Spotlight Case Delirium or Dementia Source and Credits
- Slides: 20
Spotlight Case Delirium or Dementia?
Source and Credits • This presentation is based on the May 2009 AHRQ Web. M&M Spotlight Case – See the full article at http: //webmm. ahrq. gov – CME credit is available • Commentary by: James L. Rudolph, MD, SM – Editor, AHRQ Web. M&M: Robert Wachter, MD – Spotlight Editor: Sumant Ranji, MD – Managing Editor: Erin Hartman, MS 2
Objectives • • 3 At the conclusion of this educational activity, participants should be able to: State the key diagnostic differences between delirium and dementia Describe the Confusion Assessment Method for workup of suspected delirium Explain the risks associated with using physical restraints in geriatric inpatients Describe the initial workup of delirium in a hospitalized patient
Case: Delirium or Dementia? An 86 -year-old woman, admitted with complaints of shortness of breath and cough, was found to have pneumonia. Her past medical history included cataract surgery, hypertension controlled with medications, and type 2 diabetes controlled by diet. She was ambulatory, lived alone, and at baseline completed all activities of daily living independently. According to her daughter, the patient was never disoriented. 4
Case: Delirium or Dementia? (2) At admission, the patient appeared mildly dehydrated. Her oxygen saturation was 94% on 2 liters oxygen by nasal cannula, and an arterial blood gas showed a normal p. CO 2 of 40 mm. Hg. Her daughter requested to spend the night at the bedside, but was told she could not stay, per hospital policy. 5
Case: Delirium or Dementia? (3) Overnight, nursing staff noted the patient to be disoriented. She began pulling at her intravenous lines and attempting to get out of bed. The covering physician was called, and ordered that the patient be placed in four-point restraints. The next morning, the daughter returned to find her mother in restraints, speaking incoherently and severely short of breath. The daughter asked the nurse what happened, and reiterated that her mother had never been confused before. 6
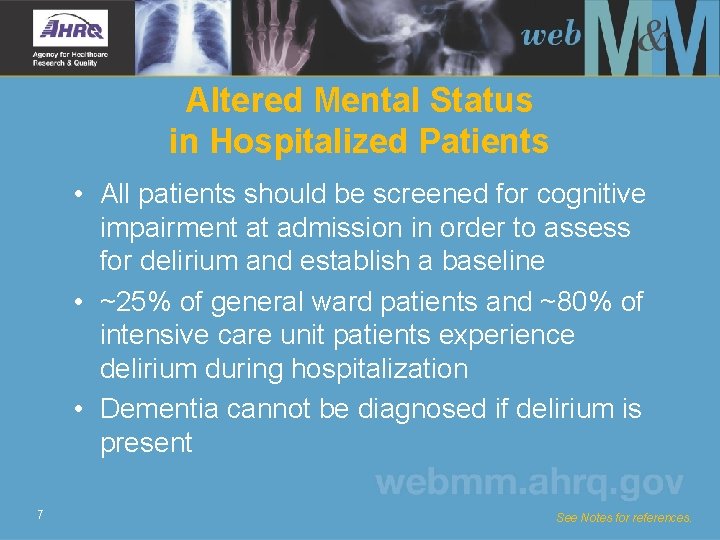
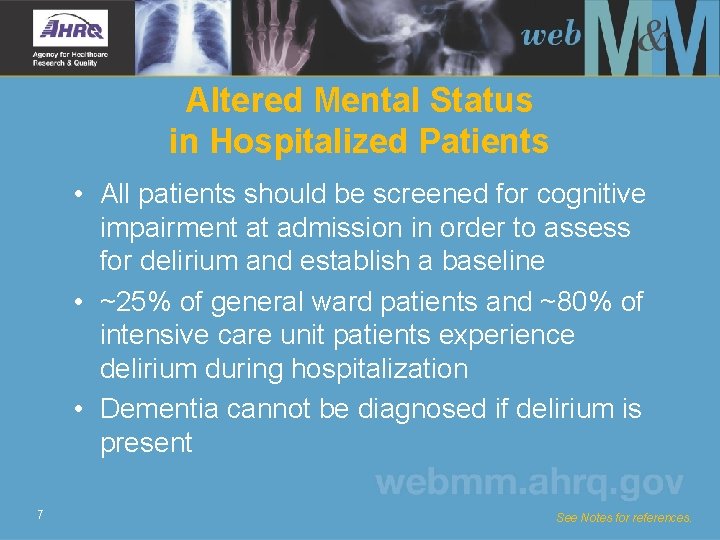
Altered Mental Status in Hospitalized Patients • All patients should be screened for cognitive impairment at admission in order to assess for delirium and establish a baseline • ~25% of general ward patients and ~80% of intensive care unit patients experience delirium during hospitalization • Dementia cannot be diagnosed if delirium is present 7 See Notes for references.
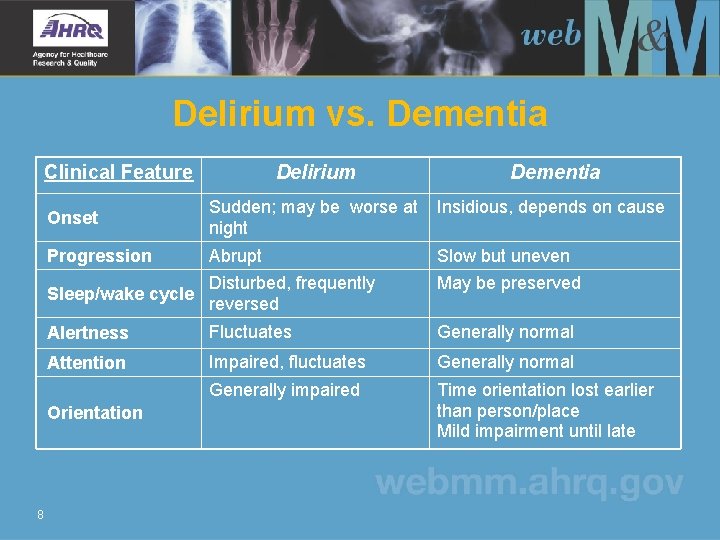
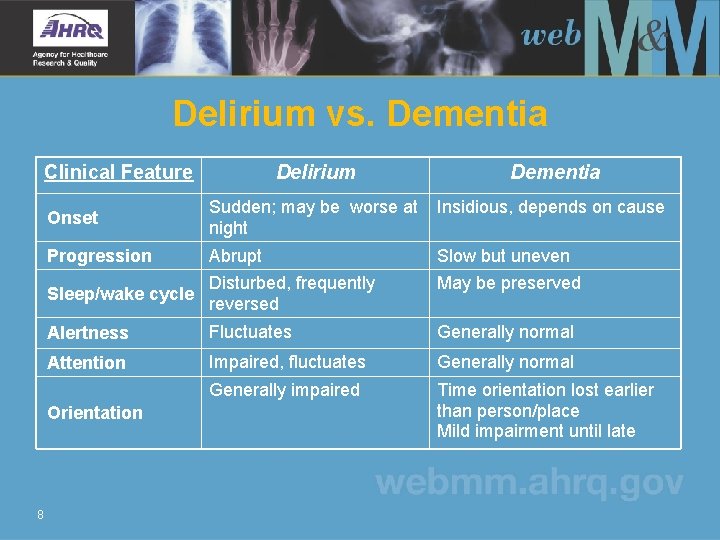
Delirium vs. Dementia Clinical Feature Delirium Dementia Onset Sudden; may be worse at night Insidious, depends on cause Progression Abrupt Slow but uneven Sleep/wake cycle Disturbed, frequently reversed May be preserved Alertness Fluctuates Generally normal Attention Impaired, fluctuates Generally normal Generally impaired Time orientation lost earlier than person/place Mild impairment until late Orientation 8
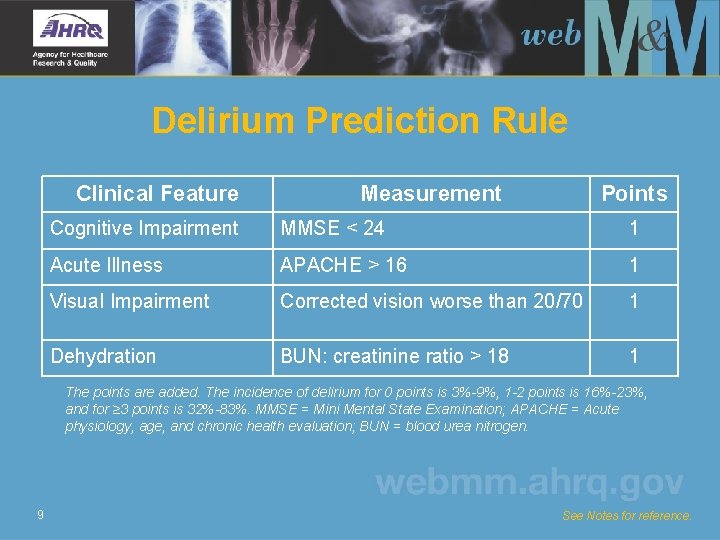
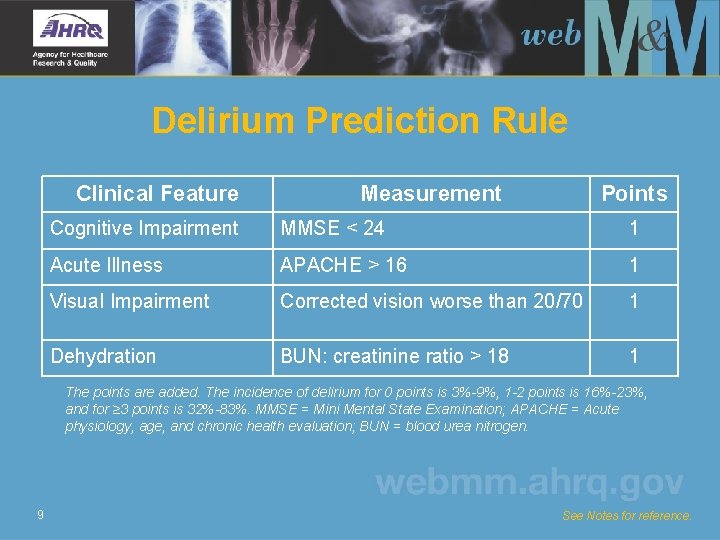
Delirium Prediction Rule Clinical Feature Measurement Points Cognitive Impairment MMSE < 24 1 Acute Illness APACHE > 16 1 Visual Impairment Corrected vision worse than 20/70 1 Dehydration BUN: creatinine ratio > 18 1 The points are added. The incidence of delirium for 0 points is 3%-9%, 1 -2 points is 16%-23%, and for ≥ 3 points is 32%-83%. MMSE = Mini Mental State Examination; APACHE = Acute physiology, age, and chronic health evaluation; BUN = blood urea nitrogen. 9 See Notes for reference.
Hospital Environment Predisposes To Delirium • Many new faces: 10 -20 staff may see patient in one day, leading to disorientation • Decreased cognitive stimuli: urinary catheters and restraints confine patients to bed, with attendant risks • Loss of sleep due to noise or intrusions 10 See Notes for references.
Psychomotor Variants of Delirium • Hyperactive (25%) – These patients are more likely to receive chemical or physical restraints • Hypoactive (50%) – May be misdiagnosed as depression or dementia • Mixed (25%) 11 See Notes for reference.
Risks of Delirium in Hospitalized Patients • Underlying cause of delirium may be missed • Over-medication (especially in hyperactive and mixed subtypes) • Amplifies risks of hospitalization – Deconditioning and malnutrition – Aspiration pneumonia – Nosocomial infection (especially due to urinary catheters) – Pressure ulcers 12 See Notes for reference.
Physical Restraints • Risky for several reasons – Independently associated with development of delirium – Reduce external stimuli may exacerbate delirium – May exacerbate hyperactive behavior 13 See Notes for references.
Before Applying Restraints • Consider: – – – What is intended effect of restraint? Can intended effect be achieved by other means? Is this the least invasive restraint? Is using restraints in the patient’s best interest? Are restraints being used for secondary benefits (i. e. , to limit calls or pages)? – When will restraint be removed? 14 See Notes for references.
Case: Delirium or Dementia? (4) The doctor was called an arterial blood gas was performed. The patient’s Pa. O 2 was 91 mm. Hg, but the Pa. Co 2 was 58 mm. Hg, a marked increase since admission. Despite the patient’s deteriorating clinical condition, the patient’s worsening level of consciousness was attributed to “senile dementia” and not impending respiratory failure (as evidenced by the significant carbon dioxide retention). No further action was taken. 15
Case: Delirium or Dementia? (5) Over the course of the day, the patient developed worsening respiratory distress, became comatose, and was transferred to the intensive care unit. She subsequently developed respiratory failure requiring intubation and renal failure requiring dialysis. Her condition did not significantly improve, and she died 2 weeks later. 16
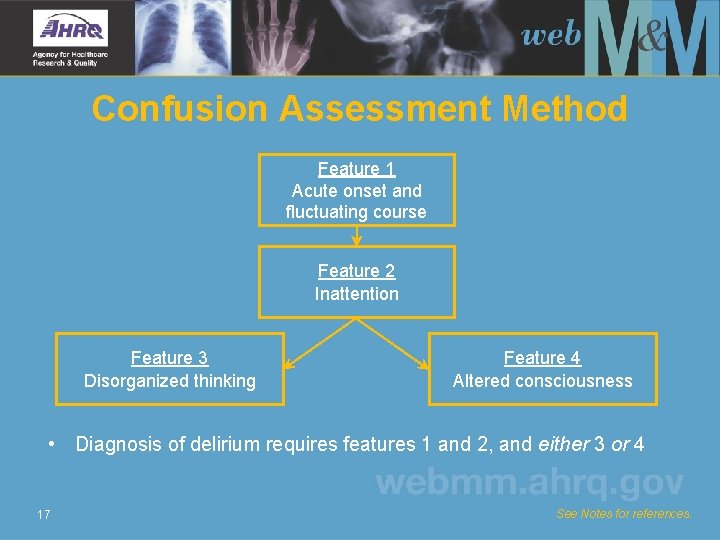
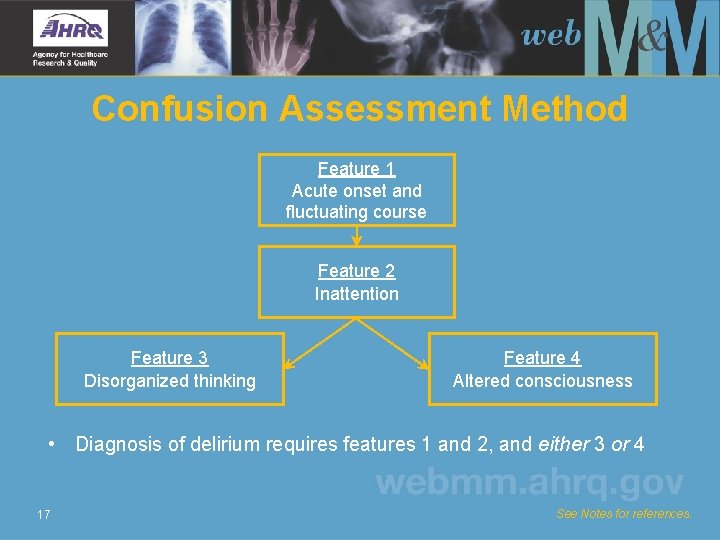
Confusion Assessment Method Feature 1 Acute onset and fluctuating course Feature 2 Inattention Feature 3 Disorganized thinking Feature 4 Altered consciousness • Diagnosis of delirium requires features 1 and 2, and either 3 or 4 17 See Notes for references.
Workup of Delirium • History and physical examination • Neurological examination • Collateral information from family, nursing • Review of medications • Especially benzodiazepines, anticholinergics, and antipsychotics • Drugs that were recently stopped and may cause withdrawal syndrome (opioids, antidepressants, alcohol) • Basic laboratory tests for electrolytes, kidney function, workup of suspected infection Identify and treat underlying cause that precipitated delirium 18
The Role of Family Members at the Bedside • Reorienting stimulus for patient – 10 -20 staff may see patient daily, facilitating disorientation • Source of cognitive stimulation • Participate in care of patient to the extent possible 19 See Notes for reference.
Take-Home Points • Delirium, an acute change in cognition and attention, is common, morbid, and costly • In the inpatient setting, all new changes in mental status should be assumed to be delirium until proven otherwise • The treatment of delirium is to identify and remedy the underlying causes • Elements of the hospital environment can contribute to delirium and expose patients to safety risk • Family members and caregivers are crucial to the diagnosis and management of delirium; incorporating them into the plan of care is strongly recommended 20