Spontaneous extensor tendon rupture in RA wrist Risk
- Slides: 12
Spontaneous extensor tendon rupture in RA wrist: Risk factor & Prevention Jung-Hua Hsueh, Lee-Wei Chen, M. D. , Ph. D Department of Plastic Surgery, Kaohsiung Veterans General Hospital, Taiwan 2015. 10 ~10. 14 Relevant Financial Interests: nothing to disclose
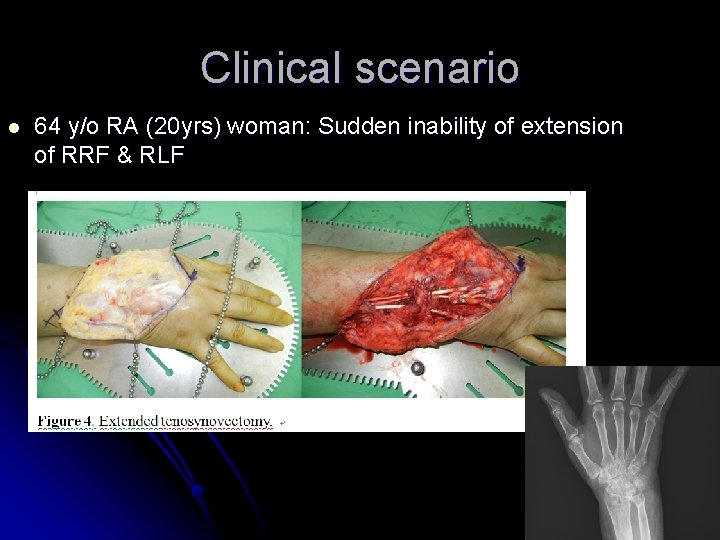
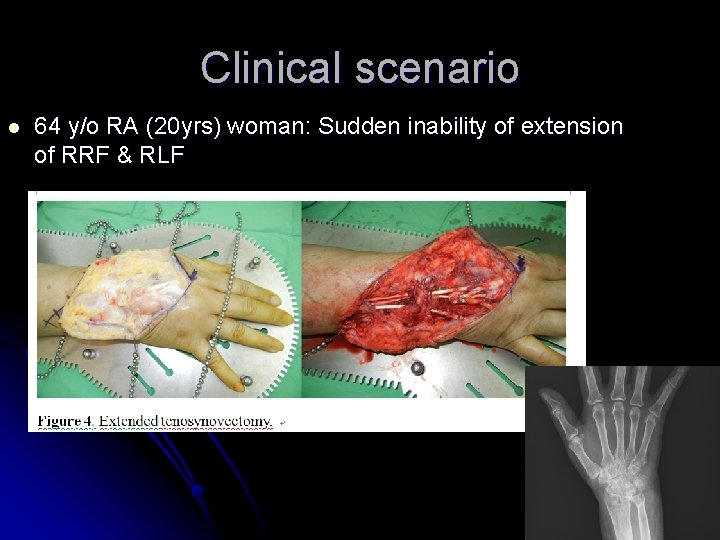
Clinical scenario l 64 y/o RA (20 yrs) woman: Sudden inability of extension of RRF & RLF
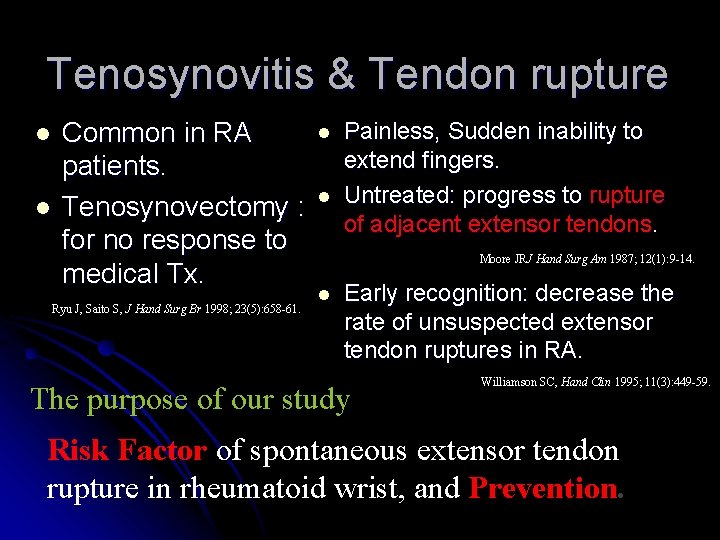
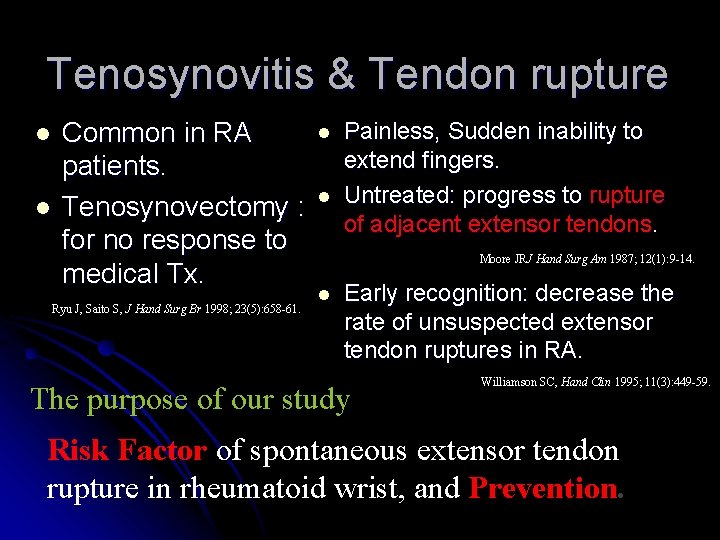
Tenosynovitis & Tendon rupture l l Common in RA patients. Tenosynovectomy : for no response to medical Tx. Ryu J, Saito S, J Hand Surg Br 1998; 23(5): 658 -61. l l Painless, Sudden inability to extend fingers. Untreated: progress to rupture of adjacent extensor tendons. Moore JRJ Hand Surg Am 1987; 12(1): 9 -14. l Early recognition: decrease the rate of unsuspected extensor tendon ruptures in RA. The purpose of our study Williamson SC, Hand Clin 1995; 11(3): 449 -59. Risk Factor of spontaneous extensor tendon rupture in rheumatoid wrist, and Prevention.
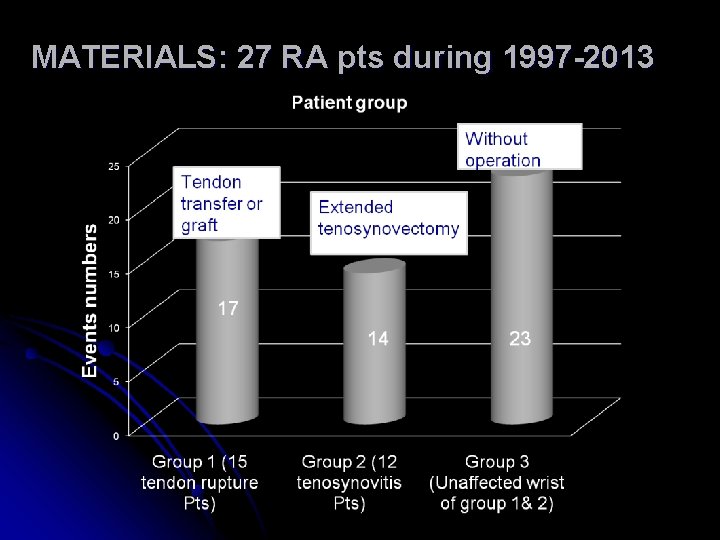
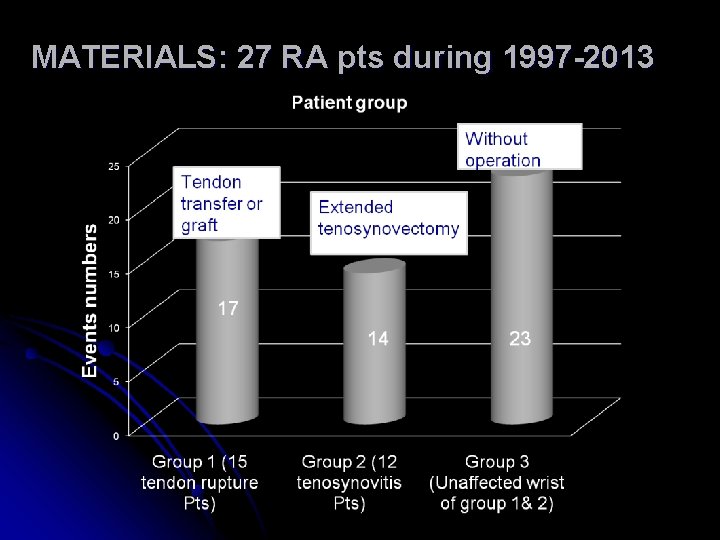
MATERIALS: 27 RA pts during 1997 -2013
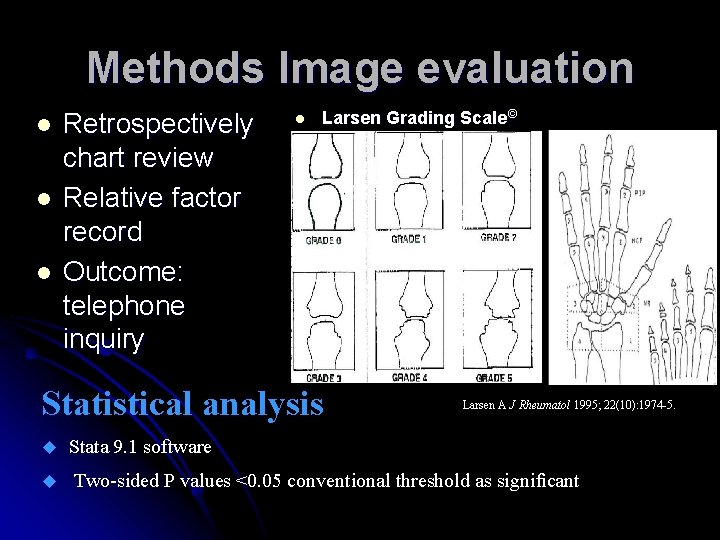
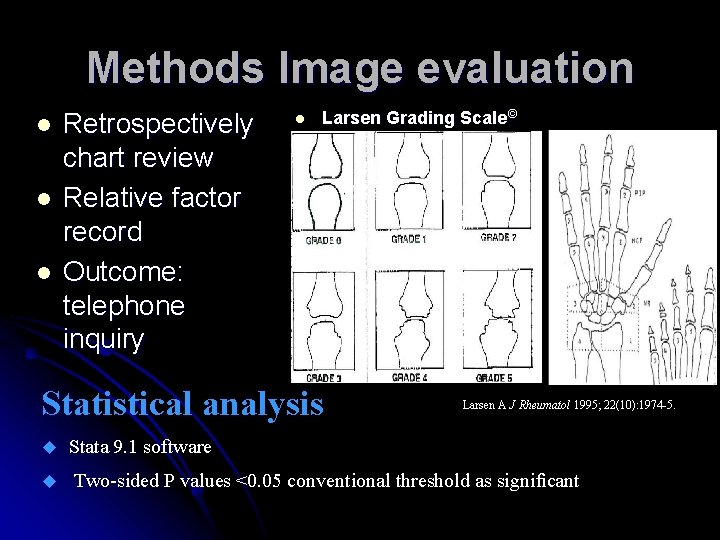
Methods Image evaluation l l l Retrospectively chart review Relative factor record Outcome: telephone inquiry l Larsen Grading Scale© Statistical analysis Larsen A J Rheumatol 1995; 22(10): 1974 -5. Stata 9. 1 software Two-sided P values <0. 05 conventional threshold as significant
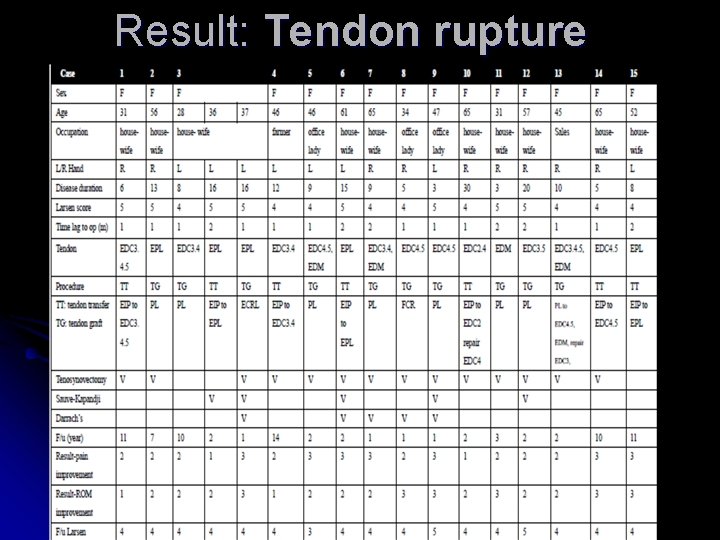
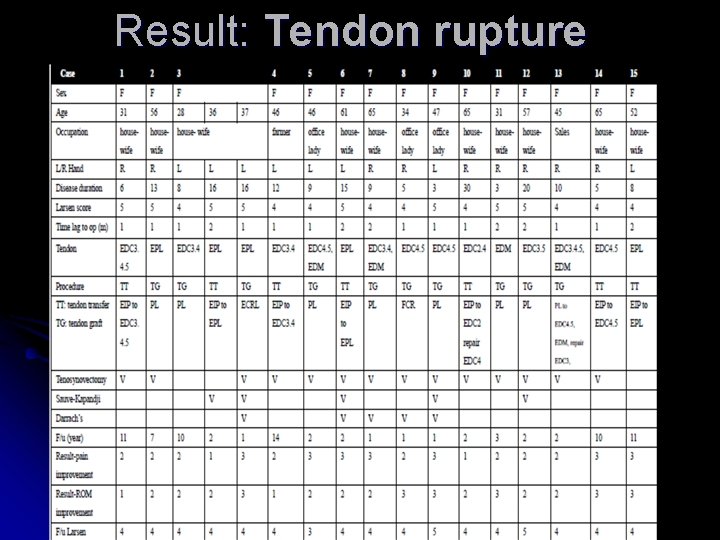
Result: Tendon rupture group data
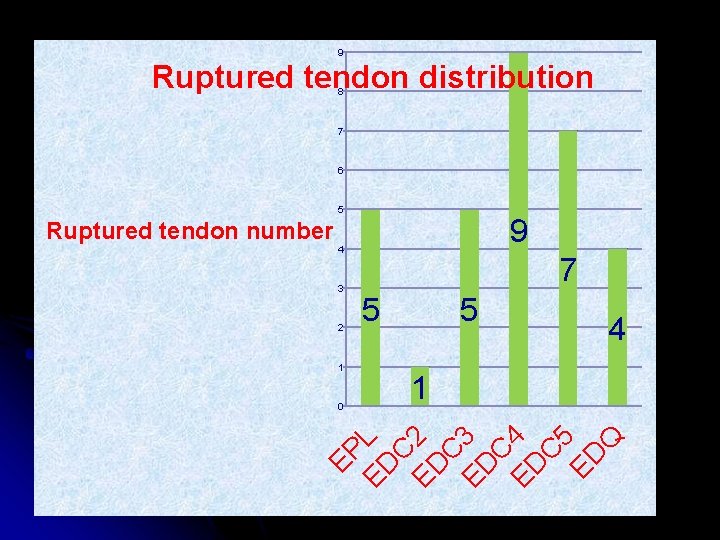
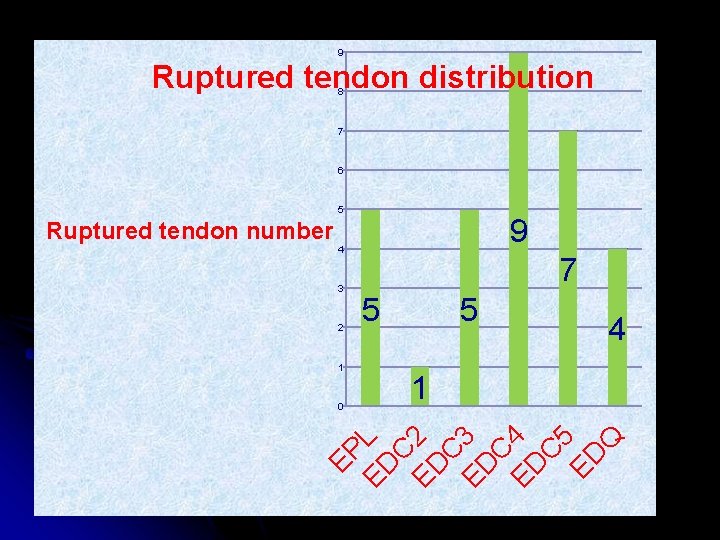
9 Ruptured tendon distribution 8 7 6 5 Ruptured tendon number 9 4 3 2 1 5 5 4 1 EP ED L C ED 2 C ED 3 C ED 4 C 5 ED Q 0 7
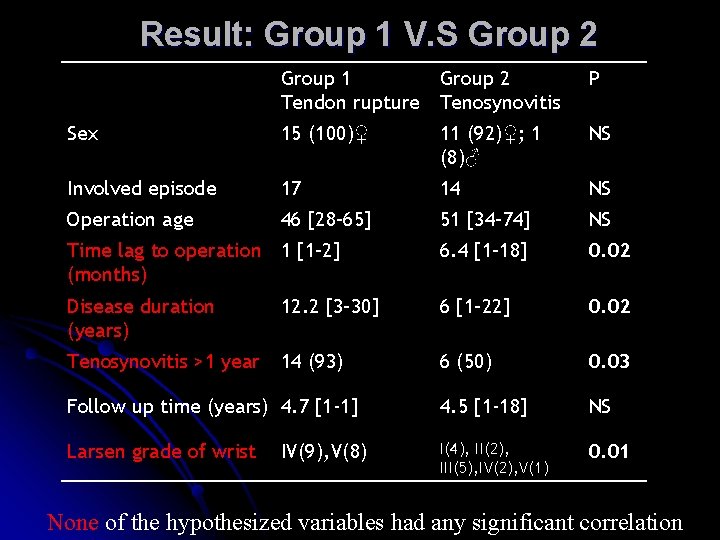
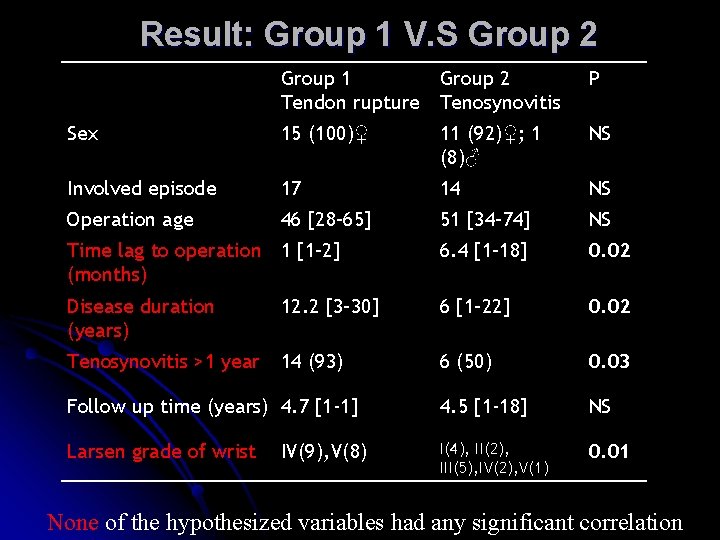
Result: Group 1 V. S Group 2 Group 1 Group 2 Tendon rupture Tenosynovitis P Sex 15 (100)♀ 11 (92)♀; 1 (8)♂ NS Involved episode 17 14 NS Operation age 46 [28– 65] 51 [34– 74] NS Time lag to operation 1 [1– 2] (months) 6. 4 [1– 18] 0. 02 Disease duration (years) 12. 2 [3– 30] 6 [1– 22] 0. 02 Tenosynovitis >1 year 14 (93) 6 (50) 0. 03 Follow up time (years) 4. 7 [1 -1] 4. 5 [1 -18] NS Larsen grade of wrist I(4), II(2), III(5), IV(2), V(1) 0. 01 IV(9), V(8) None of the hypothesized variables had any significant correlation
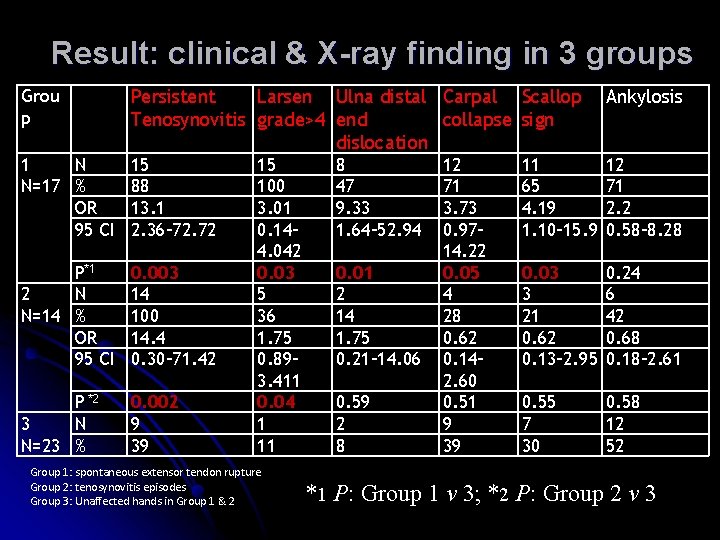
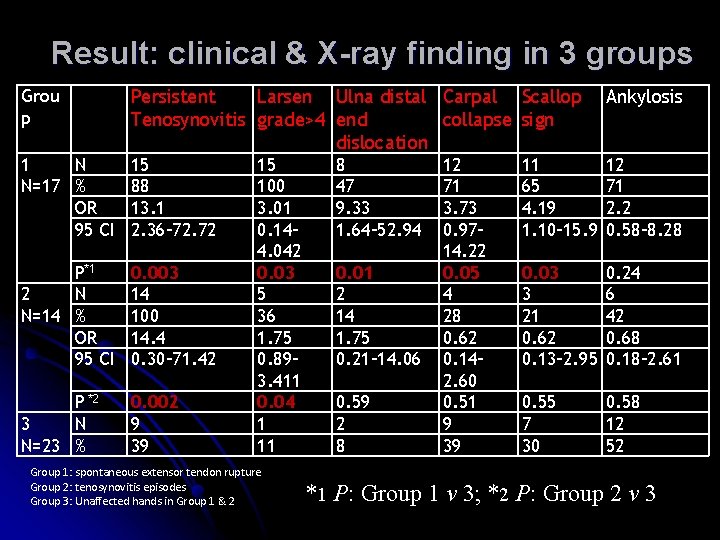
Result: clinical & X-ray finding in 3 groups Grou p Persistent Larsen Ulna distal Carpal Scallop Tenosynovitis grade>4 end collapse sign dislocation Ankylosis 1 N N=17 % OR 95 CI 15 88 13. 1 2. 36– 72. 72 11 65 4. 19 1. 10– 15. 9 12 71 2. 2 0. 58– 8. 28 P*1 2 N N=14 % OR 95 CI 0. 003 14 100 14. 4 0. 30– 71. 42 0. 03 3 21 0. 62 0. 13– 2. 95 0. 24 6 42 0. 68 0. 18– 2. 61 P *2 3 N N=23 % 0. 002 9 39 0. 55 7 30 0. 58 12 52 15 100 3. 01 0. 14– 4. 042 0. 03 5 36 1. 75 0. 89– 3. 411 0. 04 1 11 Group 1: spontaneous extensor tendon rupture Group 2: tenosynovitis episodes Group 3: Unaffected hands in Group 1 & 2 8 47 9. 33 1. 64– 52. 94 0. 01 2 14 1. 75 0. 21– 14. 06 0. 59 2 8 12 71 3. 73 0. 97– 14. 22 0. 05 4 28 0. 62 0. 14– 2. 60 0. 51 9 39 *1 P: Group 1 v 3; *2 P: Group 2 v 3
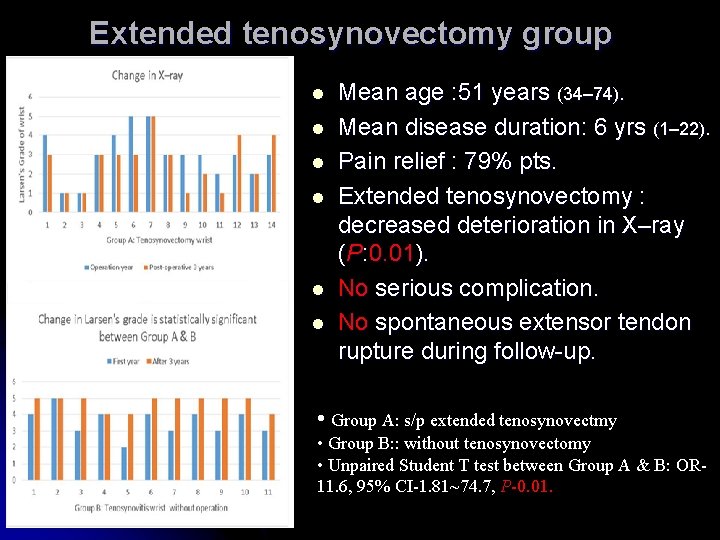
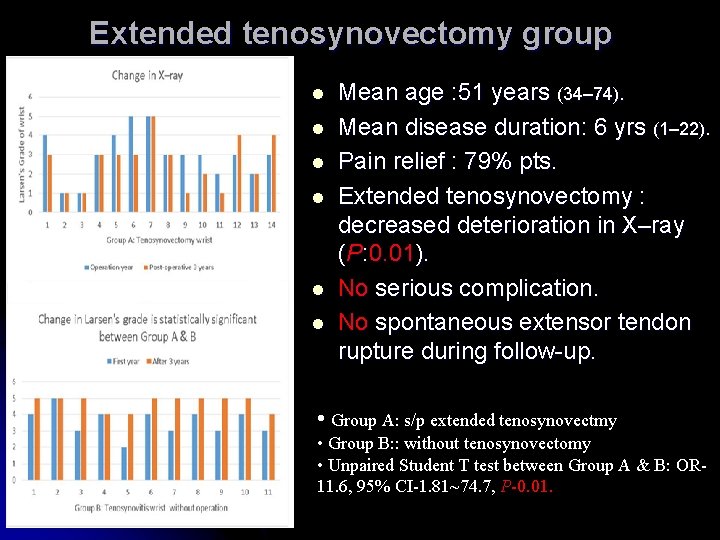
Extended tenosynovectomy group l l l Mean age : 51 years (34– 74). Mean disease duration: 6 yrs (1– 22). Pain relief : 79% pts. Extended tenosynovectomy : decreased deterioration in X–ray (P: 0. 01). No serious complication. No spontaneous extensor tendon rupture during follow-up. • Group A: s/p extended tenosynovectmy • Group B: : without tenosynovectomy • Unpaired Student T test between Group A & B: OR 11. 6, 95% CI-1. 81~74. 7, P-0. 01.
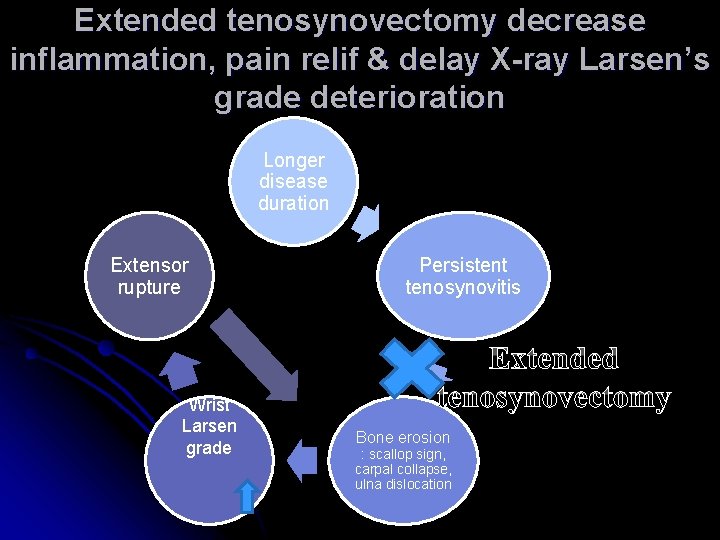
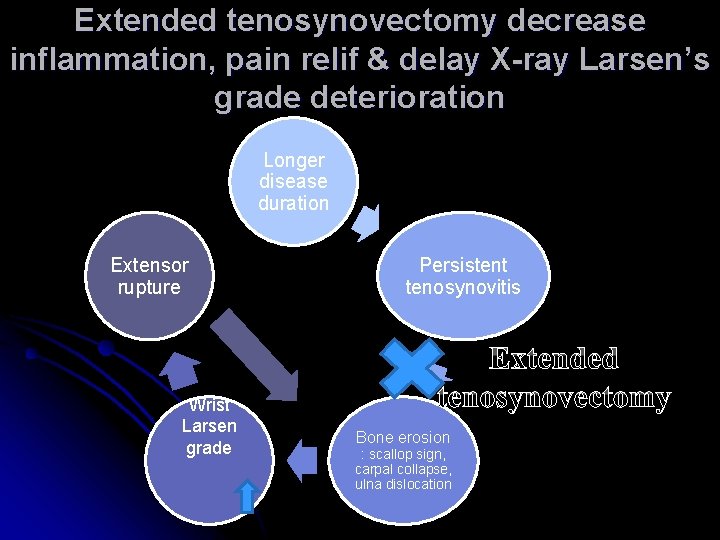
Extended tenosynovectomy decrease inflammation, pain relif & delay X-ray Larsen’s grade deterioration Longer disease duration Extensor rupture Wrist Larsen grade Persistent tenosynovitis Extended tenosynovectomy Bone erosion : scallop sign, carpal collapse, ulna dislocation
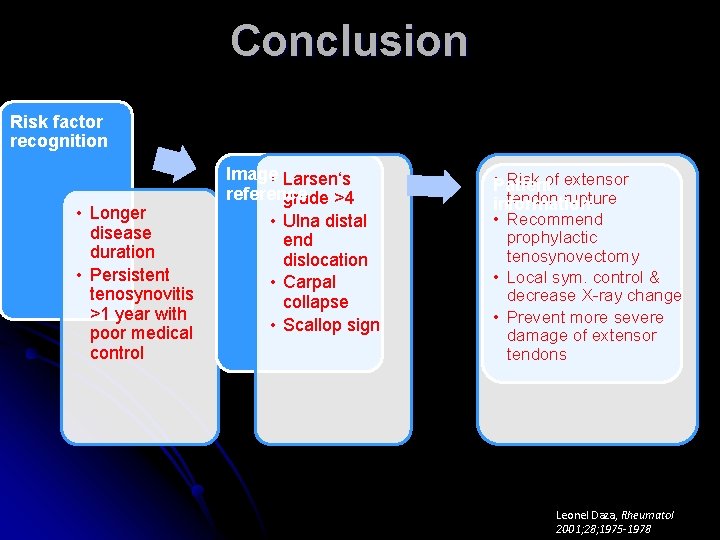
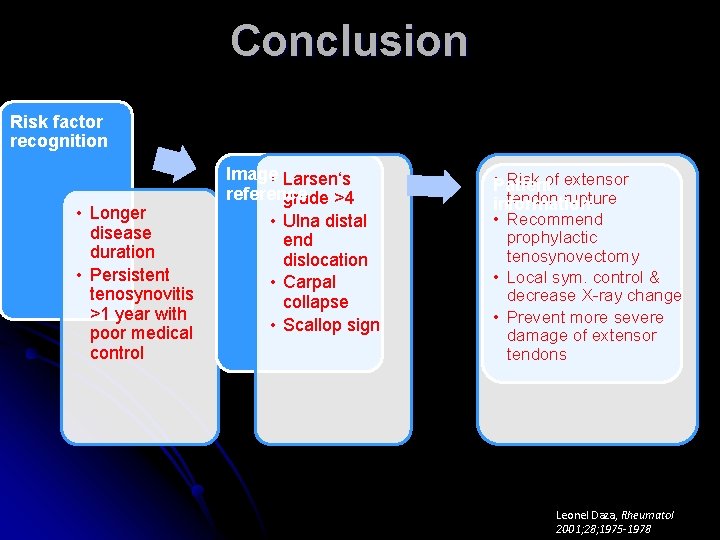
Conclusion Risk factor recognition • Longer disease duration • Persistent tenosynovitis >1 year with poor medical control Image • Larsen‘s reference grade >4 • Ulna distal end dislocation • Carpal collapse • Scallop sign • Risk of extensor Patient tendon rupture information • Recommend prophylactic tenosynovectomy • Local sym. control & decrease X-ray change • Prevent more severe damage of extensor tendons Leonel Daza, Rheumatol 2001; 28; 1975 -1978