Squamous Cell Carcinoma Basal Cell Carcinoma Malignant Melanoma
Squamous Cell Carcinoma, Basal Cell Carcinoma & Malignant Melanoma Prof C V Raghuveer II MBBS Class. February 2013, Dec 2014.
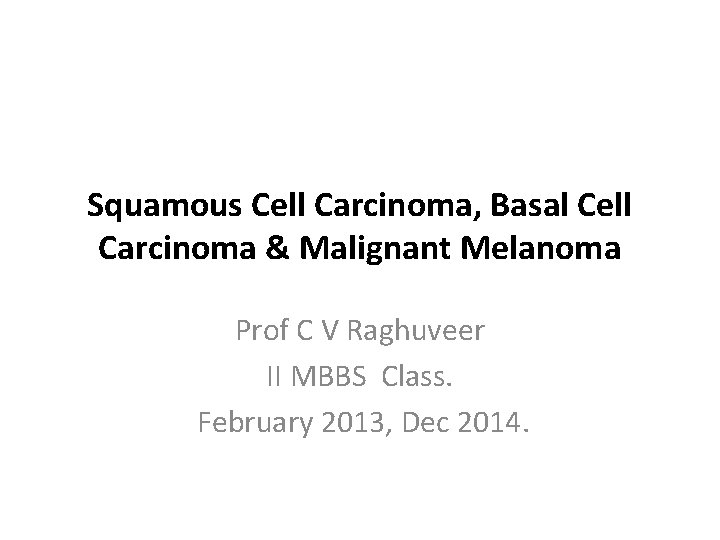
60 years old man with lesions on Arm, growing for 2 years

&0 years old paraplegic man with a big bed sore for 15 years and a tumor 6 years

3 years old child with lesions on face and mental deficiency
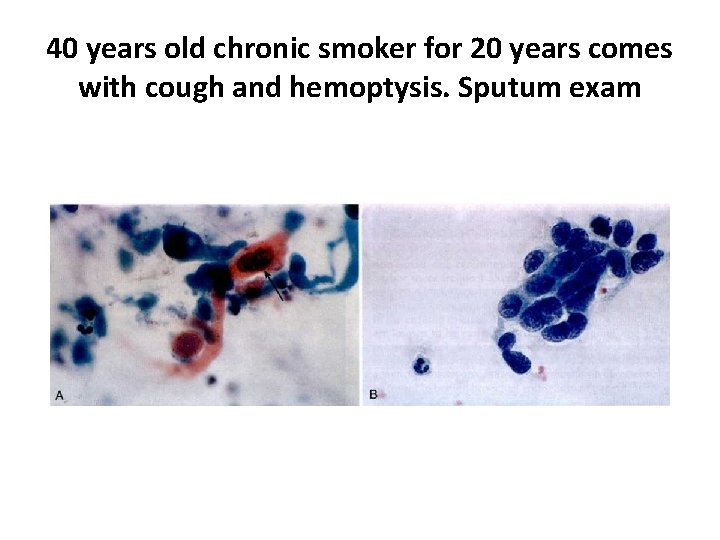
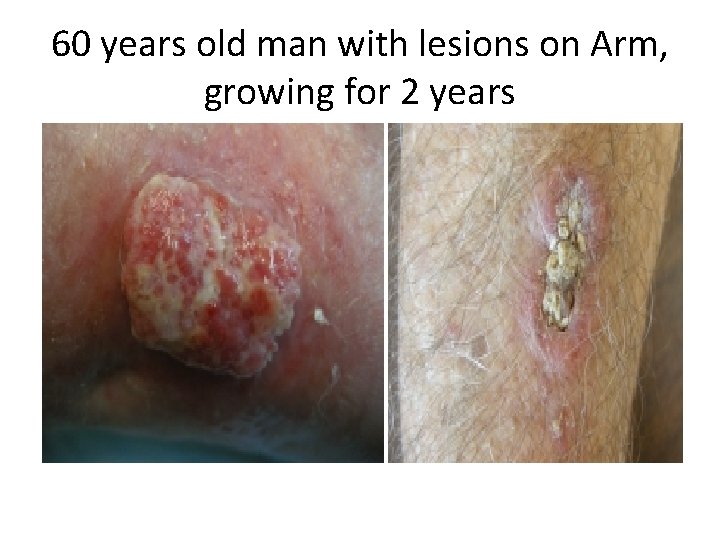
40 years old chronic smoker for 20 years comes with cough and hemoptysis. Sputum exam
After sputum examination he had to undergo an operation
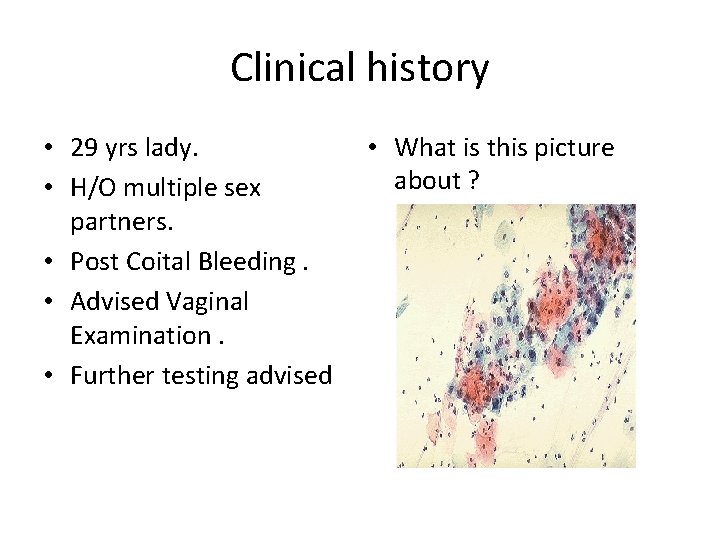
Clinical history • 29 yrs lady. • H/O multiple sex partners. • Post Coital Bleeding. • Advised Vaginal Examination. • Further testing advised • What is this picture about ?
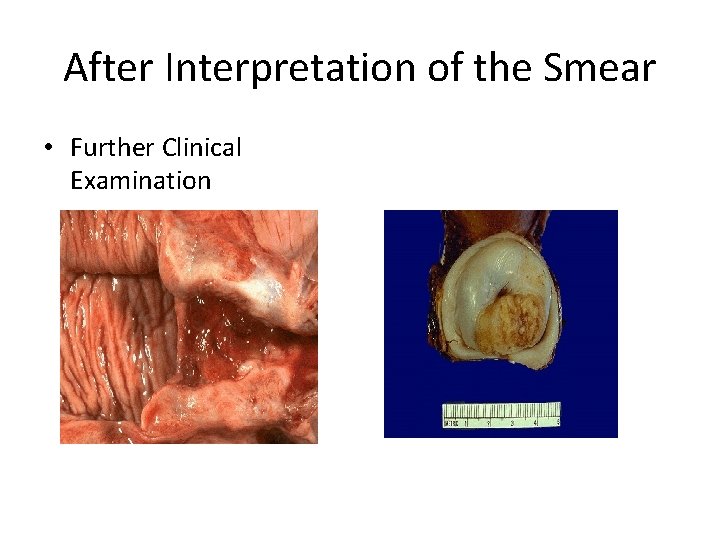
After Interpretation of the Smear • Further Clinical Examination
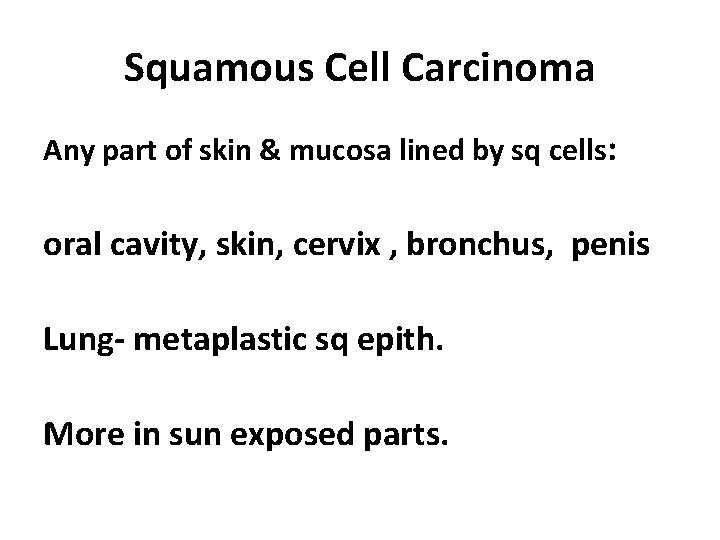
Squamous Cell Carcinoma Any part of skin & mucosa lined by sq cells: oral cavity, skin, cervix , bronchus, penis Lung- metaplastic sq epith. More in sun exposed parts.
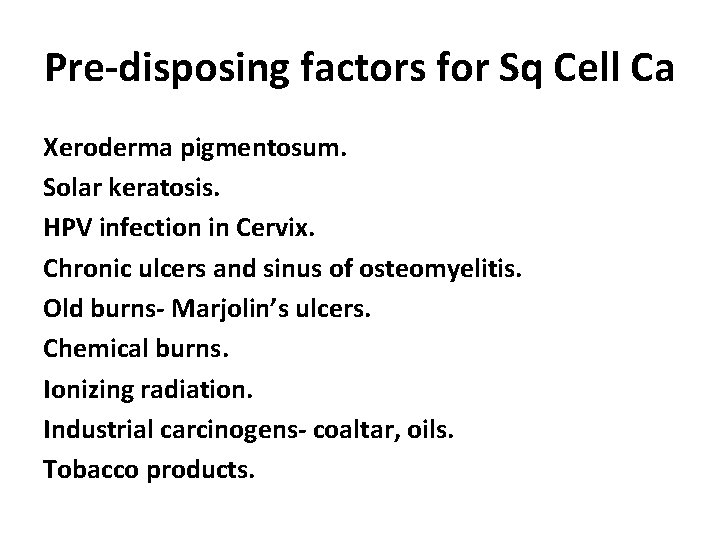
Pre-disposing factors for Sq Cell Ca Xeroderma pigmentosum. Solar keratosis. HPV infection in Cervix. Chronic ulcers and sinus of osteomyelitis. Old burns- Marjolin’s ulcers. Chemical burns. Ionizing radiation. Industrial carcinogens- coaltar, oils. Tobacco products.
Gross Morphology • One of the two patterns. • Ulcerated growth with indurated , infiltrating, elevated margins. • Fungating/polypoidal growth pattern.
Microscopy • Irregular proliferation of squamous cells infiltrating deeper down. • Depending on grade, atypical features vary, with keratin formation, intercellular bridges etc. • Better differentiated tumors have whorled arrangement of tumor cells with horn pearls/ keratin pearls.
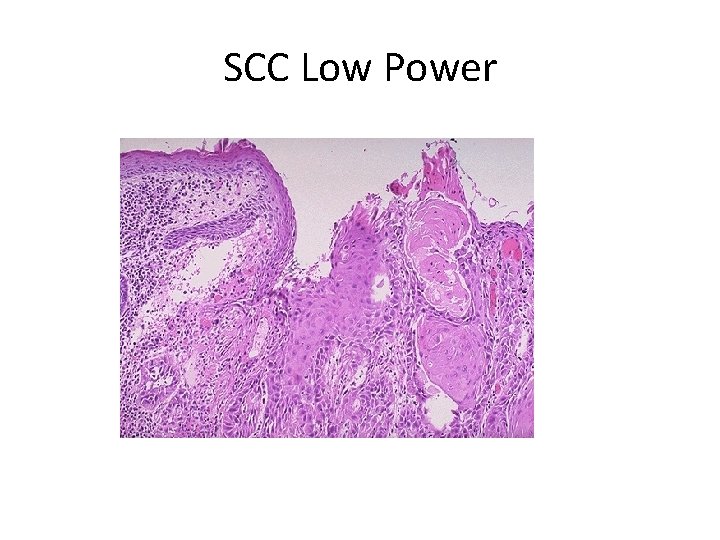
SCC Low Power
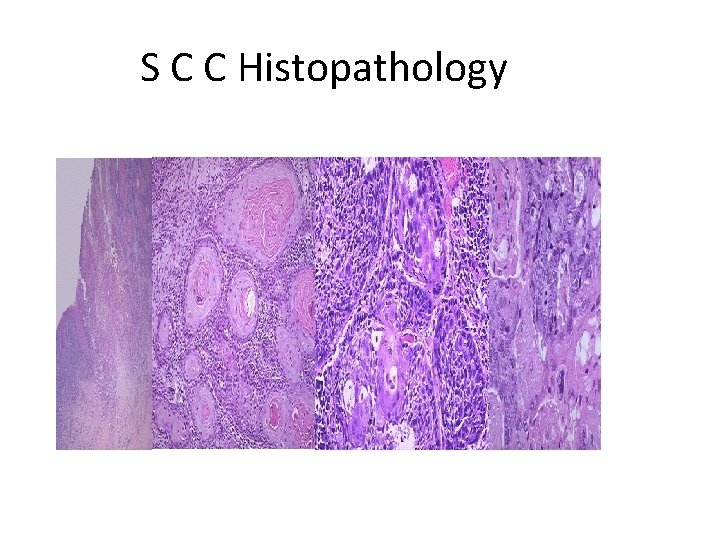
S C C Histopathology
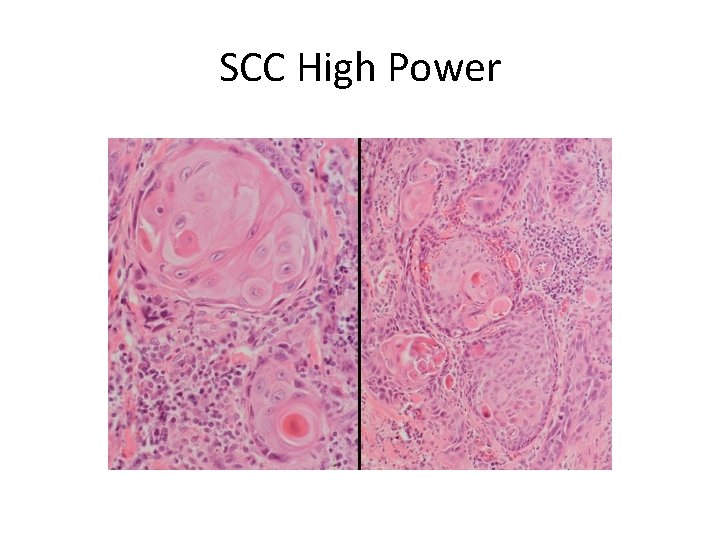
SCC High Power
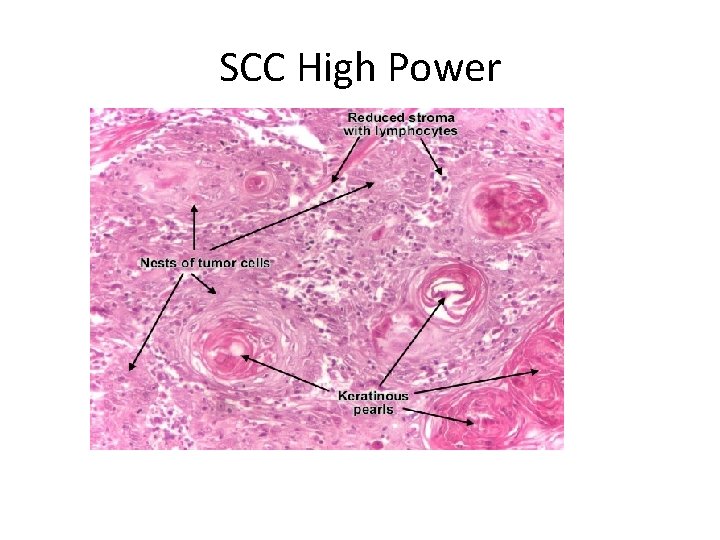
SCC High Power
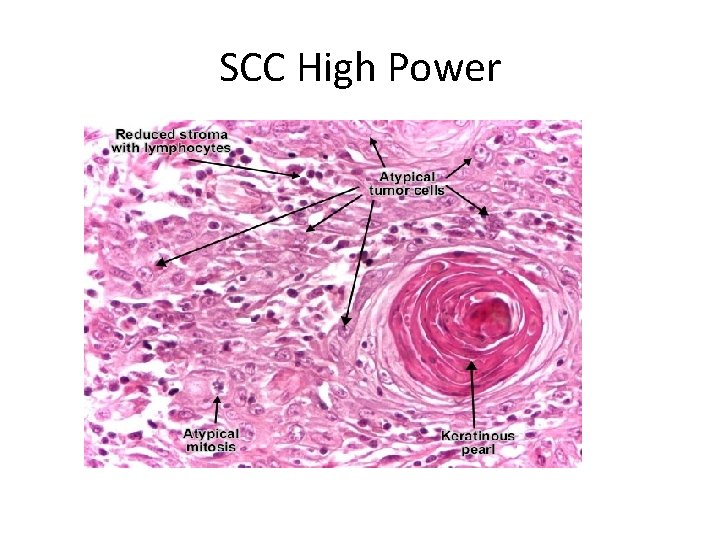
SCC High Power
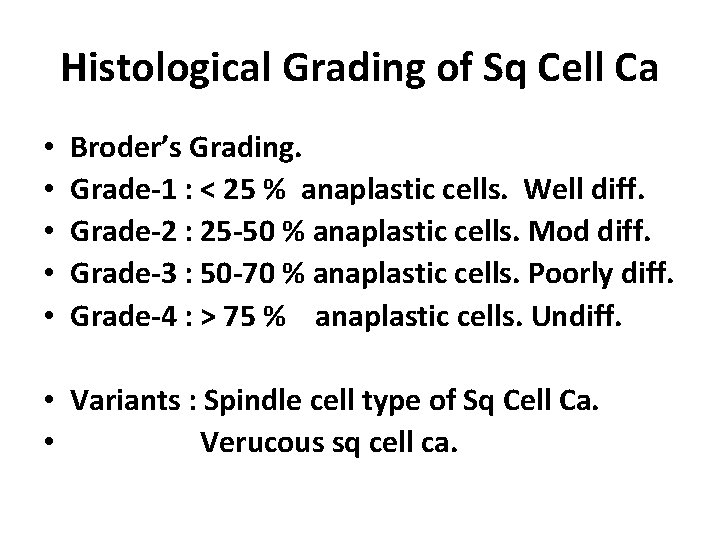
Histological Grading of Sq Cell Ca • • • Broder’s Grading. Grade-1 : < 25 % anaplastic cells. Well diff. Grade-2 : 25 -50 % anaplastic cells. Mod diff. Grade-3 : 50 -70 % anaplastic cells. Poorly diff. Grade-4 : > 75 % anaplastic cells. Undiff. • Variants : Spindle cell type of Sq Cell Ca. • Verucous sq cell ca.

60 years old man ulcerative tumor on face 6 months
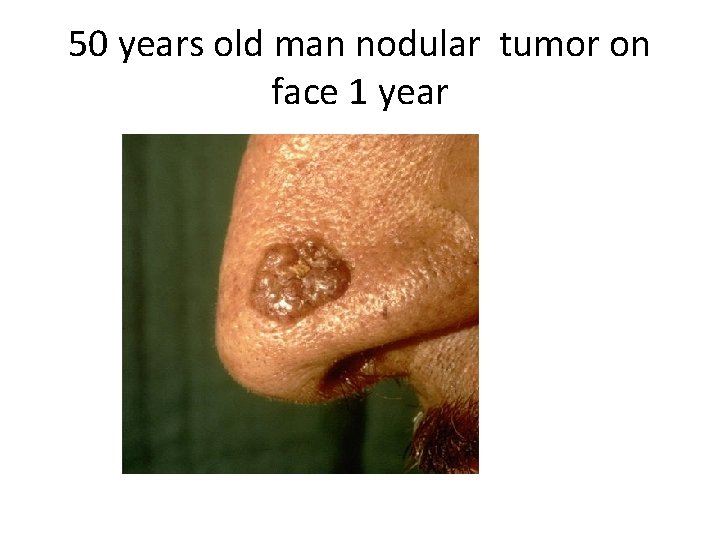
50 years old man nodular tumor on face 1 year

Basal Cell Carcinoma • Locally invasive, slow growing, arising from basal cells. • Common on hairy skin- face. • More in white skinned people. • Prolonged exposure to sun light.
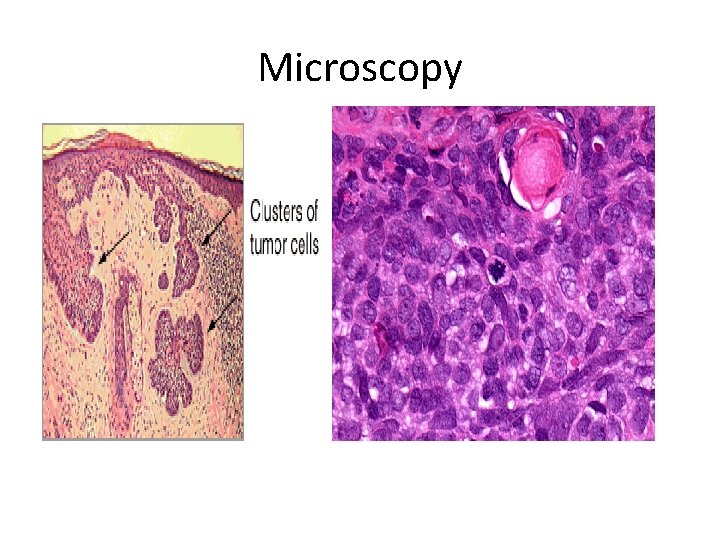
Microscopy
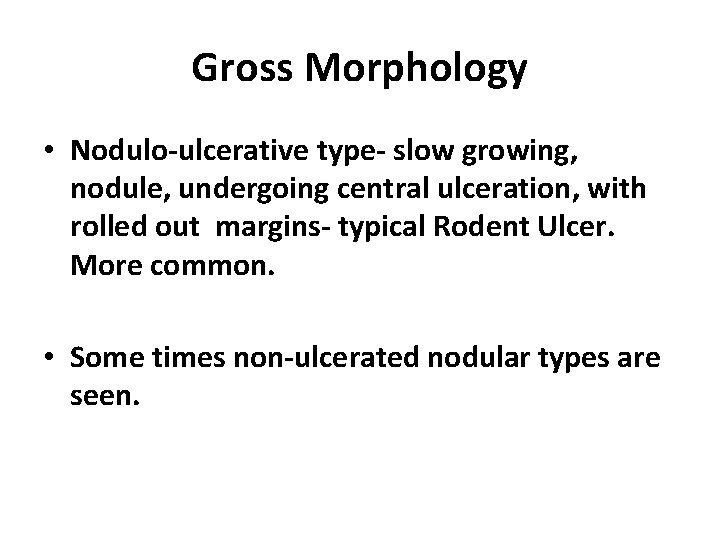
Gross Morphology • Nodulo-ulcerative type- slow growing, nodule, undergoing central ulceration, with rolled out margins- typical Rodent Ulcer. More common. • Some times non-ulcerated nodular types are seen.

Microscopy • Proliferation of basaloid cells. • Variety of patterns seen • Solid masses, nests, strands, adenoid pattern etc. • Most common pattern is solid pattern with peripheral palisading.
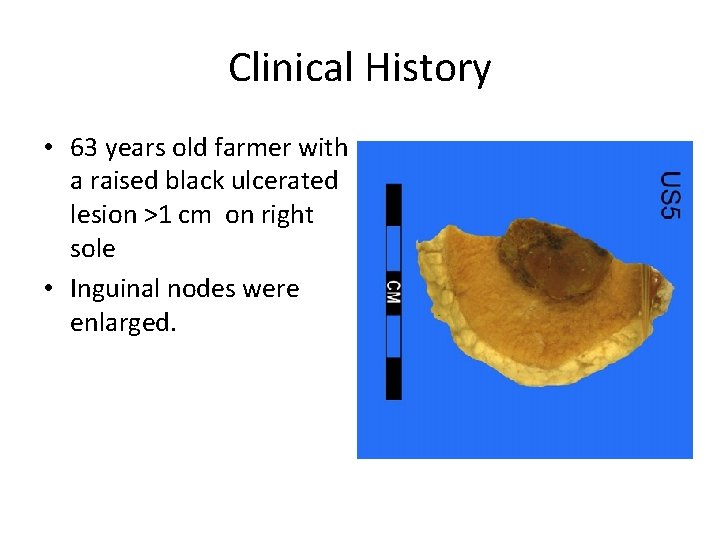
Clinical History • 63 years old farmer with a raised black ulcerated lesion >1 cm on right sole • Inguinal nodes were enlarged.
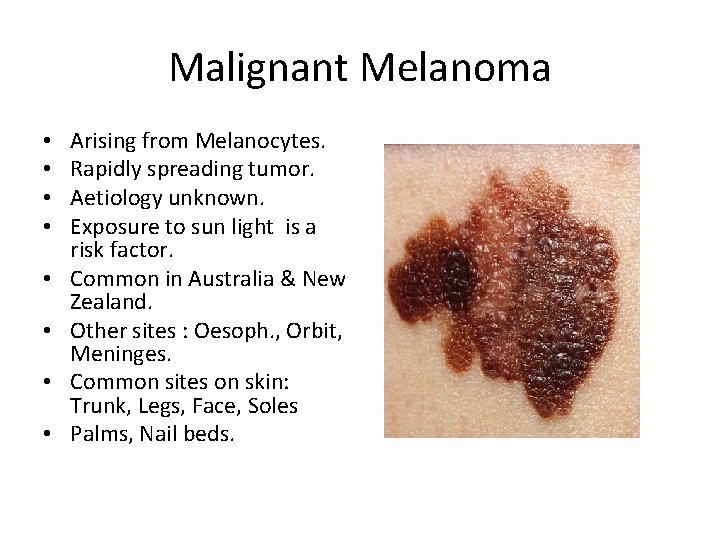
Malignant Melanoma • • Arising from Melanocytes. Rapidly spreading tumor. Aetiology unknown. Exposure to sun light is a risk factor. Common in Australia & New Zealand. Other sites : Oesoph. , Orbit, Meninges. Common sites on skin: Trunk, Legs, Face, Soles Palms, Nail beds.
Some high risk factors • Persistent change in appearance of a mole. • Presence of pre-existing dysplastic naevus. • Family H/O melanoma in a patient with atypical mole. • Higher age of the patient. • More than 50 moles > 2 mm in diameter. • May arise from pre-existing mole or de novo.
Molecular Studies • • Germ line mutation in CDKN 2 A gene. PTEN Gene mutation. Mutation of other tumor suppressor genes. No p 53 gene mutation.
Morphology • • Grossly based on Clinical course & prognosis: 1. Lentigo Maligna Melanoma: Arises from a pre-existing lentigo (flat nevus) Essentially a melanoma-in-situ. Slow growing, good prognosis. 2. Superficial spreading melanoma: Slightly elevated, variegated colors. Prognosis worse than lentigo maligna melanoma.
Morphology (contd. ) • • 3. Acral lentiginous melanoma: Soles & palms, mucosal surfaces. Ulcerated, with early metastasis. Prognosis worse than superficial spreading type. 4. Nodular melanoma: Elevated deeply pigmented nodule Rapidly growing, ulcerated. Worst prognosis.
A B C D Of Melanoma • A = Asymmetry. • B= Borders irregular. • C= Color variation. • D= Diameter > 6 mm.

. A 1. 5 -cm melanoma with characteristic asymmetry, irregular borders, and color variation.
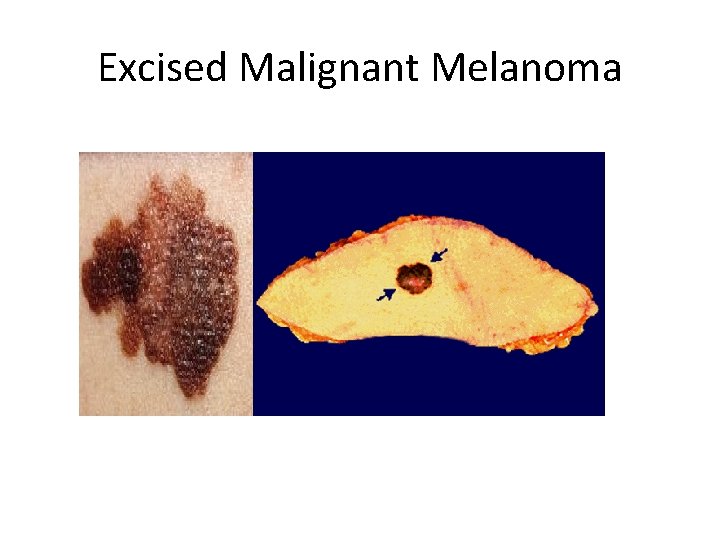
Excised Malignant Melanoma
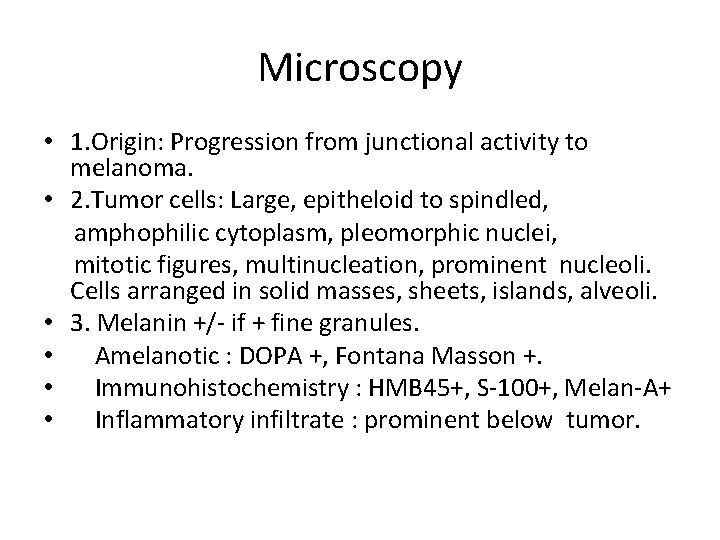
Microscopy • 1. Origin: Progression from junctional activity to melanoma. • 2. Tumor cells: Large, epitheloid to spindled, amphophilic cytoplasm, pleomorphic nuclei, mitotic figures, multinucleation, prominent nucleoli. Cells arranged in solid masses, sheets, islands, alveoli. • 3. Melanin +/- if + fine granules. • Amelanotic : DOPA +, Fontana Masson +. • Immunohistochemistry : HMB 45+, S-100+, Melan-A+ • Inflammatory infiltrate : prominent below tumor.

Malignant Melanoma Skin: Clinical

Prognosis Depends on Depth of invasion, size, ulceration, mitosis, 2° Clark’s levels : Level I: Confined to epidermis. Level II: Papillary dermis. Level III: Interface between papillary & reticular dermis. • Level IV: Reticular dermis. • Level V: Subcutaneous tissue. • Spontaneous regression of primary lesion may + • • •
- Slides: 36