Spine Stabilization Concepts J Scott Bainbridge MD Denver

Spine Stabilization Concepts J. Scott Bainbridge, MD Denver Back Pain Specialists www. denverbackpainspecialists. com
History of “Spine Stab” l 1924 Von Lackum proposes that much back pain is caused by instability of spine l 1944 Knutson notes that intervertebral disk degeneration leads to abnormal motion which he terms “segmental instability”
History l 1980 s “Neutral spine” concept introduced l Position of comfort where muscular support reduces stress on painful structures (disc, facet, nerve, etc. ) l 1990 “dynamic stabilization” developed to be more functional – interest increased after Joe Montana returns to football after LB surgery
History l 1996 – current: Back stabilization continues to evolve and become more sport and work specific l Quality research and educational efforts by Hodges, Richardson, Hides, Jull, Comerford and others l Popularization of ball, pool, Pilates, pulley and other exercise systems
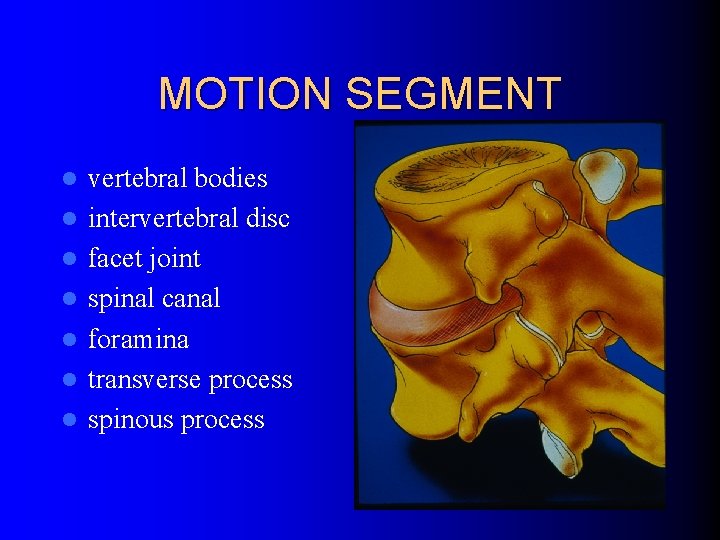
MOTION SEGMENT l l l l vertebral bodies intervertebral disc facet joint spinal canal foramina transverse process spinous process
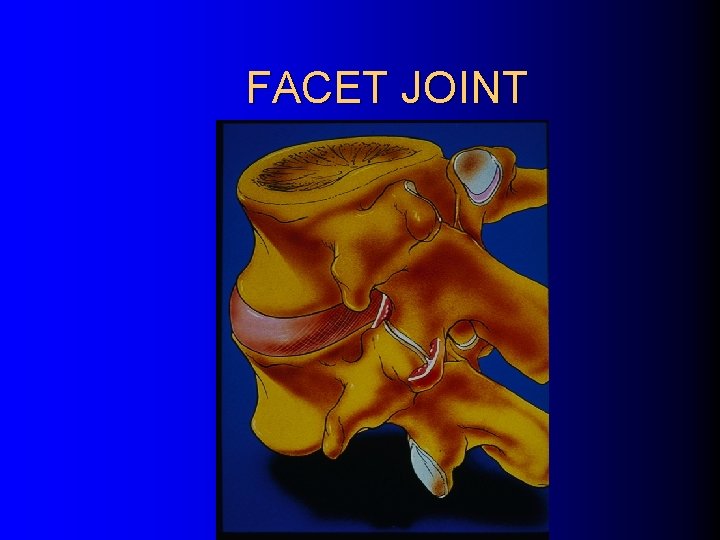
FACET JOINT
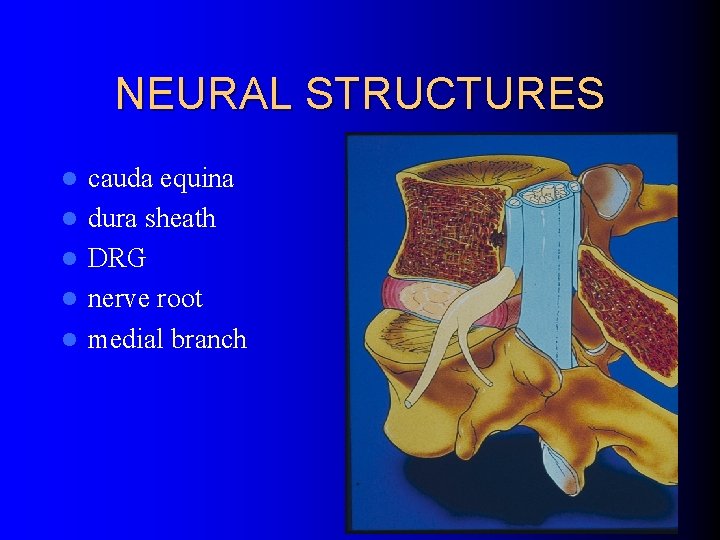
NEURAL STRUCTURES l l l cauda equina dura sheath DRG nerve root medial branch
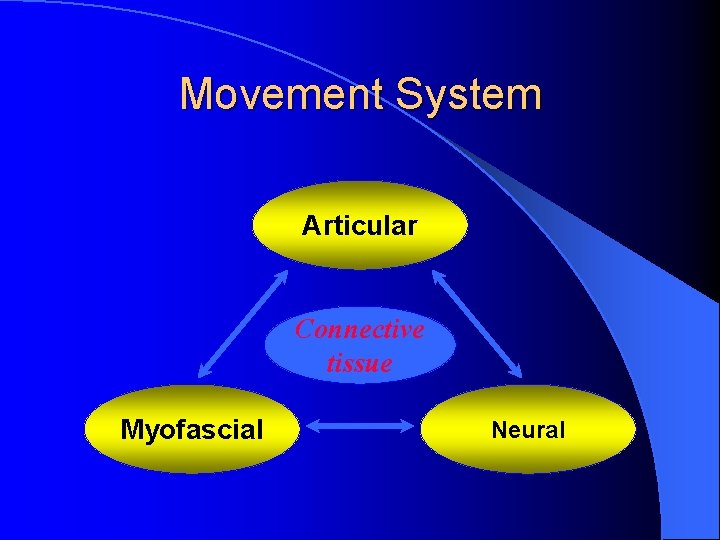
Movement System Articular Connective tissue Myofascial Neural

Pain Mechanisms l Nociceptive – mechanical & inflammatory l Sensitisation – peripheral – central l l autonomic Behavioural / Psycho-social
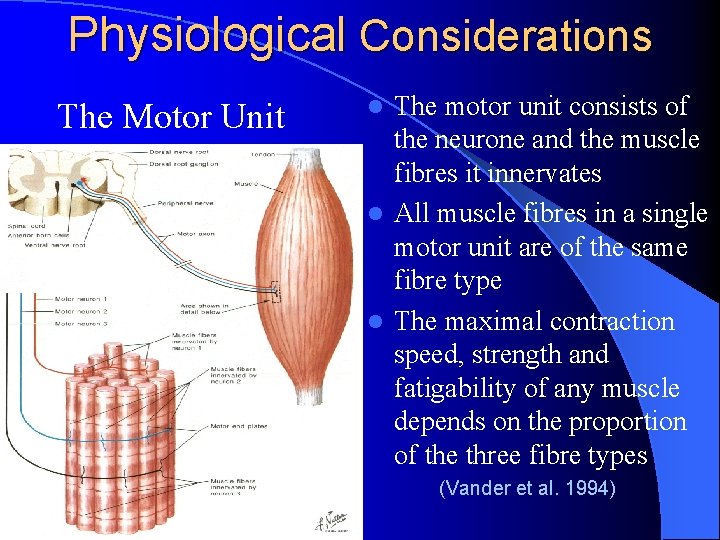
Physiological Considerations The Motor Unit The motor unit consists of the neurone and the muscle fibres it innervates l All muscle fibres in a single motor unit are of the same fibre type l The maximal contraction speed, strength and fatigability of any muscle depends on the proportion of the three fibre types l (Vander et al. 1994)
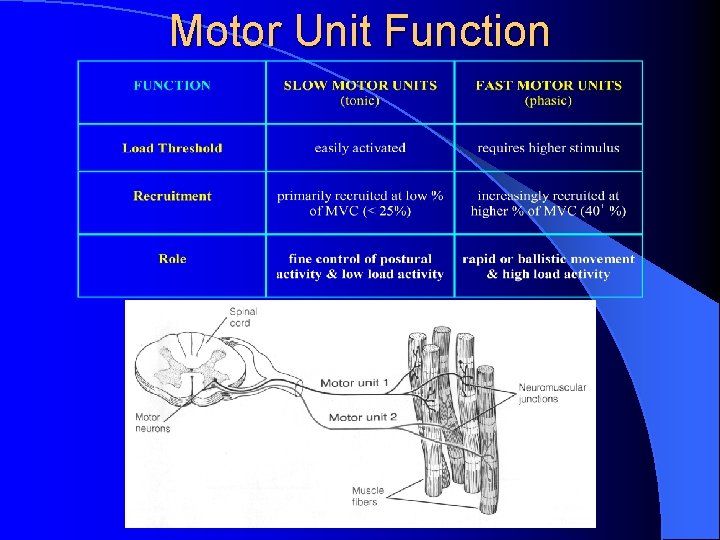
Motor Unit Function
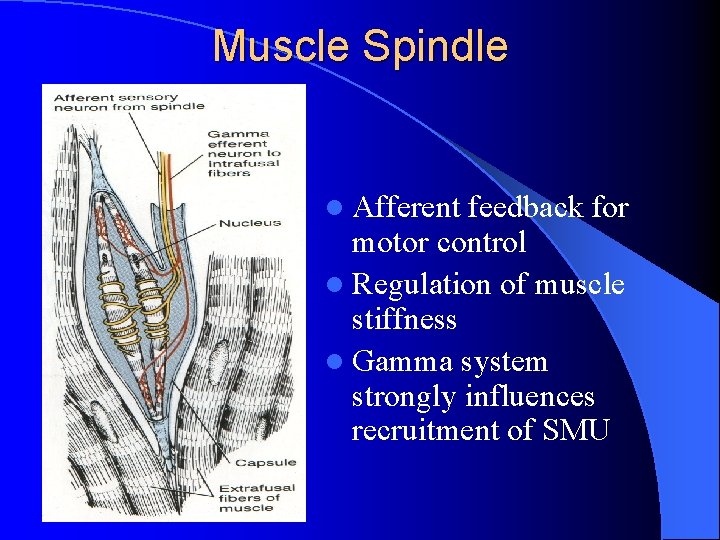
Muscle Spindle l Afferent feedback for motor control l Regulation of muscle stiffness l Gamma system strongly influences recruitment of SMU

Local Stability Muscles Function muscle stiffness to control segmental translation l no or minimal length change in function movements l anticipatory recruitment prior to functional loading provides protective stiffness l activity is continuous and independent of the direction of movement l (review: Comerford & Mottram 2001)
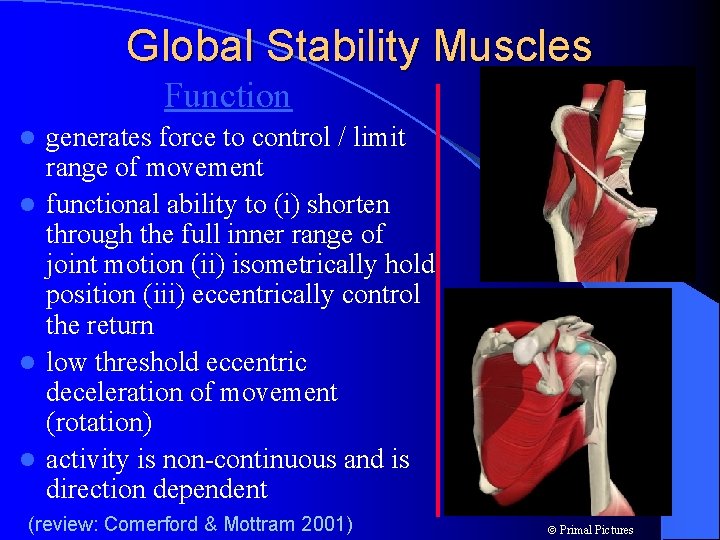
Global Stability Muscles Function generates force to control / limit range of movement l functional ability to (i) shorten through the full inner range of joint motion (ii) isometrically hold position (iii) eccentrically control the return l low threshold eccentric deceleration of movement (rotation) l activity is non-continuous and is direction dependent l (review: Comerford & Mottram 2001) Primal Pictures
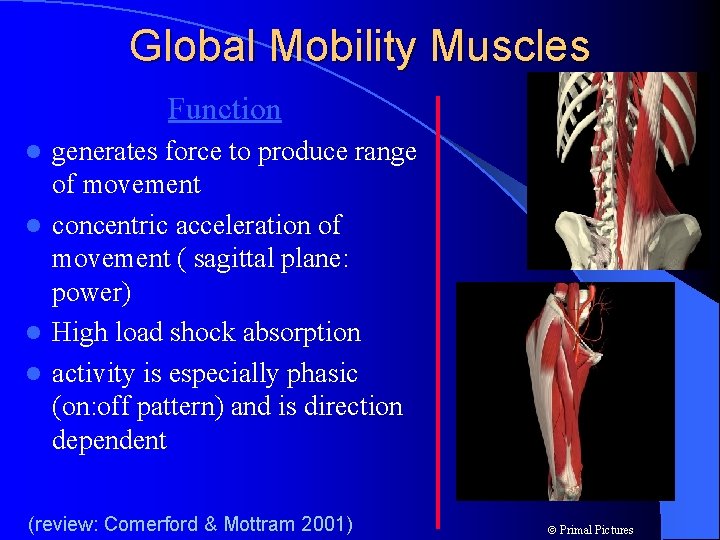
Global Mobility Muscles Function generates force to produce range of movement l concentric acceleration of movement ( sagittal plane: power) l High load shock absorption l activity is especially phasic (on: off pattern) and is direction dependent l (review: Comerford & Mottram 2001) Primal Pictures
l The Local stability segmental control segmental stability of the spine is dependent on recruitment of the deep local stability muscles l The spine will fail if local activity is insufficient even if the global muscles work strongly – 3 % MVC muscle stiffness significantly increases stability l 1 l 25% MVC = optimal stiffness & stability (Cholewicki & Mc. Gill 1996, Crisco & Panjabi 1991, Hoffer & Andreasson 1981)
Local Muscle System Dysfunction There are changes in motor recruitment resulting in a loss of segmental control local inhibition
Dysfunction in Local Stability System l Motor control deficit associated with delayed timing or recruitment deficiency (Hodges & Richardson 1996) l Reacts to pain & pathology with inhibition (Stokes & Young 1984, Hides et al. 1994) l Decrease in muscle stiffness and poor segmental control l Loss of control of joint neutral position
Vastus Medialis Oblique l 60 ml knee effusion significantly inhibits all of the quadriceps l 40 ml effusion (sub clinical) inhibits VMO selectively (Stokes & Young 1984)
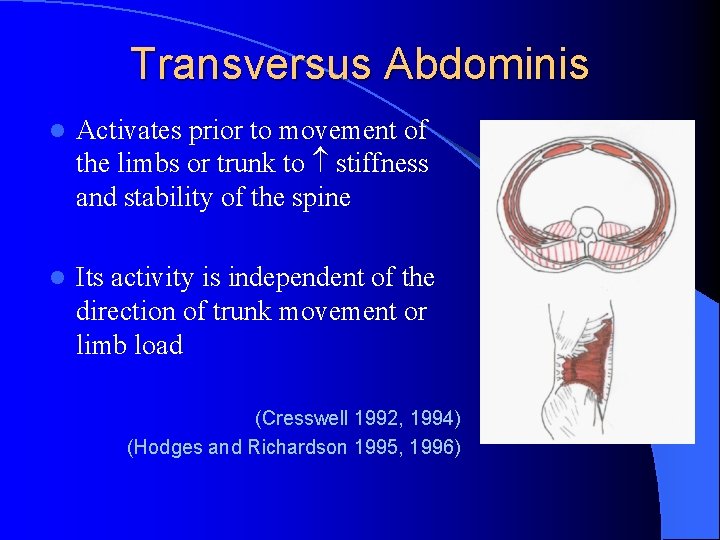
Transversus Abdominis l Activates prior to movement of the limbs or trunk to stiffness and stability of the spine l Its activity is independent of the direction of trunk movement or limb load (Cresswell 1992, 1994) (Hodges and Richardson 1995, 1996)
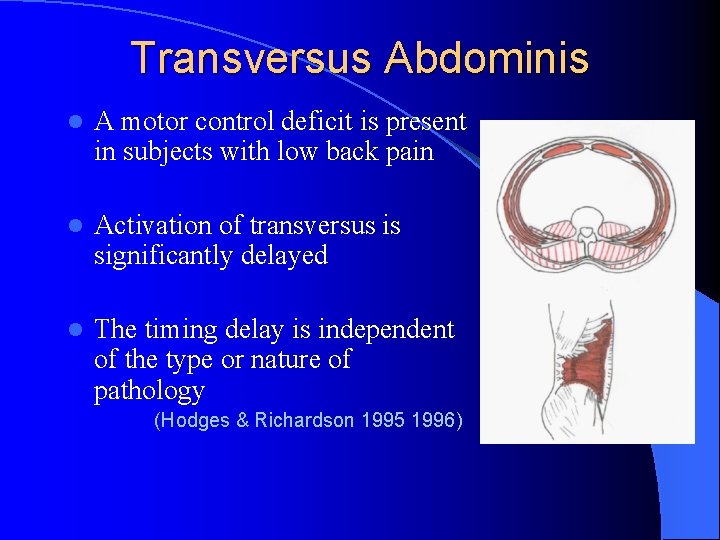
Transversus Abdominis l A motor control deficit is present in subjects with low back pain l Activation of transversus is significantly delayed l The timing delay is independent of the type or nature of pathology (Hodges & Richardson 1995 1996)
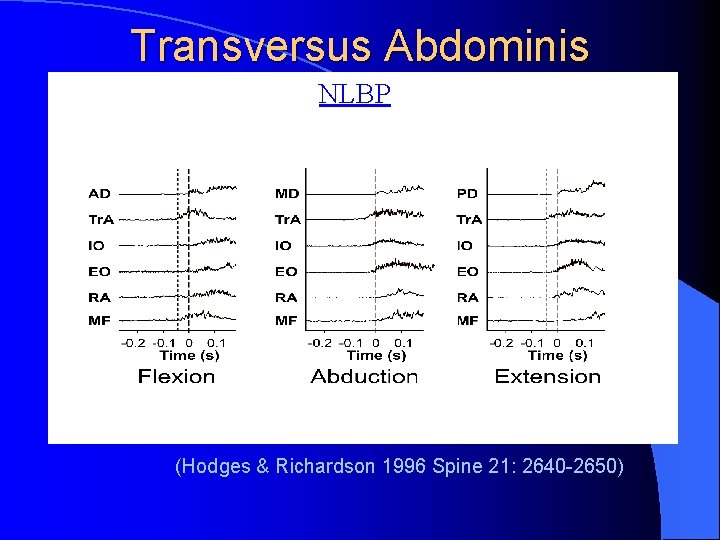
Transversus Abdominis NLBP (Hodges & Richardson 1996 Spine 21: 2640 -2650)
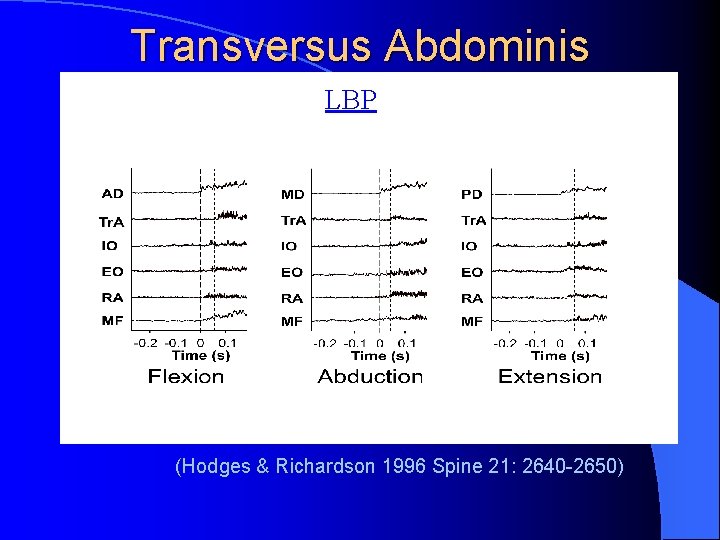
Transversus Abdominis LBP (Hodges & Richardson 1996 Spine 21: 2640 -2650)
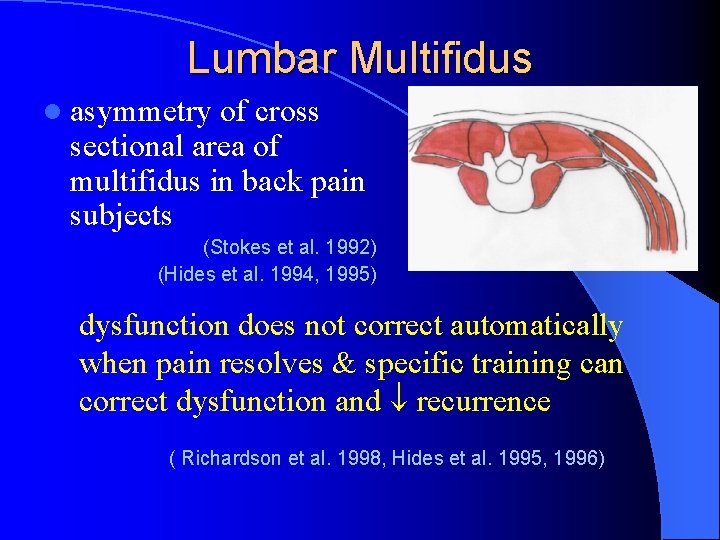
Lumbar Multifidus l asymmetry of cross sectional area of multifidus in back pain subjects (Stokes et al. 1992) (Hides et al. 1994, 1995) dysfunction does not correct automatically when pain resolves & specific training can correct dysfunction and recurrence ( Richardson et al. 1998, Hides et al. 1995, 1996)
Dysfunction in Global Mobility System l Myofascial shortening which limits physiological and / or accessory motion l Overactive recruitment l Reacts low load or low threshold to pain and pathology with spasm
DYSFUNCTION: What comes 1 st ? l Global dysfunction l Local dysfunction does can precede and not precede the contribute to the development of pain & and pathology but pathology rather is due to pain & pathology l Pain & pathology are l Pain & pathology do not a necessary consequence of global not have to be present dysfunction (may be related to distant history)
‘Motor Control’ Stability versus ‘Core’ Stability l Motor control stability = low threshold recruitment of local and global stability muscle system – Well supported by the research literature l Core stability = high threshold recruitment of proximal trunk & girdle muscles
Multifidus Muscle Recovery Is Not Automatic After Acute First Episode LBP l Hides, Richardson, Jull. SPINE 1996: 21 l Control(n=19) medical management/ activity l Specific ex. (n=20) +med manage/ activity l Multifidus ex. 2 x/wk x 4 weeks l Ultrasound image: smaller multifidus on painful side in all at start
Results l Multifidus CSA at most affected vertebral level painful side difference corrected in ex group but not in controls at 4 and 10 weeks. l P<0. 0001 at both times l Pain and Disability scores same in groups (pain and disability resolved at 4 wks in 90%)
Long Term Effects of Stabilizing Exercises for First. Episode LBP l Hides, Jull, Richardson. SPINE 2001: 26 l Control(n=19) medical management/ activity l Specific Ex(n=20) +med manage/ activity l Multifidus ex. 2 x/wk for 4 weeks
Results l 1 year recurrence: control=84%, ex. =30% l P<0. 001 l 3 year recurrence: control=75%, ex. =35% l P<0. 01 (3 controls lost at 3 year)
Therapeutic Exercise for Spinal Segmental Stabilization in LBP l Scientific Basis and Clinical Approach l Richardson, Jull, Hodges, and Hides l Churchill Livingstone 1999
Cervical muscle dysfunction l RCPMaj & RCPMin show atrophy and fatty degeneration in chronic neck pain (Hallgren et al 1994, Mc. Partland et al 1997) neck muscles show slow fast fiber transformation in chronic neck pain l Anterior (Uhlig et al 1995) meningeal stimulation neck and jaw EMG activity l Noxious (Hu et al 1995)
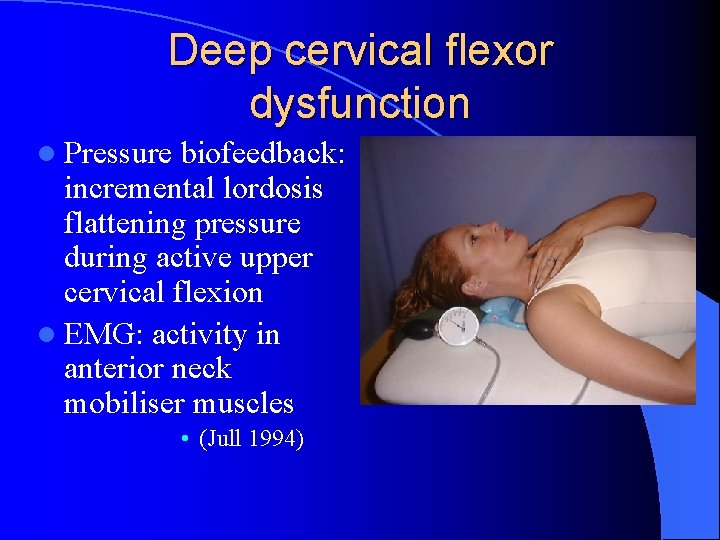
Deep cervical flexor dysfunction l Pressure biofeedback: incremental lordosis flattening pressure during active upper cervical flexion l EMG: activity in anterior neck mobiliser muscles • (Jull 1994)
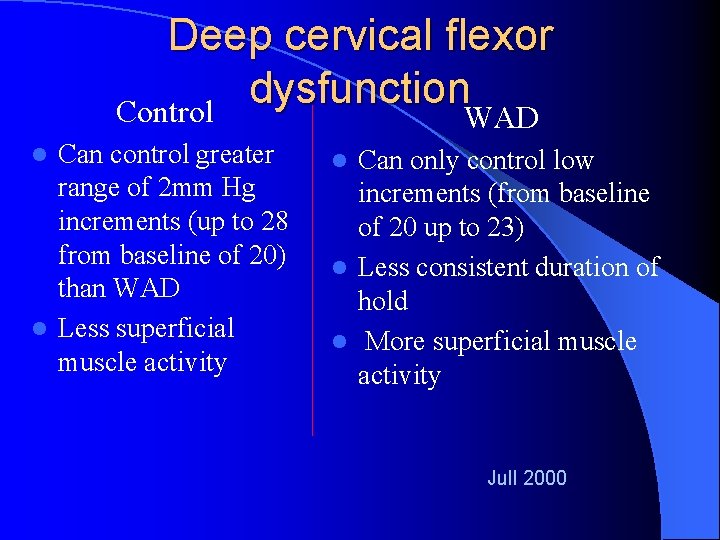
Deep cervical flexor dysfunction Control WAD Can control greater range of 2 mm Hg increments (up to 28 from baseline of 20) than WAD l Less superficial muscle activity l Can only control low increments (from baseline of 20 up to 23) l Less consistent duration of hold l More superficial muscle activity l Jull 2000
Deep cervical flexor dysfunction l identified in different pathological situations – Whiplash Associated Disorder (Jull 2000) – Post-concussional headache (Treleaven et al 1994) – Cervical headache (Watson & Trott 1993, Jull et al 1999) – Mechanical neck pain (Silverman et al 1991, White & Sahrmann 1994, Jull 1998)
A Randomized Controlled Trial of Exercise and Manipulative Therapy for Cervicogenic Headache l Jull, Trott, Potter, et. al. l SPINE: Vol. 27, No. 17, pp. 1835 -1843
Inclusion Criteria l 1 + HA/week for 2 mo. – 10 yr l Cervicogenic headache (not MT or Migraine)
Methods l Randomized: Control, Manual Therapy (Maitland), Exercise (motor control), or Exercise and Manual Therapy l 6 weeks of treatment (8 -12 visits) l Outcome Measures: 7 weeks, 3, 6, and 12 mo. l Change in HA frequency (intensity and duration were secondary measures) l Physical assessments
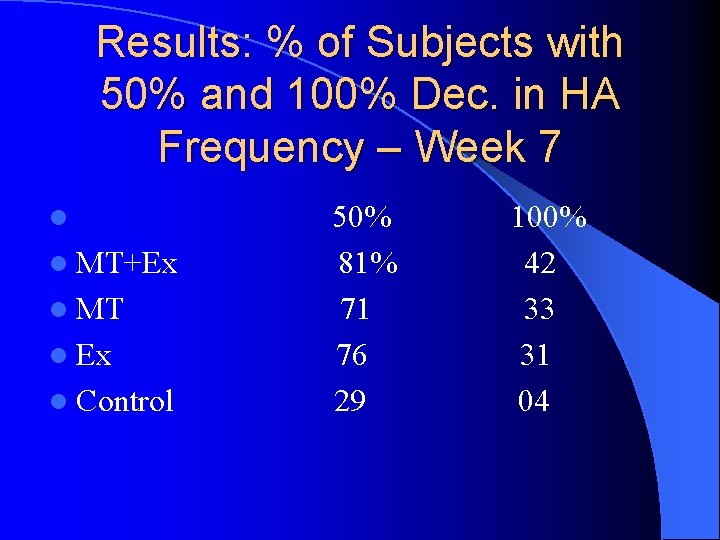
Results: % of Subjects with 50% and 100% Dec. in HA Frequency – Week 7 l l MT+Ex l MT l Ex l Control 50% 81% 71 76 29 100% 42 33 31 04
The meaning of Life ?
The control of stability dysfunction !
- Slides: 42