Standard Cause Analysis Model Norton Healthcare Kelly Johnson



- Slides: 15
Standard Cause Analysis Model Norton Healthcare Kelly Johnson, DNP, RN, CPPS November 2018
Background Rationale Significance • 1 in 4 American families are affected by healthcare harm in the U. S. • As many as 16% of Americans will experience preventable healthcare harm • Between 100 K and 400 K Americans die each year from preventable healthcare harm • If ranked, patient safety events would be the 3 rd leading cause of death in the US • A medication error affecting a child occurs every 8 minutes in the US (Denham et al. , 2012; Macrae, 2008)
Why Here? Why Now? • Reaching for Zero strategic plan to eliminate preventable healthcare harm • Significant variation in process • Voice of customer revealed opportunities for improvement – Punitive feeling meetings – Not getting to real causes – Lack of accountability for actions/demonstration of real change – Repeat events

International Guidelines System Analysis of Clinical Incidents: The London Protocol (2001) WHO Draft Guidelines for Adverse Event Reporting & Learning Systems (2005) Patient Safety Handbook, VA (2011) Respectful Management of Serious Clinical Incidents, IHI (2011) Serious Safety Events: Getting to Zero, ASHRM 2012 Optimizing RCA & Organizational Learning, HPI, LLC (2014) RCA 2: Root Cause Analysis & Actions to Prevent Harm, NPSF (2015)
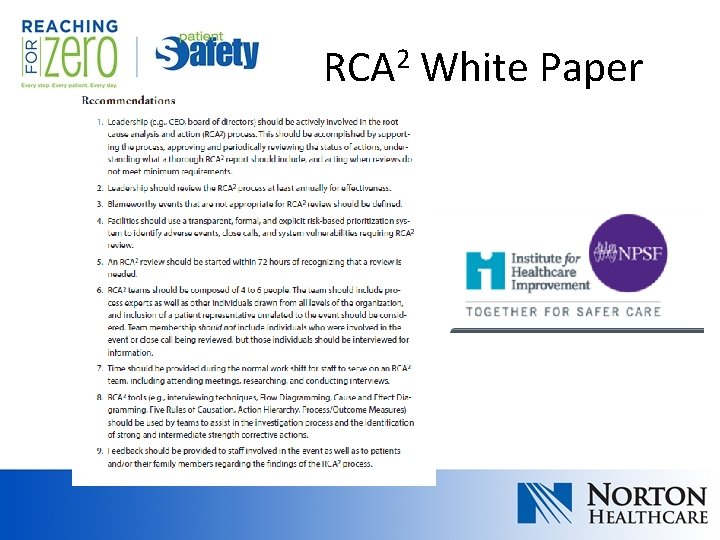
RCA 2 White Paper
Graduated Approach • Written into strategic plan over multiple years • Foundational work on root cause analyses: – DMAIC PI methodology – Lewin’s Change Theory – Team included people from pilot hospital as well as system for planned replication – Piloted for 90 days at largest hospital with specialized services • Staged replication throughout rest of healthcare system over several months • Control plan still in place • Current focus on other types of cause analysis

Cause Analysis Model • • Root cause analysis Apparent cause analysis Aggregate analysis Common cause analysis
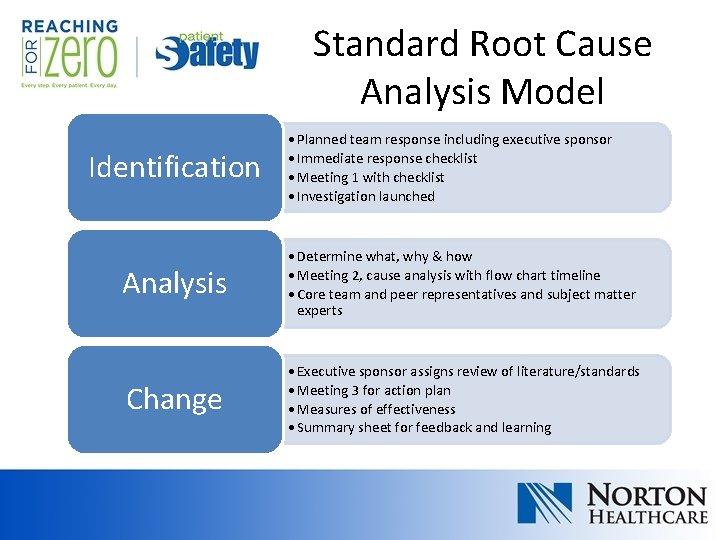
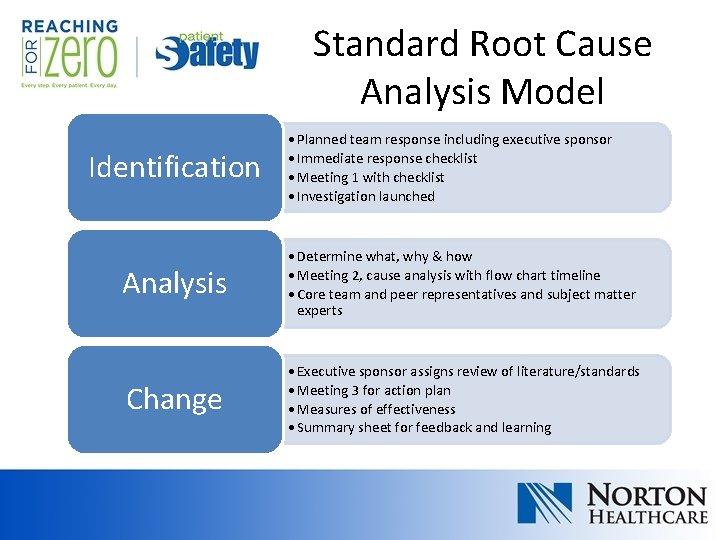
Standard Root Cause Analysis Model Identification • Planned team response including executive sponsor • Immediate response checklist • Meeting 1 with checklist • Investigation launched Analysis • Determine what, why & how • Meeting 2, cause analysis with flow chart timeline • Core team and peer representatives and subject matter experts Change • Executive sponsor assigns review of literature/standards • Meeting 3 for action plan • Measures of effectiveness • Summary sheet for feedback and learning
Standard Root Cause Analysis Model • Planned team response including executive sponsor Identification • Immediate response checklist • Meeting 1 with checklist • Investigation launched

Standard Root Cause Analysis Model Analysis • Determine what, why & how • Meeting 2, cause analysis with flow chart timeline • Core team and peer representatives and subject matter experts
Standard Root Cause Analysis Model Change • Executive sponsor assigns review of literature/standards • Meeting 3 for action plan • Measures of effectiveness • Summary sheet for feedback and learning
Apparent Cause Analysis • Smaller, faster review • Conducted at unit/department with their leaders • May include people involved • Typical tools utilized: – Causal Factor Fishbone – Cause Analysis Interviewing Tips – Cause Analysis Probing Questions by Causal Factor – Event Timeline Flowsheet
Lessons Learned • Stakeholder support was crucial • Organizational assessment and gap analysis was needed to know where to start and what level of change could be accepted • Critical to have investigation completed before analysis meeting • Leaders must be engaged in action item tracking and accountability
Current State • Monitor RCA process through control plan • Extended education on ACA process • Trial of risk grading and aggregate ACA with pharmacy on no-harm medication errors • Common cause analysis with RCAs 2016 -2018
References • Dearholt, S. , & Dang, D. (2012). Johns Hopkins nursing evidence - based practice: Model and guidelines (2 nd ed. ). Indianapolis, IN: Sigma Theta Tau International. • Denham et al. , (2012). An NTSB for healthcare - learning from innovation: Debate and innovate or capitulate. Journal of Patient Safety, 8(1), 3 -14. • Parker, J. (Ed. ). (2015). Root cause analysis in healthcare: Tools and techniques (5 th ed. ). [Adobe Digital Edition]. Retrieved from www. jcrinc. com • Macrae, C. (2008). Learning from patient safety incidents: Creating participative risk regulation in healthcare. Health, Risk & Society, 10(1): 5367. • Mitchell, G. (2013). Selecting the best theory to implement planned change. Nursing Management, 20, 32 -37. • Shirey, M. (2013). Strategic leadership for organizational change. Journal of Nursing Administration, 43, 69 -72. *Full evidence table for project available separately