Spinal and Spinal Cord Trauma EMS Professions Temple












- Slides: 65
Spinal and Spinal Cord Trauma EMS Professions Temple College
Spinal Injuries z Morbidity and Mortality z Anatomy: Spine & Spinal Cord z General Assessment z Spinal Cord Injuries z Management z Spine Injury Clearance z Injury Prevention
Incidence of SCI z 10, 000 - 20, 000 spinal cord injuries per year z Incidence y~ 82% occur in men y ~ 61% occur in 16 -30 yoa z Common causes y. MVC (48%) y. Falls (21%) y. Penetrating injuries (15%) y. Sports injuries (14%)
Morbidity & Mortality z 40% of trauma patients with neuro deficits will have temporary or permanent SCI z Many more vertebral injuries that do not result in cord injury z Most commonly injured vertebrae y. C 5 -C 7 y. C 1 -C 2 y. T 12 -L 2

Prevention z Education in proper handling and movement can decrease SCI z Primary Injury Prevention y. Public Education y. EMS Community Service Projects z Secondary Injury Prevention y. First Responder Care y. EMS Care y. Tertiary Hospital Care
Anatomy Review z 33 Vertebrae z Spine supported by pelvis z key ligaments and muscles connect head to pelvis yanterior longitudinal ligament xanterior portion of the vertebral body xmajor source of stability xprotects against hyperextension yposterior longitudinal ligament xposterior vertebral body within the vertebral canal xprevents hyperflexion
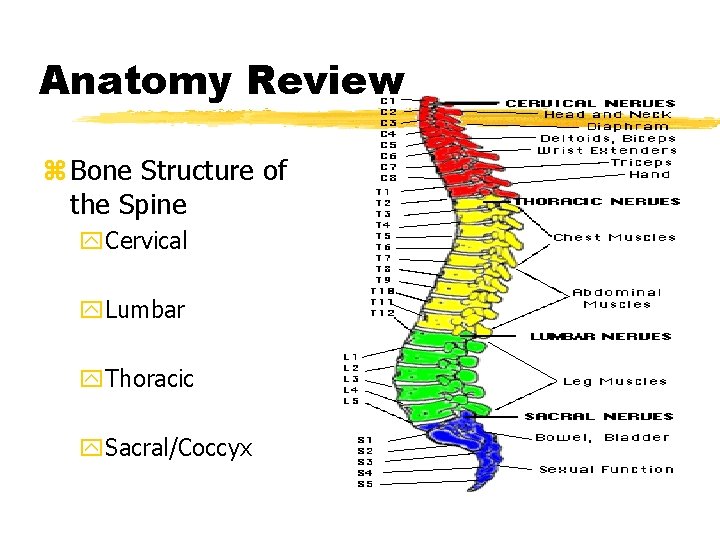
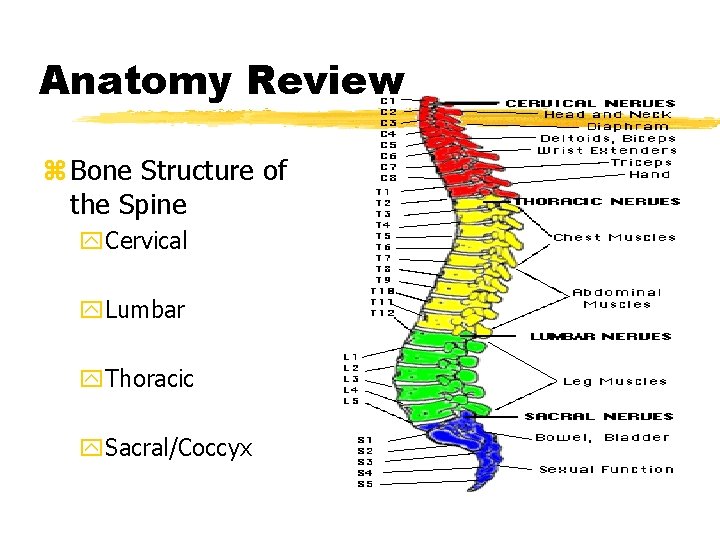
Anatomy Review z Bone Structure of the Spine y. Cervical y. Lumbar y. Thoracic y. Sacral/Coccyx
Anatomy Review z Cervical Spine y 7 vertebrae yvery flexible y. C 1: also known as the atlas y. C 2: also known as the axis z Thoracic Spine y 12 vertebrae yribs connected to spine yprovides rigid framework of thorax
Anatomy Review z Lumbar Spine y 5 vertebrae ylargest vertebral bodies ycarries most of the body’s weight z Sacrum y 5 fused vertebrae ycommon to spine and pelvis z Coccyx y 4 fused vertebrae y“tailbone”
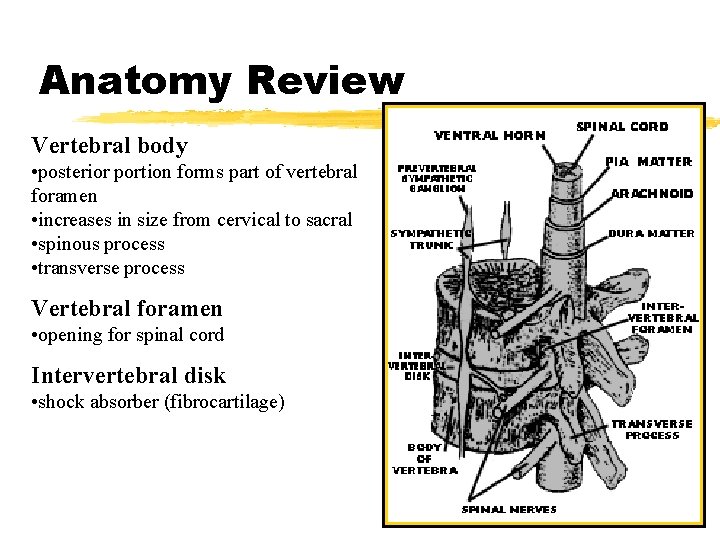
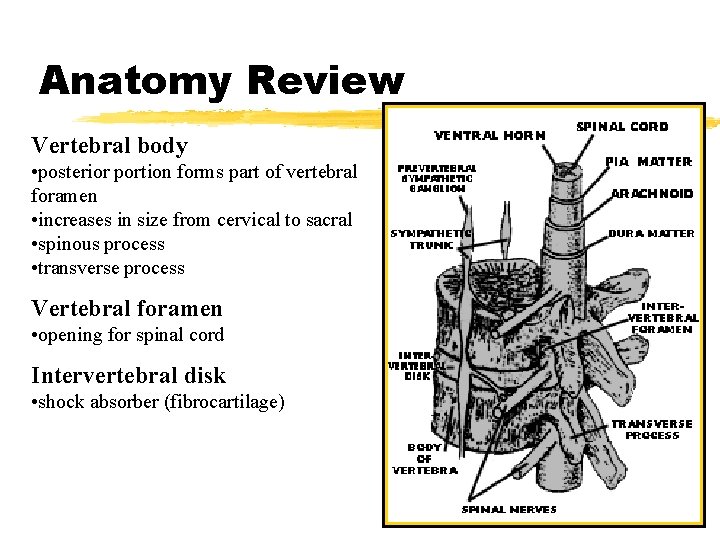
Anatomy Review Vertebral body • posterior portion forms part of vertebral foramen • increases in size from cervical to sacral • spinous process • transverse process Vertebral foramen • opening for spinal cord Intervertebral disk • shock absorber (fibrocartilage)
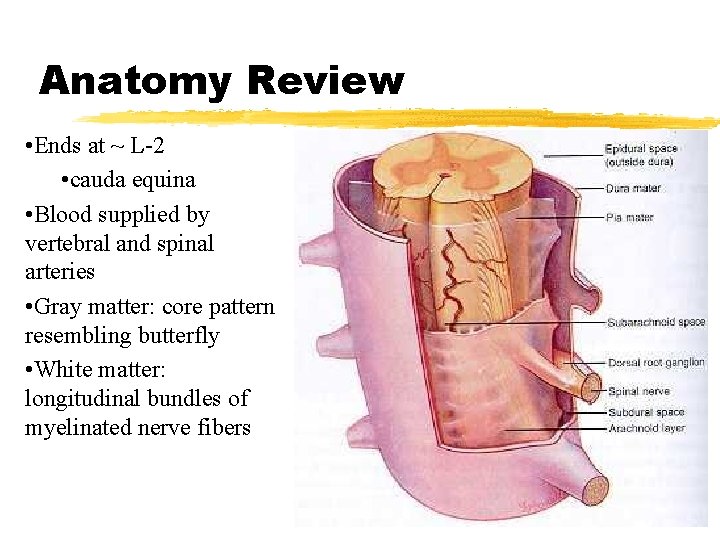
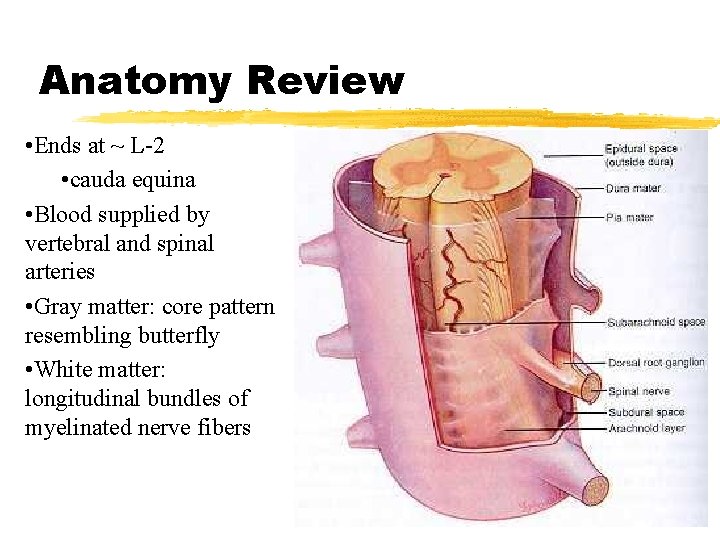
Anatomy Review • Ends at ~ L-2 • cauda equina • Blood supplied by vertebral and spinal arteries • Gray matter: core pattern resembling butterfly • White matter: longitudinal bundles of myelinated nerve fibers
Anatomy Review z Spinal Cord y. Thoracic and lumbar levels supply sympathetic nervous system fibers y. Cervical and sacral levels supply parasympathetic nervous system fibers

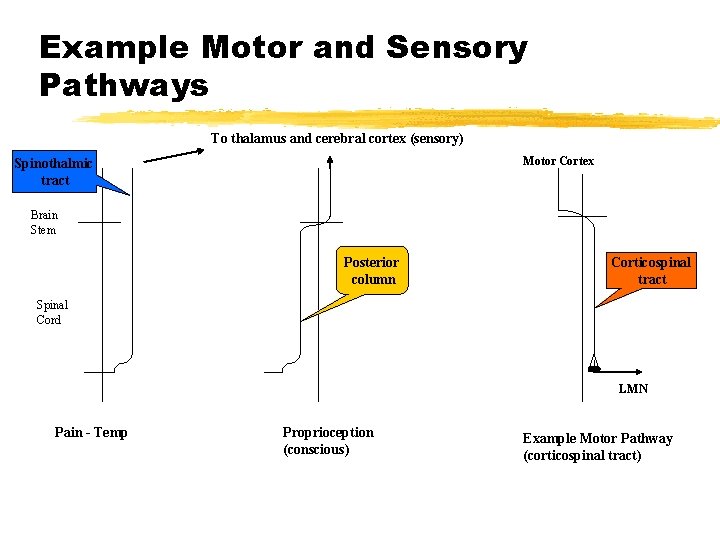
Spinal Cord Pathways z Ascending Nerve Tracts (sensory input) ycarry impulses from body structures and sensory information to the brain y. Posterior column (dorsal) xconveys nerve impulses for proprioception, discriminative touch, pressure, vibration, & two-point discrimination xcross over at the medulla from one side to the other • e. g. impulses from left side of body ascend to the right side of the brain
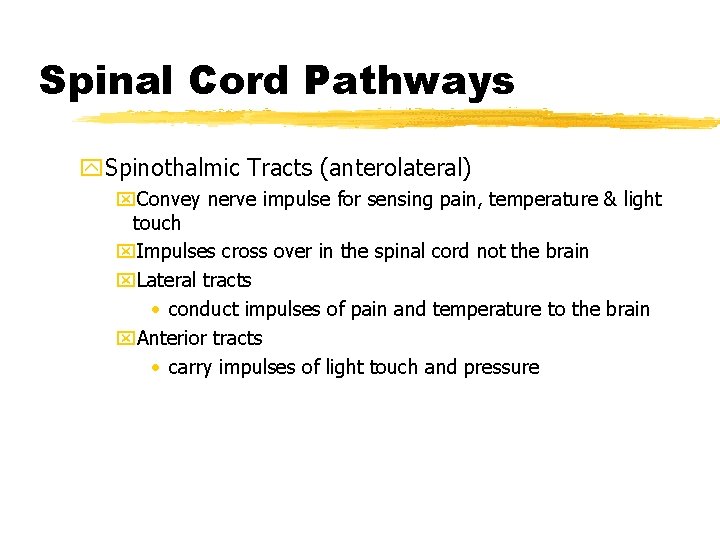
Spinal Cord Pathways y. Spinothalmic Tracts (anterolateral) x. Convey nerve impulse for sensing pain, temperature & light touch x. Impulses cross over in the spinal cord not the brain x. Lateral tracts • conduct impulses of pain and temperature to the brain x. Anterior tracts • carry impulses of light touch and pressure
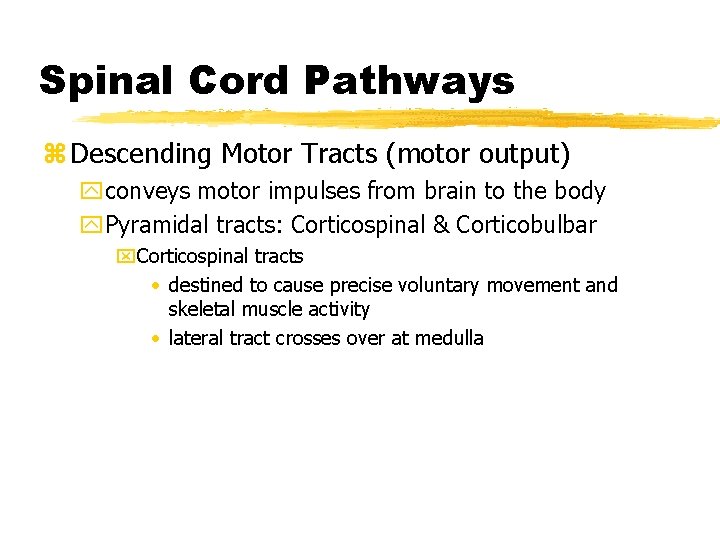
Spinal Cord Pathways z Descending Motor Tracts (motor output) yconveys motor impulses from brain to the body y. Pyramidal tracts: Corticospinal & Corticobulbar x. Corticospinal tracts • destined to cause precise voluntary movement and skeletal muscle activity • lateral tract crosses over at medulla
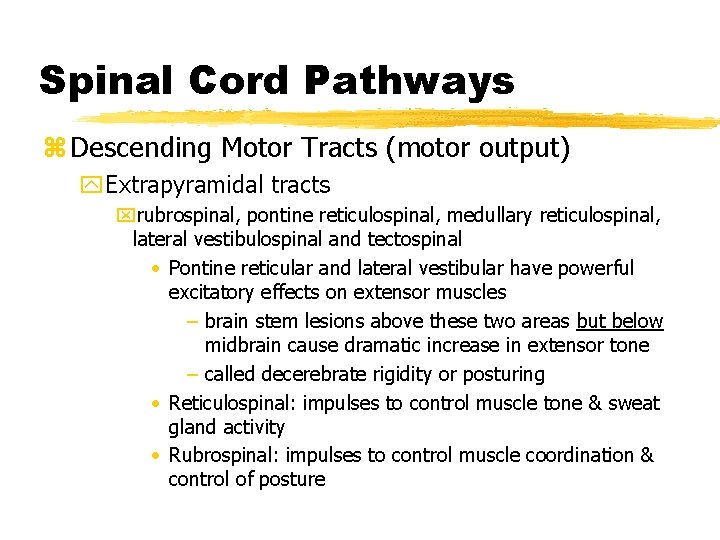
Spinal Cord Pathways z Descending Motor Tracts (motor output) y. Extrapyramidal tracts xrubrospinal, pontine reticulospinal, medullary reticulospinal, lateral vestibulospinal and tectospinal • Pontine reticular and lateral vestibular have powerful excitatory effects on extensor muscles – brain stem lesions above these two areas but below midbrain cause dramatic increase in extensor tone – called decerebrate rigidity or posturing • Reticulospinal: impulses to control muscle tone & sweat gland activity • Rubrospinal: impulses to control muscle coordination & control of posture
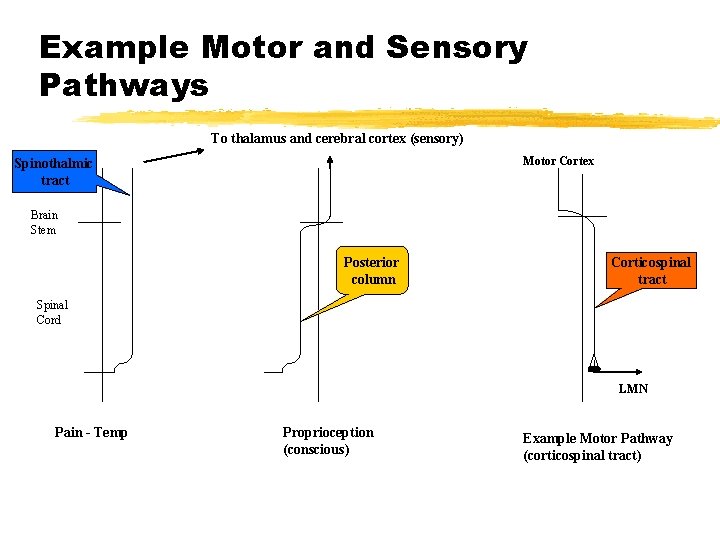
Example Motor and Sensory Pathways To thalamus and cerebral cortex (sensory) Motor Cortex Spinothalmic tract Brain Stem Posterior column Corticospinal tract Spinal Cord LMN Pain - Temp Proprioception (conscious) Example Motor Pathway (corticospinal tract)
Spinal Nerves z 31 pairs originate from the spinal cord z Carry both sensation and motor function z Named according to level of spine from where they arise y. Cervical 1 -8 y. Thoracic 1 -12 y. Lumbar 1 -5 y. Sacral 1 -5 y. Coccygeal 1
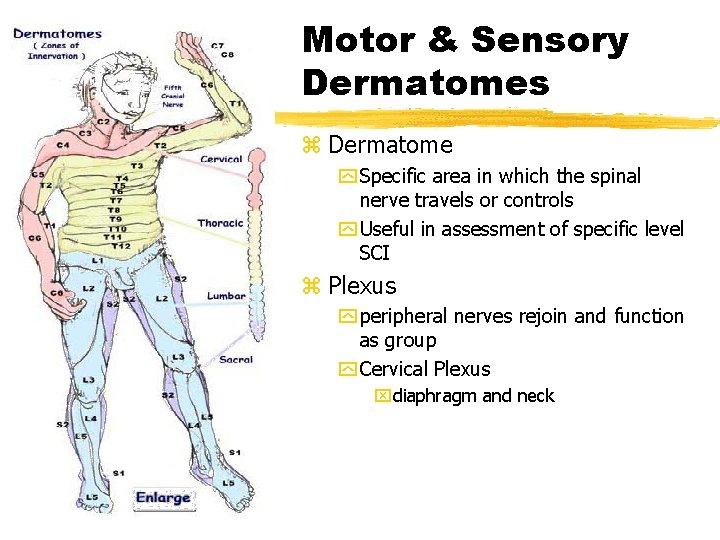
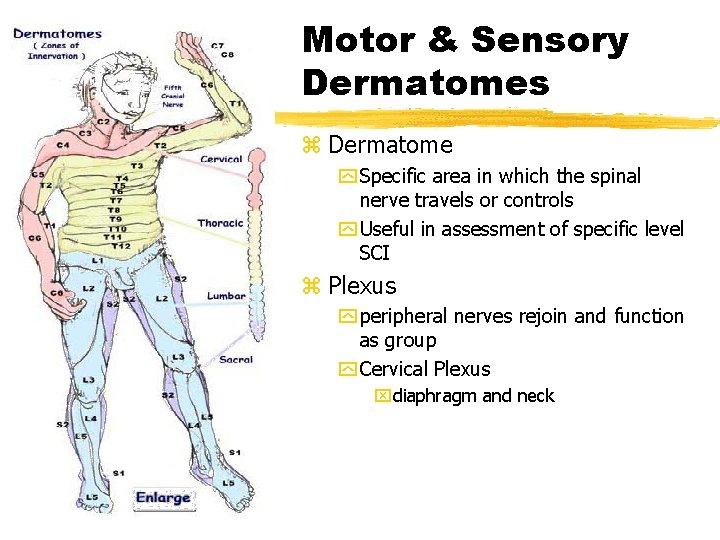
Motor & Sensory Dermatomes z Dermatome y Specific area in which the spinal nerve travels or controls y Useful in assessment of specific level SCI z Plexus y peripheral nerves rejoin and function as group y Cervical Plexus xdiaphragm and neck
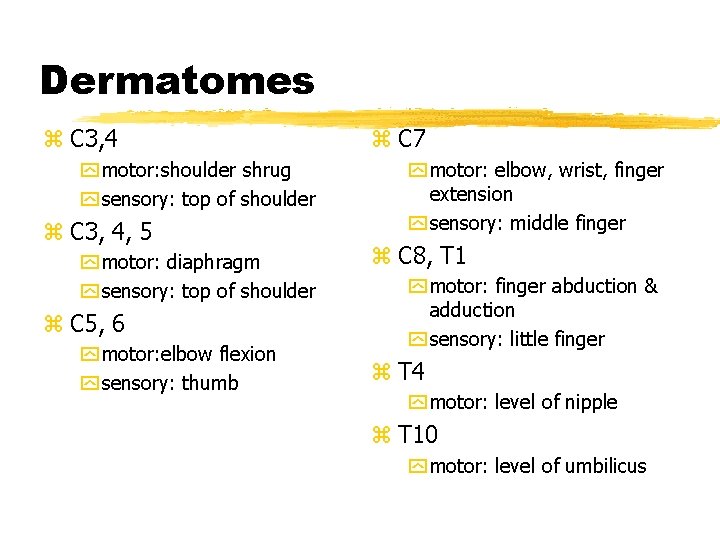
Dermatomes z C 3, 4 y motor: shoulder shrug y sensory: top of shoulder z C 3, 4, 5 y motor: diaphragm y sensory: top of shoulder z C 5, 6 y motor: elbow flexion y sensory: thumb z C 7 y motor: elbow, wrist, finger extension y sensory: middle finger z C 8, T 1 y motor: finger abduction & adduction y sensory: little finger z T 4 y motor: level of nipple z T 10 y motor: level of umbilicus
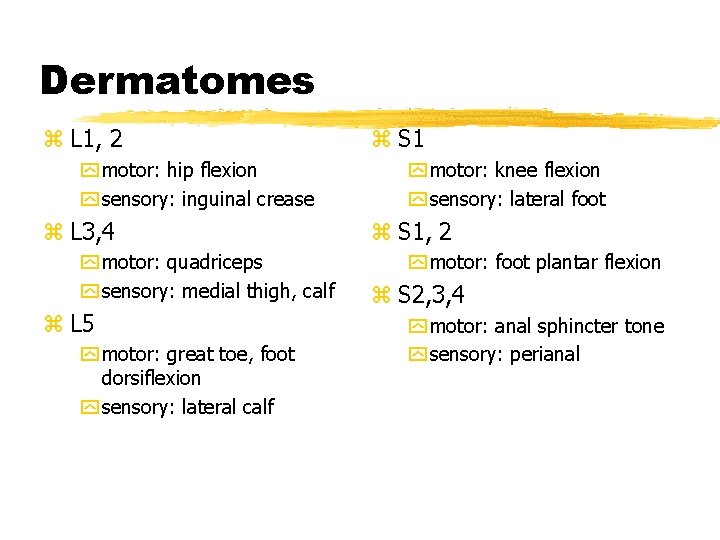
Dermatomes z L 1, 2 y motor: hip flexion y sensory: inguinal crease z L 3, 4 y motor: quadriceps y sensory: medial thigh, calf z L 5 y motor: great toe, foot dorsiflexion y sensory: lateral calf z S 1 y motor: knee flexion y sensory: lateral foot z S 1, 2 y motor: foot plantar flexion z S 2, 3, 4 y motor: anal sphincter tone y sensory: perianal
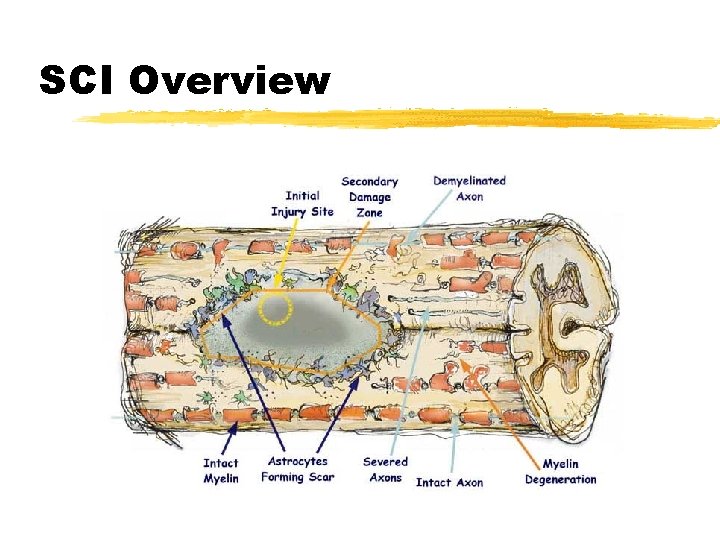
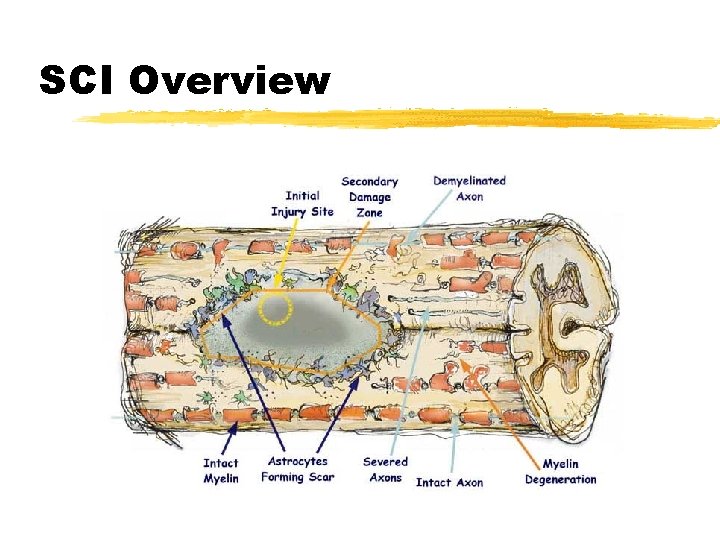
SCI Overview
Assessment of Spinal Injury z Mechanism of Injury y. No longer consider all MOIs lead to SCI x. Severe mechanism of injury is consistent with SCI x. Other MOIs don’t correlate to the risk of SCI y. ED & Field Clearance protocols now commonly used x. Exam and History findings help identify the potential SCI x. Do No Harm!
Assessment of Spinal Injury z Traditional Approach y. Based on MOI y. Emphasis on spinal immobilization in xunconscious trauma victims xpatients with a “motion” injury y. No clear clinical guidelines or specific criteria to evaluate for SCI y. Signs xpain, tenderness, painful movement xdeformity, injury over spinal area, shock xparesthesias, paresis, priapism

Assessment of Spinal Injury z Traditional Approach y. Not always practical to “immobilize” every “motion” injury y. Most suspected injuries were moved to a normal anatomical position y. No exclusion criteria used for moving patients
SCI General Assessment z Consider Mechanism of Injury & Kinematics y. Positive MOI Should Require SMR xhigh speed motor vehicle collision xfall greater than 3 times the patient’s height xviolent situations occurring near the spine • stabbing • gun shot xsports injury (with force or velocity) xconfounding factors such as osteoporosis, extreme age xother high impact, high force or high velocity conditions involving the head, spine or trunk

SCI General Assessment z Consider Mechanism of Injury & Kinematics y. Negative MOI Probably Do Not Require SMR xforce or impact does not suggest a potential spinal injury • dropped a rock on foot • twisted ankle while running • isolated musculoskeletal injury • simple fall from standing position • low speed motor vehicle collision
SCI General Assessment z ABCs y. Airway and/or Breathing impairment x. Inability to maintain airway x. Apnea x. Diaphragmatic breathing y. Cardiovascular impairment x. Neurogenic Shock x. Hypoperfusion
SCI General Assessment z Neurologic Status: y. Level of Consciousness x. Brain injury also? x. Cooperative x. No impairment (drugs, alcohol) x. Understands & Recalls events surrounding injury x. No Distracting injuries x. No difficulty in communication
SCI General Assessment z Assess Function & Sensation y. Palpate over each spinous process y. Motor function x. Shrug shoulders x. Spread fingers of both hands and keep apart with force x“Hitchhike” {T 1} x. Foot plantar flexors (gas pedal) {S 1, 2} y. Sensation (Position and Pain) xweakness, numbness, paresthesia xpain (pinprick), sharp vs dull, symmetry y. Priapism
Spinal Cord Injuries z Forces y. Direct traumatic injury xstab or gunshot directly to the spine y. Excessive Movement xacceleration xdeformation y. Directional Forces xflexion, hyperflexion xextension, hyperextension xrotational xlateral bending xvertical compression xdistraction
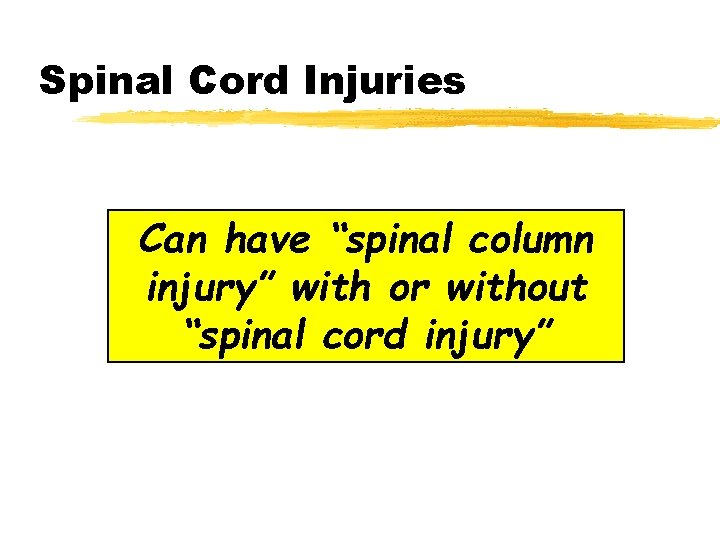
Spinal Cord Injuries Can have “spinal column injury” with or without “spinal cord injury”

Spinal Cord Injuries z Primary Injury yoccurs at the time of injury ymay result in xcord compression xdirect cord injury xinterruption in cord blood supply z Secondary Injury yoccurs after initial injury ymay result from xswelling/inflammation xischemia xmovement of body fragments
Spinal Cord Injuries z Cord concussion & Cord contusion ytemporary loss of cord-mediated function z Cord compression ydecompression required to minimize permanent injury z Laceration ypermanent injury dependent on degree of damage z Hemorrhage ymay result in local ischemia
Spinal Cord Injuries z Cord transection y. Complete xall tracts disrupted xcord mediated functions below transection are permanently lost xdetermined ~ 24 hours post injury xpossible results • quadriplegia • paraplegia
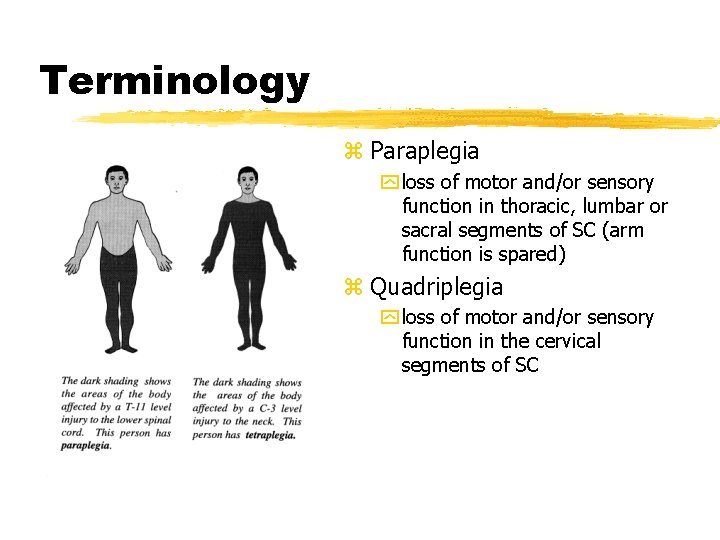
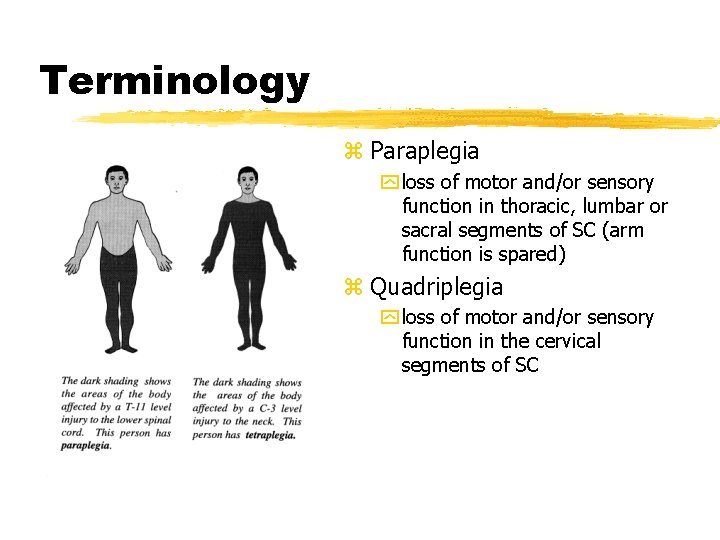
Terminology z Paraplegia y loss of motor and/or sensory function in thoracic, lumbar or sacral segments of SC (arm function is spared) z Quadriplegia y loss of motor and/or sensory function in the cervical segments of SC
Spinal Cord Injuries z Cord transection y. Incomplete xsome tracts and cord mediated functions remain intact xpotential for recovery of function x. Possible syndromes • Brown-Sequard Syndrome • Anterior Cord Syndrome • Central Cord Syndrome
Brown Sequard Syndrome z Incomplete Cord Injury y. Injury to one side of the cord (Hemisection) y. Often due to penetrating injury or vertebral dislocation y. Complete damage to all spinal tracts on affected side y. Good prognosis for recovery

Brown Sequard Syndrome z Exam Findings y. Ipsilateral loss of motor function motion, position, vibration, and light touch y. Contralateral loss of sensation to pain and temperature y. Bladder and bowel dysfunction (usually short term)
Anterior Cord Syndrome z Anterior Spinal Artery Syndrome y. Supplies the anterior 2/3 of the spinal cord to the upper thoracic region ycaused by bony fragments or pressure on spinal arteries

Anterior Cord Syndrome z Exam Findings y. Variable loss of motor function and sensitivity to pinprick and temperature yloss of motor function and sensation to pain, temperature and light touch y. Proprioception (position sense) and vibration are preserved
Central Cord Syndrome z Usually occurs with a hyperextension of the cervical region z Exam Findings yweakness or paresthesias in upper extremities but normal strength in lower extremities yvarying degree of bladder dysfunction
Cauda Equina Syndrome z Injury to nerves within the spinal cord as they exit the lumbar and sacral regions y. Usually fractures below L 2 y. Specific dysfunction depends on level of injury z Exam Findings y. Flaccid-type paralysis of lower body y. Bladder and bowel impairment

Neurogenic Shock z Temporary loss of autonomic function of the cord at the level of injury y. Usually results from cervical or high thoracic injury z Does not always involve permanent primary injury z Effects may be temporary and resolve in hours to weeks z Goal is to avoid secondary injury
Neurogenic Shock z Presentation y. Flaccid paralysis distal to injury site y. Loss of autonomic function xhypotension or relative hypotension xvasodilation xloss of bladder and bowel control xpriapism xloss of thermoregulation xwarm, pink, dry below injury site xrelative bradycardia xmay have class SNS response presentation above injury
Autonomic Hyperreflexia Syndrome z Associated with SCI patients (usually T-6 or above) some time after initial injury y. Vasculature has adapted to loss of sympathetic tone y. Blood pressure normalized y. No vasodilation response to increased BP z ANA reflexively responds with arteriolar spasm yincreased BP ystimulates PNS yresults in bradycardia yperipheral and visceral vessels unable to dilate
Autonomic Hyperreflexia Syndrome z Presentation y. Paroxysmal hypertension, possible extreme yheadache yblurred vision ysweating and flushed skin above level of injury yincreased nasal congestion ynausea ybradycardia ydistended bladder or rectum
Non-Traumatic Conditions z Low Back Pain (LBP) y 60 -90% of population experience some form of LBP y. Very small number due to sciatica (lumbar nerve root) y. Most causes can not be specifically diagnosed y. Risk Factors xrepetitious lifting or straining xchronic exposure to vibration (e. g. vehicle) xosteoporosis xage
Non-Traumatic Conditions z Low Back Pain (LBP) y. Causes xtumor xprolapsed disk xbursitis xdegenerative joint disease xproblems with spinal mobility xinflammation caused by infection xfractures xligament strains
Non-Traumatic Conditions z Low Back Pain (LBP) y. Degenerative Disk disease xcommon over 50 years of age xnarrowing of the disk xbiochemical alterations of intervertebral disk y. Herniated intervertebral Disk xtear in the posterior rim of capsule enclosing the gelatinous center of the disk xtrauma, degenerative disk disease, improper lifting xcommonly affects L-5, S-1 and L-4, L-5 disks

Management of SCI z Primary Goal y. Prevent secondary injury z Stabilization of the spine begins in the initial assessment y. Treat the spine as a long bone x. Secure joint above and below y. Caution with “partial” spine splinting x. Dr. Robert’s Rule: All or None z Immobilization vs Motion Restriction
Management of SCI z Neutral positioning of head and neck if at all possible yallows for the most space for cord ymost stable position for spinal column ydon’t force it
Management of SCI z Cervical Motion Restriction y. Manual method y. Rigid collar comes later y. Interim device (KED) y. Move to long board or full body vacuum splint y. Manual continues until trunk and head secured y“CID” x. Don’t use sand bags or IV fluid bags as head blocks x. Tape works wonders! x. Improvise with blanket rolls
Management of SCI z Don’t forget the Padding y. Maintains anatomical position y. Limits movement on board xespecially during transport on board or in vehicle yfill all the voids xcurvature of the lower back is normal - fill it xpillows, blankets, towels x. Tape along (even duct tape) is not enough
Management of SCI z Securing to the Board y. Straps, Tape, Cravats, whatever y. Torso first xthen legs and feet and head y. Even patients extricated with a KED are secured to the board

Management of SCI z Pediatric Patient Considerations y. Elevate the entire torso if large occiput x. Pad underneath x. Short board underneath x. Vacuum mattress y. Lots of voids to fill y. Difficult to find a correctly sized rigid collar x. Improvise with • horse collar • blanket or towel rolls

Management of SCI z Helmeted Patients y. Removal should be limited to emergent need for access to airway and ventilation y. Leave in place if xgood fit with little or no head movement within xno impending airway or breathing problems xcan perform spinal motion restriction with helmet on xno interference in airway assessment or management xno cardiac arrest

Management of SCI z Helmeted Patients y. Types of Helmets x. Sports (football, hockey) • Shoulder pads and helmet go together x. Racing (motorcycle, car racer) x. Recreational (motorcycle, bicycle) y. Various helmets create different problems for patient and for removal
Management of SCI z General y. Manual Spinal Motion Restriction y. ABCs x. Increase Fi. O 2 x. Assist ventilations prn x. IV Access & fluids titrated to BP ~ 90 -100 mm Hg y. Consider High Dose methylprednisolone [Solu. Medrol]: 30 mg/kg bolus over 15 mins then infusion after 1 st hour y. Look for other injuries: “Life over Limb” y. Transport to appropriate SCI center
Clearing Protocols z Spinal Clearance y First initiated in Maine with a state-wide protocol y Now much more common in US z Current Practice y Assess scene and MOI y Assess neuro status y Immobilize x. Most MOIs x. Prevent further injury x. CYA x. No 100% method to rule out in the field xfear of litigation xdevastating consequences possible
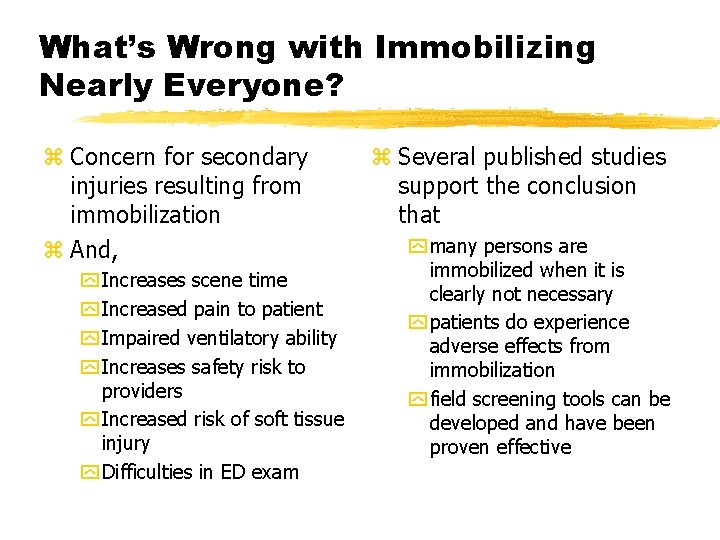
What’s Wrong with Immobilizing Nearly Everyone? z Concern for secondary injuries resulting from immobilization z And, y Increases scene time y Increased pain to patient y Impaired ventilatory ability y Increases safety risk to providers y Increased risk of soft tissue injury y Difficulties in ED exam z Several published studies support the conclusion that y many persons are immobilized when it is clearly not necessary y patients do experience adverse effects from immobilization y field screening tools can be developed and have been proven effective
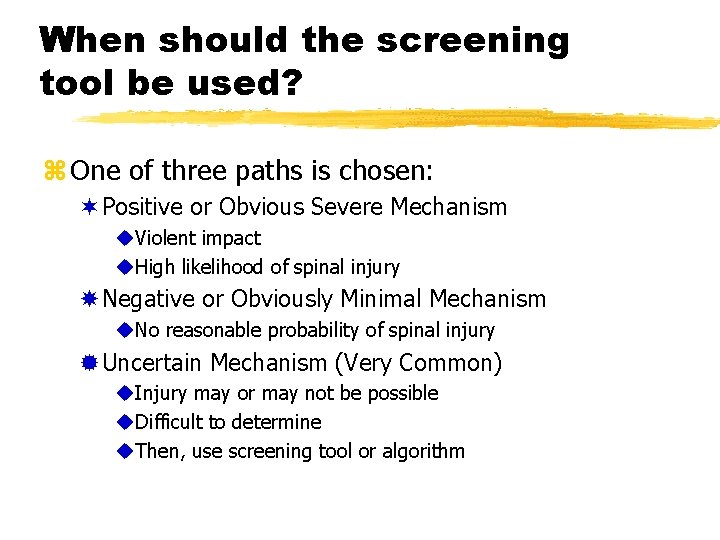
When should the screening tool be used? z One of three paths is chosen: ¬Positive or Obvious Severe Mechanism u. Violent impact u. High likelihood of spinal injury Negative or Obviously Minimal Mechanism u. No reasonable probability of spinal injury ®Uncertain Mechanism (Very Common) u. Injury may or may not be possible u. Difficult to determine u. Then, use screening tool or algorithm
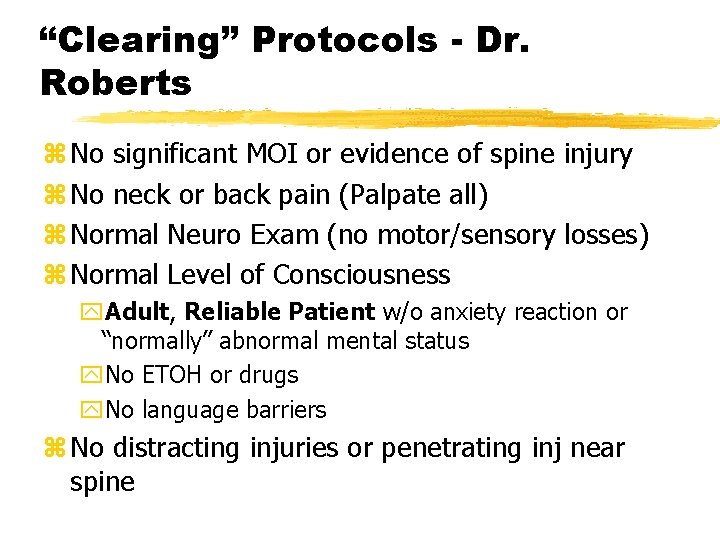
“Clearing” Protocols - Dr. Roberts z No significant MOI or evidence of spine injury z No neck or back pain (Palpate all) z Normal Neuro Exam (no motor/sensory losses) z Normal Level of Consciousness y. Adult, Reliable Patient w/o anxiety reaction or “normally” abnormal mental status y. No ETOH or drugs y. No language barriers z No distracting injuries or penetrating inj near spine
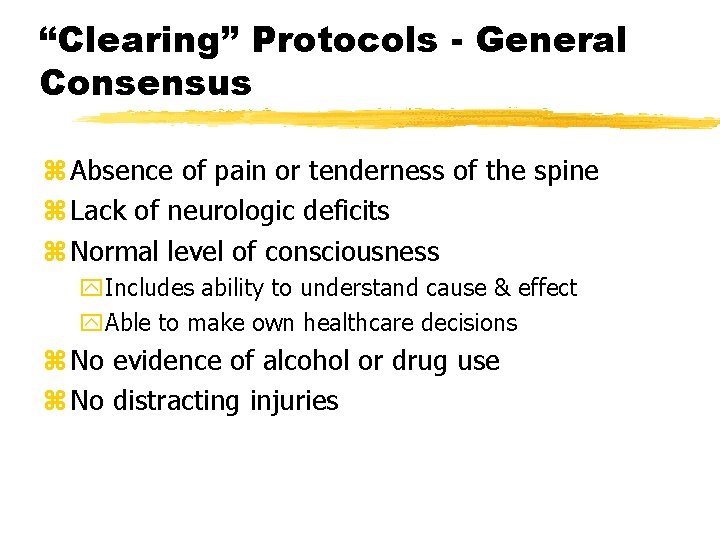
“Clearing” Protocols - General Consensus z Absence of pain or tenderness of the spine z Lack of neurologic deficits z Normal level of consciousness y. Includes ability to understand cause & effect y. Able to make own healthcare decisions z No evidence of alcohol or drug use z No distracting injuries
Other Topics z Rapid Extrication z Log Roll yposition of the arms z Diving Incidents