Steroid hormone synthesis Steroidogenesis Conversion of cholesterol into
- Slides: 31
Steroid hormone synthesis
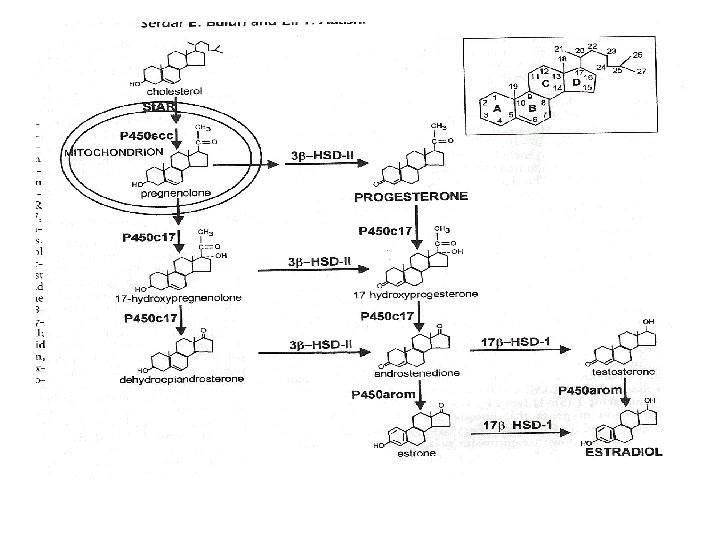
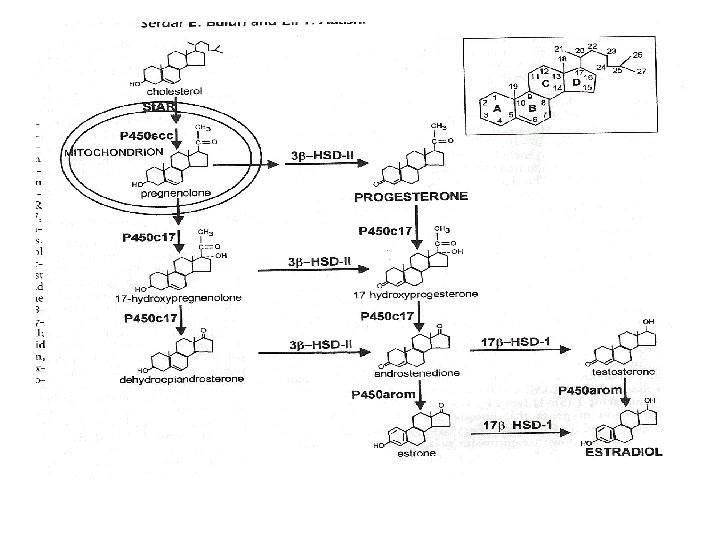
Steroidogenesis • Conversion of cholesterol into hormones – Chemical modification • Ring formation • Reduction of ketone to alcohol – Structural modification • Removal of carbon side-chains
Site of steroidogenesis • Mitochondria – Uptake of cholesterol • Circulation – Lipoproteins • De Novo synthesis – Side-chain cleavage • Production of pregnenolone (P 5) – From 27 -C molecule to 21 -C molecule
• Cytoplasm – Conversion of P 5 to progesterone (P 4) • C-21 steroids – Conversion of progestigens to androgens • C-21 steroids to C-19 steroids – Conversion of androgens to estrogens • C-19 steroids to C-18 steroids • Armatization of the sterol ring
Steroidogenic cells • Male – Leydig cells • Testosterone production – Sertoli cells • Estradiol production • Females – Theca cells • Androgen production – Granulosa cells • Estradiol production – Progesterone production by both theca and granulosa cells
Two-cell, two-gonadotropin theory • Ovarian steroidogenesis – LH acts on theca cells to produce androgens – FSH acts on granulosa cells to produce estradiol using thecal androgens • FSH – Essential for normal granulosa cell development and function • Expression of LH receptors in large follicle
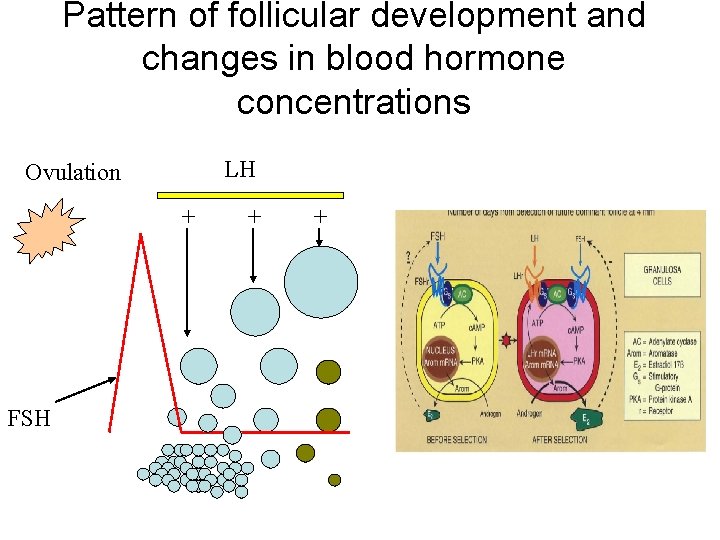
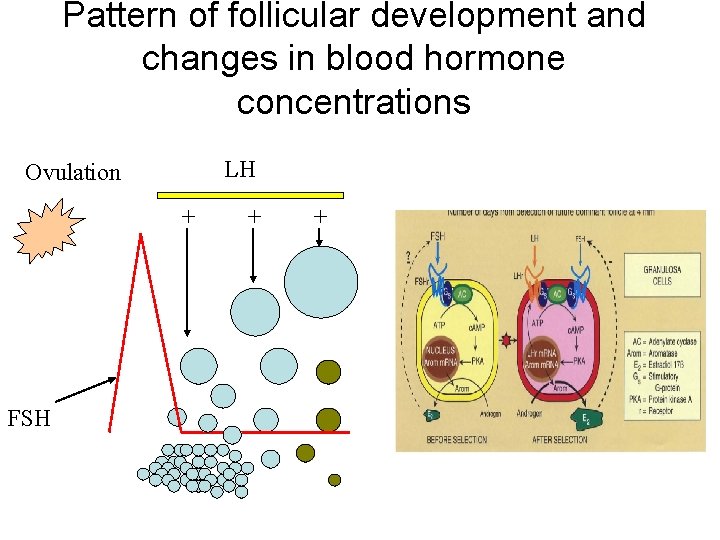
Pattern of follicular development and changes in blood hormone concentrations LH Ovulation + FSH + +
Role of gonadotropins • Production of c. AMP – Activation of protein kinase A pathway • Increased binding of steroidogenic factor-1 (SF-1) to DNA – Transcription factor • Activation of genes involved in steroidogenesis
Role of gonadotropins • Increased cholesterol uptake – Increased number of steroidogenic acute regulate protein (St. AR) – Most critical step for androgen synthesis • Increased enzyme activity – Aromatase expression in the granulosa cells
Action of steroid hormones • Development of reproductive organs – Fetal – Pubertal • Determinative – Adult • Regulatory • Regulation of gonadotropin secretion – Long feedback loop
Role of androgens in male • Fetal life – Determinative action • Development of male genitalia • Defeminization and masculinization • Adult life – Essential for normal spermatogenesis – Development and function of accessory sex organs
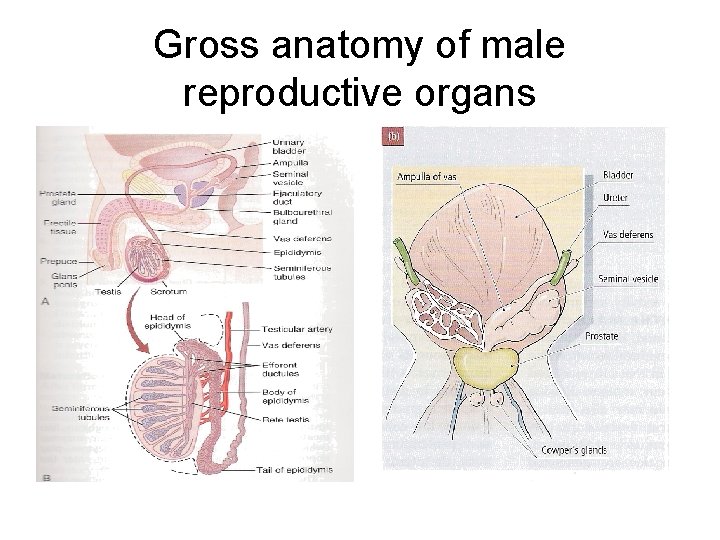
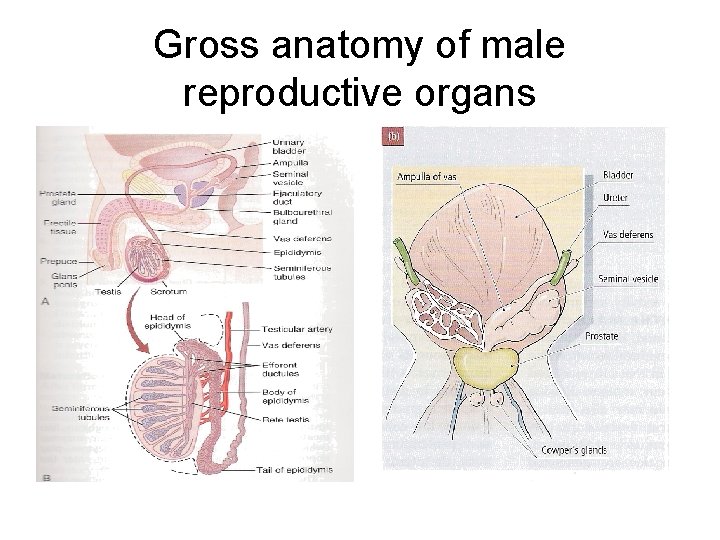
Gross anatomy of male reproductive organs
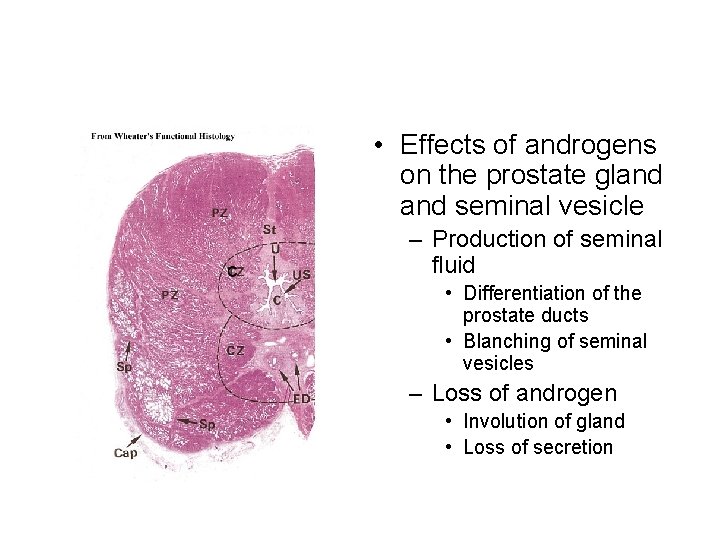
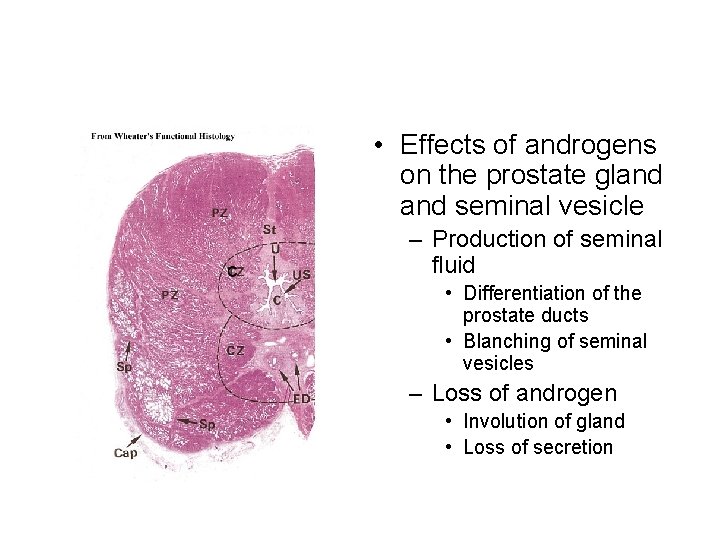
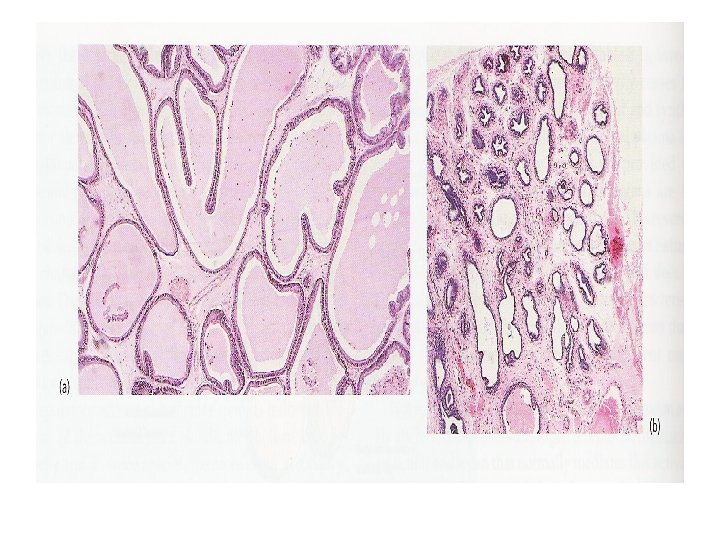
• Effects of androgens on the prostate gland seminal vesicle – Production of seminal fluid • Differentiation of the prostate ducts • Blanching of seminal vesicles – Loss of androgen • Involution of gland • Loss of secretion
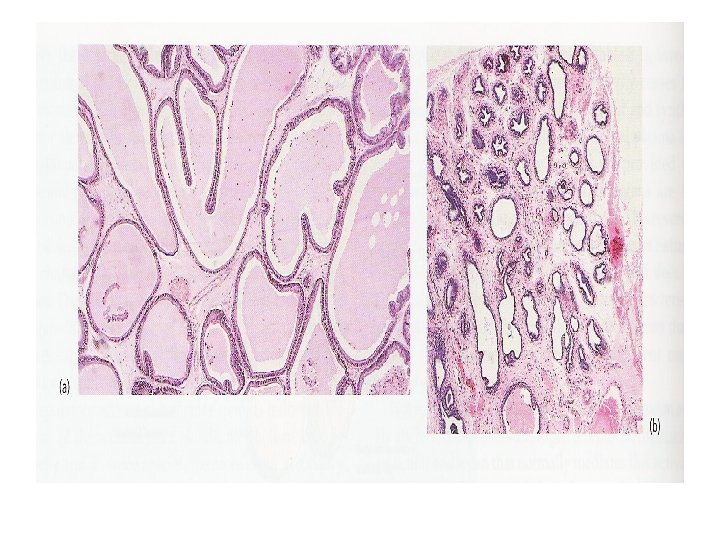
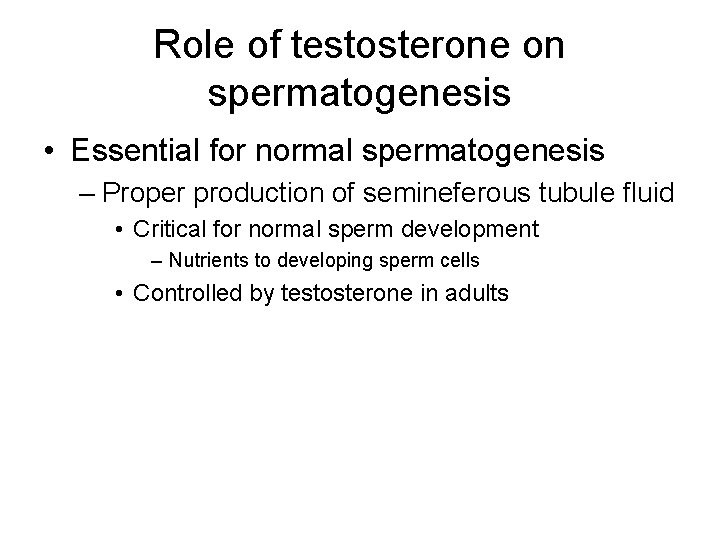
Role of testosterone on spermatogenesis • Essential for normal spermatogenesis – Proper production of semineferous tubule fluid • Critical for normal sperm development – Nutrients to developing sperm cells • Controlled by testosterone in adults
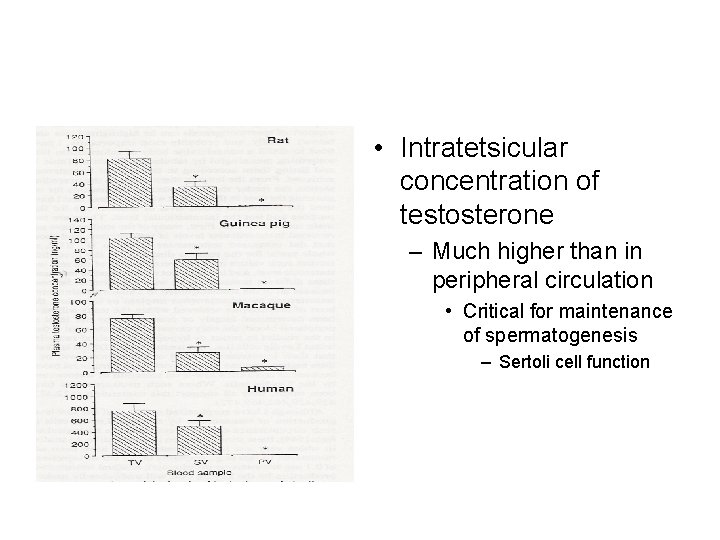
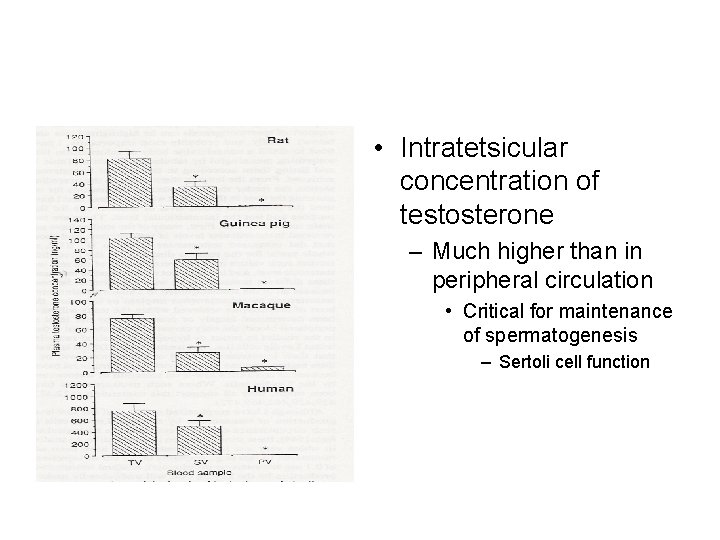
• Intratetsicular concentration of testosterone – Much higher than in peripheral circulation • Critical for maintenance of spermatogenesis – Sertoli cell function
• Loss of testosterone – Reduced Sertoli cell function • Reduced semineferous tubule fluid production • Stage-specific effects – Later stages (7 and 8)
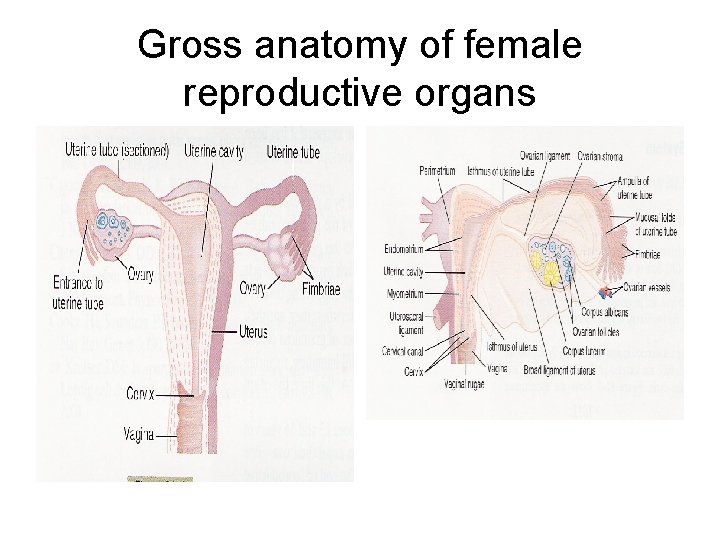
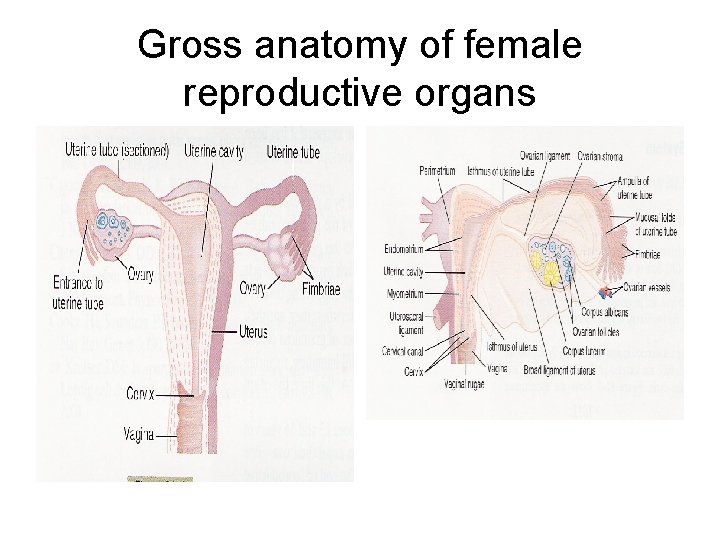
Gross anatomy of female reproductive organs
Role of estradiol and progesterone in female • Cyclic changes – Cyclic changes in ovarian structure • Cyclic changes in uterine structure • Follicular phase – High estradiol – Low progesterone – Preparation of reproductive tract for fertilization • Oviduct • Uterus
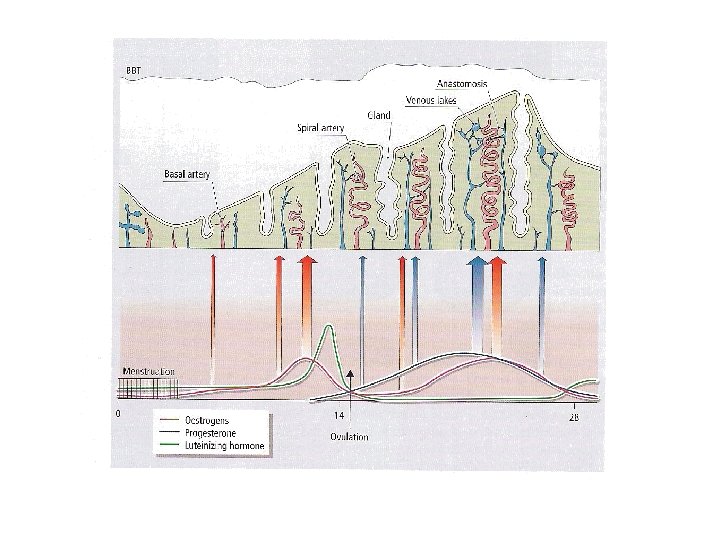
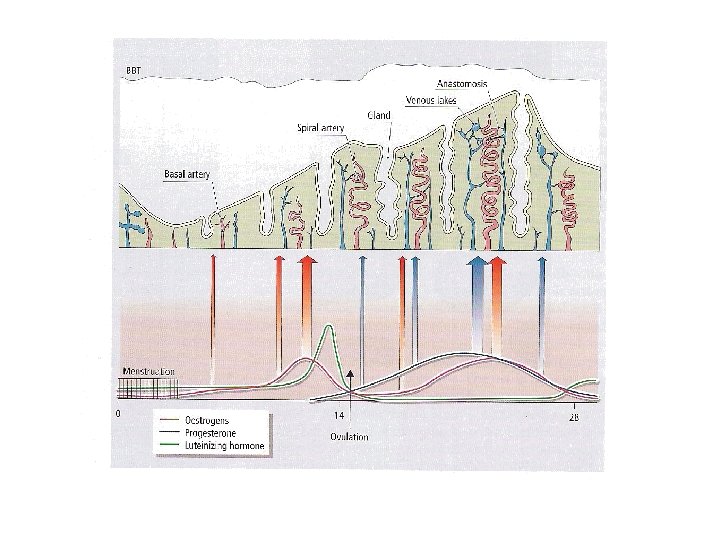
• Uterine endometrium – Mucosal lining of the uterus • Inner-most lining • Well-developed in human compared to other species – Placentation • Menstruation (shedding of endomertial tissue) – Spiral arteries – Hemorrhage (changes in blood flow) – Renewal of endometrium during each reproductive cycle
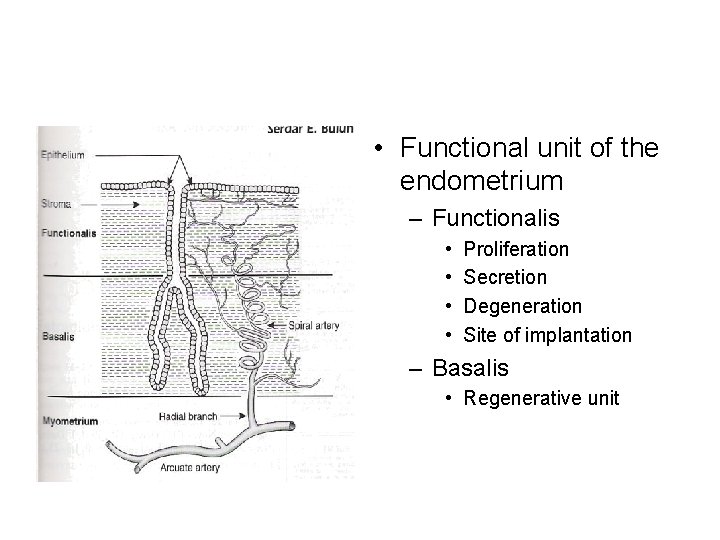
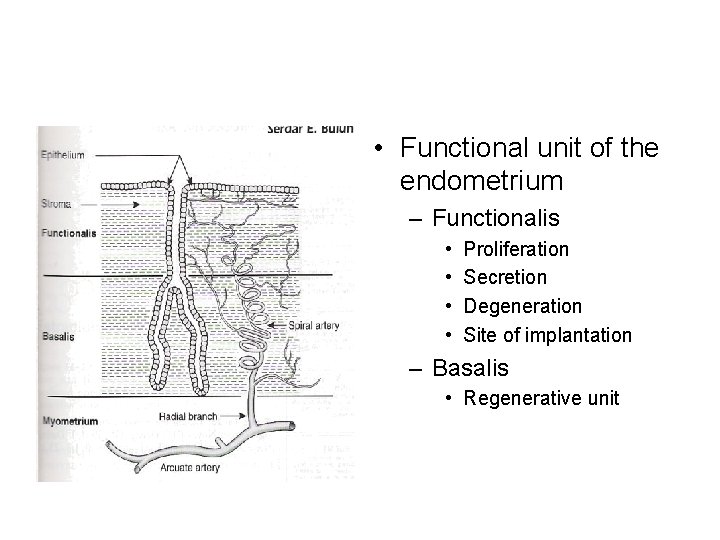
• Functional unit of the endometrium – Functionalis • • Proliferation Secretion Degeneration Site of implantation – Basalis • Regenerative unit
• Hormone-induced changes in endometrium – Cyclic in nature • Re-epithelialization – Menstrual-postmenstrual transition • Endometrial proliferation – Estradiol • Epithelial secretion – Estradiol and progesterone • Premestrual ischemia – Loss of blood supply to epithelia • Menstruation
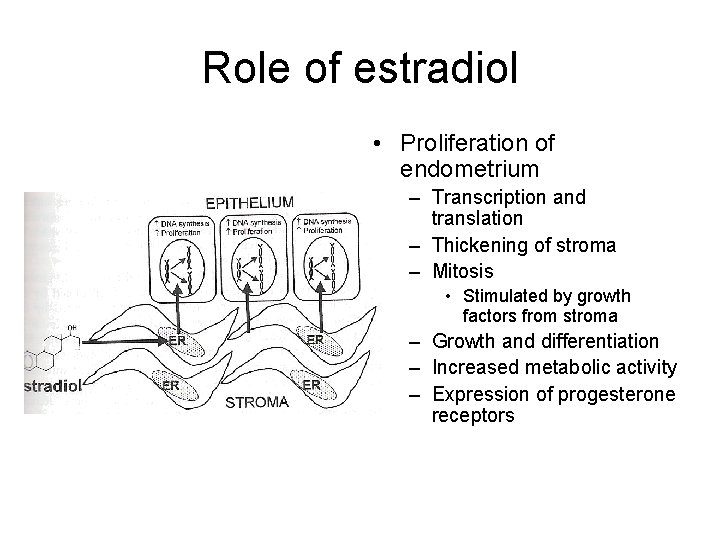
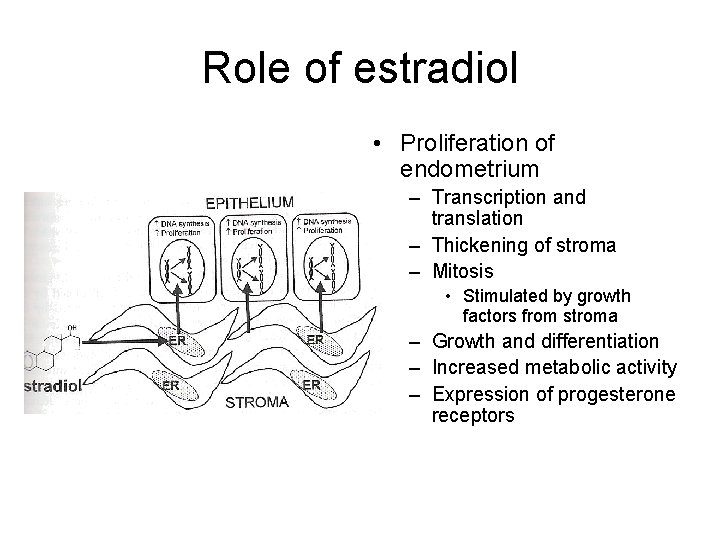
Role of estradiol • Proliferation of endometrium – Transcription and translation – Thickening of stroma – Mitosis • Stimulated by growth factors from stroma – Growth and differentiation – Increased metabolic activity – Expression of progesterone receptors
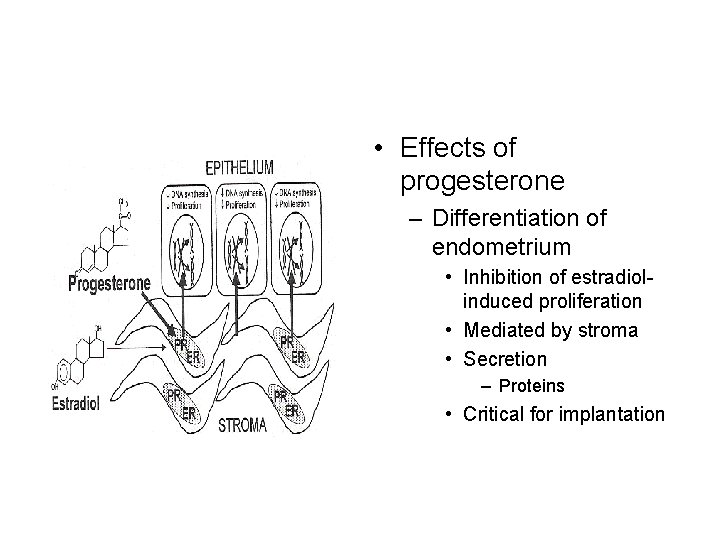
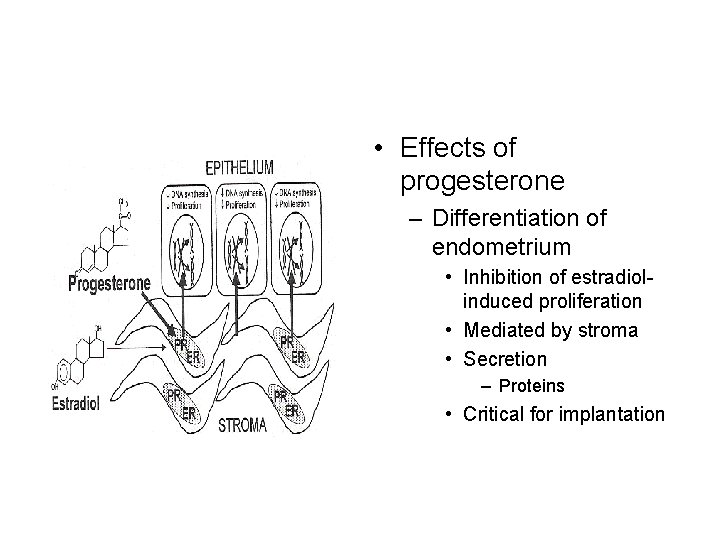
• Effects of progesterone – Differentiation of endometrium • Inhibition of estradiolinduced proliferation • Mediated by stroma • Secretion – Proteins • Critical for implantation
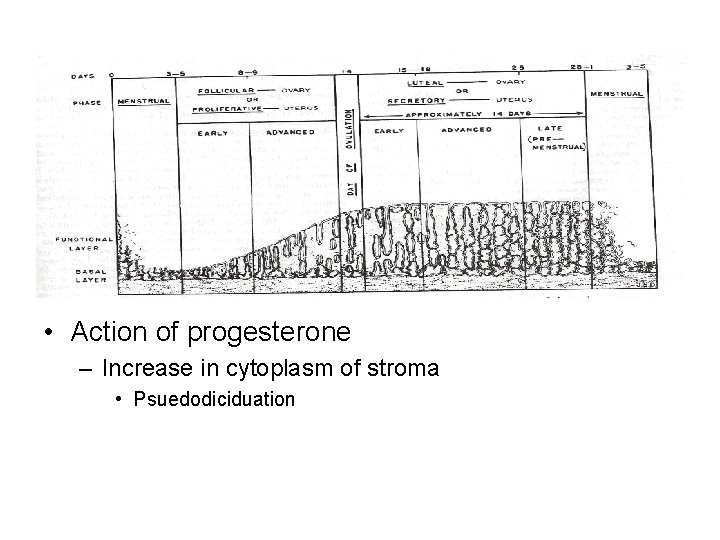
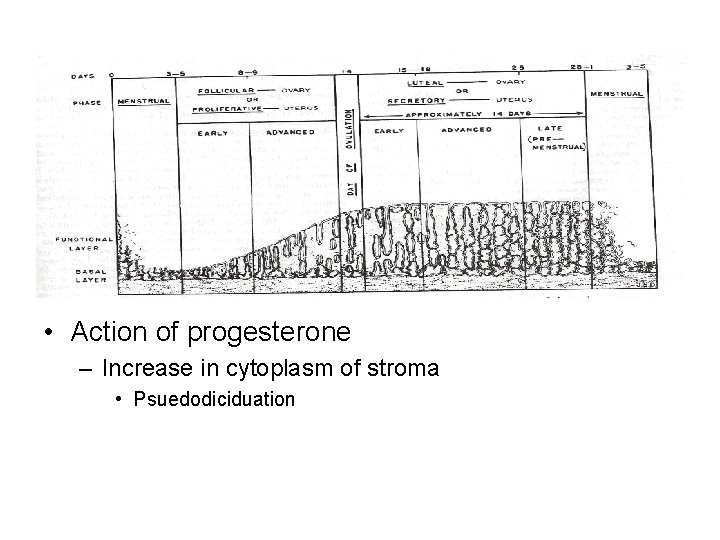
• Action of progesterone – Increase in cytoplasm of stroma • Psuedodiciduation
• Effects on other uterine tissues – Myometrium (smooth muscle) • Excitability and contraction – Depressed by progesterone – Increased by estradiol
• Menstruation – Absence of pregnancy – Initiation of endometrium remodeling • • Alteration of extracellular matrix Leukocyte infiltration Death and removal of tissue Regeneration of tissue
• Menstruation – Withdraw of steroid hormones • Constriction of arterioles and coiled arteries – Ischemia – Precedes bleeding • Bleeding – Relaxation of arteries – Induction of hypoxia-reperfusion injury (formation of hematoma) – Detachment of tissue fragments
Effects of steroid hormones on female reproductive tract • Oviduct – Secretion of oviductal fluid • Nutrients for the oocytes • Sperm survival and capacitation • Early embryonic development • Cervix – Estradiol • Relaxation of muscle • Secretion of watery mucus – Progesterone • Tightening of muscle • Secretion of thick mucus