Special Topics in CostEffectiveness Analysis Indirect Costs Discounting
- Slides: 20
Special Topics in Cost-Effectiveness Analysis: Indirect Costs, Discounting Gerald F. Kominski, Ph. D. Professor, UCLA Department of Health Services 1
Direct Costs n Health Care Costs - Hospital costs - Other institutional costs, including nursing home, rehabilitation, etc. - Ambulatory costs, including physicians, home health services, etc. - Pharmaceuticals n Non-Health Care Costs - Costs borne by patients and their families, including travel costs, time lost from work, etc. - Costs borne by society, such as criminal justice system costs 2
Direct Costs n Caregiving Costs - Both unpaid voluntary care as well as purchased services n Patient Time Costs (in Treatment) - Opportunity cost of receiving care - Equal to foregone income or value of time in next best activity - Recuperation time and recovery time are captured in the quality of life measure 3
Indirect Costs Productivity costs related: n Morbidity, including lost ability to work and lost functionality to engage in leisure activity n Mortality, i. e. , the loss of economic productivity due to premature death - Medical costs of mortality should be captured in the measurement of direct health care costs 4
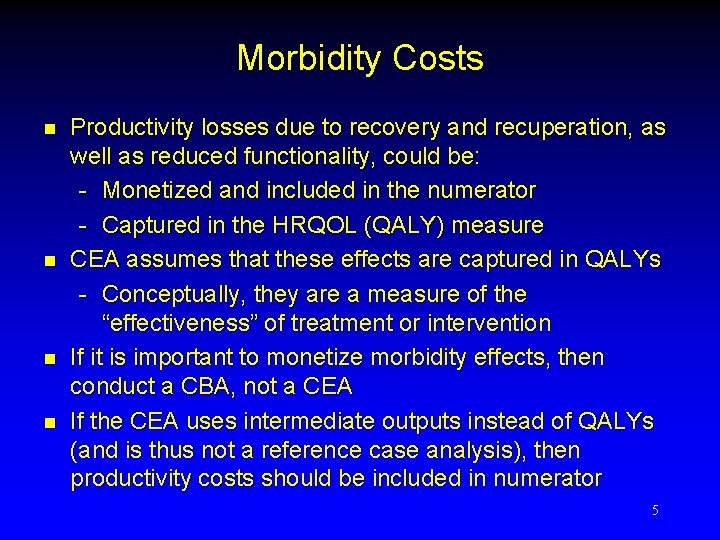
Morbidity Costs n n Productivity losses due to recovery and recuperation, as well as reduced functionality, could be: - Monetized and included in the numerator - Captured in the HRQOL (QALY) measure CEA assumes that these effects are captured in QALYs - Conceptually, they are a measure of the “effectiveness” of treatment or intervention If it is important to monetize morbidity effects, then conduct a CBA, not a CEA If the CEA uses intermediate outputs instead of QALYs (and is thus not a reference case analysis), then productivity costs should be included in numerator 5
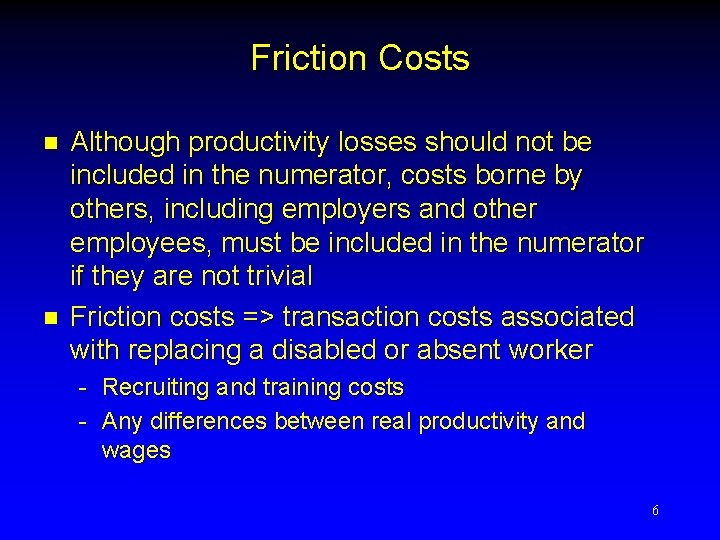
Friction Costs n n Although productivity losses should not be included in the numerator, costs borne by others, including employers and other employees, must be included in the numerator if they are not trivial Friction costs => transaction costs associated with replacing a disabled or absent worker - Recruiting and training costs - Any differences between real productivity and wages 6
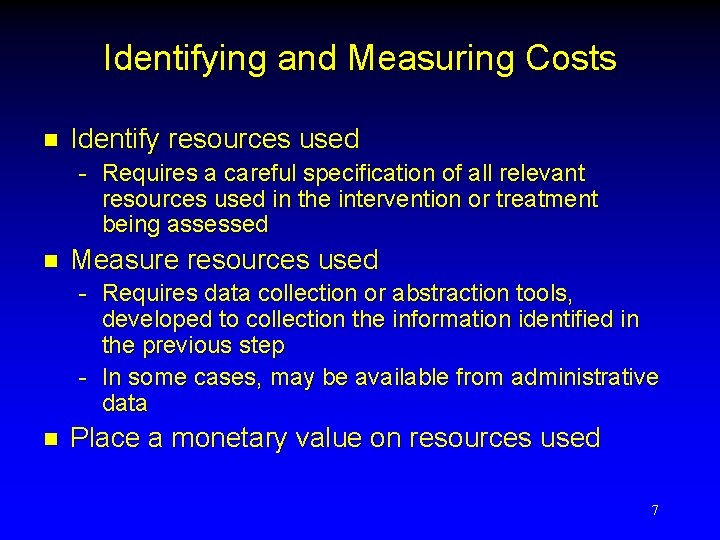
Identifying and Measuring Costs n Identify resources used - Requires a careful specification of all relevant resources used in the intervention or treatment being assessed n Measure resources used - Requires data collection or abstraction tools, developed to collection the information identified in the previous step - In some cases, may be available from administrative data n Place a monetary value on resources used 7
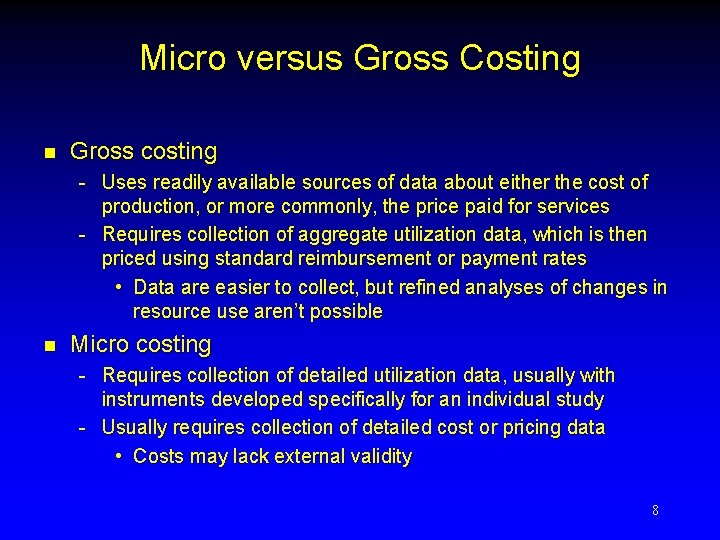
Micro versus Gross Costing n Gross costing - Uses readily available sources of data about either the cost of production, or more commonly, the price paid for services - Requires collection of aggregate utilization data, which is then priced using standard reimbursement or payment rates • Data are easier to collect, but refined analyses of changes in resource use aren’t possible n Micro costing - Requires collection of detailed utilization data, usually with instruments developed specifically for an individual study - Usually requires collection of detailed cost or pricing data • Costs may lack external validity 8
Measuring Costs n Pharmaceuticals - acquisition costs - costs of administering, monitoring, compliance n Hospitals - time and motion studies may be necessary to obtain accurate measure of resources used in treatment - costs are often estimated from charges using the ratio of costs-to-charges (RCC) - public payment rates, such as Medicare DRG rates, can be used if we assume that marginal revenue for public payers (roughly) equals marginal costs 9
Measuring Costs n Physicians - Cost data are virtually impossible to obtain - Payment data, such as Medicare payment rates based on the Resource-Based Relative Value Scale, may be used assuming that marginal revenue roughly equals marginal cost - Private payment data is commercially available • MEDSTAT 10
Measuring Costs n Personal/Family Costs - Often ignored, because in CEA/CUA, costs of lost productivity or functional status are already included in outcome measure (i. e. , QALY) - Depending on the intervention, may be important • Caregiver costs, including costs related to lost days of school • Travel costs • Time in treatment n Social Costs - Criminal justice system • May be important for MH and SA interventions - Social services 11
Measuring Costs n Induced costs, i. e. , costs of added years of life - may have a large impact on programs with low CE ratios - Panel on Cost-Effectiveness in Health and Medicine suggests ignoring these costs, unless they are likely to have a large impact 12
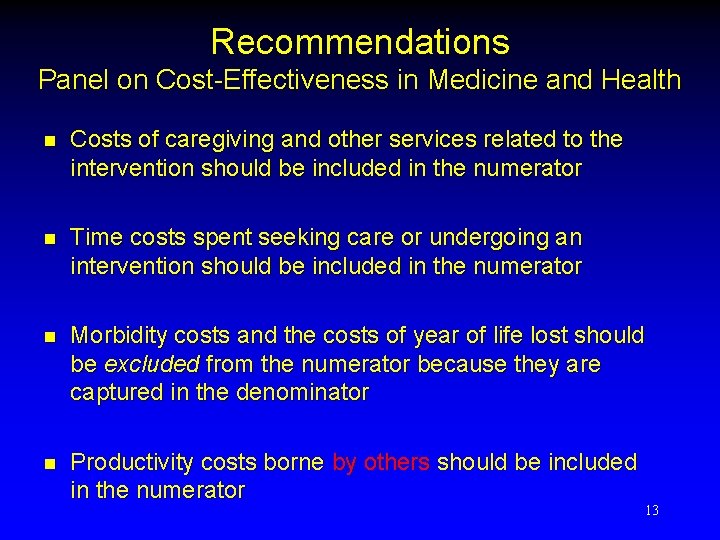
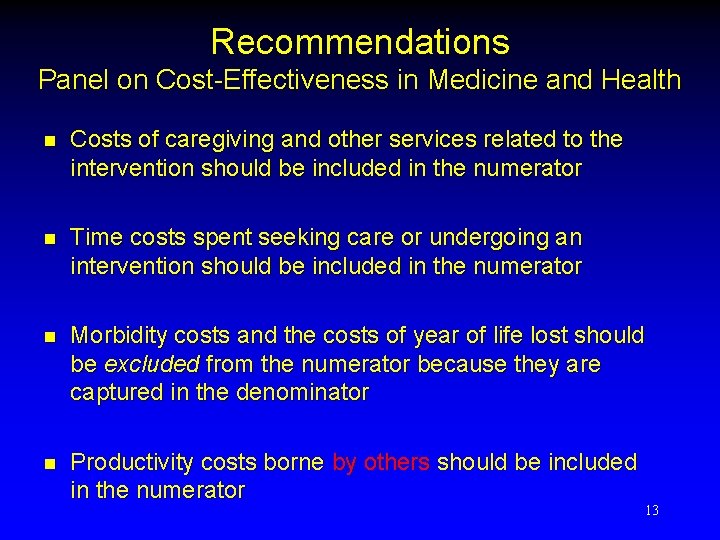
Recommendations Panel on Cost-Effectiveness in Medicine and Health n Costs of caregiving and other services related to the intervention should be included in the numerator n Time costs spent seeking care or undergoing an intervention should be included in the numerator n Morbidity costs and the costs of year of life lost should be excluded from the numerator because they are captured in the denominator n Productivity costs borne by others should be included in the numerator 13
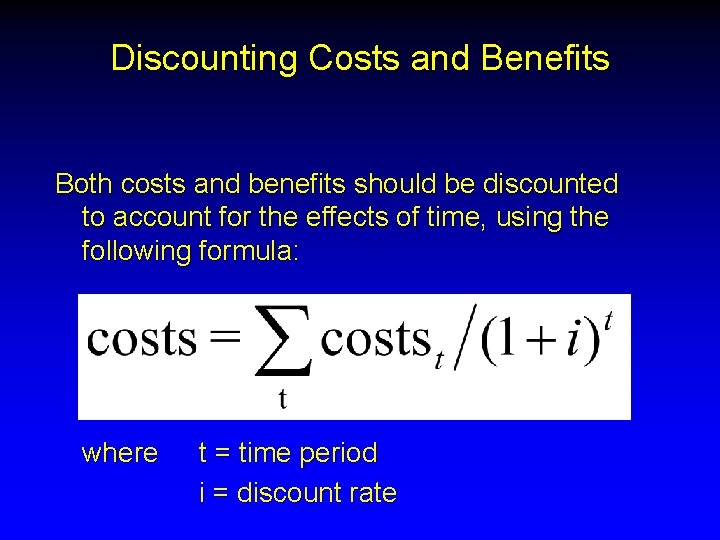
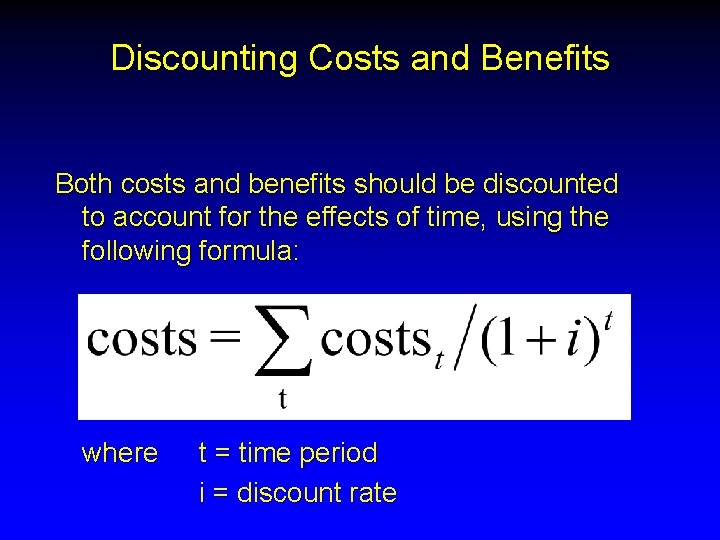
Discounting Costs and Benefits Both costs and benefits should be discounted to account for the effects of time, using the following formula: where t = time period i = discount rate
Discounting Costs vs. Benefits discounting is justified because of: n time preference rate of consumption => we will accept less of a good in order to use it today rather than next year, or we require compensation for delaying use of a good n opportunity costs => rate of return on capital in private markets
Discounting Costs vs. Benefits (cont. ) n but is our time preference for wealth different from our time preference for health? - some studies have shown that individuals are more risk averse in choices involving years of life than in financial matters - one obvious reason is that wealth can be reacquired if lost, whereas health and years of life cannot n Olsen (1993) concludes that time preferences for health are different, and research is needed to elicit the appropriate time preferences for health Olsen JA. On what basis should health be discounted? J Health Econ 1993; 12: 39 -53.
Recommendations Panel on Cost-Effectiveness in Medicine and Health n n Costs and outcomes should be discounted using the same discount rate, to avoid the Keeler-Cretin paradox (Keeler and Cretin, 1983) Discount rate should reflect the shadow price of capital - Reflects the trade-off between present and future consumption made by social decision makers - Social rate of time preference (SRTP) - SRTP has been pegged to the real rate of return on low-risk, long-term government investments, roughly 3% n 3% is therefore the preferred discount rate - Because so many studies have been conducted using 5%, studies should also include a 5% discount rate - Sensitivity analyses should be conducted ranging from 0% to 7% Keeler EB, Cretin S. Discounting of life-saving and other nonmonetary effects. Management Sci 1983; 29: 300– 306.
Is There A Suitable Alternative to Using a Constant Discount Rate? n Discounting seems most problematic for interventions where most of the costs are borne in the present, but most of the benefits accrue in the (distant) future - Most health promotion/preventive measures Is prevention better than cure? Underinvestment in health promotion/disease prevention by health insurers, because benefits accrue to someone other than the payer (market failure due to externality) 18
Is There A Suitable Alternative to Using a Constant Discount Rate? n n Some empirical research suggests that individuals have high discount rates (i. e. , high time preference) for health benefits in the near future, but lower discount rates for health benefits in the more distant future Similarly, older individuals may have higher time preferences for health benefits than younger individuals, reflecting their shorter (relative) life expentencies 19
Is There A Suitable Alternative to Using a Constant Discount Rate? n One alternative to a constant discount rate, therefore, is a declining (hyperbolic) discount rate - Substitute discount factor = 1 / (1 + r) t with discount factor = 1 / (1 + r * a(t)) where a(t) = b / (b + t) and b > 0 n Disadvantages: - CE ratios can shift over time solely due to the passage of time => choices become time variant • This may make sense from an individual perspective, but does it make sense from a societal perspective? - Incompatibility with vast majority of published studies 20