Standardization of Social Work Intake Notes at the



- Slides: 26

Standardization of Social Work Intake Notes at the East Harlem Health Outreach Partnership Amreen Rahman, Eric Woods, Sandra Fong, Ryan Devenyi, and Ioannis Konstantinidis,
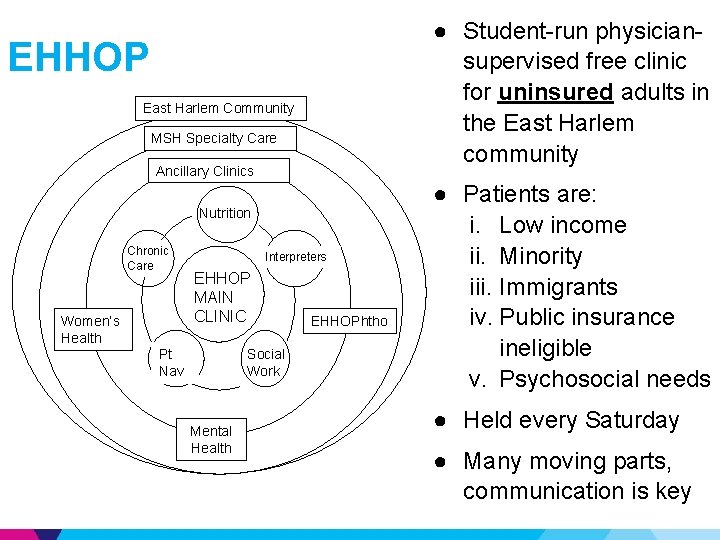
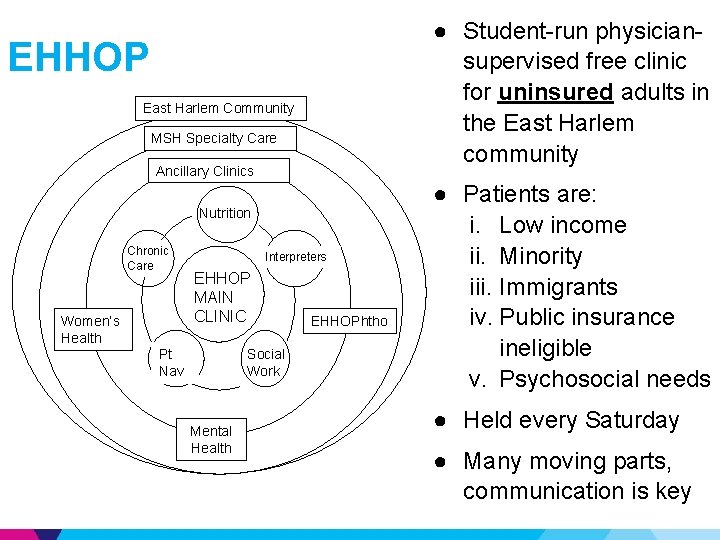
● Student-run physiciansupervised free clinic for uninsured adults in the East Harlem community EHHOP East Harlem Community MSH Specialty Care Ancillary Clinics Nutrition Chronic Care Women’s Health Interpreters EHHOP MAIN CLINIC Social Work Pt Nav Mental Health EHHOPhtho ● Patients are: i. Low income ii. Minority iii. Immigrants iv. Public insurance ineligible v. Psychosocial needs ● Held every Saturday ● Many moving parts, communication is key
Social Work (SW) at EHHOP ▶ SW has been a part of EHHOP from the start (2004) ▶ 5 social workers at EHHOP – One social worker on-site every Saturday – From different sites throughout Mt. Sinai
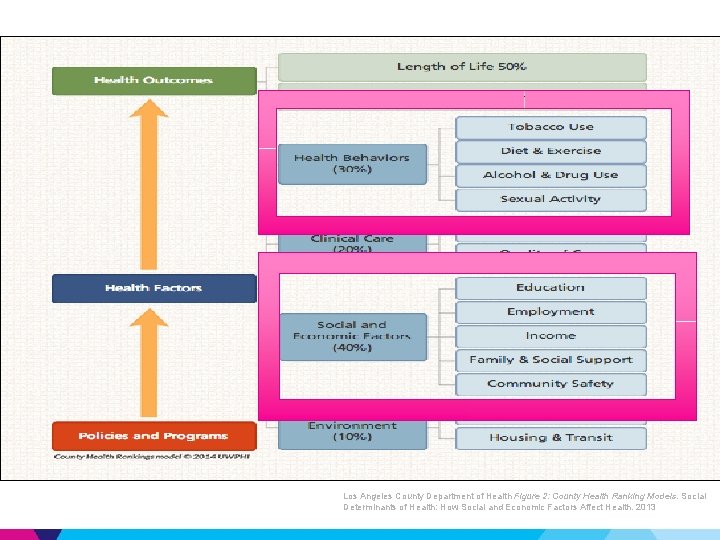
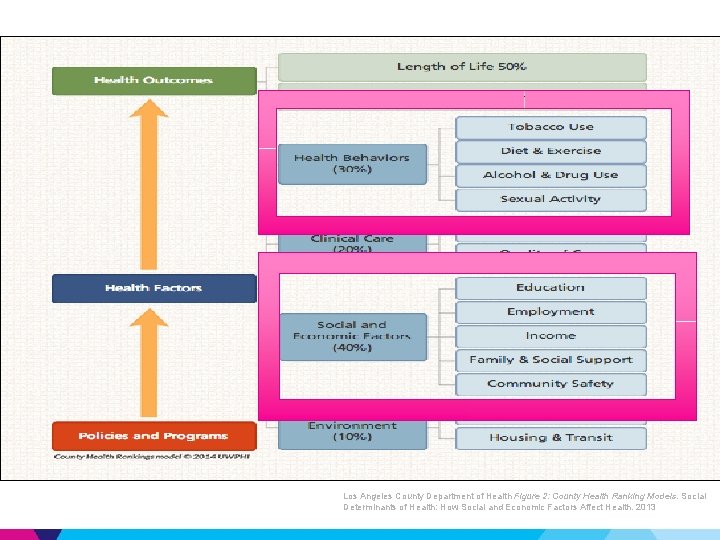
Importance ▶ SW is a critical component of EHHOP – First point of contact – Screen for eligibility – Psychosocial and environmental concerns common ▶ 25% ($13, 000) of total clinic expenditures in 2013 Los Angeles County Department of Health Figure 2: County Health Ranking Models. Social Determinants of Health: How Social and Economic Factors Affect Health. 2013
Are we using it efficiently? ▶ Current utilization statistics of SW unclear ▶ Variability of SW care – Constant rotation of social workers – Lapses in communication ▶ Formalized process for SW referrals often not used properly – Impromptu SW consultation during patient’s medical clinic visit – Clinicians unsure when to refer patients to SW – SW unsure why patients have been referred to them
What is relevant? Consulted with multiple stakeholders: – Social Workers – Patient Navigators – MS 3/4 student clinicians Resources: – National Association of Social Workers Standards for Social Work Practice in Health Care Settings – New York State Department of Health Case Management Standards
Relevant SW categories 1. Employment 2. Immigration Status 8. Currently receiving benefits 3. Housing 9. Educational Level 4. Mental Health 10. Domestic Violence 5. Income 11. Child Services 6. Primary Source of Income 12. Nutrition/Food Security 7. Substance Abuse 13. Legal Services
Pre-Intervention Data Time period: Intake notes from 1/1/2014 - 6/30/2014 Cohort: New EHHOP patients for whom SW intake notes were written (N=31) Methods: – The notes were coded in duplicate – Coding discrepancies were resolved by consensus
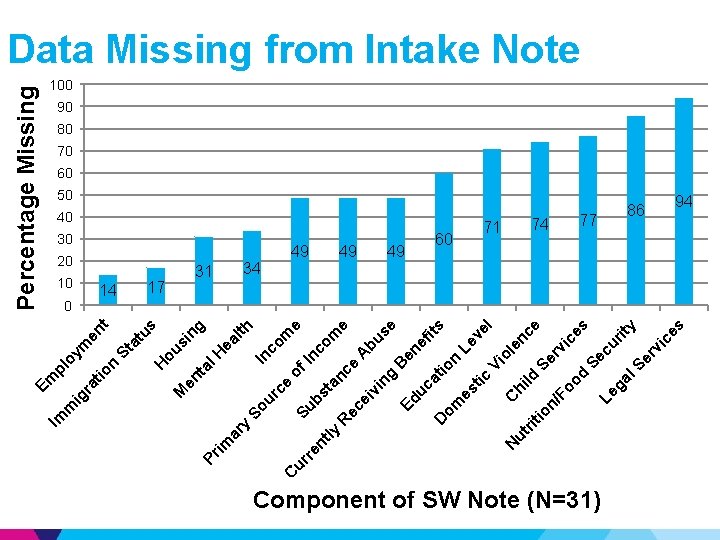
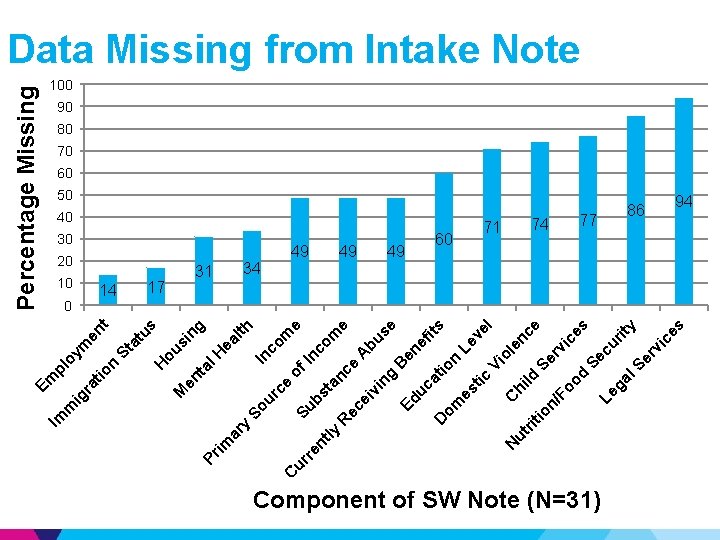
e m 34 bs Su of I co In 30 nc om ta ly nc e R ec e A ei bu vi ng se B Ed en uc ef its a tio D om n Le es ve tic l Vi ol C N en h ut i ce ld rit io Se n/ rv Fo ic od es Se Le cu ga rit y l. S er vi ce s nt re ur ce ur So ea lth 31 C y ar ng 17 im al H si ou 20 Pr en t M 14 H us 0 St at t Percentage Missing 10 n en oy m pl tio ra ig m Im Em Data Missing from Intake Note 100 90 80 70 60 50 40 49 49 49 60 71 74 77 Component of SW Note (N=31) 86 94

To standardize or not to standardize? ▶ Prospective randomized trial showed mixed results concerning standardized versus free form documentation in a primary care clinic –Clinic Time –Billing –Physician satisfaction ▶ Significance of balancing flexibility with structure Mulvehill, S. , G. Schneider, C. M. Cullen, S. Roaten, B. Foster, and A. Porter. "Template-Guided Versus Undirected Written Medical Documentation: A Prospective, Randomized Trial in a Family Medicine Residency Clinic. " The Journal of the American Board of Family Medicine 18. 6 (2005): 464 -69. Web Rosenbloom, S. T. , J. C. Denny, H. Xu, N. Lorenzi, W. W. Stead, and K. B. Johnson. "Data from Clinical Notes: A Perspective on the Tension between Structure and Flexible Documentation. " Journal of the American Medical Informatics Association 18. 2 (2011): 181 -86. Web.
Standardize social work intake notes using the electronic medical record
Generate standardized intake form Goals – To improve patient care by optimizing the utilization of SW Important Aspects 1. Create a standardized and efficient way to assess EHHOP patients’ psychosocial needs 2. Improve communication between social workers and other clinic teams 3. Gather surveillance data
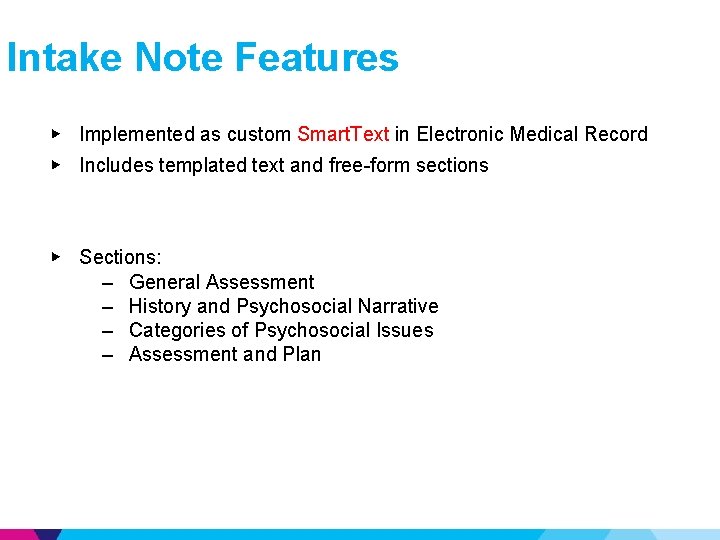
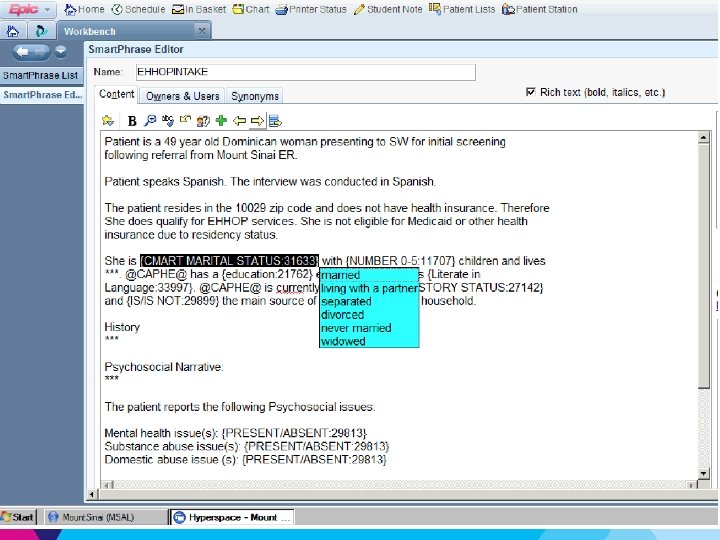
Intake Note Features ▶ Implemented as custom Smart. Text in Electronic Medical Record ▶ Includes templated text and free-form sections ▶ Sections: – General Assessment – History and Psychosocial Narrative – Categories of Psychosocial Issues – Assessment and Plan
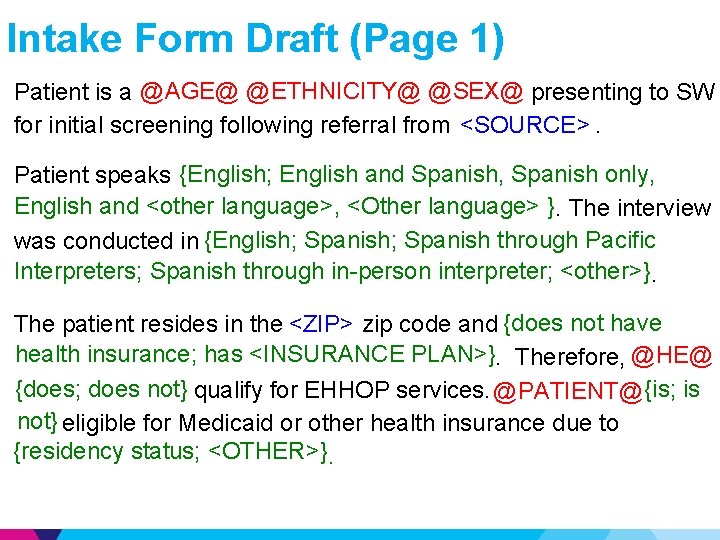
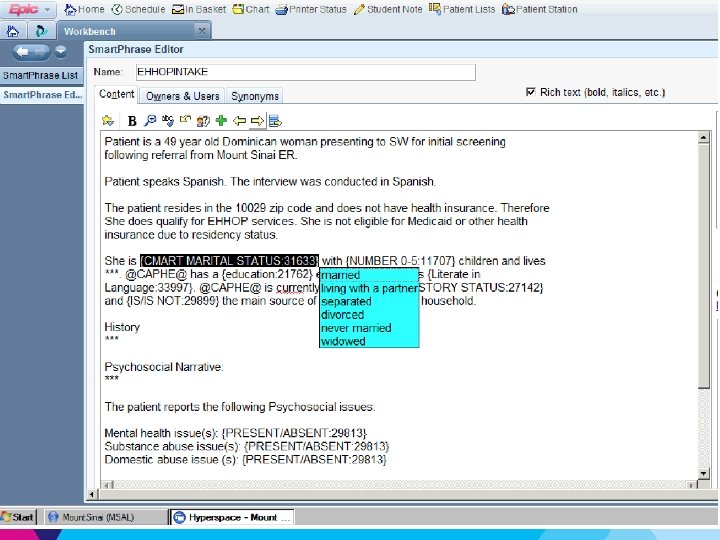
Intake Form Draft (Page 1) Patient is a @AGE@ @ETHNICITY@ @SEX@ presenting to SW <SOURCE> for initial screening following referral from <SOURCE>. . Patient speaks {English; English and Spanish, Spanish only, English and <other language>, <Other language> }}. The interview was conducted in {English; Spanish through Pacific Interpreters; Spanish through in-person interpreter; <other>} The patient resides in the <ZIP> zip code and {does not have health insurance; has <INSURANCE PLAN>} Therefore, @HE@ {does; does not} qualify for EHHOP services. @PATIENT@ @CAPHE@ {is; is not} eligible for Medicaid or other health insurance due to not} {residency status; <OTHER>}.

Intake Form Draft (Page 1 - c’td) @PATIENT@ @CAPHE@ is {single; married; divorced; separated; living with partner; <other>} with {no; 1; 2; 3; 4; 5; <other>} children and aa partner; @PATIENT@ has a {elementary; lives <living arrangement>. @CAPHE@ {elementary; secondary; some college; college degree; graduate degree; <other>} level education and is {literate in <language(s)>, illiterate, {employedfulltime; illiterate, <other>}. @PATIENT@ @CAPHE@ is currently {employed part time; unemployed; self-employed; retired; a <other>} and {is; is not} the main source of income for student; <other>}, @HIS@ household. History: <HISTORY> Psychosocial narrative: <PSYCHOSOCIAL NARRATIVE>
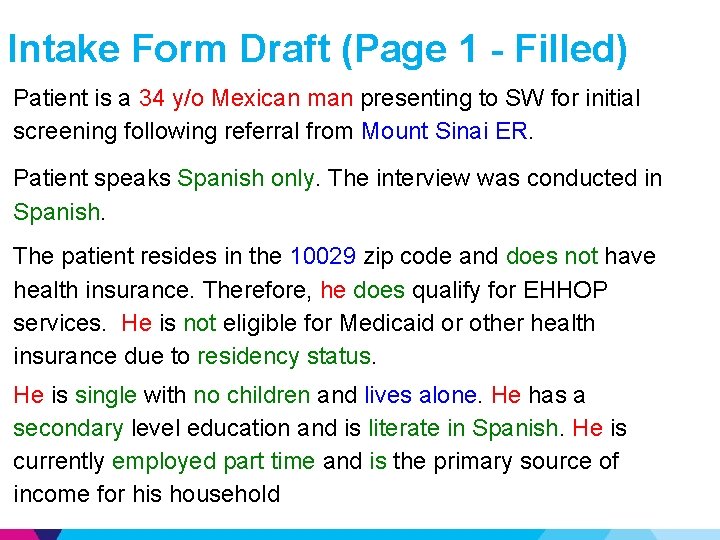
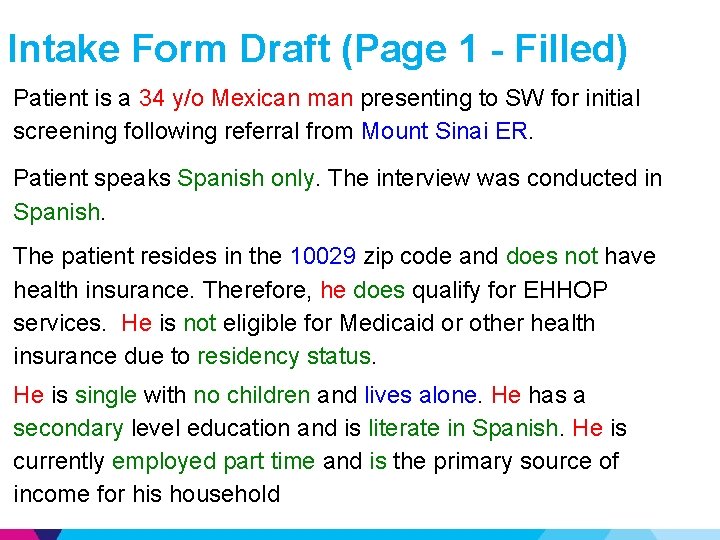
Intake Form Draft (Page 1 - Filled) Patient is a 34 y/o Mexican man presenting to SW for initial screening following referral from Mount Sinai ER. Patient speaks Spanish only. The interview was conducted in Spanish. The patient resides in the 10029 zip code and does not have health insurance. Therefore, he does qualify for EHHOP services. He is not eligible for Medicaid or other health insurance due to residency status. He is single with no children and lives alone. He has a secondary level education and is literate in Spanish. He is currently employed part time and is the primary source of income for his household
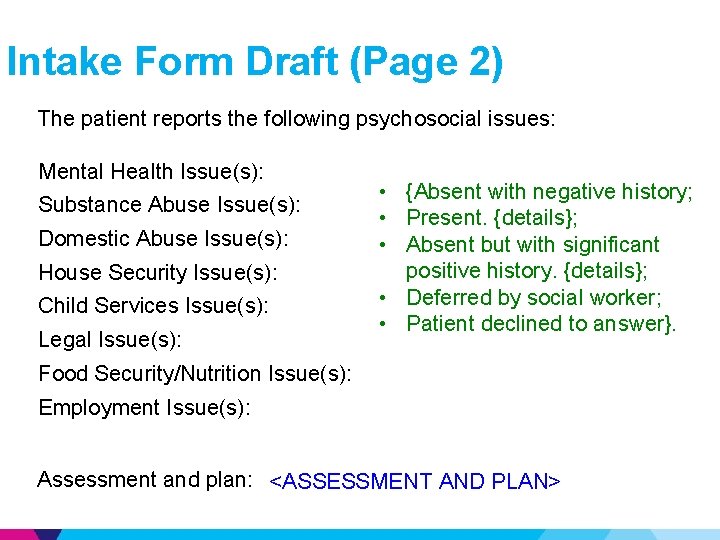
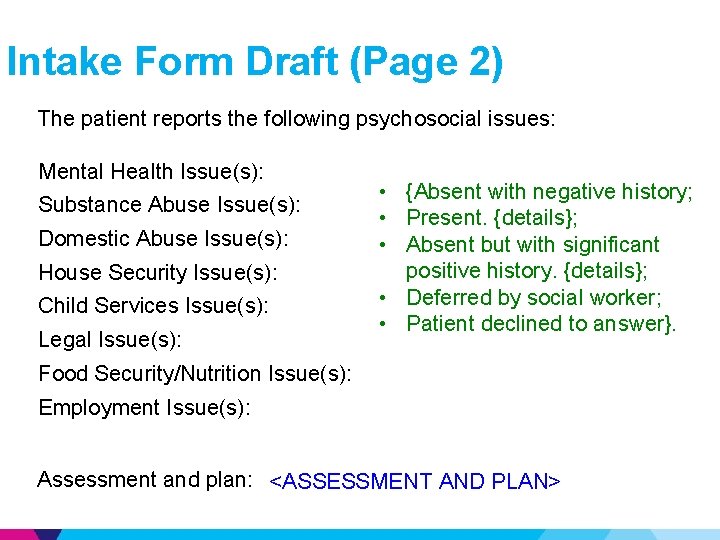
Intake Form Draft (Page 2) The patient reports the following psychosocial issues: Mental Health Issue(s): Substance Abuse Issue(s): Domestic Abuse Issue(s): House Security Issue(s): Child Services Issue(s): Legal Issue(s): • {Absent with negative history; • Present. {details}; • Absent but with significant positive history. {details}; • Deferred by social worker; • Patient declined to answer}. Food Security/Nutrition Issue(s): Employment Issue(s): Assessment and plan: <ASSESSMENT AND PLAN>
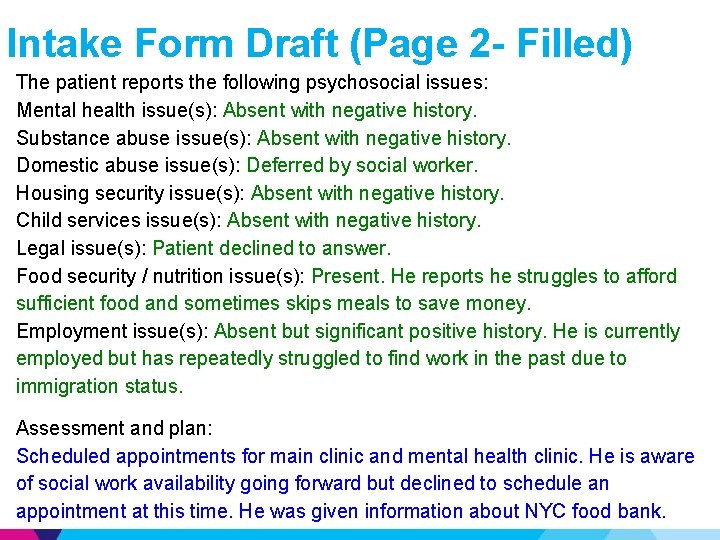
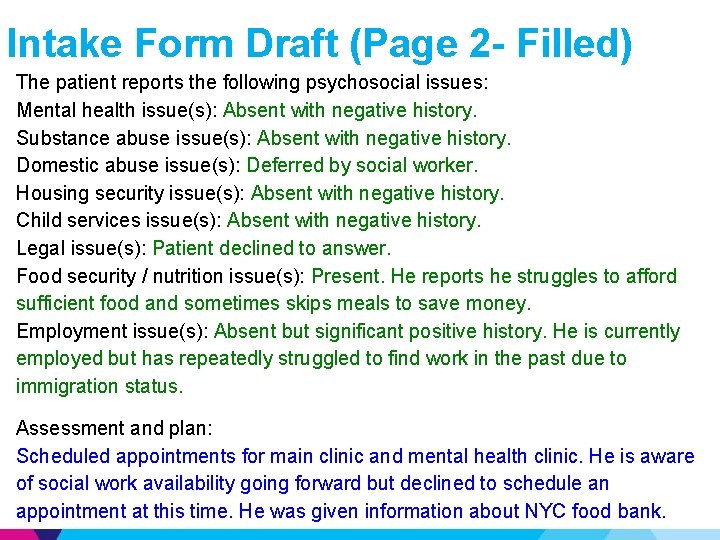
Intake Form Draft (Page 2 - Filled) The patient reports the following psychosocial issues: Mental health issue(s): Absent with negative history. Substance abuse issue(s): Absent with negative history. Domestic abuse issue(s): Deferred by social worker. Housing security issue(s): Absent with negative history. Child services issue(s): Absent with negative history. Legal issue(s): Patient declined to answer. Food security / nutrition issue(s): Present. He reports he struggles to afford sufficient food and sometimes skips meals to save money. Employment issue(s): Absent but significant positive history. He is currently employed but has repeatedly struggled to find work in the past due to immigration status. Assessment and plan: Scheduled appointments for main clinic and mental health clinic. He is aware of social work availability going forward but declined to schedule an appointment at this time. He was given information about NYC food bank.
Goals Overall – To improve patient care by optimizing the utilization of SW Intervention – Create a standardized comprehensive and efficient way to assess EHHOP patients’ psychosocial needs – Improve communication between social workers and other clinic teams – Qualify and quantify social work actions
Upcoming Goals Post-Intervention ▶ Assess success of intervention by conducting postintervention chart review ▶ Modify standardized intake note to fill EMR snapshot ▶ Track rates of follow-up ▶ Conduct interprofessional training sessions
Conclusions 1. First steps to improving social work utilization 2. Potential for improved patient care, communication, and clinic efficiency 3. Applicability of standardized notes for any provider with variability
Acknowledgments ▶ ▶ ▶ ▶ ▶ Yasmin Meah, MD Brijen Shah, MD David Thomas, MD Leslie Garcia, LCSW Joennis Almeida, LCSW Maia Alejandro, LMSW David Chiang Ammar Siddiqui EHHOP Quality Improvement Council Funding from ISMMS MSRO, ISMMS Student Council, Mount Sinai Auxiliary Board
Appendix
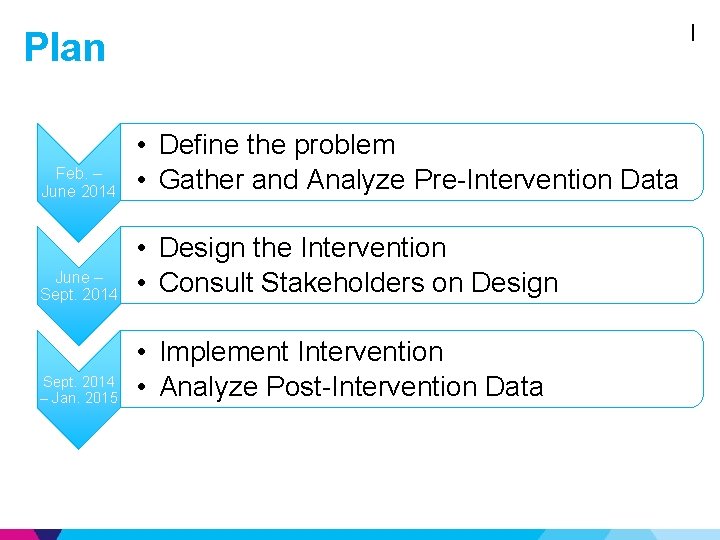
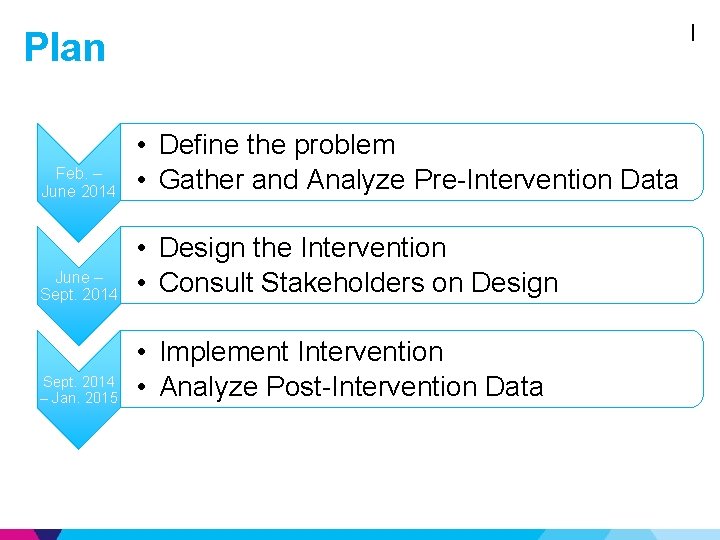
I Plan Feb. – June 2014 • Define the problem • Gather and Analyze Pre-Intervention Data June – Sept. 2014 • Design the Intervention • Consult Stakeholders on Design Sept. 2014 – Jan. 2015 • Implement Intervention • Analyze Post-Intervention Data
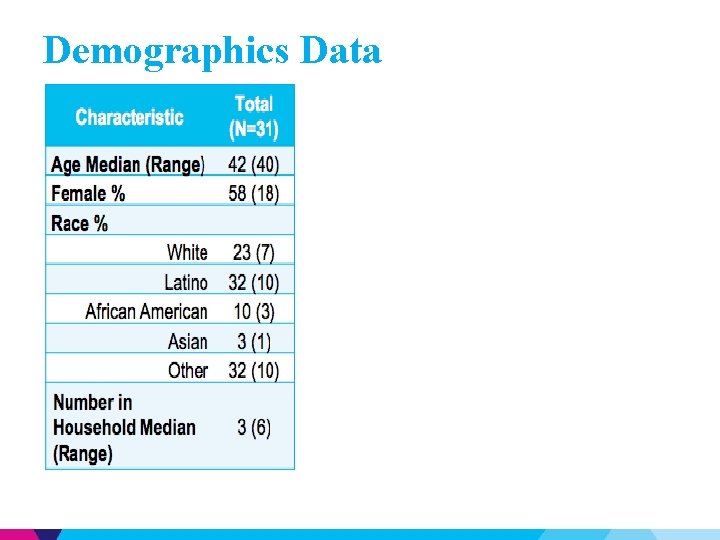
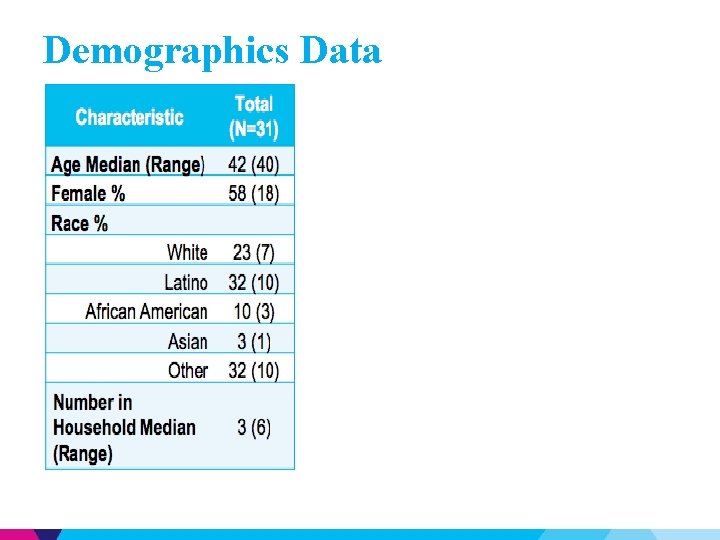
Demographics Data