Sterile Gloving Dressing Change 1 Applying Sterile Gloves




- Slides: 41
Sterile Gloving & Dressing Change 1
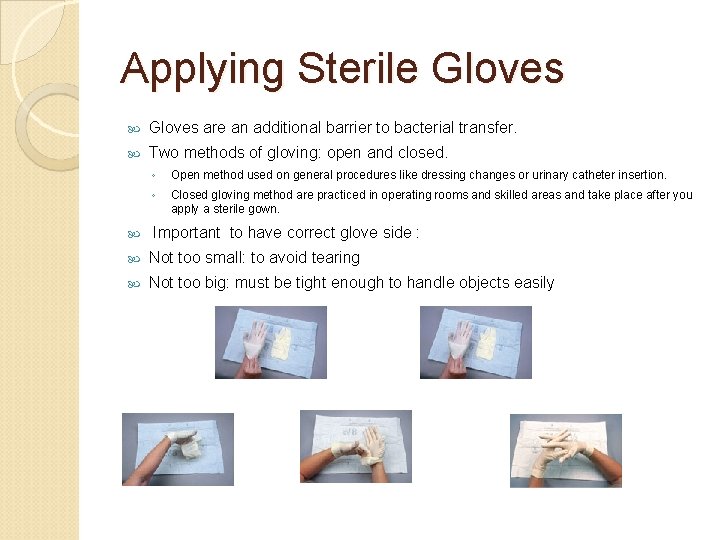
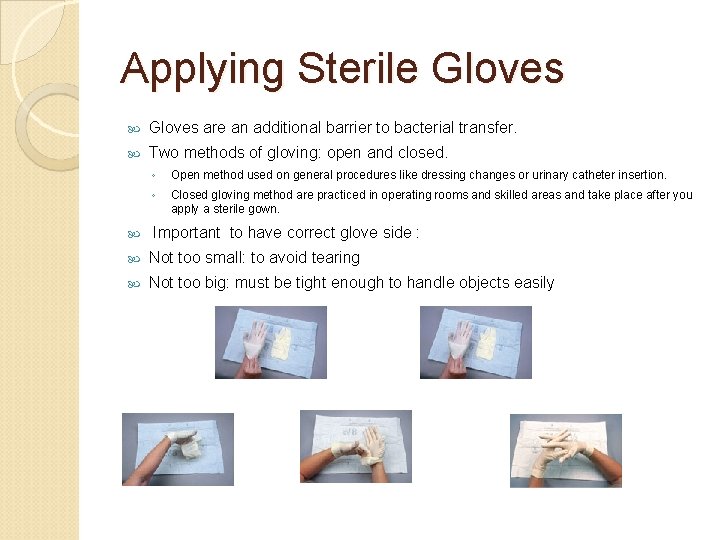
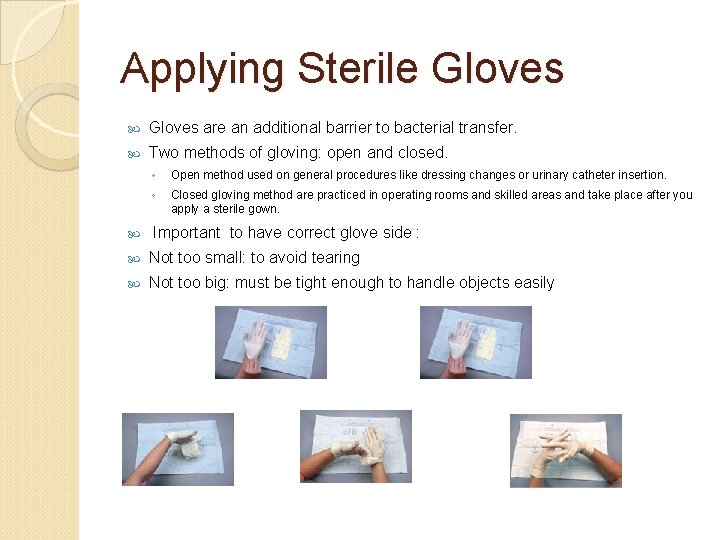
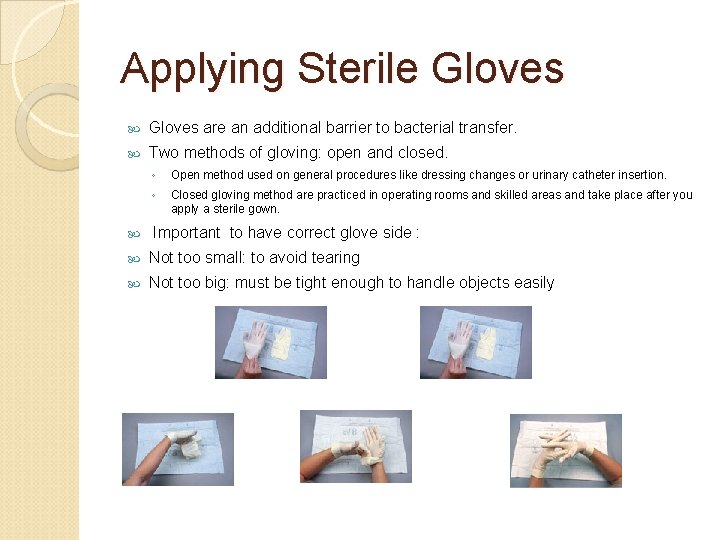
Applying Sterile Gloves are an additional barrier to bacterial transfer. Two methods of gloving: open and closed. ◦ Open method used on general procedures like dressing changes or urinary catheter insertion. ◦ Closed gloving method are practiced in operating rooms and skilled areas and take place after you apply a sterile gown. Important to have correct glove side : Not too small: to avoid tearing Not too big: must be tight enough to handle objects easily 2
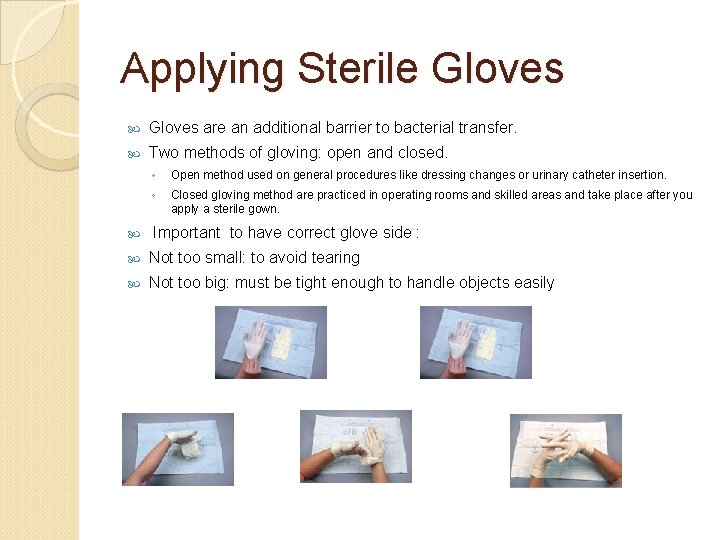
Applying Sterile Gloves are an additional barrier to bacterial transfer. Two methods of gloving: open and closed. ◦ Open method used on general procedures like dressing changes or urinary catheter insertion. ◦ Closed gloving method are practiced in operating rooms and skilled areas and take place after you apply a sterile gown. Important to have correct glove side : Not too small: to avoid tearing Not too big: must be tight enough to handle objects easily 3
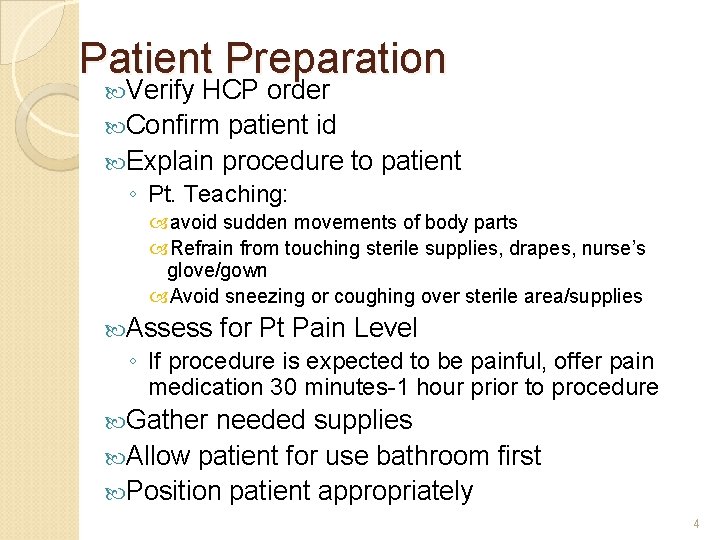
Patient Preparation Verify HCP order Confirm patient id Explain procedure to patient ◦ Pt. Teaching: avoid sudden movements of body parts Refrain from touching sterile supplies, drapes, nurse’s glove/gown Avoid sneezing or coughing over sterile area/supplies Assess for Pt Pain Level ◦ If procedure is expected to be painful, offer pain medication 30 minutes-1 hour prior to procedure Gather needed supplies Allow patient for use bathroom first Position patient appropriately 4
Principles of Surgical Asepsis -- STERILE TECHNIQUE 1. A sterile object remains sterile only when touched by another sterile object 2. Only sterile objects may be placed on a sterile field 3. A sterile object or field out of the range of vision or an object held below a person’s waist is contaminated. 4. A sterile object or field becomes contaminated by prolonged exposure to air. 5. When a sterile surface comes in contact with a wet, contaminated surface, the sterile object or field becomes contaminated by capillary action. 6. Fluid flows in the direction of gravity 7. The edges of a sterile field or container are considered to be contaminated. Performing a Sterile Procedure Always gather needed supplies PRIOR to procedure. Have a few extra supplies available if needed Explain procedure to patient Discard item if it becomes contaminated 5
PREPARATION OF STERILE FIELD OPENING STERILE PACKAGES Bedside Table or countertop for opening items ◦ Work area must be above waist level ◦ Do not open supplies in an area where contamination may occur Open Sterile Item on a FLAT Surface ◦ Must be opened w/o contaminating contents ◦ Tear away wrapper/cover while holding object in opposite hand. ◦ Sterile Wrapper may be used as a sterile drape to create sterile field ◦ Use INNER surface of package as sterile field. May add sterile items to sterile field by dropping items into the sterile area. ◦ May touch the outer 1” inch edges to manipulate package/drape ◦ If wrapper has flaps: open top flap and then in order that flaps appear Always start with area furtherest away from you & work towards you Open flaps 1 at a time from SIDE– do NOT reach over item or sterile field Open Sterile Item While HOLDING It ◦ Hold in non-dominant hand & use dominant hand to pull top flap back AWAY from you ◦ Open sides & flaps away from sterile item to allow transfer of item Sterile Field 6
Preparing a Sterile Field 7
POURING STERILE SOLUTION Sterile solution must be poured into sterile containers Outside of bottle & neck of bottle is unsterile Fluid inside is sterile Outside of cap is unsterile and inside of cap is sterile Cap Removal: hold in hand or place inside up on a clean surface in order to keep cap inside sterile. (You can see the inside of the cap). Do NOT put in sterile field. Outer edge of cap is unsterile Hold bottle Label To Palm (so label stays dry & readable) “Lip” solution: pour small amount (1 -2 ml) of sterile solution into a disposable cup or plastic bag. This cleans bottle lip. Hold bottle OUTSIDE the edge of sterile field Do not touch bottle edge to receiving container Pour slowly to avoid splashing or dripping 8
Surgical Scrub -for Surgical Areas Clients having surgery are at increase risk for infection. Therefore, nurses will need to perform a surgical scrub. Remove jewelry and nails short, no artificial nails. If cuts or open abrasions one should not be on the surgical team. This will involve scrubbing from fingernails to elbows with aseptic soap. The scrub initial time should be five minutes. Follow protocol from hospital on using sponge brush because it does decrease infection but however some studies have found this is not necessary. 9
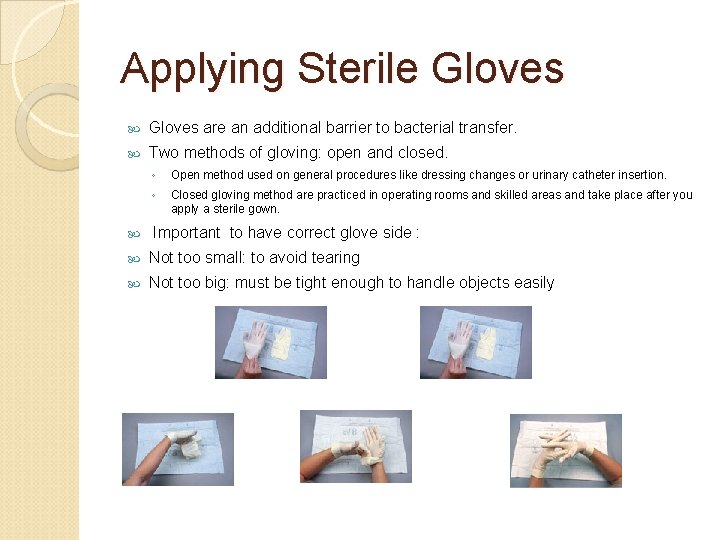
Applying Sterile Gloves are an additional barrier to bacterial transfer. Two methods of gloving: open and closed. ◦ Open method used on general procedures like dressing changes or urinary catheter insertion. ◦ Closed gloving method are practiced in operating rooms and skilled areas and take place after you apply a sterile gown. Important to have correct glove side : Not too small: to avoid tearing Not too big: must be tight enough to handle objects easily 10
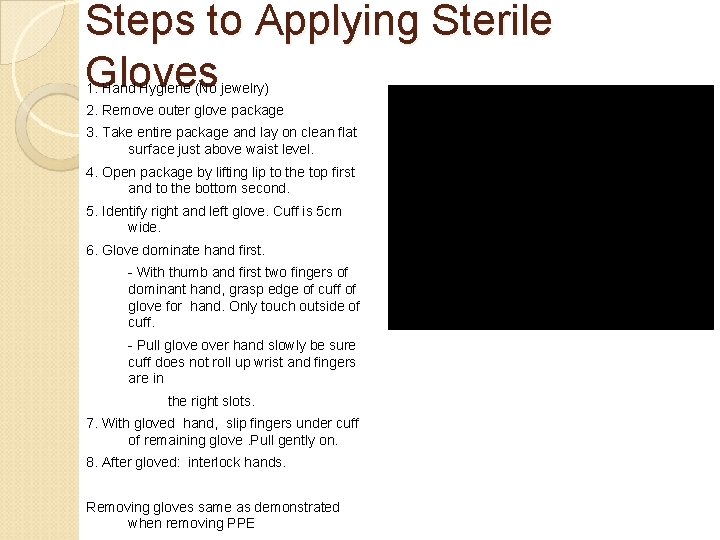
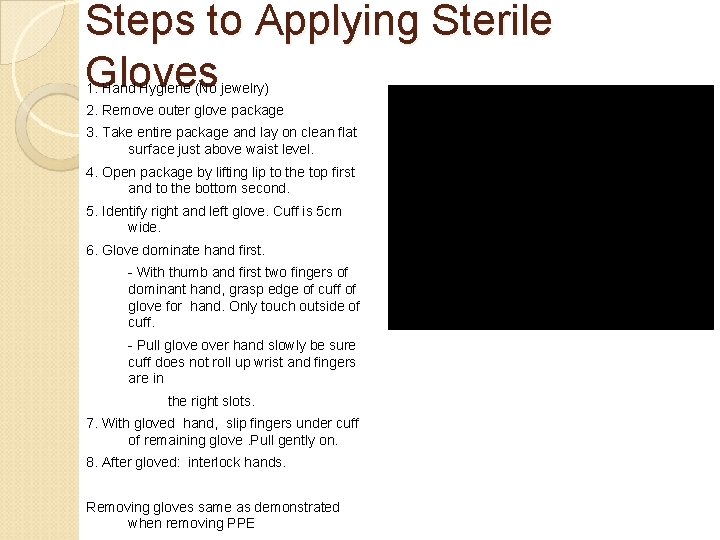
Steps to Applying Sterile Gloves 1. Hand Hygiene (No jewelry) 2. Remove outer glove package 3. Take entire package and lay on clean flat surface just above waist level. 4. Open package by lifting lip to the top first and to the bottom second. 5. Identify right and left glove. Cuff is 5 cm wide. 6. Glove dominate hand first. - With thumb and first two fingers of dominant hand, grasp edge of cuff of glove for hand. Only touch outside of cuff. - Pull glove over hand slowly be sure cuff does not roll up wrist and fingers are in the right slots. 7. With gloved hand, slip fingers under cuff of remaining glove. Pull gently on. 8. After gloved: interlock hands. Removing gloves same as demonstrated when removing PPE 11
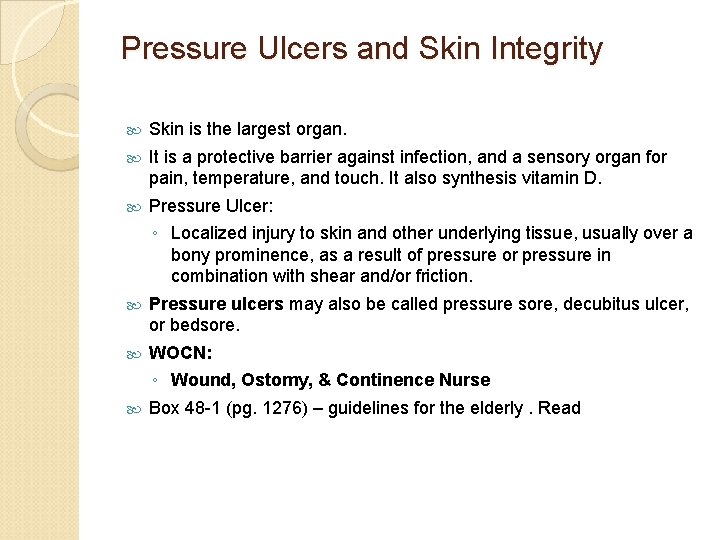
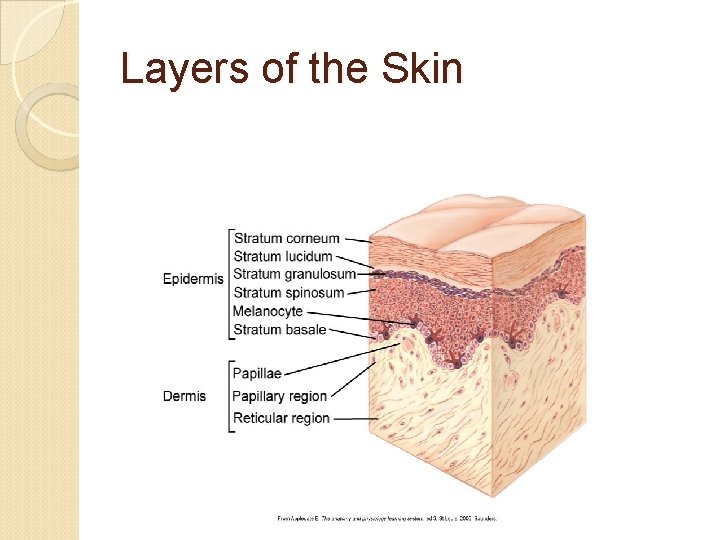
Pressure Ulcers and Skin Integrity Skin is the largest organ. It is a protective barrier against infection, and a sensory organ for pain, temperature, and touch. It also synthesis vitamin D. Pressure Ulcer: ◦ Localized injury to skin and other underlying tissue, usually over a bony prominence, as a result of pressure or pressure in combination with shear and/or friction. Pressure ulcers may also be called pressure sore, decubitus ulcer, or bedsore. WOCN: ◦ Wound, Ostomy, & Continence Nurse Box 48 -1 (pg. 1276) – guidelines for the elderly. Read 12
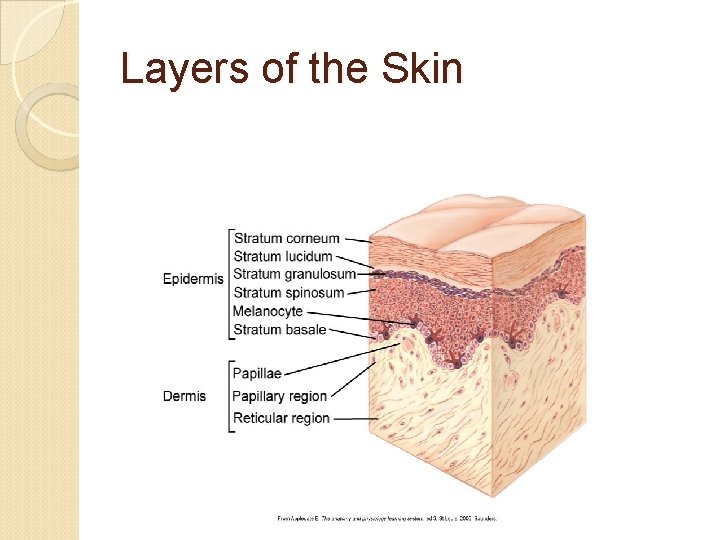
Layers of the Skin
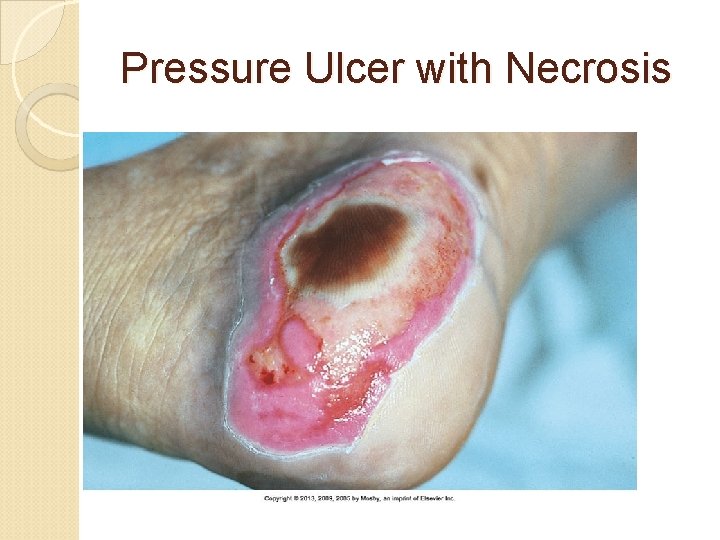
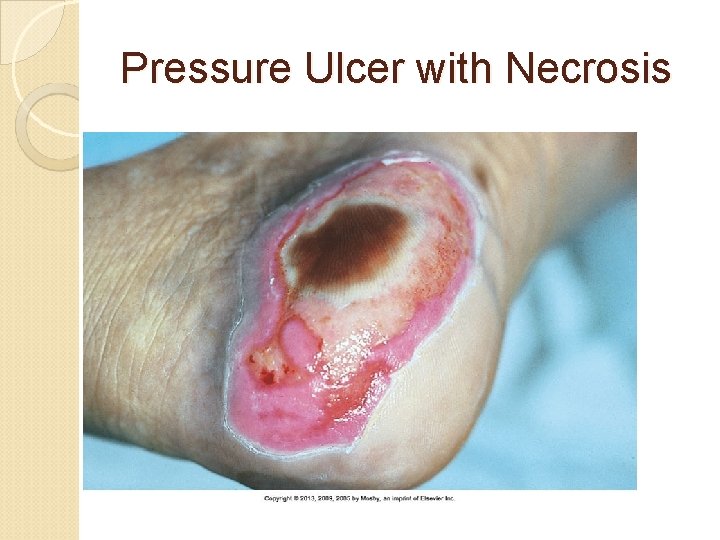
Pressure Ulcer with Necrosis
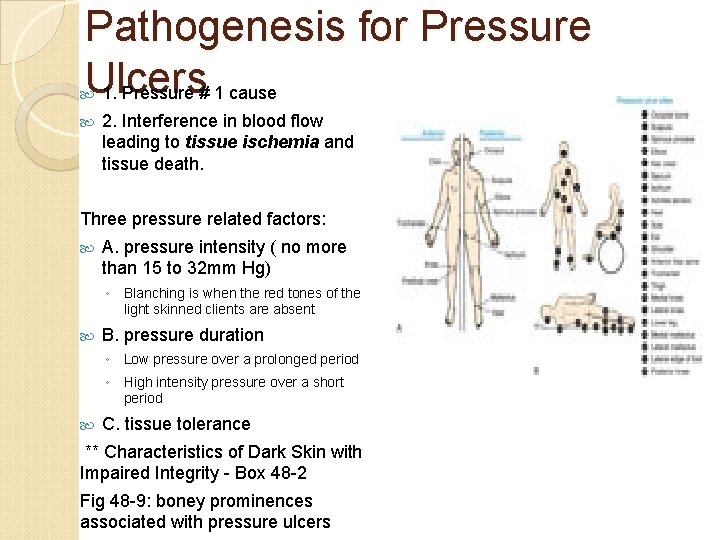
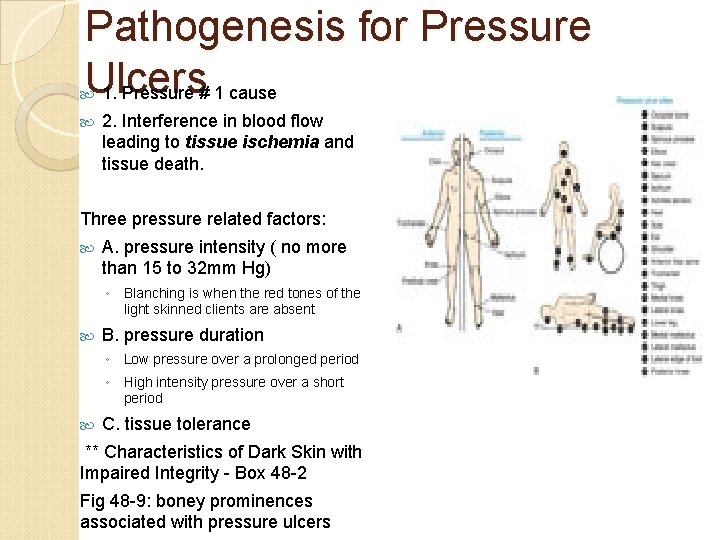
Pathogenesis for Pressure Ulcers 1. Pressure # 1 cause 2. Interference in blood flow leading to tissue ischemia and tissue death. Three pressure related factors: A. pressure intensity ( no more than 15 to 32 mm Hg) ◦ Blanching is when the red tones of the light skinned clients are absent B. pressure duration ◦ Low pressure over a prolonged period ◦ High intensity pressure over a short period C. tissue tolerance ** Characteristics of Dark Skin with Impaired Integrity - Box 48 -2 Fig 48 -9: boney prominences associated with pressure ulcers 15
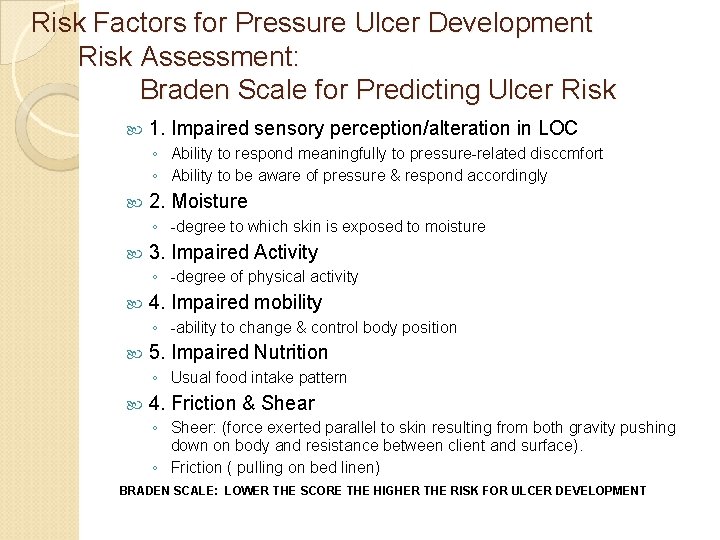
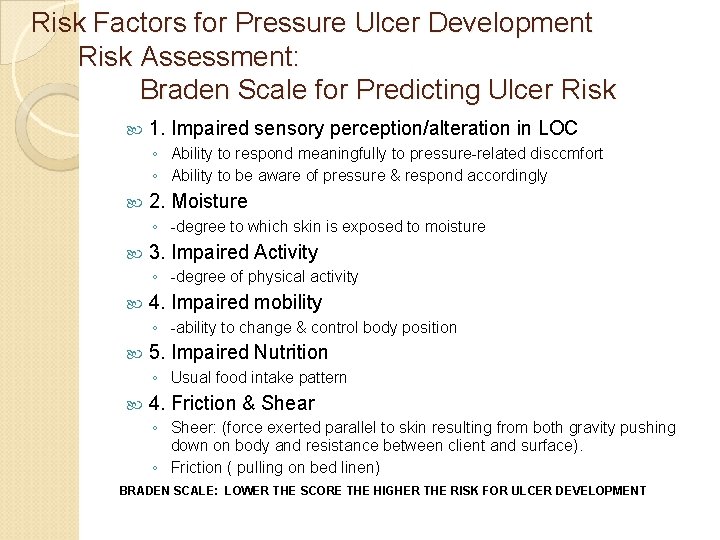
Risk Factors for Pressure Ulcer Development Risk Assessment: Braden Scale for Predicting Ulcer Risk 1. Impaired sensory perception/alteration in LOC ◦ Ability to respond meaningfully to pressure-related disccmfort ◦ Ability to be aware of pressure & respond accordingly 2. Moisture ◦ -degree to which skin is exposed to moisture 3. Impaired Activity ◦ -degree of physical activity 4. Impaired mobility ◦ -ability to change & control body position 5. Impaired Nutrition ◦ Usual food intake pattern 4. Friction & Shear ◦ Sheer: (force exerted parallel to skin resulting from both gravity pushing down on body and resistance between client and surface). ◦ Friction ( pulling on bed linen) BRADEN SCALE: LOWER THE SCORE THE HIGHER THE RISK FOR ULCER DEVELOPMENT 16

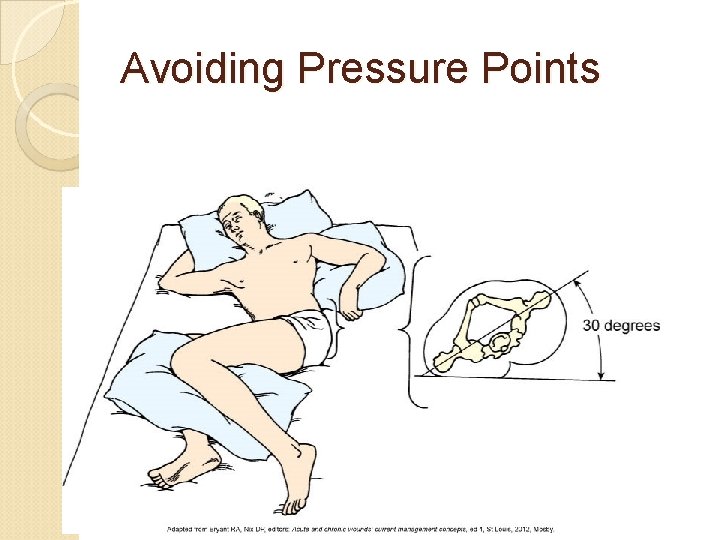
Implementation Health promotion: PREVENTION ◦ Topical skin care Protect bony prominences, skin barriers for incontinence. ◦ Positioning Turn every 1 to 2 hours as indicated. Written turning schedule 30 degree lateral position (avoids pressure points) Figure 48 -15 ◦ Support surfaces Therapeutic Beds & Mattresses/seat cushions: provides pressure redistribution. Decrease the amount of pressure exerted over bony prominences. Wound, Ostomy and Continence Nurses Society (WOCN)
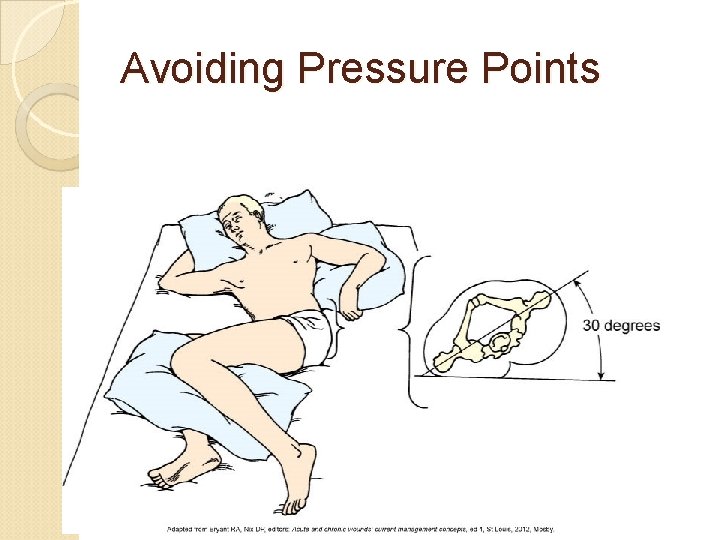
Avoiding Pressure Points
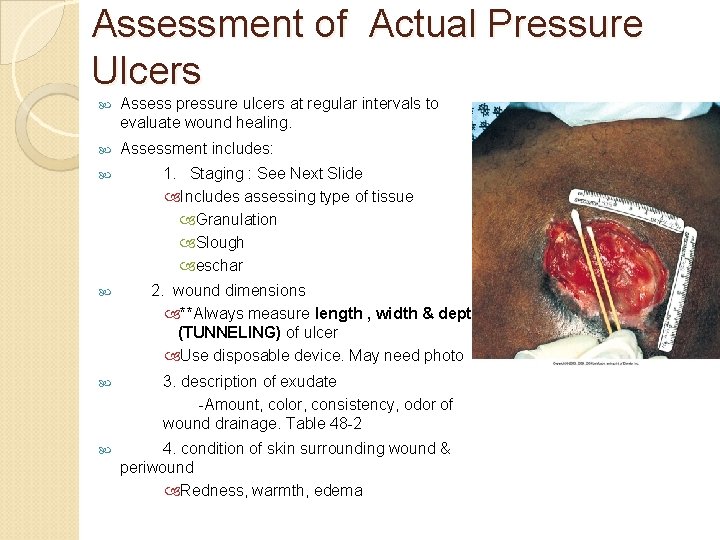
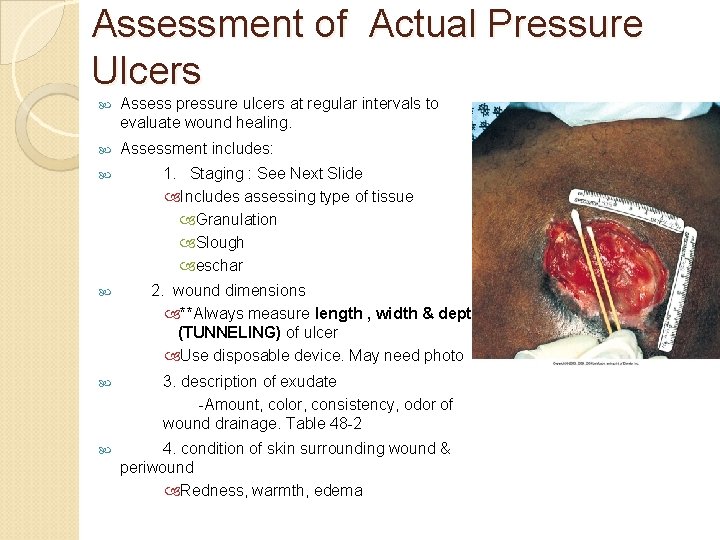
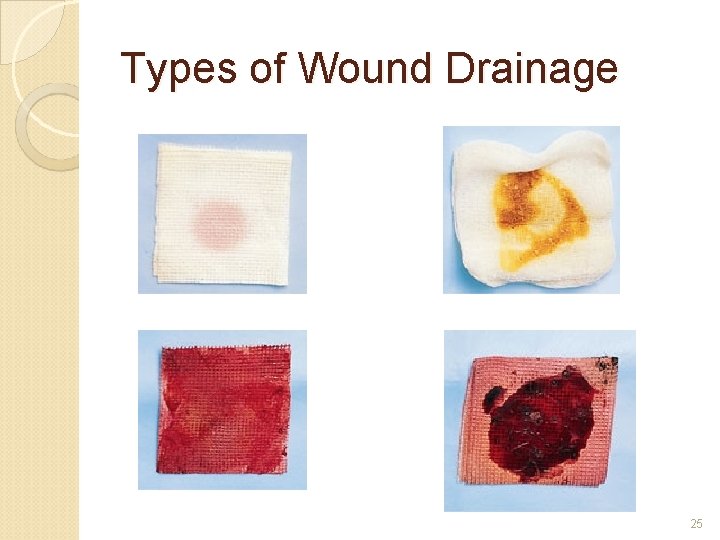
Assessment of Actual Pressure Ulcers Assess pressure ulcers at regular intervals to evaluate wound healing. Assessment includes: 1. Staging : See Next Slide Includes assessing type of tissue Granulation Slough eschar 2. wound dimensions **Always measure length , width & depth (TUNNELING) of ulcer Use disposable device. May need photo 3. description of exudate -Amount, color, consistency, odor of wound drainage. Table 48 -2 4. condition of skin surrounding wound & periwound Redness, warmth, edema 19
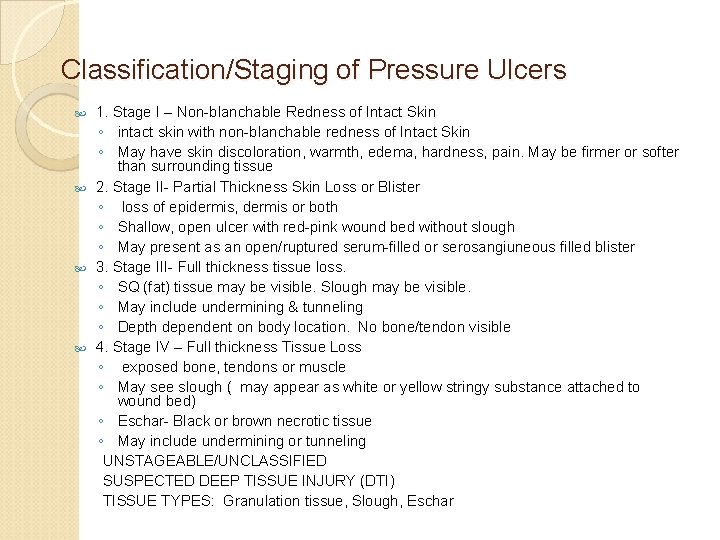
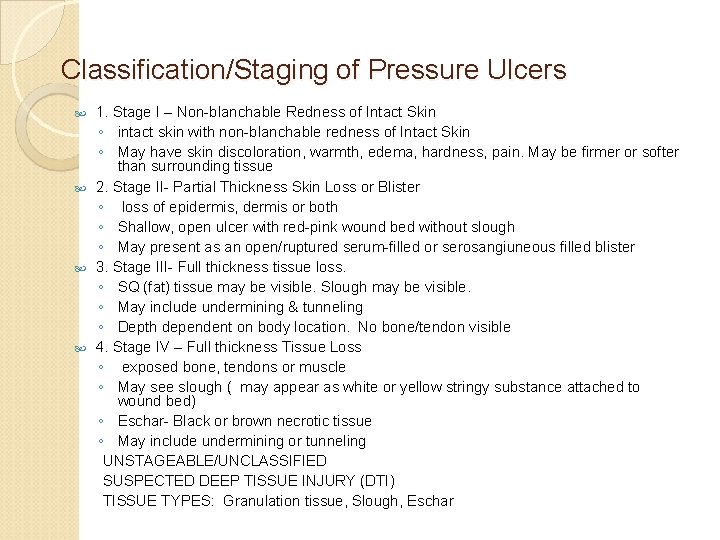
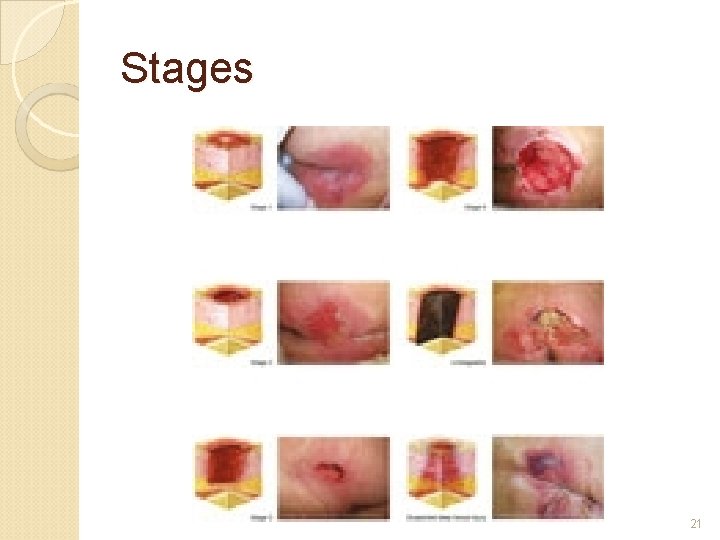
Classification/Staging of Pressure Ulcers 1. Stage I – Non-blanchable Redness of Intact Skin ◦ intact skin with non-blanchable redness of Intact Skin ◦ May have skin discoloration, warmth, edema, hardness, pain. May be firmer or softer than surrounding tissue 2. Stage II- Partial Thickness Skin Loss or Blister ◦ loss of epidermis, dermis or both ◦ Shallow, open ulcer with red-pink wound bed without slough ◦ May present as an open/ruptured serum-filled or serosangiuneous filled blister 3. Stage III- Full thickness tissue loss. ◦ SQ (fat) tissue may be visible. Slough may be visible. ◦ May include undermining & tunneling ◦ Depth dependent on body location. No bone/tendon visible 4. Stage IV – Full thickness Tissue Loss ◦ exposed bone, tendons or muscle ◦ May see slough ( may appear as white or yellow stringy substance attached to wound bed) ◦ Eschar- Black or brown necrotic tissue ◦ May include undermining or tunneling UNSTAGEABLE/UNCLASSIFIED SUSPECTED DEEP TISSUE INJURY (DTI) TISSUE TYPES: Granulation tissue, Slough, Eschar 20
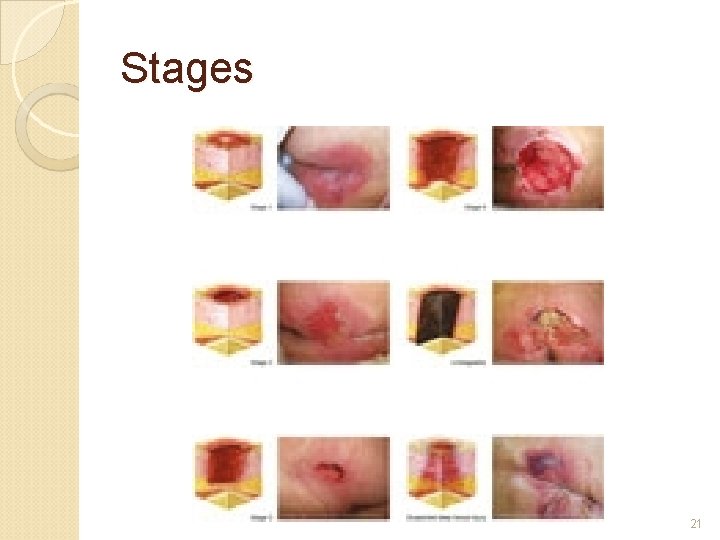
Stages 21
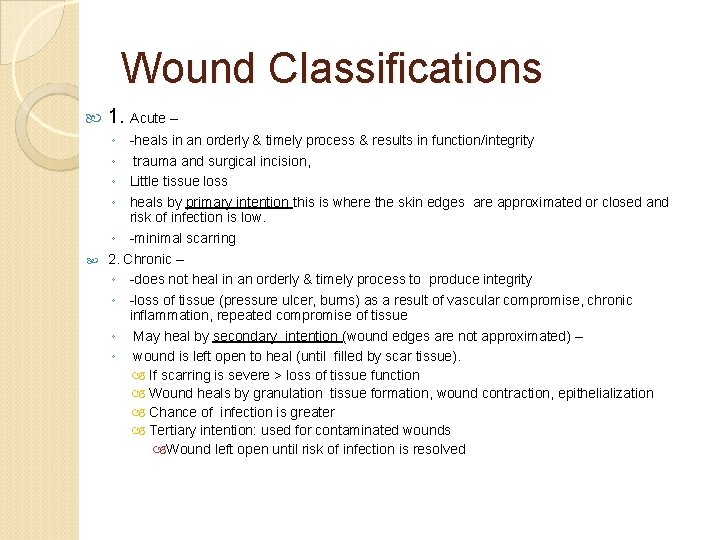
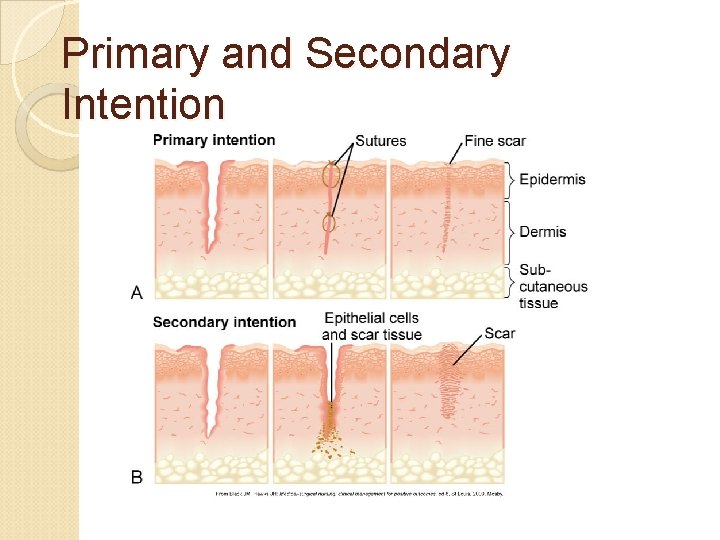
Wound Classifications 1. Acute – ◦ -heals in an orderly & timely process & results in function/integrity ◦ trauma and surgical incision, ◦ Little tissue loss ◦ heals by primary intention this is where the skin edges are approximated or closed and risk of infection is low. ◦ -minimal scarring 2. Chronic – ◦ -does not heal in an orderly & timely process to produce integrity ◦ -loss of tissue (pressure ulcer, burns) as a result of vascular compromise, chronic inflammation, repeated compromise of tissue ◦ May heal by secondary intention (wound edges are not approximated) – ◦ wound is left open to heal (until filled by scar tissue). If scarring is severe > loss of tissue function Wound heals by granulation tissue formation, wound contraction, epithelialization Chance of infection is greater Tertiary intention: used for contaminated wounds Wound left open until risk of infection is resolved 22
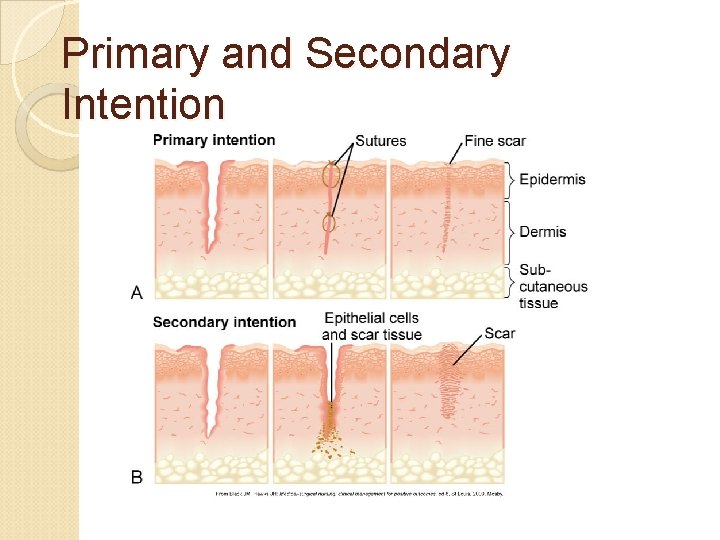
Primary and Secondary Intention

Wound Colors
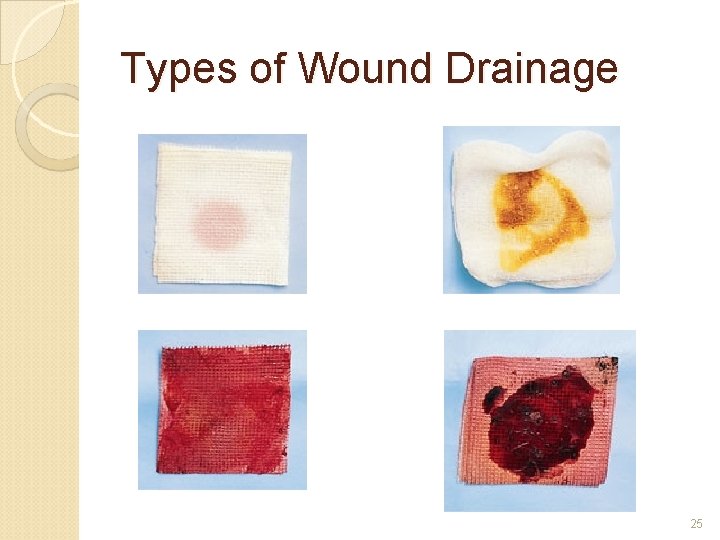
Types of Wound Drainage 25
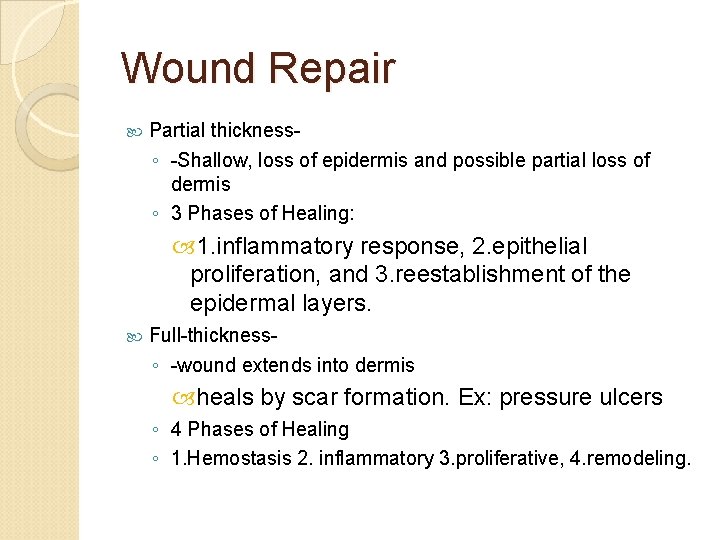
Wound Repair Partial thickness◦ -Shallow, loss of epidermis and possible partial loss of dermis ◦ 3 Phases of Healing: 1. inflammatory response, 2. epithelial proliferation, and 3. reestablishment of the epidermal layers. Full-thickness◦ -wound extends into dermis heals by scar formation. Ex: pressure ulcers ◦ 4 Phases of Healing ◦ 1. Hemostasis 2. inflammatory 3. proliferative, 4. remodeling. 26
Complications of Wound Healing Hemorrhage- bleeding from wound ◦ s/s hypovolemic shock : hypotension, tachypnea, tachycardia, cool/ clammy skin, decreased urine output Infection – second most common nosocomial infection ◦ Color of exudate/Odor Dehiscence- partial or total separation of wound layer Fistulas- abnormal opening between two organs and outside of the body. Evisceration- opening of wound with visceral organs protruding through wound opening. 27
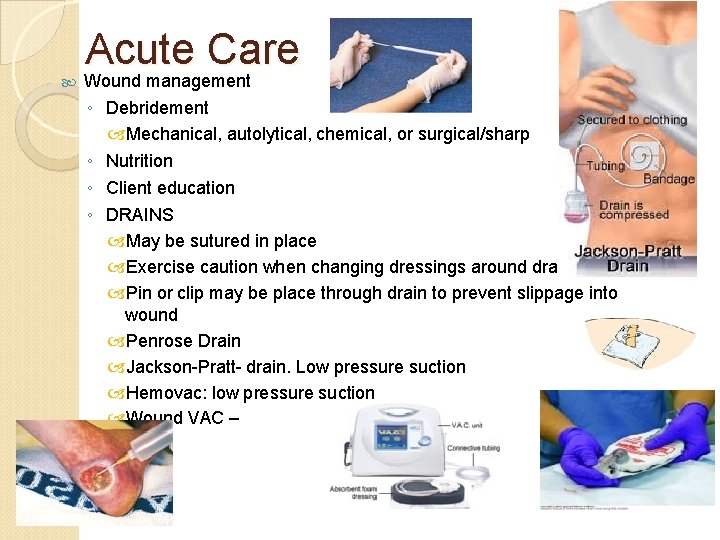
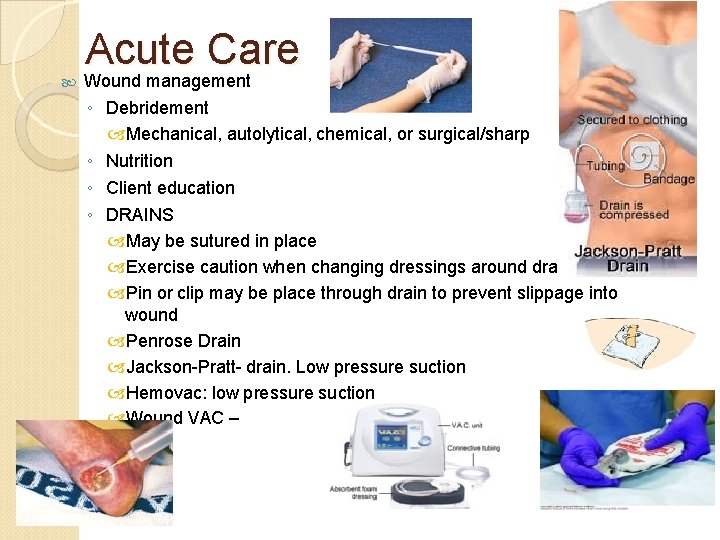
Acute Care Wound management ◦ Debridement Mechanical, autolytical, chemical, or surgical/sharp ◦ Nutrition ◦ Client education ◦ DRAINS May be sutured in place Exercise caution when changing dressings around drain Pin or clip may be place through drain to prevent slippage into wound Penrose Drain Jackson-Pratt- drain. Low pressure suction Hemovac: low pressure suction Wound VAC –
Wound Assessment 29

Wound Irrigation 30
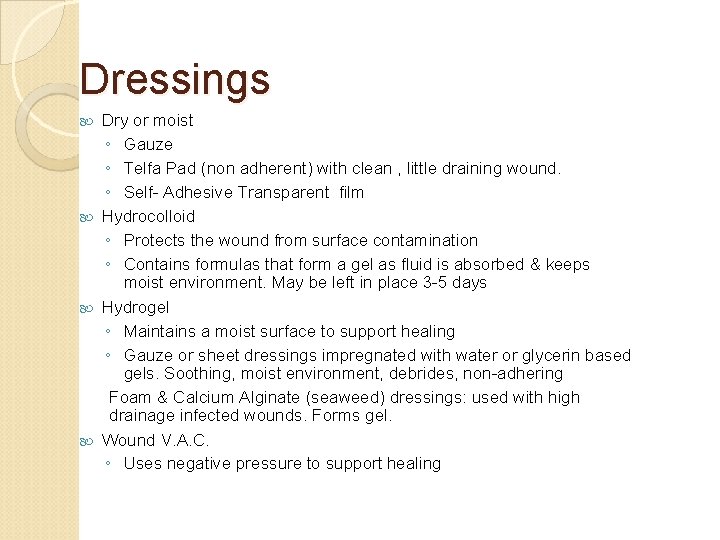
Dressings Dry or moist ◦ Gauze ◦ Telfa Pad (non adherent) with clean , little draining wound. ◦ Self- Adhesive Transparent film Hydrocolloid ◦ Protects the wound from surface contamination ◦ Contains formulas that form a gel as fluid is absorbed & keeps moist environment. May be left in place 3 -5 days Hydrogel ◦ Maintains a moist surface to support healing ◦ Gauze or sheet dressings impregnated with water or glycerin based gels. Soothing, moist environment, debrides, non-adhering Foam & Calcium Alginate (seaweed) dressings: used with high drainage infected wounds. Forms gel. Wound V. A. C. ◦ Uses negative pressure to support healing
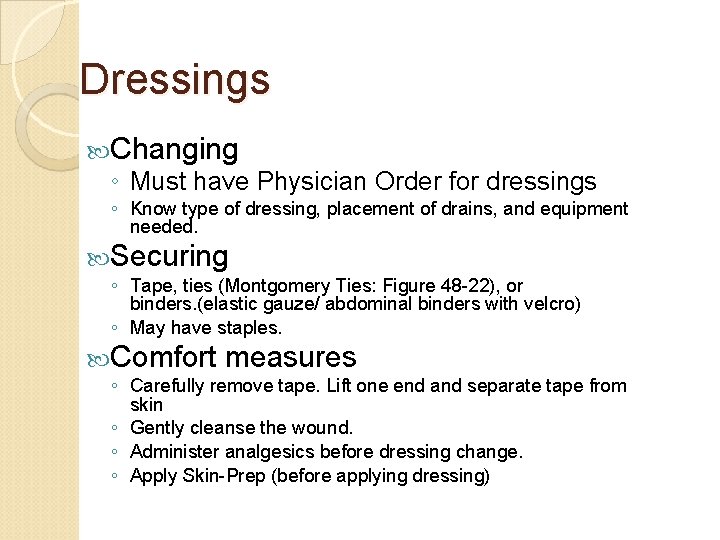
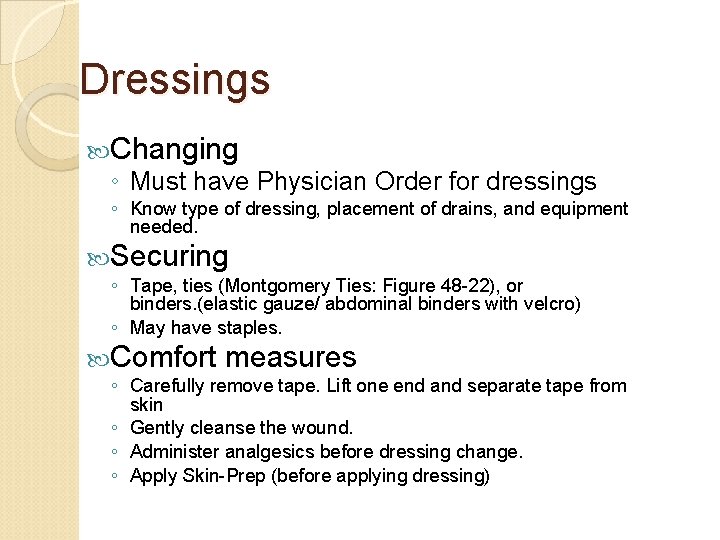
Dressings Changing ◦ Must have Physician Order for dressings ◦ Know type of dressing, placement of drains, and equipment needed. Securing ◦ Tape, ties (Montgomery Ties: Figure 48 -22), or binders. (elastic gauze/ abdominal binders with velcro) ◦ May have staples. Comfort measures ◦ Carefully remove tape. Lift one end and separate tape from skin ◦ Gently cleanse the wound. ◦ Administer analgesics before dressing change. ◦ Apply Skin-Prep (before applying dressing)
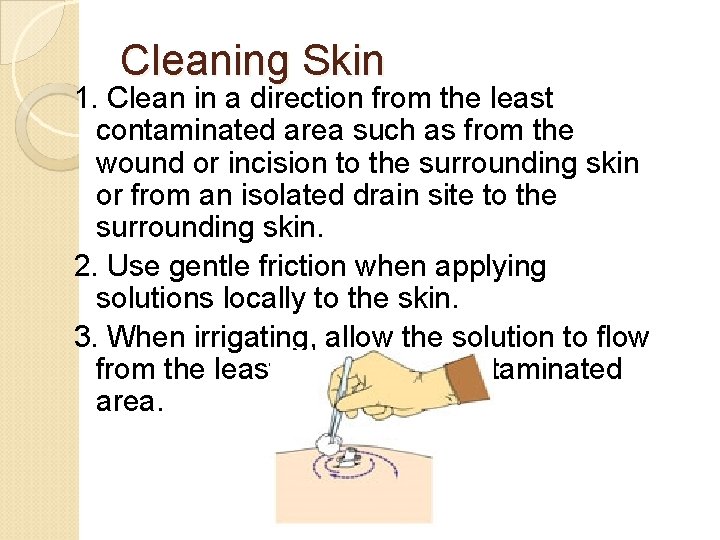
Cleaning Skin 1. Clean in a direction from the least contaminated area such as from the wound or incision to the surrounding skin or from an isolated drain site to the surrounding skin. 2. Use gentle friction when applying solutions locally to the skin. 3. When irrigating, allow the solution to flow from the least to the most contaminated area.
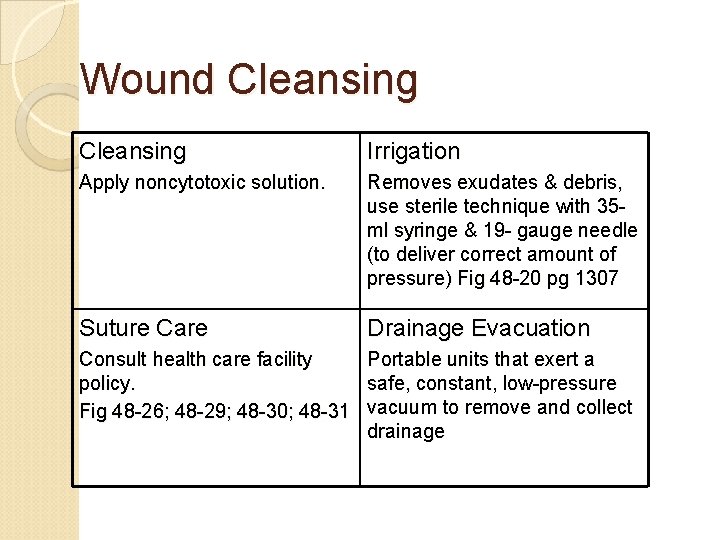
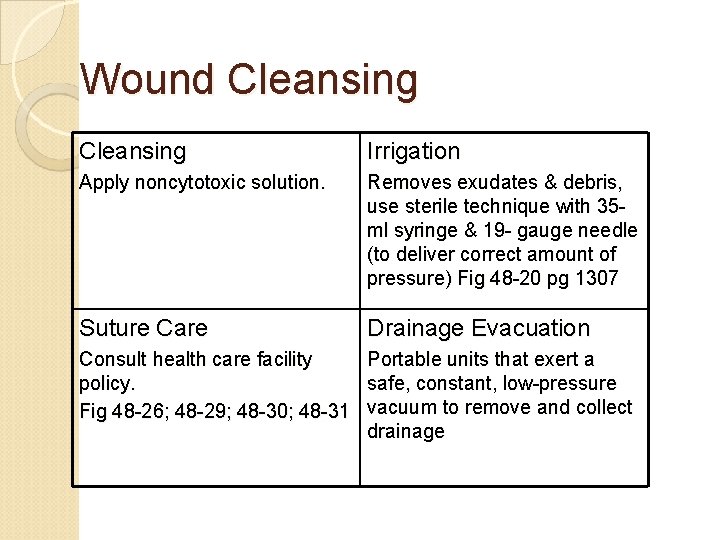
Wound Cleansing Irrigation Apply noncytotoxic solution. Removes exudates & debris, use sterile technique with 35 ml syringe & 19 - gauge needle (to deliver correct amount of pressure) Fig 48 -20 pg 1307 Suture Care Drainage Evacuation Consult health care facility Portable units that exert a policy. safe, constant, low-pressure Fig 48 -26; 48 -29; 48 -30; 48 -31 vacuum to remove and collect drainage

Bandages and Binders Bandages & Binders – Assessment inspect skin for ◦ abrasions, edema, discoloration, ◦ open wounds, ◦ circulatory impairment (coolness, pallor, cyanosis, pulses, swelling, numbness or tingling
Heat and Cold Therapy Assessment for temperature tolerance Bodily responses to heat and cold Factors influencing heat and cold tolerance Education
Contraindications to Cold and Heat Cold is contraindicated: ◦ ◦ If the site of injury is edematous In the presence of neuropathy If the patient is shivering If the patient has impaired circulation Heat is contraindicated: ◦ For areas of active bleeding ◦ For an acute localized inflammation ◦ Over a large area if a patient has cardiovascular problems
Applying wet to dry dressing Skill 48 -3 ID patient with 2 identifiers ◦ assess pain. Provide pain med as ordered Review Order for Dressing Change Gather Supplies Enter room/explain procedure/wash hands Lay out supplies Wash hands Proceed with procedure per order. SWGTC Wet to Dry Dressing Change 38
Ex: Documentation Wound Care Charting: Dressing change per MD orders to left hip. Old dressing removed and placed in red biohazardous waste bag. Cleansed wound with H 202, NS rinse & NS wet to dry dressing applied. Covered with abd pad & taped to secure. Stage III reddened wound bed at 6 x 3 cm 1. 5 cm deep. Granulating edges. Moderate amount of yellow/green exudates noted at site. Slight odor present. Dr. Adams notified. Pt tolerated without difficulty. First Name Last Name, SN, SWGTC 39
Evaluation Nursing interventions for reducing and treating pressure ulcers need to be evaluated to determine if the client has met the identified outcomes or goals. Was the etiology of the skin impairment addressed? Were the pressure, friction, shear, and moisture components identified; and did the plan of care decrease the contribution of each of these components? Was wound healing supported by providing the wound base with a moist protected environment? Were issues such as nutrition assessed and a plan of care developed that provided the patient with the calories to support healing?
This work is licensed under a Creative Commons Attribution 4. 0 International License. Except where otherwise noted, this content by Southern Regional Technical College is licensed under the Creative Commons Attribution 4. 0 International License. To view a copy of this license, click https: //creativecommons. org/licenses/by/4. 0/ Healthcare Careers Work!(HCW) is sponsored by a $2. 3 million grant from the U. S. Department of Labor, Employment & Training Administration. TAACCCT Grant #TC- 26488 -14 -60 -A-13. Southern Regional Technical College is an equal opportunity employer and will make adaptive equipment available to persons with disabilities upon request. This workforce product was funded by a grant awarded by the U. S. Department of Labor’s Employment and Training Administration. The product was created by the grantee and does not necessarily reflect the official position of the U. S. Department of Labor. The U. S. Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership.