Spinal Cord Injuries in Critical Care How do










- Slides: 29
Spinal Cord Injuries in Critical Care How do you manage?
INTRODUCTION n Almost 50% of all patients with acute traumatic spinal cord injury (SCI) are admitted to a Critical Care Unit prior to their transfer to a specialist SCI Centre. n Therefore, it is not unreasonable to expect critical care practitioners to maintain an appropriate awareness of the specific care needs of SCI patients admitted for critical care.

Do I know what we do? Do I understand why do we do it? Should we do it differently? Should we do it for different reasons?

Critical Care is Rehabilitation is a continuous process, beginning at the moment of injury, and is an integral part of Critical Care. If Critical Care and Rehabilitative Care not combined, people with SCI are subject to serious clinical and economic consequences that could otherwise have been prevented. (Oakes 1990)
THE CHALLENGE n n Acute SCI patients are most at risk of developing preventable complications when admitted outside of SCI Centres. ‘Critical Illness’ is the commonest reason for delayed transfer to a specialist centre. Pre-transfer complications increase length of stay, care costs and long-term quality of life for the SCI person. Many unplanned post-admission transfers of SCI patients to Critical Care avoidable
EARLY COMPLICATIONS n n n Secondary neurological deterioration Pressure ulcers leading to sepsis HCAIs & VAPs Pulmonary oedema (overinfusion) Renal impairment (diuretic use) VTE Gastric bleeding Colorectal dysfunctional morbidity / necrosis Joint contractures Anxiety, Pain, Depression Increased Dependency
CRITICAL CARE ISSUES 2000 n n n Understanding ‘spinal shock’ Clearing the cervical spine The use of cervical collars Steroid therapy Turning/positioning patients Head-tilting for SCI patients Thromboprophylaxis Gastric protection Enteral feeding Bowel management Patient transfer guidelines The SCI-LINK scheme www. spinal. co. uk/on-lineshop (With thanks to the SCI-LINK Critical Care Forum)
Do I know what we do? Do I understand why do we do it?
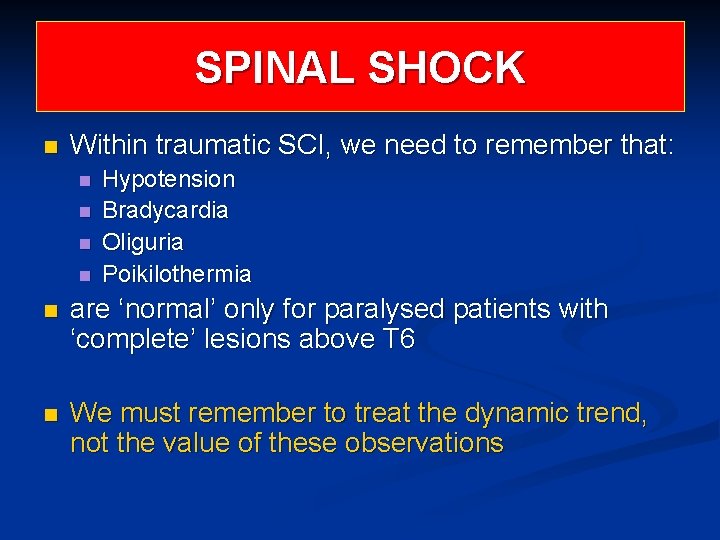
SPINAL SHOCK n Within traumatic SCI, we need to remember that: n n Hypotension Bradycardia Oliguria Poikilothermia n are ‘normal’ only for paralysed patients with ‘complete’ lesions above T 6 n We must remember to treat the dynamic trend, not the value of these observations

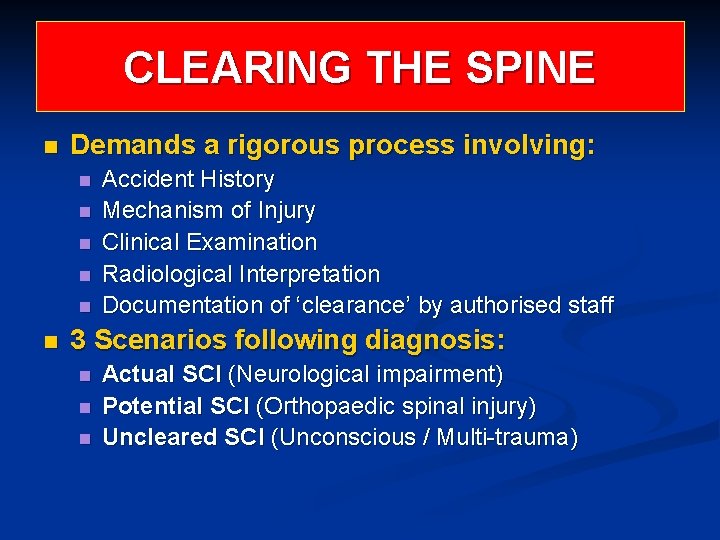
CLEARING THE SPINE n Demands a rigorous process involving: n n n Accident History Mechanism of Injury Clinical Examination Radiological Interpretation Documentation of ‘clearance’ by authorised staff 3 Scenarios following diagnosis: n n n Actual SCI (Neurological impairment) Potential SCI (Orthopaedic spinal injury) Uncleared SCI (Unconscious / Multi-trauma)

CERVICAL COLLARS n Raised ICP: n n Limited evidence to suggest any risk if properly selected, sized and fitted Range of collars available – Aspen model preferred Significant ICP is >20 (Neuro consensus) Pressure sores: n n n Limited incidence if properly selected, sized and fitted Range of collars available – Aspen preferred for extended use May be loosened or removed between turning if appropriate to clinical scenario Person ordering removal must be a) authorised and b) must document decision in patient notes before removal with reference to criteria evidence used to inform clearance.
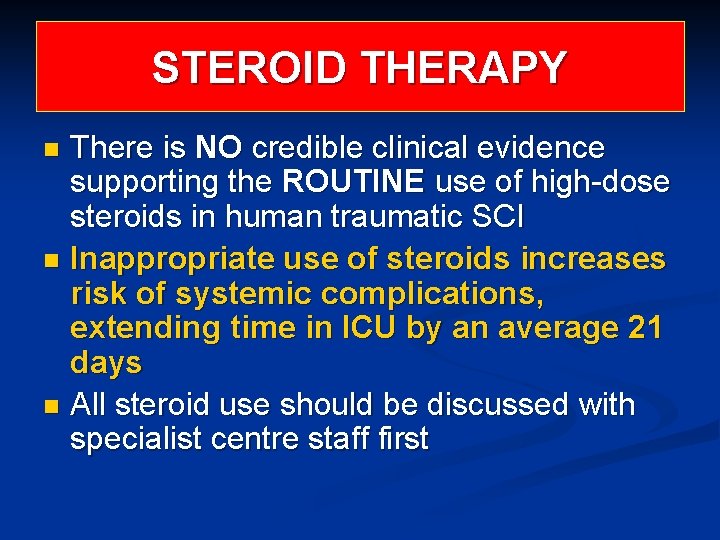
STEROID THERAPY There is NO credible clinical evidence supporting the ROUTINE use of high-dose steroids in human traumatic SCI n Inappropriate use of steroids increases risk of systemic complications, extending time in ICU by an average 21 days n All steroid use should be discussed with specialist centre staff first n
SURGICAL PRINCIPLES (Bedbrook. 1985) “Surgical judgement or surgical balance is of much greater importance than surgical technique. The advantages or disadvantages of any particular method of acute management of spinal injuries must be considered before a particular programme of management is laid down to suit the individual, as well as the individual’s fractures”. This implies ‘informed consent’ must be satisfied before operation including notation of treatment options offered to patient / next-of-kin

AVOIDABLE ADMISSIONS A Critical Care Tale of Two Hospitals ST ELSEWHERE’S: ST ALLSORT’S: n Admits 13 SCI patients n Admits 11 SCI patients n 11 are operated on within 24 hours of admission and all before referral to SCI Centre n 6 were operated on 2 -14 days after admission and all after prior discussion with SCI Centre n 3 patients already in ITU but 3 HDU and 5 ward patients required unplanned ITU admission n 2 patients were already in ITU and 2 ward-based patients underwent pre-planned 48 hour admission to ITU n These 11 patients totalled 379 ITU bed nights between them n These 4 patients totalled 70 bed nights between them

TURNING AND HANDLING n n n 2 -4 hourly turning is recommended to prevent fluid stasis as well as pressure relief Manual turning is staff intensive but mechanical turning beds are available Never use dynamic pressure relieving mattresses for acute SCI patients Spinal logrolling should be familiar to CCU staff Failure to implement regular turning increases risk of multiple complications of bedrest Flat-lifter scoop stretchers are also available for transfers
REALITY BITES n Despite requests from SCI Centre team, a 22 year-old male paraplegic patient was not turned during first 10 days of his ward admission to hospital for the following reasons quoted in notes: n n ‘lack of staff’ ‘fear of further compromising spinal cord’ ‘unnecessary because he is now on a dynamic pressure relieving mattress’ He subsequently developed hydrostatic pneumonia (requiring ITU admission intubation and ventilation for 21 days) and 3 x Grade 3 pressure ulcers requiring surgical repair (extending his stay in the SCI Centre by 90 days).
HEAD-TILTING All requests to raise patient’s head / tilt bed should be referred to SCI Centre staff n Refer to ICS ventilation ‘care bundle’ n Preserving brain takes priority over protecting spinal cord n Start with 10 -15 degrees, increase slowly n Do not exceed 30 degrees head-up n Keep collar in situ if possible n
THROMBOPROPHYLAXIS Anticoagulation and full-length TED / PCD supported by BD physiotherapy exercise of paralysed limbs must commence within 24 hours of injury – exceptions must be documented with rationale n Thromboembolism is silent but usually preceded by pyrexia, SVT or ‘bizarre’ behaviour n
GASTRIC PROTECTION 10% of post-injury SCI deaths due to gastric bleeding n Chemical prophylaxis must commence within 24 hours of admission n And continue until transfer to SCI Centre n Question: How do you diagnose ‘A cute abdomen’ in a SCI patient?

ENTERAL FEEDING n n n All SCI patients present with loss of peristalsis as part of ‘spinal shock’ Usually lasts 2 -5 days Keep patient ‘Nil enterally’ for first 48 hours, then review (British Dietetic Association 2007) Give TPN during this time if nutritionally compromised Paralytic ileus leads to splinting of diaphragm, gastric reflux and necrotising bowel distension, usually requiring surgical intervention
BOWEL MANAGEMENT n n n All SCI patients present with neurogenic bowel dysfunction Most require digital bowel procedures Digital removal of faeces is a safe and legitimate technique for a patient with a ‘flaccid’ bowel Bowel distension in patients with lesions above T 6 can trigger ‘autonomic dysreflexia’ Failure to provide appropriate bowel care may constitute clinical negligence (RCN/NPSA/ACA)
New MASCIP Publication www. mascip. co. uk
PATIENT TRANSFER n n National ‘Training for Transfer’ programme includes patient with actual or potential SCI Must liaise with SCI Centre: n n n n ‘Fit for Transfer’ criteria must be met Appropriate mode of transport Provide TOD and ETA Spinal protection as agreed Provision of an ‘informed’ escort ALL notes, images and test results Inform centre of any change in condition en route
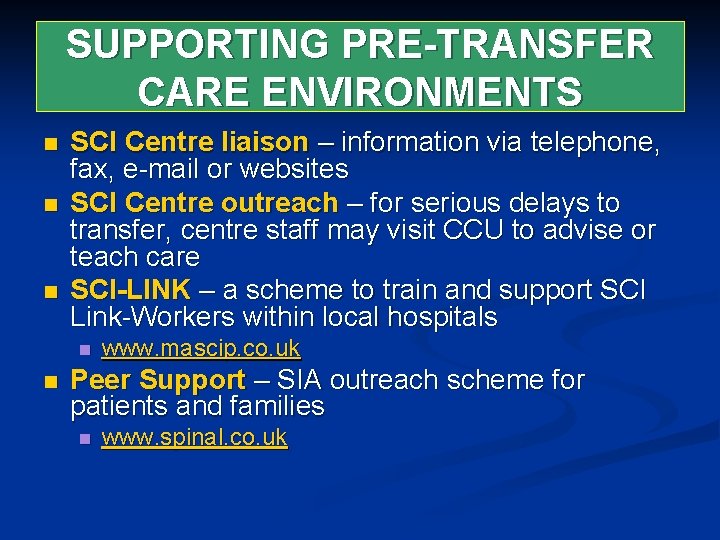
SUPPORTING PRE-TRANSFER CARE ENVIRONMENTS n n n SCI Centre liaison – information via telephone, fax, e-mail or websites SCI Centre outreach – for serious delays to transfer, centre staff may visit CCU to advise or teach care SCI-LINK – a scheme to train and support SCI Link-Workers within local hospitals n n www. mascip. co. uk Peer Support – SIA outreach scheme for patients and families n www. spinal. co. uk

CRITICAL CARE NEEDS n Common practices between CCUs n n Informed underpinning knowledge n n (Why we do what we do – in-house education) Core skills and competencies n n (The SCI Integrated Care Pathway) SCI Link-Workers / Skills for Health Confidence in our own abilities n Auditable performance standards
Do I know what we do? Do I now understand why we do it? Should we do it differently? Should we do it for different reasons? Do we have a care pathway?

What if I don’t work in Critical Care? Do I understand what we do? Should we do it differently? Should we do it for different reasons? Do we have a care pathway for our clinical area?

www. mascip. co. uk www. spinal. co. uk www. bascis. pwp. blueyonder. co. uk www. spinal-research. org
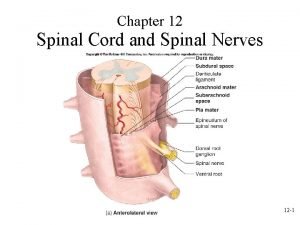
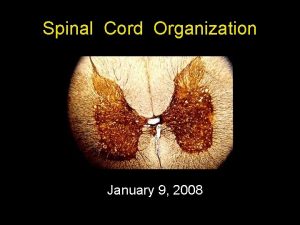
 Innervations of the brachial and lumbar enlargements
Innervations of the brachial and lumbar enlargements Exercise 15 spinal cord and spinal nerves
Exercise 15 spinal cord and spinal nerves Posterior root of spinal cord
Posterior root of spinal cord Figure 13-2 spinal nerves
Figure 13-2 spinal nerves Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Semicritical
Semicritical Spinal arteries
Spinal arteries Spinal cord muscles
Spinal cord muscles Celula pigmentaria
Celula pigmentaria Boston scientific spinal cord stimulator
Boston scientific spinal cord stimulator Axillary nerve innervation
Axillary nerve innervation Subthalamus
Subthalamus Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Spinal cord anatomy
Spinal cord anatomy Spinal cord denticulate ligament
Spinal cord denticulate ligament Spinal cord parts
Spinal cord parts Stretch reflex
Stretch reflex Espina dorsal
Espina dorsal Crossed extensor reflex
Crossed extensor reflex Site of somatic motor neuron cell bodies
Site of somatic motor neuron cell bodies Subthalamus
Subthalamus Pain pathway spinal cord
Pain pathway spinal cord Functions of cerebellum
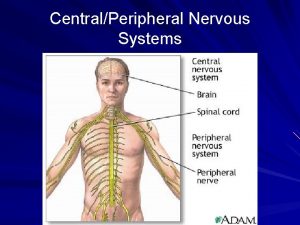
Functions of cerebellum Spinal cord and brain
Spinal cord and brain Somi brace
Somi brace Trachea and spinal cord
Trachea and spinal cord Perineurium
Perineurium Spinal nerves diagram
Spinal nerves diagram Spinal cord nerve anatomy
Spinal cord nerve anatomy Spinal cord
Spinal cord