Spinal Cord Compression Spine Fractures Department of Neurosurgery



- Slides: 51

Spinal Cord Compression & Spine Fractures Department of Neurosurgery Faculty of Medicine, Alexandria University
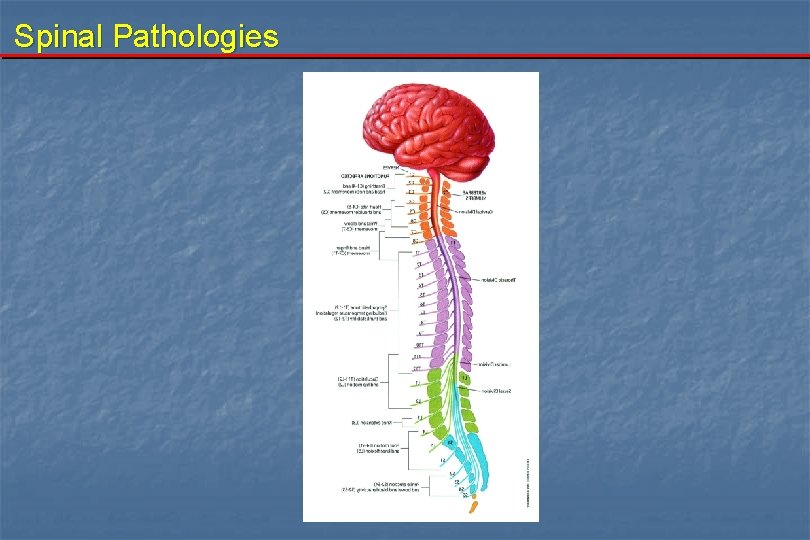
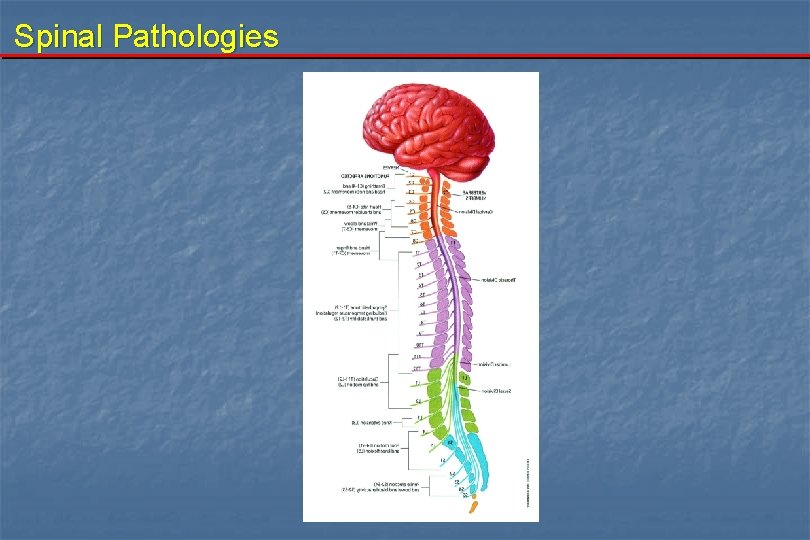
Spinal Pathologies
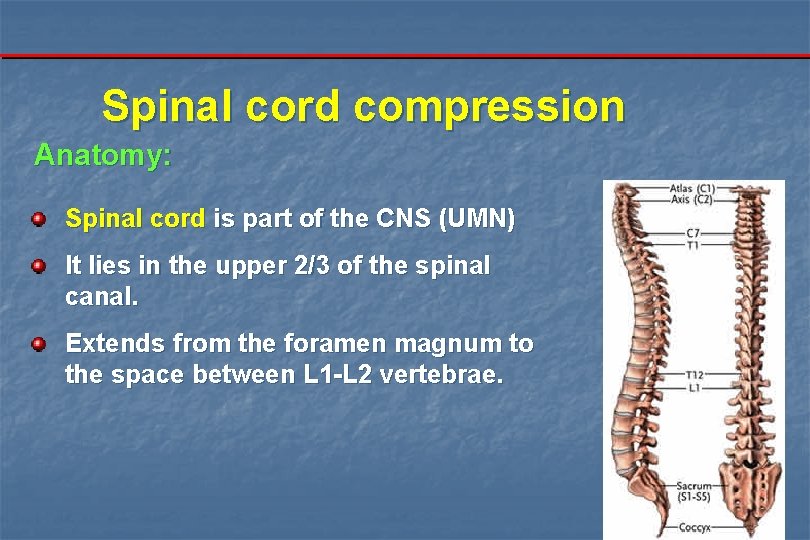
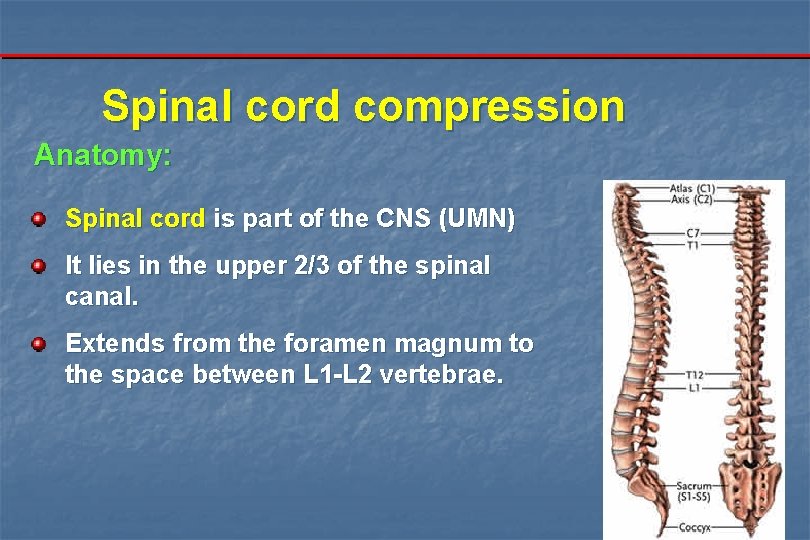
Spinal cord compression Anatomy: Spinal cord is part of the CNS (UMN) It lies in the upper 2/3 of the spinal canal. Extends from the foramen magnum to the space between L 1 -L 2 vertebrae.
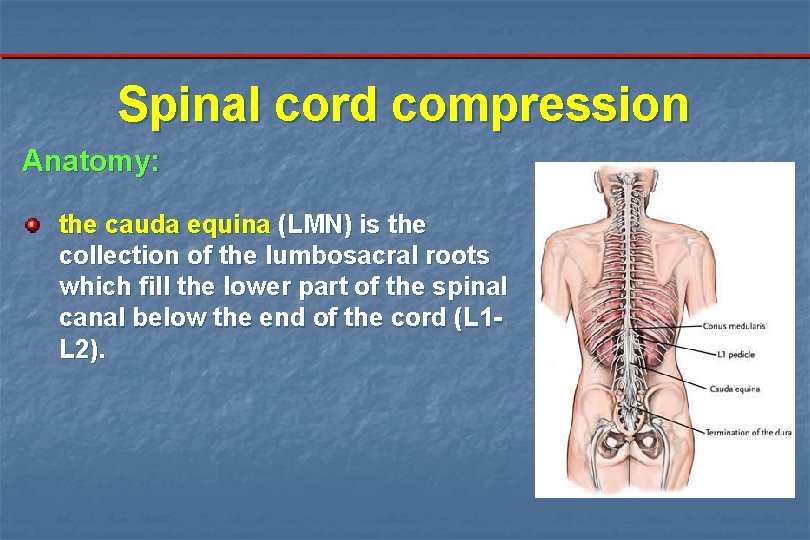
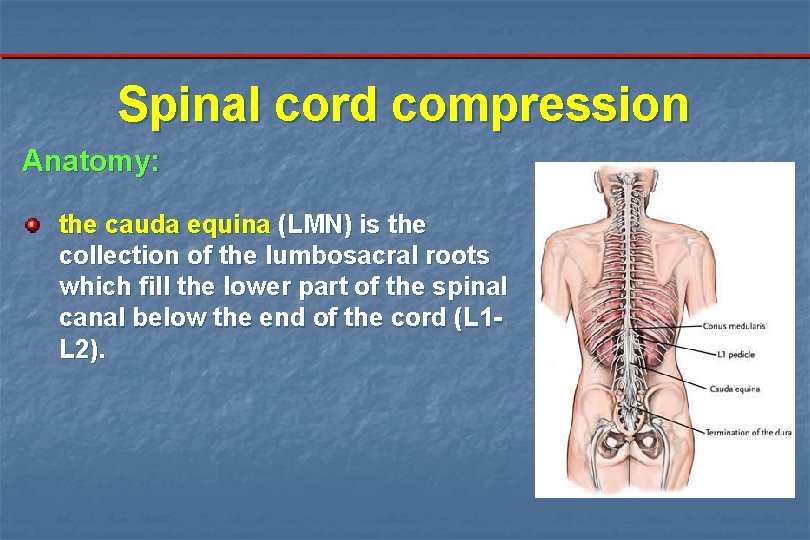
Spinal cord compression Anatomy: the cauda equina (LMN) is the collection of the lumbosacral roots which fill the lower part of the spinal canal below the end of the cord (L 1 L 2).
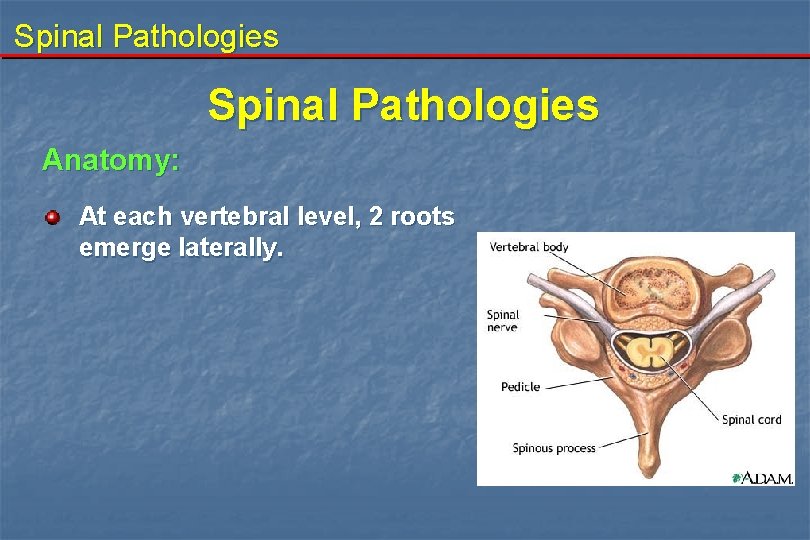
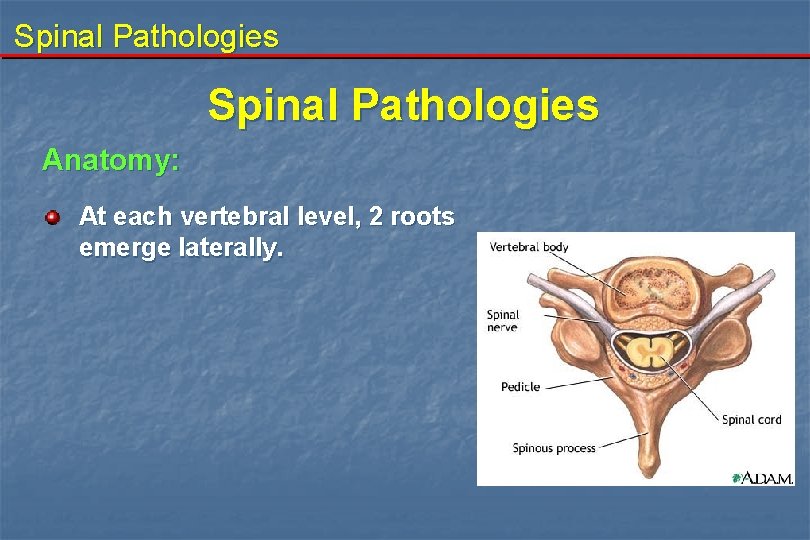
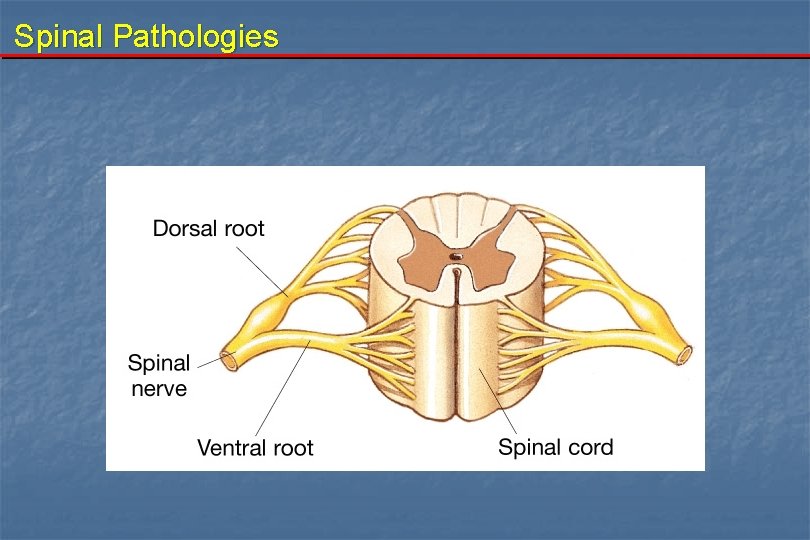
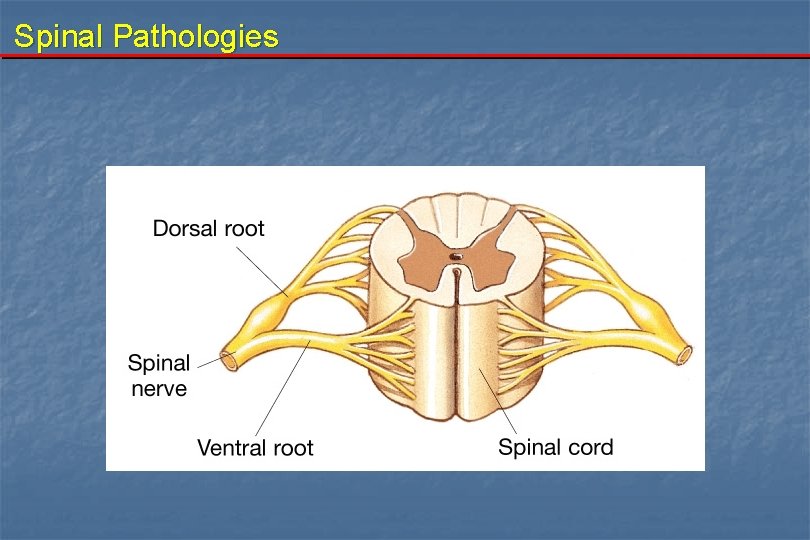
Spinal Pathologies Anatomy: At each vertebral level, 2 roots emerge laterally.
Spinal Pathologies
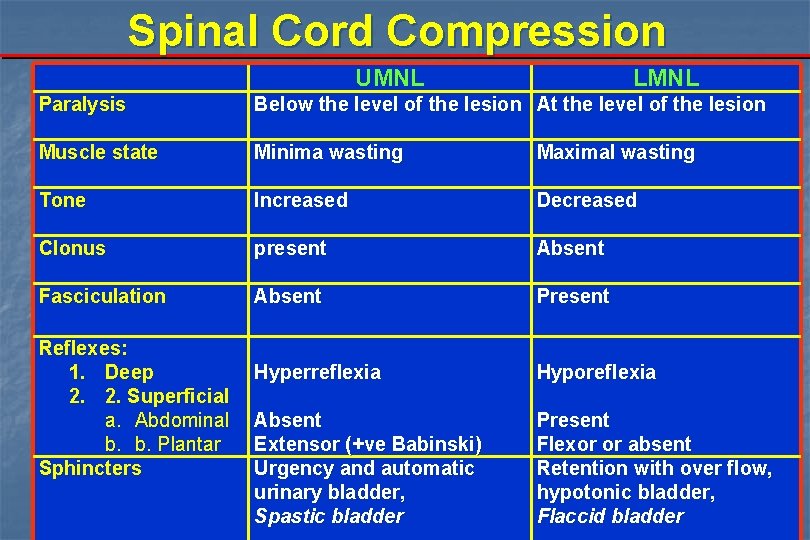
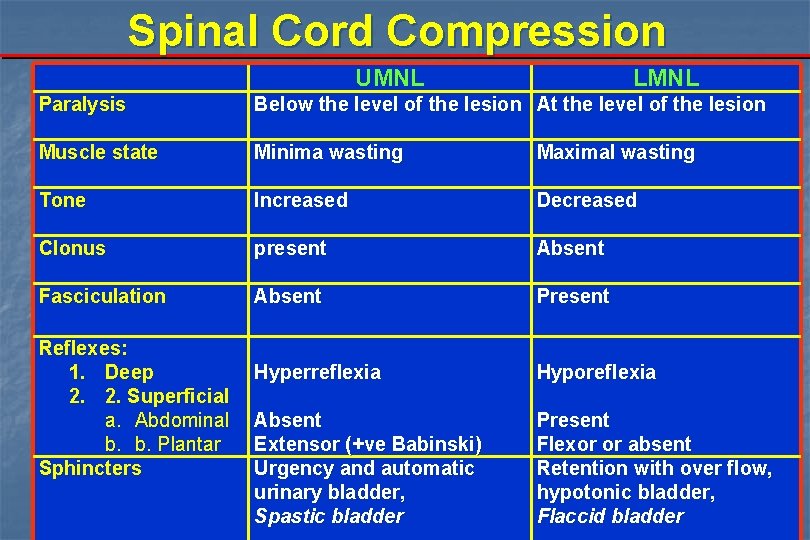
Spinal Cord Compression UMNL LMNL Paralysis Below the level of the lesion At the level of the lesion Muscle state Minima wasting Maximal wasting Tone Increased Decreased Clonus present Absent Fasciculation Absent Present Hyperreflexia Hyporeflexia Absent Extensor (+ve Babinski) Urgency and automatic urinary bladder, Spastic bladder Present Flexor or absent Retention with over flow, hypotonic bladder, Flaccid bladder Reflexes: 1. Deep 2. 2. Superficial a. Abdominal b. b. Plantar Sphincters
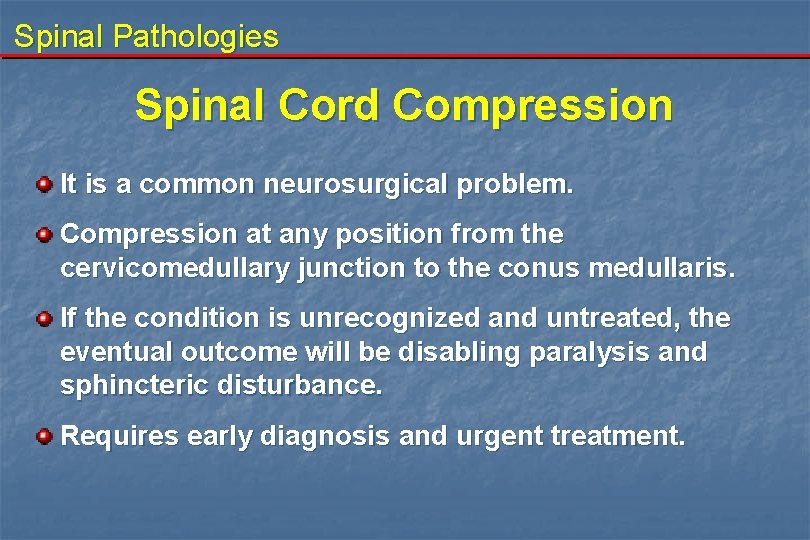
Spinal Pathologies Spinal Cord Compression It is a common neurosurgical problem. Compression at any position from the cervicomedullary junction to the conus medullaris. If the condition is unrecognized and untreated, the eventual outcome will be disabling paralysis and sphincteric disturbance. Requires early diagnosis and urgent treatment.
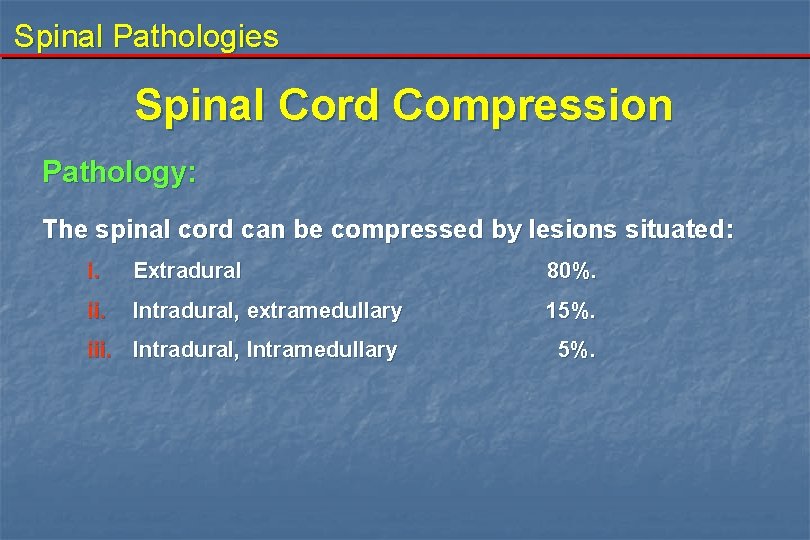
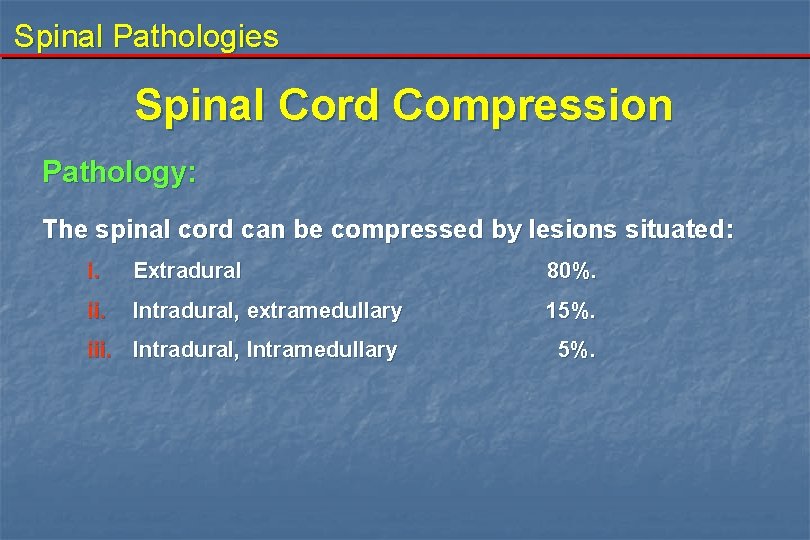
Spinal Pathologies Spinal Cord Compression Pathology: The spinal cord can be compressed by lesions situated: i. Extradural 80%. ii. Intradural, extramedullary 15%. iii. Intradural, Intramedullary 5%.
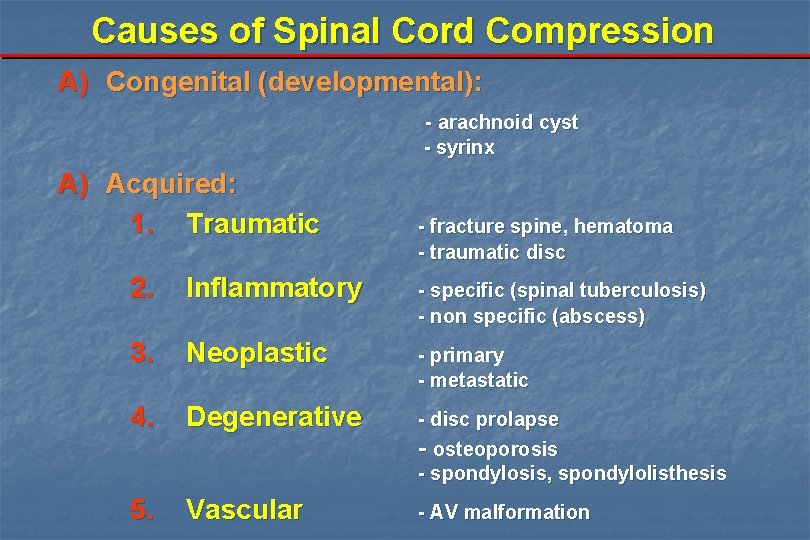
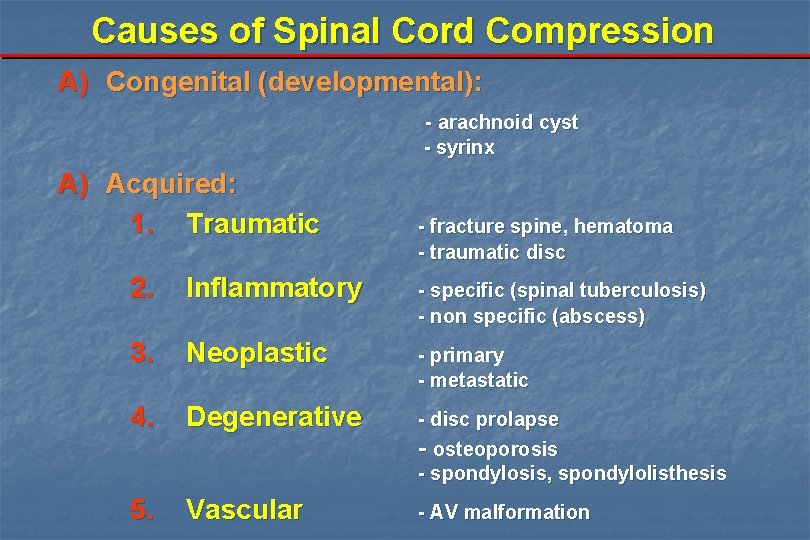
Causes of Spinal Cord Compression A) Congenital (developmental): - arachnoid cyst - syrinx A) Acquired: 1. Traumatic - fracture spine, hematoma - traumatic disc 2. Inflammatory - specific (spinal tuberculosis) - non specific (abscess) 3. Neoplastic - primary - metastatic 4. Degenerative - disc prolapse - osteoporosis - spondylosis, spondylolisthesis 5. Vascular - AV malformation
Spinal Pathologies Spinal Cord Compression Presenting features: 1. Pain 2. Neurological deficit: a- Progressive motor weakness b- Sensory disturbance c- Sphincteric disturbance
Spinal Pathologies Spinal Cord Compression 1. Pain The first and most common complaint and often precedes the onset of any neurological disturbance. Pain is due to: - Involvement of pain sensitive structures such as the bone. - Radicular pain due to spinal root compression. - Central pain due to Spinal cord compression results in unpleasant diffuse dull ache.
Spinal Pathologies Spinal Cord Compression 2. Neurological deficit: - Depends on: a- the level of compression b- site of compression c- involvement of adjacent nerve roots d- speed of compression e- the pathological nature of the compressing lesion
Spinal Pathologies 2. Neurological deficit: a. Progressive motor weakness Paraperesis or quadriparesis according to the level of compression. The pattern of weakness is also affected by the position of the compressing lesion. Conus medullaris lesions give a mixture of UMN and LMN features. Cauda equina compression produces LMN signs. Cervical or dorsal compression till L 1 : UMNL. Lumbar or sacral compression till S 2 : LMNL.
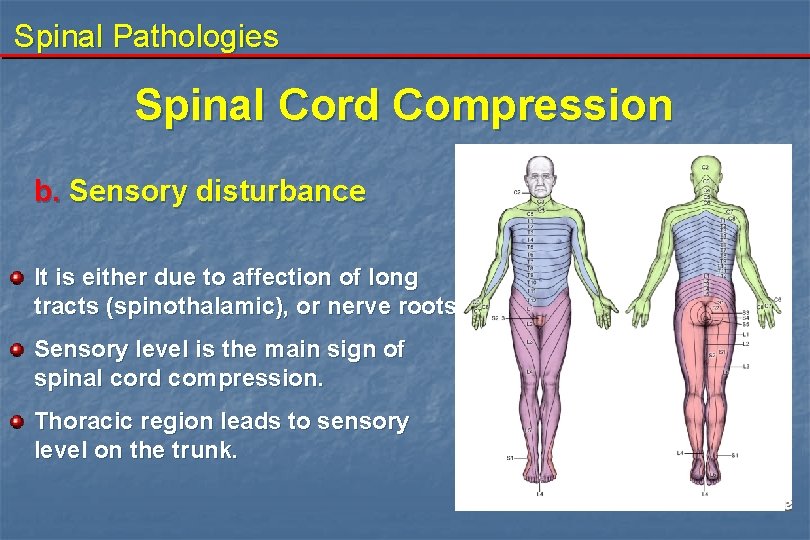
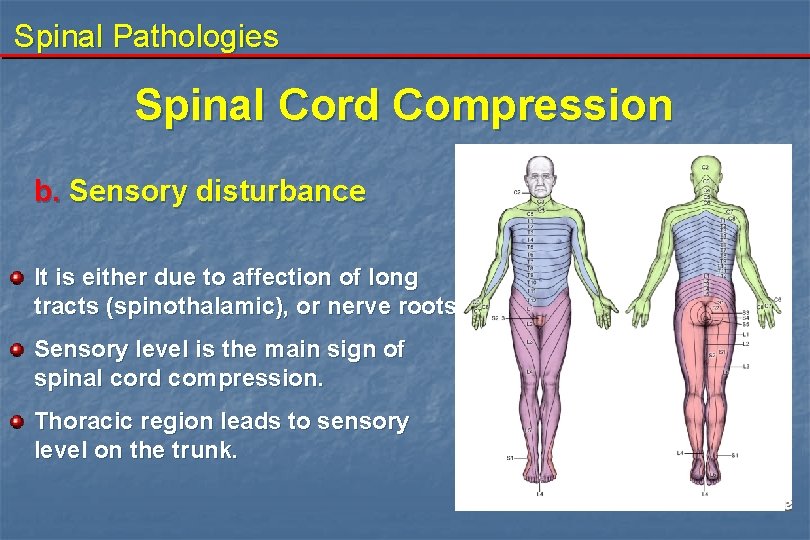
Spinal Pathologies Spinal Cord Compression b. Sensory disturbance It is either due to affection of long tracts (spinothalamic), or nerve roots. Sensory level is the main sign of spinal cord compression. Thoracic region leads to sensory level on the trunk.
Spinal Pathologies Spinal Cord Compression c. Sphincteric disturbance: Occurs following: a. Compression of the cord. b. Compression of the conus. c. Compression of the cauda equina. The first symptom is difficulty in initiating micturation leading to urinary retention. In addition to constipation and Feacal incontinence.
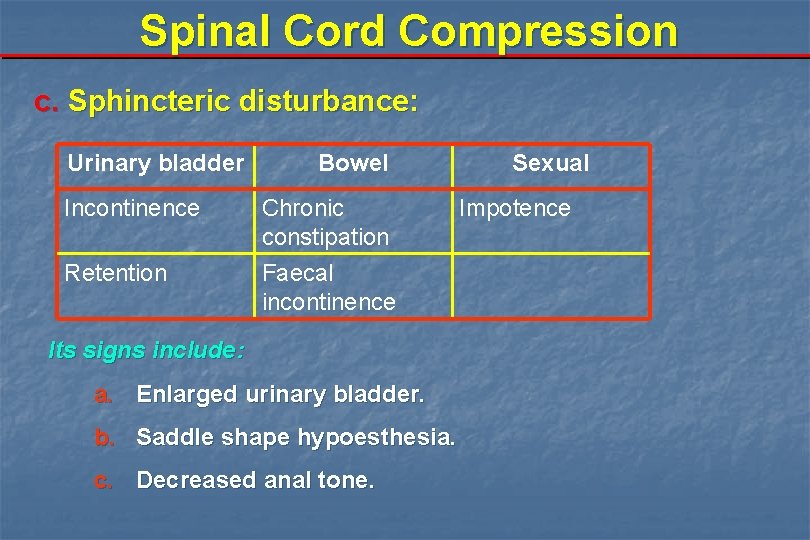
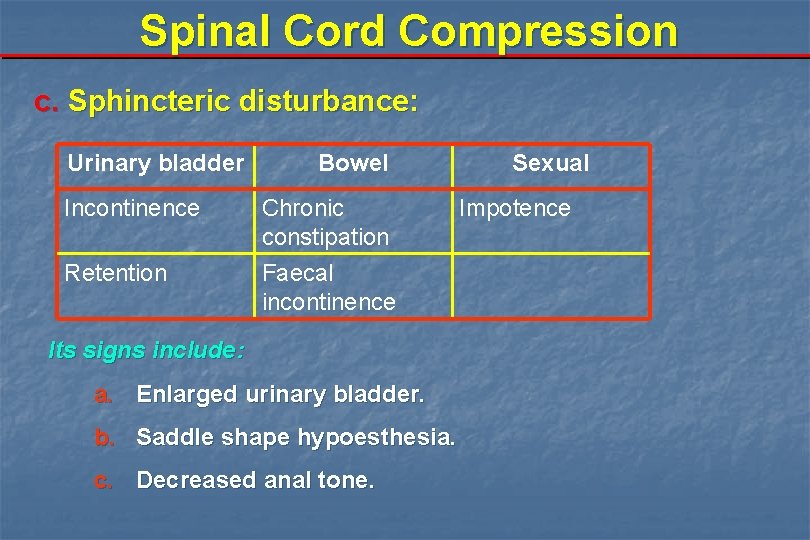
Spinal Cord Compression c. Sphincteric disturbance: Urinary bladder Bowel Incontinence Chronic constipation Retention Faecal incontinence Its signs include: a. Enlarged urinary bladder. b. Saddle shape hypoesthesia. c. Decreased anal tone. Sexual Impotence
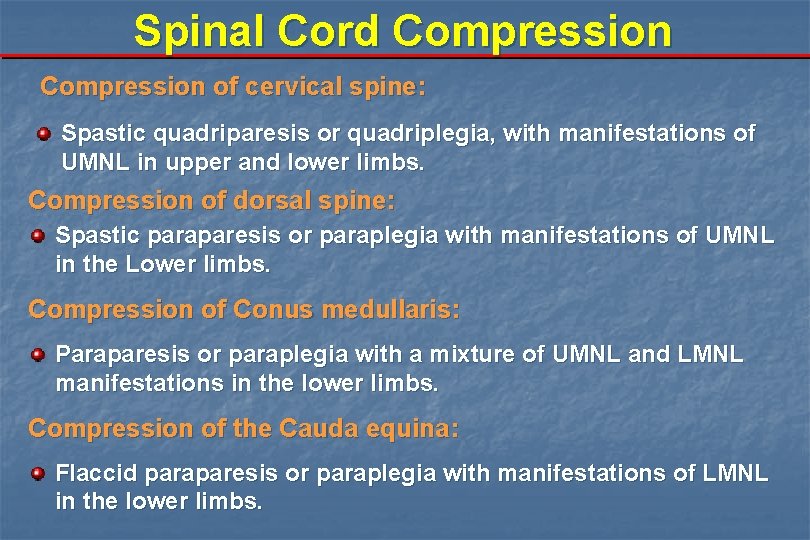
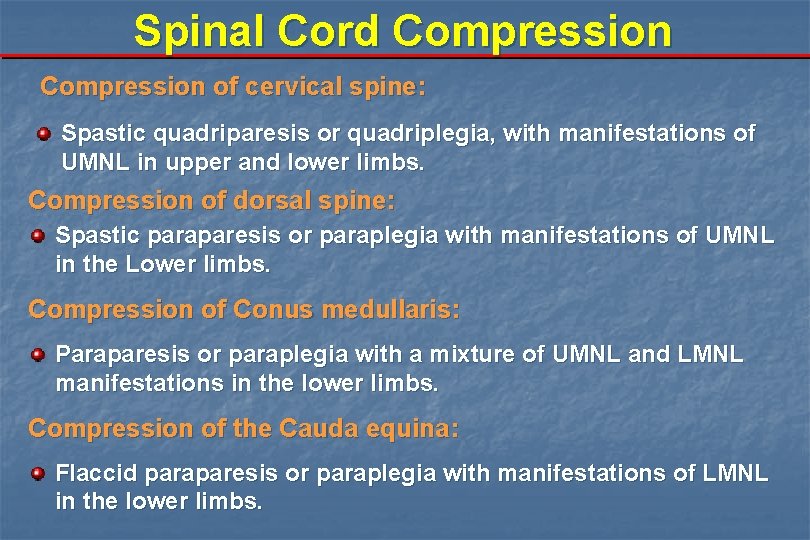
Spinal Cord Compression of cervical spine: Spastic quadriparesis or quadriplegia, with manifestations of UMNL in upper and lower limbs. Compression of dorsal spine: Spastic paraparesis or paraplegia with manifestations of UMNL in the Lower limbs. Compression of Conus medullaris: Paraparesis or paraplegia with a mixture of UMNL and LMNL manifestations in the lower limbs. Compression of the Cauda equina: Flaccid paraparesis or paraplegia with manifestations of LMNL in the lower limbs.
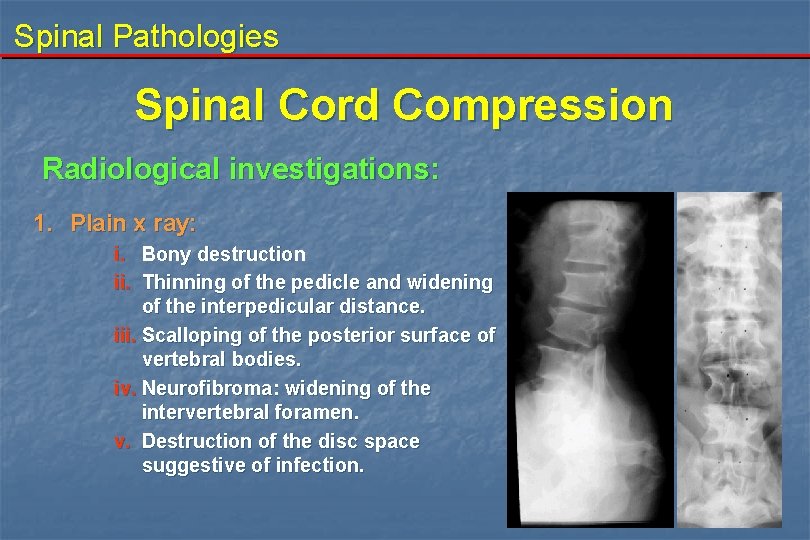
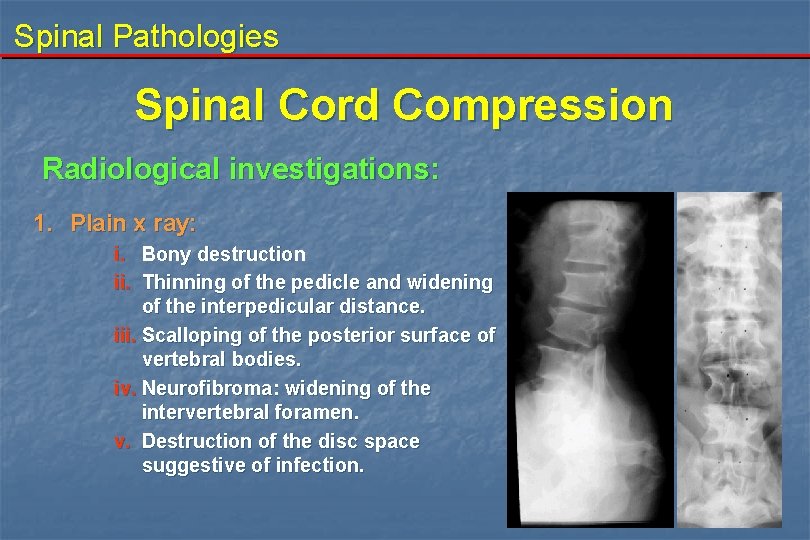
Spinal Pathologies Spinal Cord Compression Radiological investigations: 1. Plain x ray: i. Bony destruction ii. Thinning of the pedicle and widening of the interpedicular distance. iii. Scalloping of the posterior surface of vertebral bodies. iv. Neurofibroma: widening of the intervertebral foramen. v. Destruction of the disc space suggestive of infection.
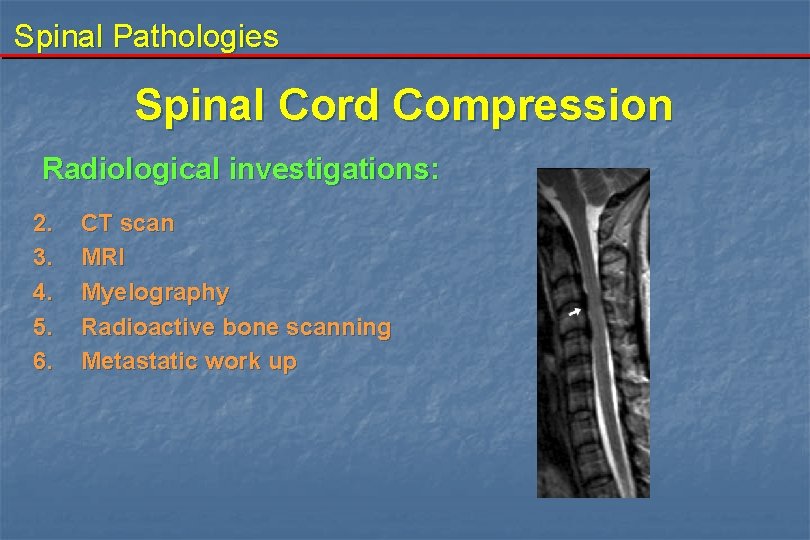
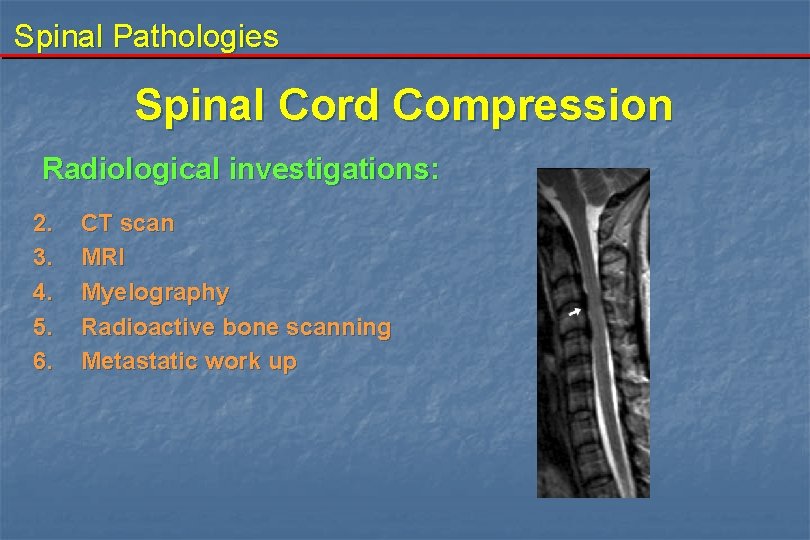
Spinal Pathologies Spinal Cord Compression Radiological investigations: 2. 3. 4. 5. 6. CT scan MRI Myelography Radioactive bone scanning Metastatic work up
Spinal Pathologies Spinal Cord Compression Treatment: n Spinal cord compression is a neurosurgical emergency. n The standard treatment of spinal compression is urgent surgery except in some cases due to malignant tumors where corticosteroids and radiotherapy are given.

Spinal Pathologies Spinal Cord Compression D. D. of upper or lower limb weakness: Different causes of spinal compression. Neuritis. Guillian Barre' Syndrome. Multiple sclerosis. Hysterical.
Spinal Pathologies Spine Fracture Epidemiology: It is common in young age (working age). In old age it is usually secondary to osteoporosis or metastatic lesions. Incidence: 2 -5/100 000 population 10% will result in paraplegia or quadriplegia
Spinal Pathologies Spine Fracture Causes : 1. Road traffic accidents (most common) 2. Sport injuries: - Swimming "diving" - Horse riding - Skiing 3. Blunt trauma 4. Falling from height 5. Falling of heavy object over the head
Spinal Pathologies Spine Fracture Mechanism of injury: the mechanism of injury will determine the type of vertebral injury and the neurological damage. I. Flexion and flexion rotation injuries II. Hyperextension injuries III. Compression injuries
Spinal Pathologies Fracture Spine Causes of spinal cord injury: I. III. IV. Direct compression by bone, ligament or disc. Interruption of the vascular supply. Traction injury. Secondary hemorrhage in or around the cord.
Spinal Pathologies Spine Fracture Type of neurological impairment: I. Incomplete lesion II. Complete lesion
Spinal Pathologies Spine Fracture I. Incomplete lesion: - It is the presence of any residual motor or sensory function below the level of the injury. Signs of incomplete lesions: a. Sensation or voluntary movement in the lower limbs. b. "Sacral sparing": sensation around the anus, voluntary rectal sphincteric contraction.
Spinal Pathologies Spine Fracture I. Incomplete lesion: Types of incomplete lesions: 1. 2. 3. 4. Central cord syndrome. Brown-Sequard syndrome (cord hemisection). Anterior cord syndrome. Posterior cord syndrome.
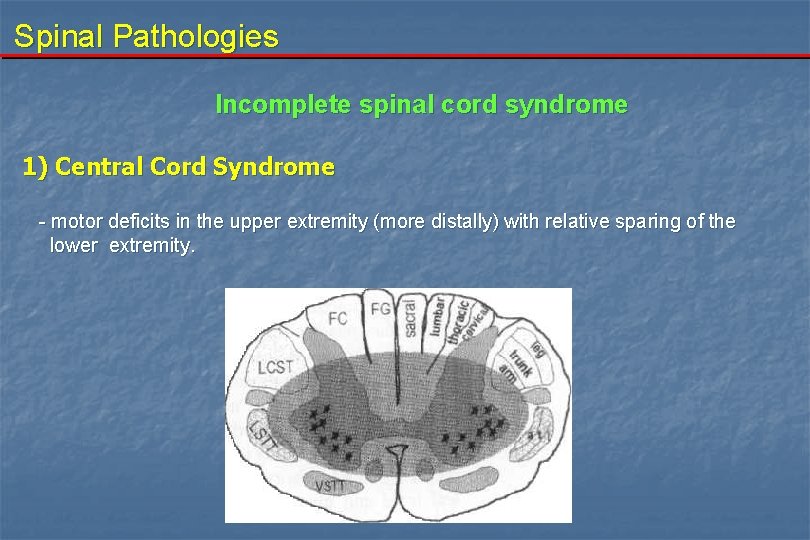
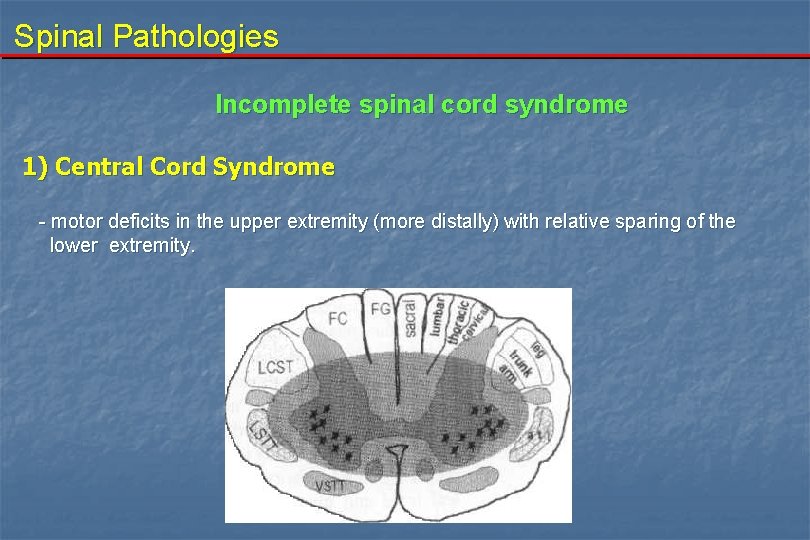
Spinal Pathologies Incomplete spinal cord syndrome 1) Central Cord Syndrome - motor deficits in the upper extremity (more distally) with relative sparing of the lower extremity.
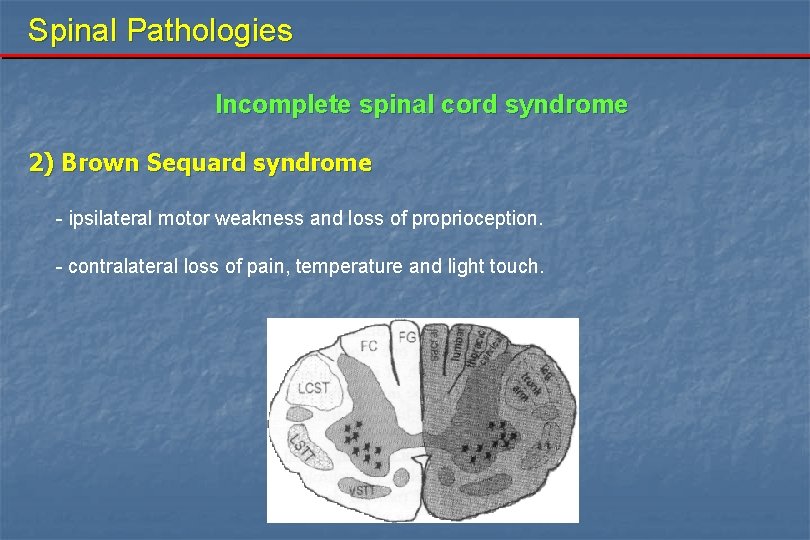
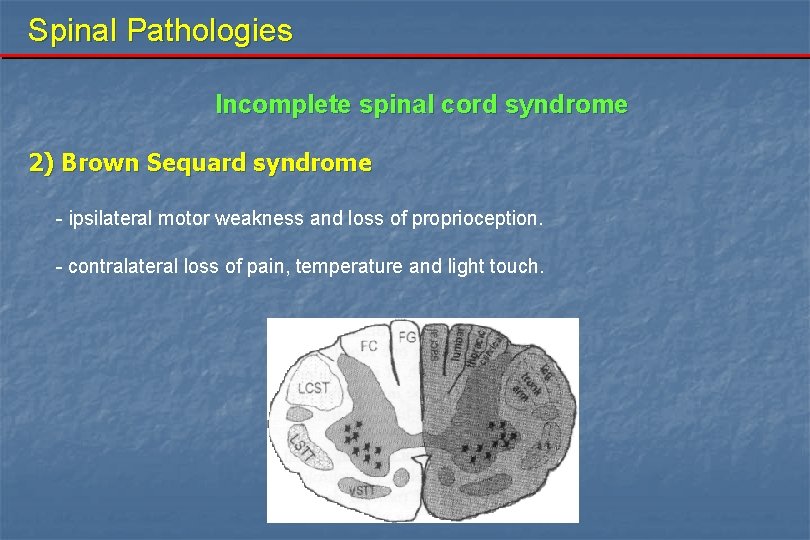
Spinal Pathologies Incomplete spinal cord syndrome 2) Brown Sequard syndrome - ipsilateral motor weakness and loss of proprioception. - contralateral loss of pain, temperature and light touch.
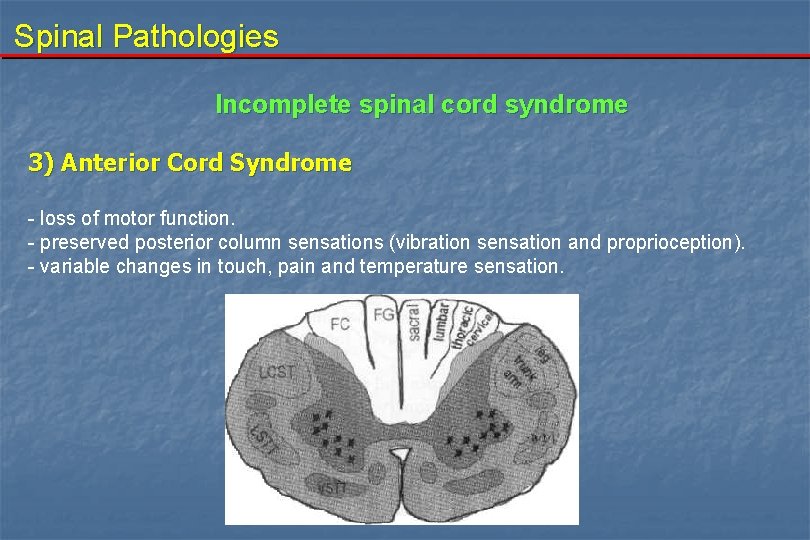
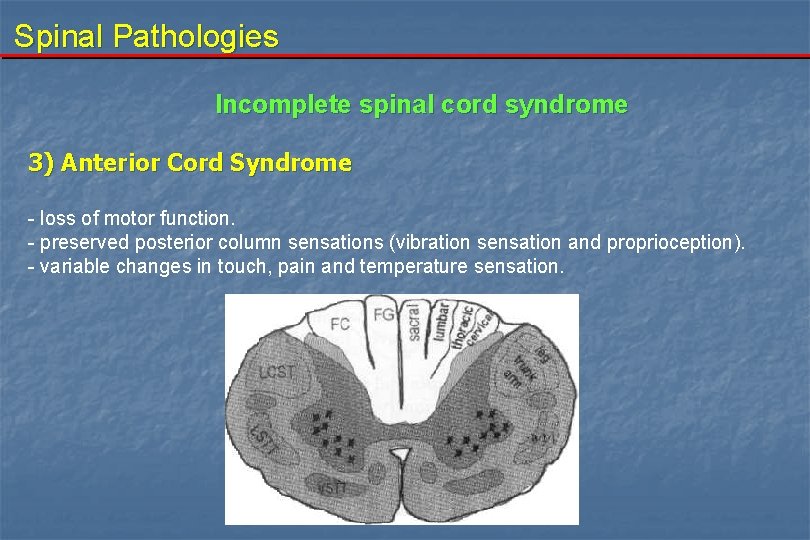
Spinal Pathologies Incomplete spinal cord syndrome 3) Anterior Cord Syndrome - loss of motor function. - preserved posterior column sensations (vibration sensation and proprioception). - variable changes in touch, pain and temperature sensation.
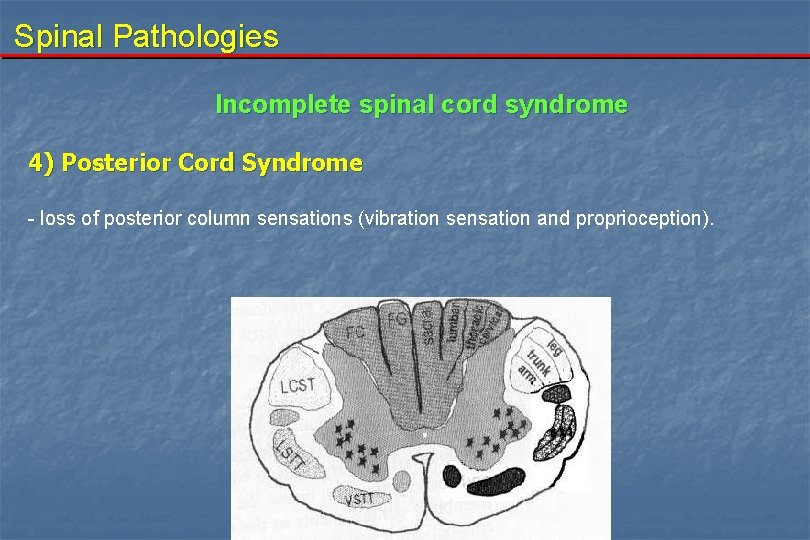
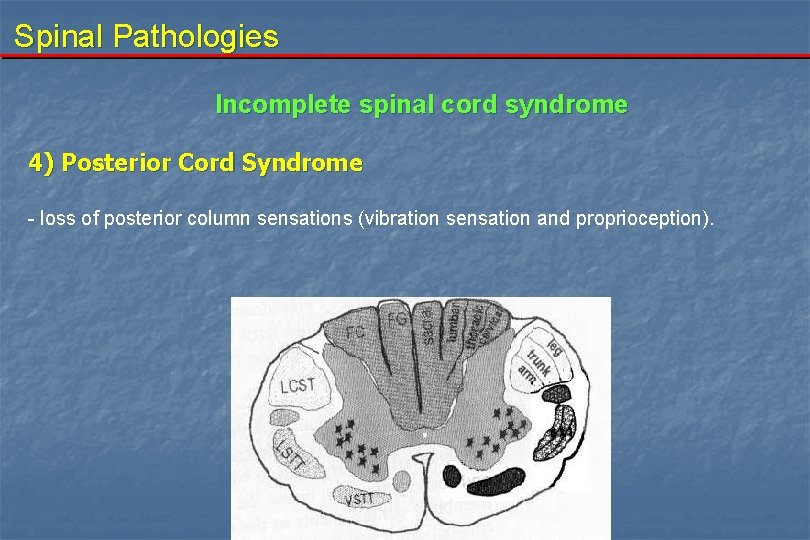
Spinal Pathologies Incomplete spinal cord syndrome 4) Posterior Cord Syndrome - loss of posterior column sensations (vibration sensation and proprioception).
Spinal Pathologies Spine Fracture Type of neurological impairment II. Complete lesion: - There is no preservation of any sensory or motor functions below the level of the injury. About 3% of patients with complete injuries on initial examination will develop some recovery within 24 hours. The persistence of complete spinal cord injury beyond 24 hours indicates that no distal function will recover. However some of them recovered after days or even weeks (very rare).
Spinal Pathologies Spine Fracture Spinal shock: This term is used in two completely different senses: 1. Hypotension (shock): that follows spinal cord injury due to: a. b. c. Interruption of sympathetic: i. Loss of vascular tone below the level of injury ii. Leaves parasympathetic relatively unopposed causing bradycardia. Loss of muscle tone below the level of injury results in venous pooling and thus hypovoleamia. Blood loss from associated wounds leading to true hypovoleamia. 2. Transient loss of all neurological functions below level of injury. There is an areflexic flaccid paralysis. The average duration is 3 -4 ws.
Spinal Pathologies Spine Fracture Denis' three column model of the spine: In an attempt to identify CT criteria of instability of the spinal fractures (especially thoracolumbar ones). 1. 2. 3. Anterior column: composed of anterior half of disc and vertebral body (includes anterior anulus fibrosus) plus the anterior longitudinal ligament. Middle column: posterior half of disc and vertebral body (includes posterior wall of vertebral body and posterior anulus fibrosus) plus the posterior longitudinal ligament. Posterior column: posterior bony complex (posterior arch) with interposed posterior ligamentous complex (suprapinous and interspinous ligament, facet joints and capsule, and ligamentum flavum).
Spine Fracture Type of fracture: I. Compression fracture: failure of the anterior column. II. burst fracture: failure of the anterior and middle columns. III. Seat belt fracrture failure of middle and posterior columns. IV. Fracture dislocation failure of anterior, middle and posterior columns
Spinal Pathologies Spine Fracture Stability of the lesion: I. Stable fracture: - It occurs if damage is in one column only. It causes wedging of the vertebra. It is more common with falling while sitting, and exaggerated flexion injury. II. Unstable fracture: - It occurs if more than 2 columns are disturbed. It is more seen in burst fracture. It is seen if torsion stress occurs.
Spinal Pathologies Spine Fracture Clinical presentation: same as mentioned before in spinal compression. Depends on: a- the level of compression b- site of compression c- involvement of adjacent nerve roots d- speed of compression
Spine Fracture Investigations: 1. Plain x ray - AP and lateral views - Dynamic study (neutral, fexion, extension) 2. CT scan - CT or 3 Dimention CT scan: more accurate than X ray and MRI for bony compression. 3. MRI - it shows the cord contusion injuries and presence of any cord insult 4. Myelography 5. Motor Evoked Potential (MEP) 6. Somatosensory Evoked Potential (SSEP)
Spinal Pathologies Spine Fracture Management: A. B. C. D. Prevention of further injury Reduction, stabilisation and decompression Prevention of complications Rehabilitation
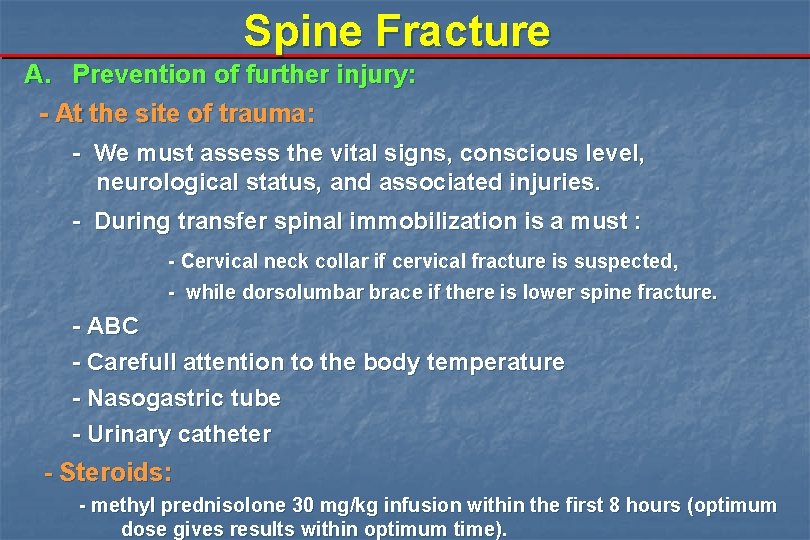
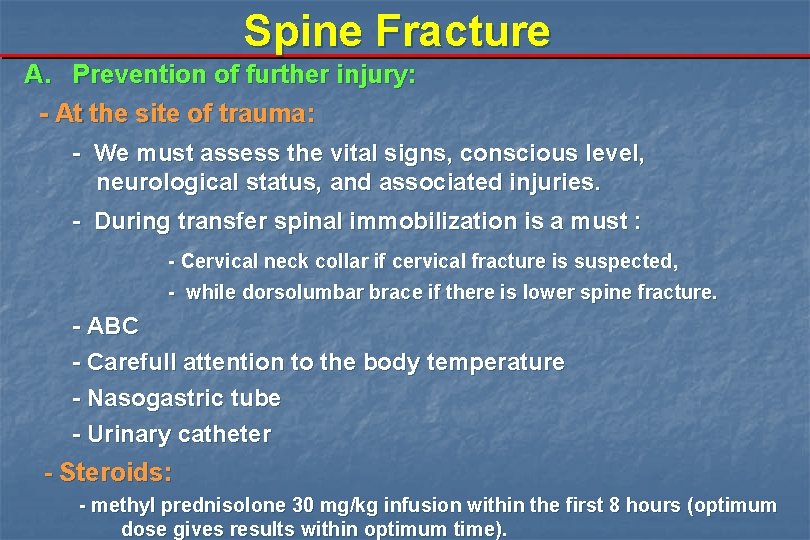
Spine Fracture A. Prevention of further injury: - At the site of trauma: - We must assess the vital signs, conscious level, neurological status, and associated injuries. - During transfer spinal immobilization is a must : - Cervical neck collar if cervical fracture is suspected, - while dorsolumbar brace if there is lower spine fracture. - ABC - Carefull attention to the body temperature - Nasogastric tube - Urinary catheter - Steroids: - methyl prednisolone 30 mg/kg infusion within the first 8 hours (optimum dose gives results within optimum time).
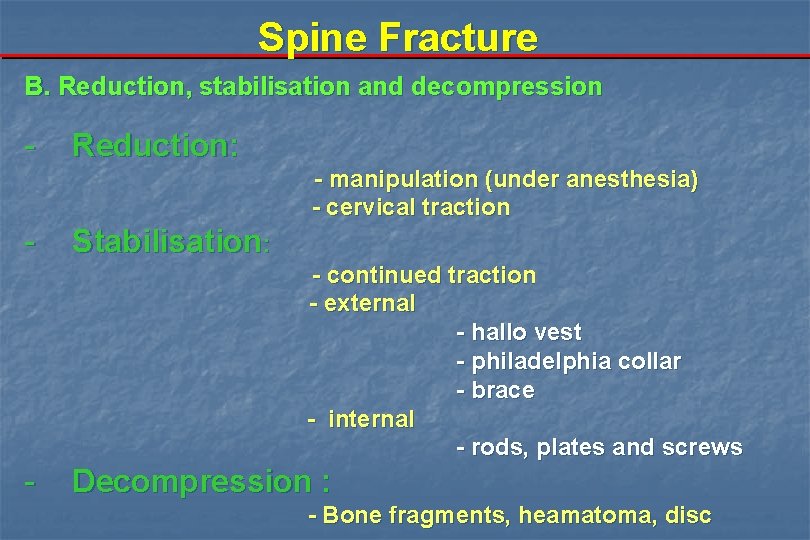
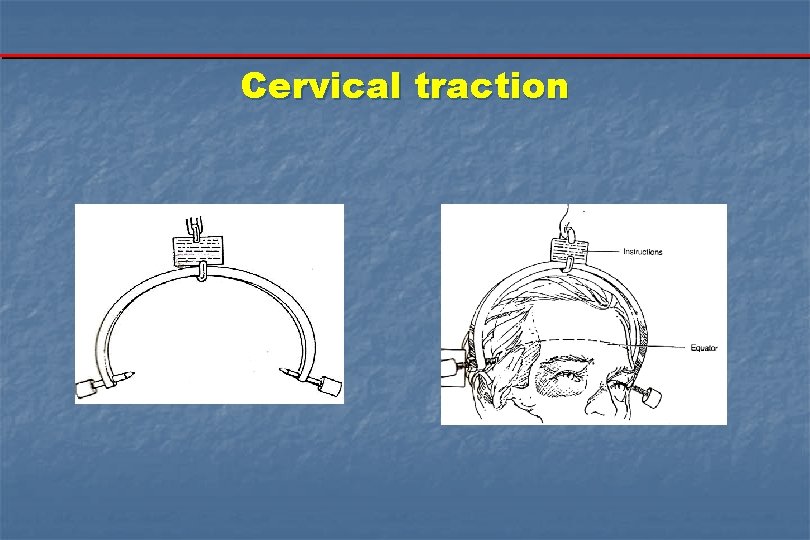
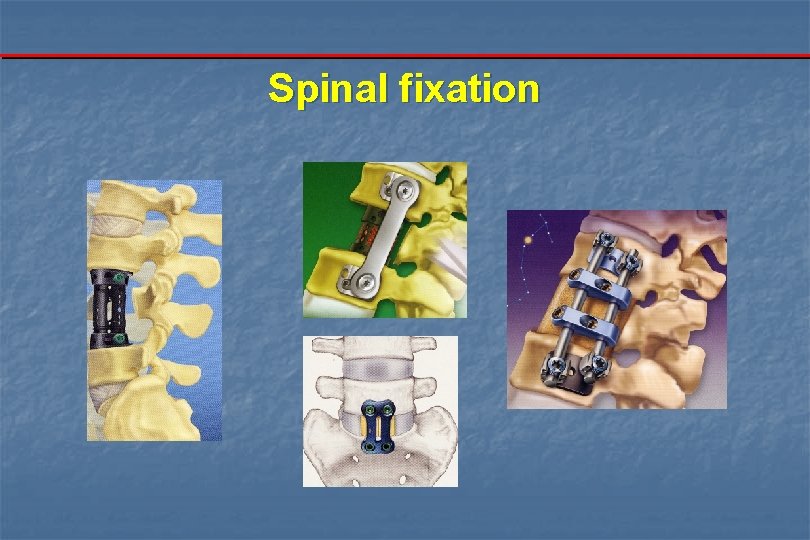
Spine Fracture B. Reduction, stabilisation and decompression - Reduction: - manipulation (under anesthesia) - cervical traction - Stabilisation: - continued traction - external - hallo vest - philadelphia collar - brace - internal - rods, plates and screws - Decompression : - Bone fragments, heamatoma, disc
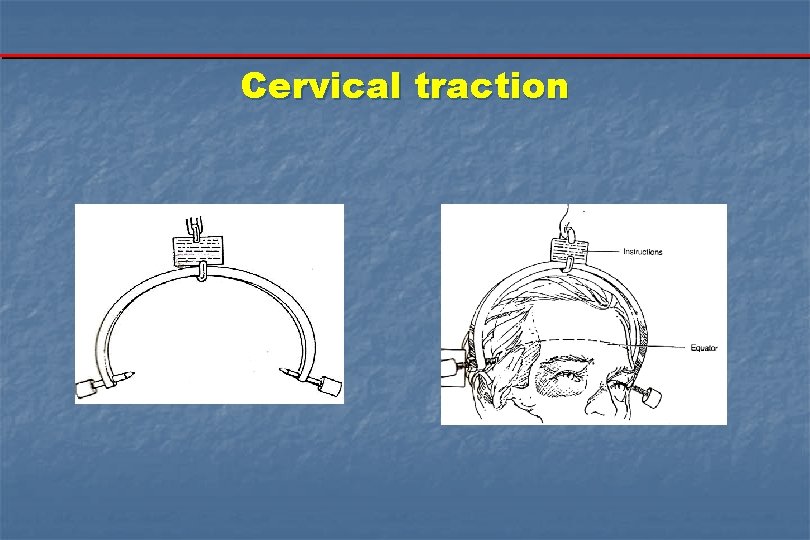
Cervical traction
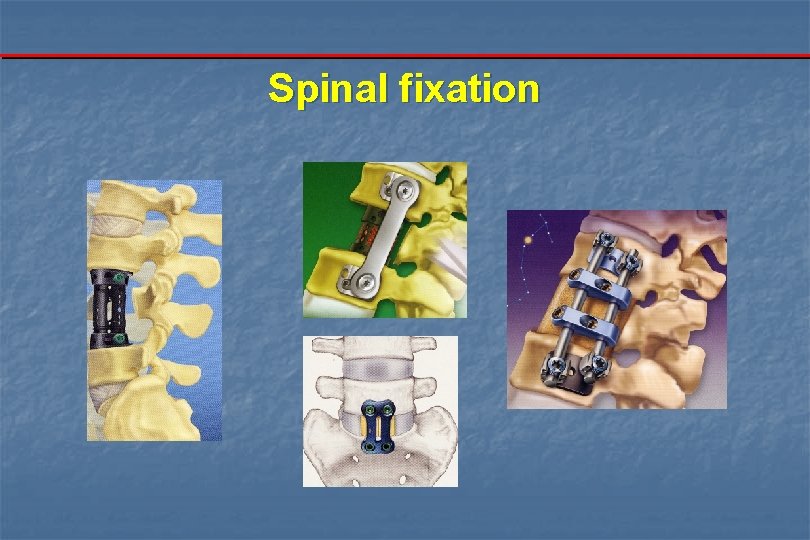
Spinal fixation
Spinal Pathologies Spine Fracture C. Prevention of complications - General - Respiratory - Skin - GIT - Urinary - Vascular - Contractures D. Rehabilitation

Data show design & preparation by : Dr. El-Sayed Amr - (012) 3106023
Spinal Pathologies Spinal Cord Compression b. Sensory disturbance: - A laterally placed mass produces "Brown Sequard Syndrome": a. contra lateral decrease in superficial sensation. b. ipsilateral decrease in cortical and deep sensation. c. ipsilateral pyramidal weakness. - Intrinsic lesions affecting the central cord produce a cape like distribution pf thermoanalgesia as in syringomyelia - Cauda equina and conus medullaris lesions produce a saddle shaped hypostheaia.
Spinal Pathologies Spine Fracture D. Rehabilitation
Akher haga khales LEBanon ya Before departure n