Spinal Cord Ischemia during TEVAR John J Ricotta
- Slides: 16
Spinal Cord Ischemia during TEVAR John J Ricotta MD FACS Professor of Surgery Georgetown University Chair of Surgery Washington Hospital Center CRT February 2012
John J. Ricotta, MD I have no real or apparent conflicts of interest to report.
Objectives • • To define the Incidence of SCI after TEVAR To Identify Factors associated with SCI To Delineate Strategies to reduce/treat SCI To discuss potential new diagnostic methods for early detection of SCI
SCI after TEVAR • SCI occurs in 5 -20% of Open TAA • SCI occurs in 3 -8% of TEVAR • Incidence of SCI is related to the indication for intervention and the extent of TAA • Results from decreased SC perfusion from inadequate collateral perfusion or I/R injury • Presentation and Prevention of SCI differs somewhat from Open Surgery.
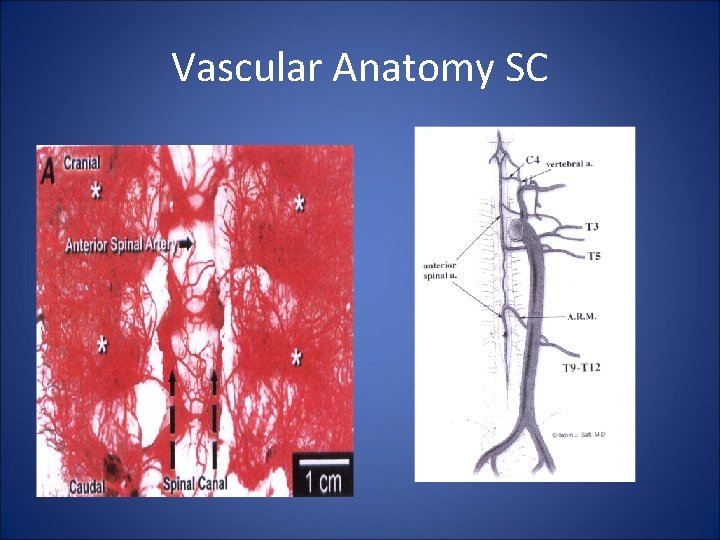
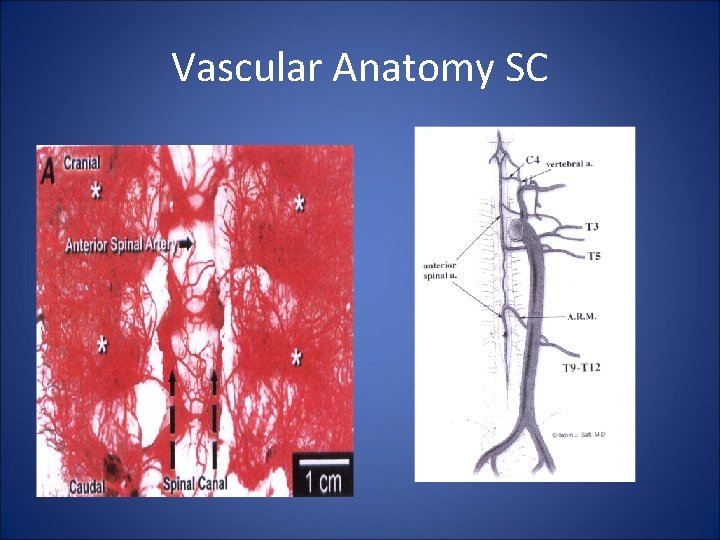
Vascular Anatomy SC
Factors associated with SCI in TEVAR • • • Length of Operation Hypotension Extent of TA coverage Indication for Intervention Female Gender Adequacy Collateral Circulation - Left SCA Coverage - prior AAA repair
Differences in SCI: OPEN vs. EV • OPEN – poor collateral flow during X clamp is a factor, as is prolonged hypotension RX: retrograde perfusion, cooling, CSF drainage, intercostal reimplantation, delayed deficits less common • TEVAR – no X clamp, limited hypotension, reimplantation is impossible RX: limit coverage of important arteries, maintain SPP, delayed deficit is more common than with Open repair
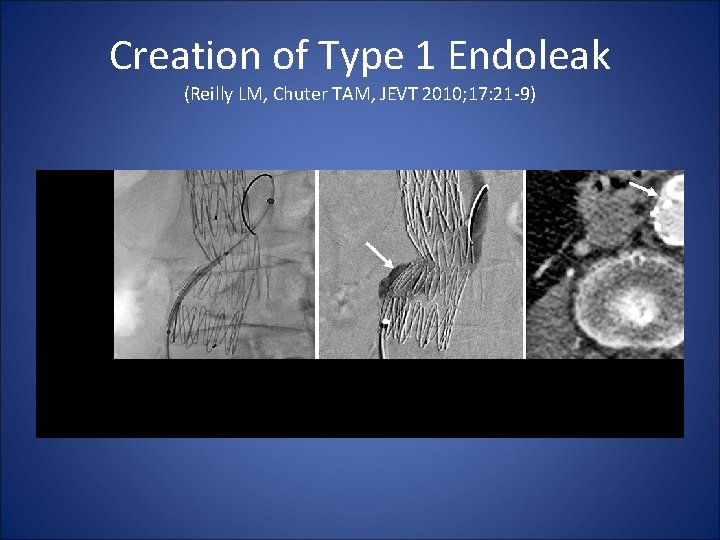
Prevention of SCI • Early Diagnosis is Critical!! • Increase SPPF – reduce CSFP to < 10 mm - increase MAP to >90 mm • Identify and avoid covering important Spinal Arteries - CTA • Create Type I or Type IV endoleak • Treat Reperfusion Injury - naloxone , scavengers
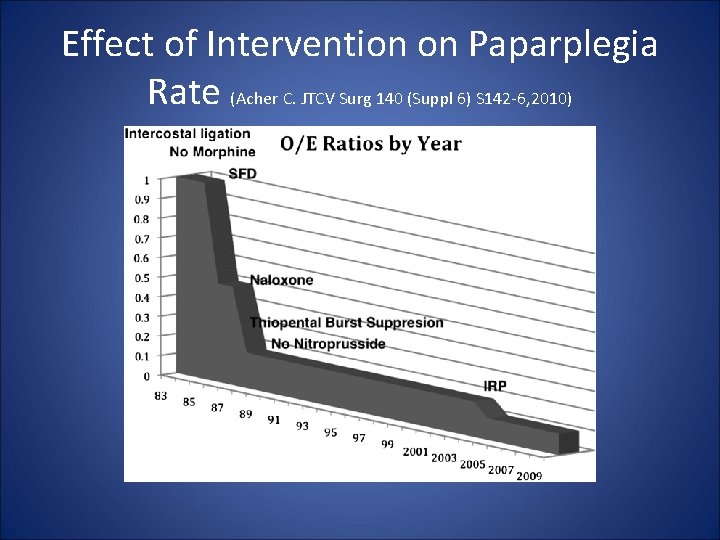
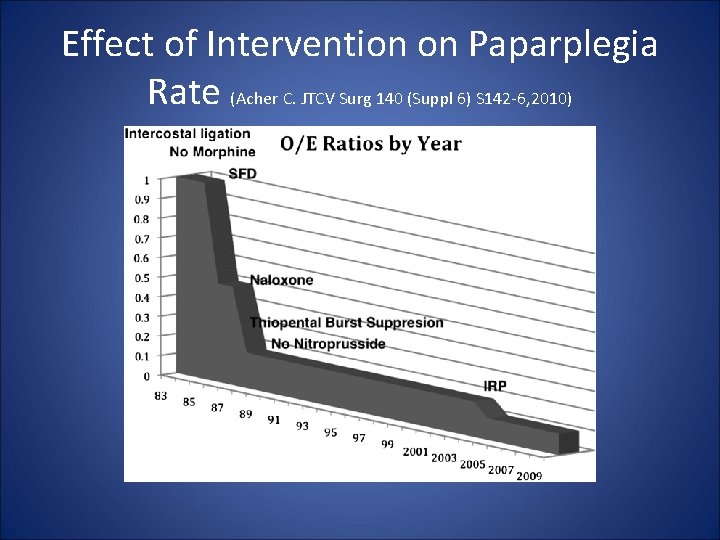
Effect of Intervention on Paparplegia Rate (Acher C. JTCV Surg 140 (Suppl 6) S 142 -6, 2010)
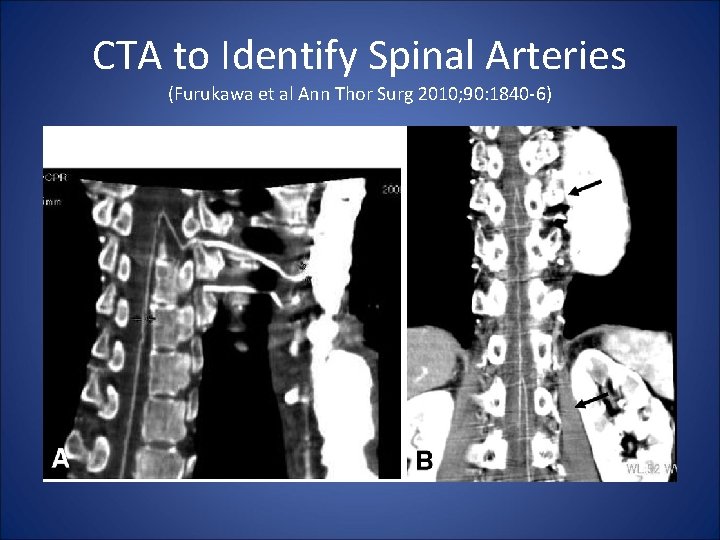
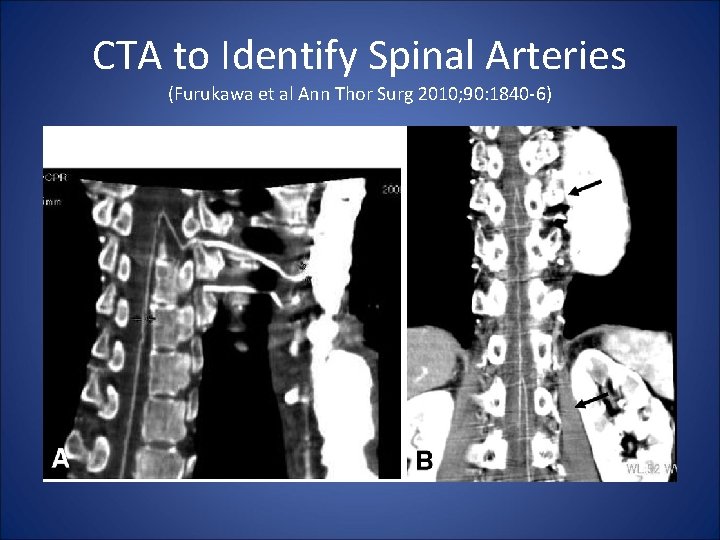
CTA to Identify Spinal Arteries (Furukawa et al Ann Thor Surg 2010; 90: 1840 -6)
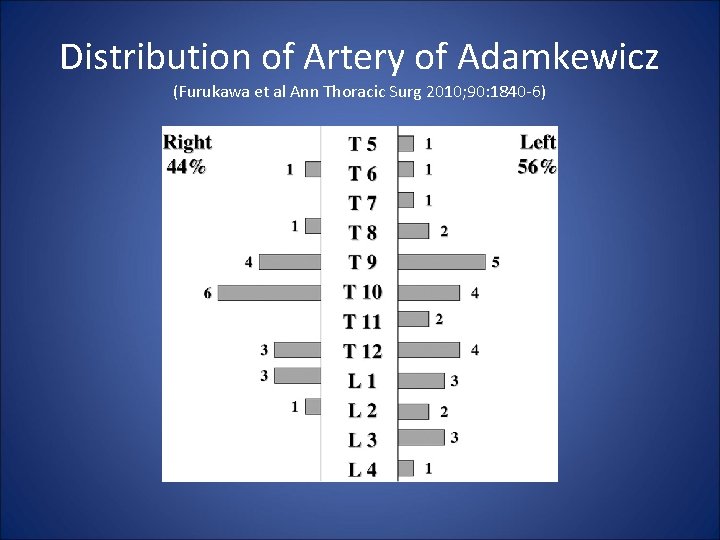
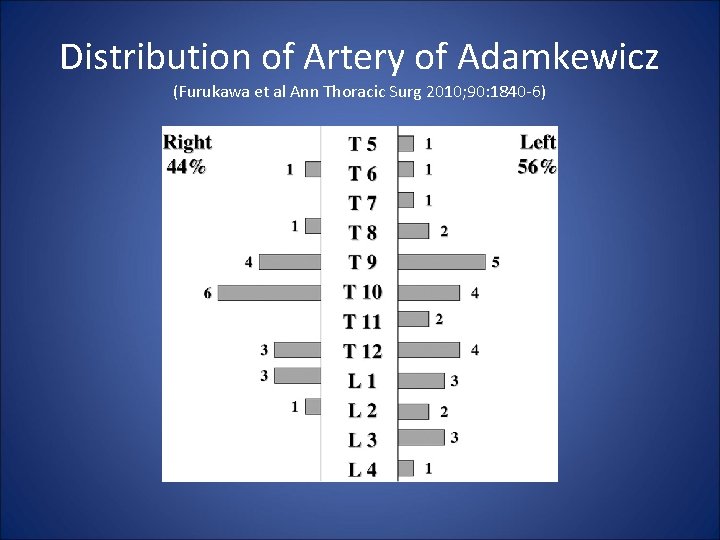
Distribution of Artery of Adamkewicz (Furukawa et al Ann Thoracic Surg 2010; 90: 1840 -6)
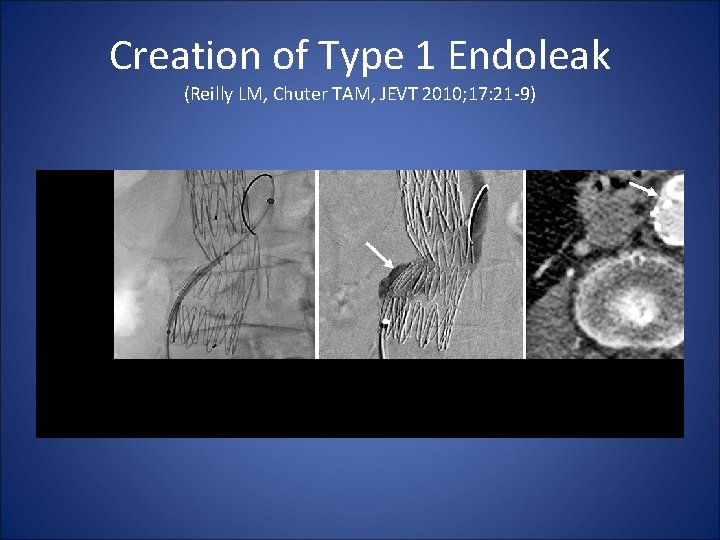
Creation of Type 1 Endoleak (Reilly LM, Chuter TAM, JEVT 2010; 17: 21 -9)
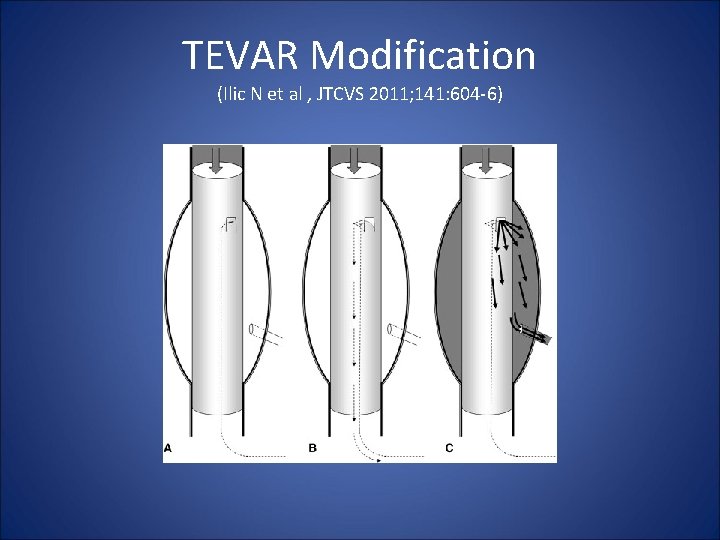
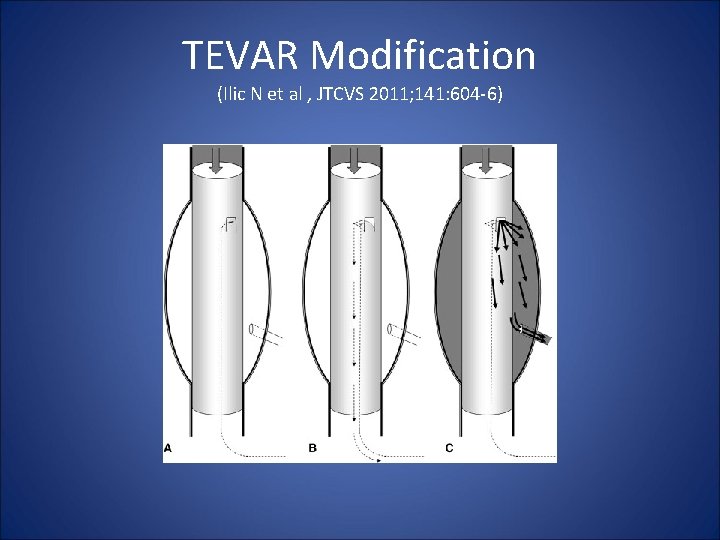
TEVAR Modification (Ilic N et al , JTCVS 2011; 141: 604 -6)
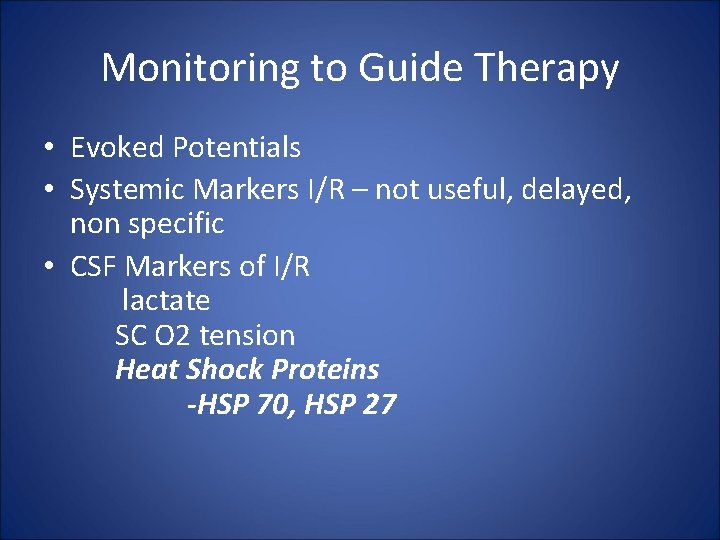
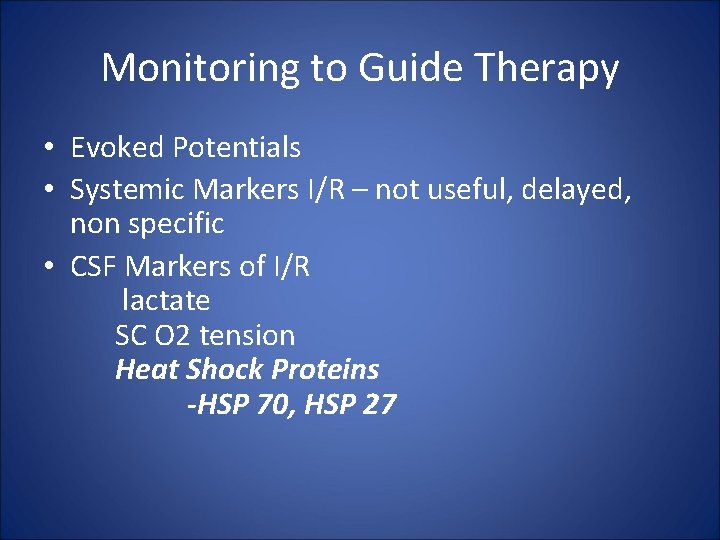
Monitoring to Guide Therapy • Evoked Potentials • Systemic Markers I/R – not useful, delayed, non specific • CSF Markers of I/R lactate SC O 2 tension Heat Shock Proteins -HSP 70, HSP 27
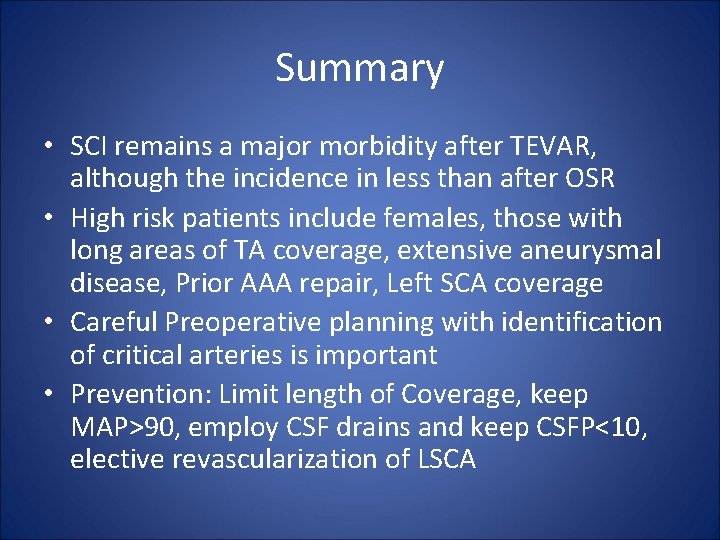
Summary • SCI remains a major morbidity after TEVAR, although the incidence in less than after OSR • High risk patients include females, those with long areas of TA coverage, extensive aneurysmal disease, Prior AAA repair, Left SCA coverage • Careful Preoperative planning with identification of critical arteries is important • Prevention: Limit length of Coverage, keep MAP>90, employ CSF drains and keep CSFP<10, elective revascularization of LSCA
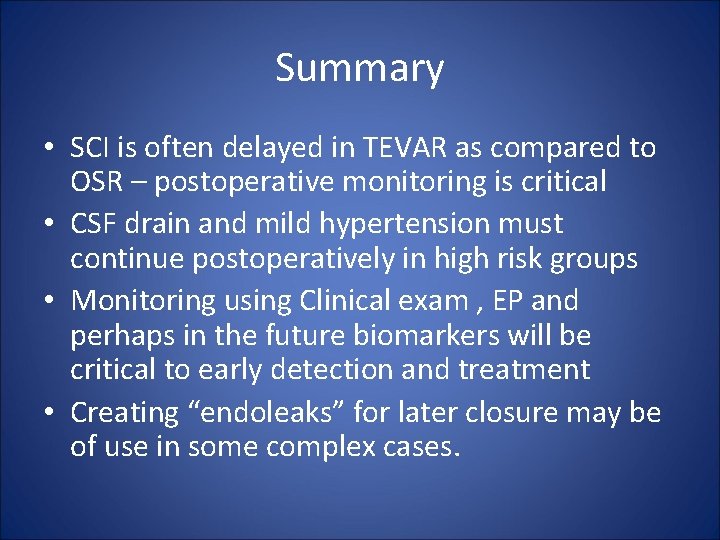
Summary • SCI is often delayed in TEVAR as compared to OSR – postoperative monitoring is critical • CSF drain and mild hypertension must continue postoperatively in high risk groups • Monitoring using Clinical exam , EP and perhaps in the future biomarkers will be critical to early detection and treatment • Creating “endoleaks” for later closure may be of use in some complex cases.