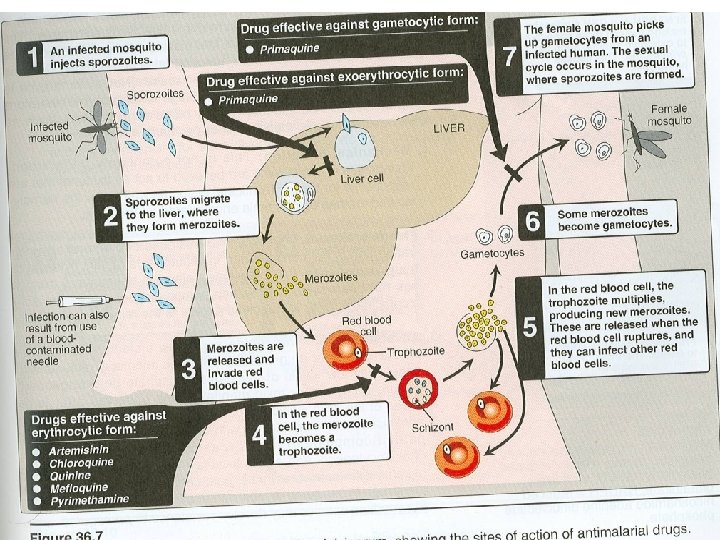
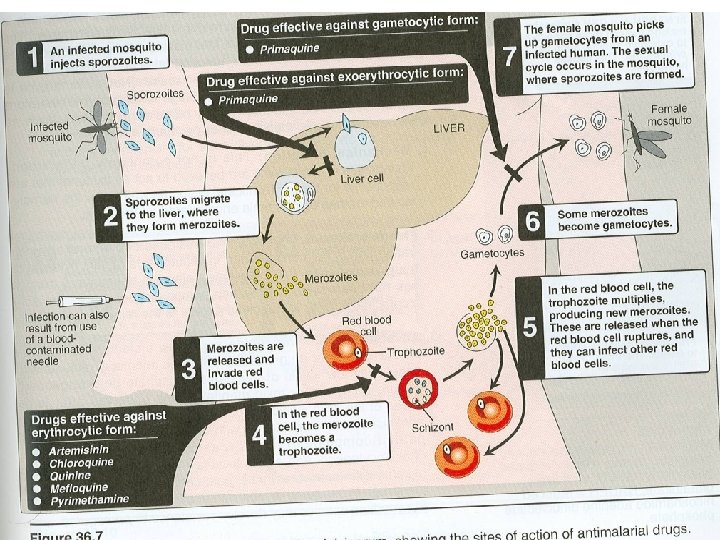
Species of plasmodium Clinical features and complications Lifecycle
![Derived from the herb qing haosu [Artemisia]. Artemisinin is poorly soluble in water & Derived from the herb qing haosu [Artemisia]. Artemisinin is poorly soluble in water &](https://slidetodoc.com/presentation_image_h/15ec7b7b7d76765e0e82a599f27f15ce/image-49.jpg)
![Artesunate[a water- soluble derivative], artemether & artether[synthetic analogues] have higher activity & are better Artesunate[a water- soluble derivative], artemether & artether[synthetic analogues] have higher activity & are better](https://slidetodoc.com/presentation_image_h/15ec7b7b7d76765e0e82a599f27f15ce/image-50.jpg)


- Slides: 68
Species of plasmodium. Clinical features and complications. Life-cycle of plasmodium. Classification of antimalarial drugs. Individual drugs.
Each year, it causes disease in approximately 650 million people and kills between one and three million.
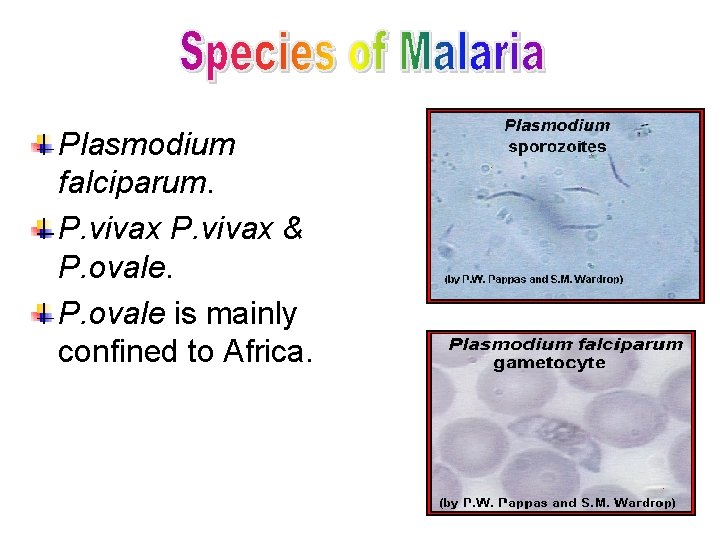
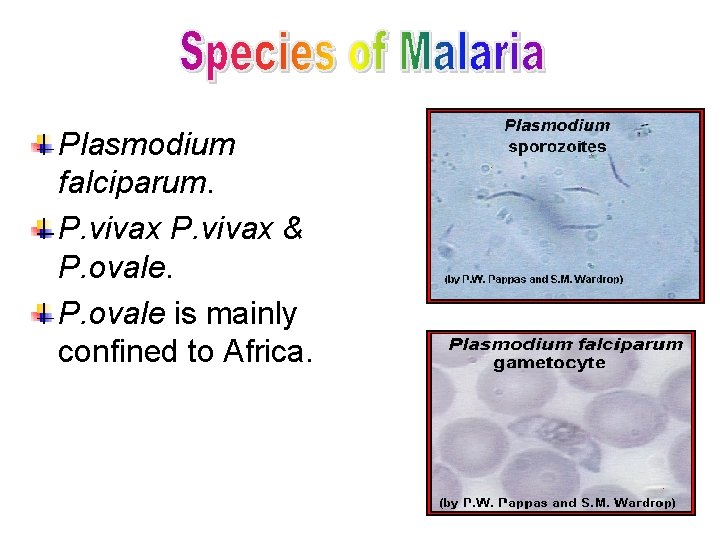
Plasmodium falciparum. P. vivax & P. ovale is mainly confined to Africa.
Acute falicparum malaria is potentially fatal. Symptoms of malaria.
Complications: -. Chronic repeated infection.
Quiz? • One cycle of liver invasion and multiplication: • A) P vivax B) P falciparum C) P. malariae D) P ovale
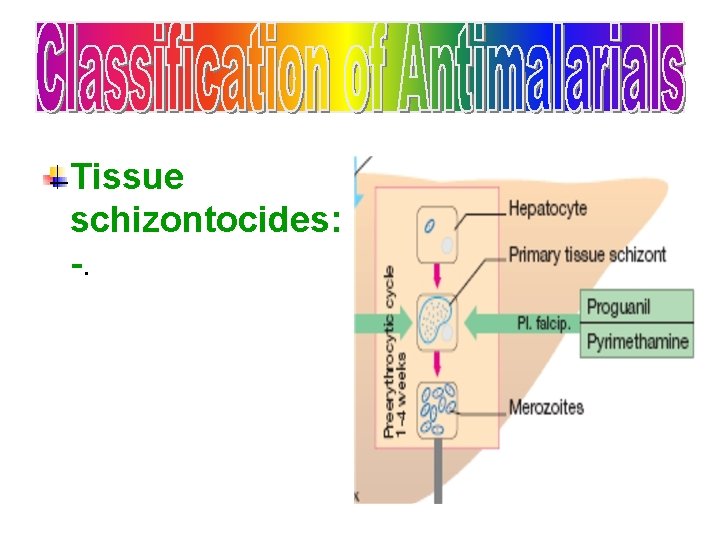
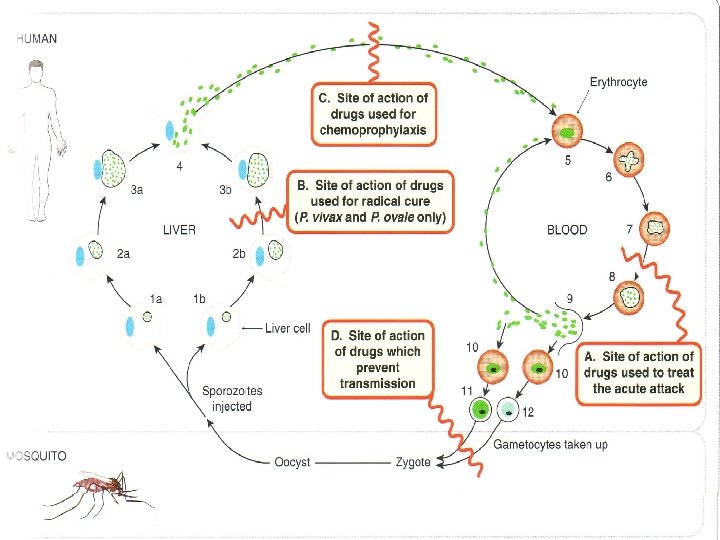
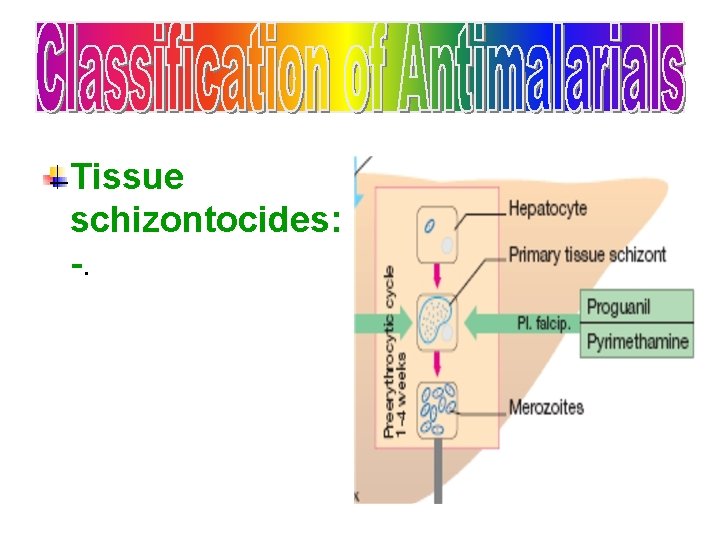
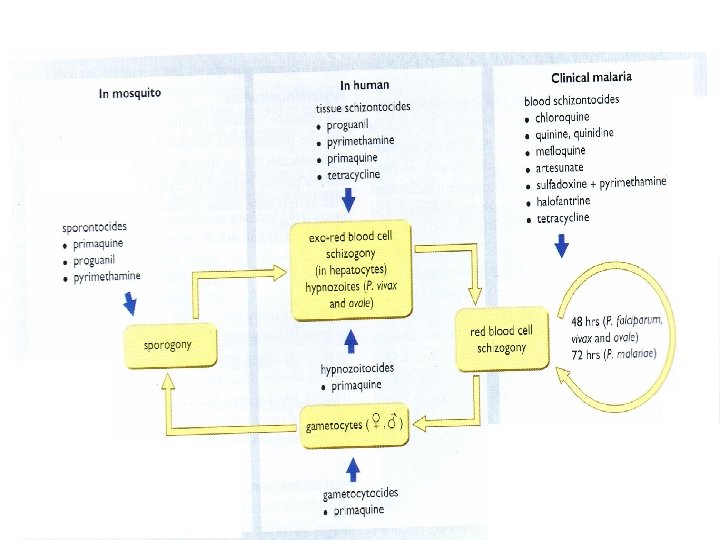
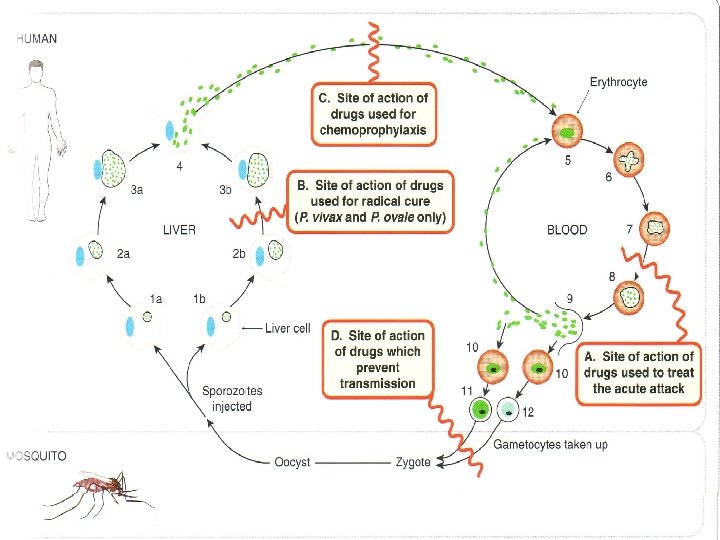
Tissue schizontocides: -.
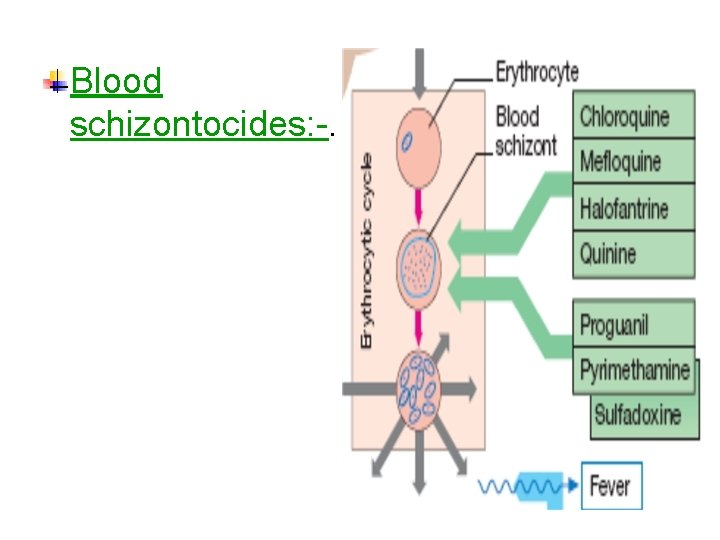
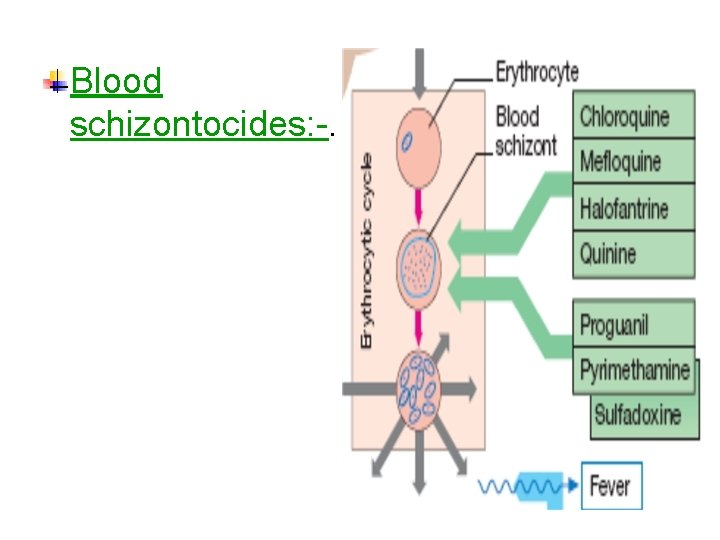
Blood schizontocides: -.
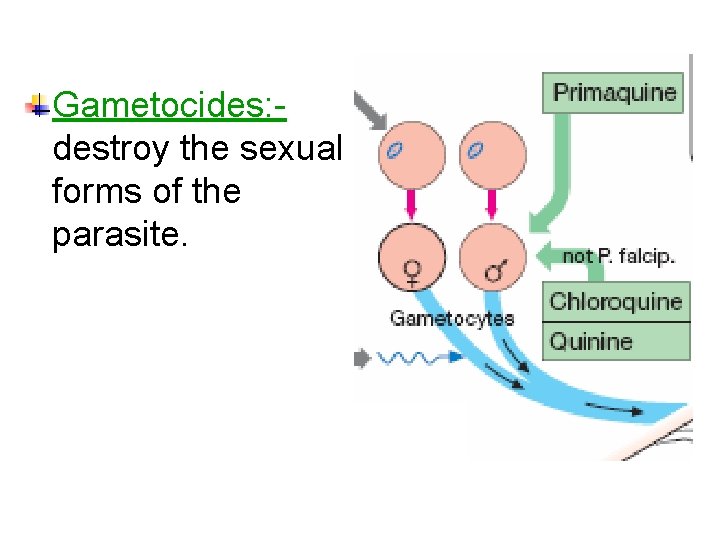
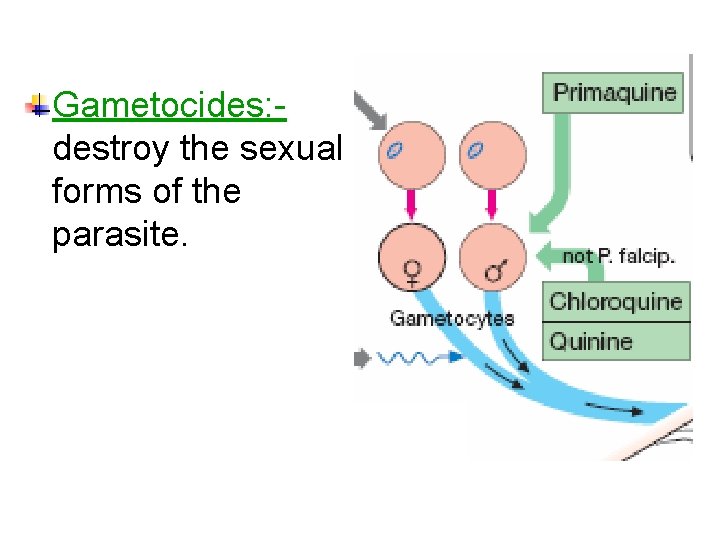
Gametocides: destroy the sexual forms of the parasite.
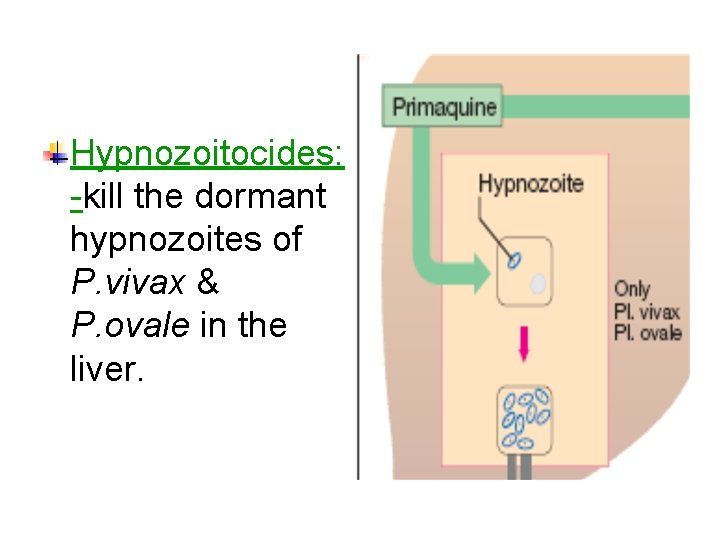
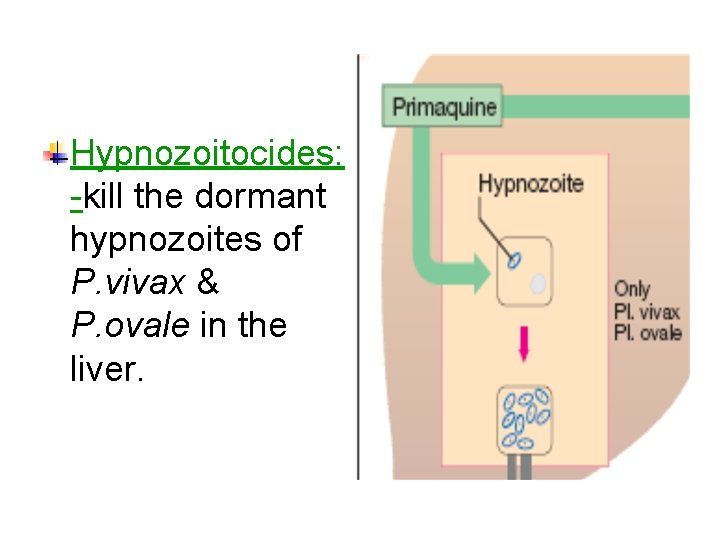
Hypnozoitocides: -kill the dormant hypnozoites of P. vivax & P. ovale in the liver.
Sprontocides: interupt development of sporogonic phase in mosquitoes.
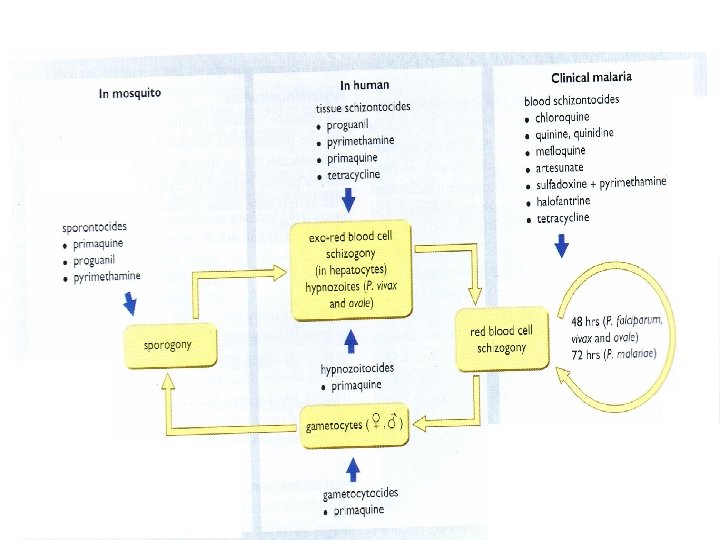
Prophylactic: -to prevent clinical attack 1. Suppressive prophylaxis: -use of blood schizontocides to prevent acute attack 2. Causal prophylaxis: -use of tissue schizontocides to prevent the parasite from establishing in the liver
Curative: -suppressive treatment of the acute attack usually with blood schizontocides. Prevention of transmission: Erradication of infection in mosquitoes using gametocytocides or sprontocides.
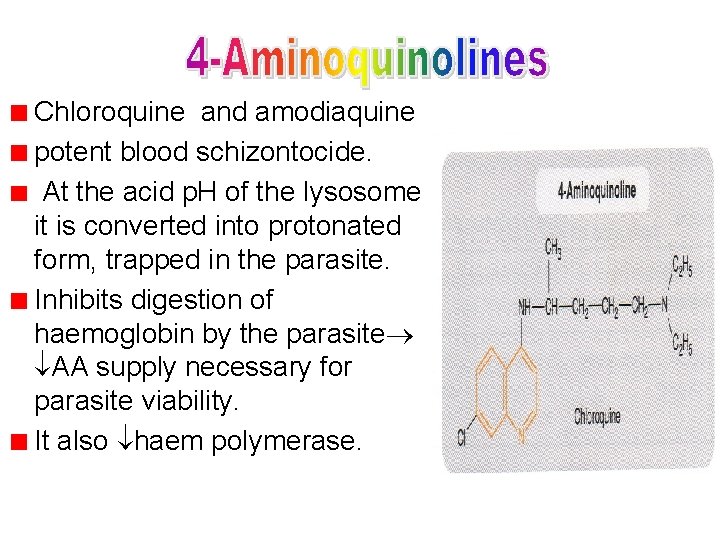
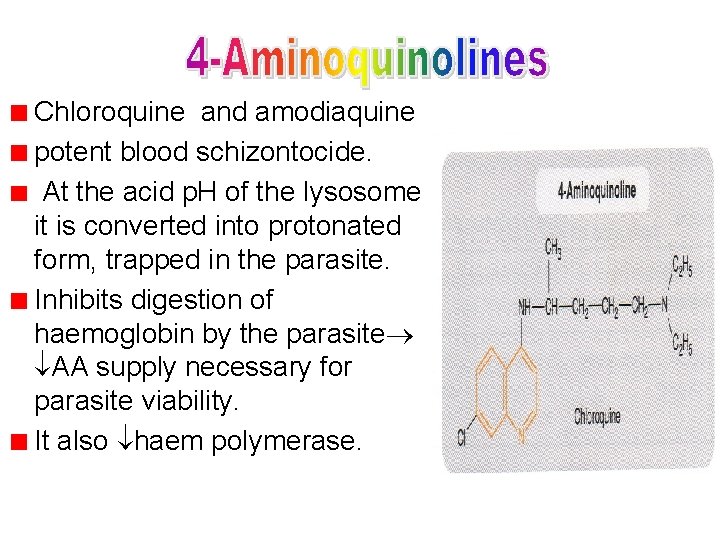
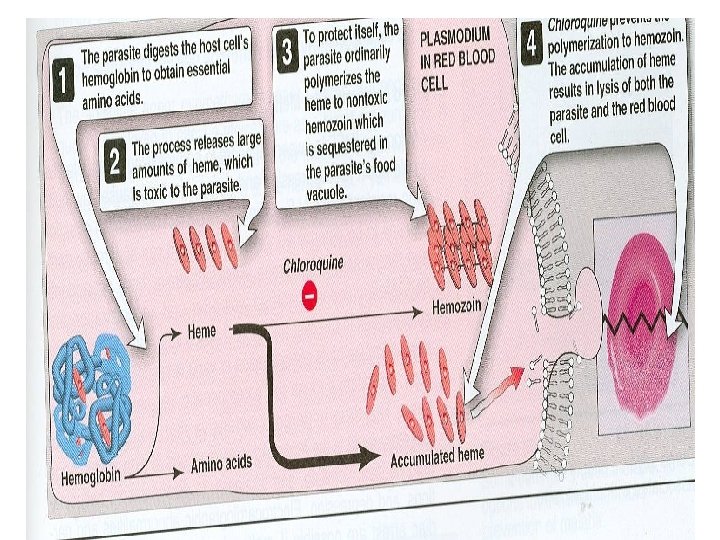
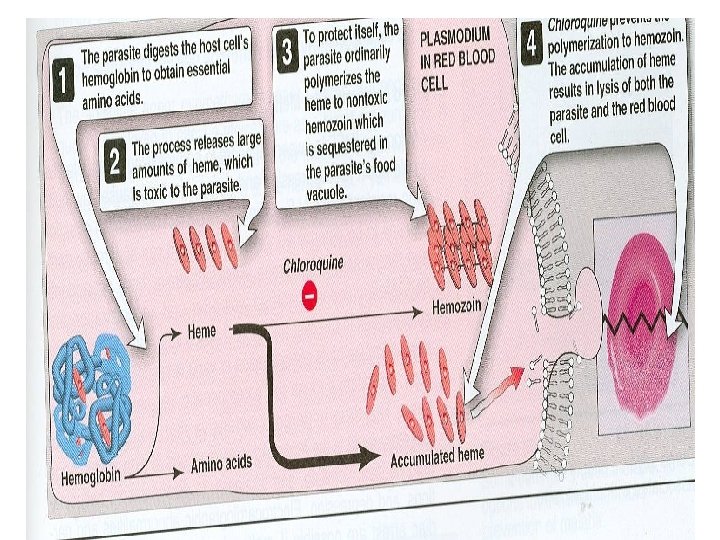
Chloroquine and amodiaquine potent blood schizontocide. At the acid p. H of the lysosome it is converted into protonated form, trapped in the parasite. Inhibits digestion of haemoglobin by the parasite AA supply necessary for parasite viability. It also haem polymerase.
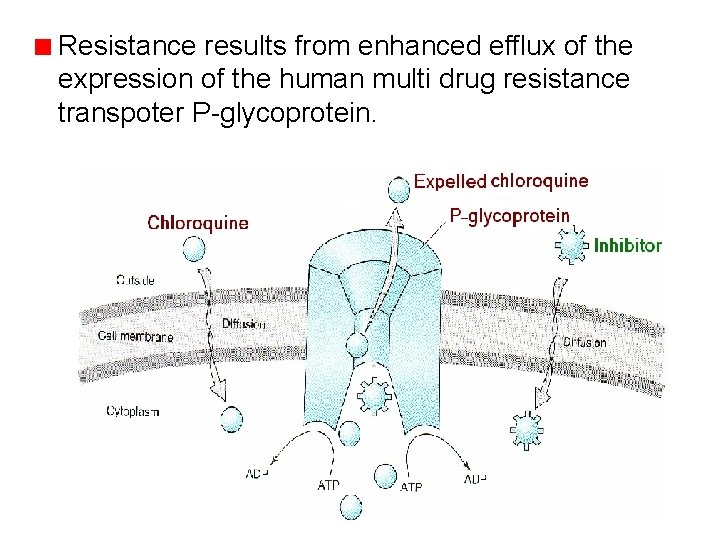
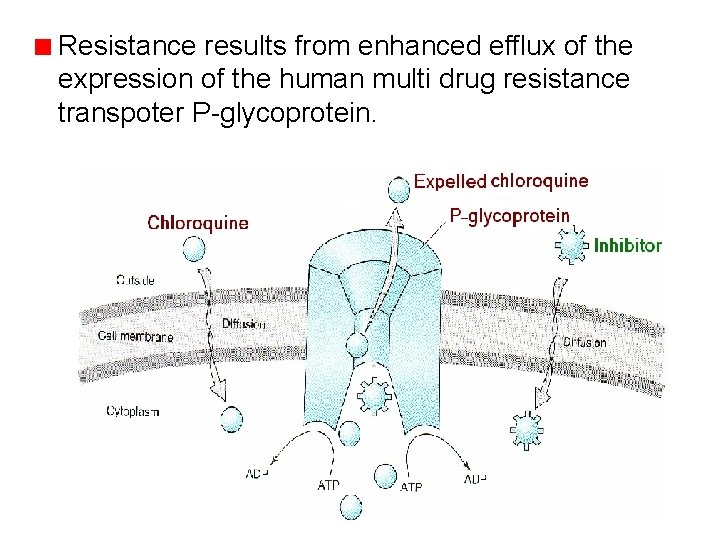
Resistance results from enhanced efflux of the expression of the human multi drug resistance transpoter P-glycoprotein.
It is a disease modifying antirheumatoid drug. Rapidly & completely absorbed from the GIT, has high volume of distribution(1001000 l/kg). Concentrated into parasitised RBCs.
Released slowly from tissues & metabolized in the liver, excreted in the urine 70% unchanged. Elimination is slow. Initial t½ =2 -3 days & terminal t ½=12 months. ADR: -Nausea, vomiting, dizziness, blurring of vision, headache, urticarial symptoms. Large doses retinopathy. Bolus injection hypotension & dysrrhythmias Safe for pregnant women.
Quiz? • Plasmodial resistance to chloroquine is due to (A) Change in receptor structure (B) Increased expression of Pglycoprotein (C) Increase in the activity of DNA repair mechanisms (D) Induction of inactivating enzymes (E) Inhibition of dihydrofolate reductase
Quiz? • Of the following which is not a clinical use of chloroquine are: • A) amebiasis B) malaria prophylaxis C) acute malarial attacks D) guardiasis • E) rheumatoid arthritis
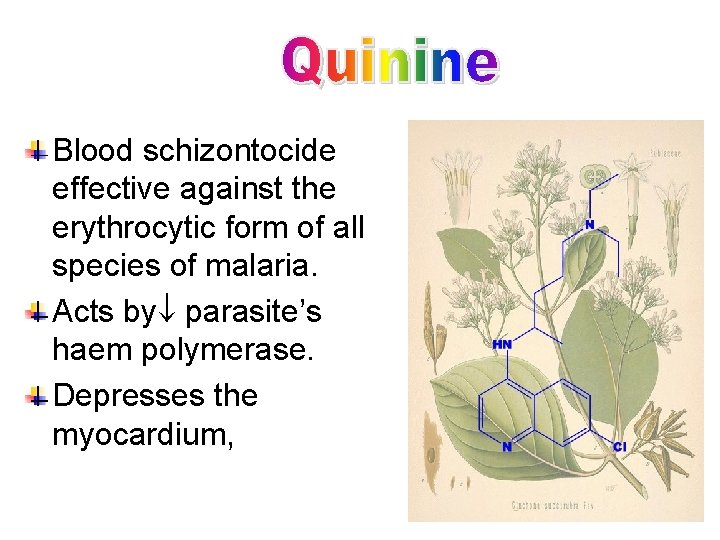
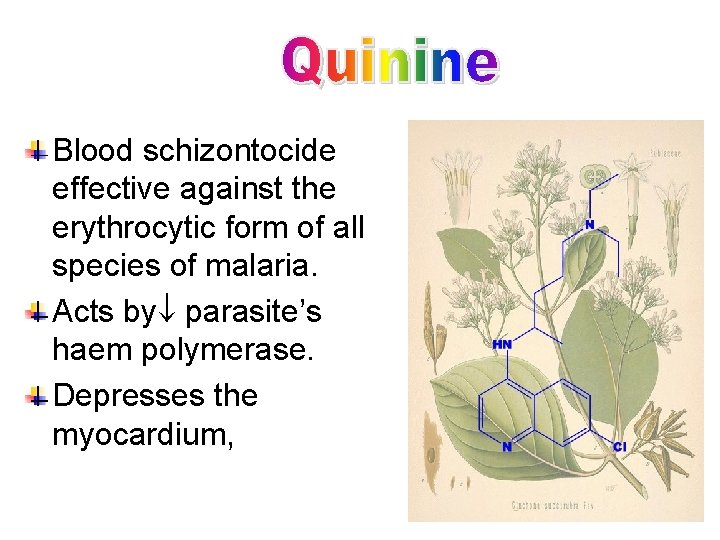
Blood schizontocide effective against the erythrocytic form of all species of malaria. Acts by parasite’s haem polymerase. Depresses the myocardium,
Mild oxytoxic effect on pregnant uterus, Slight neuromuscular blocking action, weak antipyretic action. Given orally in a 7 day course or by slow IV for severe P. falciparum infection, Metabolized in the liver, t½=10 h.
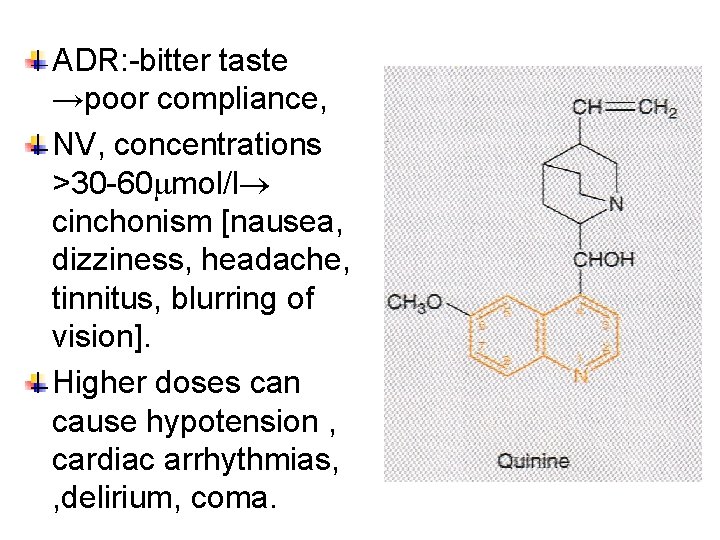
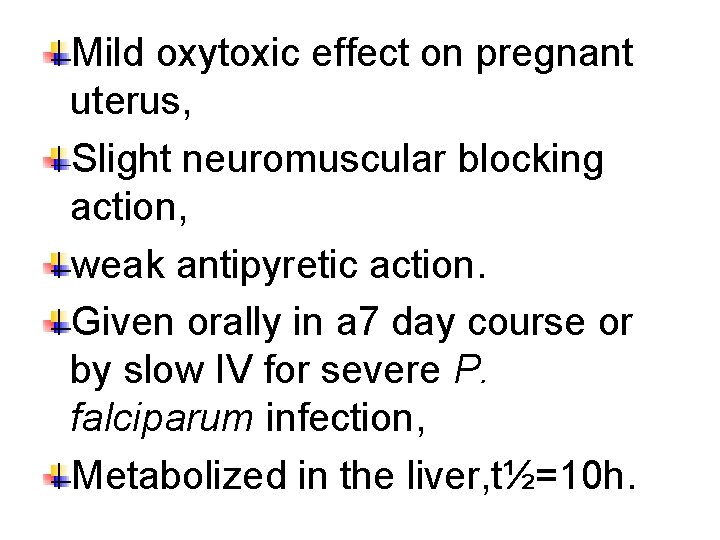
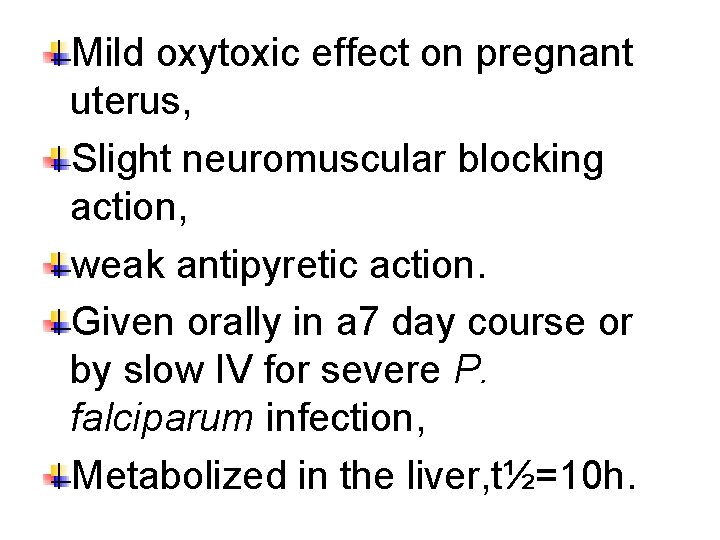
ADR: -bitter taste →poor compliance, NV, concentrations >30 -60 mol/l cinchonism [nausea, dizziness, headache, tinnitus, blurring of vision]. Higher doses can cause hypotension , cardiac arrhythmias, , delirium, coma.
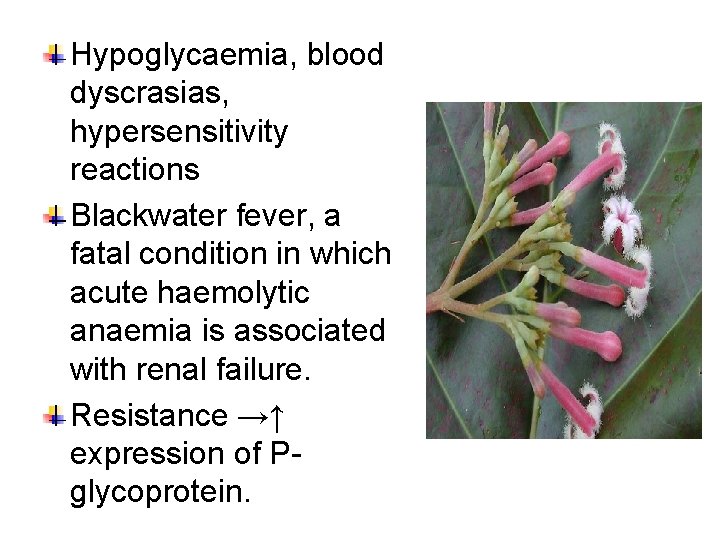
Hypoglycaemia, blood dyscrasias, hypersensitivity reactions Blackwater fever, a fatal condition in which acute haemolytic anaemia is associated with renal failure. Resistance →↑ expression of Pglycoprotein.
CONTRAINDICATIONS Prolonged QT Interval Glucose-6 -Phosphate Dehydrogenase Deficiency Myasthenia Gravis Hypersensitivity Optic Neuritis, auditory problems Dose should be reduced in renal insufficiency
Drug Interactions: Antacids containing aluminum and/or magnesium may delay or decrease absorption of quinine. Erythromycin (CYP 3 A 4 inhibitor): Cimetidine Mefloquine. Quinine can raise plasma levels of warfarin and digoxin.
Quiz? • Which is false about quinine : A) rapid onset B) poorly effective blood schizonticide against P vivax C) gametocidal for P ovale D) causes cinchonism E) causes hypoglycemia
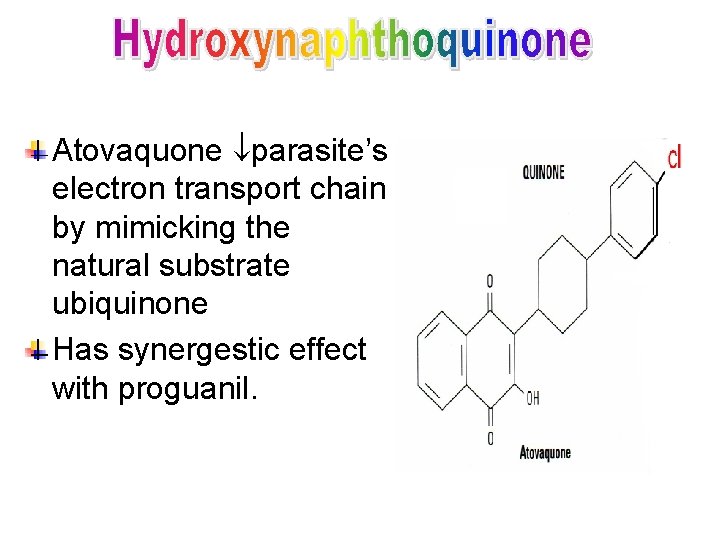
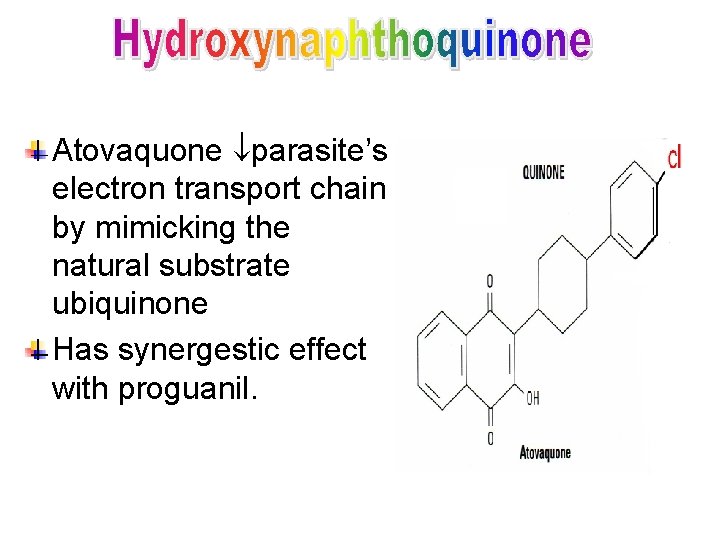
Atovaquone parasite’s electron transport chain by mimicking the natural substrate ubiquinone Has synergestic effect with proguanil.
Pregnant & breast feeding women should not use atavaquone. Resistance to atavaquone is rapid , results from a single point mutation in the gene for cytochrome b. Low bioavailability, slow, erratic absorption, ↑by food, highly protein- bound, t½ =2 -3 d, eliminated unchanged in faeces. ADR: - fever, rash, NVD, insomnia
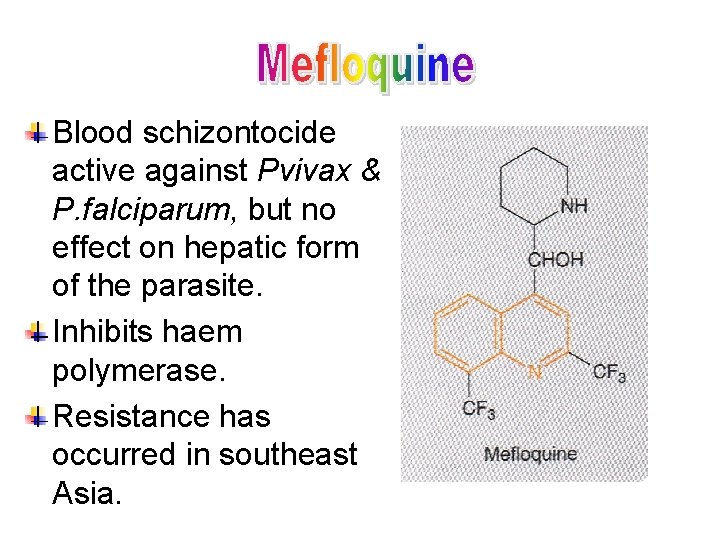
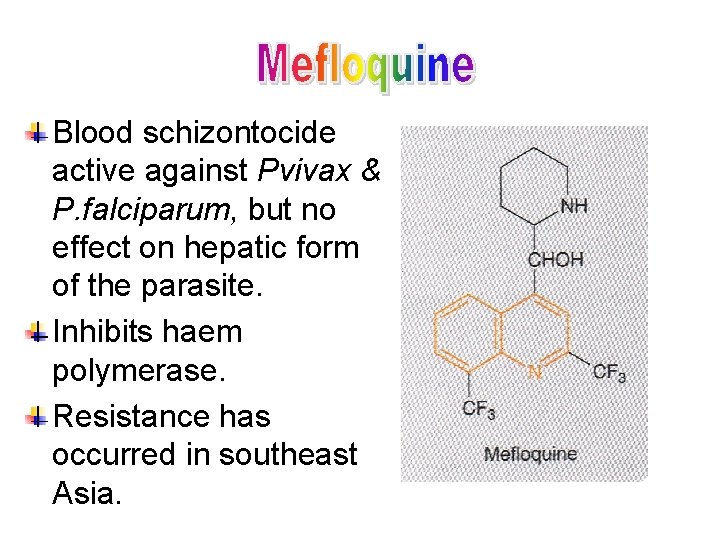
Blood schizontocide active against Pvivax & P. falciparum, but no effect on hepatic form of the parasite. Inhibits haem polymerase. Resistance has occurred in southeast Asia.
Given orally , well absorbed, slow onset of action, t½=30 d enterohepatic recycling or tissue storage. ADR: -GIT disturbances, transient CNS toxicity, confusion, Gidiness, dysphoria, insomnia. May provoke neuropsychiatric disorder. Contra-indicated in pregnant women.
Quiz? • Mefloquine : • A) active against P falciparum gametocytes B) indicated to pregnant women C) active against hepatic stages of P vivax D) contraindicated in cardiac conduction anomalies
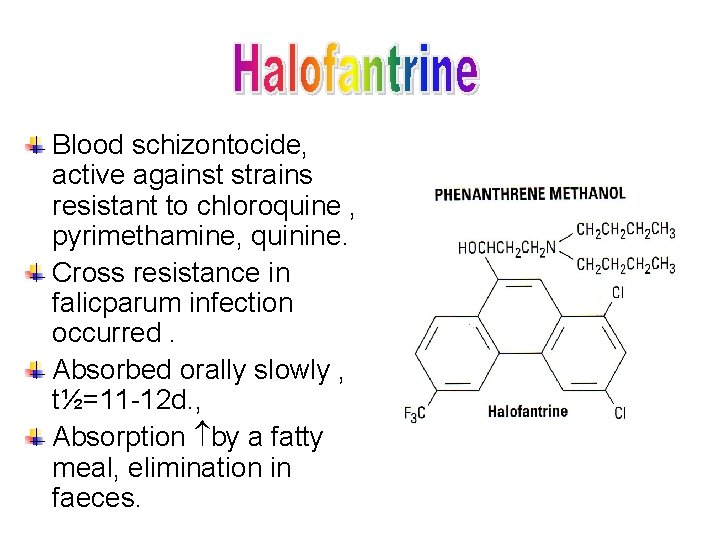
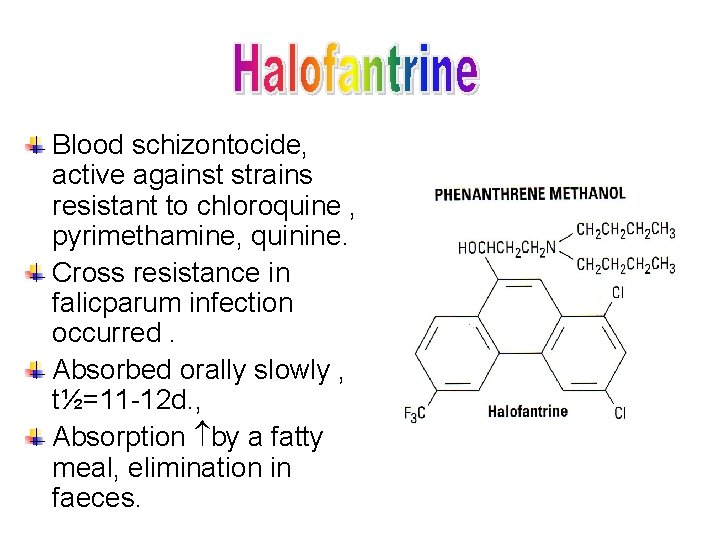
Blood schizontocide, active against strains resistant to chloroquine , pyrimethamine, quinine. Cross resistance in falicparum infection occurred. Absorbed orally slowly , t½=11 -12 d. , Absorption by a fatty meal, elimination in faeces.
ADR: -abdominal pain, headache, transient in hepatic enzymes, cough, pruritus, lengthening of Q-T interval. May cause haemolytic anaemia & convulsions. Reserved for infection caused by resistant organisms. Contraindicated with mefloquine. Patients with cardiac conduction defects. In pregnancy → embriotoxic in animals
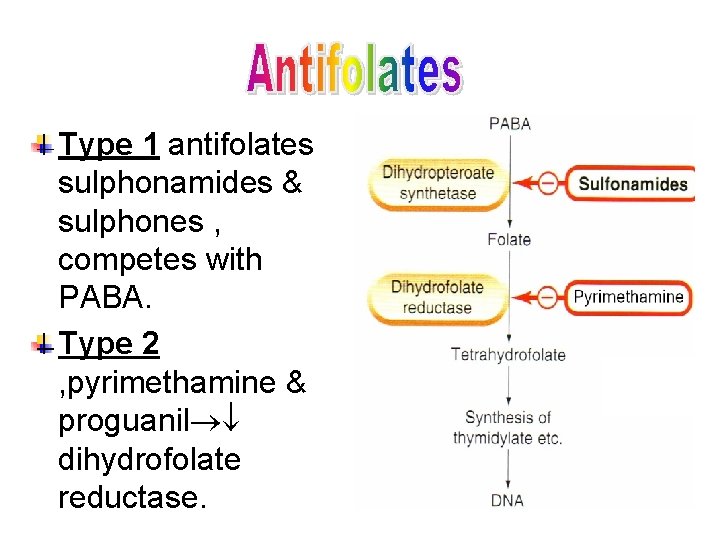
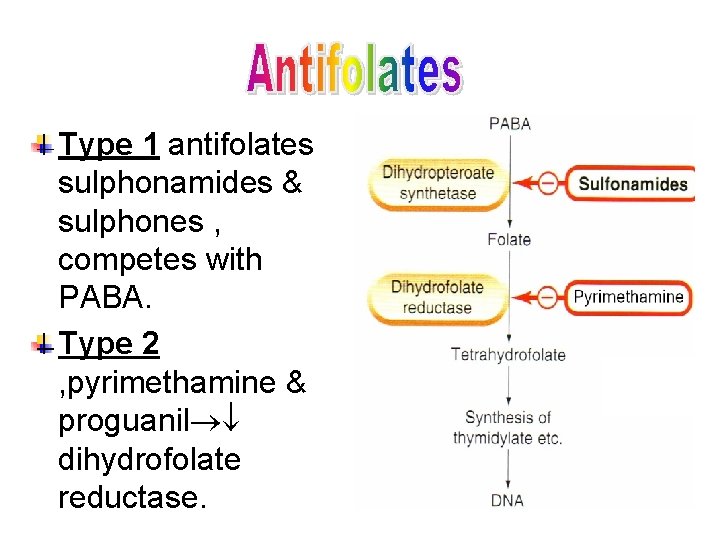
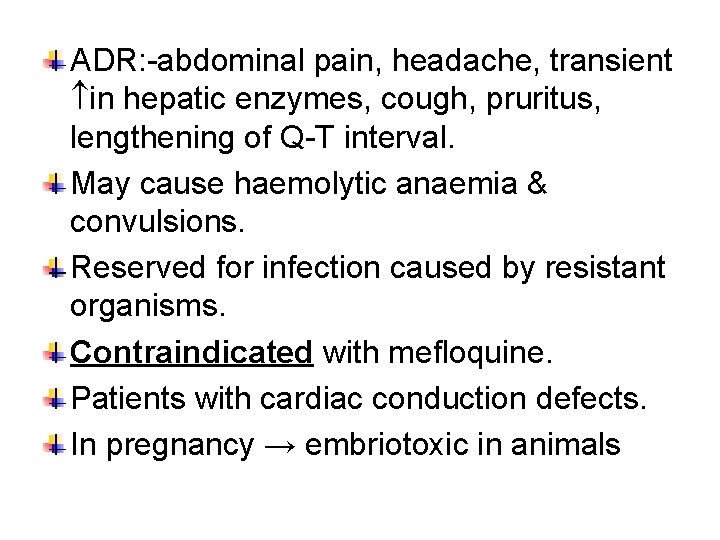
Type 1 antifolates sulphonamides & sulphones , competes with PABA. Type 2 , pyrimethamine & proguanil dihydrofolate reductase.
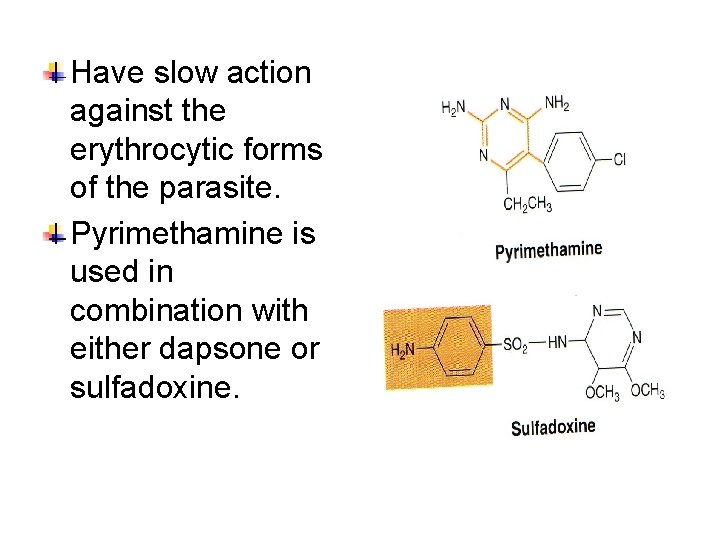
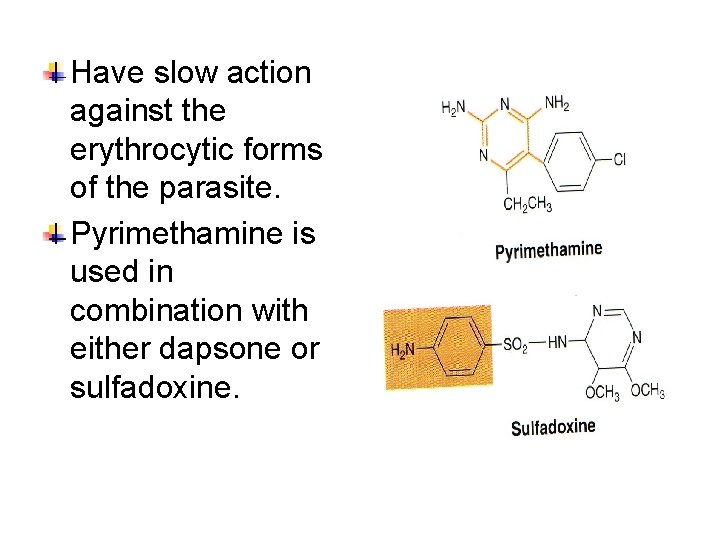
Have slow action against the erythrocytic forms of the parasite. Pyrimethamine is used in combination with either dapsone or sulfadoxine.
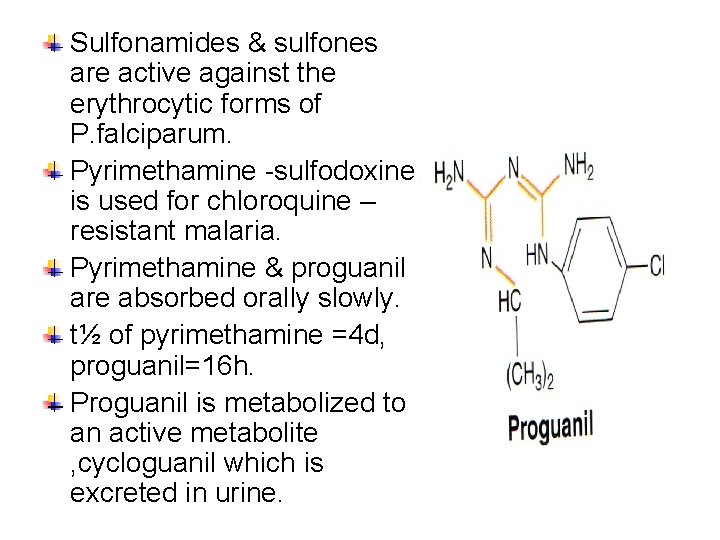
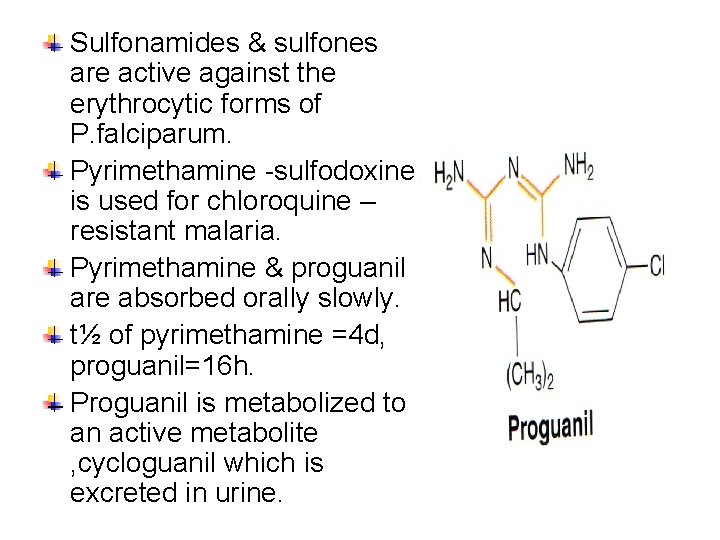
Sulfonamides & sulfones are active against the erythrocytic forms of P. falciparum. Pyrimethamine -sulfodoxine is used for chloroquine – resistant malaria. Pyrimethamine & proguanil are absorbed orally slowly. t½ of pyrimethamine =4 d, proguanil=16 h. Proguanil is metabolized to an active metabolite , cycloguanil which is excreted in urine.
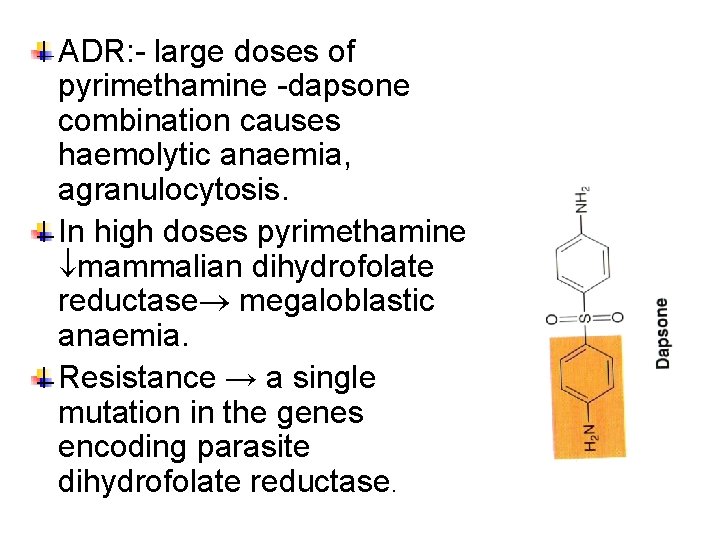
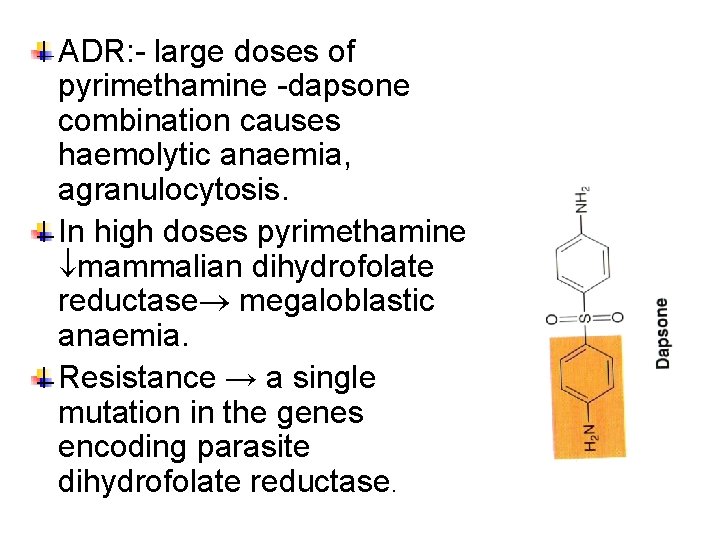
ADR: - large doses of pyrimethamine -dapsone combination causes haemolytic anaemia, agranulocytosis. In high doses pyrimethamine mammalian dihydrofolate reductase megaloblastic anaemia. Resistance → a single mutation in the genes encoding parasite dihydrofolate reductase.
Quiz? • Antimalarials dihydrofolate reductase inhibitors: • A) chloroquine • B) chloroguanide C) pyrimethamine • D) trimethoprim E) primaquine
Quiz? • Concerning sulfonamides & sulfones and antimalarial activity: - a) Blood schizonticidal activity against P falciparum b) useful in acute sever attack of P falciparum c) Active against liver stages of P falciparum or P vivax d) rapid onset of action e) minimal side effects
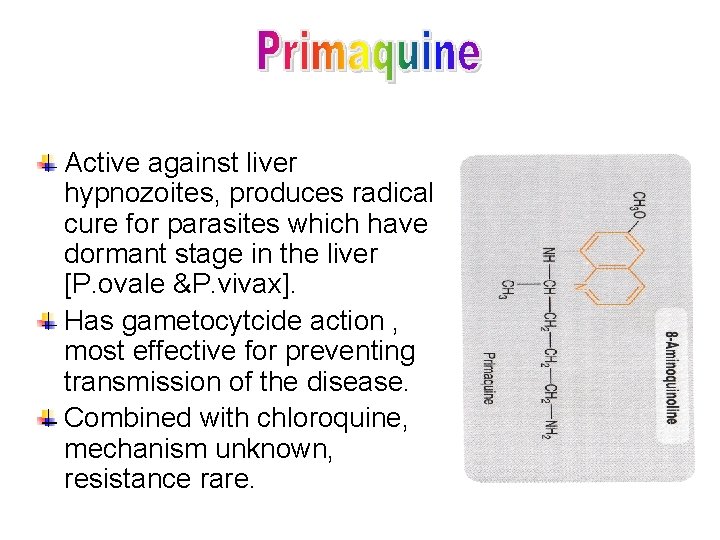
Active against liver hypnozoites, produces radical cure for parasites which have dormant stage in the liver [P. ovale &P. vivax]. Has gametocytcide action , most effective for preventing transmission of the disease. Combined with chloroquine, mechanism unknown, resistance rare.
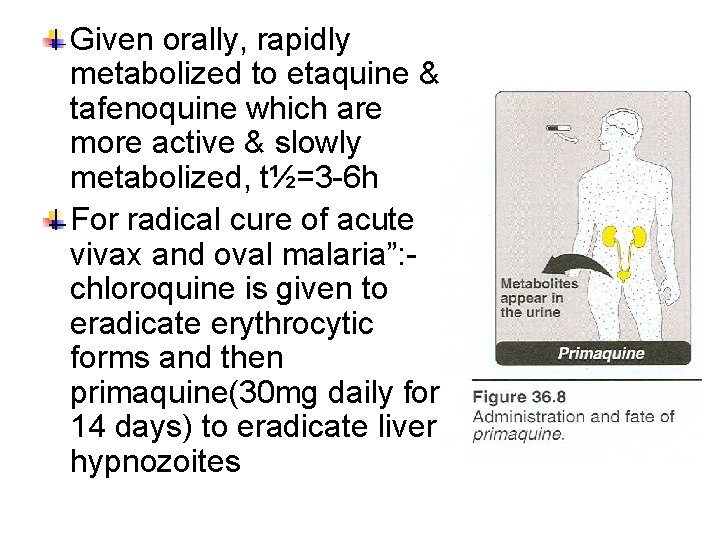
Given orally, rapidly metabolized to etaquine & tafenoquine which are more active & slowly metabolized, t½=3 -6 h For radical cure of acute vivax and oval malaria”: - chloroquine is given to eradicate erythrocytic forms and then primaquine(30 mg daily for 14 days) to eradicate liver hypnozoites
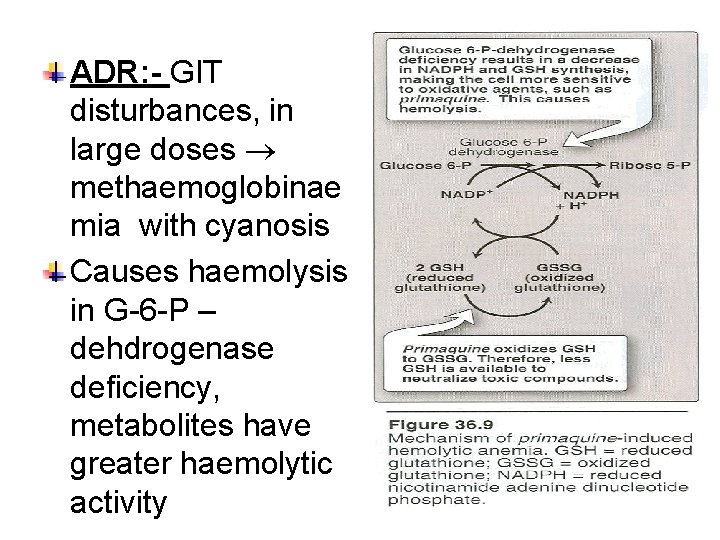
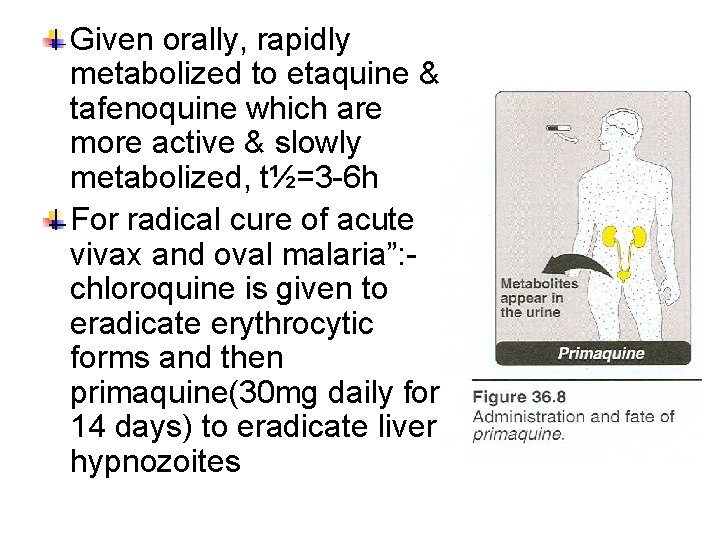
ADR: - GIT disturbances, in large doses methaemoglobinae mia with cyanosis Causes haemolysis in G-6 -P – dehdrogenase deficiency, metabolites have greater haemolytic activity
Quiz? • This is the antimalarial agent most commonly associated with causing an acute hemolytic reaction in patients with glucose 6 -phosphate dehydrogenase deficiency. • (A) Chloroquine • (B) Clindamycin • (C) Mefloqui • (D) Primaquine • (E) Quinine
![Derived from the herb qing haosu Artemisia Artemisinin is poorly soluble in water Derived from the herb qing haosu [Artemisia]. Artemisinin is poorly soluble in water &](https://slidetodoc.com/presentation_image_h/15ec7b7b7d76765e0e82a599f27f15ce/image-49.jpg)
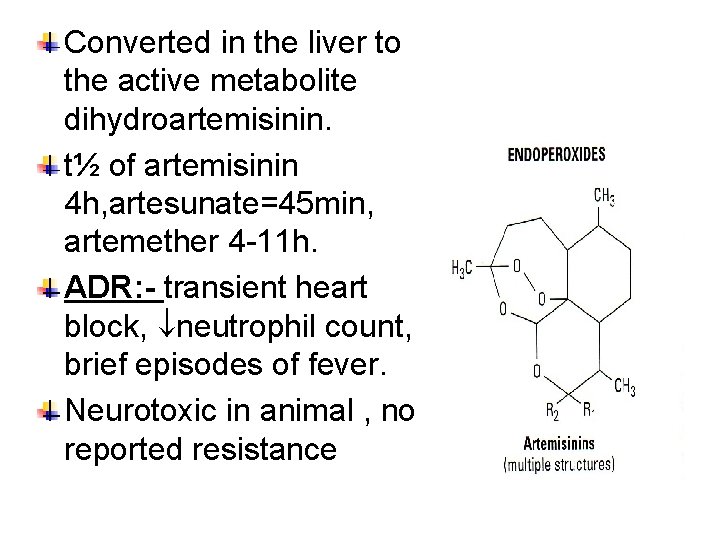
Derived from the herb qing haosu [Artemisia]. Artemisinin is poorly soluble in water & fast acting blood schizontocide. Effective in treating acute attack , including chloroquine –resistant & cerebral malaria. Artemesia annua
![Artesunatea water soluble derivative artemether artethersynthetic analogues have higher activity are better Artesunate[a water- soluble derivative], artemether & artether[synthetic analogues] have higher activity & are better](https://slidetodoc.com/presentation_image_h/15ec7b7b7d76765e0e82a599f27f15ce/image-50.jpg)
Artesunate[a water- soluble derivative], artemether & artether[synthetic analogues] have higher activity & are better absorbed. It damages the parasite membrane by carbon- centered free radicals. Rapidly absorbed , widely distributed,
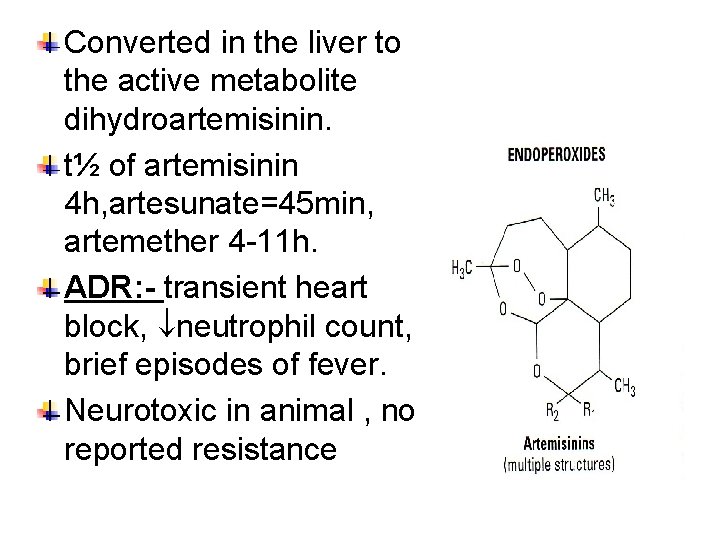
Converted in the liver to the active metabolite dihydroartemisinin. t½ of artemisinin 4 h, artesunate=45 min, artemether 4 -11 h. ADR: - transient heart block, neutrophil count, brief episodes of fever. Neurotoxic in animal , no reported resistance
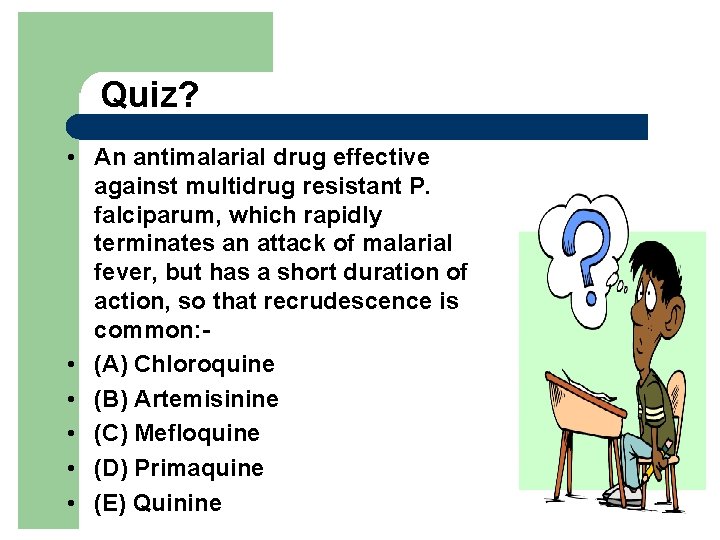
Quiz? • An antimalarial drug effective against multidrug resistant P. falciparum, which rapidly terminates an attack of malarial fever, but has a short duration of action, so that recrudescence is common: • (A) Chloroquine • (B) Artemisinine • (C) Mefloquine • (D) Primaquine • (E) Quinine

Doxycycline is used as a suppressive prophylactic in areas where mefloquine resistance is common. Clindamycin has proved effective in the treatment of uncomplicated falicparum malaria, may be used in combination with quinine.
Use of prophylactic drugs is seldom practical for full-time residents of malariaendemic areas, and their use is usually restricted to short-term visitors and travelers to malarial regions. People temporarily visiting malariaendemic areas usually begin taking the drugs one to two weeks before arriving and must continue taking them for 4 weeks after leaving.
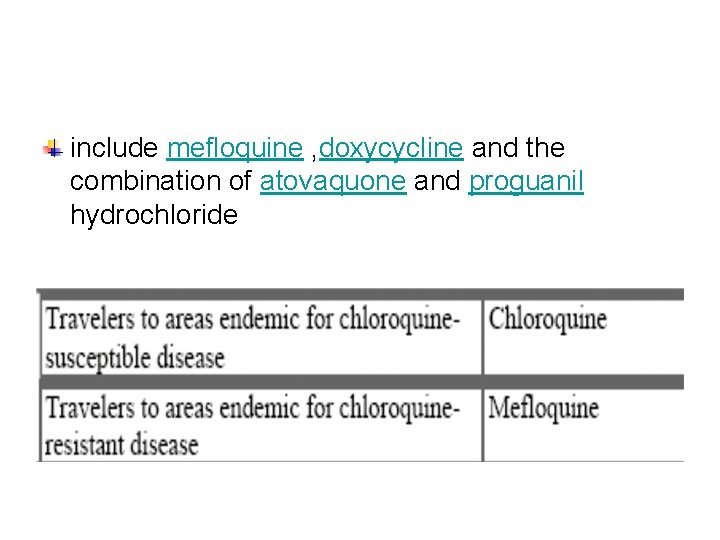
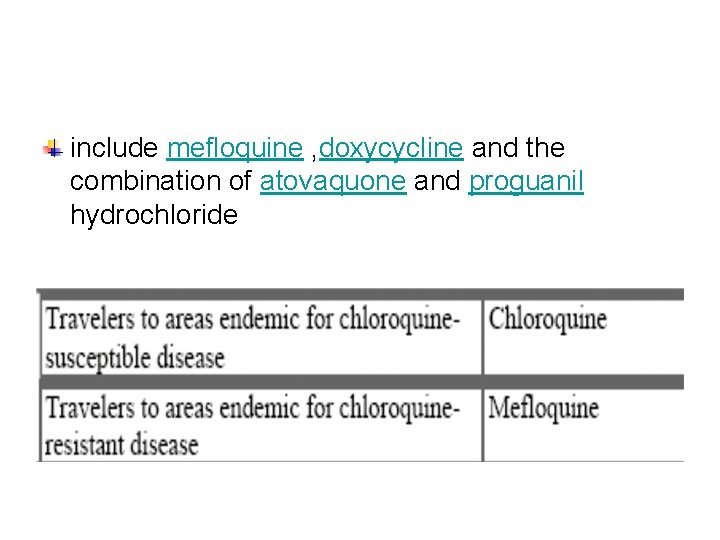
include mefloquine , doxycycline and the combination of atovaquone and proguanil hydrochloride
A 35 -year-old medical entomologist comes to the hospital with chief complaints of fever, headache, and photophobia. This illness began about 6 days prior to admission, when he returned from a 2 month visit to the jungles of Central and South America. He took a drug for prophylaxis of malaria before starting the trip. On his return flight, about 6 days prior to admission, he described having fever and shaking chills. He saw his physician 2 days prior to admission; the physician made a diagnosis of influenza and prescribed tetracycline.
On the day of admission, the patient had shaking chills followed by temperature elevation to 104°F (40°C). Physical examination revealed a well-developed man who appeared ill. There is some left upper quadrant tenderness but no organomegaly; blood pressure, 126/90; pulse, 120; and respirations, 22. Laboratory findings were hemoglobin, 14. 5 mg/d. L (normal, 13. 4– 17. 4 mg/d. L); hematocrit, 45% (normal, 40– 54%); Giemsa-stained blood smear (thick and thin) revealed Plasmodium vivax
Q 1 • The drug she took for prophylaxis was probably (A) Chloroquine (B) Mefloquine (C) Primaquine (D) Proguanil (E) Pyrimethamine
Q 2? • Which of the following drugs should be used for oral treatment of the entomologist's acute attack of P vivax malaria? • (A) Chloroquin • (B) Mefloquine • (C) Primaquin • (D) Pyrimethamine-sulfadoxine • (E) Quinine
Q 3? • Which of the following drugs should be given later in order to eradicate schizonts and latent hypnozoites in the patient's liver? (A) Chloroquine (B) Mefloquine (C) Primaquine (D) Proguanil (E) Quinine
About 90% of malaria deaths occur in sub Saharan Africa. The key factor contributing to malarial morbidity & mortality is resistance of P. falciparum to chloroquine, sulfodoxin-pyrimethamin [SP] & amodiaquine. Artemisinin compounds produce a very rapid therapeutic response , active against multi-drug resistant P. falciparum, well tolerated by the patient, gametocyte carriage, no resistance is detected. Artemisinins cure falciparum malaria in 7 d, if combined with another drug in 3 d.
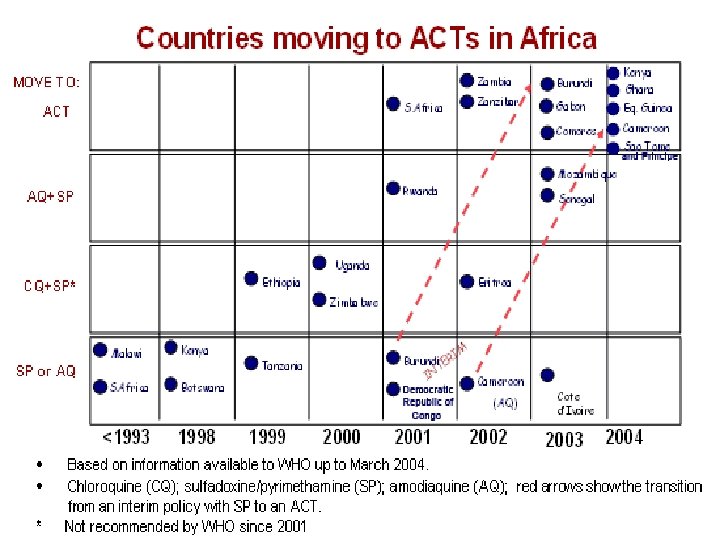
1. 2. 3. 4. 5. WHO recommends that all countries experiencing resistance to conventional monotherapies should use combination therapy, preferably containing artemisinins [ACTs -artemisinin-based combination therapies]. WHO recommends the following therapeutic options: Artemether/lumefantrine Artesunate+amodiaquine Artesunate+SP Artesunate+ mefloquine [area with low to moderate transmission. Amodiaquine+SP

Quiz? • Regarding drugs used for malaria, which one of the following statements is false? (A) Chloroquine is the drug of choice for acute attacks of non falciparum malaria (B) Cinchonism is associated with the use of quinine (C) Hemolysis has occurred with primaquine in patients deficient in G 6 P dehydrogenase (D) Mefloquine is used for prophylaxis in regions where chloroquine resistance occurs (E) Quinine is contraindicated in pregnancy
A 57 -year-old photographer developed fever, diarrhea, headache, vomiting, and dark urine about 10 days after returning to the United States from a month-long trip to East Africa. The patient has been taking chloroquine and proguanil chemoprophylaxis. On physical examination the patient is feverish, agitated, sweating, weak, and in mild distress, with a blood pressure 95/60 (normal, 120/80), a pulse of 120 (normal, 60– 100),
and temperature of 104°F (40°C) (normal, 98. 6°F, 37°C). Laboratory findings are a hematocrit of 25% (normal for male, 40– 54%); platelet count 29, 000 (normal, 150, 000– 400, 000/mm 3); parasitemia 6% (P. falciparum); serum creatinine 3. 5 mg/d. L (Normal for male, 0. 8– 1. 5 mg/d. L); and plasma glucose 39 mg/d. L (Normal fasting, 65– 110 mg/d. L).
Q 1 • What is the best choice of drug therapy?