Specific learning objectives Classify hypoxia and Explain each
Specific learning objectives • Classify hypoxia and Explain each type with examples. • Cyanosis. • Artificial respiration.
Hypoxia Oxygen deficiency at tissue level is known as hypoxia
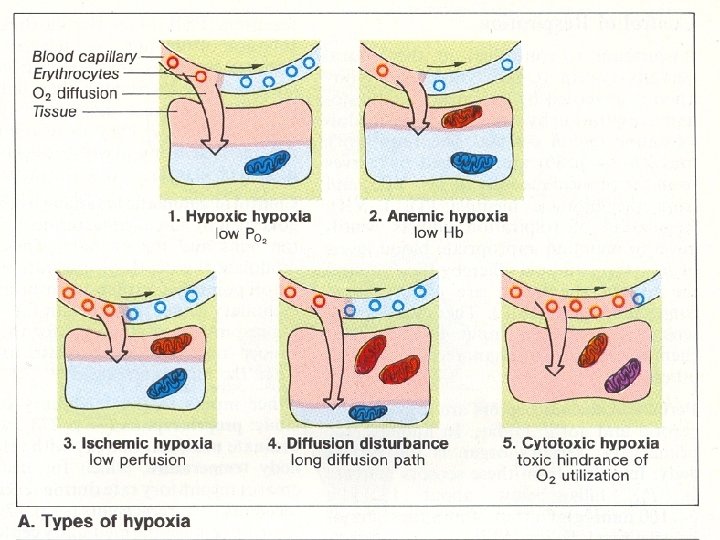
O 2 deficiency occurs at tissue level due to -either due to • Decrease O 2 content in the blood –which may be due to • (1) Decrease O 2 tension in arterial blood • (2) Decrease O 2 carrying capacity of blood Or • Decrease O 2 supply by decrease blood flow Or • Decrease O 2 utilization by the tissue
Specific learning objectives • After the End of this chapter students should able to: • List the types of hypoxia • Define cyanosis • Uses of artificial respiration.
Classification of hypoxia 1. Hypoxic hypoxia or Arterial hypoxia 2. Anemic hypoxia 3. Stagnant hypoxia or Ischemic hypoxia or Hypo kinetic hypoxia 4. Histotoxic hypoxia
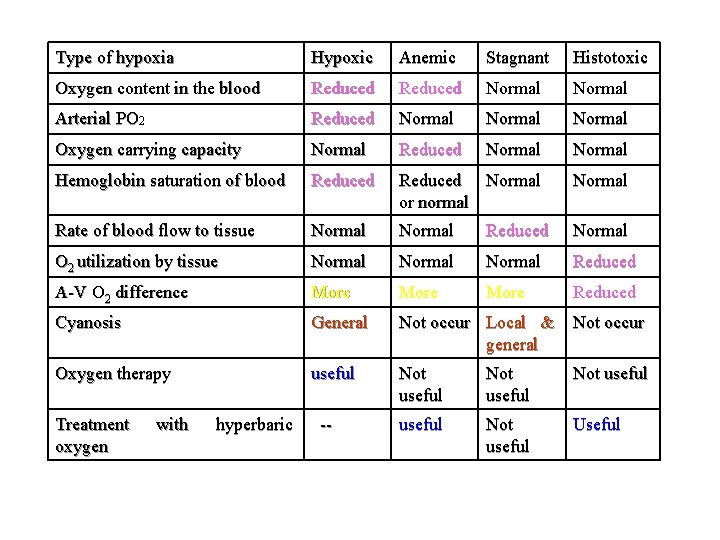
Type of hypoxia Hypoxic Anemic Stagnant Histotoxic Oxygen content in the blood Reduced Normal Arterial PO 2 Reduced Normal Oxygen carrying capacity Normal Reduced Normal Hemoglobin saturation of blood Reduced Normal or normal Normal Rate of blood flow to tissue Normal Reduced Normal O 2 utilization by tissue Normal Reduced A-V O 2 difference More Reduced Cyanosis General Not occur Local & general Not occur Oxygen therapy useful Not useful Useful Treatment oxygen with hyperbaric --
Hypoxic hypoxia • Seen in – • Physiological condition – High altitude (alveolar PO 2 is decreased) • Pathological condition – Cardio-respiratory diseases (O 2 diffusion capacity is decreased)
• As altitude increases the partial pressure (Pa. O 2) decreases (Dalton’s Law) • As the Pa. O 2 falls in the alveoli, the amount of O 2 which diffuses into the blood decreases (Henry’s Law) • Results in a decrease in oxygen available to the tissues
• Low PAO 2 due to the atmosphere • Hypoventilation – PCO 2 is rising • Diffusion Defects • The Pa. O 2 will be lower in all cases, but the PCO 2 may or may not be increased. • Treatment: Compensatory actions to reduce inequalities, supplemental oxygen
• • Low po 2 in inspired air Hypoventilation Diffusion defect V-p mismatch
Anemic hypoxia • Seen in • Anemia –only in severe anemia; where Hb deficiency is marked (because in hypoxic condition increase 2, 3 -DPG level shift O 2 dissociation curve to right) • Carbon-monoxide poisoning.
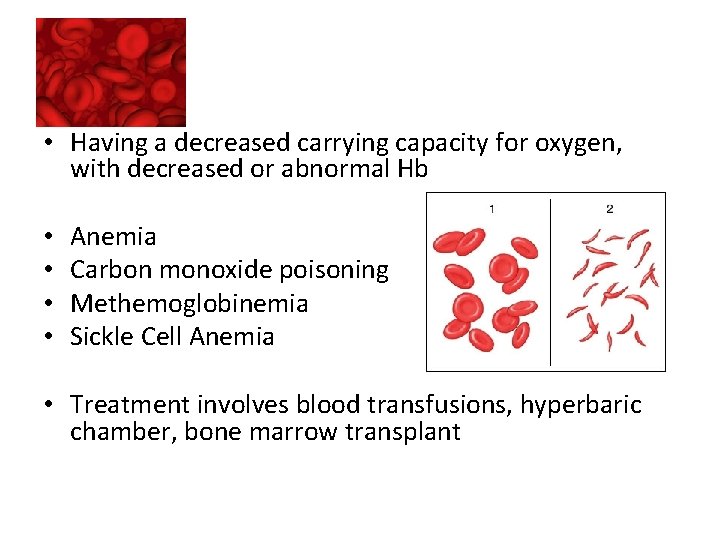
• Having a decreased carrying capacity for oxygen, with decreased or abnormal Hb • • Anemia Carbon monoxide poisoning Methemoglobinemia Sickle Cell Anemia • Treatment involves blood transfusions, hyperbaric chamber, bone marrow transplant
CO poisoning • • CO has 200 times more affinity to Hb than O 2. CO with Hb is Carboxyhemoglobin (COHb) COHb is cherry red color COHb cannot take O 2 & liberation of CO from Hb also is slow Also COHb shifts remaining Hb. O 2 shift to left Hyperventilation is absent as arterial PO 2 is normal—no peripheral chemoreceptor drive Symptoms –like other hypoxia –headache, nausea etc. Hyperbaric O 2 therapy is useful
Stagnant hypoxia • Due to slowing of circulation • Local –vasoconstriction due to cold or obstruction to venous outflow; & peripheral circulatory failure • General – cardiac failure
• A decrease in cardiac output results in a low BP and a prolonged systemic transit time • The Pa. O 2 can be high, but because of the time it takes to get to the tissues, the pt is hypoxic • Cardiovascular instability or failure • Shock • Arrhythmias • Treatment include increasing cardiac output with use of cardiovascular drugs and therapy, supplemental oxygen
Histotoxic Hypoxia • Inability for tissues to utilize oxygen available • Cyanide Poisoning will inhibit cellular metabolism from occuring; the cells can not process the O 2 • Treatment: Reversal of poisoning, supplemental oxygen and/or ventilation
• Seen in cyanide poisoning • Cyanide inhibit cytochrome oxidase & other iron containing enzymes • Treatment –Administration of methylene blue or nitrates (oxidizing agents) • –oxidized Hb to methemoglobin which react with cyanide to form cyanmethemoglobin, a non-toxic compound • Hyperbaric O 2 therapy is useful
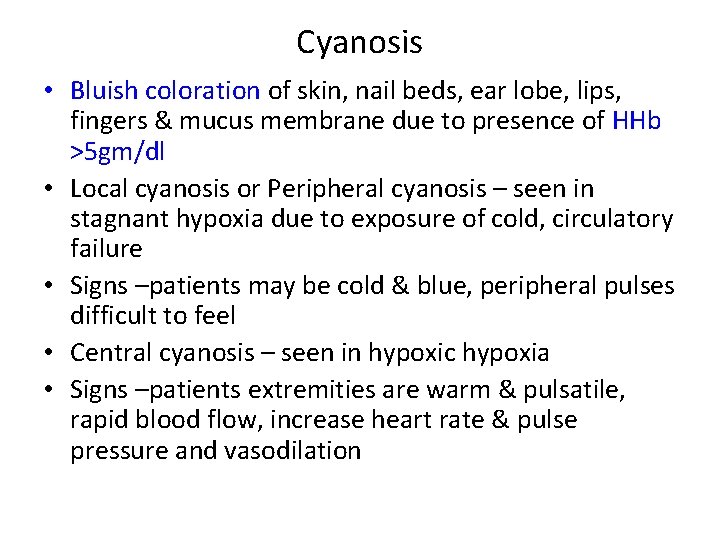
Cyanosis • Bluish coloration of skin, nail beds, ear lobe, lips, fingers & mucus membrane due to presence of HHb >5 gm/dl • Local cyanosis or Peripheral cyanosis – seen in stagnant hypoxia due to exposure of cold, circulatory failure • Signs –patients may be cold & blue, peripheral pulses difficult to feel • Central cyanosis – seen in hypoxic hypoxia • Signs –patients extremities are warm & pulsatile, rapid blood flow, increase heart rate & pulse pressure and vasodilation
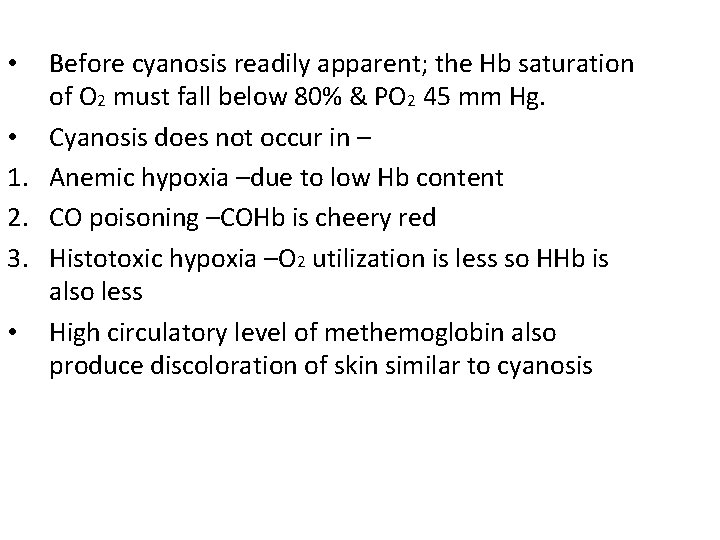
Before cyanosis readily apparent; the Hb saturation of O 2 must fall below 80% & PO 2 45 mm Hg. • Cyanosis does not occur in – 1. Anemic hypoxia –due to low Hb content 2. CO poisoning –COHb is cheery red 3. Histotoxic hypoxia –O 2 utilization is less so HHb is also less • High circulatory level of methemoglobin also produce discoloration of skin similar to cyanosis •
O 2 therapy • • • Useful in treatment of Hypoxic hypoxia (except in shunt condition) Cyanosis Only limited value in treatment of – Anemic, Stagnant & Histotoxic hypoxia
Asphyxia • Existence of acute hypercapnia & hypoxia together due to closed airway breathing • Leads to improper aeration of blood • Occur in – • Drowning • Hanging • Pneumothorax
Effect of asphyxia Stage 1 –Stage of hyperpnoea – duration 1 min Features – Rate & depth of respiration increased Respiratory efforts are Violent Dyspnea results Initially both inspiratory & expiratory movements are increased • Later expiratory movements are more pronounced • Unconsciousness marked end of this stage • Cause –due to hypercapnea • •
• Stage 2 –Stage of central excitation – • duration 1 to 2 minutes • Expiratory movements are still more pronounced with each expiration, the whole body enters into convulsion • Saliva secretion & vomiting occurs • Blood p. H decreases –acidosis (accumulation of lactic acid due to convulsion) • Increased wide spread sympathetic stimulation • Signs of central excitations appear – such as • Increase heart rate & BP; • Pupillary constriction (myosis) • Exaggeration of reflexes • Cause –hypercapnia, hypoxia & acidosis
• • Stage 3 –Stage of central depression Duration 2 to 3 minutes Expiratory convulsion ceased Replaced by slow deep spasmodic inspiration – individuals stretches out & open mouth wide as if gasping for breath (gasping type of breathing) Signs of central depression appear – Pupillary dilation (mydriasis) Abolition of reflexes Decreased HR & BP and vasodilation
• As this stage is progressed interval between successive gasping longer • Cause –direct hypoxic effect on respiratory & other brain centers which is depressive. • Asphyxiated victim can still be saved by artificial respiration • Victim may develop ventricular fibrillation due to hypoxic myocardial damage & high circulatory catecholamine • If artificial respiration is not started – • At the end of 4 to 5 minutes of stage 3, the victim dies.
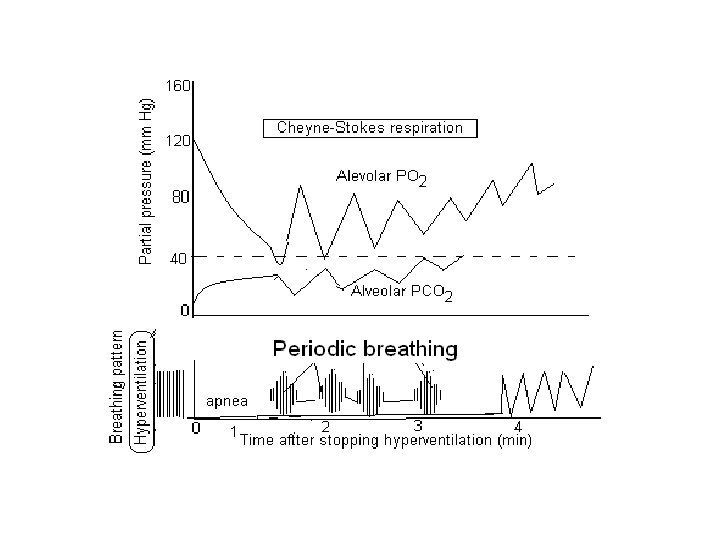
Periodic breathing • When breathing is non-rhythmic & irregular, it is said to be periodic breathing • Two types • Cheyne-Stoke breathing –Regularly irregular type of periodic breathing • Biot’s breathing –Irregularly irregular type of periodic breathing
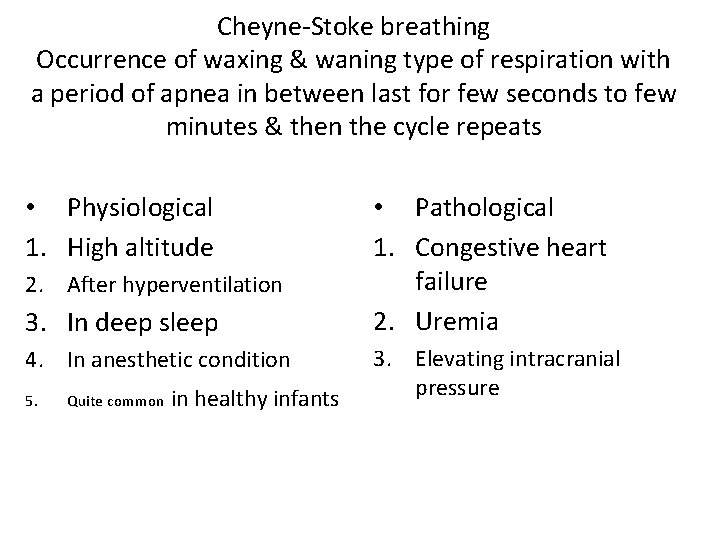
Cheyne-Stoke breathing Occurrence of waxing & waning type of respiration with a period of apnea in between last for few seconds to few minutes & then the cycle repeats • Physiological 1. High altitude 2. After hyperventilation 3. In deep sleep 4. In anesthetic condition 5. Quite common in healthy infants • Pathological 1. Congestive heart failure 2. Uremia 3. Elevating intracranial pressure
Biot’s breathing • Varying breathing time alternate with apnoeic periods of different lengths • Transition from periods of activity to apnea & back are abrupt • Occurs only in pathological conditions affect CNS –such as meningitis
Respiratory adjustment to High Altitude, Deep Sea Diving & Exercise
Effect of High Altitude • High Altitude : – Mountain climbing – Aviation – Space vehicles
Effect of High Altitude • Atmospheric (Barometric) pressure : progressively declines as altitude increases. • Height above 10, 000 feet (3000 mts) above sea level. • The effects are same as hypoxic hypoxia. • Rate at which hypoxia depends upon • Rapid ascent • And slow ascent. • Hazards • Pulmonary edema • Degree of hypoxia –severe • Compensatory mechanism-nil
• At any altitude above 10000 feet arterial PO 2 falls into steep proportion of the O 2 -Hb curve. • As a result % saturation of Hb in arterial blood declines resulting in hypoxia. • So people who rapidly ascend to high altitudes of 10000 ft or more experience symptoms of acute mountain sickness attributable to hypoxic hypoxia
Acclimatization • Physiological readjustments and compensatory mechanisms that reduce the effect of hypoxia.
Acute mountain sickness: �is due to hypoxic hypoxia �This syndrome develops 8 -24 hours after arrival at altitude and lasts 4 -8 days �Whenever arterial PO 2 reaches below 60 mmhg it stimulate peripheral chemoreceptors which leads to increase respiratory rate ( hyperventilation) �As a consequence arterial PCO 2 decreases producing respiratory alkalosis. �Symptoms: fatigue , headache , nausea , loss of appetite, difficulty of breathing & rapid heart rate & nerve dysfunction , Dizziness & incoordination. & unacclimatized person may land in coma followed by death
�Acclimatization to low PO 2: �People remaining at high altitude for days or week or years become acclimatized to low PO 2 �Acclimatization is due to compensatory responses that occurs in body �Acute compensatory response �Long term compensatory responses
Acute compensatory response – Increase pulmonary ventilation – Increase cardiac out put Long term compensatory responses – increase red blood cells – Increase 2, 3 DPG (RBC) – Increase no capillaries with in the tissues – Increase mitochondria in tissue cells – Kidney restores the arterial p. H towards normal by conserving H ions
Decompression sickness : – Reduction in partial pressure of nitrogen causes N 2 to quickly come out of the solution & form bubbles in the body – Decompression sickness or “bends” because victim often bends over because of joint or muscle pain. – Bubbles in pulmonary capillaries are apparently responsible for dyspnoea -"chokes”.
Decompression sickness Dysbarism Caission disease Bends • Symptoms takes place to a diver, if he ascends rapidly from underwater to surface • In underwater breathing, due to high pressure, volume of gas equilibration (content) in body fluid & tissue is more. • In surface, as pressure is normal, excess gas equilibrates at high pressure begins to come out as bubbles.
• Small bubbles –no physiological disturbance • Formation of large bubbles (if ascends rapidly) –which when, • Coming out in the region of joints –Bends –pain around joints • Enter in pulmonary circulation –Chokes –a feeling of shortness of breath often accompanying cough • Enter coronary circulation –myocardial damage –heart attack • Enter in cerebral circulation –leads to neurological symptoms such as --

Effect of deep sea diving • Symptoms of decompression sickness : – nervous symptoms occurs ranging from dizziness, paralysis , unconsciousness – Occasionally pulmonary edema & death can also occur – O 2 toxicity(super oxide free radicals) caused by Increase in PO 2 is another possible harmful effect of deep sea diving
• Treatment of this disease is prompt recompression in a pressure chamber, followed by slow decompression. Recompression is frequently lifesaving.
• • Neurological symptoms are – Parenthesis Itching Deafness Impaired vision Vestibular disturbance Even stroke (Diver’s paralysis) In extreme case patient may collapse & die
• Prevention – • Slow ascends enough to prevent bubbles from being unduly large • Wearing SCUBA gear (Self-Contained Underwater Breathing Apparatus) • Treatment – • Recompression in a pressure chamber followed by slow decompression • Note – Half-time for elimination of N 2 – From blood is 2 minutes; from muscle 20 minutes & from fat 60 minutes.
Nitrogen narcosis : – At sea level N 2 is poorly soluble in tissue fluid. But the high PN 2 that occurs in deep sea diving causes more of the N 2 than normal to dissolve that leads to N 2 narcosis Causes: 1. Fat depot 2. Diver's palsy 3. Chokes 4. Bends Treatment : Compression chamber High pressure nervous syndrome Scuba diving
• Treatment of this disease is prompt recompression in a pressure chamber, followed by slow decompression. Recompression is frequently lifesaving.
Methods of artificial respiration • I. Manual methods & • II. Instrumental methods
• The purpose of giving artificial respiration is - • To maintain the gaseous interchange, the vitality of the nerve centers, as well as that of the heart. • It also helps to maintain circulation. • It is expected that after sometime, the respiratory centers will start functioning spontaneously. • During artificial respiration, the alternate inflation and deflation of lungs reflex stimulate the respiratory centers, and revived the spontaneous respiration
Instrumental methods • Negative pressure breathing method – • By alternately compressing and relaxing the chest wall – • Drinker’s method • Bragg-Paul’s method • Positive-pressure breathing – • By introducing air or oxygen directly into the lungs – • Continuous inflation method • Intermittent inflation method
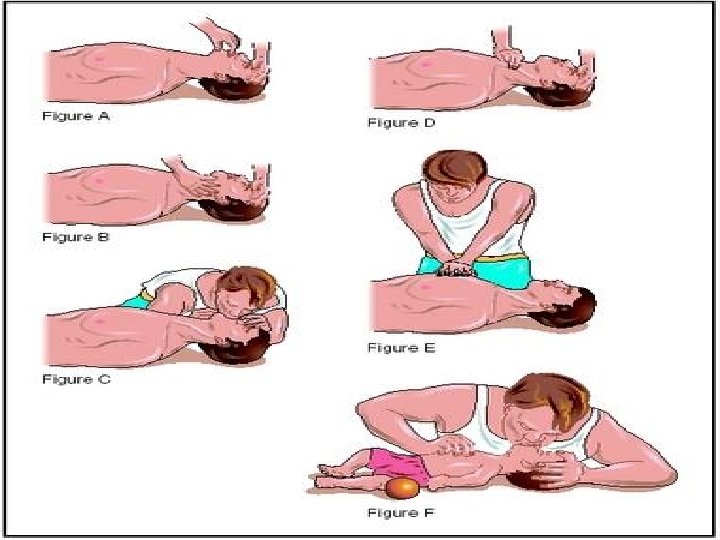
Manual methods • The different types of manual methods are-1. Schafer’s method- Subject in prone position; Head tilted side; Operator-side by 2. Holger-Nielsen method (Arm-lift back pressure method) –Subject in prone position, hands folded rested under head; Operator –head end 3. Sylvester’s method —subject in supine position, Operator at head end 4. Mouth-to-mouth method –better than others 5. Eve’s rocking method
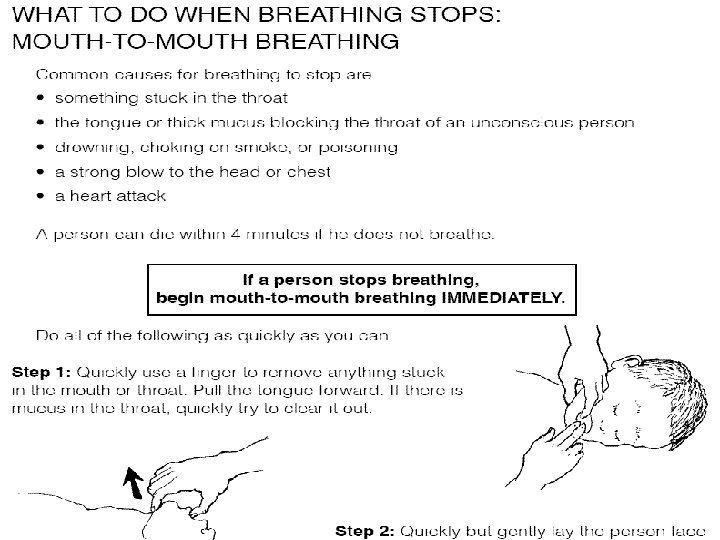
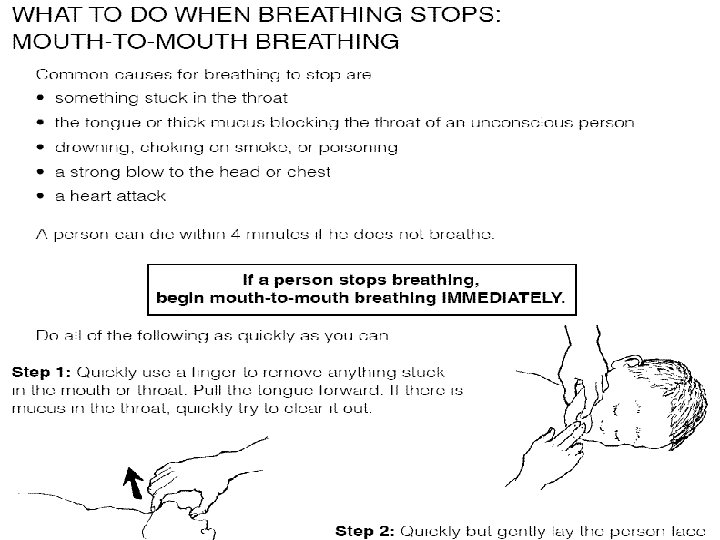
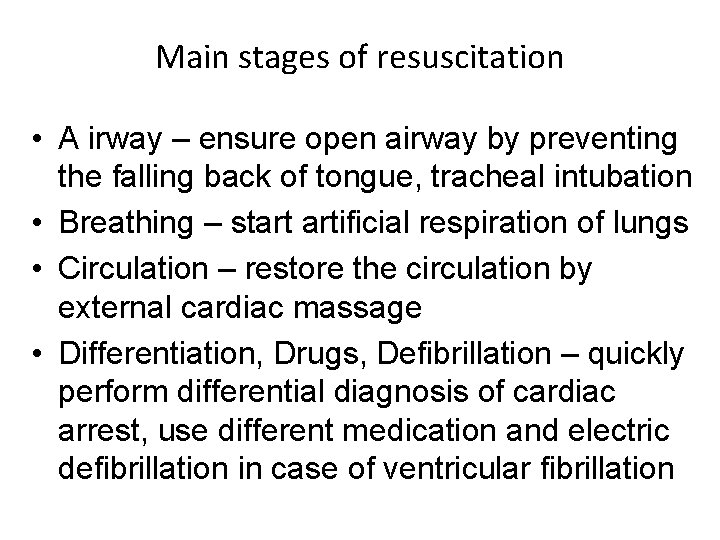
Main stages of resuscitation • A irway – ensure open airway by preventing the falling back of tongue, tracheal intubation • Breathing – start artificial respiration of lungs • Circulation – restore the circulation by external cardiac massage • Differentiation, Drugs, Defibrillation – quickly perform differential diagnosis of cardiac arrest, use different medication and electric defibrillation in case of ventricular fibrillation
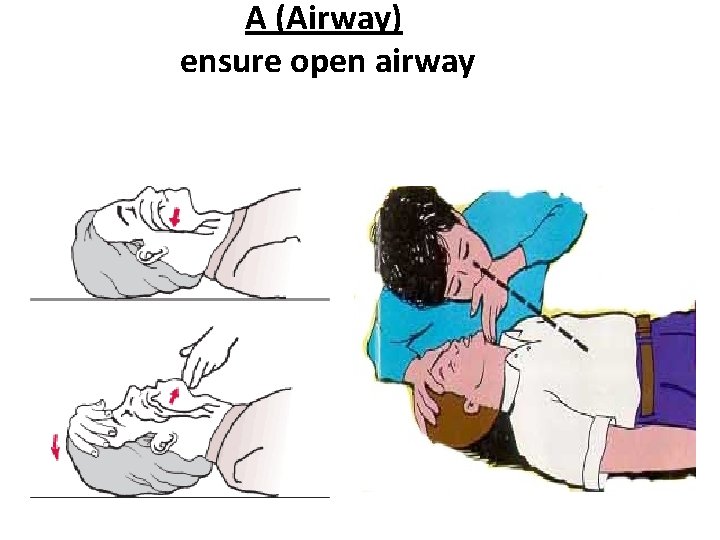
A (Airway) ensure open airway
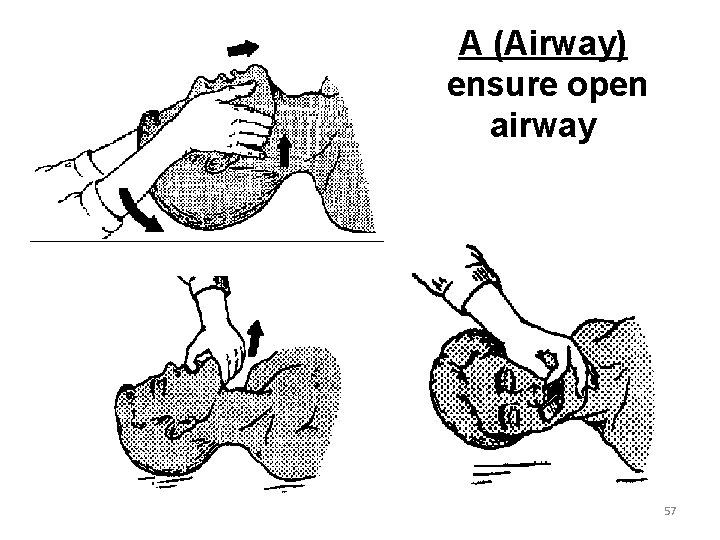
A (Airway) ensure open airway 57
- Slides: 57