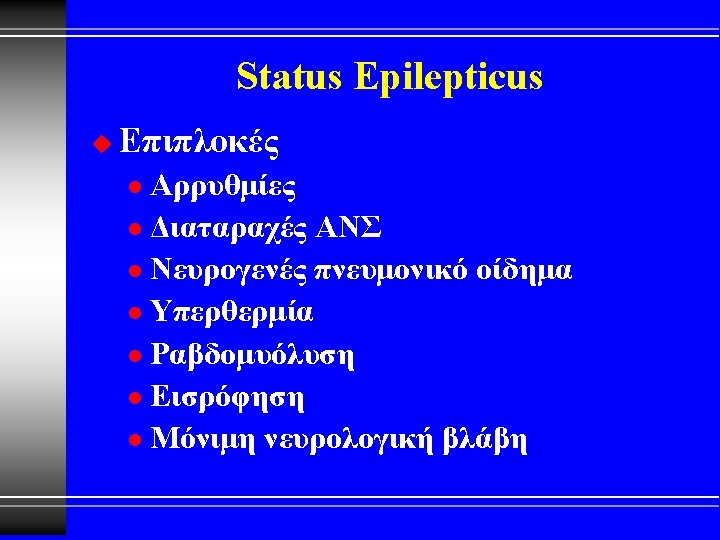
Status Epilepticus u Electroclinical features convulsive status epilepticus




- Slides: 69
Status Epilepticus
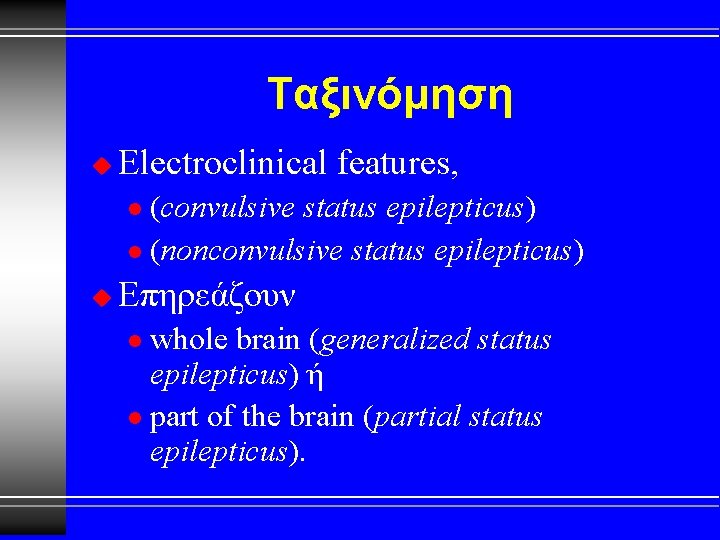
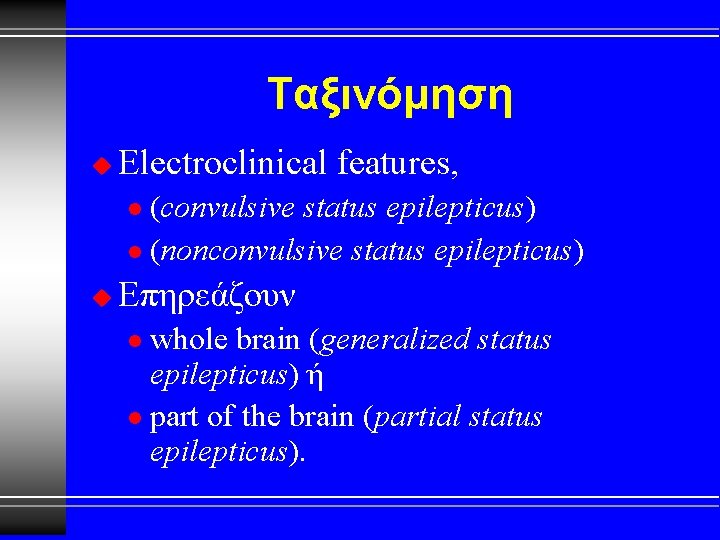
Ταξινόμηση u Electroclinical features, (convulsive status epilepticus) l (nonconvulsive status epilepticus) l u Επηρεάζουν whole brain (generalized status epilepticus) ή l part of the brain (partial status epilepticus). l
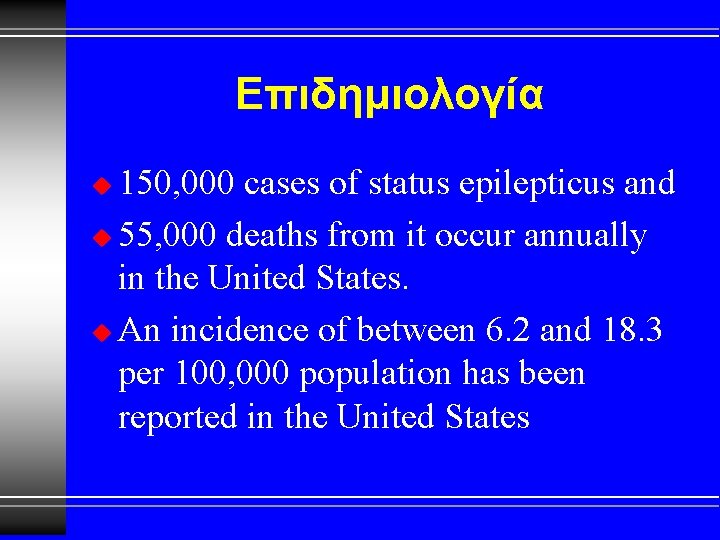
Επιδημιολογία 150, 000 cases of status epilepticus and u 55, 000 deaths from it occur annually in the United States. u An incidence of between 6. 2 and 18. 3 per 100, 000 population has been reported in the United States u
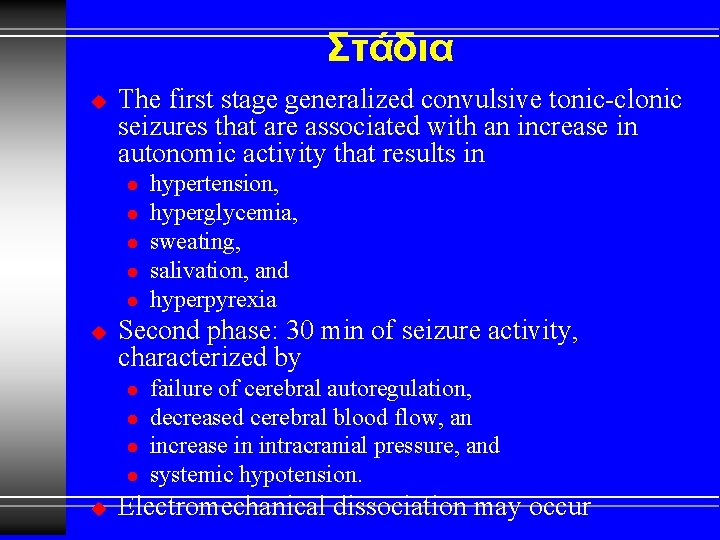
Στάδια u The first stage generalized convulsive tonic-clonic seizures that are associated with an increase in autonomic activity that results in l l l u Second phase: 30 min of seizure activity, characterized by l l u hypertension, hyperglycemia, sweating, salivation, and hyperpyrexia failure of cerebral autoregulation, decreased cerebral blood flow, an increase in intracranial pressure, and systemic hypotension. Electromechanical dissociation may occur

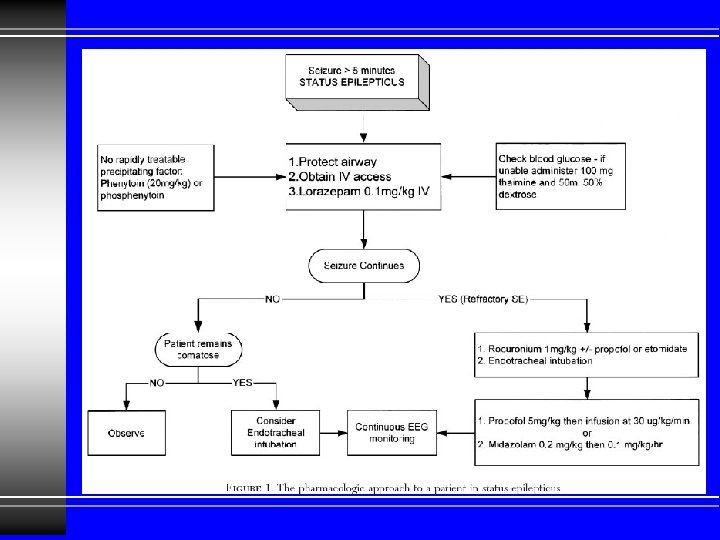
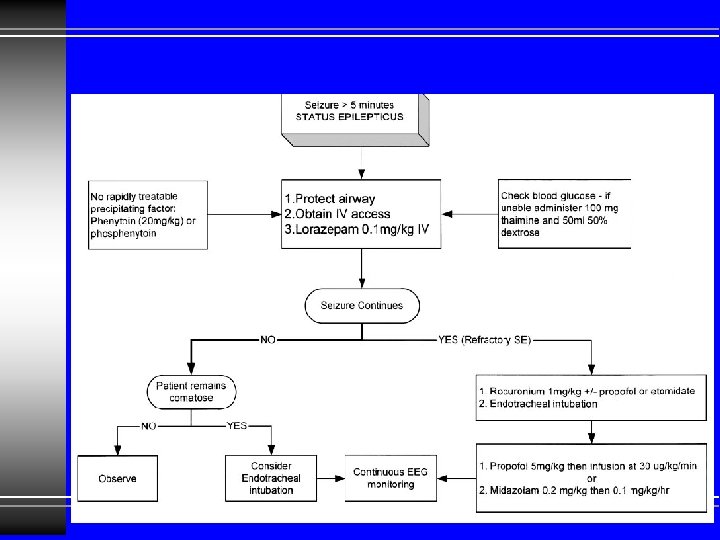
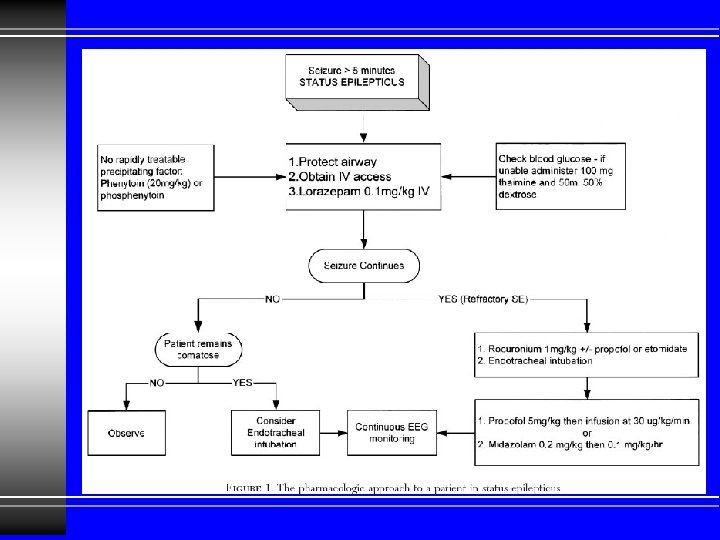
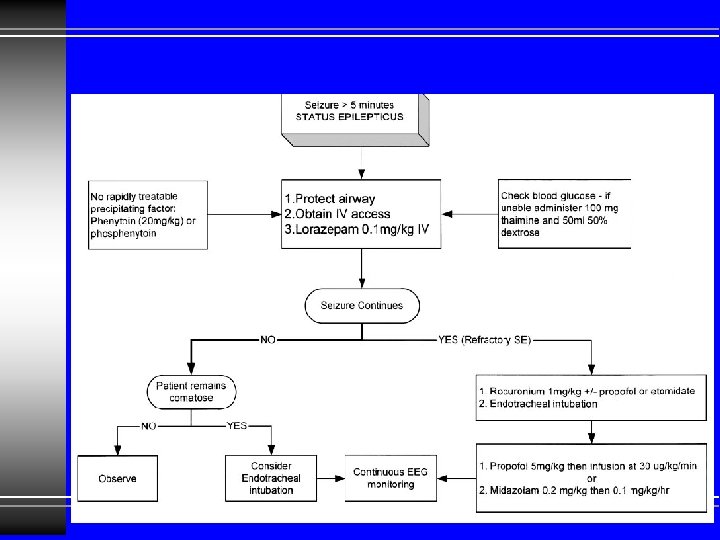
Lorazepam u Propofol, u Midazolam, or u Etomidate u Rocuronium (1 mg/kg) u Succinylcholine u
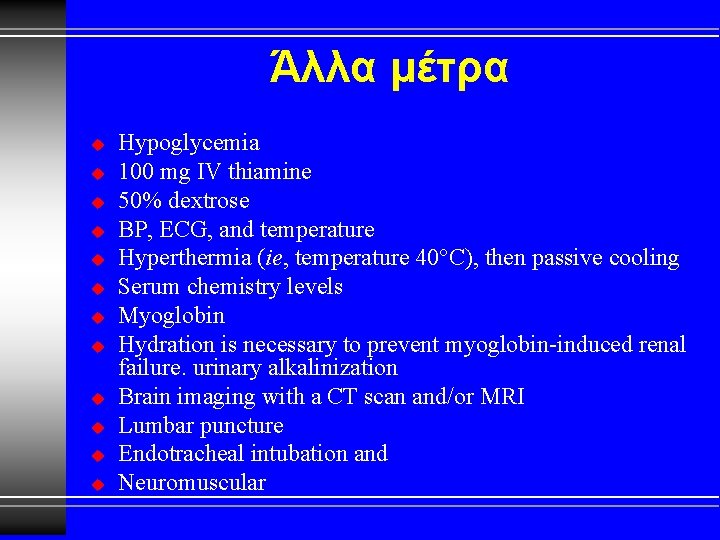
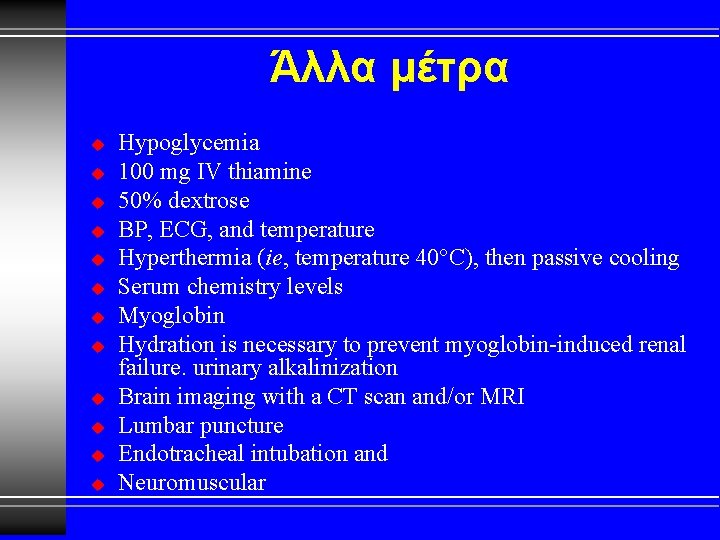
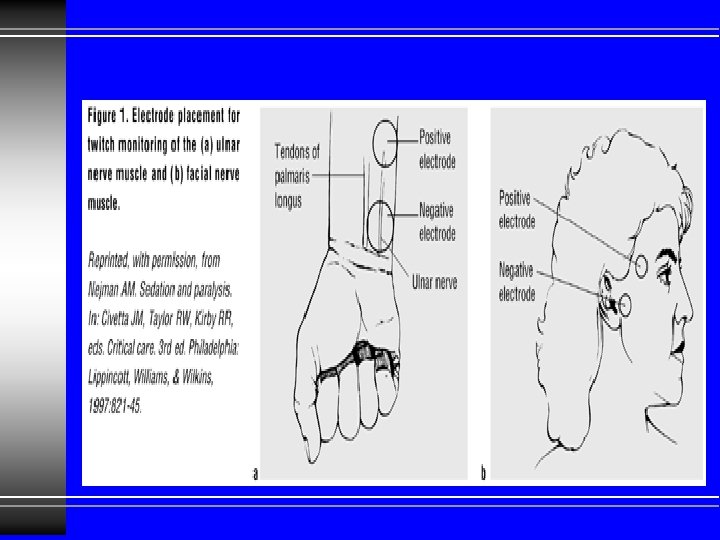
Άλλα μέτρα u u u Hypoglycemia 100 mg IV thiamine 50% dextrose BP, ECG, and temperature Hyperthermia (ie, temperature 40°C), then passive cooling Serum chemistry levels Myoglobin Hydration is necessary to prevent myoglobin-induced renal failure. urinary alkalinization Brain imaging with a CT scan and/or MRI Lumbar puncture Endotracheal intubation and Neuromuscular

Φάρμακα Diazepam, u Lorazepam, u Midazolam, u Phenytoin, u Fosphenytoin, and u Phenobarbital u l have all been used as first-line therapy for the termination of status epilepticus.
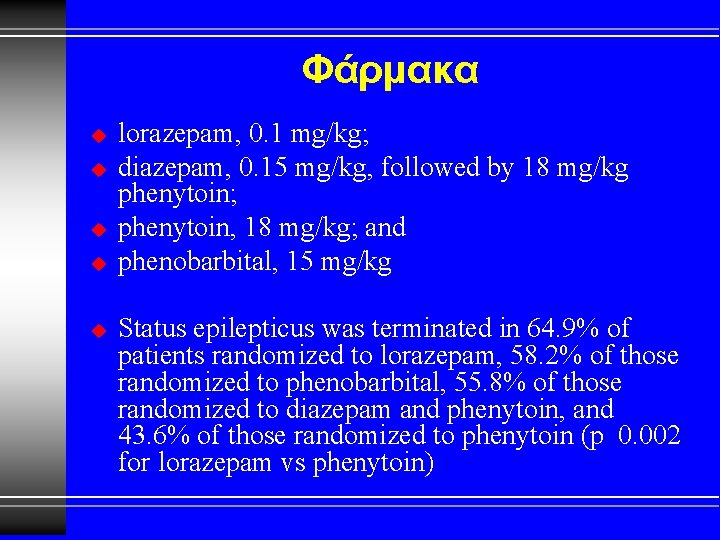
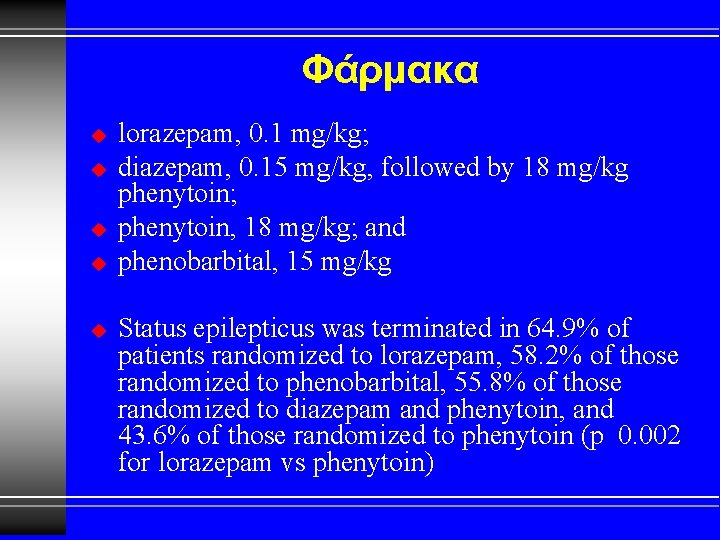
Φάρμακα u u u lorazepam, 0. 1 mg/kg; diazepam, 0. 15 mg/kg, followed by 18 mg/kg phenytoin; phenytoin, 18 mg/kg; and phenobarbital, 15 mg/kg Status epilepticus was terminated in 64. 9% of patients randomized to lorazepam, 58. 2% of those randomized to phenobarbital, 55. 8% of those randomized to diazepam and phenytoin, and 43. 6% of those randomized to phenytoin (p 0. 002 for lorazepam vs phenytoin)
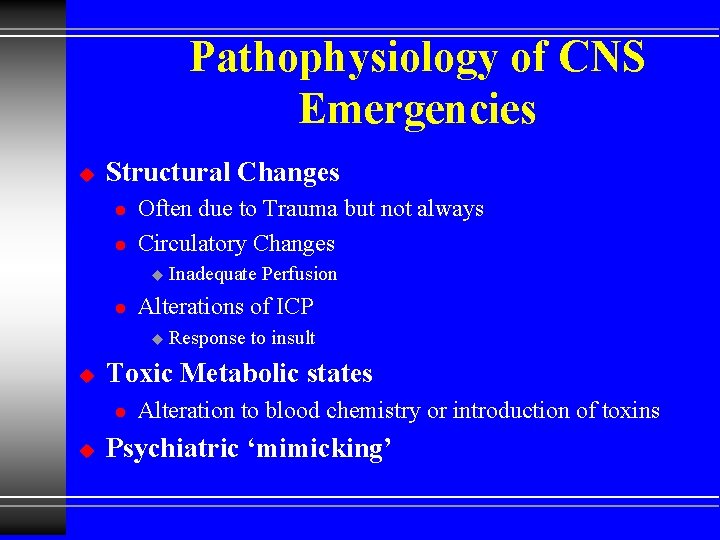
Pathophysiology of CNS Emergencies u Structural Changes l l Often due to Trauma but not always Circulatory Changes u l Alterations of ICP u u Response to insult Toxic Metabolic states l u Inadequate Perfusion Alteration to blood chemistry or introduction of toxins Psychiatric ‘mimicking’
Altered Mental Status
Coma u u A decreased state of consciousness from which a patient cannot be aroused Mechanisms Structural lesions l Toxic Metabolic states l Psychiatric ‘mimicking’ l
Brain injury u Recall that Brain injury is often shown by: Altered Mental Status l Seizures l Localizing signs l
Is unconsciousness itself an immediate life threat? YES, IT IS! Loss of airway u Vomiting, aspiration u
Altered Mental State Manage ABC’s Before Investigating Cause!
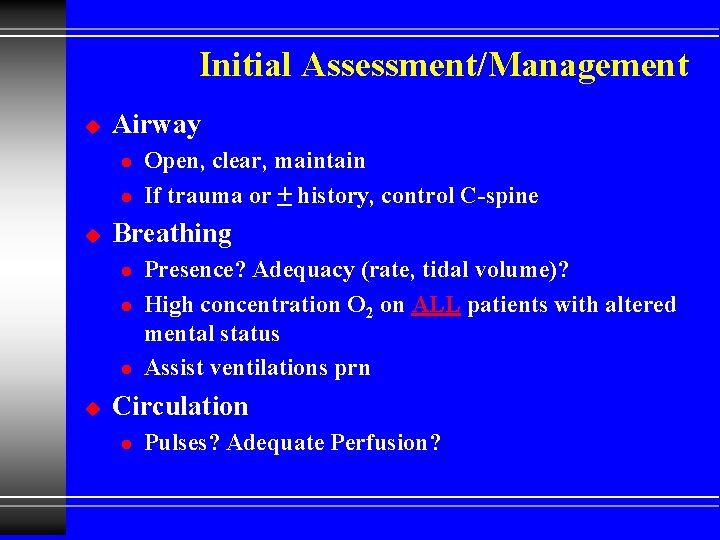
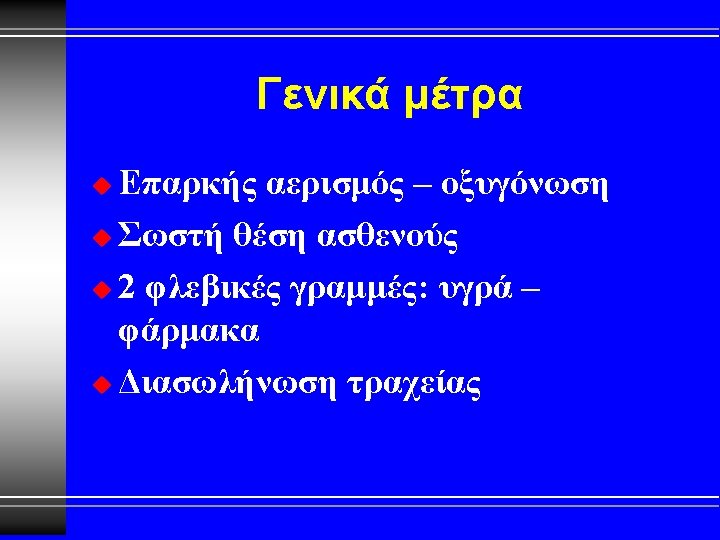
Initial Assessment/Management u Airway l l u Breathing l l l u Open, clear, maintain If trauma or + history, control C-spine Presence? Adequacy (rate, tidal volume)? High concentration O 2 on ALL patients with altered mental status Assist ventilations prn Circulation l Pulses? Adequate Perfusion?
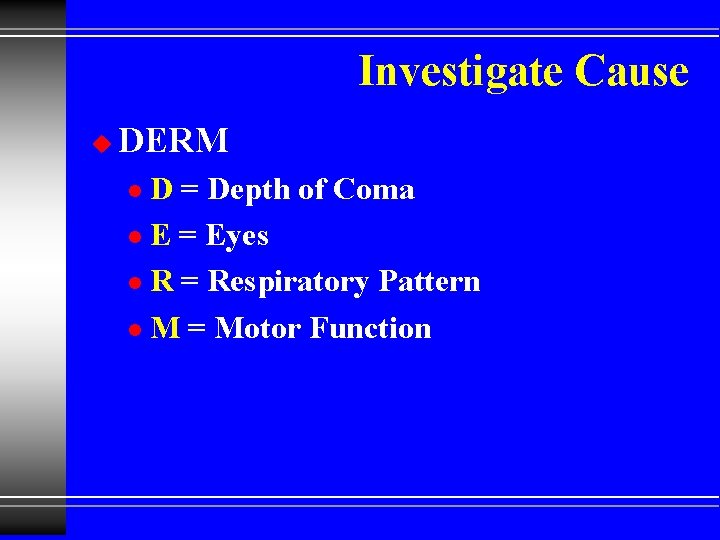
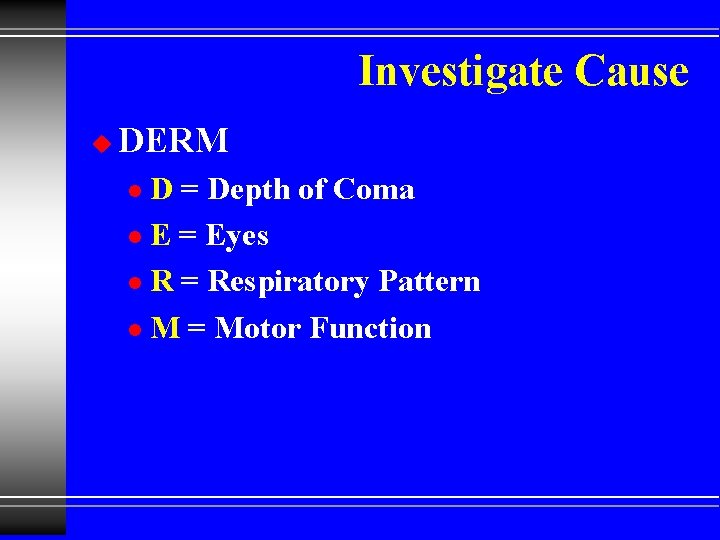
Investigate Cause u DERM D = Depth of Coma l E = Eyes l R = Respiratory Pattern l M = Motor Function l
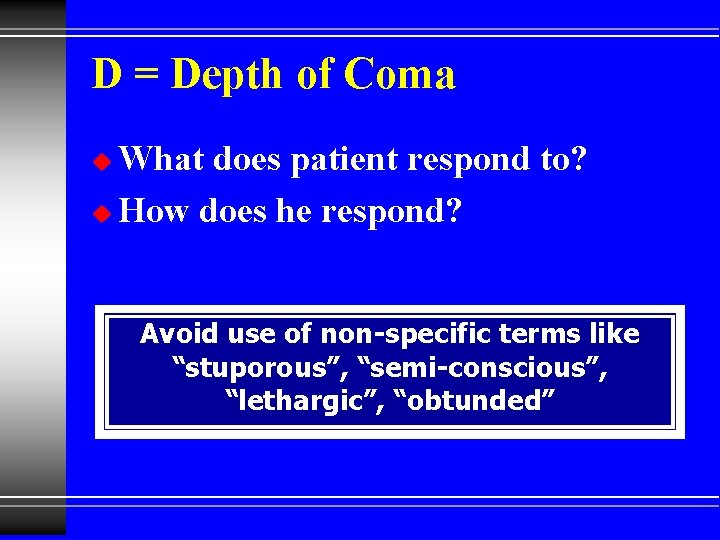
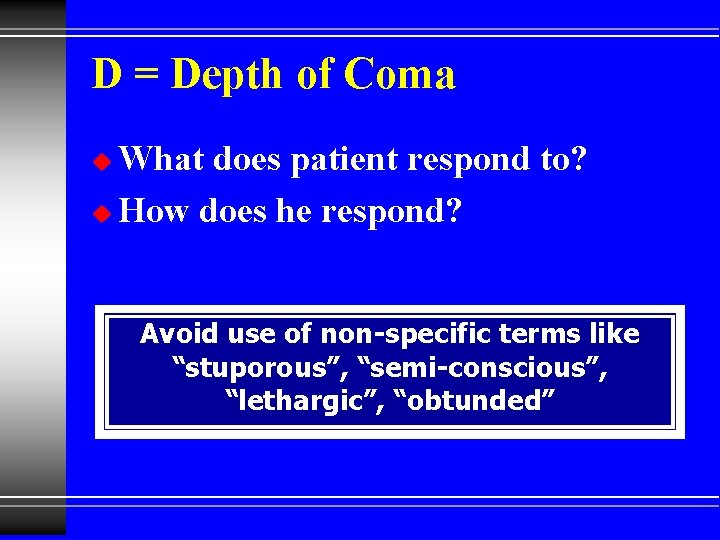
D = Depth of Coma What does patient respond to? u How does he respond? u Avoid use of non-specific terms like “stuporous”, “semi-conscious”, “lethargic”, “obtunded”
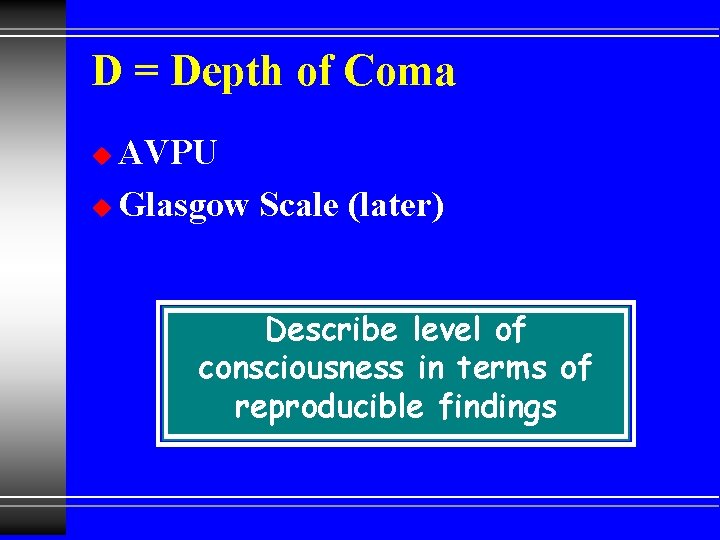
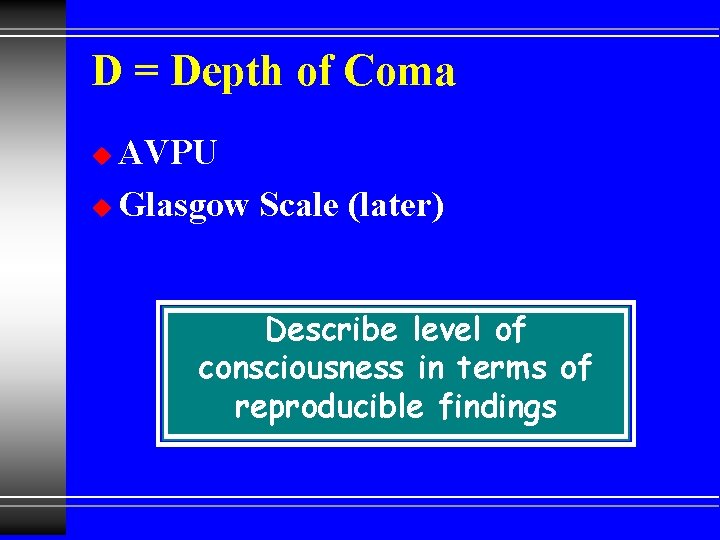
D = Depth of Coma AVPU u Glasgow Scale (later) u Describe level of consciousness in terms of reproducible findings
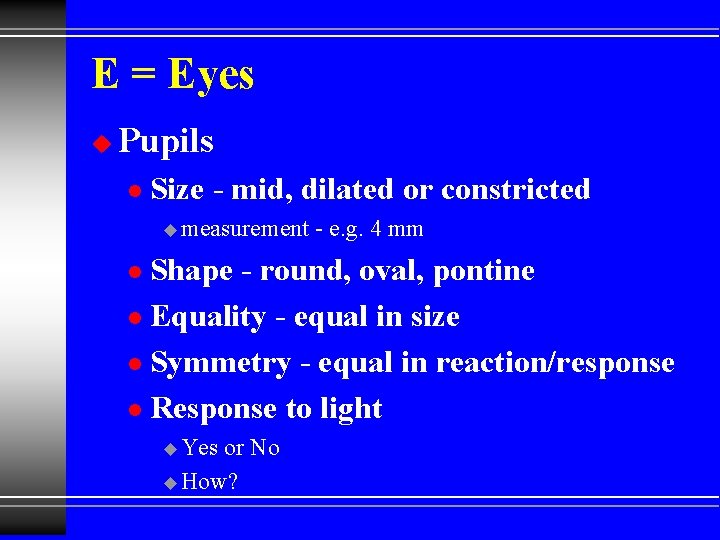
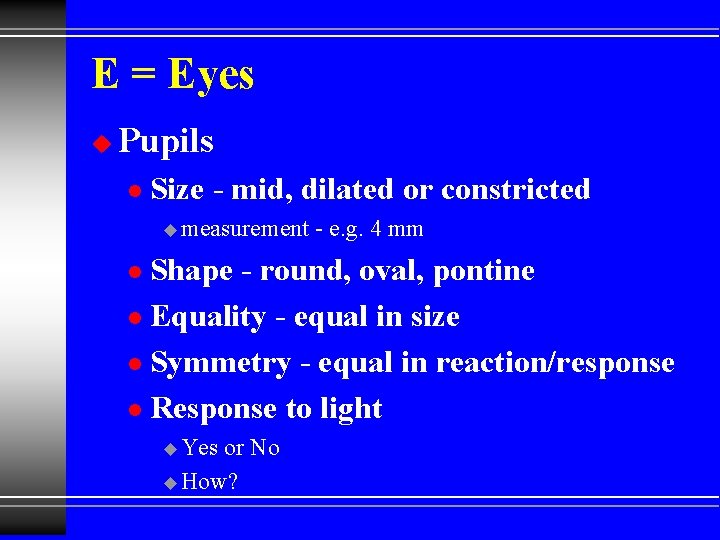
E = Eyes u Pupils l Size - mid, dilated or constricted u measurement - e. g. 4 mm Shape - round, oval, pontine l Equality - equal in size l Symmetry - equal in reaction/response l Response to light l u Yes or No u How?
R = Respiratory Pattern u Depth l u Unusually deep or shallow? Pattern l Regular or Unusual pattern u. Can you identify the pattern?
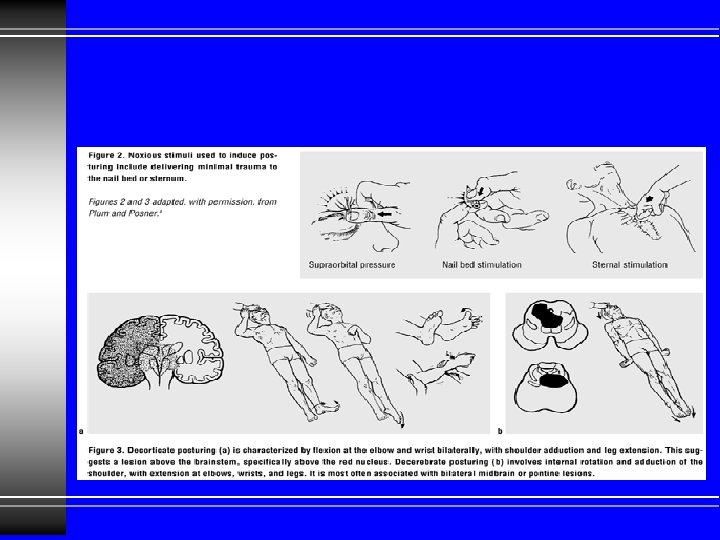
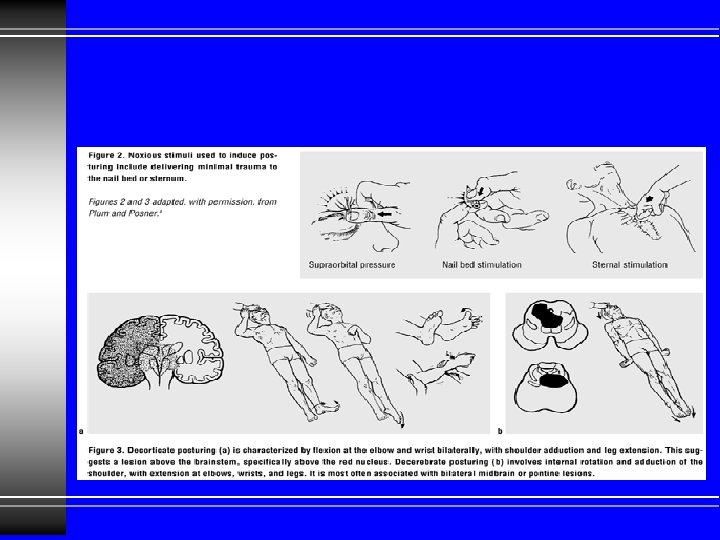
M = Motor Function u Paralysis? l u Muscle tone? l u Where? What is it like? Posturing? l u Rigid or Flaccid Movement? l u Where? How? Symmetrical Motor Function?
Physical Exam u Vital Signs Shock? l Increased ICP? l Hypoxia/Hypercarbia l u Diagnostics Dysrhythmias? l Blood glucose l Oxygen saturation l
Physical Exam u Detailed (Head-to-Toe) Exam Injuries causing coma? l Injuries caused by coma? l Clues to the cause l
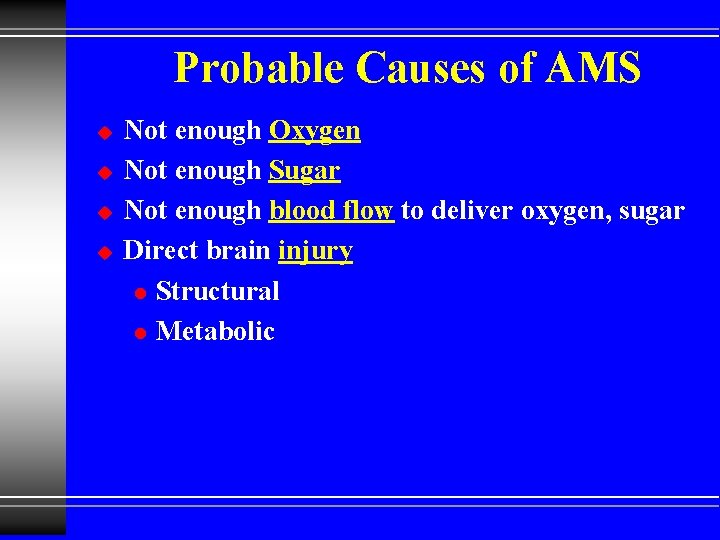
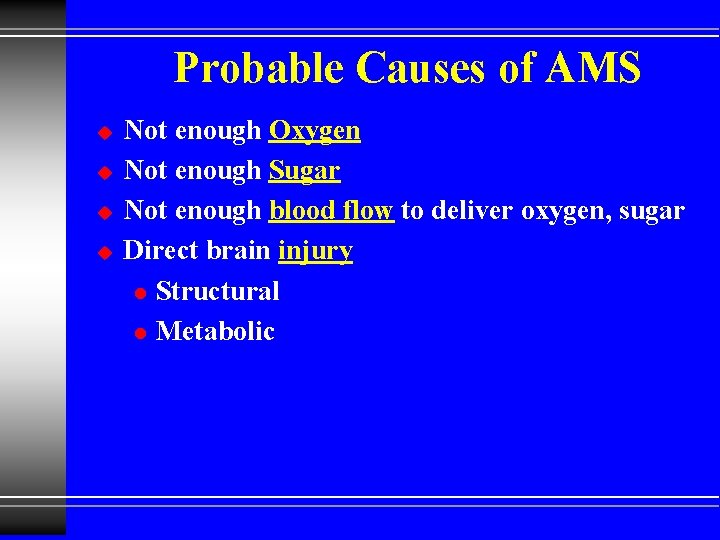
Probable Causes of AMS u u Not enough Oxygen Not enough Sugar Not enough blood flow to deliver oxygen, sugar Direct brain injury l Structural l Metabolic
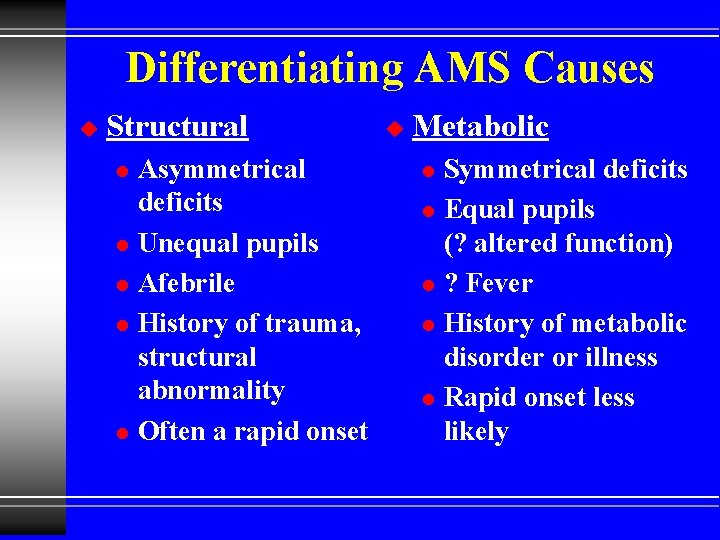
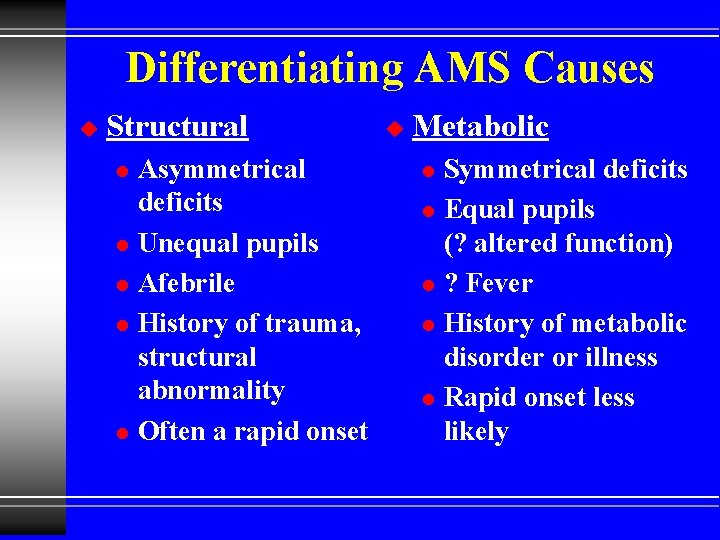
Differentiating AMS Causes u Structural l l Asymmetrical deficits Unequal pupils Afebrile History of trauma, structural abnormality Often a rapid onset u Metabolic l l l Symmetrical deficits Equal pupils (? altered function) ? Fever History of metabolic disorder or illness Rapid onset less likely
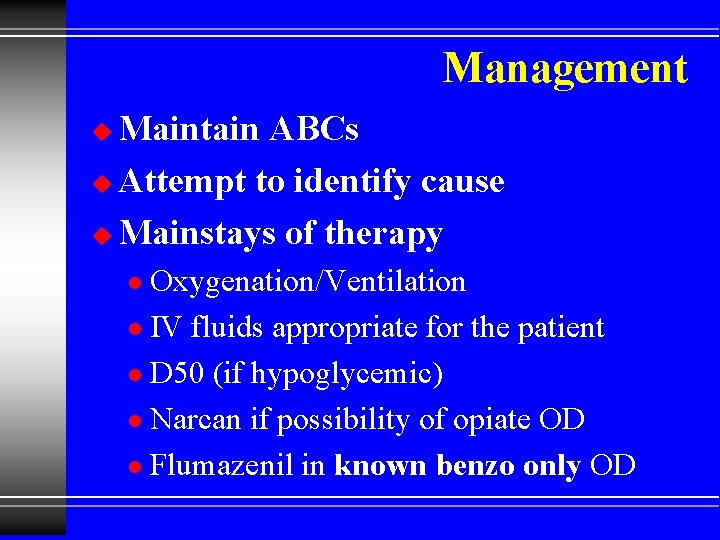
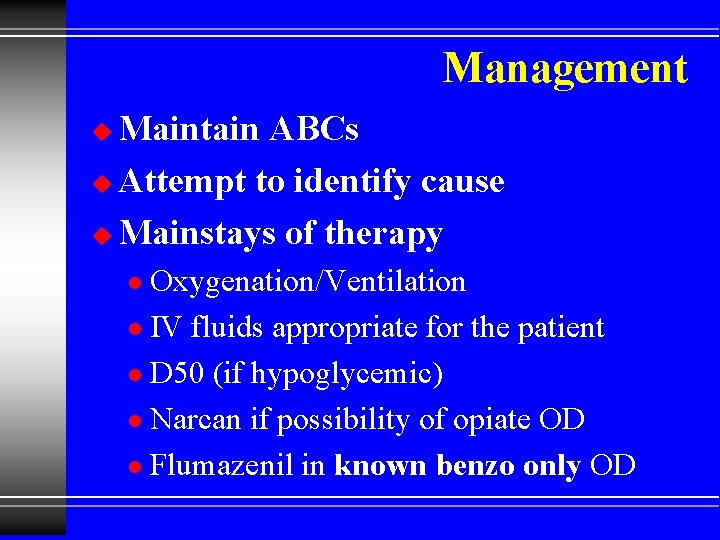
Management Maintain ABCs u Attempt to identify cause u Mainstays of therapy u Oxygenation/Ventilation l IV fluids appropriate for the patient l D 50 (if hypoglycemic) l Narcan if possibility of opiate OD l Flumazenil in known benzo only OD l
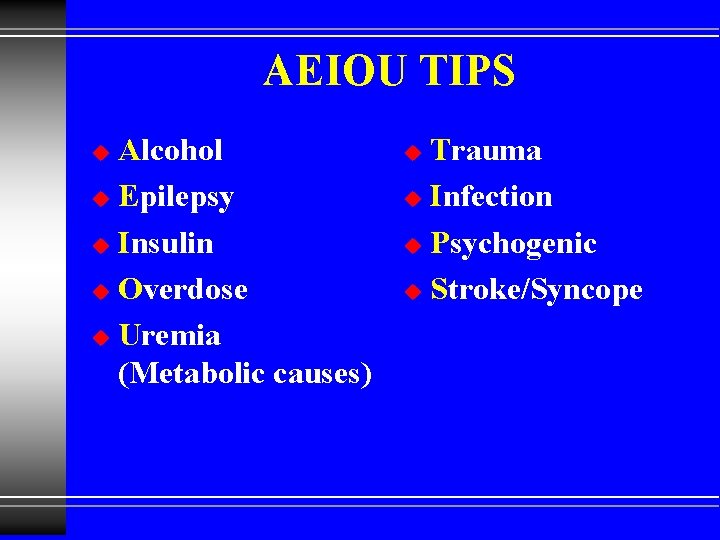
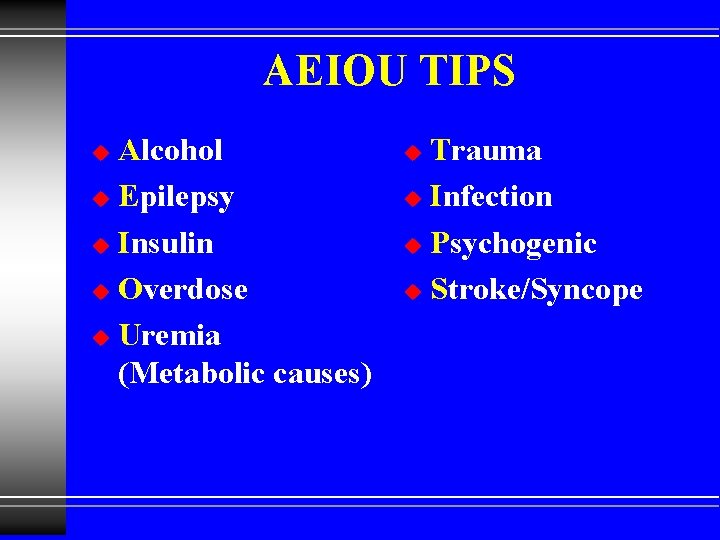
AEIOU TIPS Alcohol u Epilepsy u Insulin u Overdose u Uremia (Metabolic causes) u Trauma u Infection u Psychogenic u Stroke/Syncope u
Seizures AEIOU TIPS
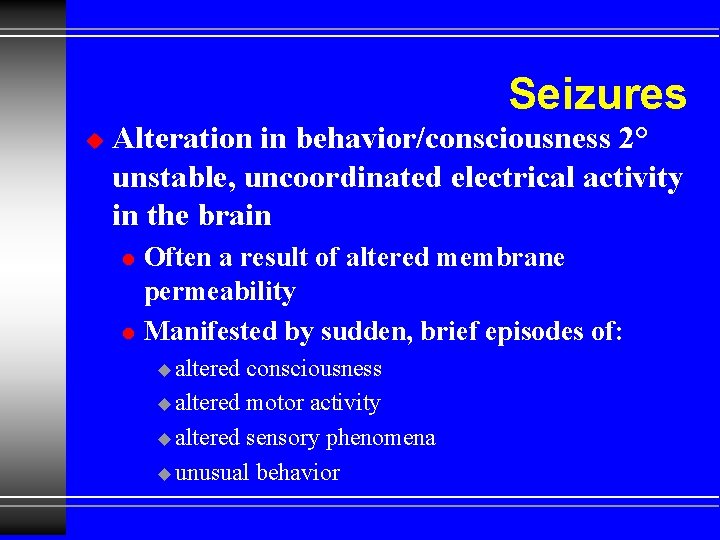
Seizures u Alteration in behavior/consciousness 2° unstable, uncoordinated electrical activity in the brain l l Often a result of altered membrane permeability Manifested by sudden, brief episodes of: u altered consciousness u altered motor activity u altered sensory phenomena u unusual behavior
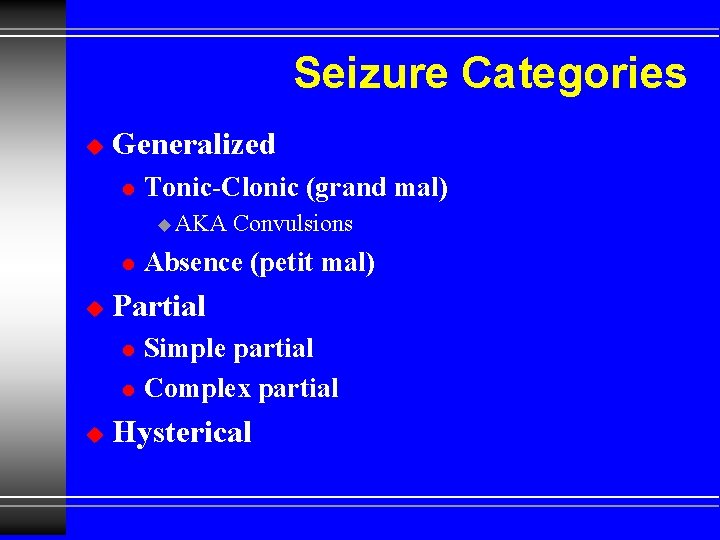
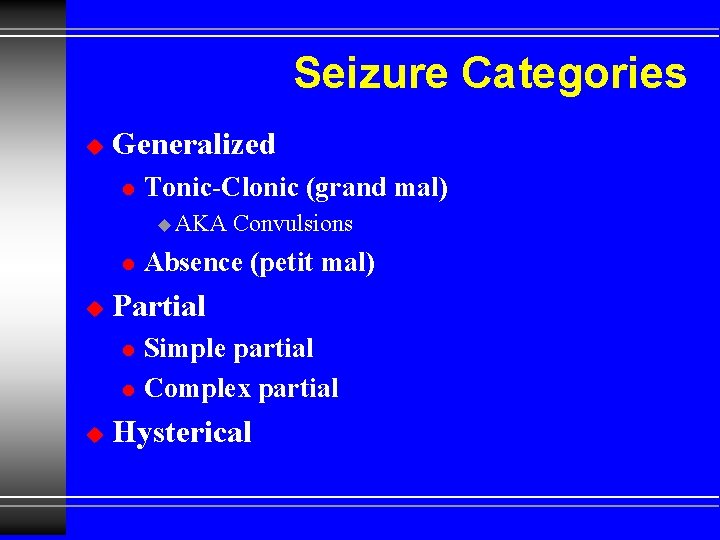
Seizure Categories u Generalized l Tonic-Clonic (grand mal) u AKA l u Absence (petit mal) Partial l l u Convulsions Simple partial Complex partial Hysterical
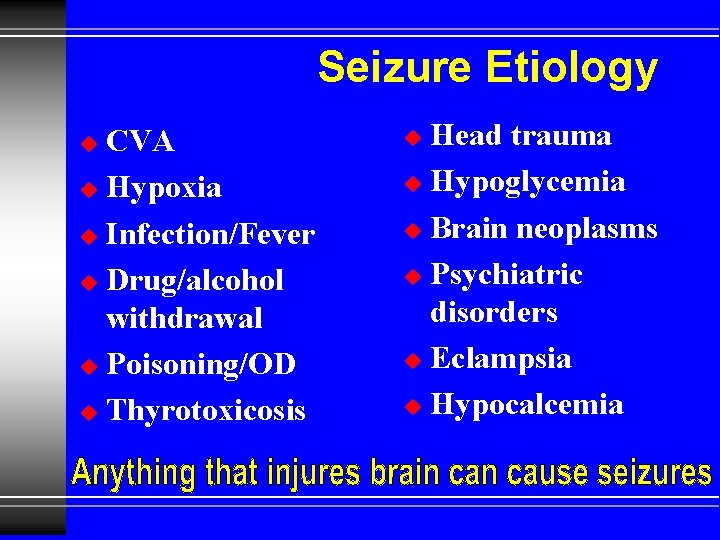
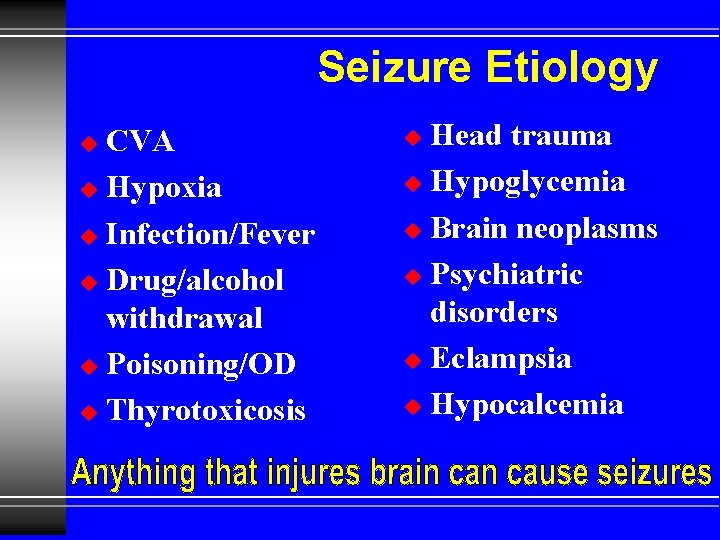
Seizure Etiology CVA u Hypoxia u Infection/Fever u Drug/alcohol withdrawal u Poisoning/OD u Thyrotoxicosis u Head trauma u Hypoglycemia u Brain neoplasms u Psychiatric disorders u Eclampsia u Hypocalcemia u
Seizures Etiology Most epileptic seizures are idiopathic in origin

Generalized Seizures u Petit Mal Absence Sz l Children l No LOC l u Grand mal aka Convulsions l Common l Often w/Aura l Sudden LOC l Tonic / Clonic l Postictal phase l Status epilepticus l
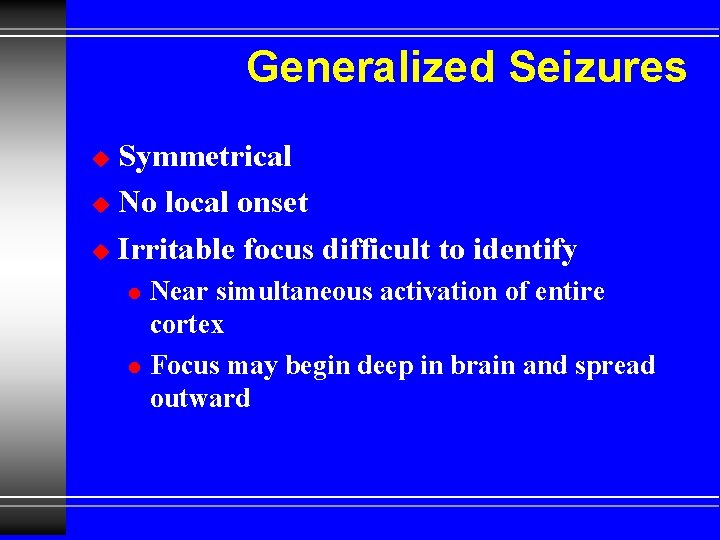
Generalized Seizures Symmetrical u No local onset u Irritable focus difficult to identify u l l Near simultaneous activation of entire cortex Focus may begin deep in brain and spread outward
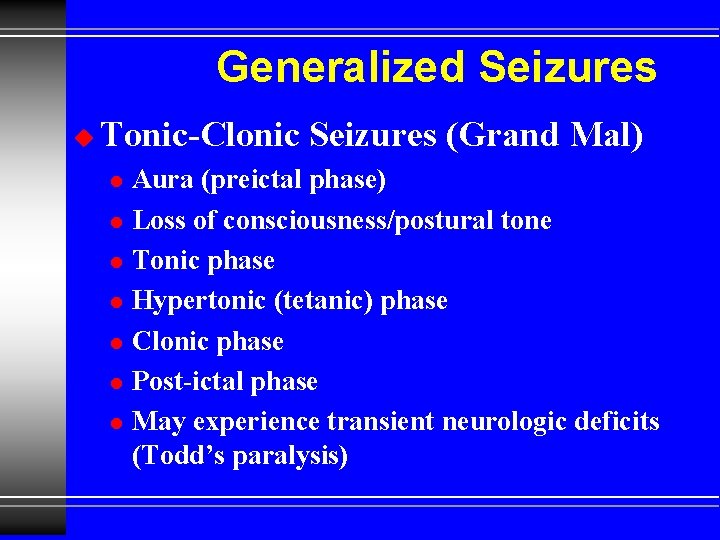
Generalized Seizures u Tonic-Clonic Seizures (Grand Mal) l l l l Aura (preictal phase) Loss of consciousness/postural tone Tonic phase Hypertonic (tetanic) phase Clonic phase Post-ictal phase May experience transient neurologic deficits (Todd’s paralysis)
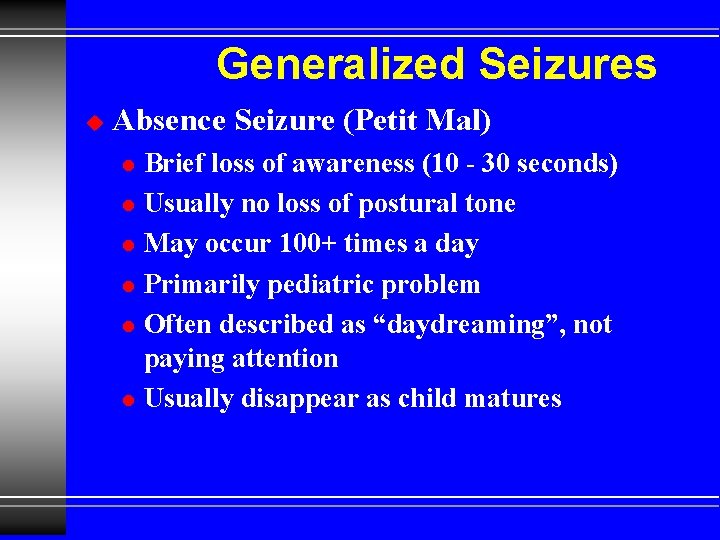
Generalized Seizures u Absence Seizure (Petit Mal) l l l Brief loss of awareness (10 - 30 seconds) Usually no loss of postural tone May occur 100+ times a day Primarily pediatric problem Often described as “daydreaming”, not paying attention Usually disappear as child matures
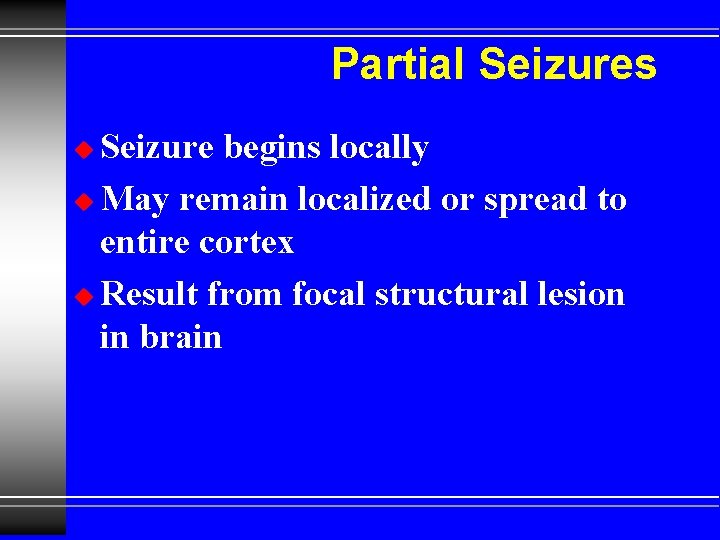
Partial Seizures Seizure begins locally u May remain localized or spread to entire cortex u Result from focal structural lesion in brain u
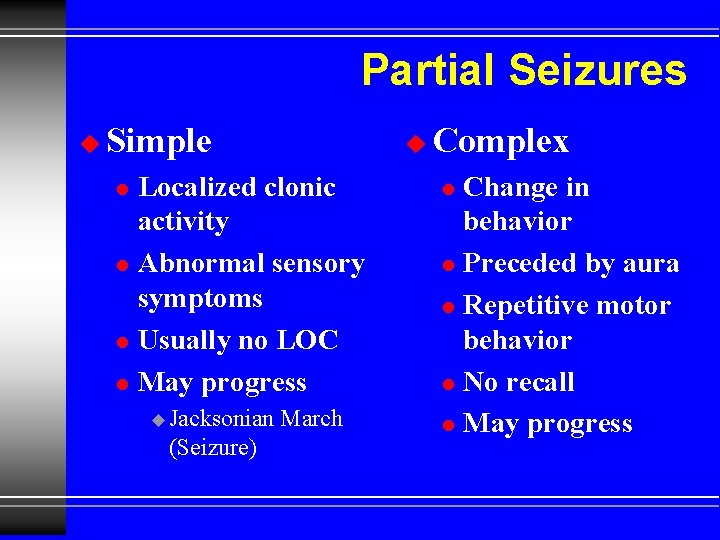
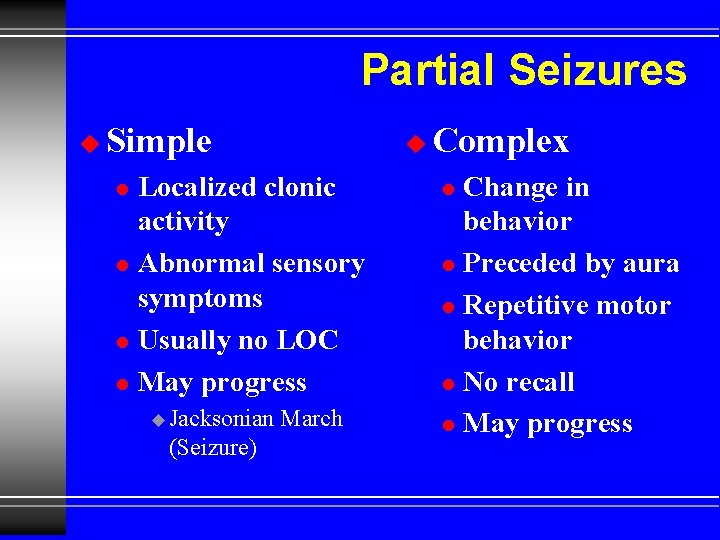
Partial Seizures u Simple u Localized clonic activity l Abnormal sensory symptoms l Usually no LOC l May progress l u Jacksonian (Seizure) March Complex Change in behavior l Preceded by aura l Repetitive motor behavior l No recall l May progress l
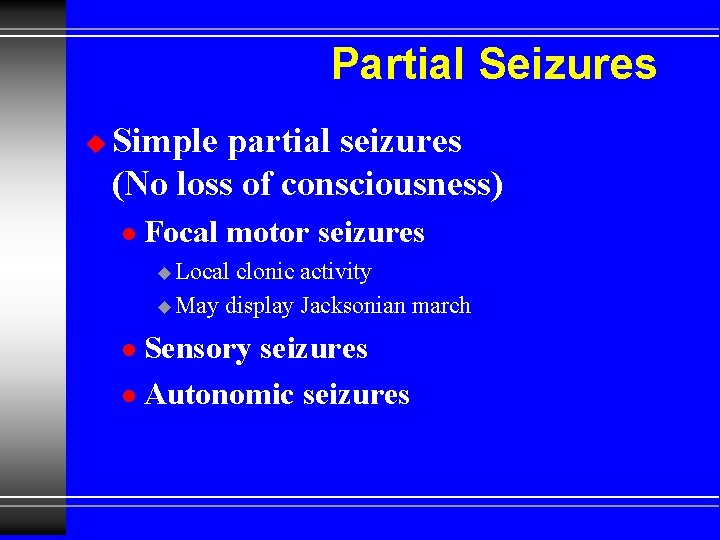
Partial Seizures u Simple partial seizures (No loss of consciousness) l Focal motor seizures u Local clonic activity u May display Jacksonian march Sensory seizures l Autonomic seizures l
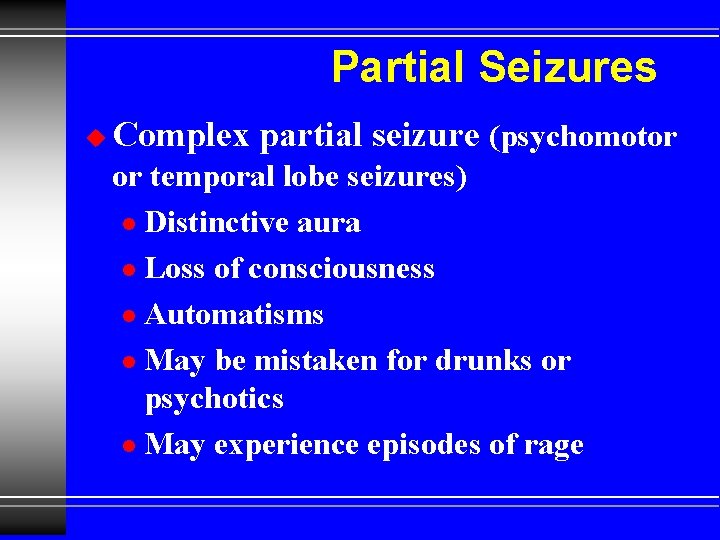
Partial Seizures u Complex partial seizure (psychomotor or temporal lobe seizures) l Distinctive aura l Loss of consciousness l Automatisms l May be mistaken for drunks or psychotics l May experience episodes of rage
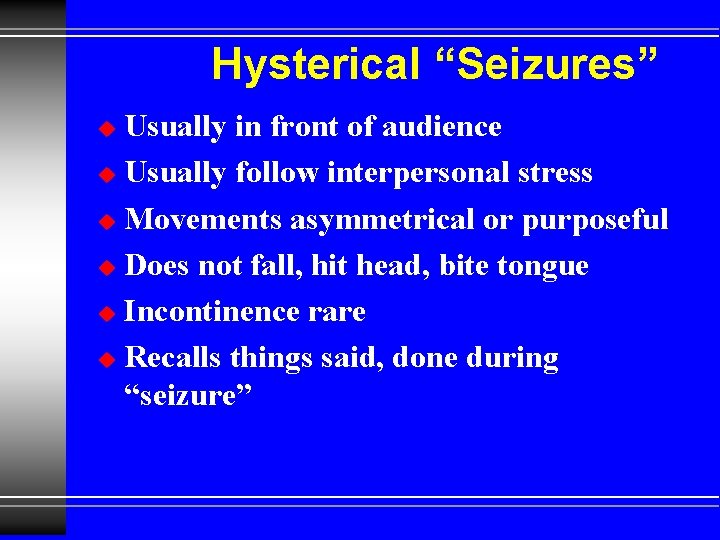
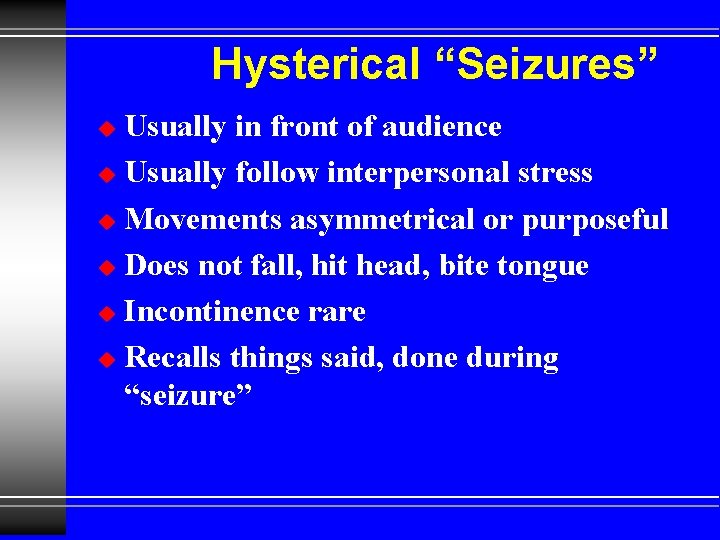
Hysterical “Seizures” Usually in front of audience u Usually follow interpersonal stress u Movements asymmetrical or purposeful u Does not fall, hit head, bite tongue u Incontinence rare u Recalls things said, done during “seizure” u
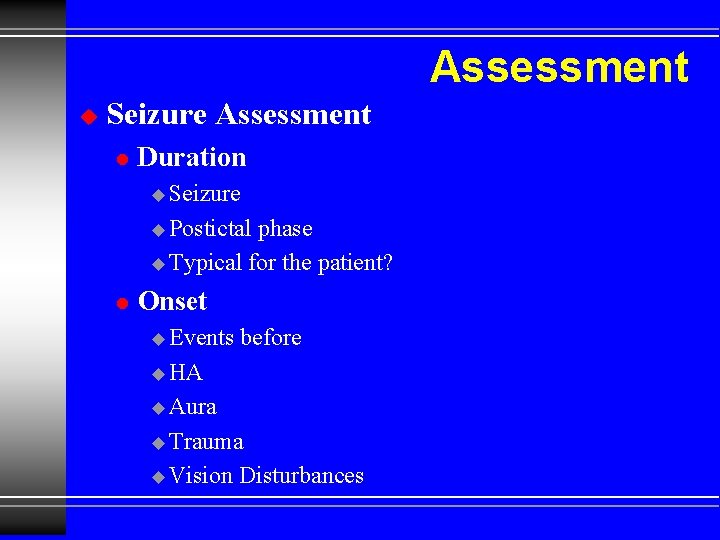
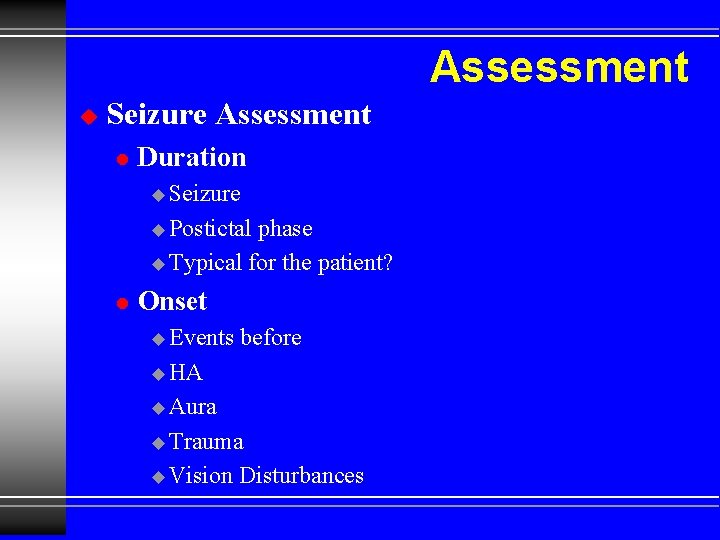
Assessment u Seizure Assessment l Duration u Seizure u Postictal phase u Typical for the patient? l Onset u Events before u HA u Aura u Trauma u Vision Disturbances
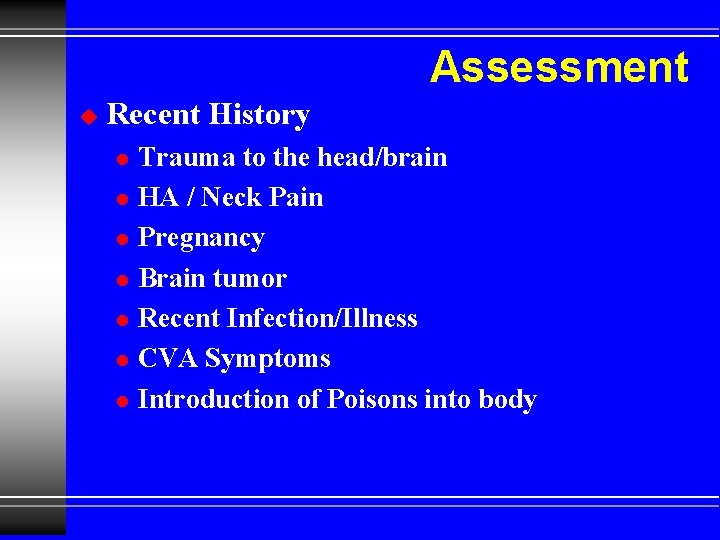
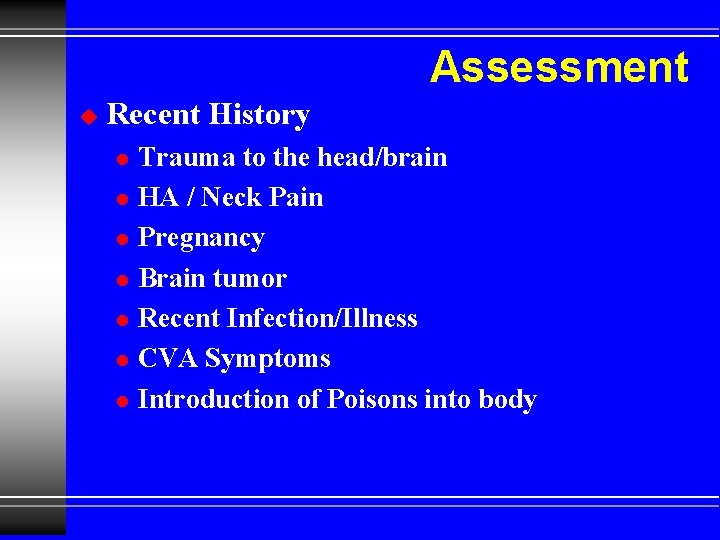
Assessment u Recent History l l l l Trauma to the head/brain HA / Neck Pain Pregnancy Brain tumor Recent Infection/Illness CVA Symptoms Introduction of Poisons into body
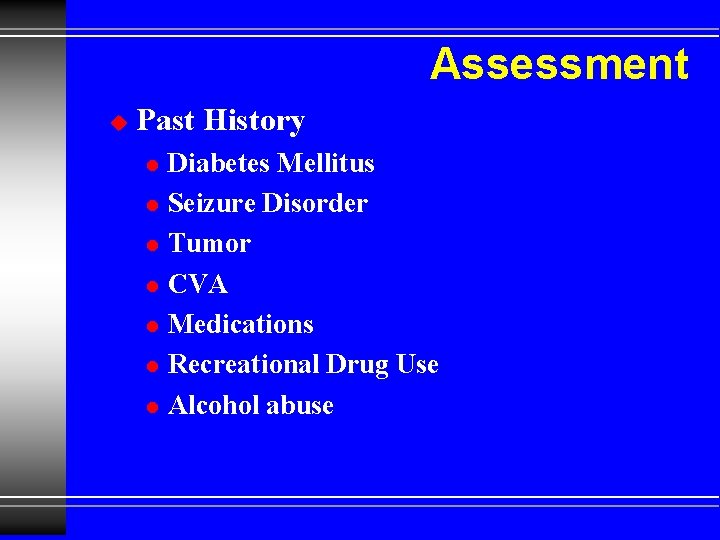
Assessment u Past History l l l l Diabetes Mellitus Seizure Disorder Tumor CVA Medications Recreational Drug Use Alcohol abuse
Assessment u Physical Exam l l l Evidence of trauma Evidence of alcohol, drug abuse Rash, stiff neck Pregnant CVA Signs Incontinence
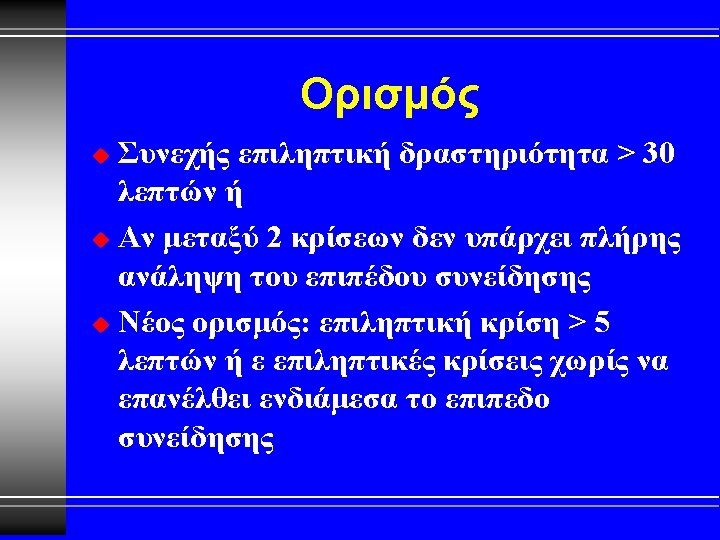
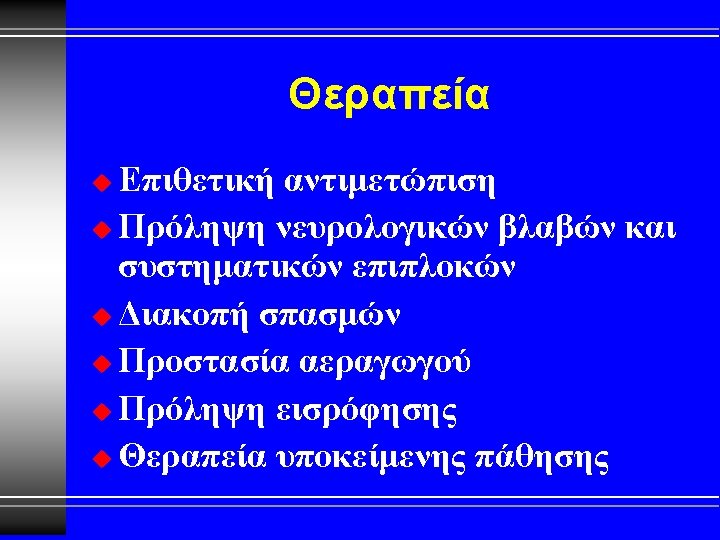
Status Epilepticus Two or more seizures without intervening conscious period u Usually due to medication noncompliance u Management same as for other Seizures just more aggressive u
Seizure Management u Patient actively seizing l l l Do NOT restrain Do NOT put anything in mouth Oxygen NRB if possible ECG Monitor when possible IV Access u Lg Bore, NS u Assess blood glucose
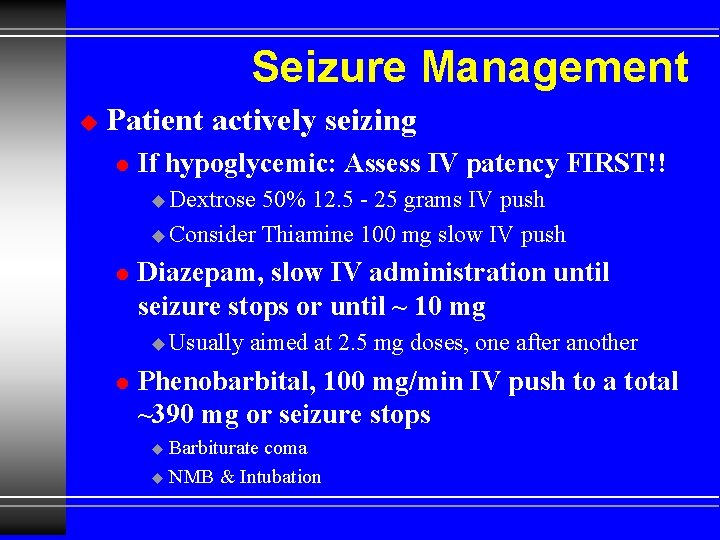
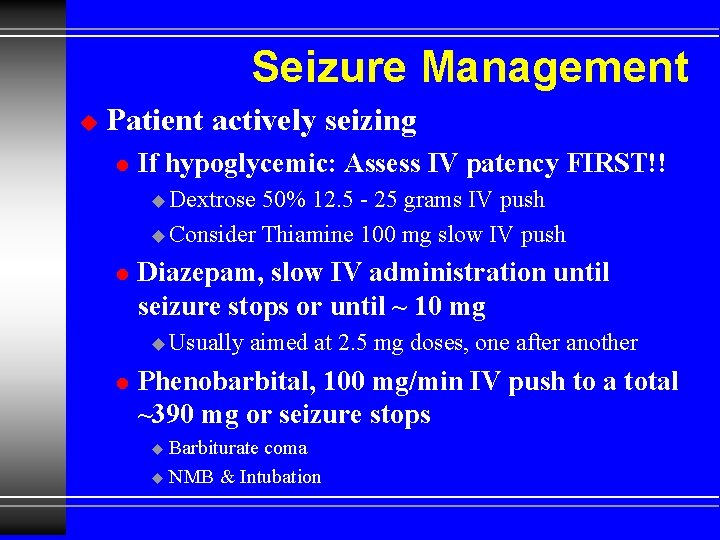
Seizure Management u Patient actively seizing l If hypoglycemic: Assess IV patency FIRST!! u Dextrose 50% 12. 5 - 25 grams IV push u Consider Thiamine 100 mg slow IV push l Diazepam, slow IV administration until seizure stops or until ~ 10 mg u Usually l aimed at 2. 5 mg doses, one after another Phenobarbital, 100 mg/min IV push to a total ~390 mg or seizure stops Barbiturate coma u NMB & Intubation u
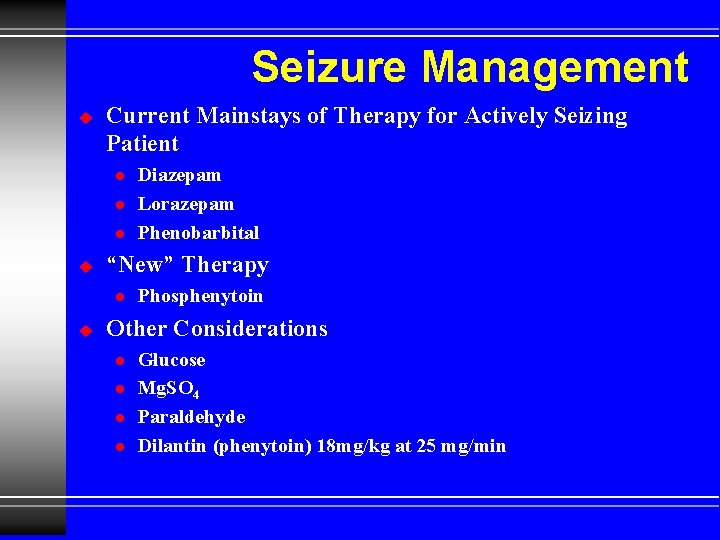
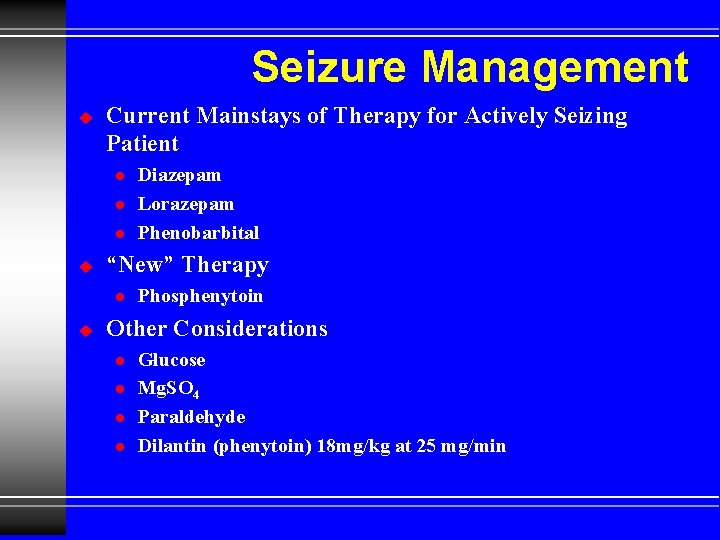
Seizure Management u Current Mainstays of Therapy for Actively Seizing Patient l l l u “New” Therapy l u Diazepam Lorazepam Phenobarbital Phosphenytoin Other Considerations l l Glucose Mg. SO 4 Paraldehyde Dilantin (phenytoin) 18 mg/kg at 25 mg/min
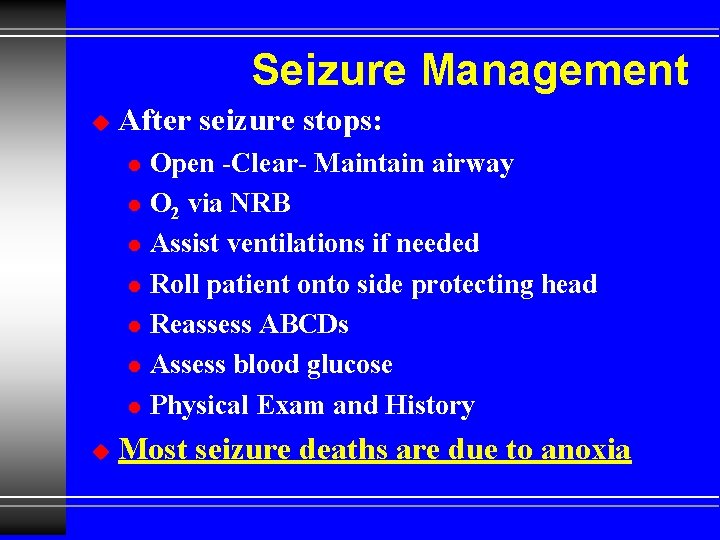
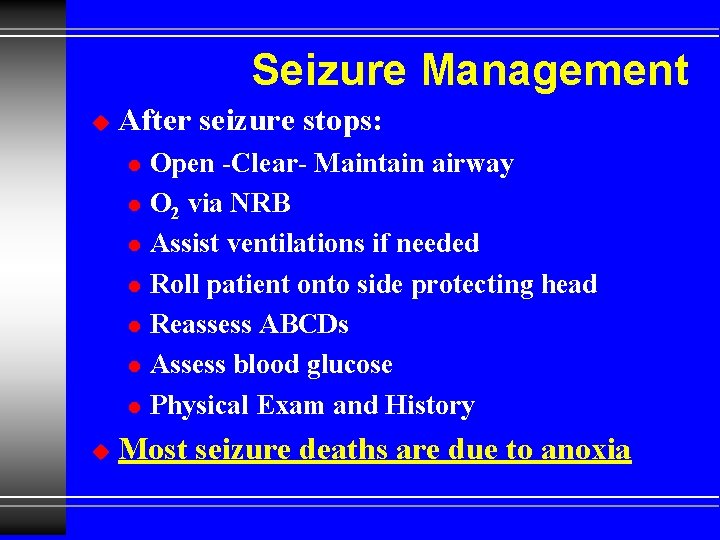
Seizure Management u After seizure stops: l l l l u Open -Clear- Maintain airway O 2 via NRB Assist ventilations if needed Roll patient onto side protecting head Reassess ABCDs Assess blood glucose Physical Exam and History Most seizure deaths are due to anoxia
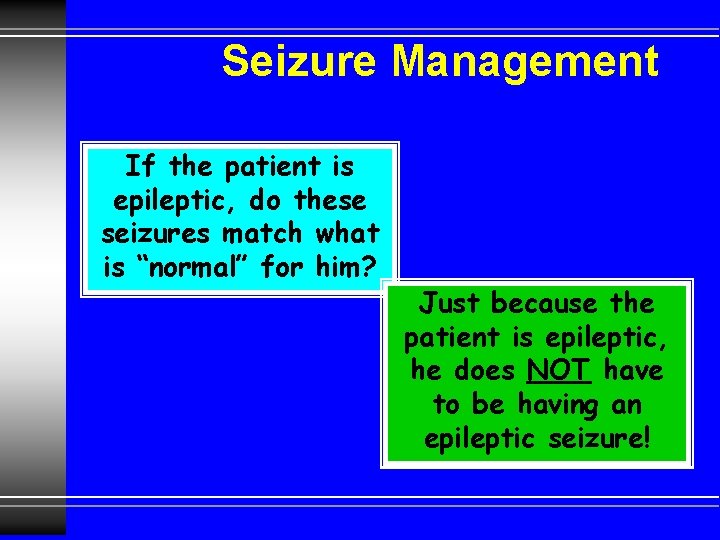
Seizure Management If the patient is epileptic, do these seizures match what is “normal” for him? Just because the patient is epileptic, he does NOT have to be having an epileptic seizure!
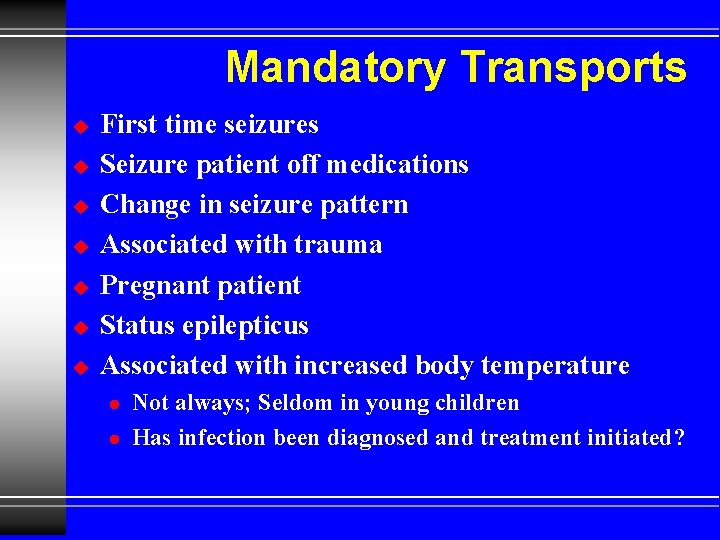
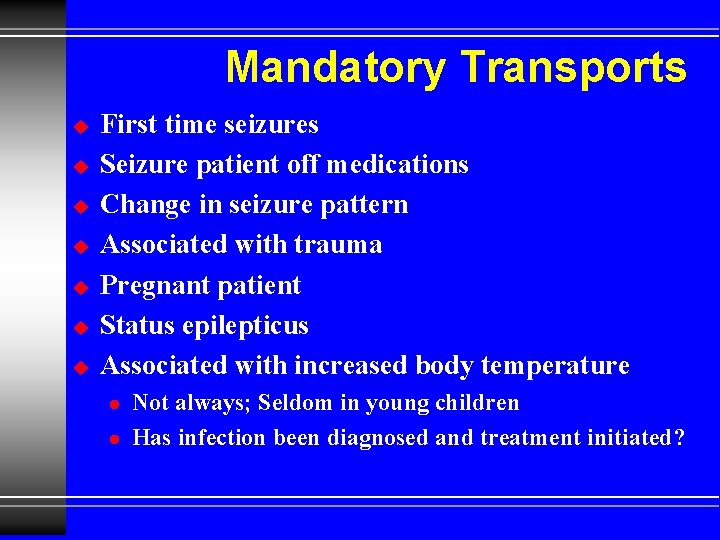
Mandatory Transports u u u u First time seizures Seizure patient off medications Change in seizure pattern Associated with trauma Pregnant patient Status epilepticus Associated with increased body temperature l l Not always; Seldom in young children Has infection been diagnosed and treatment initiated?
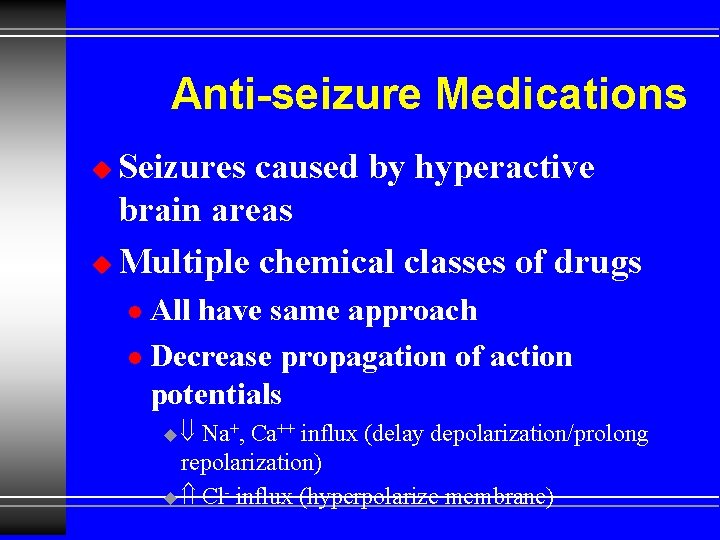
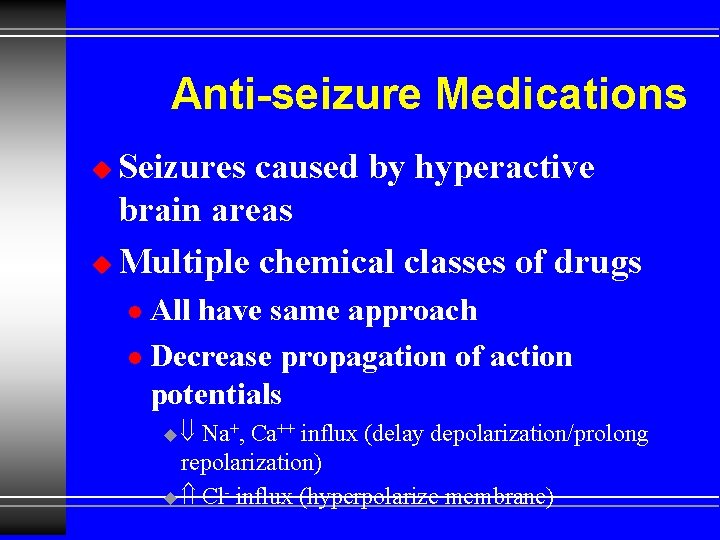
Anti-seizure Medications Seizures caused by hyperactive brain areas u Multiple chemical classes of drugs u All have same approach l Decrease propagation of action potentials l u Na+, Ca++ influx (delay depolarization/prolong repolarization) u Cl- influx (hyperpolarize membrane)
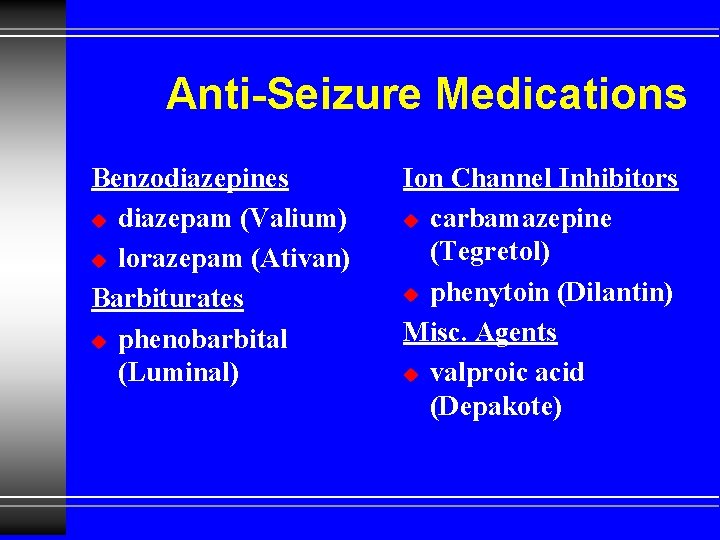
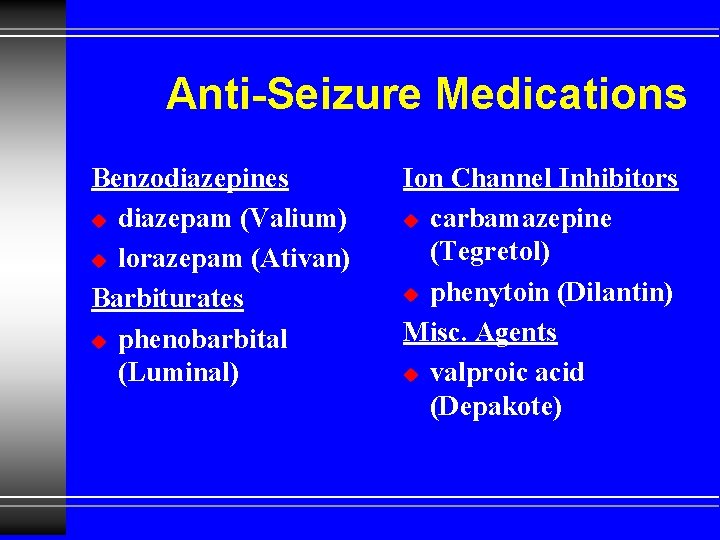
Anti-Seizure Medications Benzodiazepines u diazepam (Valium) u lorazepam (Ativan) Barbiturates u phenobarbital (Luminal) Ion Channel Inhibitors u carbamazepine (Tegretol) u phenytoin (Dilantin) Misc. Agents u valproic acid (Depakote)
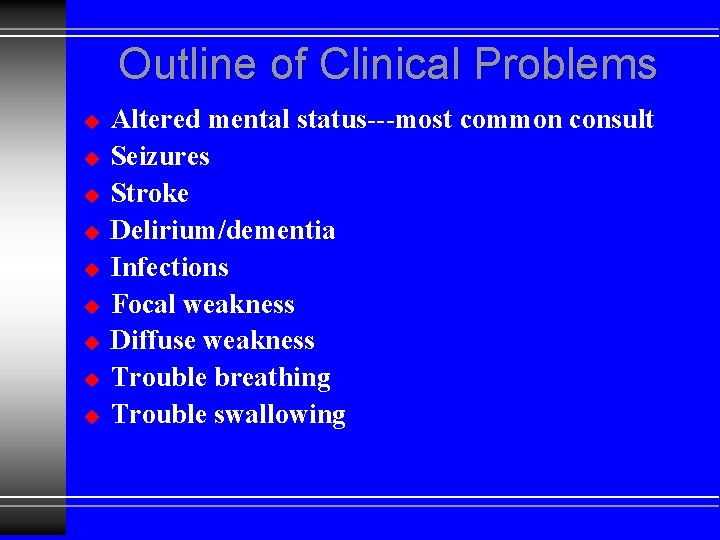
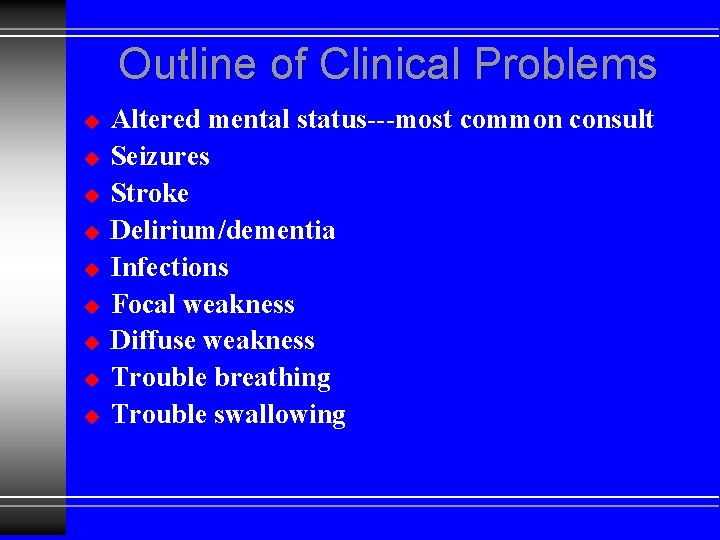
Outline of Clinical Problems u u u u u Altered mental status---most common consult Seizures Stroke Delirium/dementia Infections Focal weakness Diffuse weakness Trouble breathing Trouble swallowing
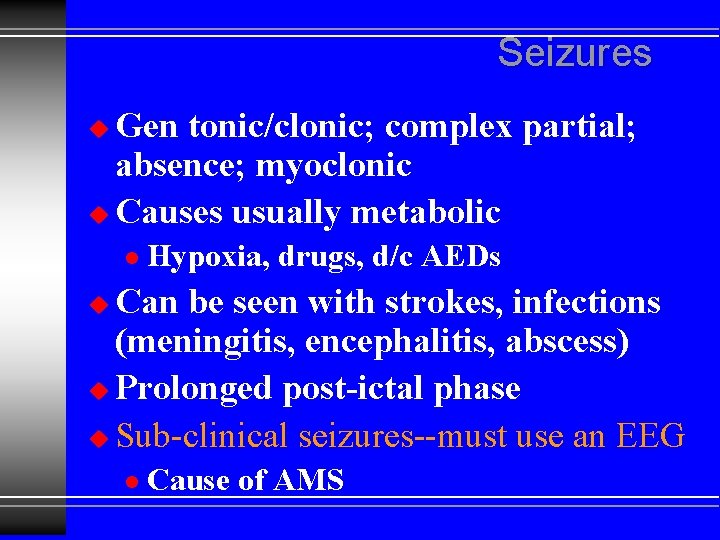
Seizures Gen tonic/clonic; complex partial; absence; myoclonic u Causes usually metabolic u l Hypoxia, drugs, d/c AEDs Can be seen with strokes, infections (meningitis, encephalitis, abscess) u Prolonged post-ictal phase u Sub-clinical seizures--must use an EEG u l Cause of AMS