Sports Medicine 25 Injury Assessment Management Sports Medicine

- Slides: 24
Sports Medicine 25 Injury Assessment & Management Sports Medicine 25 – A. Eastlake & A. Morgan 1
Injury Assessment & Management The intent of this section is NOT to make you an expert at injury assessment. It is to provide you with some basic information to help you determine the SEVERITY of an injury. The following steps should be applied to common musculoskeletal conditions sprained ankles), NOT life-threatening situations. (e. g. 2
Descriptive Assessment Terms n n Etiology or Mechanism – cause of an injury Pathology – refers to structural and functional changes that result from injury Symptom – refers to a perceived change in an athlete’s body or its functions that indicates an injury or disease. . subjective Signs – definitive, obvious indicator of a specific condition 3
Descriptive Assessment Terms n Diagnosis – name of a specific condition n Prognosis – predicted outcome of an injury n n Sequela – condition resulting from disease or injury (example: pneumonia from the flu) Syndrome – symptoms and signs together indicating a disease or condition. 4
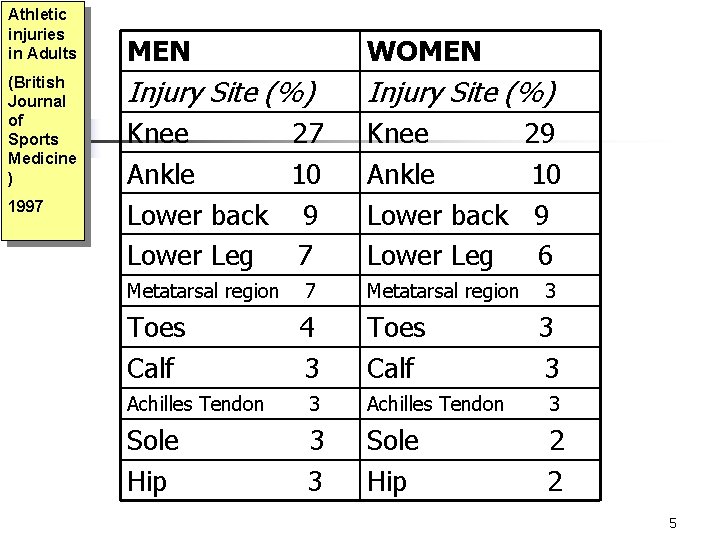
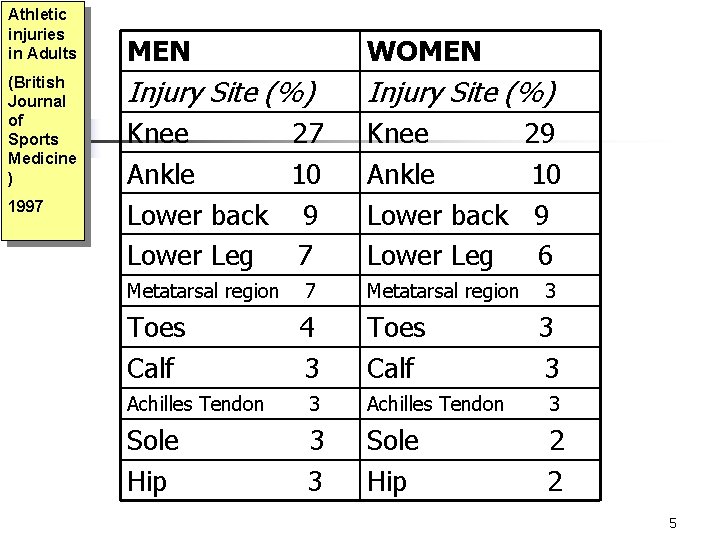
Athletic injuries in Adults (British Journal of Sports Medicine ) 1997 MEN WOMEN Injury Site (%) Knee 27 Ankle 10 Lower back 9 Lower Leg 7 Knee 29 Ankle 10 Lower back 9 Lower Leg 6 Metatarsal region 7 Metatarsal region 3 Toes Calf 4 3 Toes Calf 3 3 Achilles Tendon 3 Sole Hip 3 3 Sole Hip 2 2 5
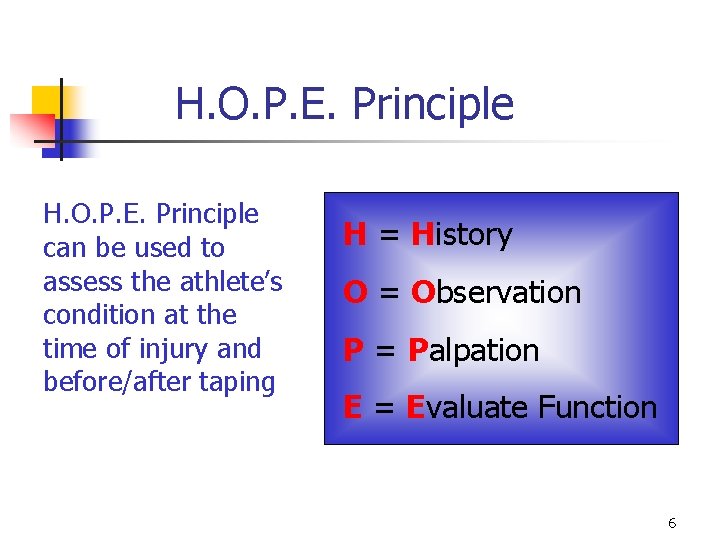
H. O. P. E. Principle can be used to assess the athlete’s condition at the time of injury and before/after taping H = History O = Observation P = Palpation E = Evaluate Function 6
H. O. P. E. Principle is sometimes recognized as “ H. O. P. S “ H = History O = Observation P = Palpation S = Special Tests 7
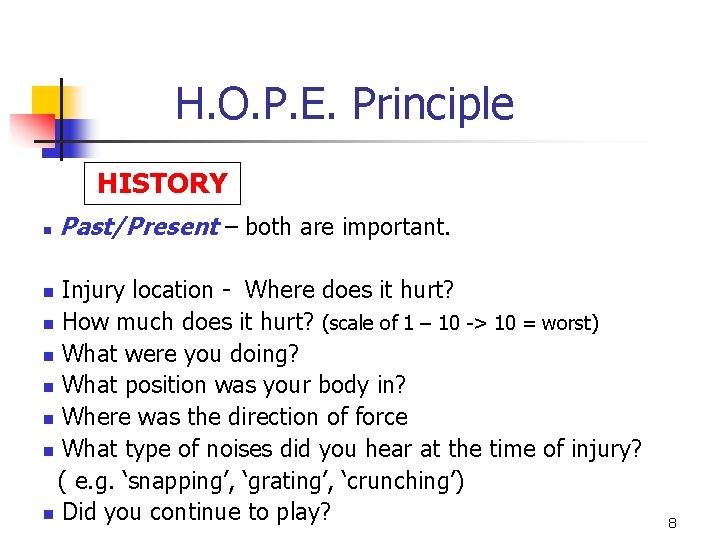
H. O. P. E. Principle HISTORY n Past/Present – both are important. Injury location - Where does it hurt? n How much does it hurt? (scale of 1 – 10 -> 10 = worst) n What were you doing? n What position was your body in? n Where was the direction of force n What type of noises did you hear at the time of injury? ( e. g. ‘snapping’, ‘grating’, ‘crunching’) n Did you continue to play? n 8
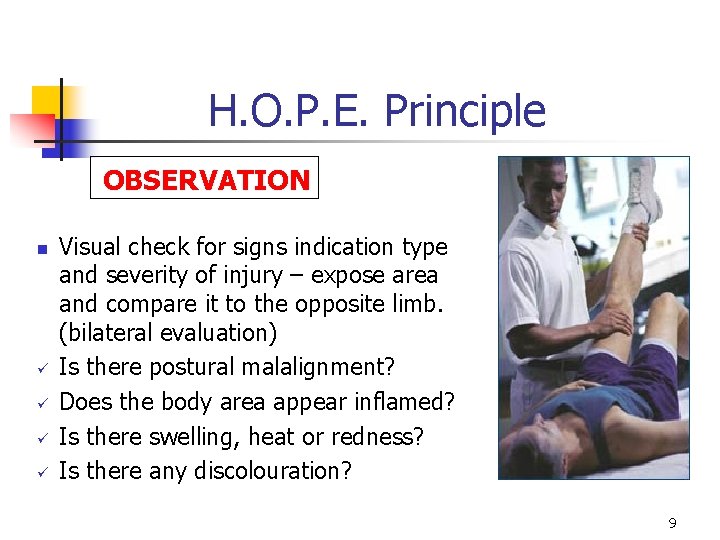
H. O. P. E. Principle OBSERVATION n ü ü Visual check for signs indication type and severity of injury – expose area and compare it to the opposite limb. (bilateral evaluation) Is there postural malalignment? Does the body area appear inflamed? Is there swelling, heat or redness? Is there any discolouration? 9
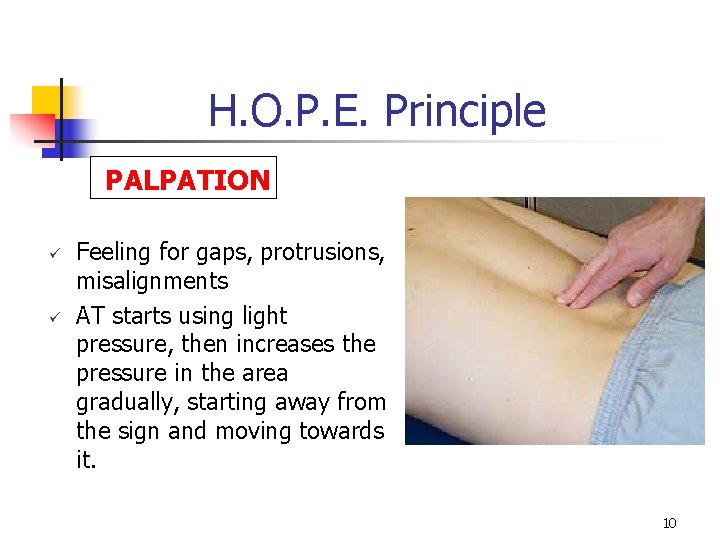
H. O. P. E. Principle PALPATION ü ü Feeling for gaps, protrusions, misalignments AT starts using light pressure, then increases the pressure in the area gradually, starting away from the sign and moving towards it. 10

H. O. P. E. Principle PALPATION ü ü Allows for further evaluation of the signs of the injury. Tenderness to touch noted by athlete’s apprehension, and warmth due to inflammation can be established through gentle palpation. . 11
H. O. P. E. Principle EVALUATE FUNCTION n n n Movement assessment – evaluating the amount of available joint and/or limb function. Must know anatomy well: Normal ROM, Muscles, Bones, Anatomical planes. Start with easy tests and progress to more difficult. The progression will depend on the athlete’s ability to satisfactorily complete tasks required for the activity. 12
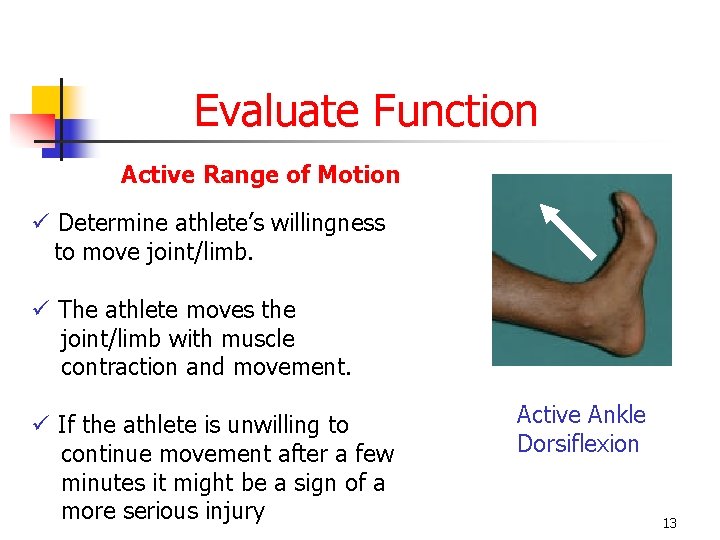
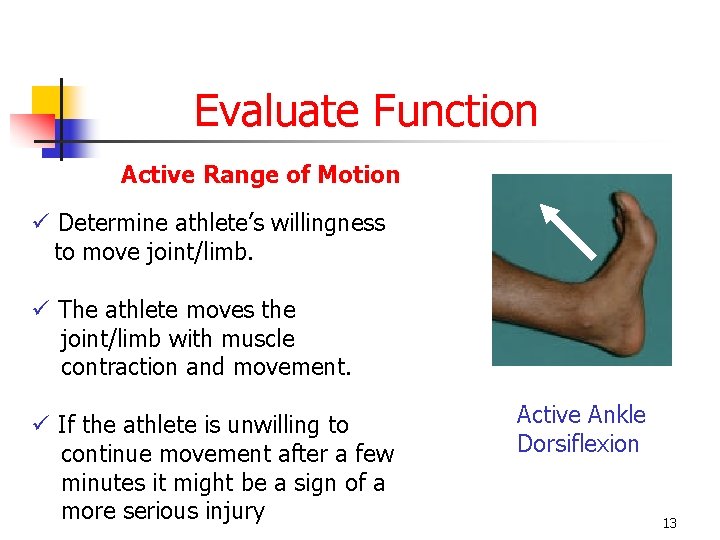
Evaluate Function Active Range of Motion ü Determine athlete’s willingness to move joint/limb. ü The athlete moves the joint/limb with muscle contraction and movement. ü If the athlete is unwilling to continue movement after a few minutes it might be a sign of a more serious injury Active Ankle Dorsiflexion 13
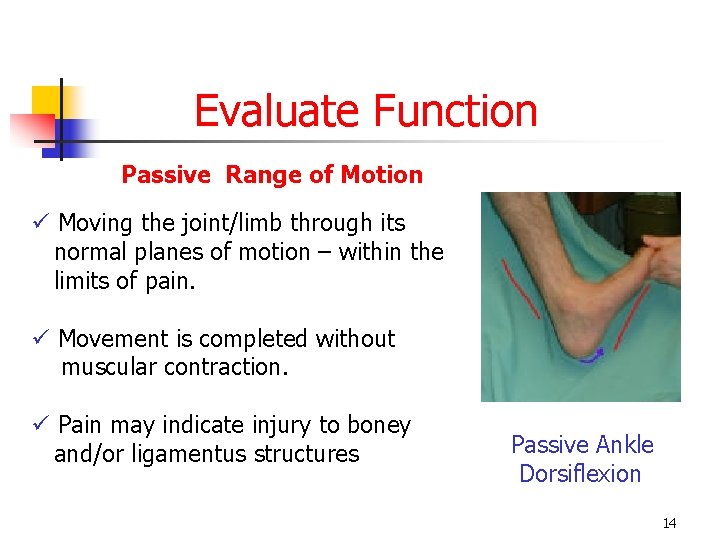
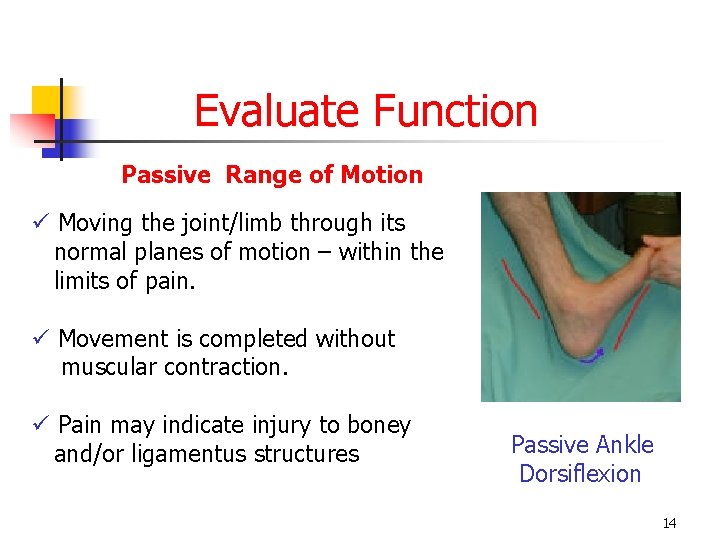
Evaluate Function Passive Range of Motion ü Moving the joint/limb through its normal planes of motion – within the limits of pain. ü Movement is completed without muscular contraction. ü Pain may indicate injury to boney and/or ligamentus structures Passive Ankle Dorsiflexion 14
Evaluate Function Resisted Range of Motion ü Injury to contractile structures (muscles & tendons) may be determined by having the athlete hold a limb or joint in a particular position while AT attempts to move it. ü The athlete provides resistance to applies pressure. ü E. G. -> “Do not let me point your toes” The athlete will have to hold the ankle in place while the AT produces resistance from the top of the foot. 15
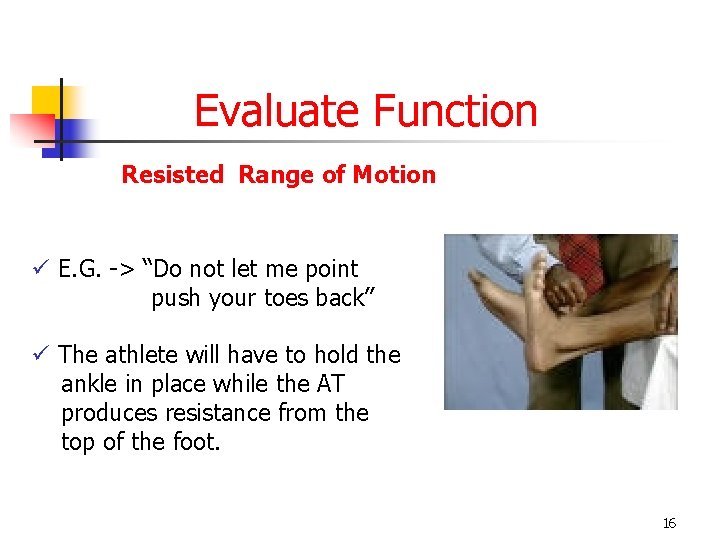
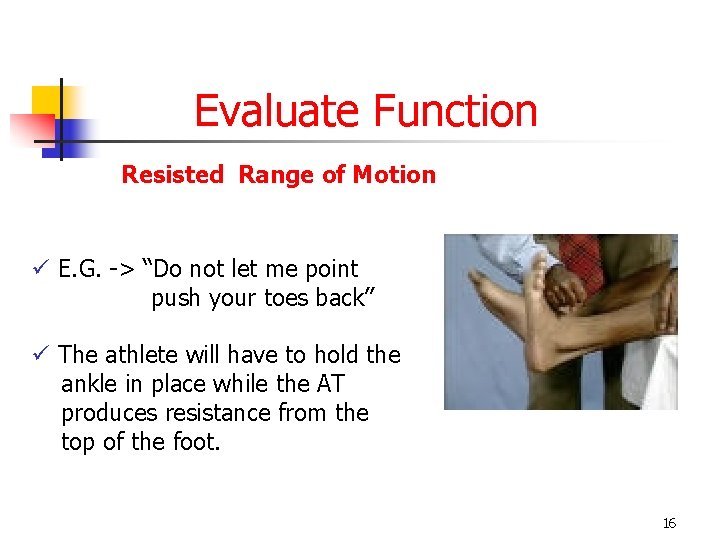
Evaluate Function Resisted Range of Motion ü E. G. -> “Do not let me point push your toes back” ü The athlete will have to hold the ankle in place while the AT produces resistance from the top of the foot. 16
Evaluate Function Active - Passive - Resisted -> Range of Motion ü The ROM evaluations will assist in clarifying which structures may be injured. ü Diagnosis must be made by a medical professional. ü Next Step -> testing balance – perform skill slowly, with little force and gradually increase speed/force -> STOP test if unable to adequately perform. 17
Evaluate Function Active - Passive - Resisted -> Range of Motion ü All observations, palpations and evaluations should be done BILATERALLY. ü In order to determine the extent of a particular injury, the uninjured joint/limb must be evaluated to establish a baseline from which to compare the joint/limb. 18
Severity of Injury It is important to immediately establish the severity of an injury to prevent mismanagement. The acronym P. Q. R. S. T can be used for non life-threatening injuries. 19
P. Q. R. S. T PAIN ü Pain is the least reliable indicator of severity of injury. ü Any degree of pain must be given serious attention. (physical and/or psychological) ü It is important to establish a complete description of the injury which can be remembered by P. Q. R. S. T. 20
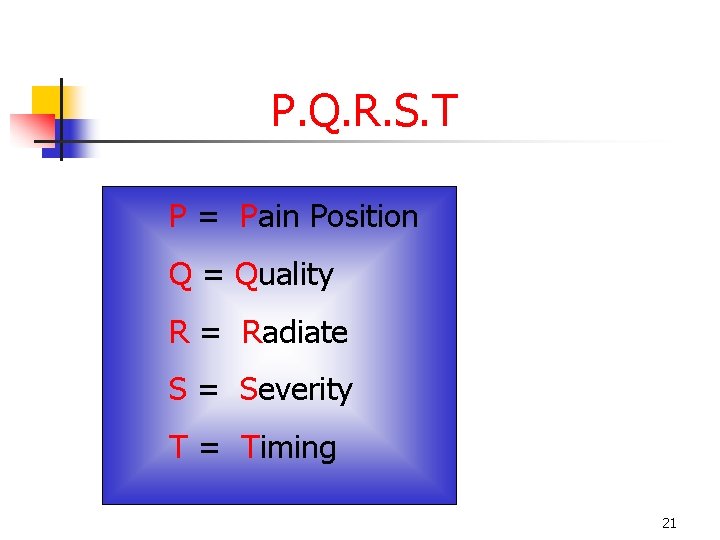
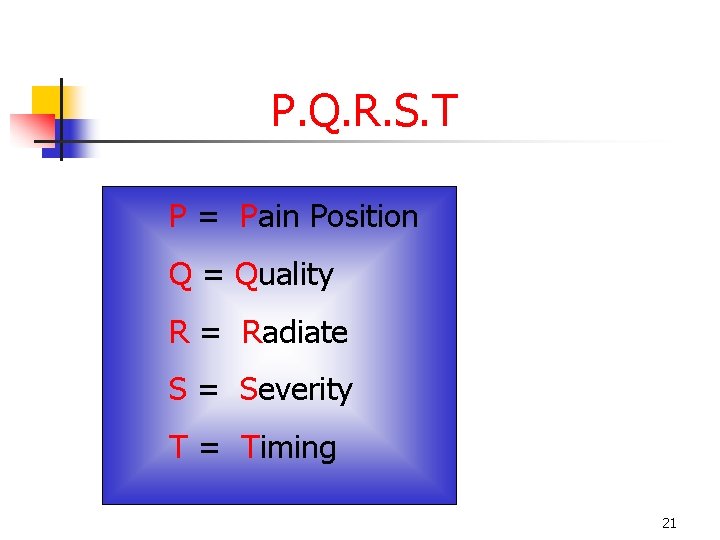
P. Q. R. S. T P = Pain Position Q = Quality R = Radiate S = Severity T = Timing 21
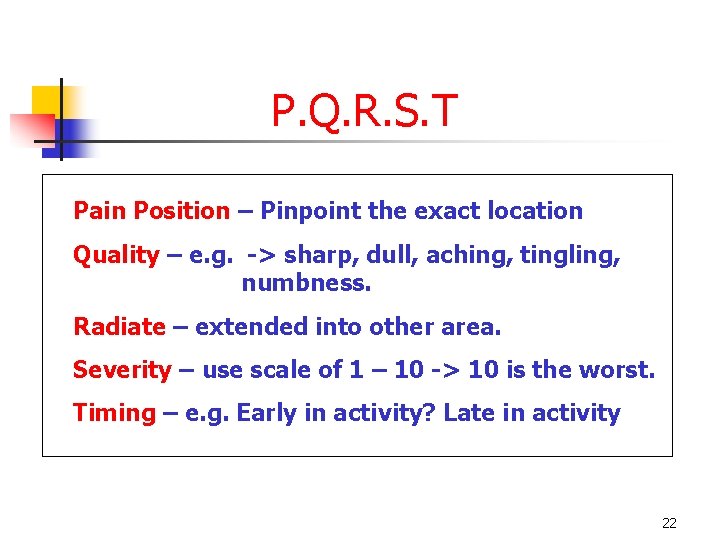
P. Q. R. S. T Pain Position – Pinpoint the exact location Quality – e. g. -> sharp, dull, aching, tingling, numbness. Radiate – extended into other area. Severity – use scale of 1 – 10 -> 10 is the worst. Timing – e. g. Early in activity? Late in activity 22
P. Q. R. S. T Other Considerations Sensation: ü At the time of injury, was there a pop or snap? ü Was there a sensation of the joint / limb ‘giving way’? ü The athlete may use descriptive words such as clicking, grating, tearing, locking, catching, numbness and warmth. 23
P. Q. R. S. T Other Considerations Know the Athlete: ü Do you know the athlete’s current physical, psychological and emotional state? e. g. -> some athletes have a higher/lower tolerance to pain or sight of blood. 24
 Examples of intentional injury
Examples of intentional injury Flipchart on safety practices and sports injury management
Flipchart on safety practices and sports injury management Sports injury definition
Sports injury definition Sports injury definition
Sports injury definition Hops in sports medicine
Hops in sports medicine Hops sports medicine examples
Hops sports medicine examples Head injury assessment
Head injury assessment Dartos tissue
Dartos tissue Troy injury management
Troy injury management Copyright
Copyright Sports medicine definition
Sports medicine definition Rop sports medicine
Rop sports medicine Sports medicine definition
Sports medicine definition Sports medicine terminology
Sports medicine terminology Meditouch sports medicine
Meditouch sports medicine Sports venues vocabulary
Sports venues vocabulary Flexion adduction internal rotation
Flexion adduction internal rotation Soap sports medicine
Soap sports medicine What is the importance of taping and wrapping?
What is the importance of taping and wrapping? Scope of sports medicine
Scope of sports medicine Sports medicine team project
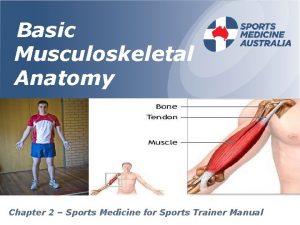
Sports medicine team project Chapter 2 sports medicine
Chapter 2 sports medicine Sports medicine umbrella
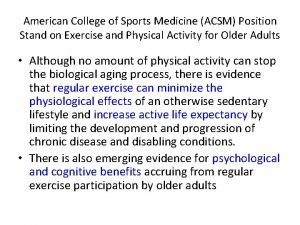
Sports medicine umbrella What does acsm stand for
What does acsm stand for Sports medicine team definition
Sports medicine team definition