SPINAL CORD DISABILITIES By Misty Hooper Overview Definition

SPINAL CORD DISABILITIES By Misty Hooper
Overview Definition Epidemiology Clinical Aspects Treatment Functional Assessment Effect on Exercise Effect of Medication on Exercise Testing Exercise Prescription Summary and Conclusion
What are Spinal Cord Disabilities? Spinal Cord Disabilities are damage or trauma to the spinal cord that results in a loss or impaired function causing reduced mobility or feeling.
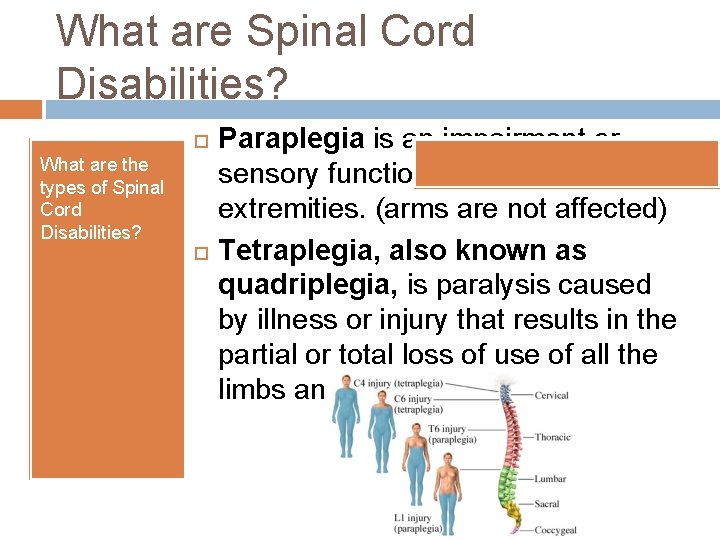
What are Spinal Cord Disabilities? What are the types of Spinal Cord Disabilities? Paraplegia is an impairment or sensory function of the lower extremities. (arms are not affected) Tetraplegia, also known as quadriplegia, is paralysis caused by illness or injury that results in the partial or total loss of use of all the limbs and torso.
Epidemiology: Incidence & Prevalence According to the CDC, about 200, 000 people are currently living with Spinal Cord Injuries in the United States. 12, 000 to 20, 000 new cases are estimated to occur annually. A regional study conducted in 2005 found that most new Spinal Cord Injury cases occur in persons younger than 30 years old, and an estimated 50 -70% occur in those aged 15 -35 years old.
Epidemiology: Incidence & Prevalence Causes of Spinal Cord Injuries: Motor Vehicle Accidents-46% According to the CDC, use of a seatbelt can reduce the odds of a spinal cord injury by 60%. Use of a seatbelt and airbag combined can reduce the odds of injury by 80%. Falls-22% Violence-16% Sports-12%
Clinical Aspects Symptoms of spinal cord injury after an accident may include: Extreme back pain or pressure in the neck, head or back Weakness, incoordination or paralysis in any part of the body Numbness, tingling or loss of sensation in hands, fingers, feet or toes Loss of bladder or bowel control Difficulty with balance or walking Impaired breathing after injury Oddly positioned or twisted neck or back
Clinical Aspects Laboratory Testing, Diagnosis & Evaluation Conducted by a healthcare professional � Clinic, � lab, hospital, doctor’s office Orthopedic Examination � Evaluation of Airway, Breathing, Circulation � Level of consciousness Inspection beginning from the top of the head until the bottom of the toes. � Palpation of the spine from the skull to the coccyx for areas of localized tenderness.
Clinical Aspects Laboratory Testing, Diagnosis & Evaluation Neurological Evaluation Neurological status must be evaluated until the spinal shock period is absent which occurs 48 hours after injury. Testing includes sensation of pain and or light touch, strength of upper and lower extremity, deep tendon reflexes, plantar reflexes, pathologic reflexes.
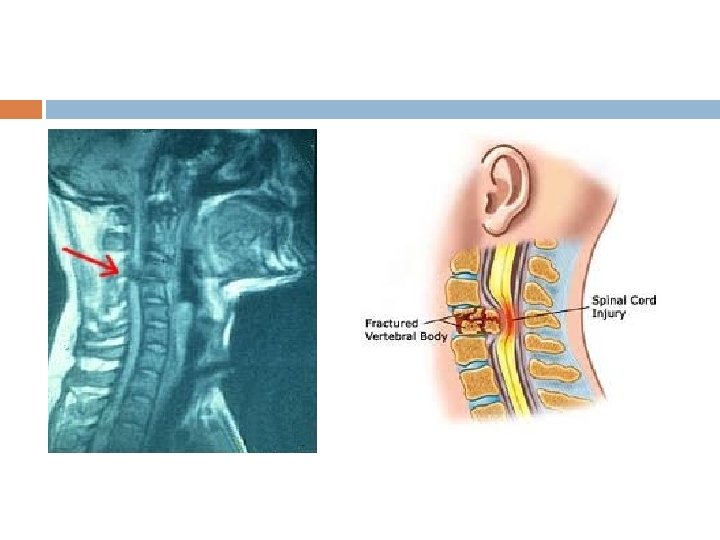
Clinical Aspects Laboratory Testing, Diagnosis & Evaluation Emergency Diagnostic Tests X-Rays X-rays reveal vertebral problems, tumors, fractures, or degenerative changes in the spine. Computerized Tomography (CT) scan Uses computers to form a series of cross-sectional images that can define bone, disk, and other problems. Magnetic Resonance Imaging (MRI) Helpful for looking at the spinal cord and identifying herniated disks, blood clots or other masses that may be compressing the spinal cord. Myelography A special dye is injected into your spinal cord to look for herniated disks or other lesions.
Clinical Aspects Complication s Severity of Spinal Cord Injuries can lead to complications or can result it: Decubitus ulcers Osteoporosis Fractures Restriction in respiratory function which can lead to pneumonia, atelectasis (collapse of a lung), aspiration Spasticity Autonomic dysreflexia (at or above T 6 level)
Treatment: Quadriplegia and Paraplegia Trauma Care • Immobilization to prevent further injury • Stabilization of heart rate, blood pressure, and condition • Possible intubation to assist breathing • Imaging tests to determine extent of injury • • Surgery may be needed to relieve pressure on the spine from bone fragments or foreign objects. No form of surgery can repair the damaged nerves of the spinal cord. Nerve damage caused by initial injury has a tendency to spread. Reasons for the spreading are not completely understood but it is related to spreading inflammation as blood circulation decreases and blood pressure drops. Inflammation causes nerve cells not directly in the injured area to die. A powerful corticosteroid can help prevent the spread of this damage if given within eight hours of the original injury.
Treatment: Quadriplegia Rehabilitation Consists of training to learn to deal with new limitations Functional neuromuscular stimulation (FNS) stimulates the intact peripheral nerves so that the paralyzed muscles will contract. This allows patients to ride a stationary bicycle to improve muscle and function to prevent the muscles from atrophying. Tendon transfer is a surgery that transfers a nonessential muscle with nerve function to the shoulder or arm to help restore function. Implantable FNS system to help regain use of hands. The shoulder’s position controls the stimulation to the hand’s nerves, allowing the individual to pick up objects at will.
Functional Assessment Functional assessment is a method for describing abilities and activities in order to measure an individual’s use of the variety of skills included in performing the tasks necessary to daily living, vocational pursuits, social interaction, leisure activities, and other required behaviors.
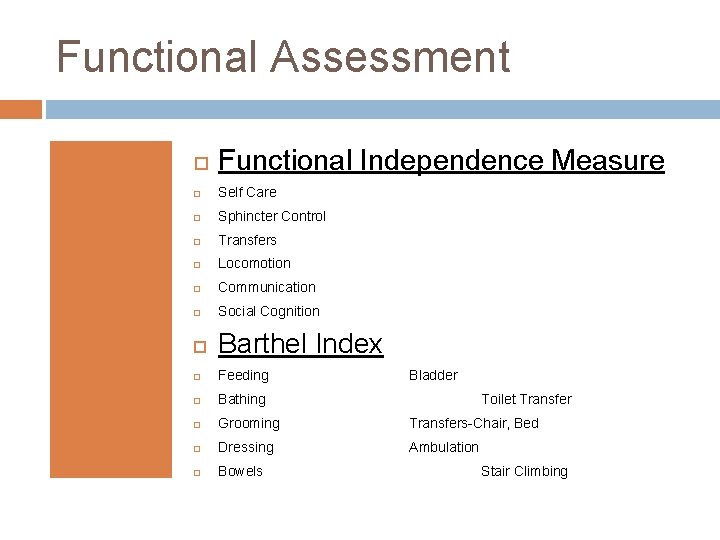
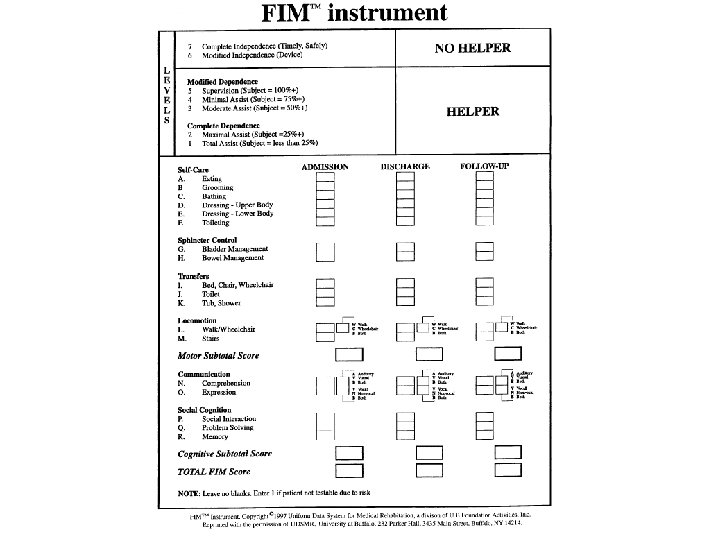
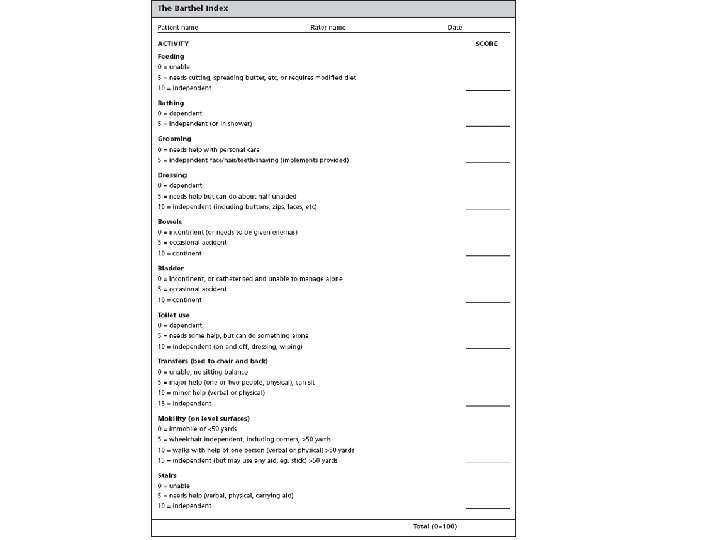
Functional Assessment Functional Independence Measure Self Care Sphincter Control Transfers Locomotion Communication Social Cognition Barthel Index Feeding Bathing Grooming Transfers-Chair, Bed Dressing Ambulation Bowels Bladder Toilet Transfer Stair Climbing
Functional Assessment Funcional Status Index Gross Mobility Hand activities Personal care Home chores Social/Role Activities
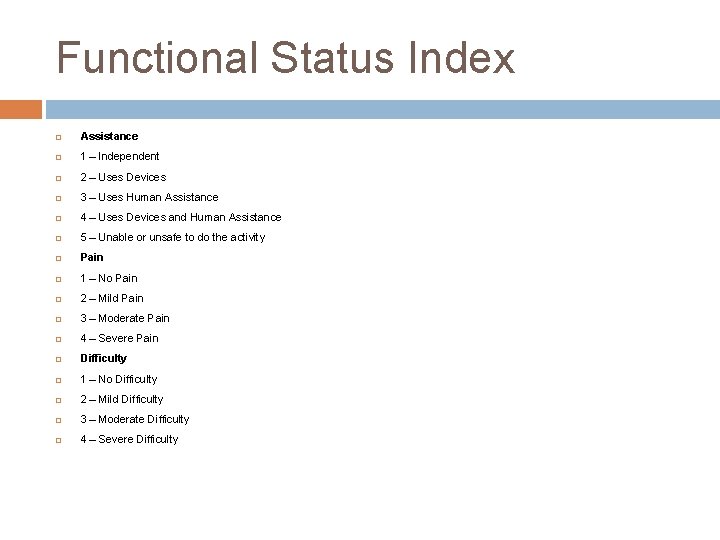
Functional Status Index Assistance 1 – Independent 2 – Uses Devices 3 – Uses Human Assistance 4 – Uses Devices and Human Assistance 5 – Unable or unsafe to do the activity Pain 1 – No Pain 2 – Mild Pain 3 – Moderate Pain 4 – Severe Pain Difficulty 1 – No Difficulty 2 – Mild Difficulty 3 – Moderate Difficulty 4 – Severe Difficulty
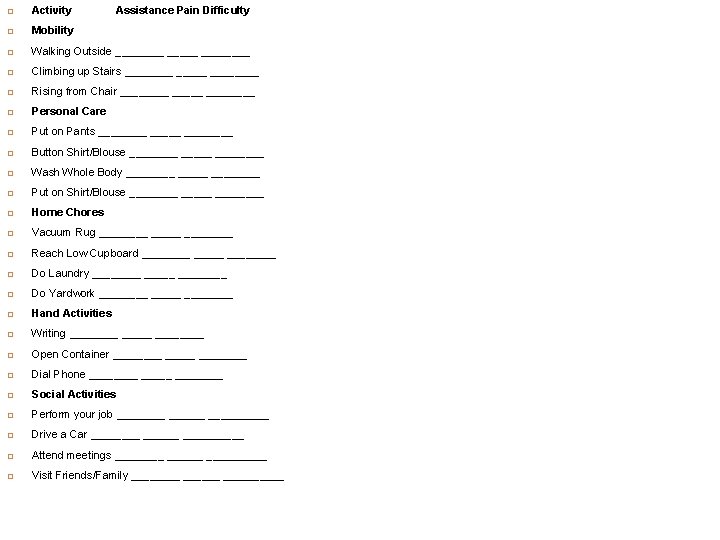
Activity Assistance Pain Difficulty Mobility Walking Outside ________ Climbing up Stairs ________ Rising from Chair ________ Personal Care Put on Pants ________ Button Shirt/Blouse ________ Wash Whole Body ________ Put on Shirt/Blouse ________ Home Chores Vacuum Rug ________ Reach Low Cupboard ________ Do Laundry ________ Do Yardwork ________ Hand Activities Writing ________ Open Container ________ Dial Phone ________ Social Activities Perform your job __________ Drive a Car __________ Attend meetings __________ Visit Friends/Family __________
Effects of Spinal Cord Injury on Exercise In paraplegia, the upper body must be used for all voluntary activities of daily living and exercise. Methods such as arm cranking, ambulation with orthotic devices and crutches, and wheelchair propulsion are used. Smaller upper body mass restricts peak values of power output, oxygen consumption, and cardiac output to one-half of the normal values for those without spinal cord injury.
Effects of Spinal Cord Injury on Exercise In tetraplegia, upper body power output, oxygen consumption, and cardiac output are reduced to onehalf to one-third of the levels seen in individuals with paraplegia. Strenuous exercise can produce dizziness, nausea, and other symptoms due to exercise hypotension. Peak heart rates typically do not exceed 120 beats per minute.
Paralyzed Utah County woman to race in Boston Marathon http: //www. ksl. com/? sid=14917457 &nid=148
Effects of Medication on Exercise • Ditropan (oxybutynin chloride) • • Dibenzyline (phenoxybenzamine hydrochloride) • • Induces hypotension Management of neuropathic bladder Alcohol, Diuretics • Diuresis
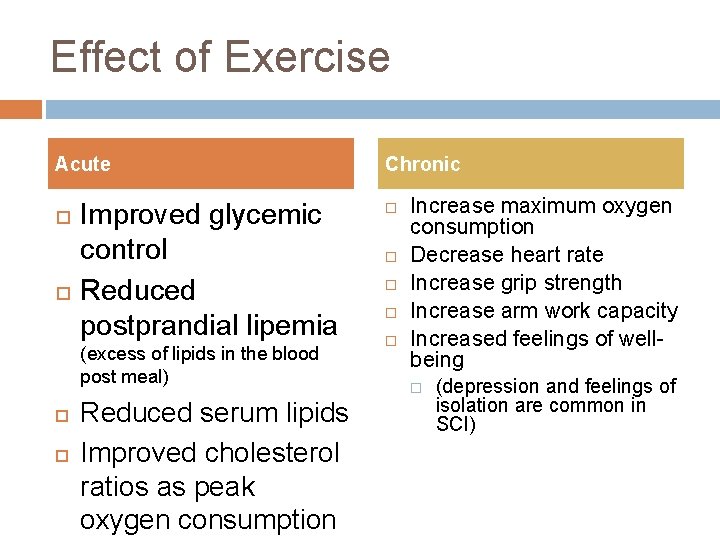
Effect of Exercise Acute Improved glycemic control Reduced postprandial lipemia (excess of lipids in the blood post meal) Reduced serum lipids Improved cholesterol ratios as peak oxygen consumption Chronic Increase maximum oxygen consumption Decrease heart rate Increase grip strength Increase arm work capacity Increased feelings of wellbeing (depression and feelings of isolation are common in SCI)
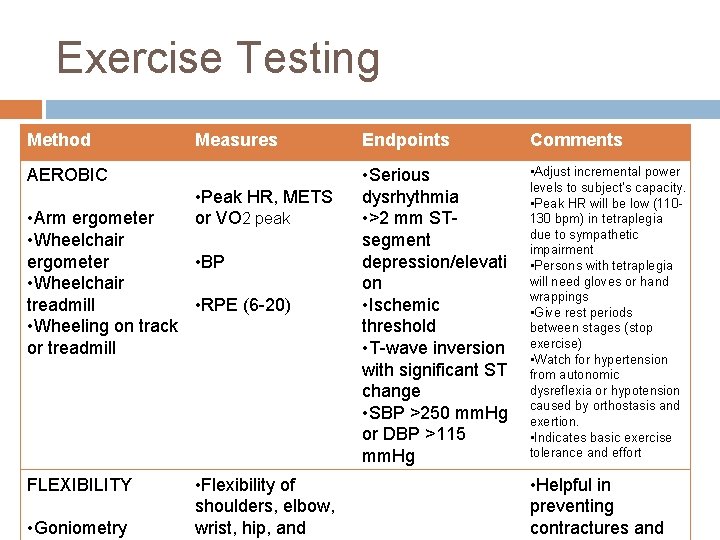
Exercise Testing Method Measures AEROBIC • Peak HR, METS or VO 2 peak • Arm ergometer • Wheelchair • BP ergometer • Wheelchair • RPE (6 -20) treadmill • Wheeling on track or treadmill FLEXIBILITY • Goniometry • Flexibility of shoulders, elbow, wrist, hip, and Endpoints Comments • Serious dysrhythmia • >2 mm STsegment depression/elevati on • Ischemic threshold • T-wave inversion with significant ST change • SBP >250 mm. Hg or DBP >115 mm. Hg • Adjust incremental power levels to subject’s capacity. • Peak HR will be low (110130 bpm) in tetraplegia due to sympathetic impairment • Persons with tetraplegia will need gloves or hand wrappings • Give rest periods between stages (stop exercise) • Watch for hypertension from autonomic dysreflexia or hypotension caused by orthostasis and exertion. • Indicates basic exercise tolerance and effort • Helpful in preventing contractures and
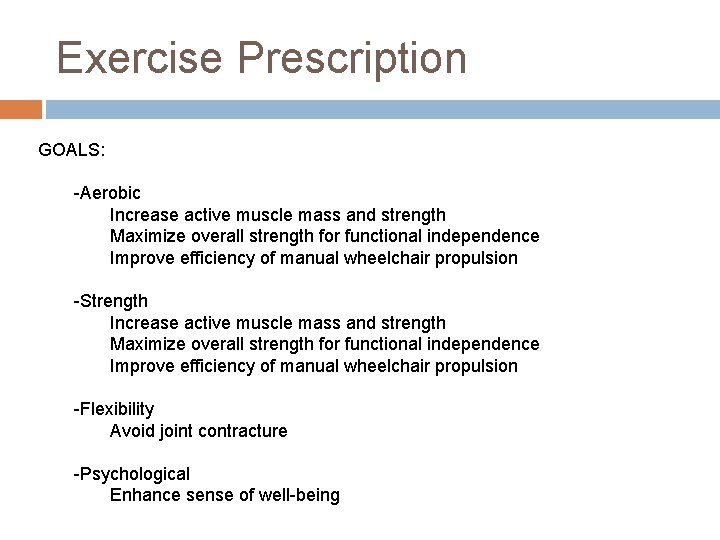
Exercise Prescription GOALS: -Aerobic Increase active muscle mass and strength Maximize overall strength for functional independence Improve efficiency of manual wheelchair propulsion -Strength Increase active muscle mass and strength Maximize overall strength for functional independence Improve efficiency of manual wheelchair propulsion -Flexibility Avoid joint contracture -Psychological Enhance sense of well-being
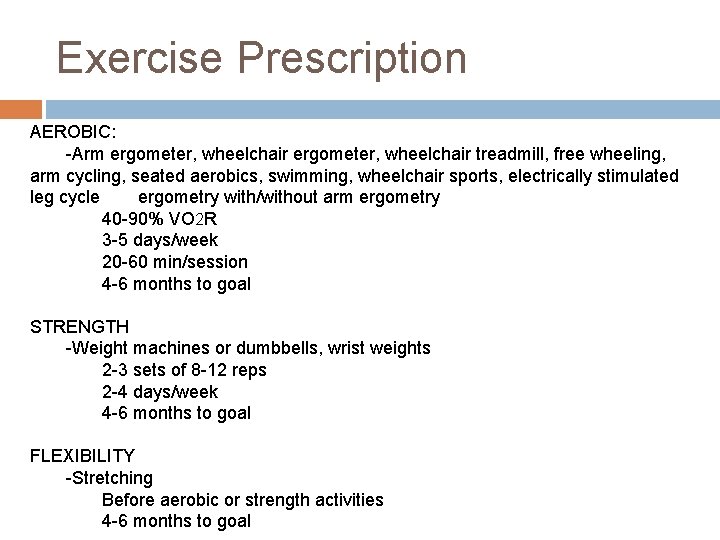
Exercise Prescription AEROBIC: -Arm ergometer, wheelchair treadmill, free wheeling, arm cycling, seated aerobics, swimming, wheelchair sports, electrically stimulated leg cycle ergometry with/without arm ergometry 40 -90% VO 2 R 3 -5 days/week 20 -60 min/session 4 -6 months to goal STRENGTH -Weight machines or dumbbells, wrist weights 2 -3 sets of 8 -12 reps 2 -4 days/week 4 -6 months to goal FLEXIBILITY -Stretching Before aerobic or strength activities 4 -6 months to goal
Summary & Conclusion There are many causes that can effect the development of Spinal Cord Injury When the spinal cord is injured the brain cannot properly communicate with it and so sensation and movement are impaired. Serious complications can result if quadriplegia or paraplegia are not managed carefully. Exercise is a great way for most individuals with spinal cord injury to improve their overall health and ability to do every day activities.
References §American Spinal Injury Association, Autonomic Standards Form, Retrieved from http: //www. asiaspinalinjury. org/presentations/presentation. php#. Retrieved March 16, 2011. §Brain and Spinal Cord. org, Quadriplegia Treatment, Retrieved from http: //www. brainandspinalcord. org/spinal-cord-injury-types/quadriplegia/index. html. Retrieved March 16, 2011. §Centers for Disease Control, Spinal Cord Injury Fact Sheet, Retrieved from http: //www. cdc. gov/Traumatic. Brain. Injury/scifacts. html. Retrieved March 16, 2011. §Collins, E. (2010). Energy Cost of Physical Activities in Persons with Spinal Cord Injury. Medicine and Science in Sports and Exercise, 42(4), 691 -700. §Durstine, J. L. , et al. Spinal Cord Disabilities ACSM’s Exercise Management for Person with Chronic Diseases and Disabilities. 3 rd edition. ACSM, USA; 2009. §Figoni, S. (1993). Exercise responses and quadriplegia. Medicine and Science in Sports and Exercise, 25 (4), 433 -441. §Hicks, A. (2005). Exercise Research Issues in the Spinal Cord Injured Population. Exercise and Sport Sciences Reviews, 33(1), 49 -53 §Hopman, M. (1997). Spinal Cord Injury and Exercise In The Heat. Sports Science Exchange, 10, 1551 -1557. § Howley, E. T. , Franks, B. D. Nutrition. Fitness Professional’s Handbook. 5 th edition. Human Kinetics, USA; 2007. § Mahan, K. L. , Escott-Stump, S. Medical Nutrition Therapy for Quadriplegia. Krause’s Food & Nutrition Therapy. 12 th edition. Saunders Elsevier, USA; 2007. §Mackie, J. W. (1989). Fitness and Spinal Cord Injuries. Canada Family Physician, 35, 1663 -1666. §Mayo Clinic, Tests and Diagnosis, Retrieved from http: //www. mayoclinic. com/health/spinal-cordinjury/DS 00460/DSECTION=tests-and-diagnosis. Retrieved March 16, 2011. §National Spinal Cord Injury Association, Exercise. Retrieved from
SPINAL CORD DISABILITY TESTING
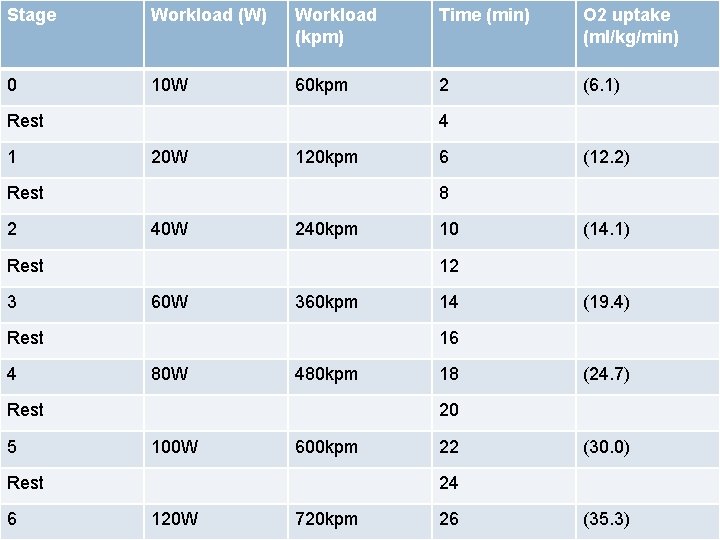
Stage 0 Workload (W) Workload (kpm) Arm 10 WErgometer 60 kpm Rest 1 20 W 120 kpm 40 W 240 kpm 60 W 360 kpm 80 W 480 kpm (12. 2) 10 (14. 1) 14 (19. 4) 18 (24. 7) 20 100 W 600 kpm Rest 6 6 16 Rest 5 (6. 1) 12 Rest 4 2 8 Rest 3 O 2 uptake (ml/kg/min) 4 Rest 2 Time (min) 22 (30. 0) 24 120 W 720 kpm 26 (35. 3)
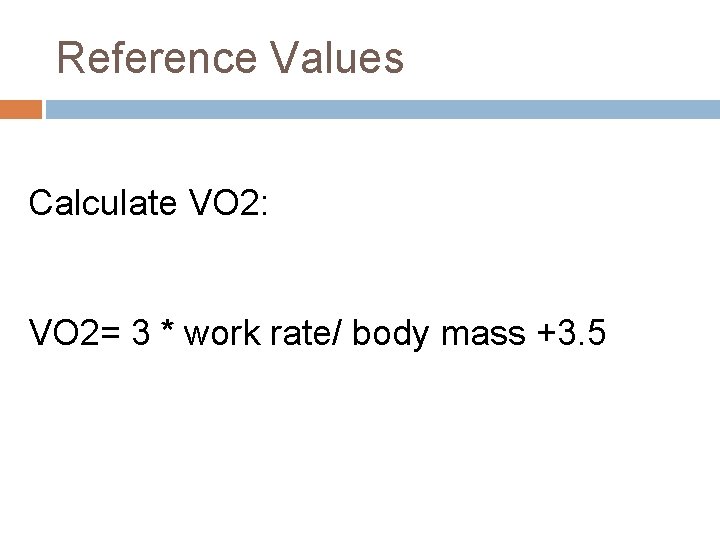
Reference Values Calculate VO 2: VO 2= 3 * work rate/ body mass +3. 5
- Slides: 34