Specialist CAMHS ADHD Neurodevelopmental Team City and Hackney




- Slides: 53
Specialist CAMHS - ADHD Neurodevelopmental Team, City and Hackney CAMHS Julie Proctor, Psychological Therapies Lead -Joint Clinical Team Lead
Neurodevelopmental Pathway Team 2 Consultant Psychiatrists * Specialist Trainee in Psychiatry FY 1 and FY 2 doctors Nurse Prescriber Clinical Nurse Specialist Consultant Clinical Psychologist Principal Clinical Psychologist Assistant Psychologist Family Therapist * Child and Adolescent Psychotherapist *
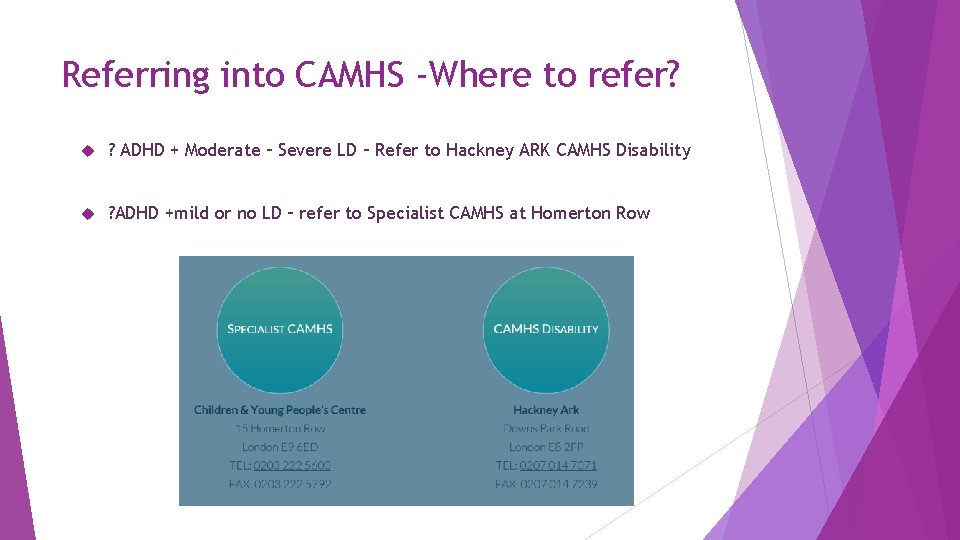
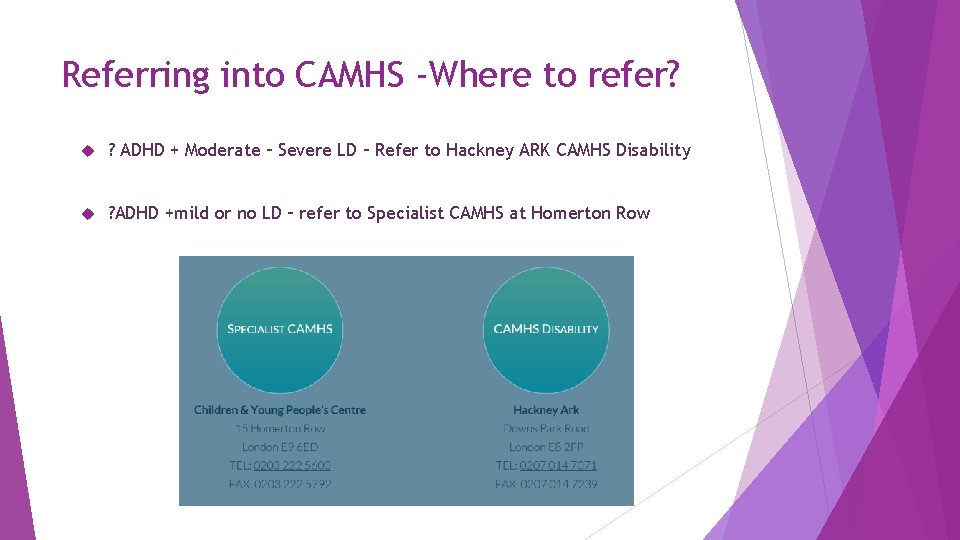
Referring into CAMHS -Where to refer? ? ADHD + Moderate – Severe LD – Refer to Hackney ARK CAMHS Disability ? ADHD +mild or no LD – refer to Specialist CAMHS at Homerton Row
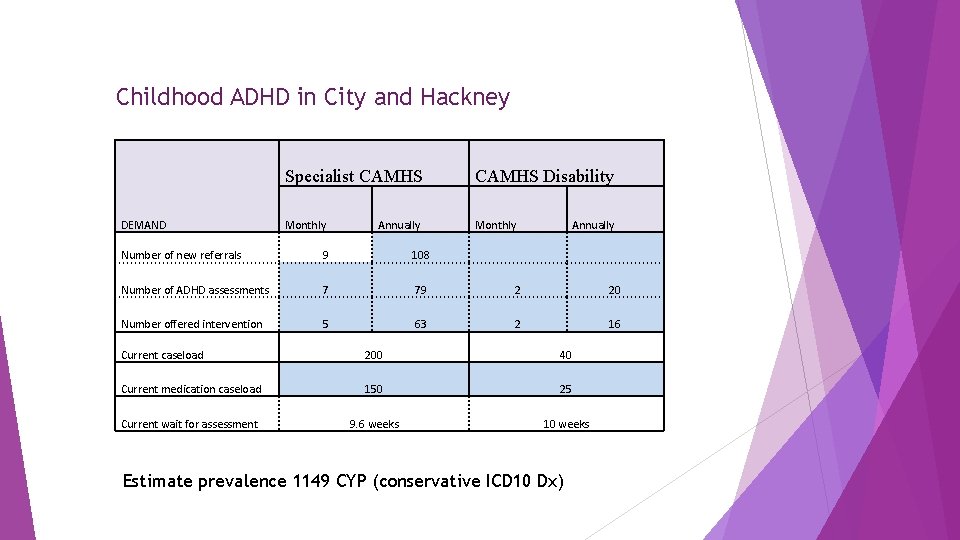
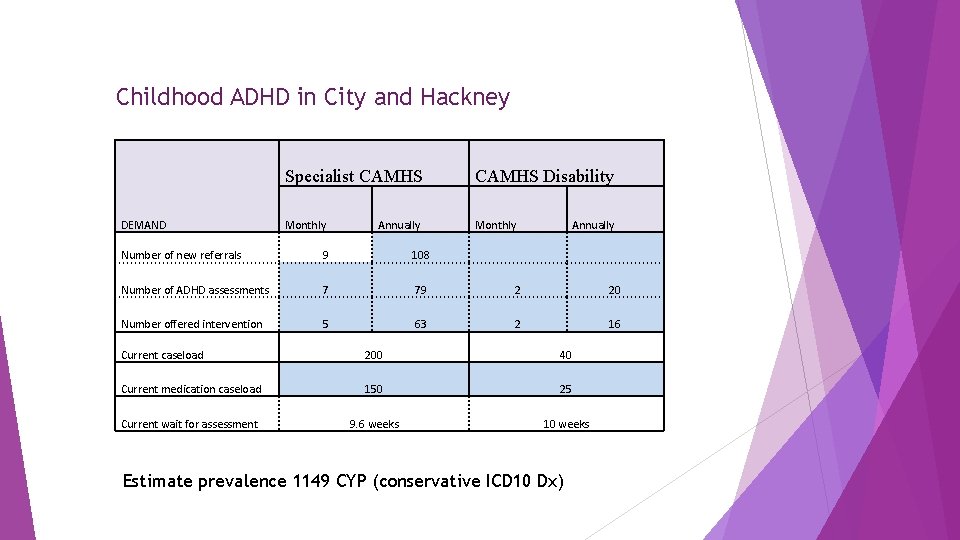
Childhood ADHD in City and Hackney DEMAND Specialist CAMHS Disability Monthly Annually Number of new referrals 9 108 Number of ADHD assessments 7 79 2 20 Number offered intervention 5 63 2 16 Current caseload 200 40 Current medication caseload 150 25 Current wait for assessment 9. 6 weeks 10 weeks Estimate prevalence 1149 CYP (conservative ICD 10 Dx)
ADHD Diagnostic Assessment Process Initial CAMHS Assessment in the Assessment Clinic – general overview MDT Assessment Clinic discussion Neurodevelopmental team MDT discussion – allocation to appropriate clinician(s) and professional discipline(s) Assessment – clinical interview, review of reports, school screening information. Plus if required - school observation, cognitive assessment, family functioning assessment, CSC referral/consultation, medical investigations, SLT/OT, genetic testing, attachment assessment etc. Neurodevelopmental team MDT discussion Assessment Feedback session and Care Planning
Service Developments ADHD Quality Improvement Project All assessments completed within 12 weeks of referral Neurodevelopmental Pathway Patient Journey Analysis CYP ADHD Primary Care Step Down Stable cases for over 12 months, 11 -18 yolds that can be safely stepped down to Primary Care Approx 60 cases in total – budget per patient for GPs Stepped Down with direct support of ADHD Primary Care Liaison Nurse Prescriber 6 monthly reviews – 20 mins using EMIS template Fast track referral back to CAMHS if required – all Diagnosis, Titration and Dose stabilisation remains in CAMHS Secondary Care
Referring to CAMHS – What do we need? A copy of your report and summary of associated investigations (bloods, genetic testing etc) Other services involved e. g. social care A detailed developmental history Information about existing conditions e. g. ASD If secondary ADHD – when was the TBI and what other services are involved? Information re current medications or treatments What other investigations are you completing, if any? Copies of additional reports you have e. g. Sa. LT, OT, EP Complete the specialist CAMHS referral form (it’s not too long) Some examples of hyperactivity, inattention and impulsivity across settings (e. g. home, school, what did you observe in clinic? If you’re not sure what to ask – complete a screening tool (SNAP IV 26 – its free and a PDF which can be accessed online) – attach this to your referral Still unsure? Ask our duty worker on 0203 222 5600
What is the definition of ADHD? Primary ADHD is a neurodevelopmental disorder affecting both children and adults. It is described as a “persistent” or on-going pattern of inattention and/or hyperactivity-impulsivity that gets in the way of daily life or typical development. There are three presentations of Primary ADHD: Inattentive Hyperactive-impulsive Combined inattentive & hyperactive-impulsive (DSM V)
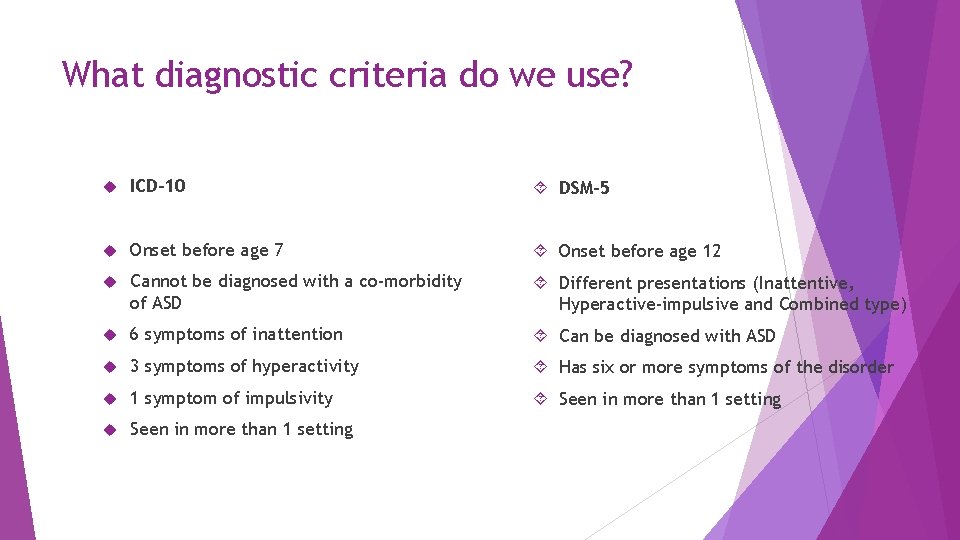
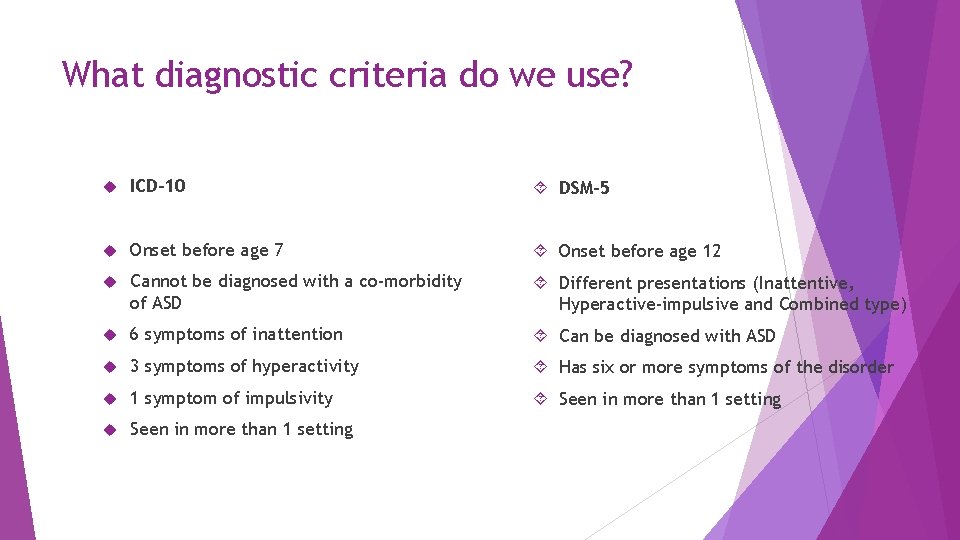
What diagnostic criteria do we use? ICD-10 DSM-5 Onset before age 7 Onset before age 12 Cannot be diagnosed with a co-morbidity of ASD Different presentations (Inattentive, Hyperactive-impulsive and Combined type) 6 symptoms of inattention Can be diagnosed with ASD 3 symptoms of hyperactivity Has six or more symptoms of the disorder 1 symptom of impulsivity Seen in more than 1 setting
Inattention Hyperactivity Impulsivity
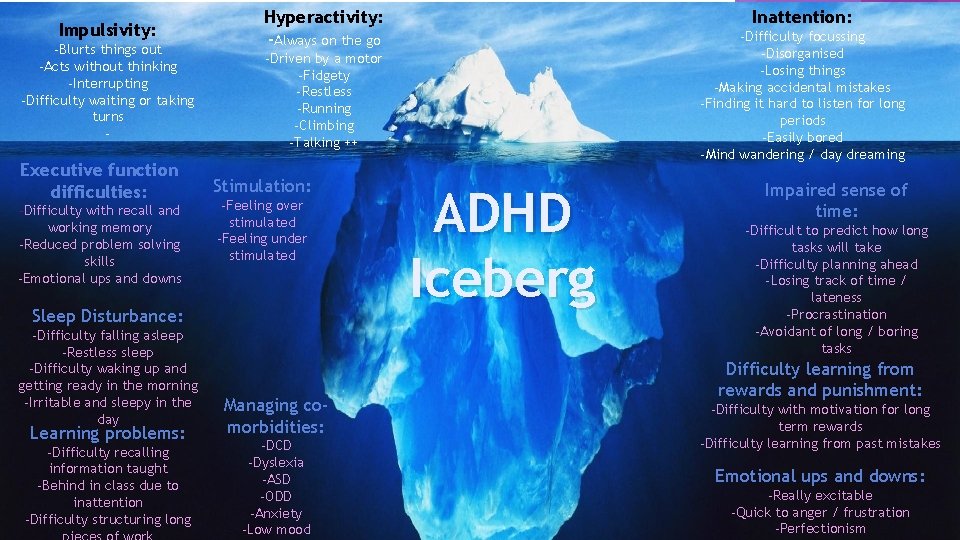
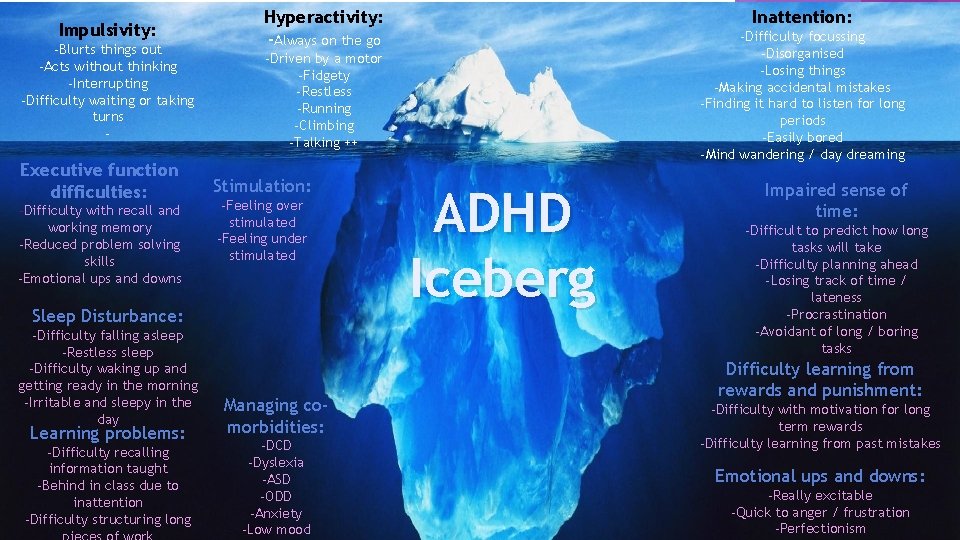
Impulsivity: -Blurts things out -Acts without thinking -Interrupting -Difficulty waiting or taking turns - Executive function difficulties: -Difficulty with recall and working memory -Reduced problem solving skills -Emotional ups and downs Hyperactivity: -Always on the go Learning problems: -Difficulty recalling information taught -Behind in class due to inattention -Difficulty structuring long -Difficulty focussing -Disorganised -Losing things -Making accidental mistakes -Finding it hard to listen for long periods -Easily bored -Mind wandering / day dreaming -Driven by a motor -Fidgety -Restless -Running -Climbing -Talking ++ Stimulation: -Feeling over stimulated -Feeling under stimulated Sleep Disturbance: -Difficulty falling asleep -Restless sleep -Difficulty waking up and getting ready in the morning -Irritable and sleepy in the day Inattention: Managing comorbidities: -DCD -Dyslexia -ASD -ODD -Anxiety -Low mood ADHD Iceberg Impaired sense of time: -Difficult to predict how long tasks will take -Difficulty planning ahead -Losing track of time / lateness -Procrastination -Avoidant of long / boring tasks Difficulty learning from rewards and punishment: -Difficulty with motivation for long term rewards -Difficulty learning from past mistakes Emotional ups and downs: -Really excitable -Quick to anger / frustration -Perfectionism
Quick Humoured Strong sense of fairness Thinking outside the box Unique personality Great leaders Hyper-focus! Creative thinkers Generous Spontaneous Passionate Loving Resilience – picking yourself back Will take a risk – put themselves out there
What are the causes of ADHD? No definitive cause for ADHD has been identified Instead, there a series of known risk factors Genetics Exposure to environmental toxins during pregnancy Exposure to toxins, such as high levels of lead at a young age Low birth weight Premature birth Late birth Brain injury Smoking, drinking alcohol or substance misuse during pregnancy (NIMH, 2016)
Prevalence ADHD affects approximately 5% of the school aged population Male to Female ratio in children is approximately 4: 1 Girls more commonly have inattentive symptoms, whereas boys more hyperactive and impulsive (could account for skewed ratio’s)
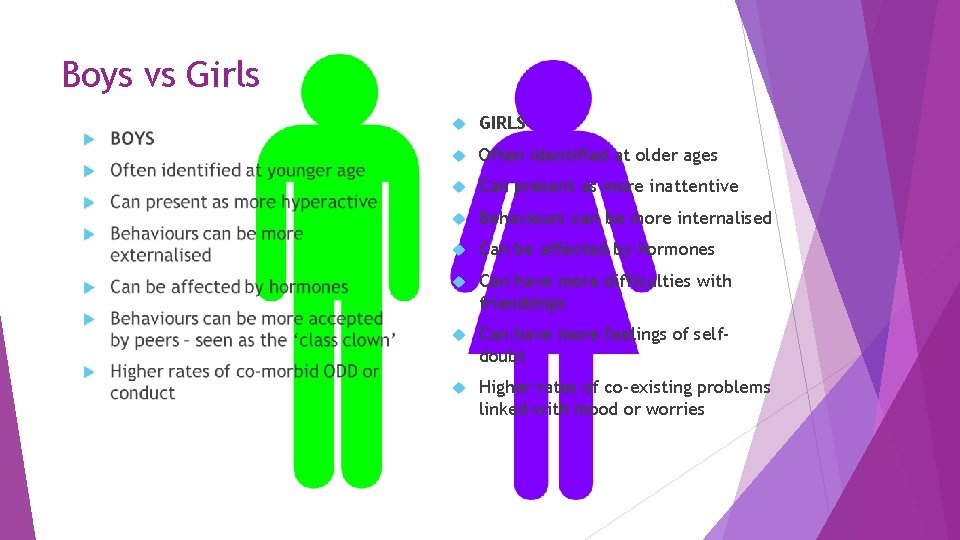
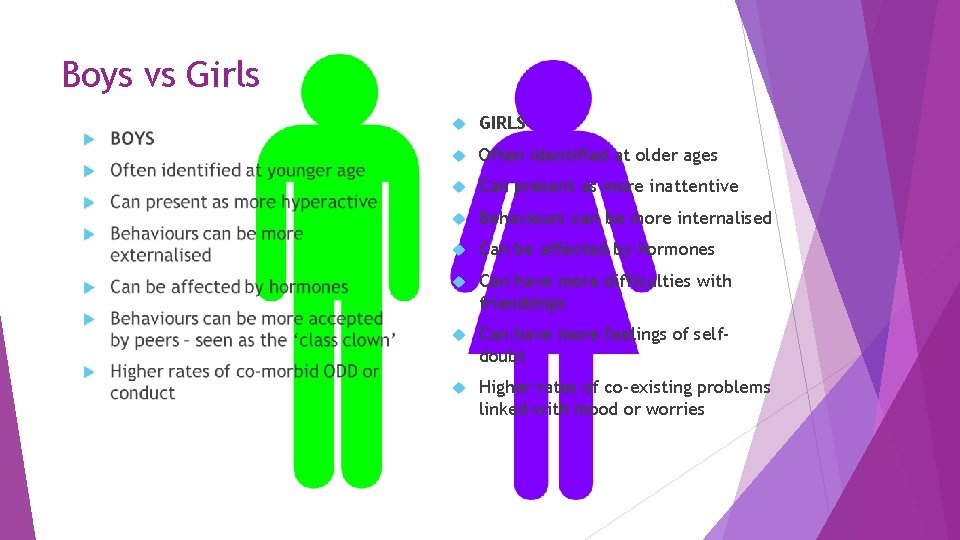
Boys vs Girls GIRLS Often identified at older ages Can present as more inattentive Behaviours can be more internalised Can be affected by hormones Can have more difficulties with friendships Can have more feelings of selfdoubt Higher rates of co-existing problems linked with mood or worries
How long does it last? ADHD does persist into adulthood for approximately 60% of children / young people diagnosed (Targum & Adler, 2014) Hyperactivity and impulsivity symptoms can be seen to “decay” (reduce) as young people move into adulthood (Wilen, 2009)
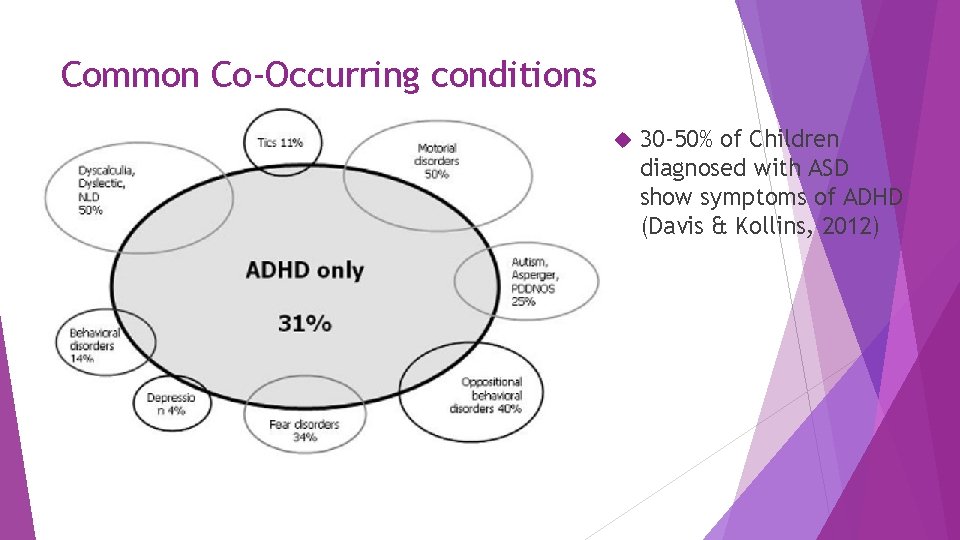
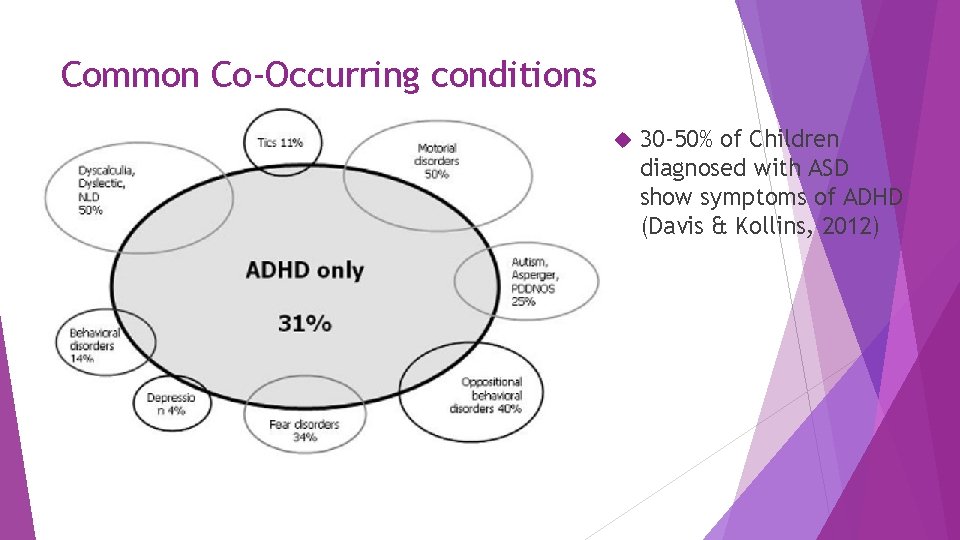
Common Co-Occurring conditions 30 -50% of Children diagnosed with ASD show symptoms of ADHD (Davis & Kollins, 2012)
What looks like ADHD? PTSD (Post Traumatic Stress Disorder) ASD (Autism Spectrum Disorder) Learning difficulties / disability FAS (Foetal Alcohol Syndrome) Chromosome deletions Attachment problems Speech and Language needs Anxiety
Interventions
What intervention is recommended and when? (NICE NG 87) Use of the NICE guidance (NG 87) Preschool children (under 5): -Parent training / education programmes are the first line treatment -Medication as a treatment is not recommended in preschool children -Liaison with the school about the diagnosis
What intervention is recommended and when? (NICE NG 87) School Age Children and Young People (5 and above) Give information about ADHD and offer additional support to parents and carers of all children aged 5 years and over and young people with ADHD. The support should be ADHD focused, can be group based and as few as 1 or 2 sessions. It should include: education and information on the causes and impact of ADHD advice on parenting strategies with consent, liaison with school, college or university both parents and carers if feasible
What intervention is recommended and when? (NICE NG 87) Medication as an intervention Offer medication for children aged 5 years and over and young people only if: their ADHD symptoms are still causing a persistent significant impairment in at least one domain after environmental modifications have been implemented and reviewed they and their parents and carers have discussed information about ADHD a baseline assessment has been carried out Medication is not recommended in child under 5 years old
What intervention is recommended and when? (NICE NG 87) Consider a course of cognitive behavioural therapy (CBT) for young people with ADHD who have benefited from medication but whose symptoms are still causing a significant impairment in at least one domain, addressing the following areas: social skills with peers problem-solving self-control active listening skills dealing with and expressing feelings
Before medication…cover all bases Should the child be wearing glasses whilst at school? Are they receiving appropriate support for co-morbid conditions? e. g. Speech and Language needs, learning difficulties, dyslexia, hypermobility, mental health needs etc. Are they being given the best opportunity to learn? e. g. where they’re sat in class, learning support in place if assessed as needed Does the child have sensory needs and are these addressed? E. g. are they affected by bright lights, noise levels in the class etc Does everyone involved with supporting your child understand their needs?

Trialling medication
Pre-screening Physical Health Checks Full CAMHS / Mental Health assessment Full health history – including family health history Cardiac Liver Kidneys Diabetes Thyroid Iron deficiency Pica Asthma Epilepsy Tic disorder / tourettes Substance misuse / diversion risk Allergies Any herb al re med ies?
Pre-screening physical observations Blood pressure Pulse Height Weight Use of centiles Baseline ECG if significant cardiac hx within the family
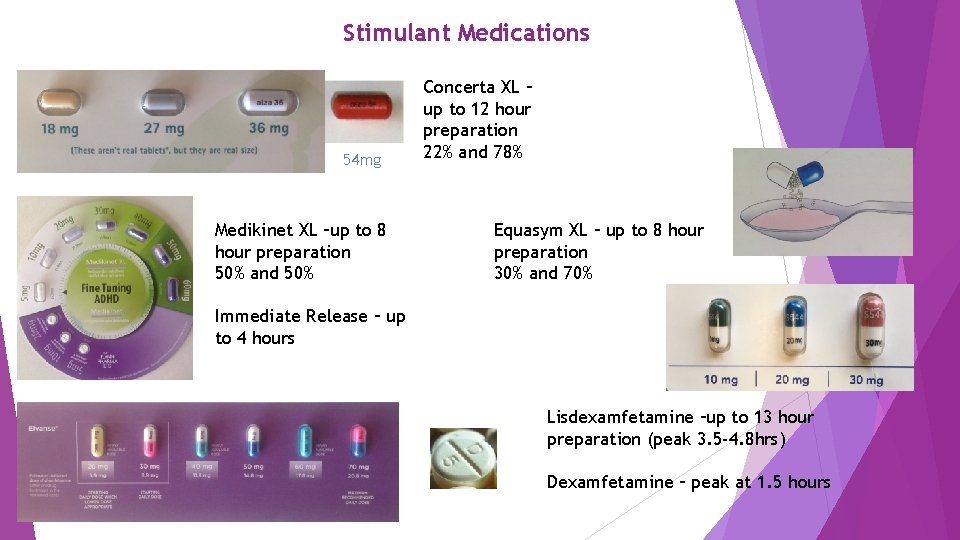
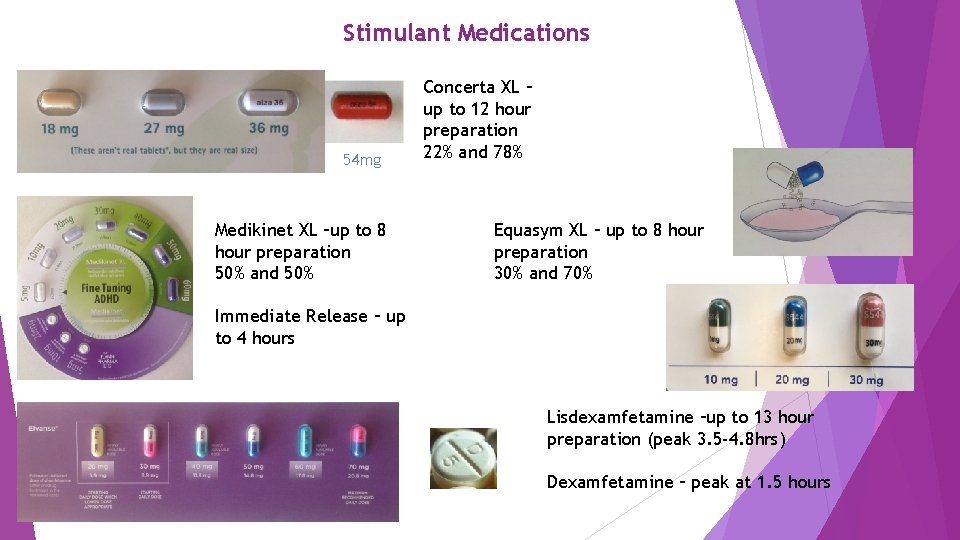
Stimulant Medications 54 mg Medikinet XL –up to 8 hour preparation 50% and 50% Concerta XL – up to 12 hour preparation 22% and 78% Equasym XL – up to 8 hour preparation 30% and 70% Immediate Release – up to 4 hours Lisdexamfetamine –up to 13 hour preparation (peak 3. 5 -4. 8 hrs) Dexamfetamine – peak at 1. 5 hours
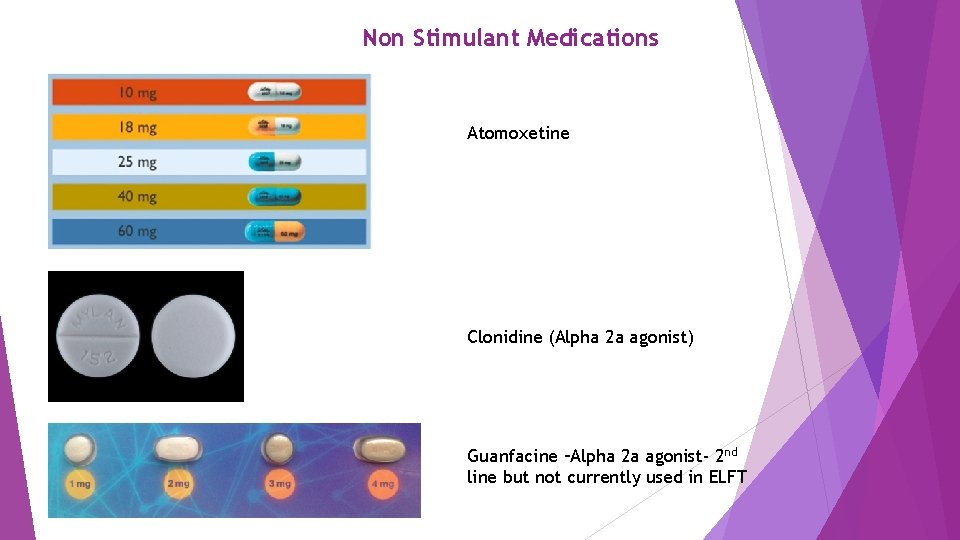
Non Stimulant Medications Atomoxetine Clonidine (Alpha 2 a agonist) Guanfacine –Alpha 2 a agonist- 2 nd line but not currently used in ELFT

Side effects Insomnia Reduced appetite Raised Blood Pressure and Heart Rate Growth deceleration Managed through monitoring and dose reduction if required Atomoxetine – side effects can include low mood + jaundice Potential increased cardiac risk when administered with salbutamol / beta 2 agonists

Medication benefits When dose is optimised, the following benefits are reported: Improved concentration Improved memory (due to improved focus) Better problem solving skills Reduced emotional outbursts Reduced restlessness / agitation Easier to engage in school which can improve outcomes Easier peer relations as able to follow conversations
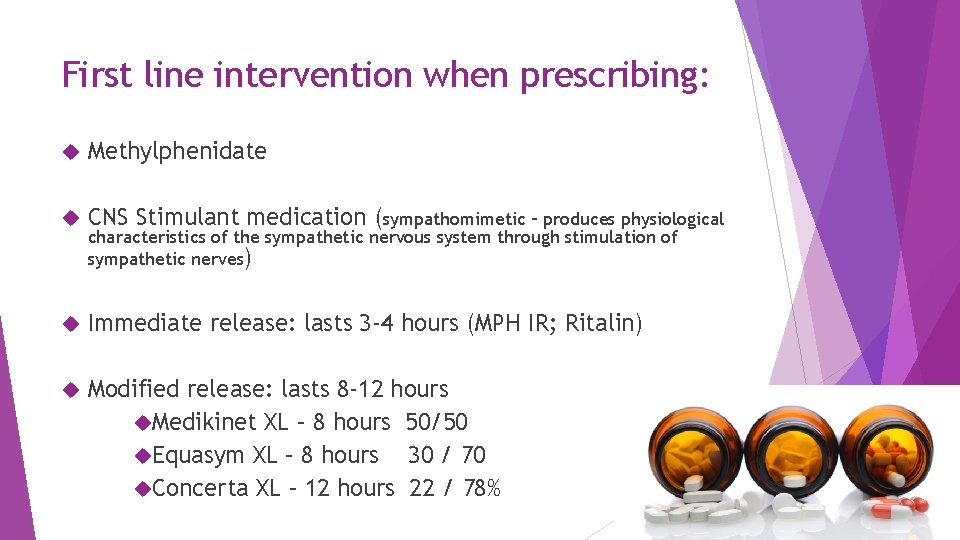
First line intervention when prescribing: Methylphenidate CNS Stimulant medication (sympathomimetic – produces physiological Immediate release: lasts 3 -4 hours (MPH IR; Ritalin) Modified release: lasts 8 -12 hours Medikinet XL – 8 hours 50/50 Equasym XL – 8 hours 30 / 70 Concerta XL – 12 hours 22 / 78% characteristics of the sympathetic nervous system through stimulation of sympathetic nerves)
I think my patient has ADHD……… What next?

Managing Adult ADHD in Hackney Jide Morakinyo Consultant Psychiatrist City and Hackney Adult ADHD Clinic City and Hackney Centre for Mental Health East London NHS Foundation Trust, Homerton Row, E 9 6 SR
Why bother about ADHD? Neurodevelopmental disorder with childhood onset and often persisting into adulthood (Chronic) Common disorder Significant functional impairment, personal distress and reduced quality of life. (education, work, family-life functioning, household economy, and social skills) Co-exist with many other psychiatric disorders and complicating matters. Often unrecognised and with prejudiced and ill informed ideas about it. Important to identify and treat Often responds well to treatment/medication Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
What is ADHD? ADHD is a childhood onset neurodevelopmental condition which manifests as cognitive and behavioural deficits. May persist into adulthood It is characterised by the core symptoms of persistent hyperactivity, impulsiveness and inattention. As well as the presence of the core symptoms identified, there must be clear evidence of psychological, social and/or educational or occupational impairment plus some impairment in two or more settings (home, at work, social, occupational). Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
Bibi: ‘my brain is like pinball machine’. People often say to her that their children have ADHD and she is like them. Attentional deficits and being often restless all through her primary and secondary school years. No longer as hyperactive or restless as she used to be. She has trouble thinking. Most difficult symptom now: problems with focusing and inability le to do things she enjoys because she can’t focus on them. Finds it hard to stay on any task especially when she finds it boring and leaves it uncompleted. She feels frustrated that people can sit down and watch TV and movies, whereas she finds it difficult to relax and sit still to partake in these activities, therefore often she might leave her friends and walk away. She finds this upsetting and disruptive to her social life. Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
School reports - inappropriate noises in class, talking when teachers were talking and arguing with teachers. A teacher commented: ‘Bibi finds it difficult to listen attentively and sustain concentration. Bibi has regularly failed to produce homework’. Other teachers made similar comments: difficulties focusing on tasks, completing homework and not being able to participate meaningfully in class. Couldn’t complete her GCSE and for most of her lessons she wasn’t let into the classes because of her restlessness. Later attended the local college for music productions; experienced same difficulties in the classes, completed the programme but with the lowest level of grades. Currently, an IT engineer apprentice and works at multiple sites: starts some work and leaves and starts something else before one of the managers would point out that she is yet to complete the initial work she started. Relationship problems: problems listening to people, saying there is a lot going on in her brain and not easy listening to people, and therefore she might easily misconstrue what people say to her. In addition, she is easily irritated and gets frustrated, which makes her relationship with her mother, friends and partner very difficult. Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
Avoids cooking, easily forgets and leaves that for hours unattended. Mother advised her not to cook because of fear that she might inadvertently cause fire. For this clinic, she was sent for ECG but she just remembered this in the course of our meeting that she didn’t go for it. She said this is often the pattern for her, as she would forget appointments and things to do. She says ‘my brain is like pinball machine’. Currently, she is on Fluoxetine and feels she was placed on it because she was feeling anxious and that sometimes she feels low in mood. She denies any ongoing psychotic experiences. Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
Genetics Family/adoption/twin studies all support the view that genes contribute to the development of ADHD Parents of an ADHD child ~ 5 times more likely to have ADHD Siblings ~ 4 times more likely to have ADHD than the general population Genetic causes of ADHD account for most of the variability in the presentation of the disorder, Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
Biology PET scan imaging indicates that methylphenidate acts to increase dopamine The neurotransmitters dopamine and norepinephrine have been associated with ADHD. The underlying brain regions predominantly thought to be involved are frontal and prefrontal. Other studies have shown structural alterations in other parts of the brain Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
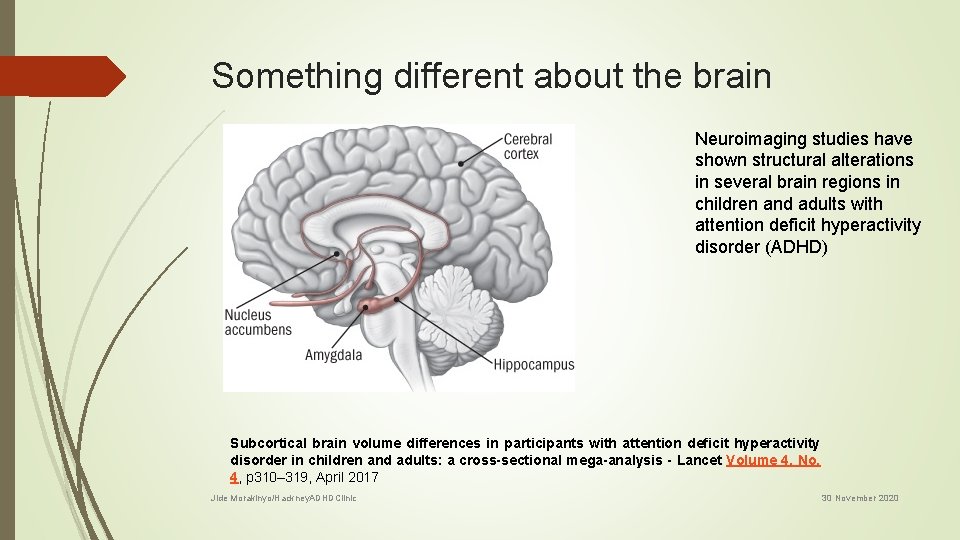
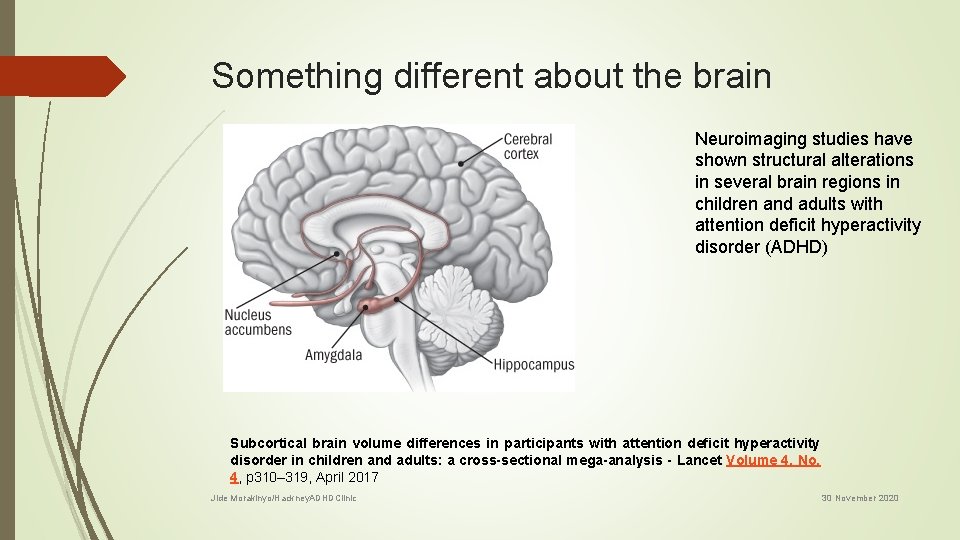
Something different about the brain Neuroimaging studies have shown structural alterations in several brain regions in children and adults with attention deficit hyperactivity disorder (ADHD) Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis - Lancet Volume 4, No. 4, p 310– 319, April 2017 Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
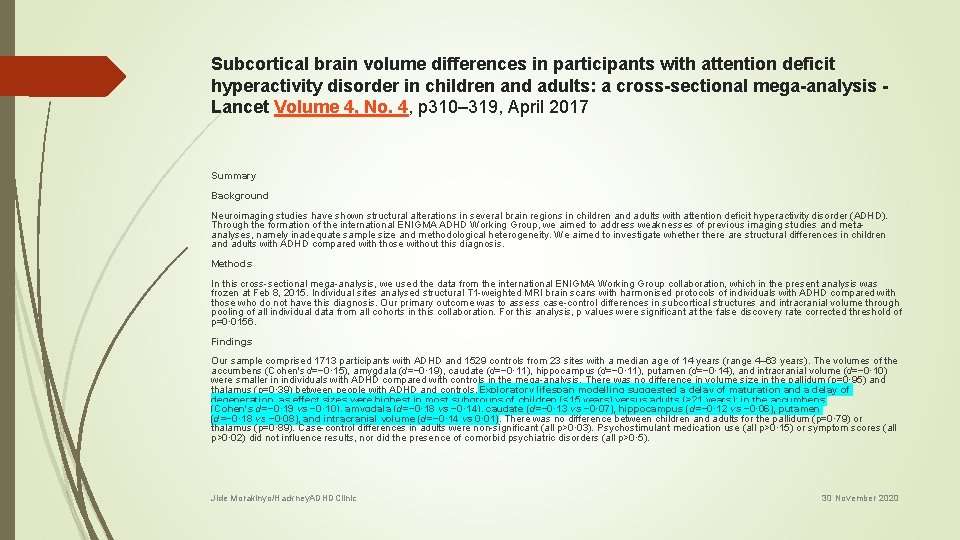
Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis - Lancet Volume 4, No. 4, p 310– 319, April 2017 Summary Background Neuroimaging studies have shown structural alterations in several brain regions in children and adults with attention deficit hyperactivity disorder (ADHD). Through the formation of the international ENIGMA ADHD Working Group, we aimed to address weaknesses of previous imaging studies and metaanalyses, namely inadequate sample size and methodological heterogeneity. We aimed to investigate whethere are structural differences in children and adults with ADHD compared with those without this diagnosis. Methods In this cross-sectional mega-analysis, we used the data from the international ENIGMA Working Group collaboration, which in the present analysis was frozen at Feb 8, 2015. Individual sites analysed structural T 1 -weighted MRI brain scans with harmonised protocols of individuals with ADHD compared with those who do not have this diagnosis. Our primary outcome was to assess case-control differences in subcortical structures and intracranial volume through pooling of all individual data from all cohorts in this collaboration. For this analysis, p values were significant at the false discovery rate corrected threshold of p=0· 0156. Findings Our sample comprised 1713 participants with ADHD and 1529 controls from 23 sites with a median age of 14 years (range 4– 63 years). The volumes of the accumbens (Cohen's d=− 0· 15), amygdala (d=− 0· 19), caudate (d=− 0· 11), hippocampus (d=− 0· 11), putamen (d=− 0· 14), and intracranial volume (d=− 0· 10) were smaller in individuals with ADHD compared with controls in the mega-analysis. There was no difference in volume size in the pallidum (p=0· 95) and thalamus (p=0· 39) between people with ADHD and controls. Exploratory lifespan modelling suggested a delay of maturation and a delay of degeneration, as effect sizes were highest in most subgroups of children (<15 years) versus adults (>21 years): in the accumbens (Cohen's d=− 0· 19 vs − 0· 10), amygdala (d=− 0· 18 vs − 0· 14), caudate (d=− 0· 13 vs − 0· 07), hippocampus (d=− 0· 12 vs − 0· 06), putamen (d=− 0· 18 vs − 0· 08), and intracranial volume (d=− 0· 14 vs 0· 01). There was no difference between children and adults for the pallidum (p=0· 79) or thalamus (p=0· 89). Case-control differences in adults were non-significant (all p>0· 03). Psychostimulant medication use (all p>0· 15) or symptom scores (all p>0· 02) did not influence results, nor did the presence of comorbid psychiatric disorders (all p>0· 5). Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
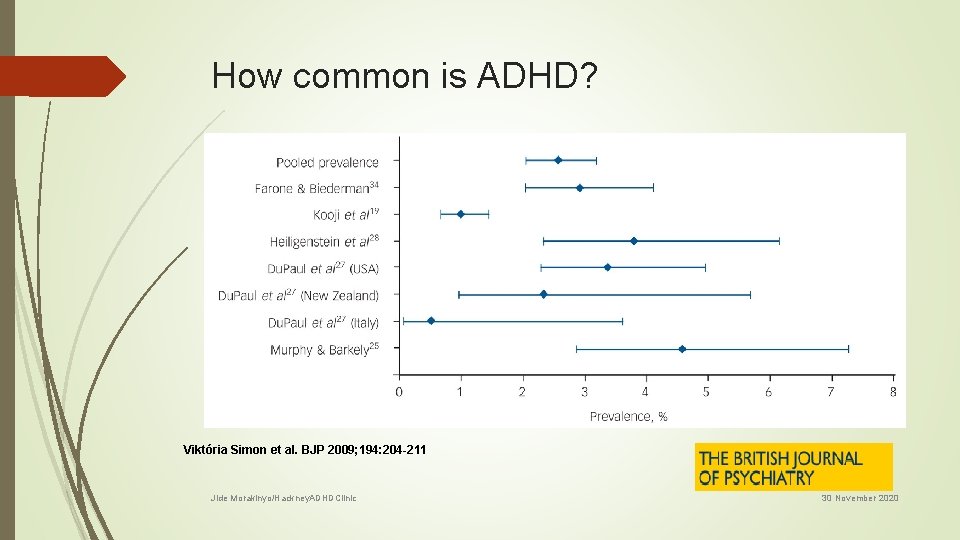
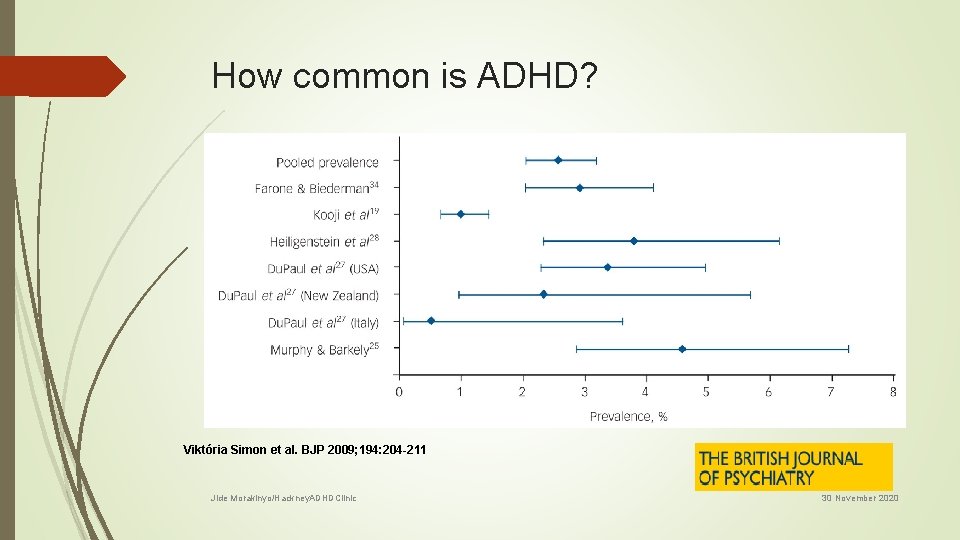
How common is ADHD? Viktória Simon et al. BJP 2009; 194: 204 -211 Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
NICE multidisciplinary specialist ADHD teams and/or clinics expertise in the diagnosis and management of ADHD provide diagnostic, treatment and consultation services for people with ADHD produce local protocols for shared care arrangements with primary care providers ensure age-appropriate psychological services are available Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
Treatments Comprehensive treatment programme that focuses on psychological, behavioural and educational or occupational needs. Medication Psychological interventions Social interventions Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
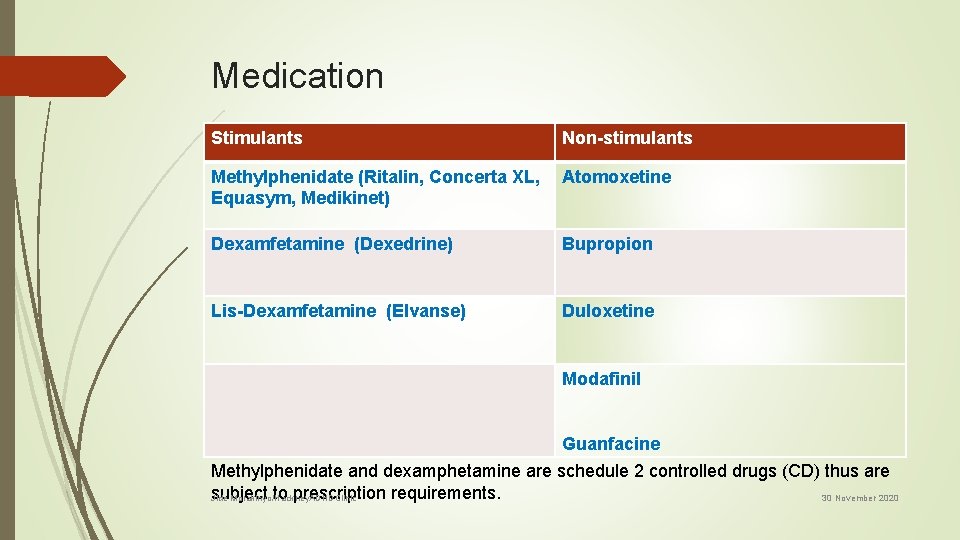
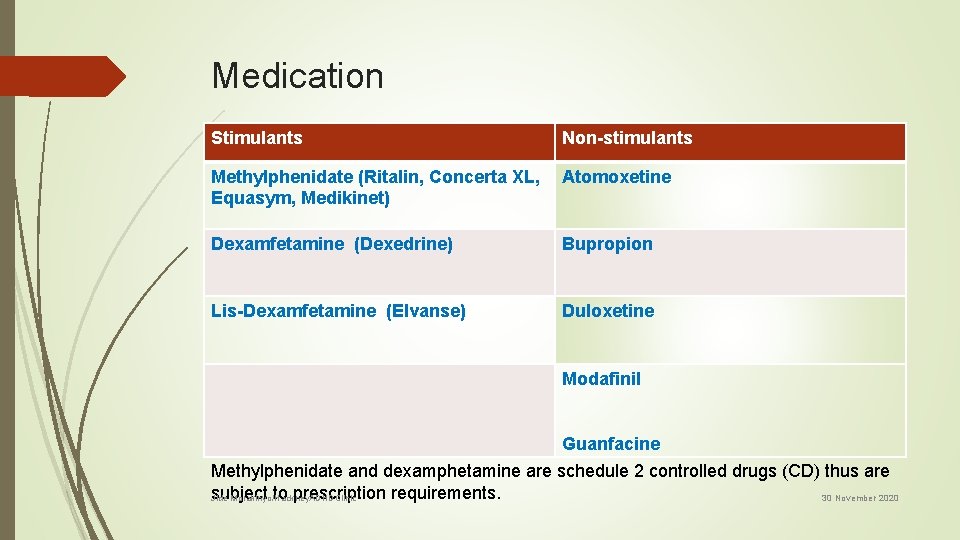
Medication Stimulants Non-stimulants Methylphenidate (Ritalin, Concerta XL, Atomoxetine Equasym, Medikinet) Dexamfetamine (Dexedrine) Bupropion Lis-Dexamfetamine (Elvanse) Duloxetine Modafinil Guanfacine Methylphenidate and dexamphetamine are schedule 2 controlled drugs (CD) thus are subject to prescription requirements. 30 November 2020 Jide Morakinyo/Hackney. ADHDClinic
NICE – Licensing arrangements Methylphenidate, Dexamfetamine and atomoxetine do not have UK marketing authorisation for use in adults with ADHD. Atomoxetine is licensed for adults with ADHD when the drug has been started in childhood. Informed consent should be obtained and documented. Drug treatment for adults with ADHD should be started only under the guidance of a psychiatrist, nurse prescriber specialising in ADHD, or other clinical prescriber with training in the diagnosis and management of ADHD Good knowledge of the drugs used in the treatment of ADHD and their different preparations is essential (refer to the BNF and summaries of product characteristics). Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
City and Hackney ADHD Team • Supernumerary Psychologist: 3 hrs/Week • Clinical Psychologist (Band 7): 0. 5 wte • Staff grade/SHO ~ 4 PA/week • Sp. R on special interest ~ 1 PA/week • Consultant ~ 1. 5 PA/week • Operational lead – Ms Maria Lee • Admin support Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
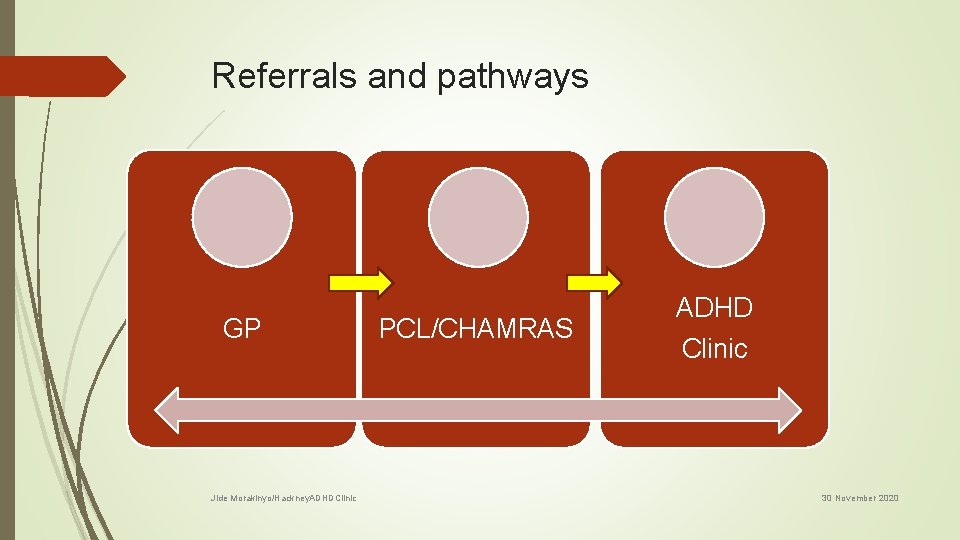
Referrals and pathways GP Jide Morakinyo/Hackney. ADHDClinic PCL/CHAMRAS ADHD Clinic 30 November 2020
Shared Care Protocol Copy of this on CCG Website An updated version should be available in coming weeks This document defines the roles of each professional involved Patients often get a copy Highlights for GP Jide Morakinyo/Hackney. ADHDClinic 30 November 2020
Conclusion Adult ADHD is a valid diagnosis and a common and disabling disorder Often co-exists with other psychiatric disorders Requires a thorough assessment by professional with expertise in diagnosis and treatment ADHD Mental health teams/services should provide clinics or MTD team providing diagnostic & treatment Treatment encompasses medication and appropriate psychosocial interventions. Good knowledge of drugs used to treat ADHD in very important Jide Morakinyo/Hackney. ADHDClinic 30 November 2020