Staphylococcus Aureus Mohsina Haq 1 Classification of Staphylococci

- Slides: 35
Staphylococcus Aureus Mohsina Haq 1
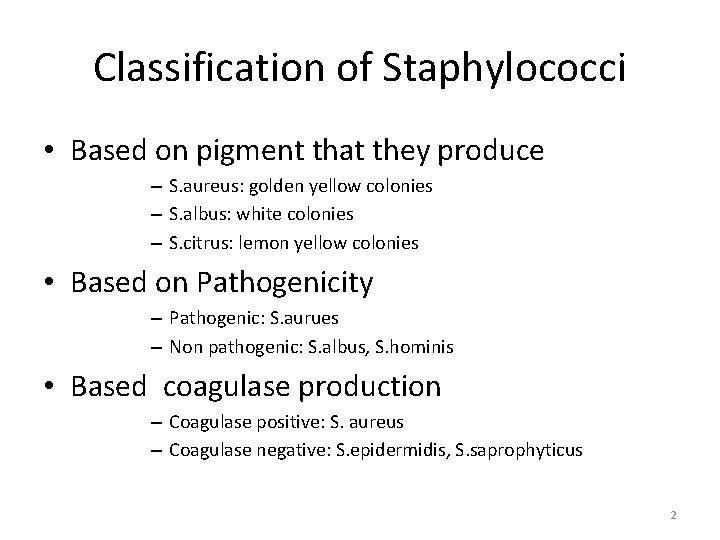
Classification of Staphylococci • Based on pigment that they produce – S. aureus: golden yellow colonies – S. albus: white colonies – S. citrus: lemon yellow colonies • Based on Pathogenicity – Pathogenic: S. aurues – Non pathogenic: S. albus, S. hominis • Based coagulase production – Coagulase positive: S. aureus – Coagulase negative: S. epidermidis, S. saprophyticus 2
Nomenclature • Family: • Staphylococcaceae • Genus: • Staphylococcus • Staphyle: bunch of grapes; kokkos: berries • Bacteria that form grape like clusters/resembles the shapes of berries 3
General Properties • Gram positive cocci • 1µm in diameter • • Non sporing Non motile Non flagellated Usually Non capsulated (some strains are capuslated) 4
Natural habitat • On human body • Nasal passages • Axilla • Perineum • In environment • In air • Contaminated surfaces • Contaminated fabric 5
Culture • • Aerobes Facultative anaerobes Optimum temperature: 35 C ph: 7. 5(6. 8 -7. 4) 6
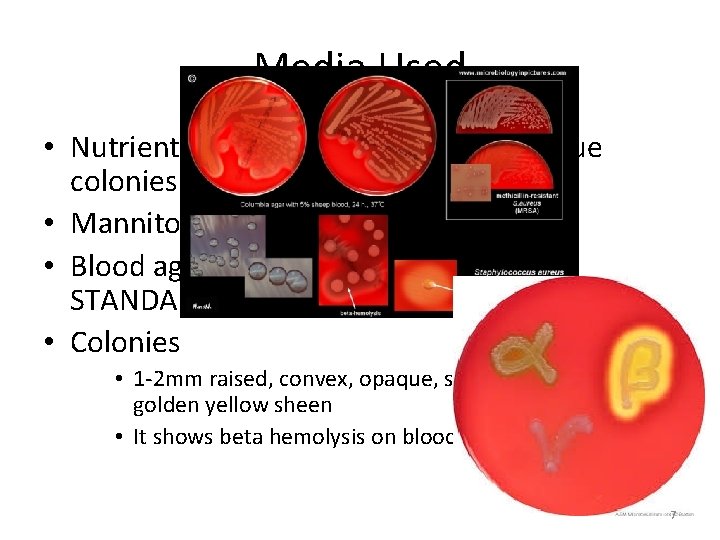
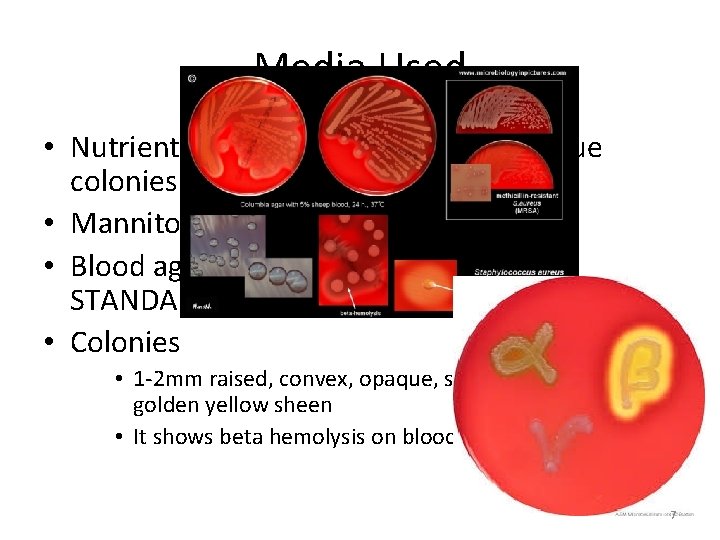
Media Used • Nutrient agar: golden yellow and opaque colonies • Mannitol salt agar • Blood agar: golden yellow color (GOLD STANDARD) • Colonies • 1 -2 mm raised, convex, opaque, smooth, shiny, with golden yellow sheen • It shows beta hemolysis on blood agar 7
Biochemical Properties • • • Catalase positive Oxidase negative Coagulase positive Liquefies gelatin Converts nitrates into nitrites Ferments glucose, lactose, maltose, sucrose and mannitol by production of acid but no gas 8
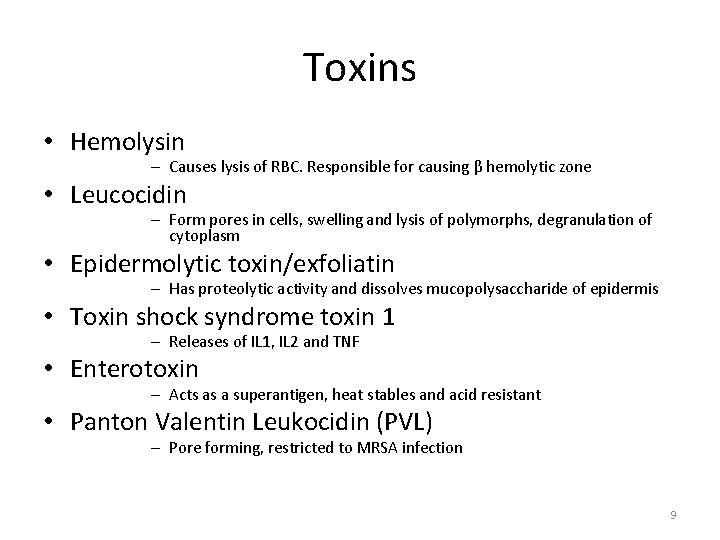
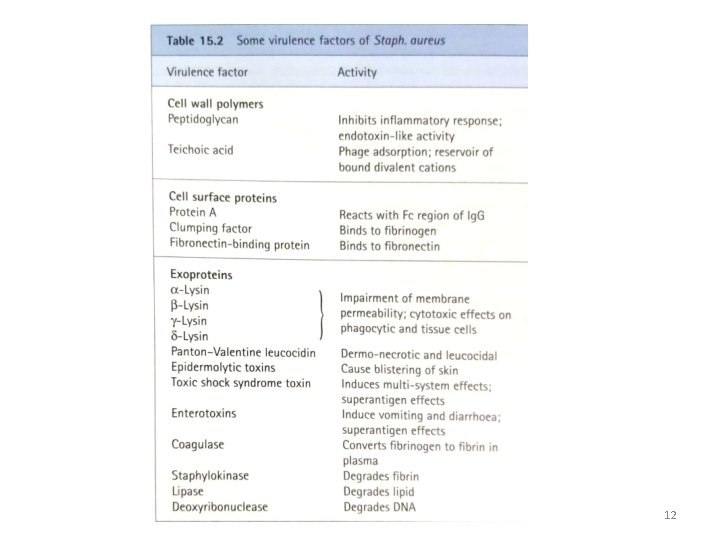
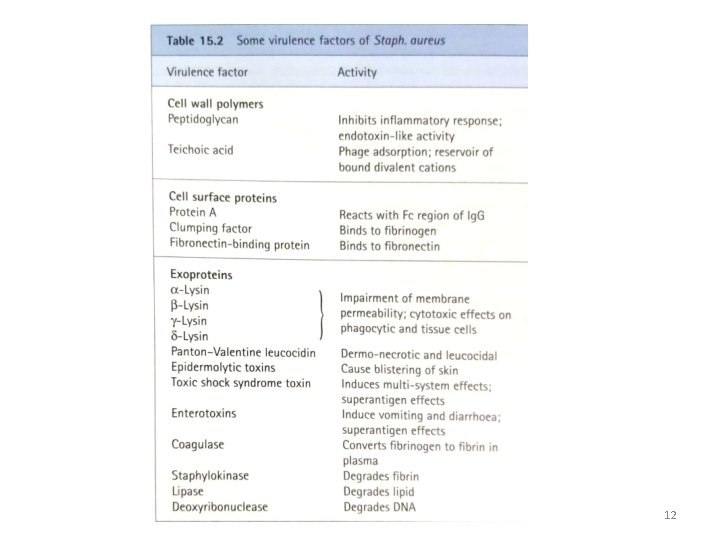
Toxins • Hemolysin – Causes lysis of RBC. Responsible for causing β hemolytic zone • Leucocidin – Form pores in cells, swelling and lysis of polymorphs, degranulation of cytoplasm • Epidermolytic toxin/exfoliatin – Has proteolytic activity and dissolves mucopolysaccharide of epidermis • Toxin shock syndrome toxin 1 – Releases of IL 1, IL 2 and TNF • Enterotoxin – Acts as a superantigen, heat stables and acid resistant • Panton Valentin Leukocidin (PVL) – Pore forming, restricted to MRSA infection 9
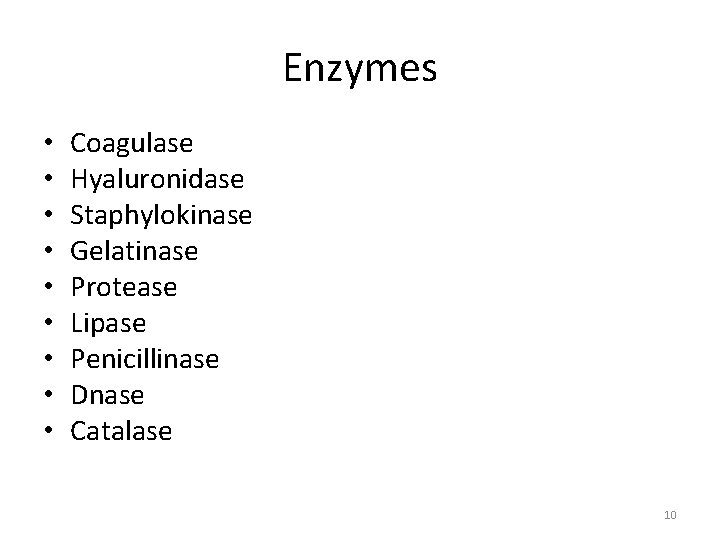
Enzymes • • • Coagulase Hyaluronidase Staphylokinase Gelatinase Protease Lipase Penicillinase Dnase Catalase 10
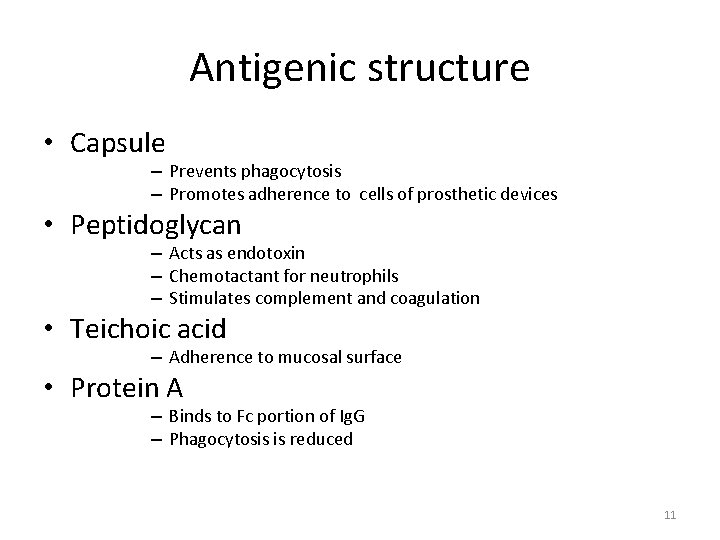
Antigenic structure • Capsule – Prevents phagocytosis – Promotes adherence to cells of prosthetic devices • Peptidoglycan – Acts as endotoxin – Chemotactant for neutrophils – Stimulates complement and coagulation • Teichoic acid – Adherence to mucosal surface • Protein A – Binds to Fc portion of Ig. G – Phagocytosis is reduced 11
12
Pathogenesis • • • Invasion Multiplication Toxins and enzymes Inflammation Repair 13
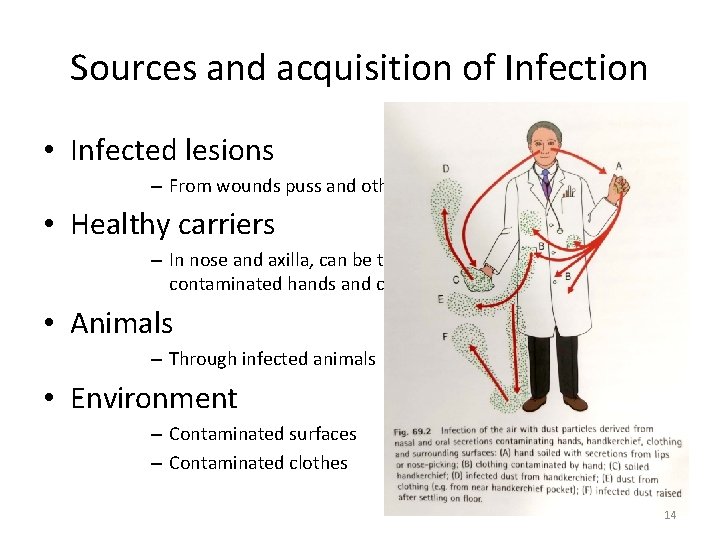
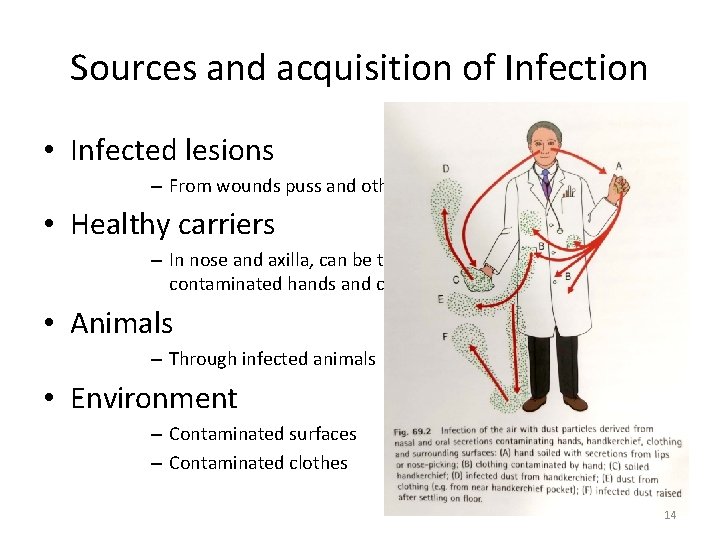
Sources and acquisition of Infection • Infected lesions – From wounds puss and other infected areas • Healthy carriers – In nose and axilla, can be transferred through direct contact, contaminated hands and cough • Animals – Through infected animals • Environment – Contaminated surfaces – Contaminated clothes 14
Methicillin resistant staphylococcus Aureus (MRSA) • Produces penicillin binding protein 2 a • This gene is carried on staph cassette chromosome (SCC Mec) • 6 types • Resistant to beta lactam group of Antibiotics • MRSA is endemic in hospitals 15
Methicillin resistant staphylococcus Aureus (MRSA) • Vulnerable group • Those who are immunocompromised • Have undergone a major surgery • Patients who are admitted in hospital for a longer period (ICU patients are more prone) • 50 -60% of patients are asymptomatic leading to respiratory track and bone infections 16
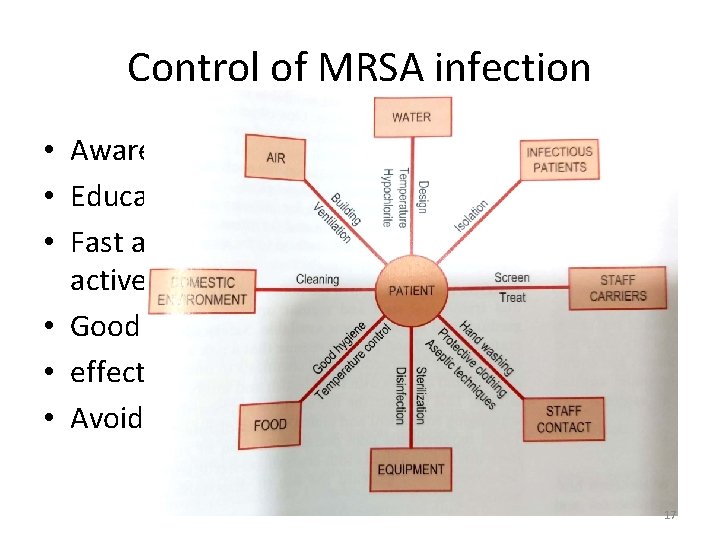
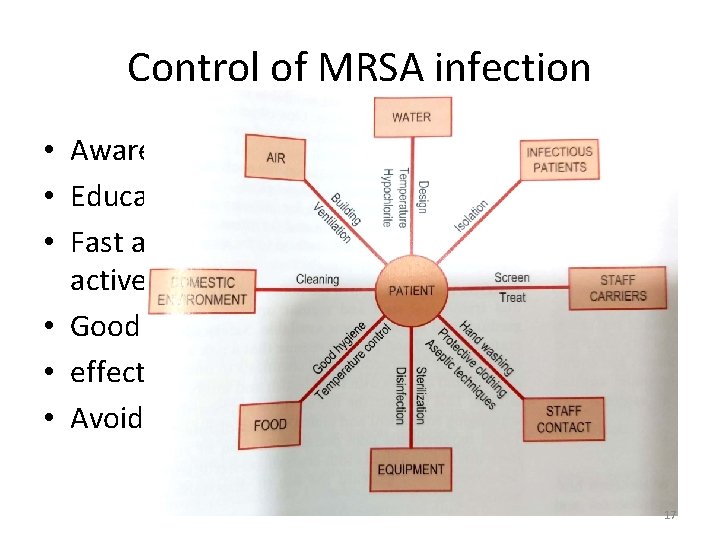
Control of MRSA infection • Awareness programs • Educating general population • Fast and reliable detection of infection and active surveillance • Good professional practice • effective hygiene programs • Avoidance of excessive used of antibiotics – Cephalosporins and fluroquinolones 17
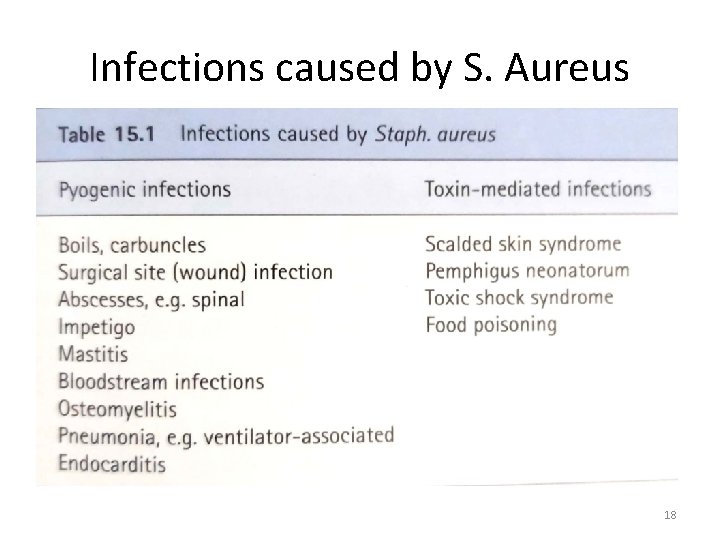
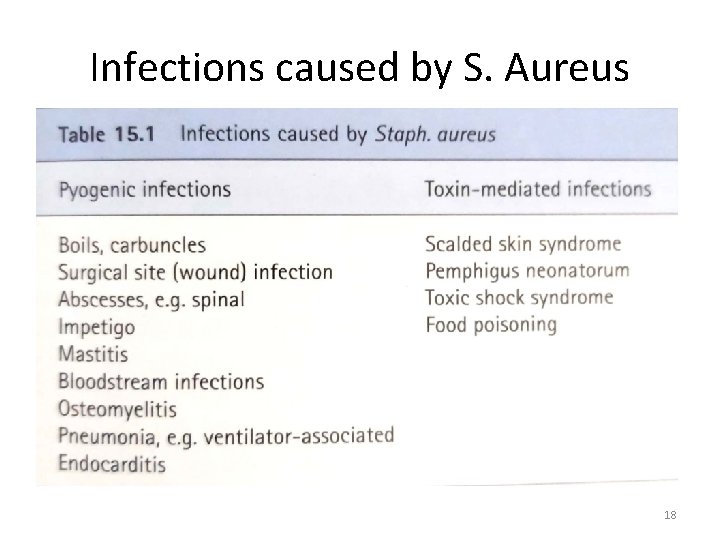
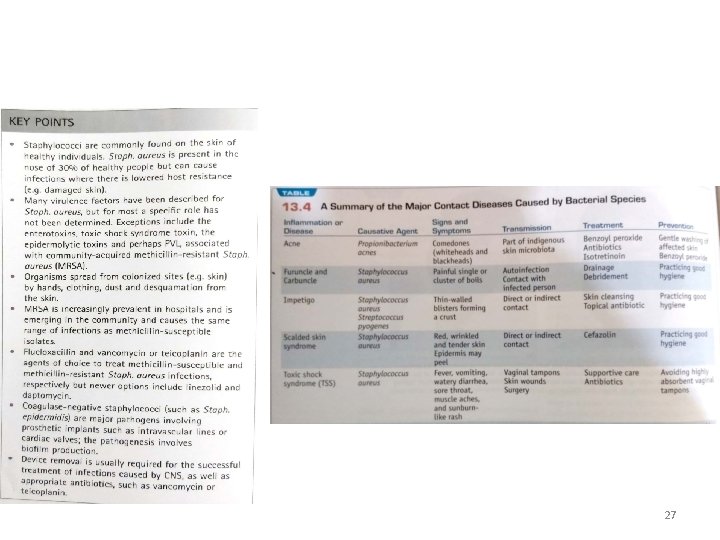
Infections caused by S. Aureus • Depending upon diseases it produces it can divided into two groups – Pyogenic/localised skin infections – Toxigenic skin infections 18
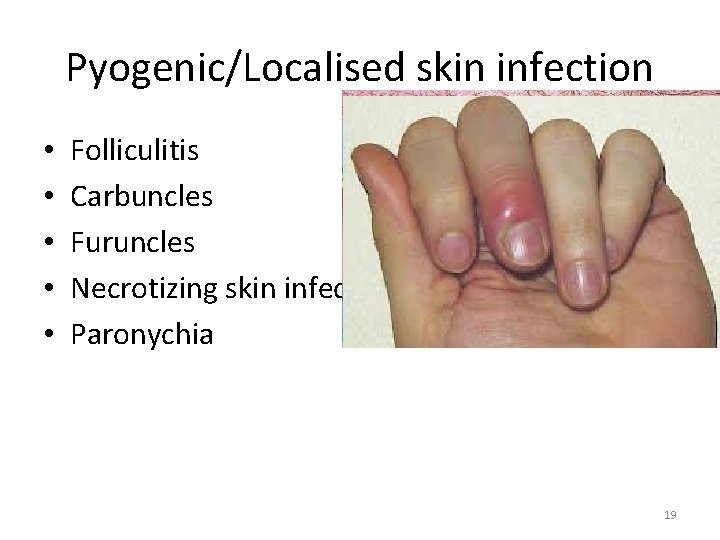
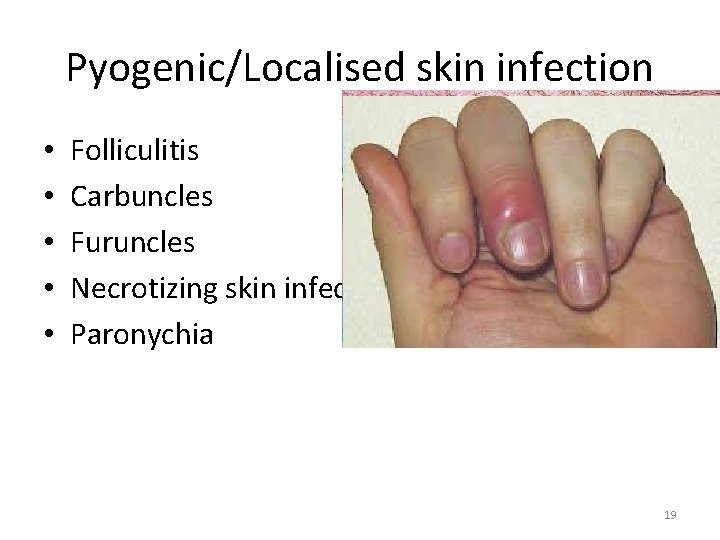
Pyogenic/Localised skin infection • • • Folliculitis Carbuncles Furuncles Necrotizing skin infections Paronychia 19
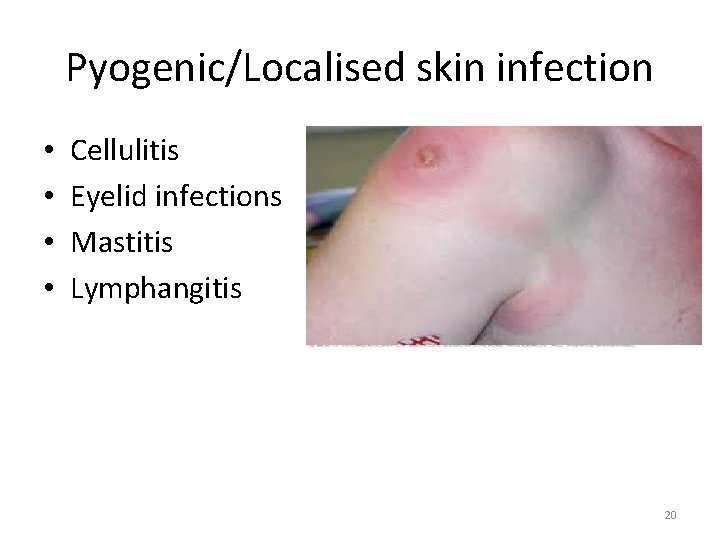
Pyogenic/Localised skin infection • • Cellulitis Eyelid infections Mastitis Lymphangitis 20
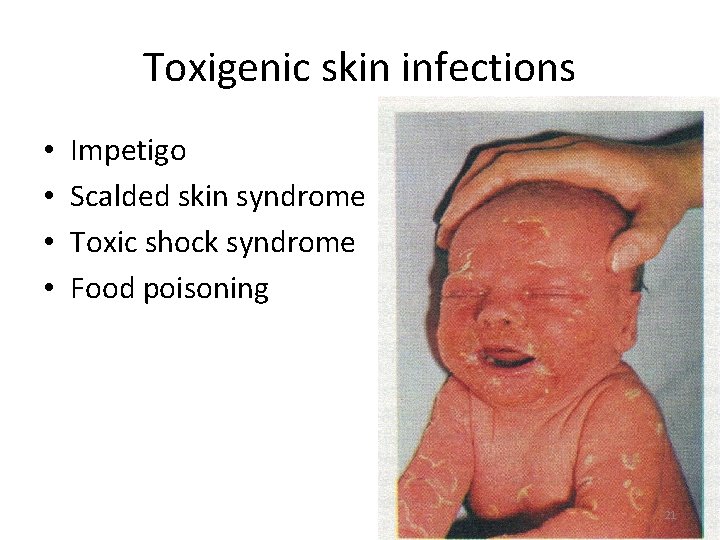
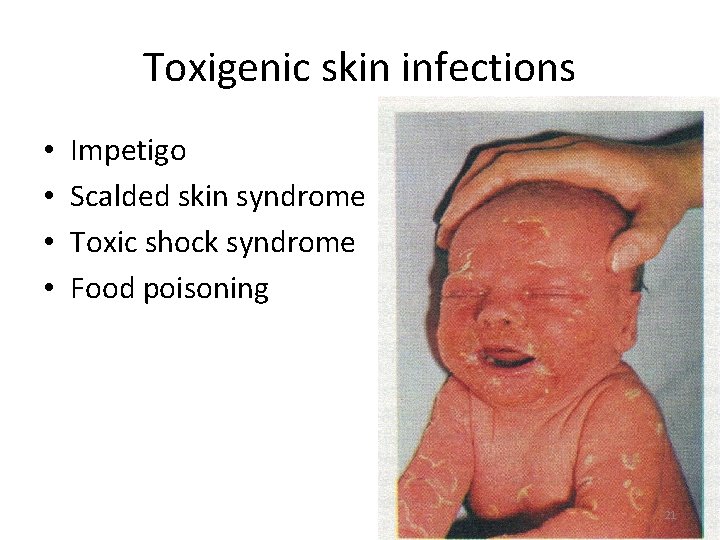
Toxigenic skin infections • • Impetigo Scalded skin syndrome Toxic shock syndrome Food poisoning 21
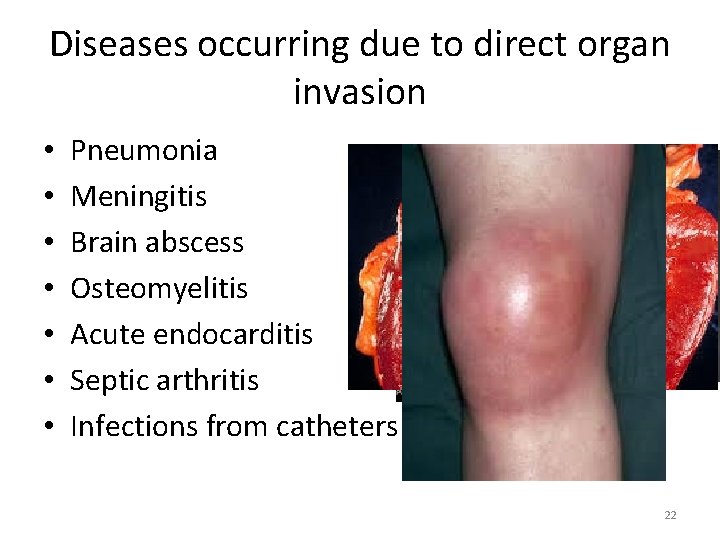
Diseases occurring due to direct organ invasion • • Pneumonia Meningitis Brain abscess Osteomyelitis Acute endocarditis Septic arthritis Infections from catheters 22
Laboratory diagnosis • Specimen should be collected from site of infection for confirmatory diagnosis • • Puss sample Blood sample Vomit sample Sputum sample Mid stream urine sample Anterior nasal swabs Perineal swabs 23
Diagnosis of S. Aureus in Lab • • • Gram positive Catalase positive Mannitol positive Dnase positive Coagulase positive 24
Characteristics of culture • On blood agar (24 hours culture) we will find • Gram positive cocci • Golden yellow small circular colonies • Coagulase test will be done to differentiate btw + and – group • Culture is done against antibiotics for ruling out MRSA infection (resistant to cefoxitin) 25
Other laboratory tests • Following test are done if infection is serious and diagnosis through culture is not satisfactory • Polymerized chain reaction (PCR) • Pulse field gene sequence (PFGE) • Multi locus sequence typing (MLST) 26
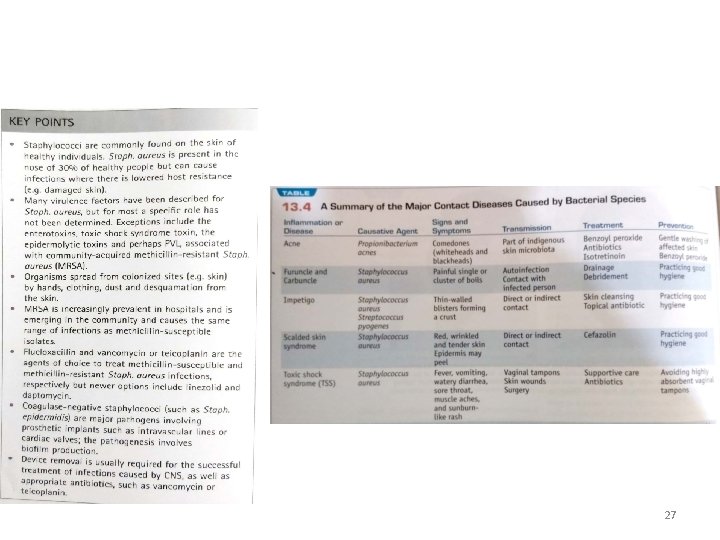
27
Case Senario 1 A 22 years old girl decides with her friends of getting a tattoo which would add uniqueness to her personality. She finally made it to the tattoo parlor and got done with it. Two weeks later she developed abdominal pain, high grade fever and a rash developed, it looked like as if her skin has burned away and was peeling off. She was taken to hospital by her parents. She was given antibiotics and was sent home. After a day her condition worsened and she was taken to emergency room. This time she was admitted to the hospital. She was given IV fluids and IV antibiotics. She stayed in hospital for next 10 days. 28
• What is your probable diagnosis? • How would you defend your answer? • What can be the probable cause of this condition? 29
Case Scenario 2 • A 48 years old man who is a known diabetic was admitted to surgical ward with an ulcer on his foot. On 3 rd day of his admission he developed fever, there was discharge from the ulcer and had disorientation. He was shifted to ICU for full time care and same IV antibiotics that were given in ward were continued. His fever did not decrease and he developed seizures and got unconscious 30
• What can be probable diagnosis? • How will you confirm your diagnosis? • How will you proceed with treatment plan? 31
Case scenario 3 • A 27 years old boy presented to OPD with injection site abscess. On examination the abscess was fluctuant and the area around it was inflamed. He was referred to surgical ward where his abscess was drained. The puss sample was sent for culture and sensitivity. Result of C/S showed growth of golden yellow color colonies with a golden sheen 32

33
• Which bacteria forms golden yellow colonies on blood agar? • Which additional tests would you perform on these bacterial colonies that would confirm your diagnosis? • Which staining procedure would we do in this case? • How do these bacteria appear on microscopy? 34
35