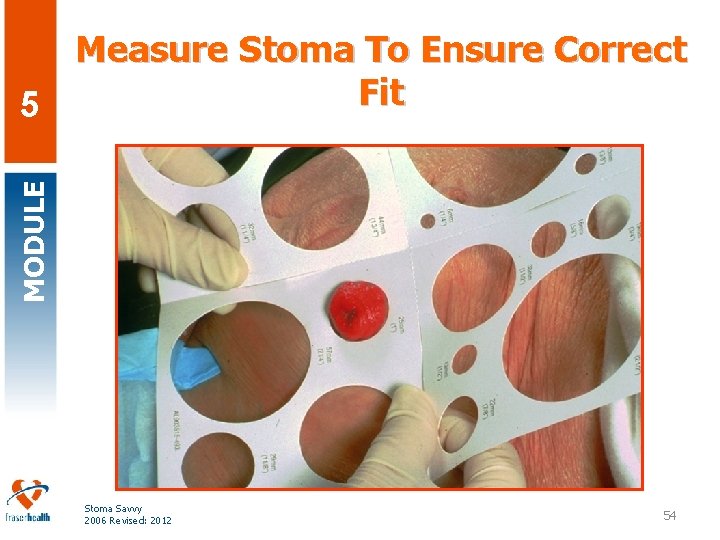
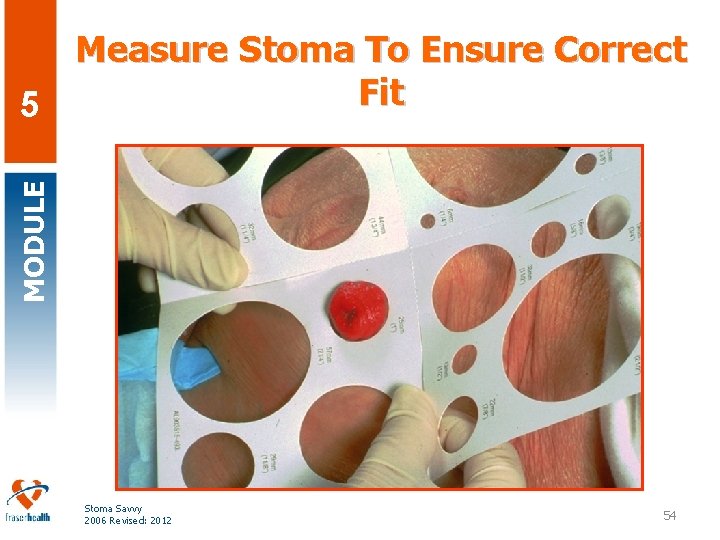
MODULE Measure Stoma To Ensure Correct Fit 5 Stoma Savvy 2006 Revised: 2012 54
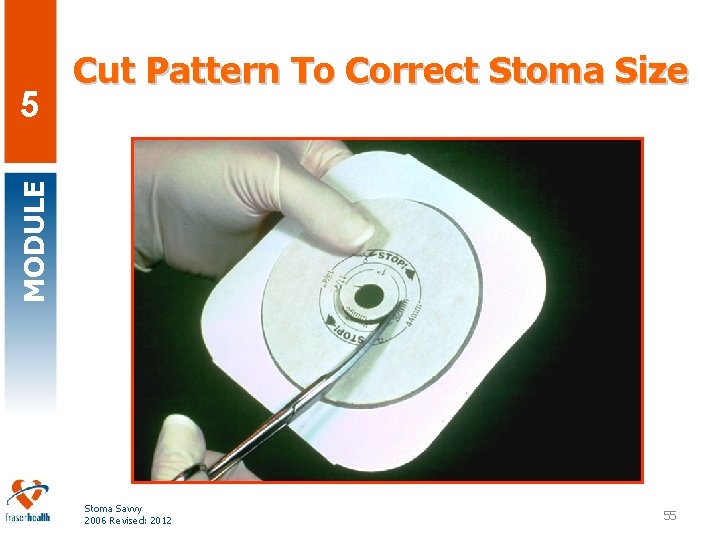
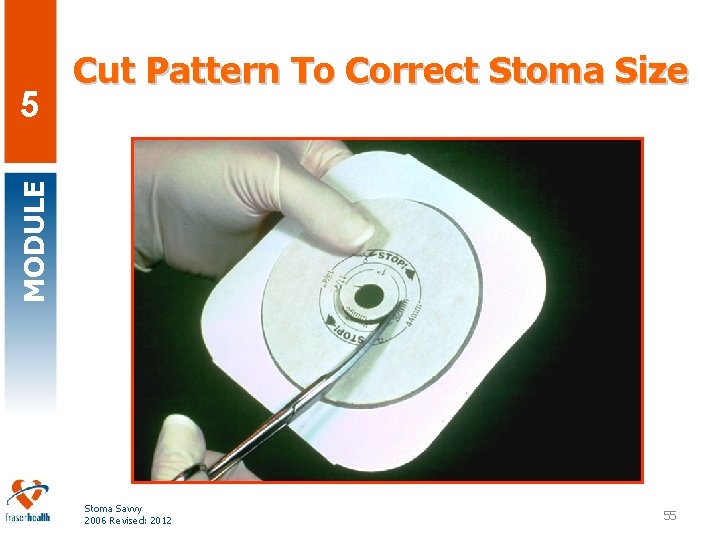
MODULE 5 Cut Pattern To Correct Stoma Size Stoma Savvy 2006 Revised: 2012 55

MODULE 5 Remove Film Backing From Flange Stoma Savvy 2006 Revised: 2012 56
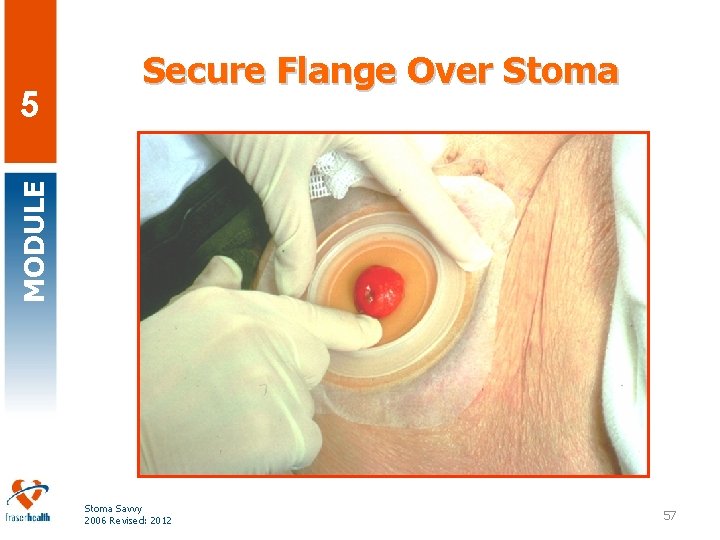
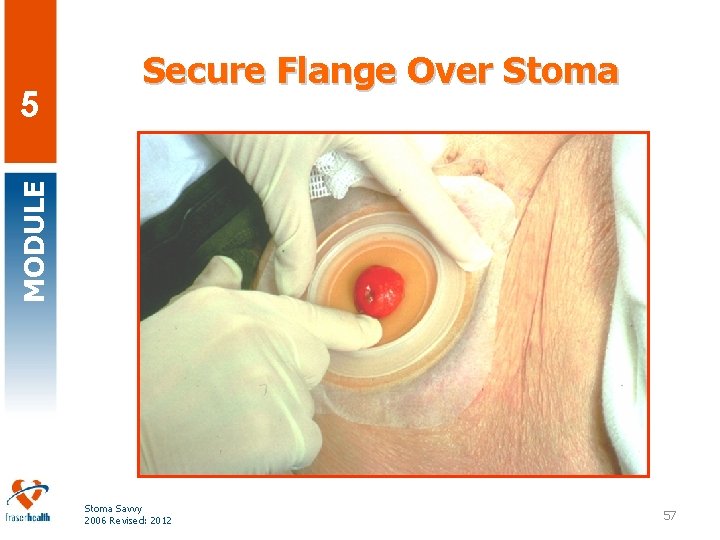
MODULE 5 Secure Flange Over Stoma Savvy 2006 Revised: 2012 57
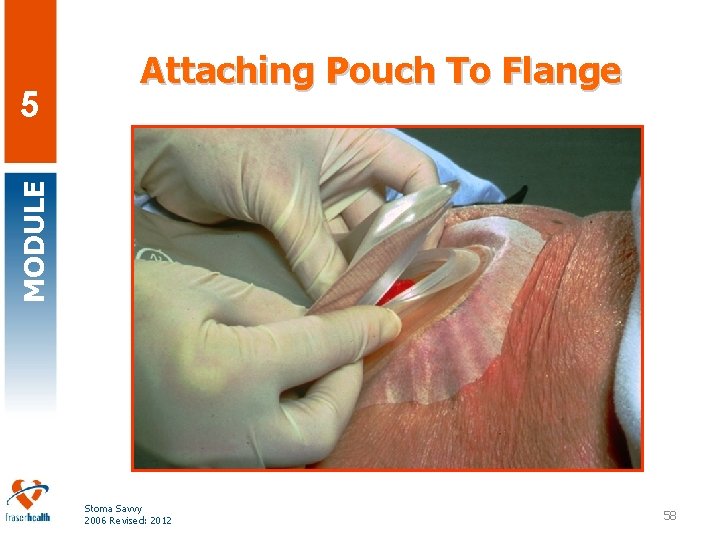
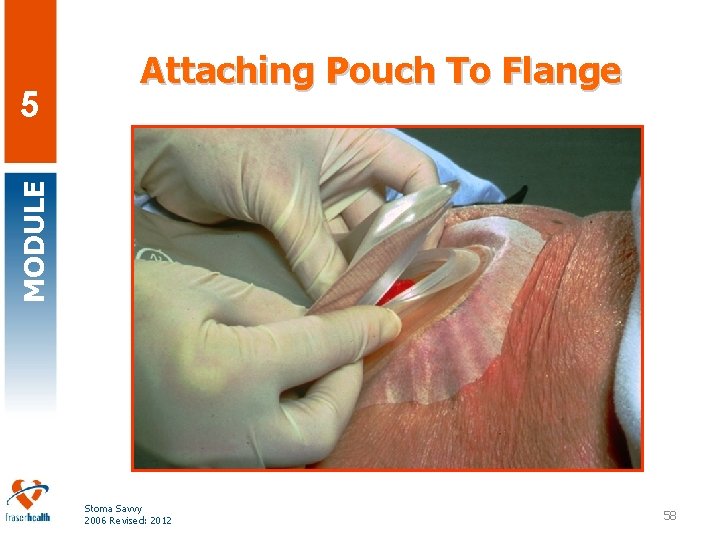
MODULE 5 Attaching Pouch To Flange Stoma Savvy 2006 Revised: 2012 58
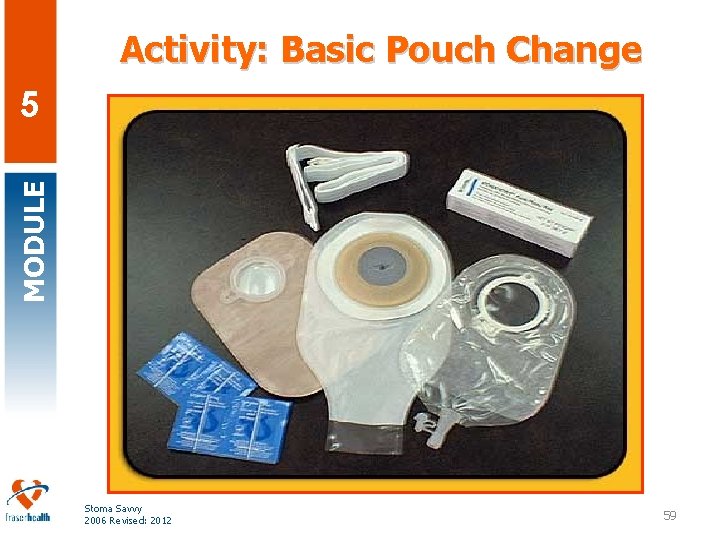
Activity: Basic Pouch Change MODULE 5 Stoma Savvy 2006 Revised: 2012 59
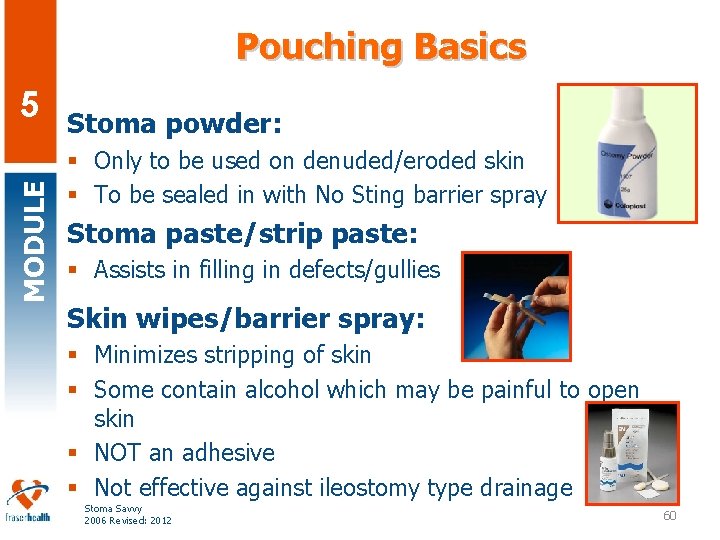
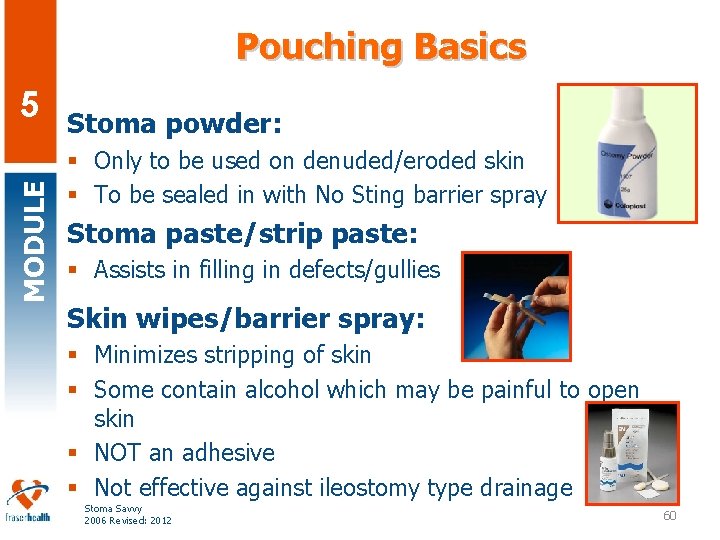
Pouching Basics MODULE 5 Stoma powder: § Only to be used on denuded/eroded skin § To be sealed in with No Sting barrier spray Stoma paste/strip paste: § Assists in filling in defects/gullies Skin wipes/barrier spray: § Minimizes stripping of skin § Some contain alcohol which may be painful to open skin § NOT an adhesive § Not effective against ileostomy type drainage Stoma Savvy 2006 Revised: 2012 60
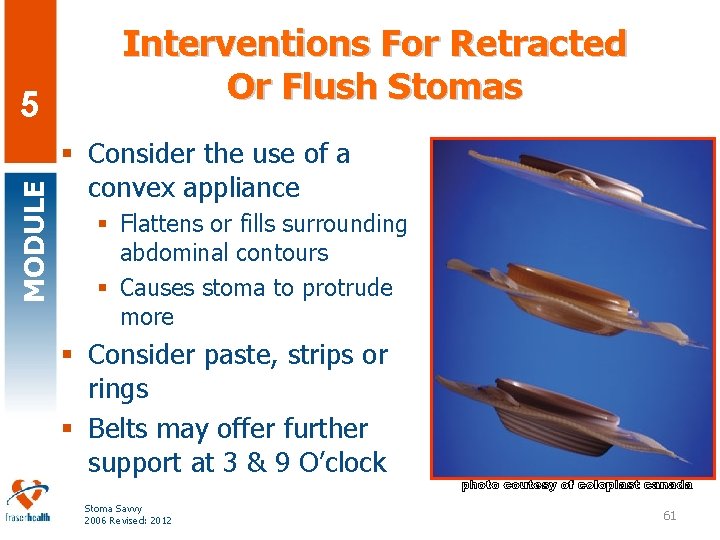
MODULE 5 Interventions For Retracted Or Flush Stomas § Consider the use of a convex appliance § Flattens or fills surrounding abdominal contours § Causes stoma to protrude more § Consider paste, strips or rings § Belts may offer further support at 3 & 9 O’clock Stoma Savvy 2006 Revised: 2012 61
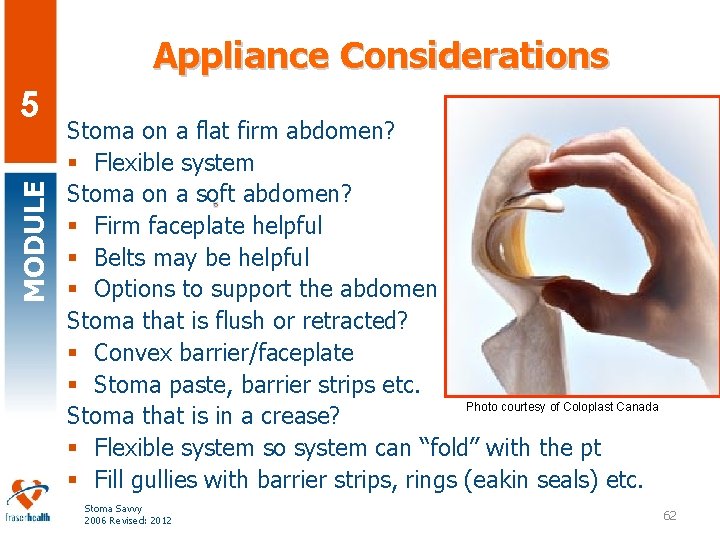
Appliance Considerations MODULE 5 Stoma on a flat firm abdomen? § Flexible system Stoma on a soft abdomen? § Firm faceplate helpful § Belts may be helpful § Options to support the abdomen Stoma that is flush or retracted? § Convex barrier/faceplate § Stoma paste, barrier strips etc. Photo courtesy of Coloplast Canada Stoma that is in a crease? § Flexible system so system can “fold” with the pt § Fill gullies with barrier strips, rings (eakin seals) etc. Stoma Savvy 2006 Revised: 2012 62
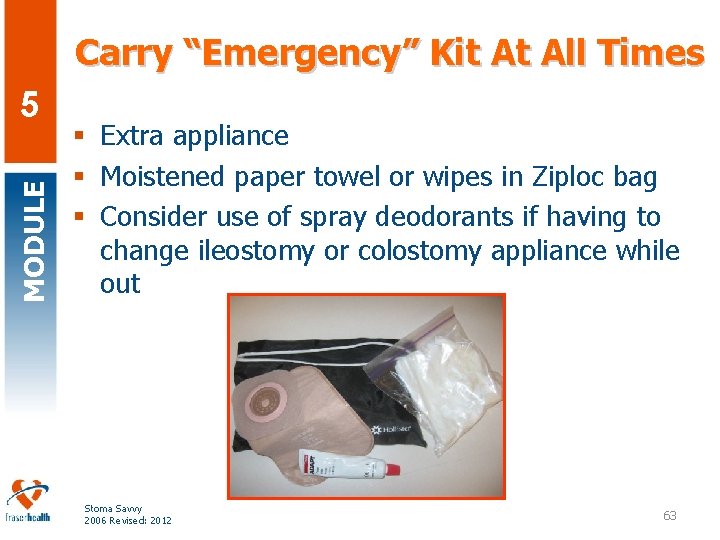
Carry “Emergency” Kit At All Times MODULE 5 § Extra appliance § Moistened paper towel or wipes in Ziploc bag § Consider use of spray deodorants if having to change ileostomy or colostomy appliance while out Stoma Savvy 2006 Revised: 2012 63
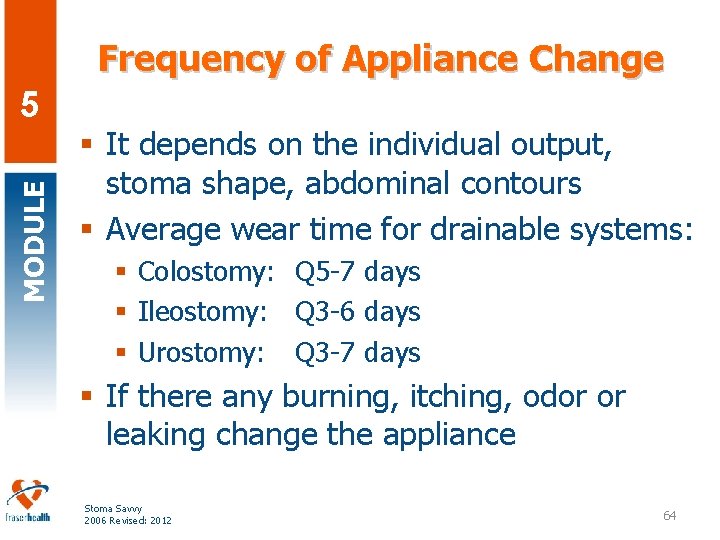
Frequency of Appliance Change MODULE 5 § It depends on the individual output, stoma shape, abdominal contours § Average wear time for drainable systems: § Colostomy: Q 5 -7 days § Ileostomy: Q 3 -6 days § Urostomy: Q 3 -7 days § If there any burning, itching, odor or leaking change the appliance Stoma Savvy 2006 Revised: 2012 64
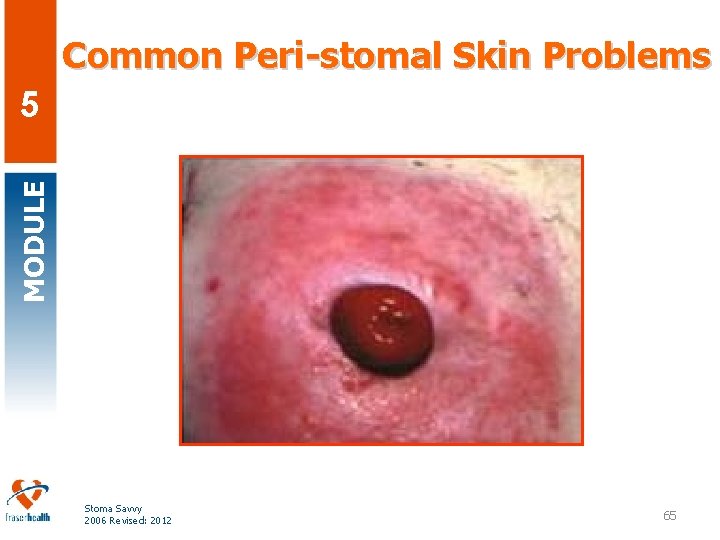
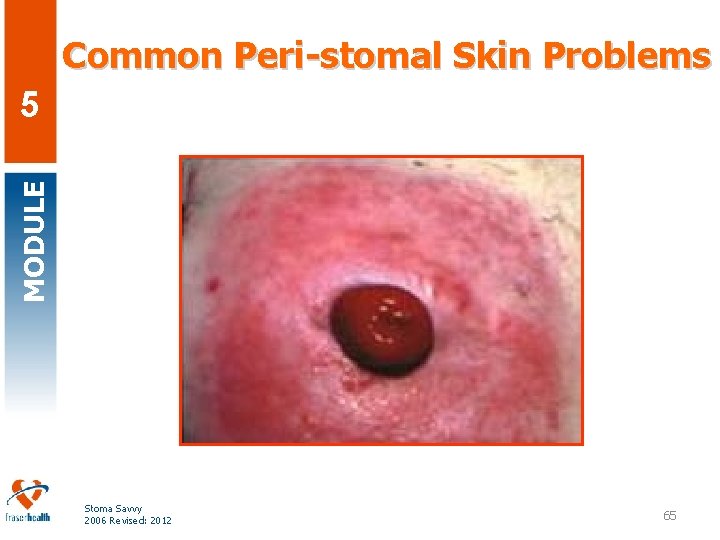
Common Peri-stomal Skin Problems MODULE 5 Stoma Savvy 2006 Revised: 2012 65
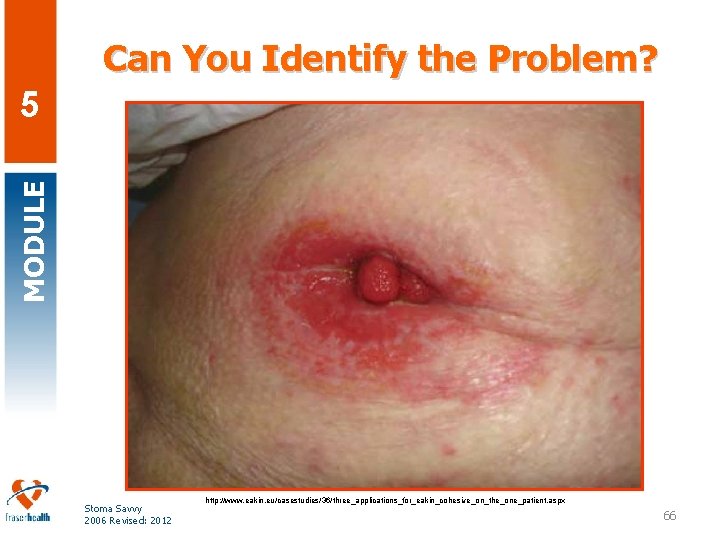
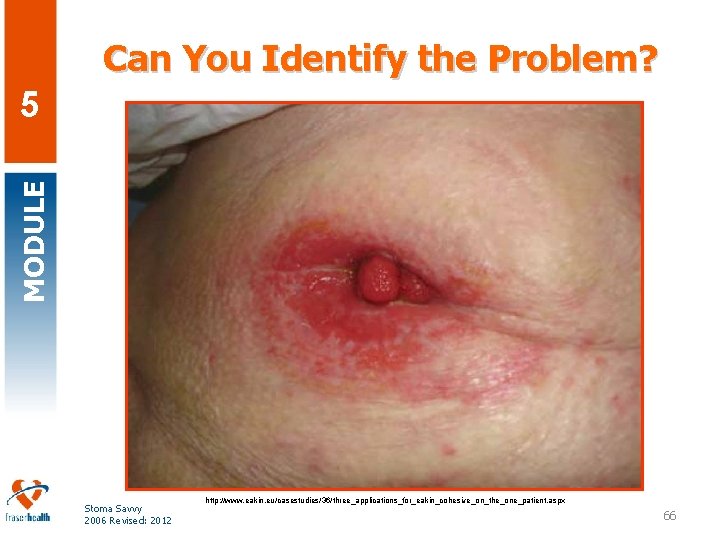
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 http: //www. eakin. eu/casestudies/36/three_applications_for_eakin_cohesive_on_the_one_patient. aspx 66
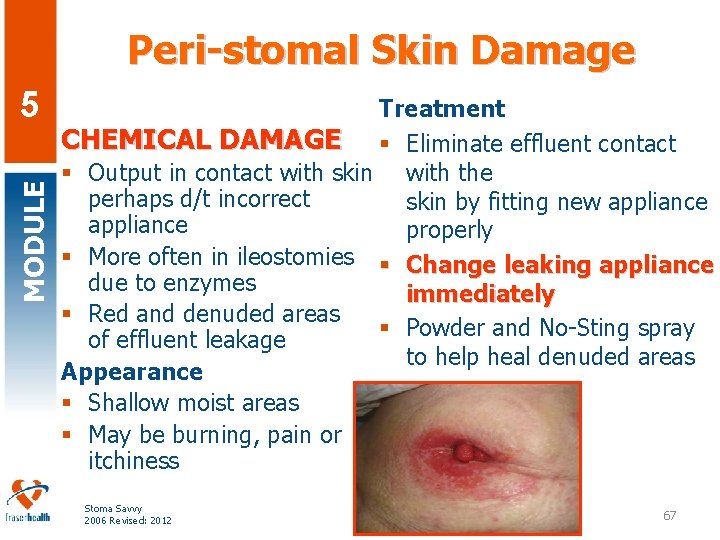
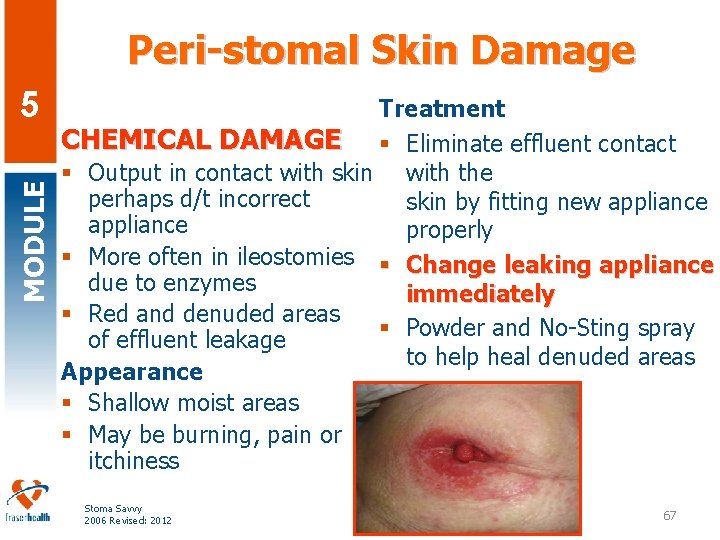
Peri-stomal Skin Damage MODULE 5 Treatment CHEMICAL DAMAGE § Eliminate effluent contact § Output in contact with skin with the perhaps d/t incorrect skin by fitting new appliance properly § More often in ileostomies § Change leaking appliance due to enzymes immediately § Red and denuded areas § Powder and No-Sting spray of effluent leakage to help heal denuded areas Appearance § Shallow moist areas § May be burning, pain or itchiness Stoma Savvy 2006 Revised: 2012 67
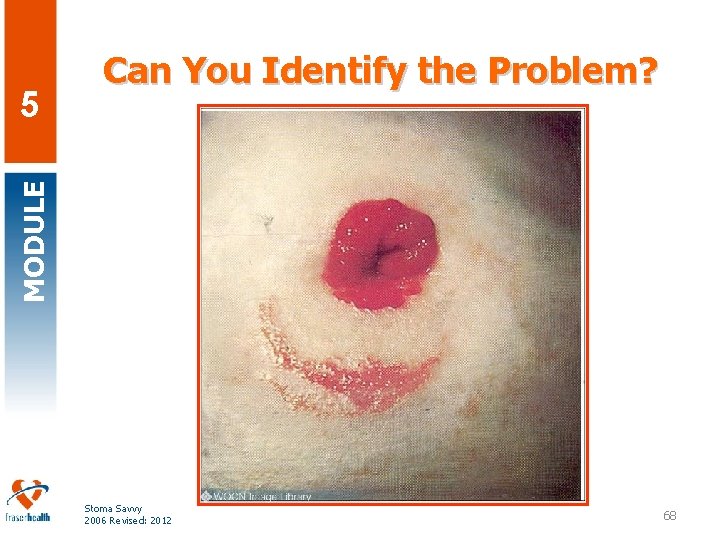
MODULE 5 Can You Identify the Problem? Stoma Savvy 2006 Revised: 2012 68
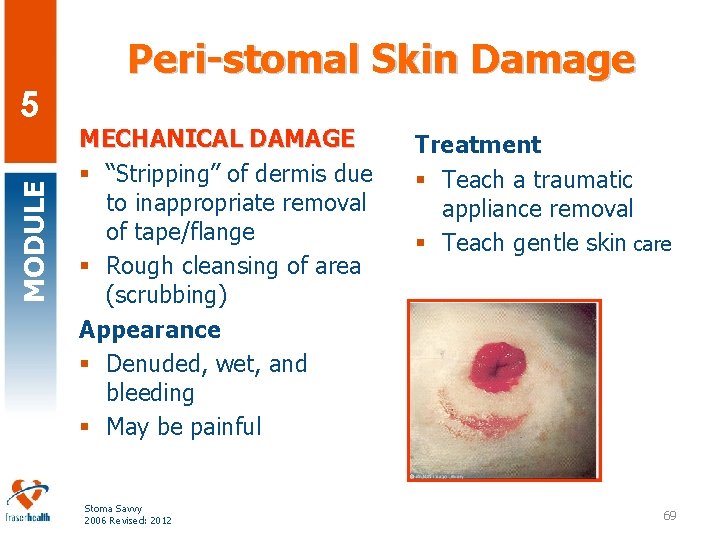
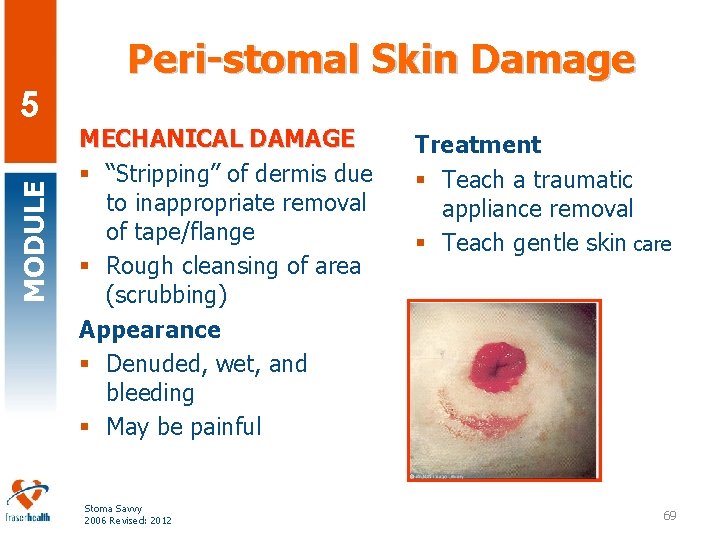
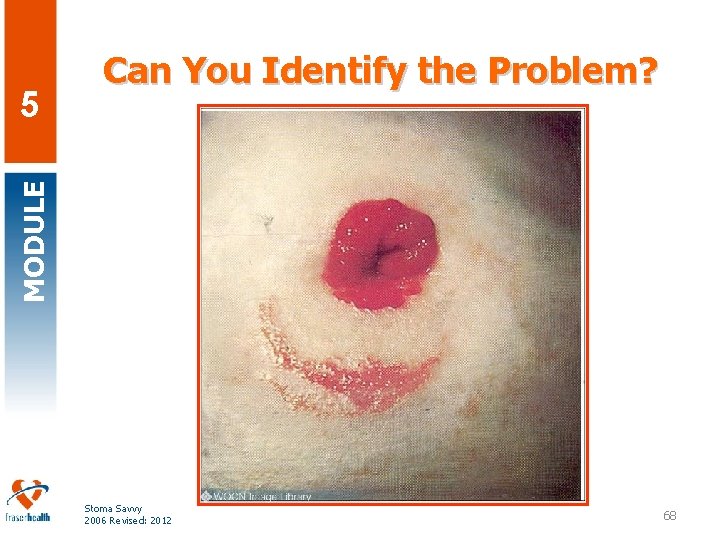
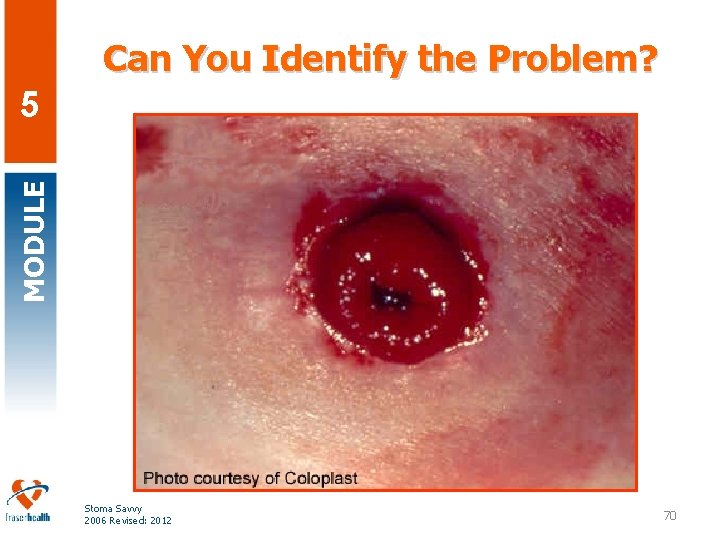
Peri-stomal Skin Damage MODULE 5 MECHANICAL DAMAGE § “Stripping” of dermis due to inappropriate removal of tape/flange § Rough cleansing of area (scrubbing) Appearance § Denuded, wet, and bleeding § May be painful Stoma Savvy 2006 Revised: 2012 Treatment § Teach a traumatic appliance removal § Teach gentle skin care 69
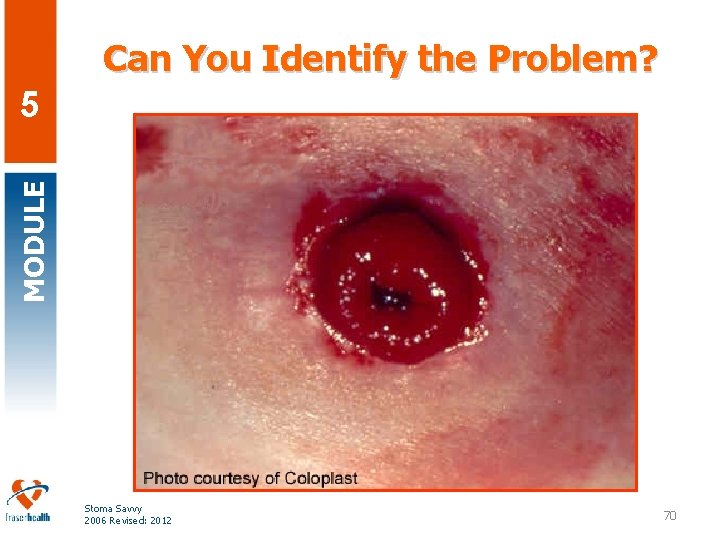
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 70
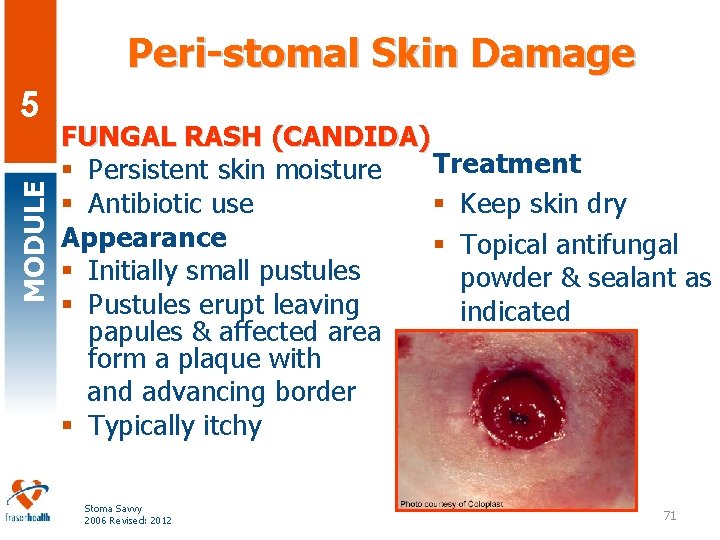
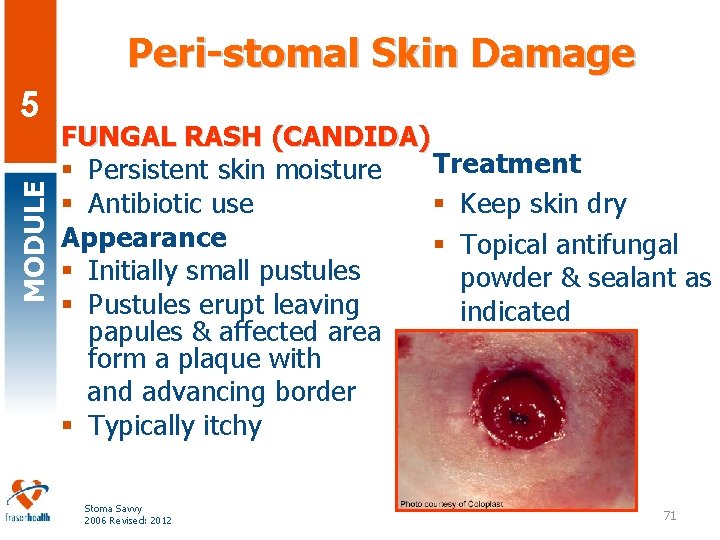
Peri-stomal Skin Damage MODULE 5 FUNGAL RASH (CANDIDA) Treatment § Persistent skin moisture § Antibiotic use § Keep skin dry Appearance § Topical antifungal § Initially small pustules powder & sealant as § Pustules erupt leaving indicated papules & affected area form a plaque with and advancing border § Typically itchy Stoma Savvy 2006 Revised: 2012 71
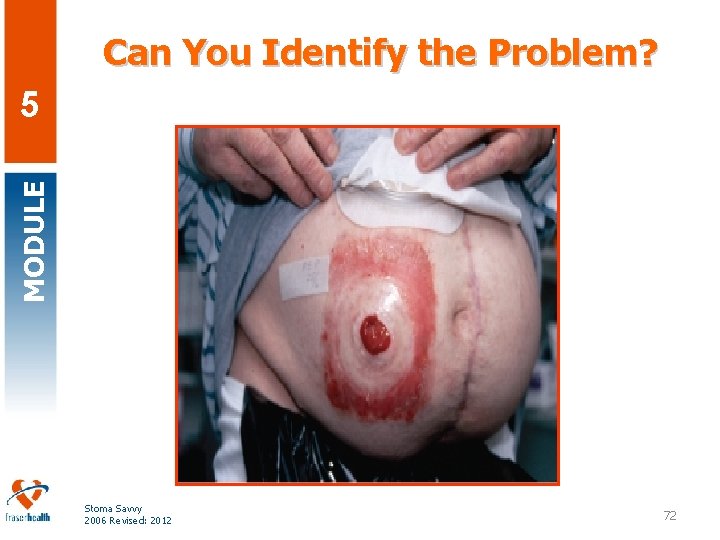
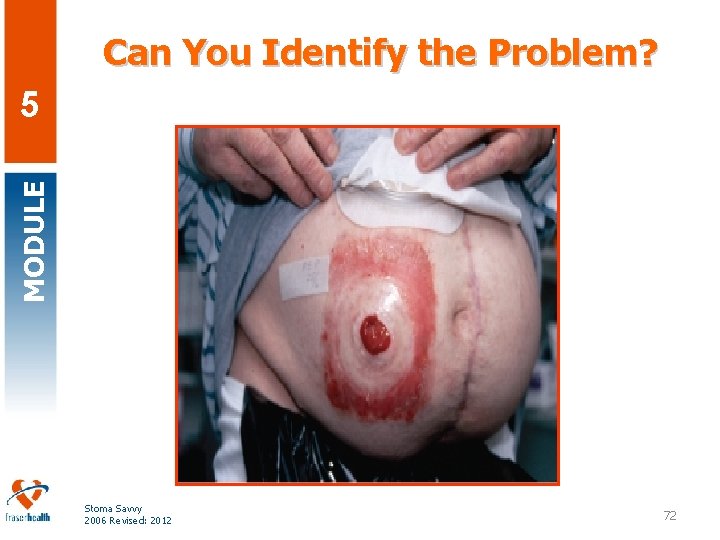
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 72

Peri-stomal Skin Damage MODULE 5 ALLERGIC REACTION § Can be caused by any product § Areas of redness exposed to allergen (e. g. tape) Appearance § “Mirror” the footprint of the offending allergen § Can lead to blistering and weepy skin Stoma Savvy 2006 Revised: 2012 Treatment § Remove allergic source (e. g. use solid wafer § Barrier instead § Corticosteroid agent if needed 73
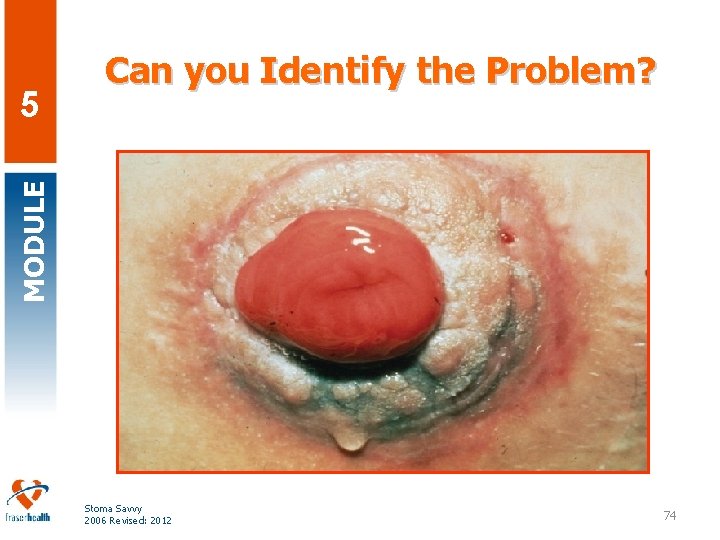
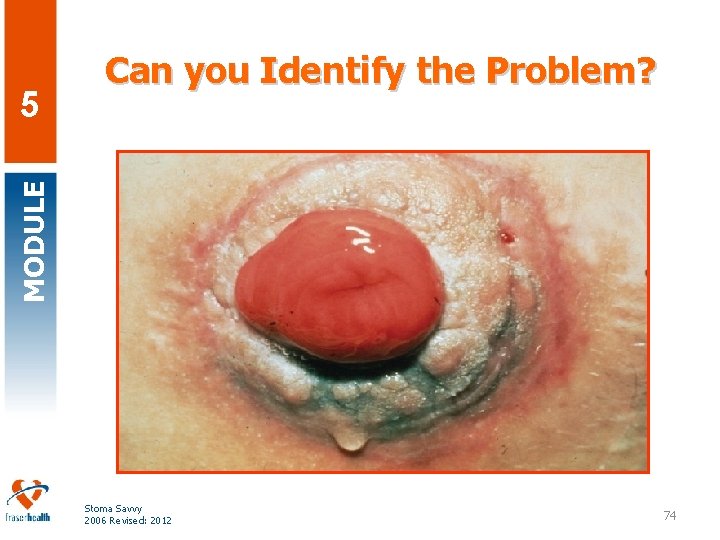
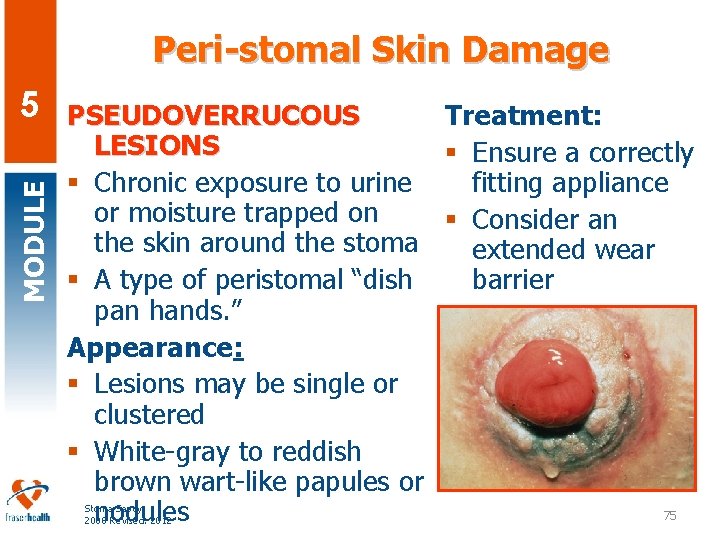
MODULE 5 Can you Identify the Problem? Stoma Savvy 2006 Revised: 2012 74
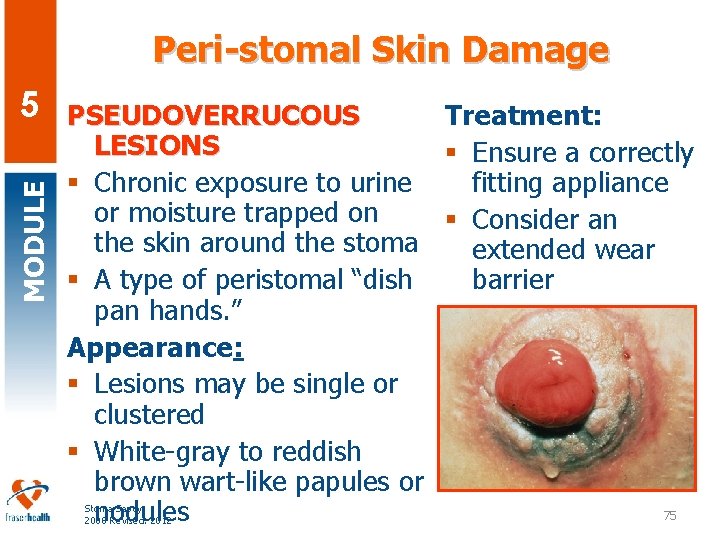
Peri-stomal Skin Damage MODULE 5 Treatment: PSEUDOVERRUCOUS LESIONS § Ensure a correctly fitting appliance § Chronic exposure to urine or moisture trapped on § Consider an the skin around the stoma extended wear barrier § A type of peristomal “dish pan hands. ” Appearance: § Lesions may be single or clustered § White-gray to reddish brown wart-like papules or 75 nodules Stoma Savvy 2006 Revised: 2012
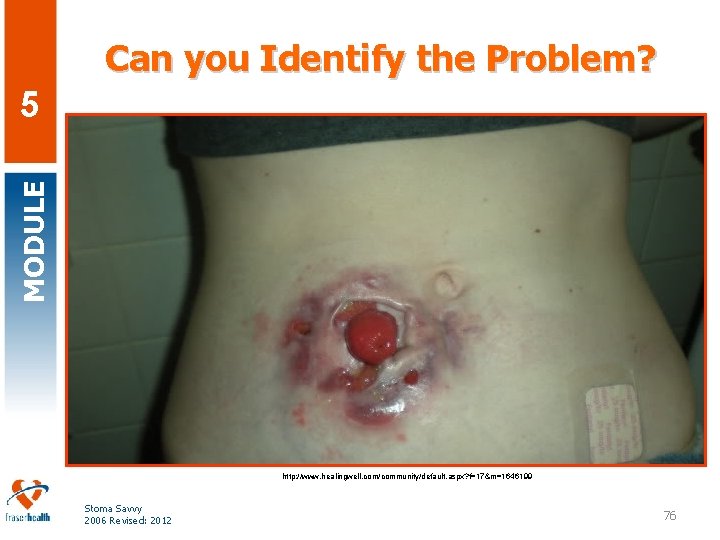
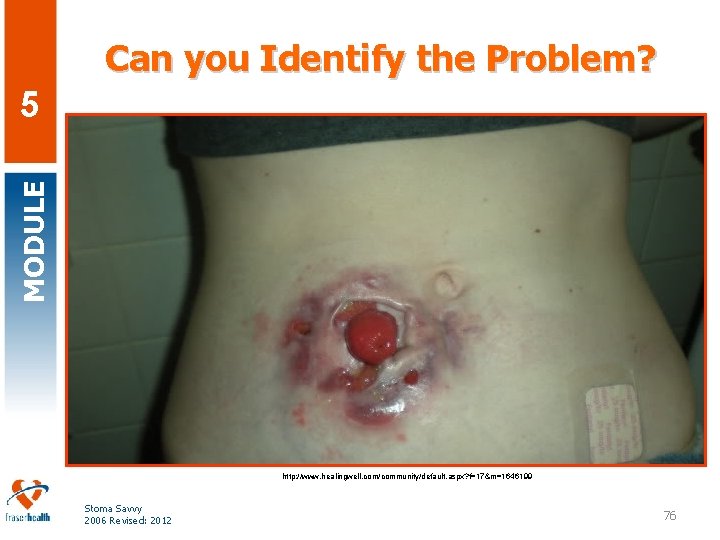
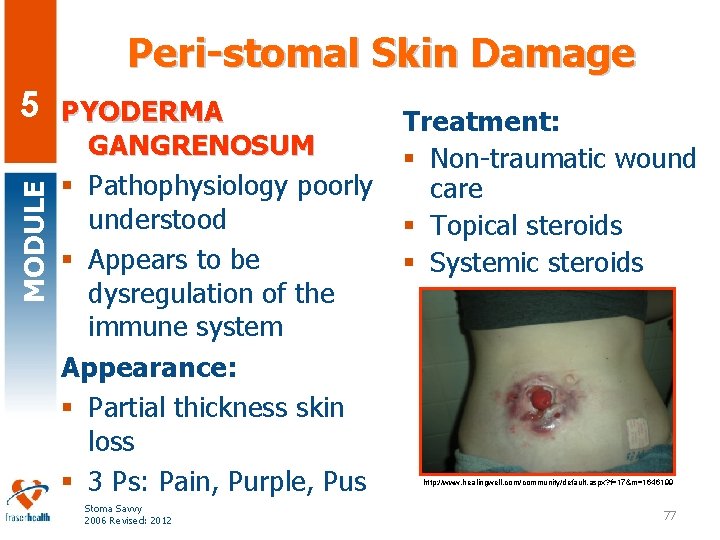
Can you Identify the Problem? MODULE 5 http: //www. healingwell. com/community/default. aspx? f=17&m=1646199 Stoma Savvy 2006 Revised: 2012 76
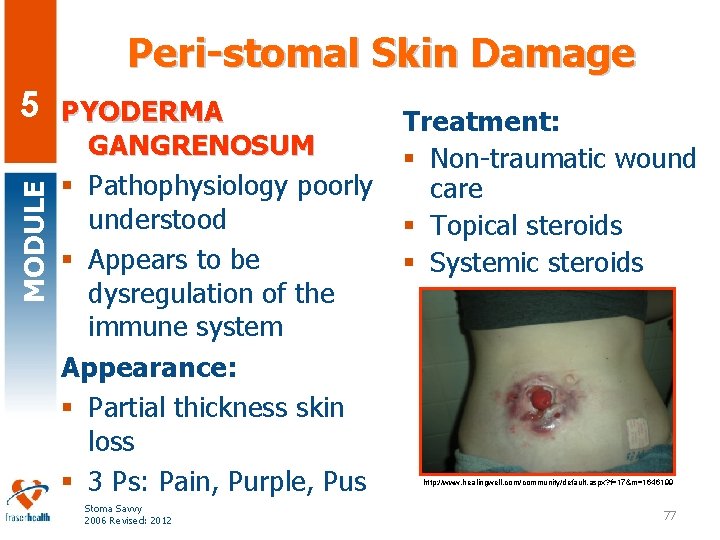
Peri-stomal Skin Damage MODULE 5 PYODERMA GANGRENOSUM § Pathophysiology poorly understood § Appears to be dysregulation of the immune system Appearance: § Partial thickness skin loss § 3 Ps: Pain, Purple, Pus Stoma Savvy 2006 Revised: 2012 Treatment: § Non-traumatic wound care § Topical steroids § Systemic steroids http: //www. healingwell. com/community/default. aspx? f=17&m=1646199 77
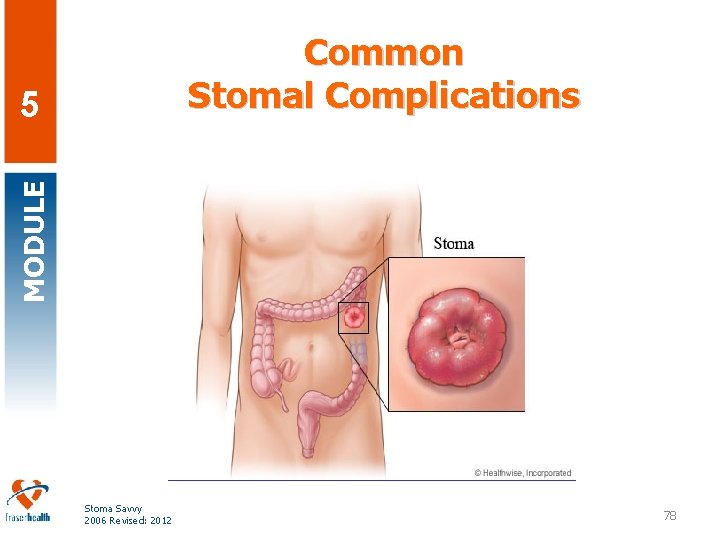
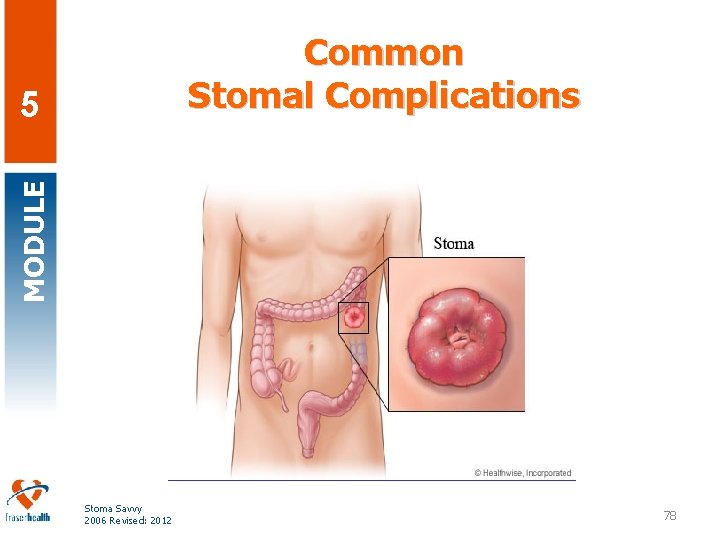
Common Stomal Complications MODULE 5 Stoma Savvy 2006 Revised: 2012 78
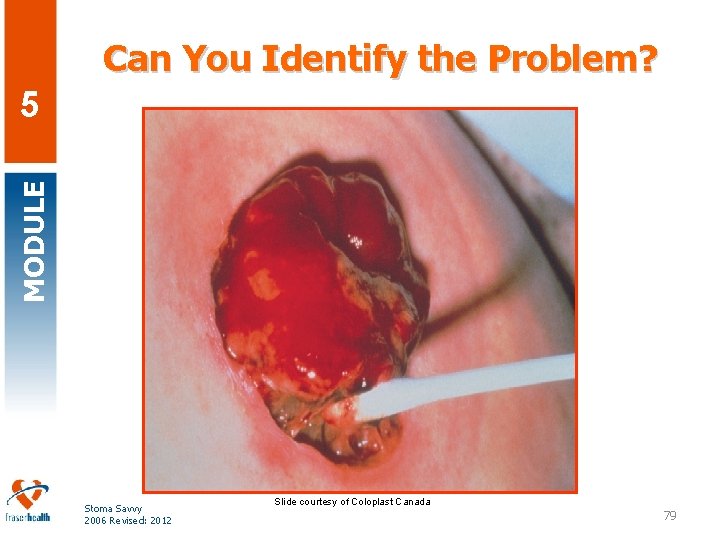
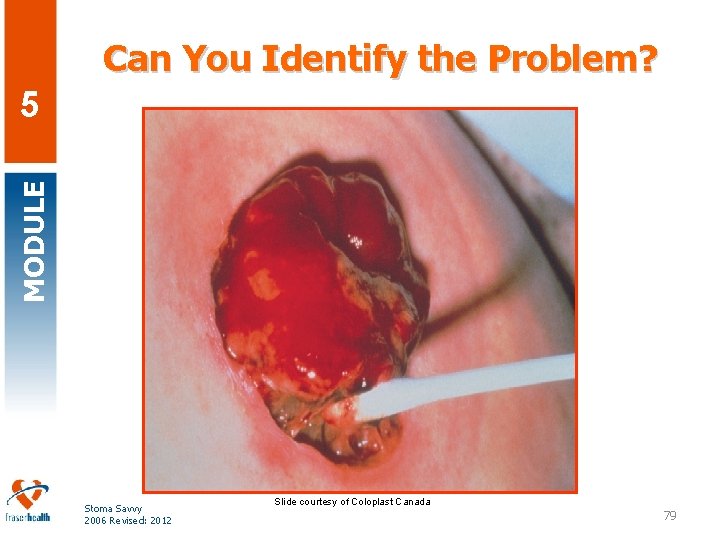
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 Slide courtesy of Coloplast Canada 79
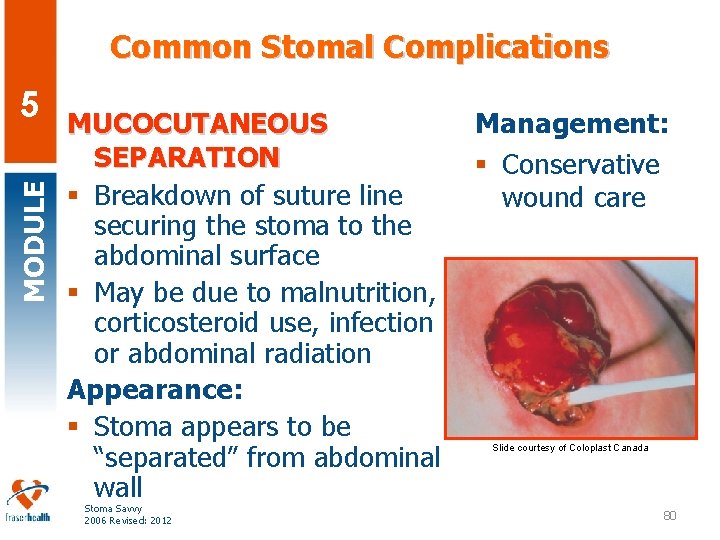
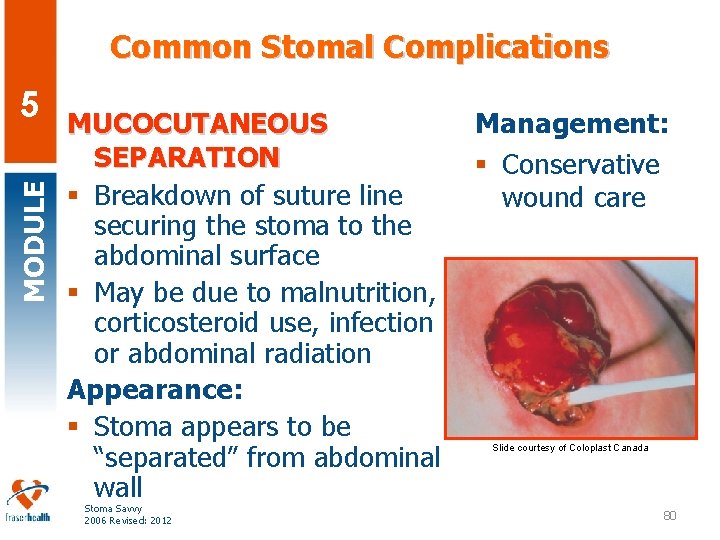
Common Stomal Complications MODULE 5 MUCOCUTANEOUS SEPARATION § Breakdown of suture line securing the stoma to the abdominal surface § May be due to malnutrition, corticosteroid use, infection or abdominal radiation Appearance: § Stoma appears to be “separated” from abdominal wall Stoma Savvy 2006 Revised: 2012 Management: § Conservative wound care Slide courtesy of Coloplast Canada 80
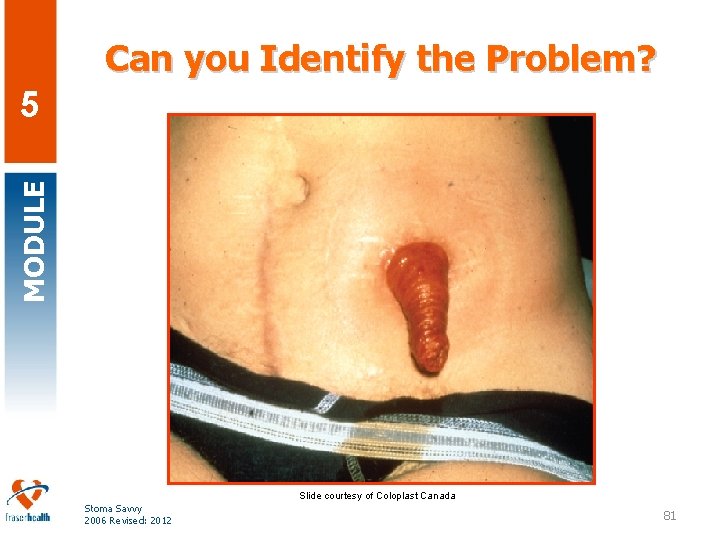
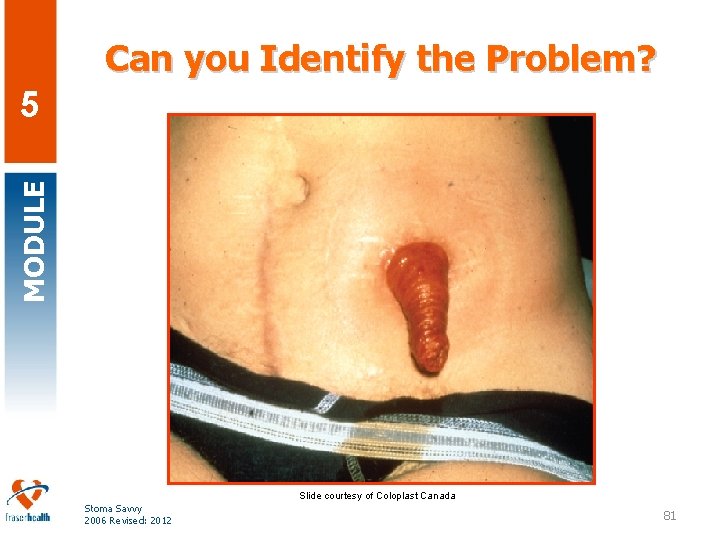
Can you Identify the Problem? MODULE 5 Slide courtesy of Coloplast Canada Stoma Savvy 2006 Revised: 2012 81
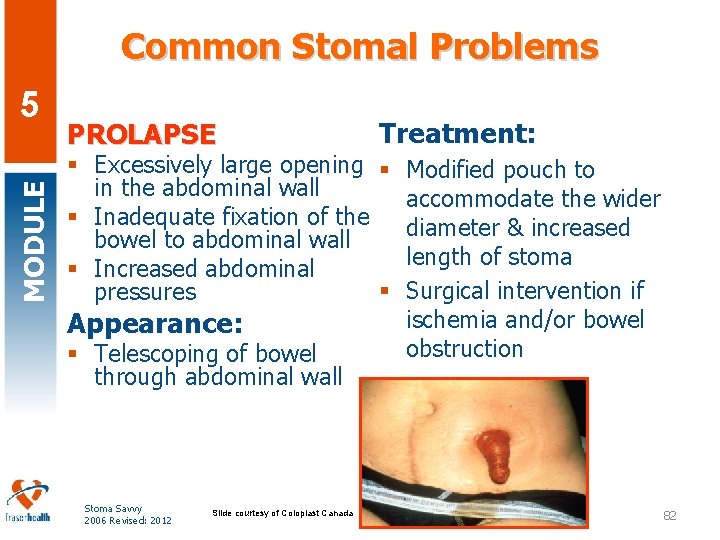
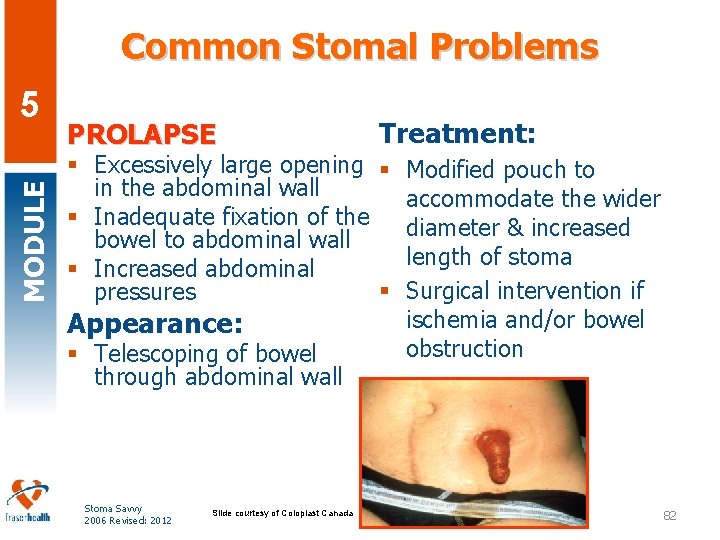
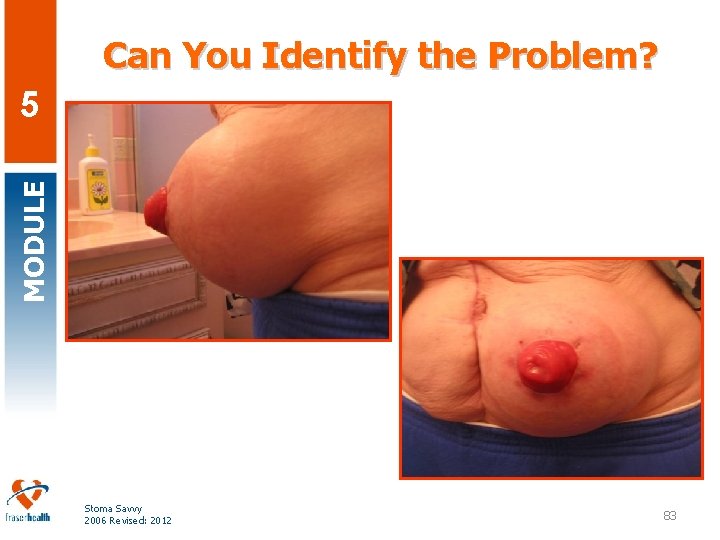
Common Stomal Problems MODULE 5 PROLAPSE Treatment: § Excessively large opening § Modified pouch to in the abdominal wall accommodate the wider § Inadequate fixation of the diameter & increased bowel to abdominal wall length of stoma § Increased abdominal § Surgical intervention if pressures ischemia and/or bowel Appearance: obstruction § Telescoping of bowel through abdominal wall Stoma Savvy 2006 Revised: 2012 Slide courtesy of Coloplast Canada 82
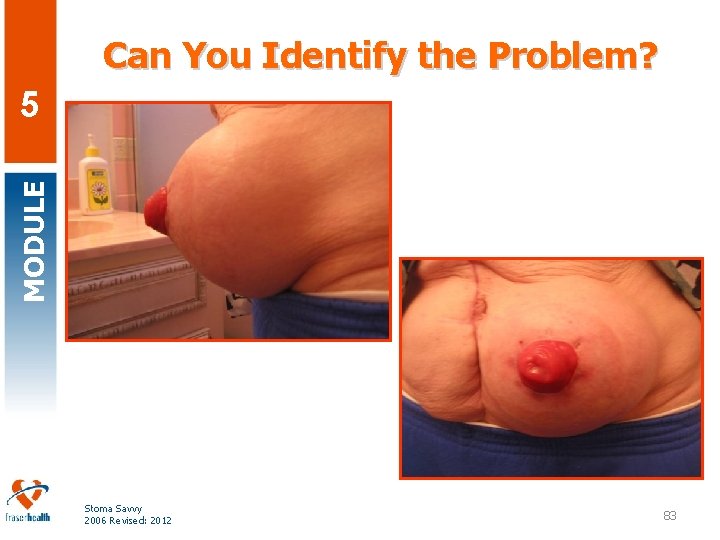
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 83
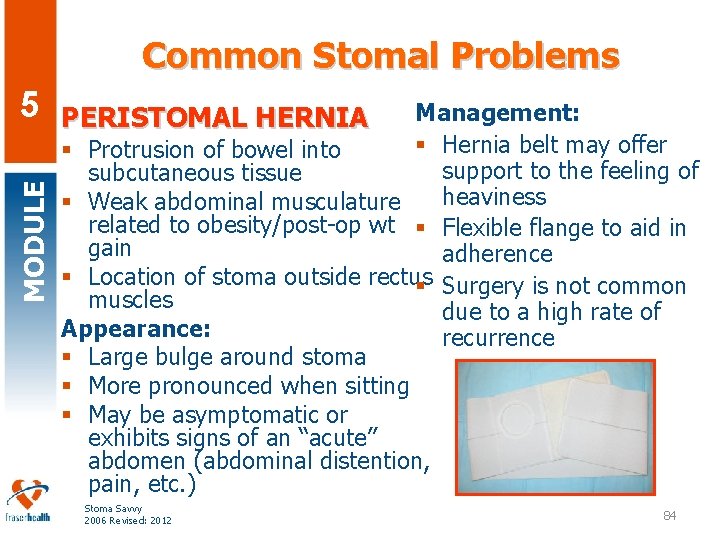
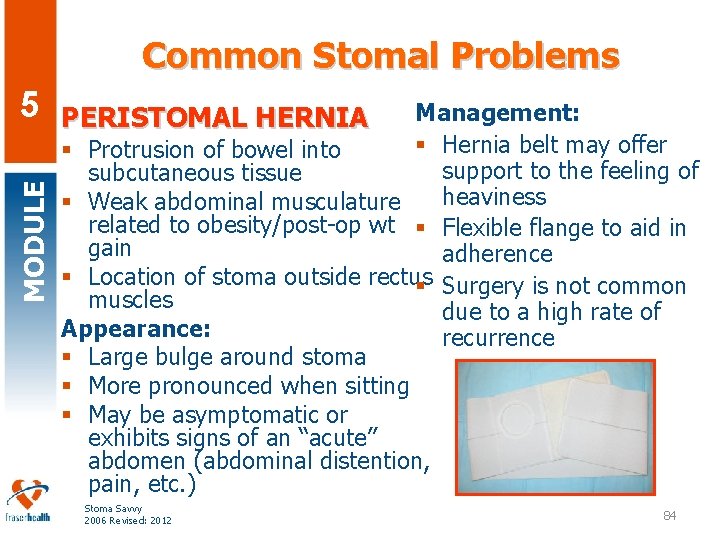
Common Stomal Problems MODULE 5 Management: § Hernia belt may offer § Protrusion of bowel into support to the feeling of subcutaneous tissue heaviness § Weak abdominal musculature related to obesity/post-op wt § Flexible flange to aid in gain adherence § Location of stoma outside rectus § Surgery is not common muscles due to a high rate of Appearance: recurrence § Large bulge around stoma § More pronounced when sitting § May be asymptomatic or exhibits signs of an “acute” abdomen (abdominal distention, pain, etc. ) PERISTOMAL HERNIA Stoma Savvy 2006 Revised: 2012 84
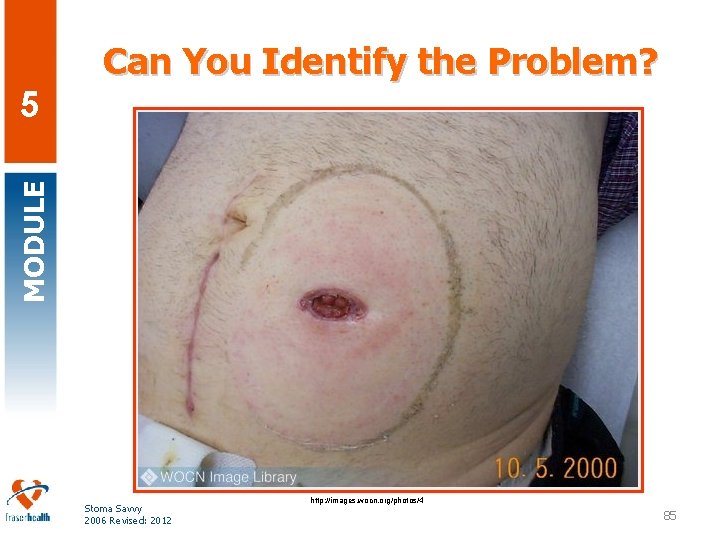
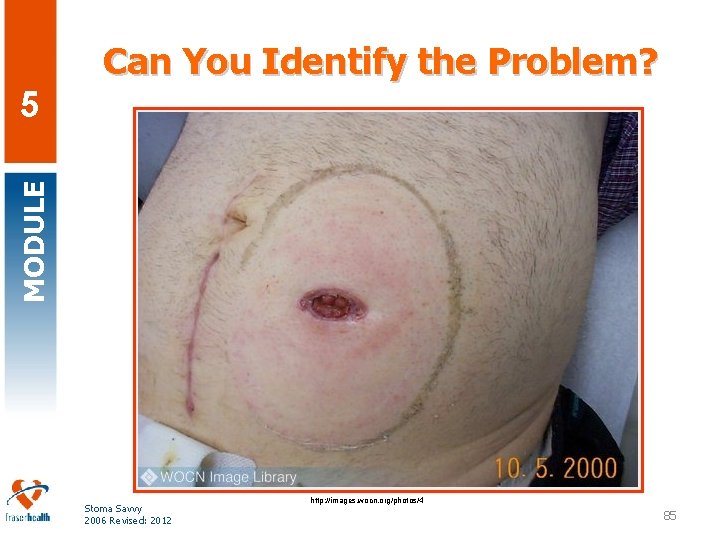
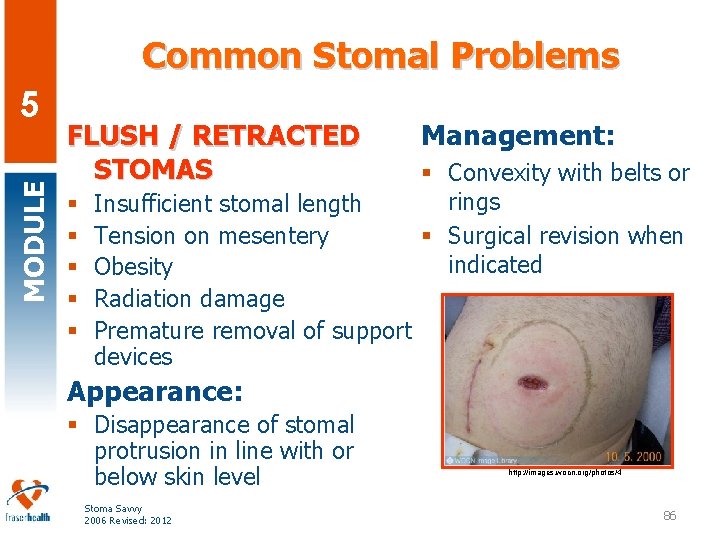
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 http: //images. wocn. org/photos/4 85
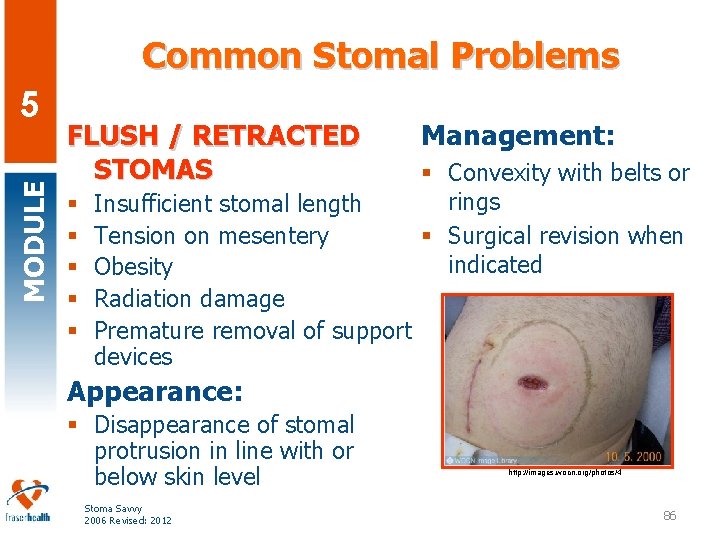
Common Stomal Problems MODULE 5 FLUSH / RETRACTED STOMAS § § § Insufficient stomal length Tension on mesentery Obesity Radiation damage Premature removal of support devices Management: § Convexity with belts or rings § Surgical revision when indicated Appearance: § Disappearance of stomal protrusion in line with or below skin level Stoma Savvy 2006 Revised: 2012 http: //images. wocn. org/photos/4 86
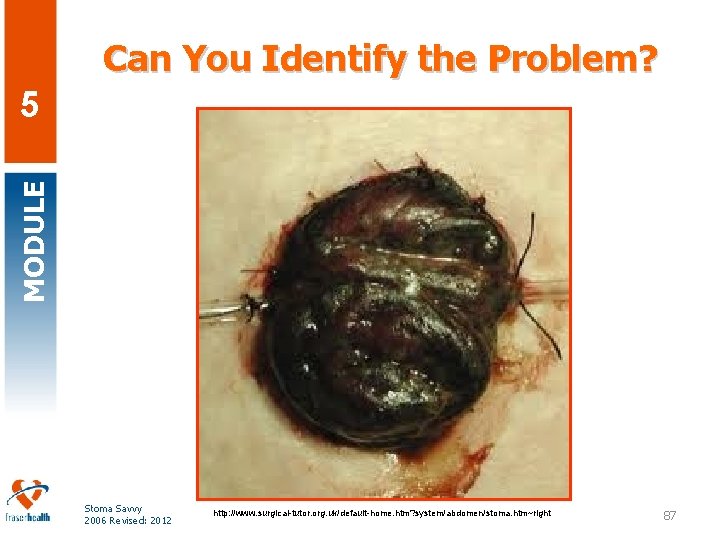
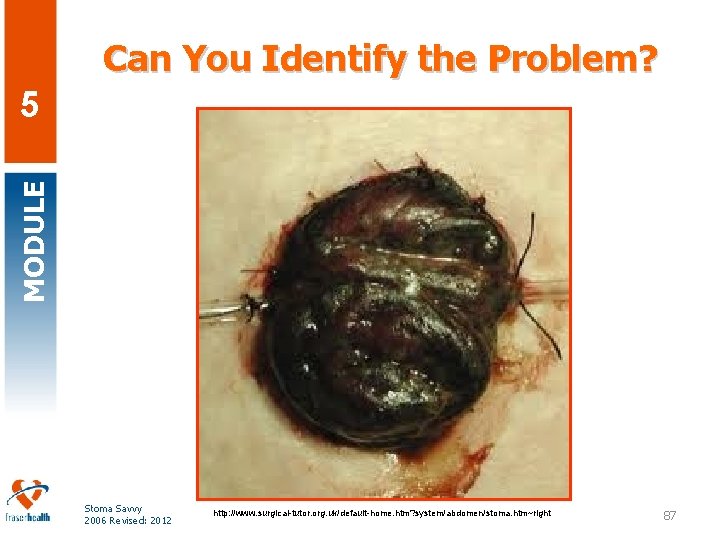
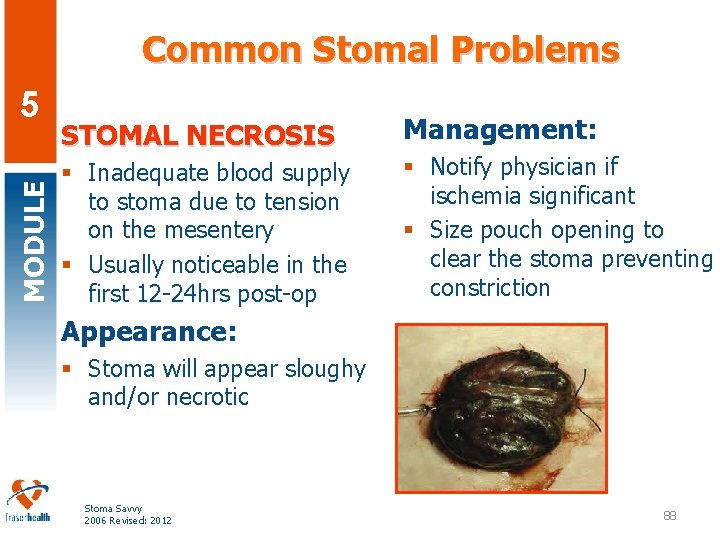
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 http: //www. surgical-tutor. org. uk/default-home. htm? system/abdomen/stoma. htm~right 87
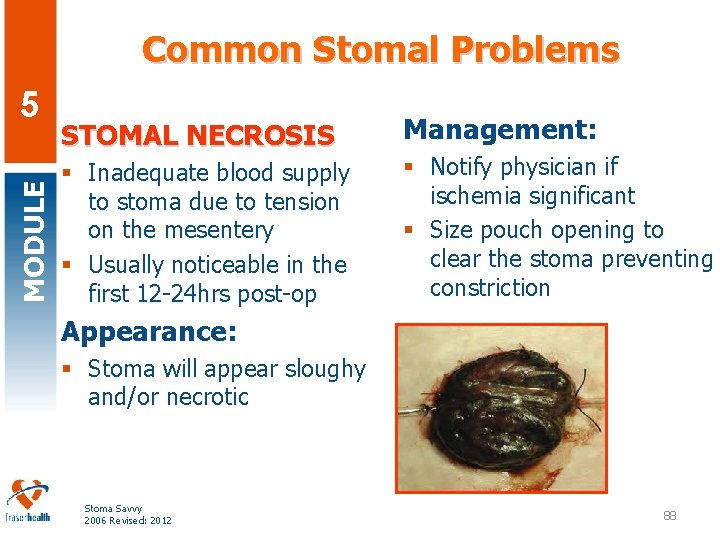
Common Stomal Problems MODULE 5 STOMAL NECROSIS § Inadequate blood supply to stoma due to tension on the mesentery § Usually noticeable in the first 12 -24 hrs post-op Management: § Notify physician if ischemia significant § Size pouch opening to clear the stoma preventing constriction Appearance: § Stoma will appear sloughy and/or necrotic Stoma Savvy 2006 Revised: 2012 88
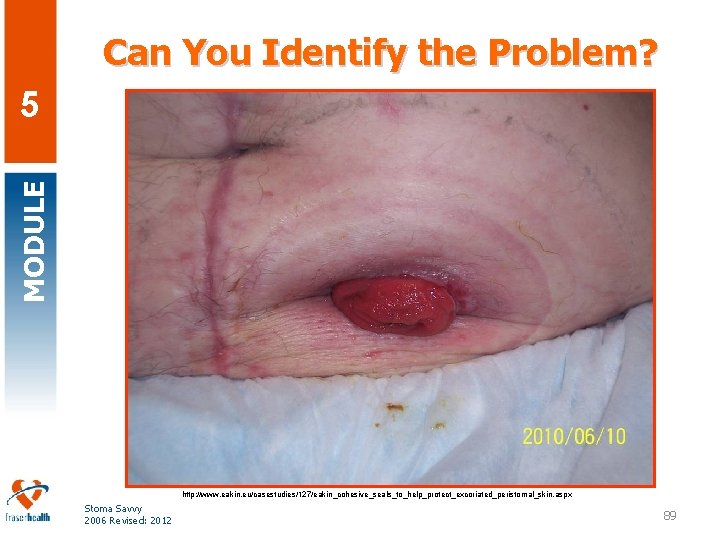
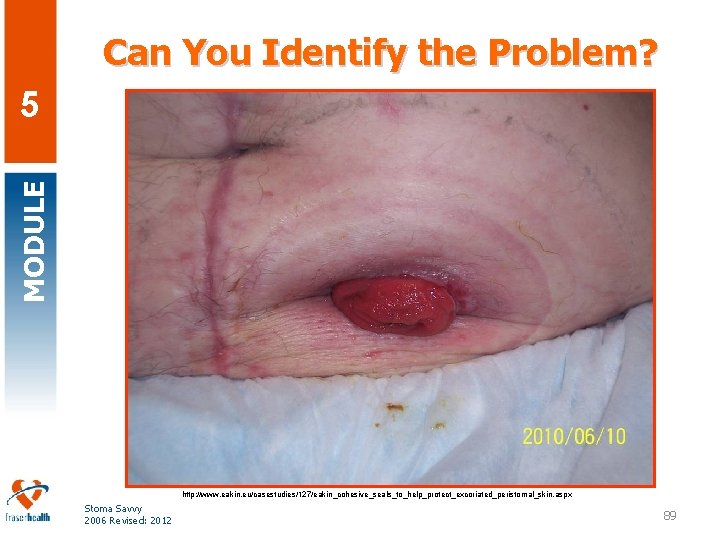
Can You Identify the Problem? MODULE 5 http: //www. eakin. eu/casestudies/127/eakin_cohesive_seals_to_help_protect_excoriated_peristomal_skin. aspx Stoma Savvy 2006 Revised: 2012 89
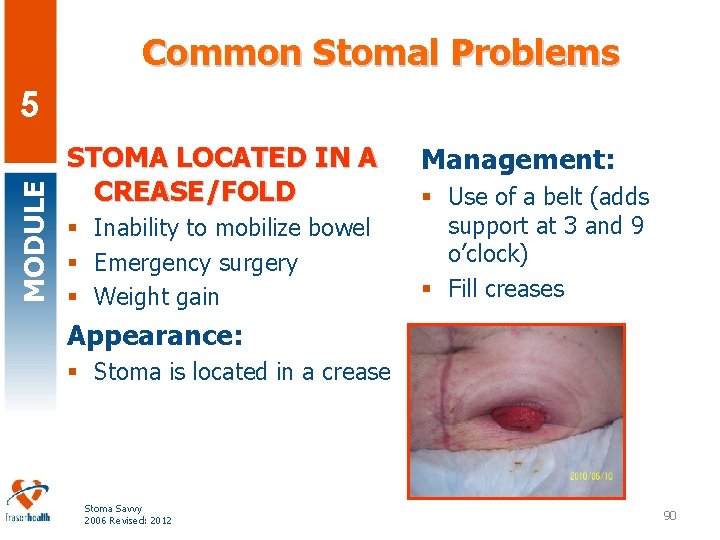
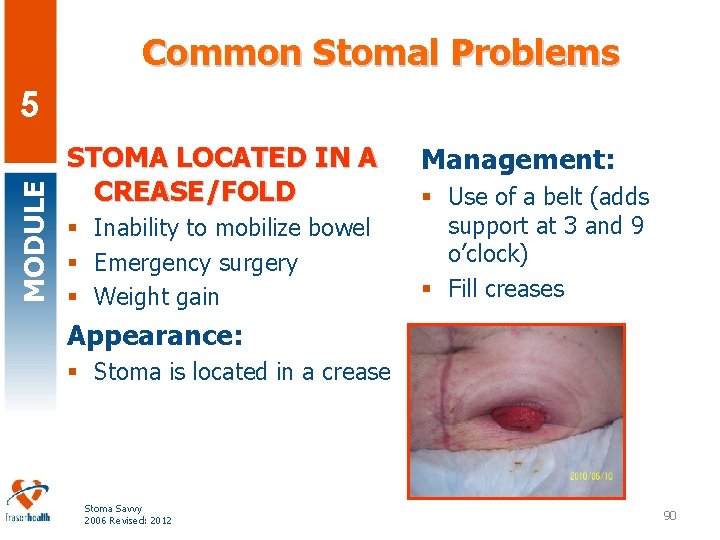
Common Stomal Problems MODULE 5 STOMA LOCATED IN A CREASE/FOLD § Inability to mobilize bowel § Emergency surgery § Weight gain Management: § Use of a belt (adds support at 3 and 9 o’clock) § Fill creases Appearance: § Stoma is located in a crease Stoma Savvy 2006 Revised: 2012 90
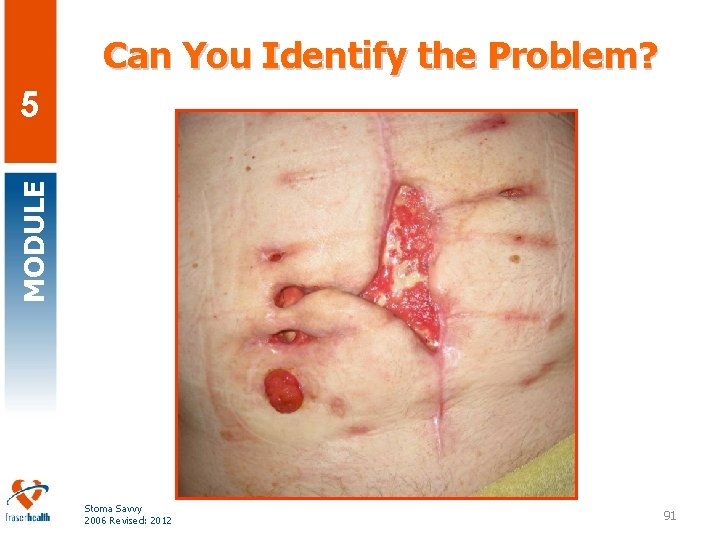
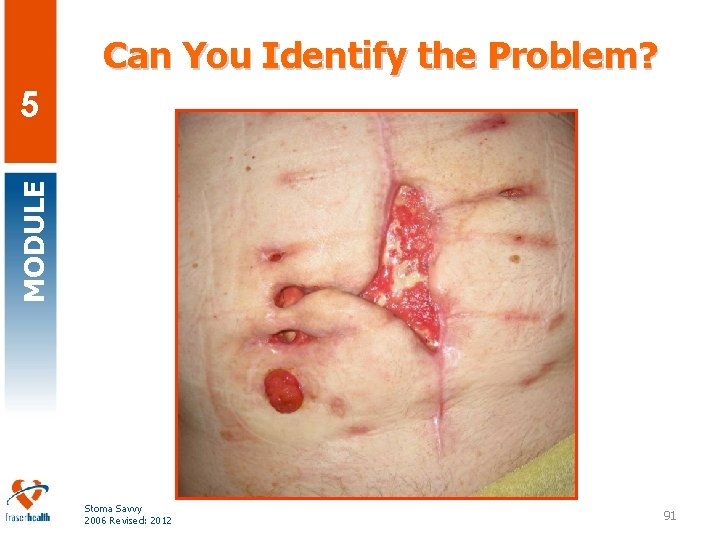
Can You Identify the Problem? MODULE 5 Stoma Savvy 2006 Revised: 2012 91
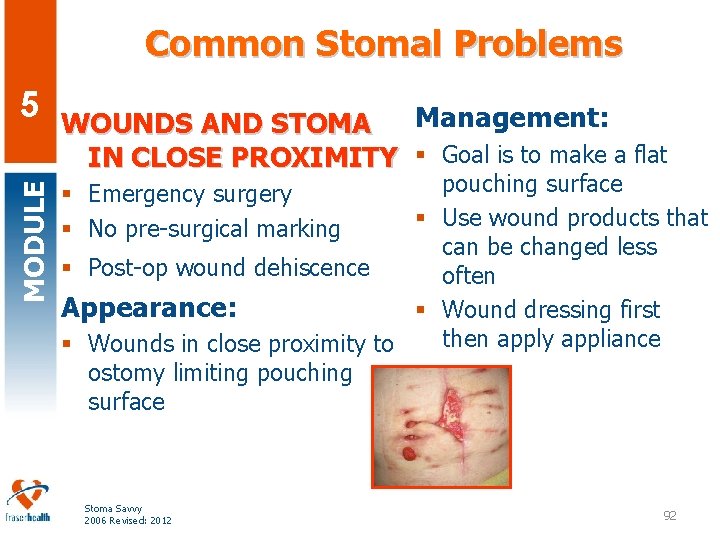
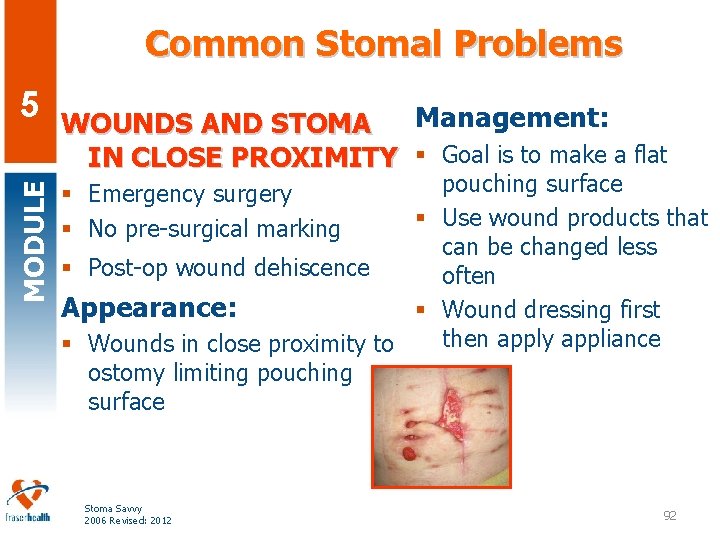
Common Stomal Problems MODULE 5 Management: WOUNDS AND STOMA IN CLOSE PROXIMITY § Goal is to make a flat pouching surface § Use wound products that can be changed less § Post-op wound dehiscence often Appearance: § Wound dressing first then apply appliance § Wounds in close proximity to ostomy limiting pouching surface § Emergency surgery § No pre-surgical marking Stoma Savvy 2006 Revised: 2012 92
MODULE 5 Stoma Savvy 2006 Revised: 2012
Summary MODULE 5 § Reviewed anatomy/physiology of GI & GU systems § Identified types of ostomies: fecal, and urinary diversions § Identified related dietary and hydration concerns § Discussed psychosocial considerations for persons with new ostomy § Explored basic ostomy management § Identified principles of ostomy product selection § Reviewed types of peristomal skin problems & their management § Reviewed stomal complications & their management Stoma Savvy 2006 Revised: 2012 94
Case Study “A” MODULE 5 § Mr. S is a 58 yr old male recently discharged with a new loop ileostomy. He was diagnosed with colon cancer and had a low anterior resection with a temporary ileostomy. He was taught how to empty his pouch but not how to change it. § Mr. S states the hospital nurses told him he didn’t have to learn the appliance change and that a nurse will assist in appliance changes at each visit. He reports he has been adding tape to reinforce the appliance, and his skin is burning. § He has lots of questions: when the stoma can be reversed? What can he eat? Can he go jogging? When can he go back to work? Stoma Savvy 2006 Revised: 2012 95

Case Study “A” MODULE 5 § What are some other topics you might discuss with Mr. S on your first visit? § What about last visit prior to discharge from Home Health? Stoma Savvy 2006 Revised: 2012 96
Case Study “B” MODULE 5 § Ms. J is a 29 year old acute care patient with Crohn’s disease and a new ileostomy. She is four days post op. § The nurse reports having to change the appliance 3 -4 times a day. § Ms. J has been on Prednisone long term for treatment of her Crohn’s. § Ms. J reports losing 30 lbs in the last 3 months. Stoma Savvy 2006 Revised: 2012 97
Case Study “B’ MODULE 5 § What is the problem? § What are the contributing factors? § How would be treat this? § What kind of pouching system would we consider? Stoma Savvy 2006 Revised: 2012 98
Stoma Savvy Education Module SWT MODULE 5 Tanya French, WCC/WOCN, Maple Ridge Home Health Corrine Out, WCC, New Westminster Home Health Kristina Cantafio, WOCN, Vancouver General Hospital Susan Andrews, WCC/WOCN, Royal Columbia Hospital Jenne Brett, CNE, Eagle Ridge Manor Lindsay Hobin, Dietitian, Abbotsford Regional Hospital and Cancer Center § Marine Chan, CNS – Skin Wound Care, Home Health § § § Stoma Savvy 2006 Revised: 2012 99
Questions? MODULE 5 Stoma Savvy 2006 Revised: 2012
MODULE 5 Stoma Savvy 2006 Revised: 2012 101
References MODULE 5 § Hampton, B. G. , Bryant, R. (1992). Ostomies and Continent Diversions. Nursing Management. St. Louis: Mosby. § RNAO Best Practice Guidelines (2009) www. rnao. org § Wound, Ostomy, and Continence Nursing Education Program (2002). Ostomy and Continent Diversions module (2 nd revision). Atlanta, GA: Emory University. § Wound Ostomy and Continence Nurses Society (2004). Basic Ostomy Skin Care. Glenview, IL: Authour § United Ostomy Association of Canada § www. ostomycanada. ca § Coloplast Canada § www. coloplast. ca § Eddins, C. W. , Scarano, K. , Willcutts, K. (2005) Ostomies and Fistulas: A Collaborative Approach. Nutrition Series in Gastroenterology, series #33. Stoma Savvy 2006 Revised: 2012 102
On-line Resources MODULE 5 § The Canadian Association of Enterostomal Therapy http: //www. caet. ca § CAWC Canadian Association for Wound Care. http: //www. cawc. net/ § CL’ck site: Connecting Learners with Knowledge. Provincial Guideline: Assessment & Treatment of Diabetic & Neuropathic Ulcers in Adults http: //www. clck. ca § RNAO Registered Nurses Association of Ontario Clinical Practice Guidelines. http: //www. rnao. org Stoma Savvy 2006 Revised: 2012 103
5 Realization of the Fraser Health Regional Wound Education to enhance skin wound care for our clients is attributed to the selfless dedication of: MODULE Acknowledgment § § § § Dr. Nigel Murray, President & CEO Lynda Foley, Executive Director Sandra Geddes, Director Catherine Barnardo, Director Sheree Hudson, Manager Cindy Robertson, QI Consultant Sylvia Jansen, Education Coordinator Jody Lewis, Education Assistant Brenda Stewart, Program Assistant Vendors, Advanced Wound Products Doris Gilbert/Judy Rousseau, HSSBC Hospital Community Foundations Print Shop Stoma Savvy 2006 Revised: 2012 n n n n n Donna Tyson & Tanya French, HH WCCs Skin Integrity Wound Management Steering Committee Regional Skin Wound (SW) Clinical Working Team Nursing Practice Professional Council Integrated Partnership Practice Council Maneet Samra, PPI Consultant Allied Health Skin Wound Task Force Provincial Nurses’ SW Committee Marie Scott, Brigitee Gutierrez, Raj Dhillon, Reveena Gill (Langara students ) & Suki Grewel, Instructor Patsy Lam, Dr Mc. Pherson & Bruce Kennedy, Palliative End-of-Life Program 104