Special Sensations A Olfactory 1 Receptors are chemoreceptors


- Slides: 63

Special Sensations
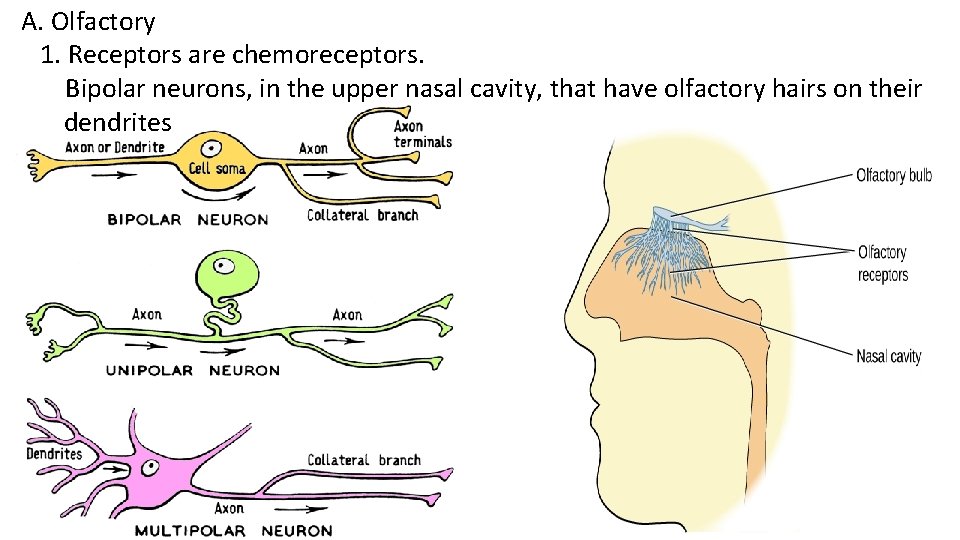
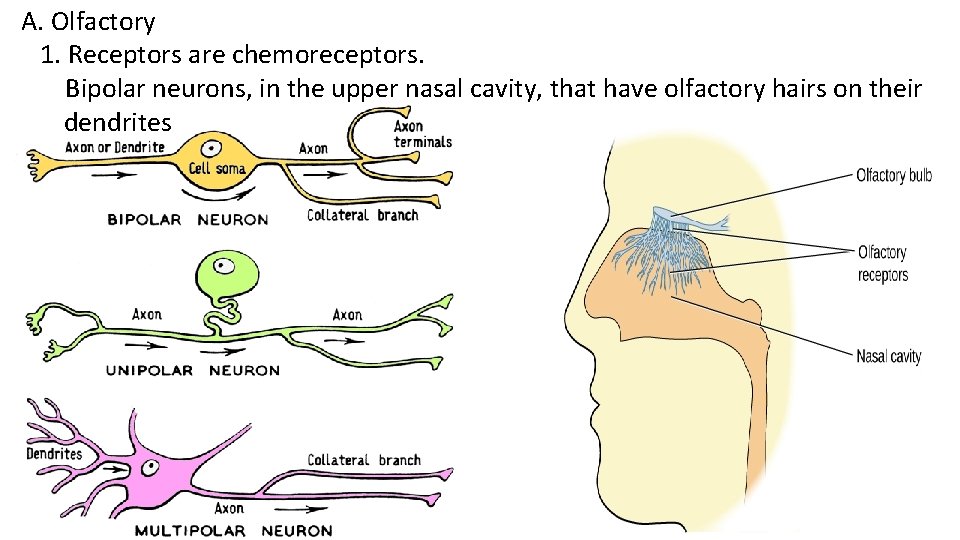
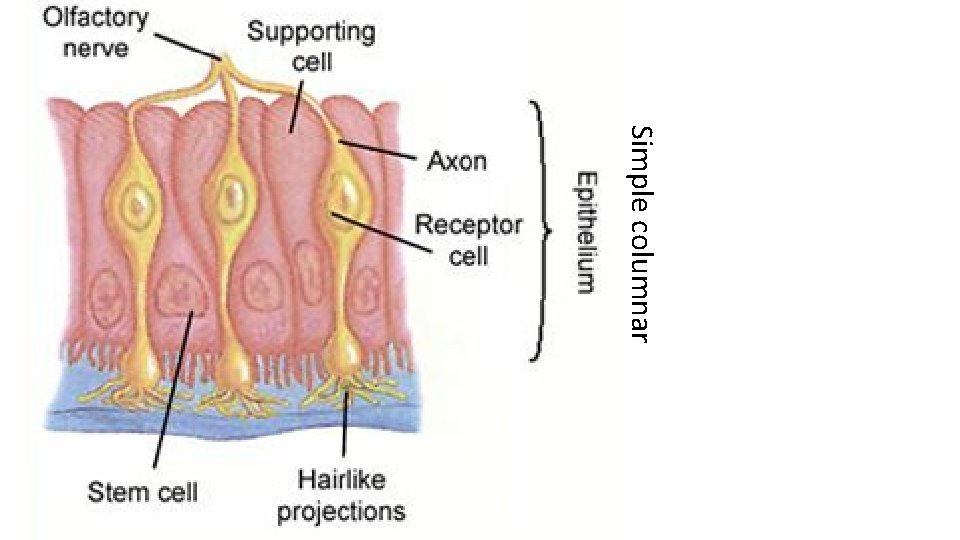
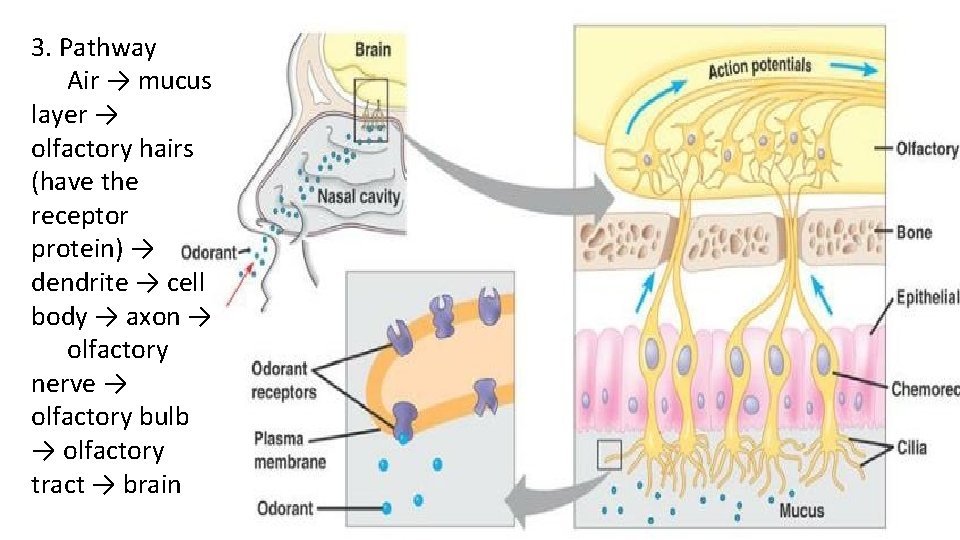
A. Olfactory 1. Receptors are chemoreceptors. Bipolar neurons, in the upper nasal cavity, that have olfactory hairs on their dendrites
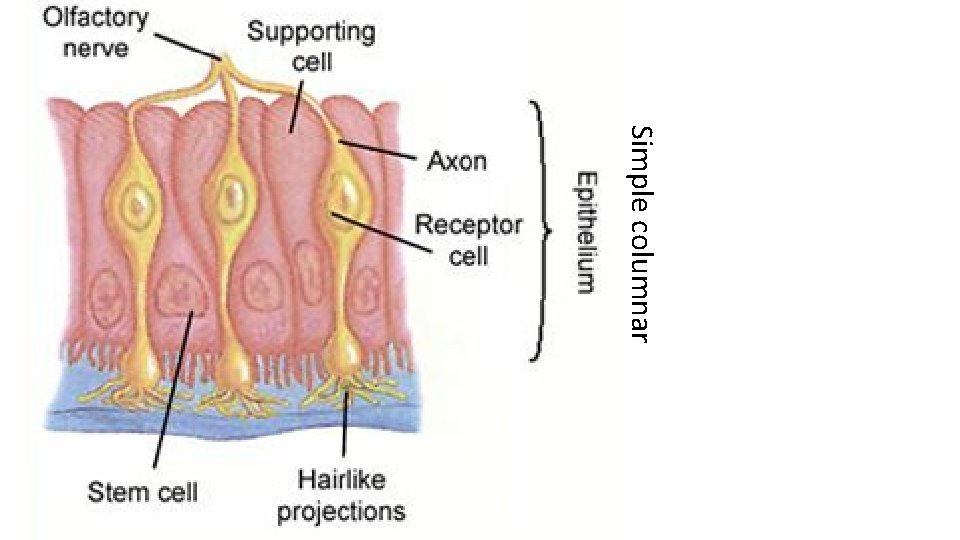
Simple columnar
2. To be smelled a substance must be (a) Gaseous (b) Water and lipid soluble
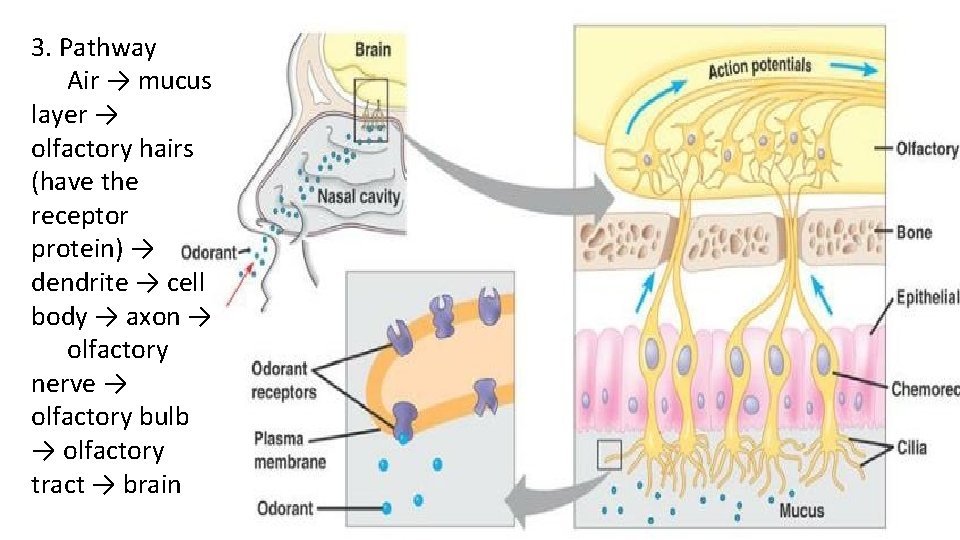
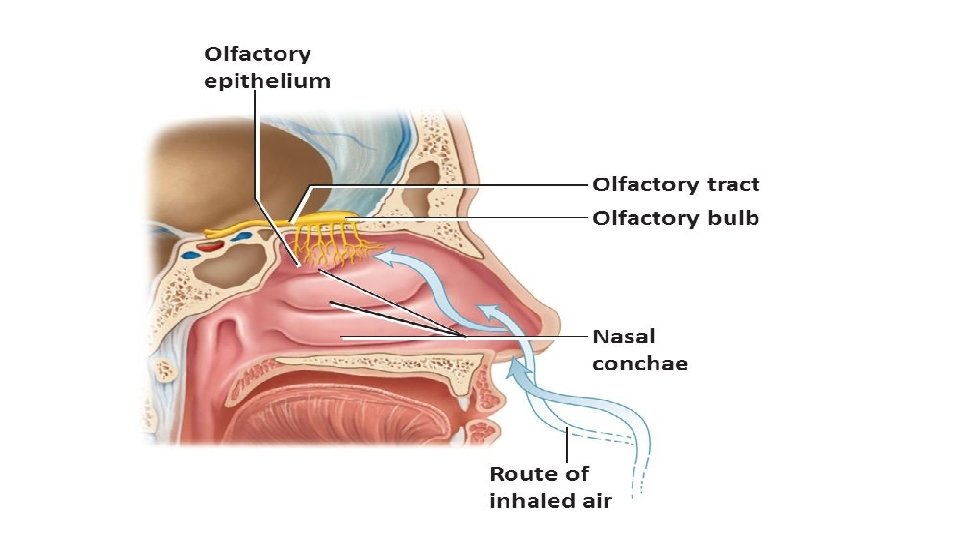
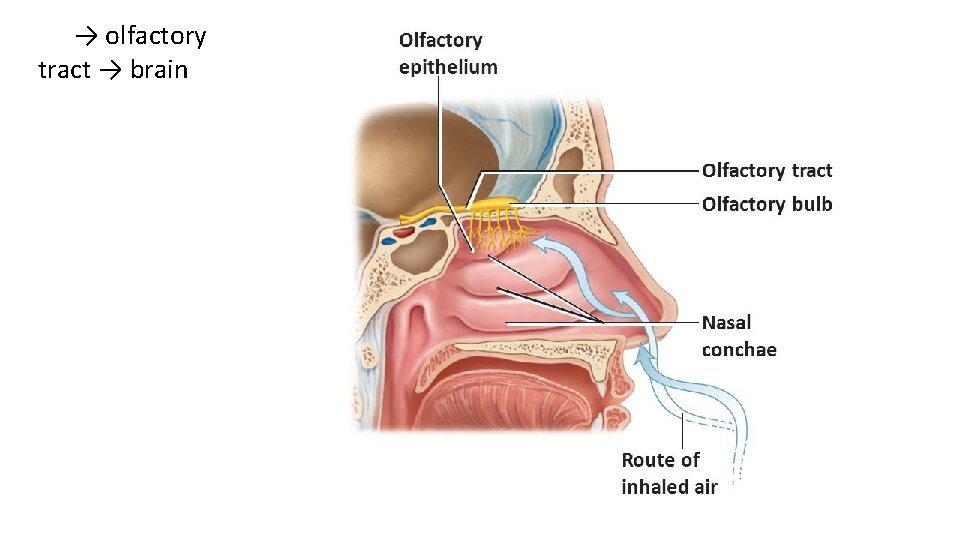
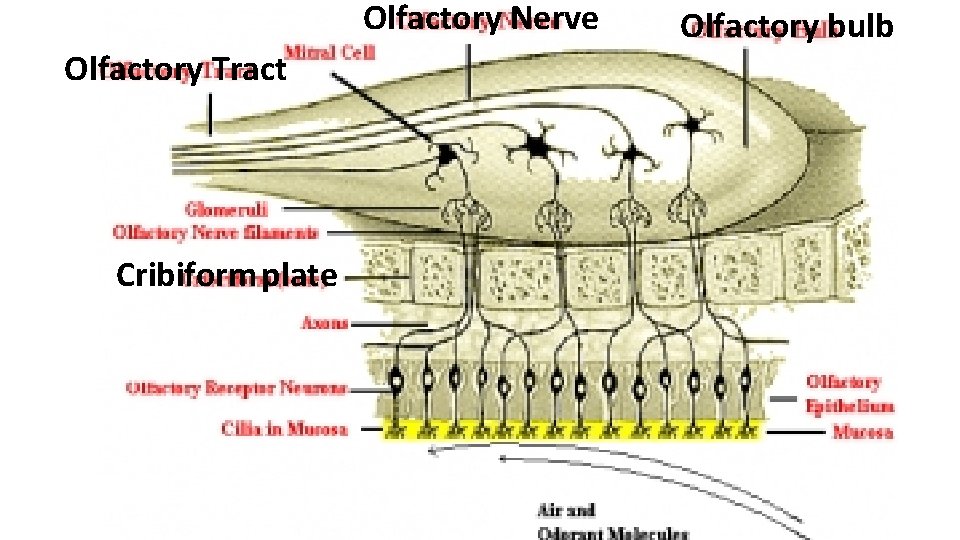
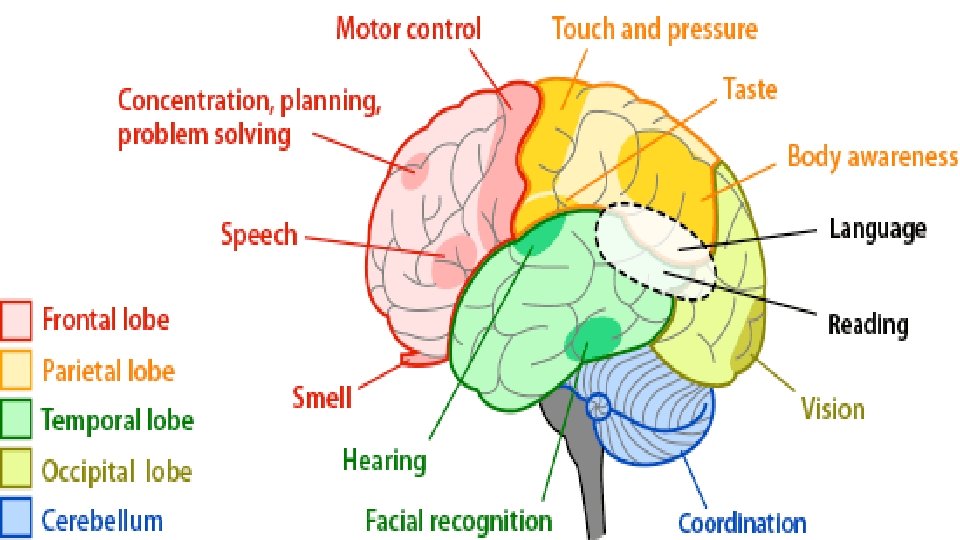
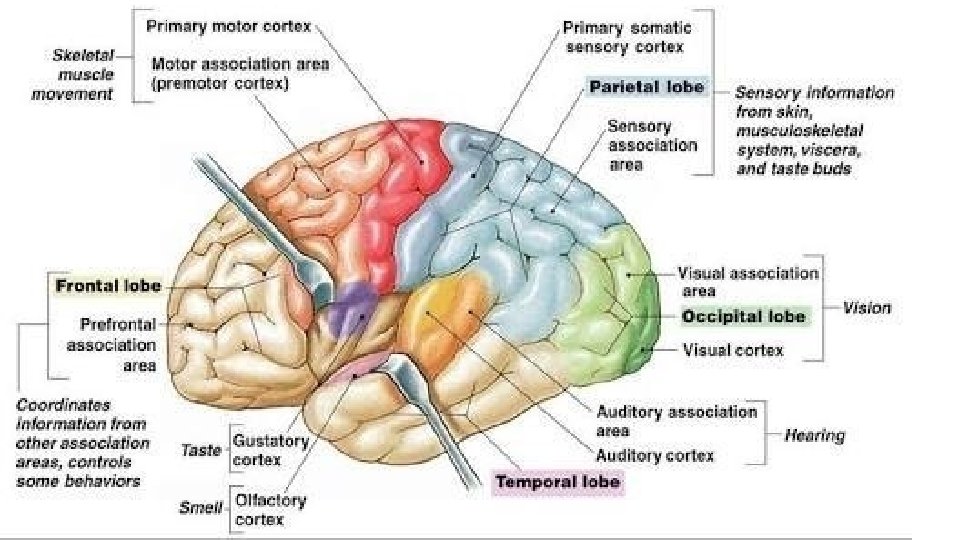
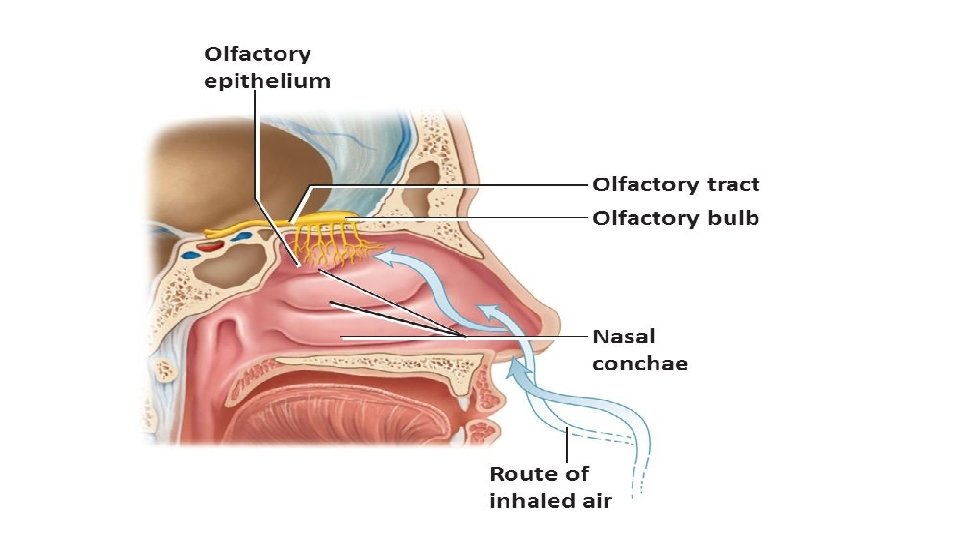
3. Pathway Air → mucus layer → olfactory hairs (have the receptor protein) → dendrite → cell body → axon → olfactory nerve → olfactory bulb → olfactory tract → brain
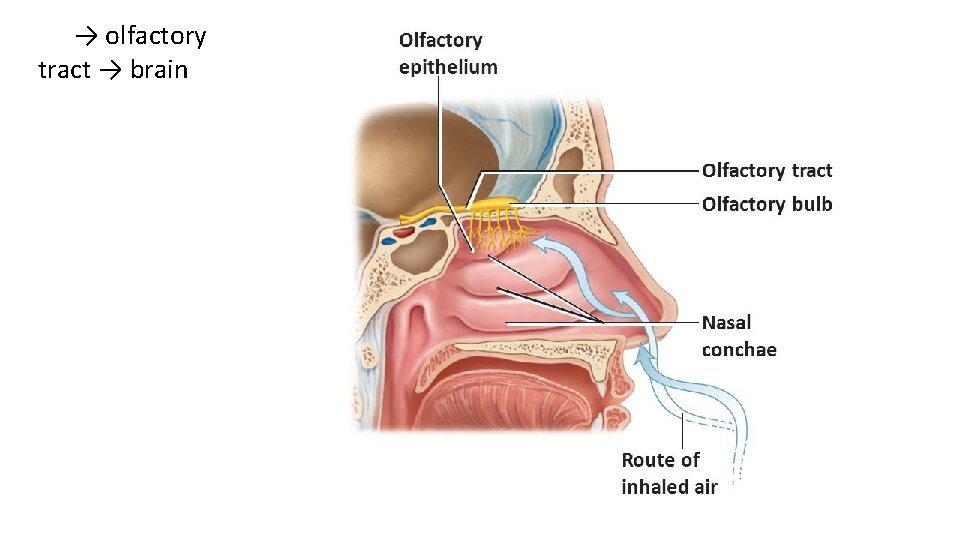
→ olfactory tract → brain
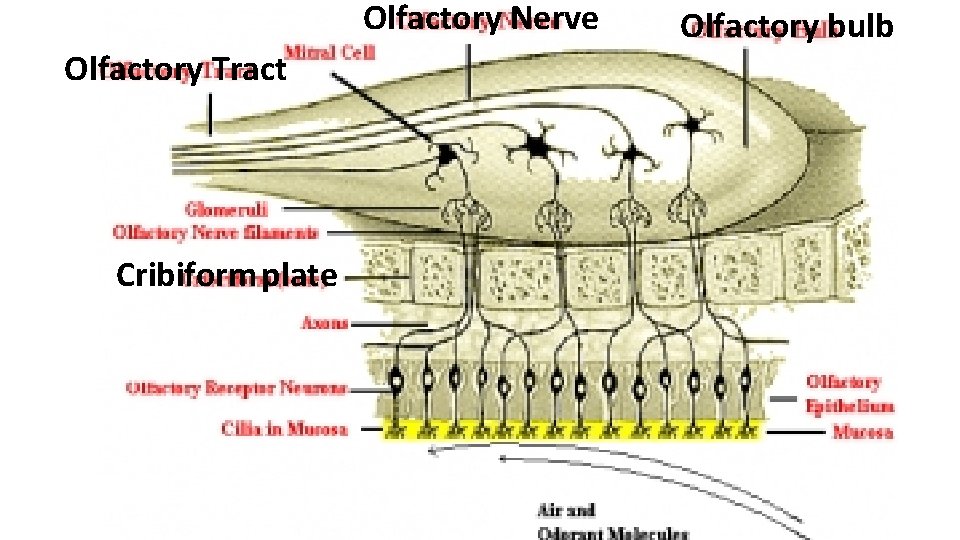
Olfactory Nerve Olfactory Tract Cribiform plate Olfactory bulb
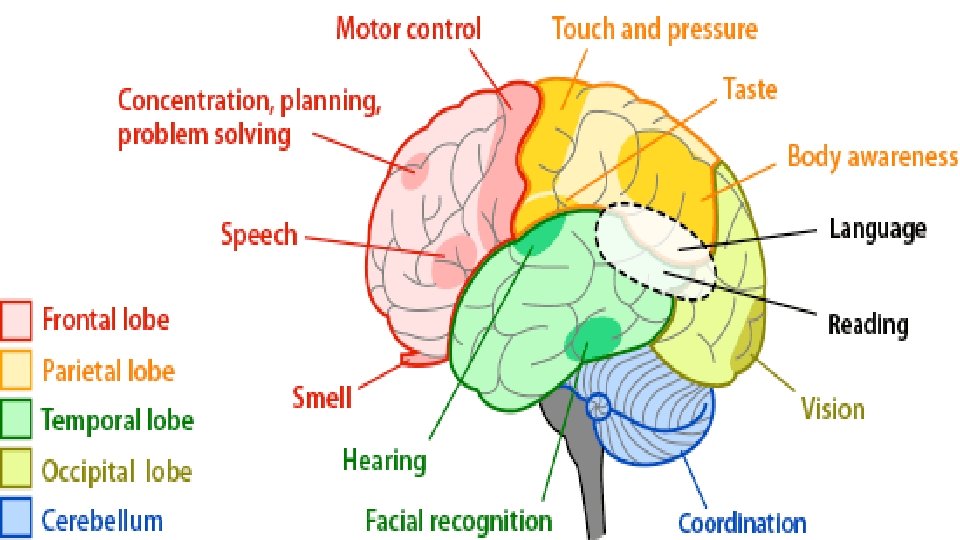
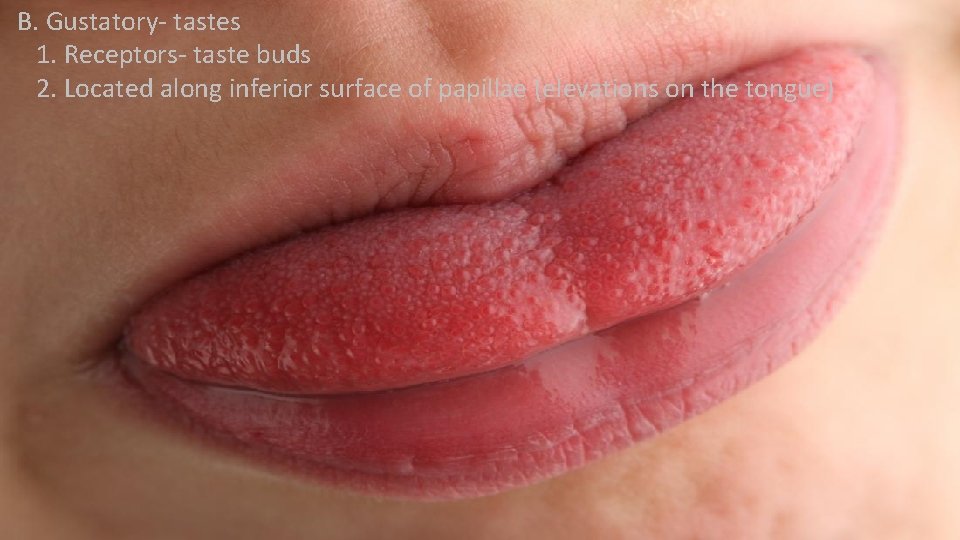
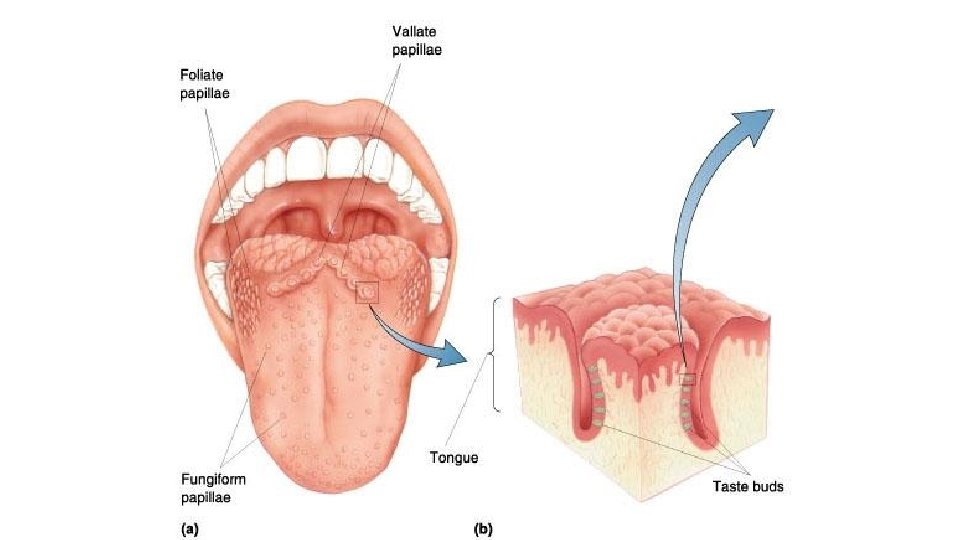
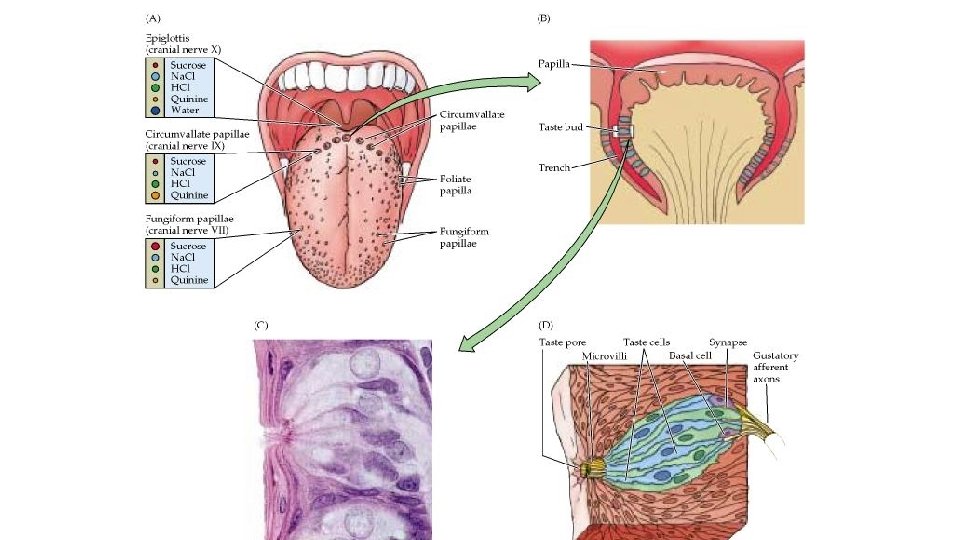
B. Gustatory- tastes 1. Receptors- taste buds 2. Located along inferior surface of papillae (elevations on the tongue)
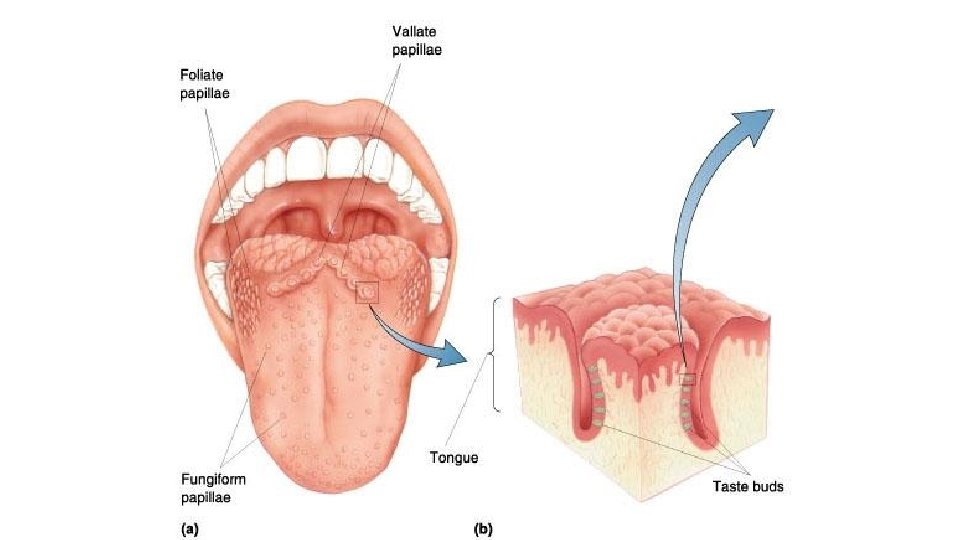
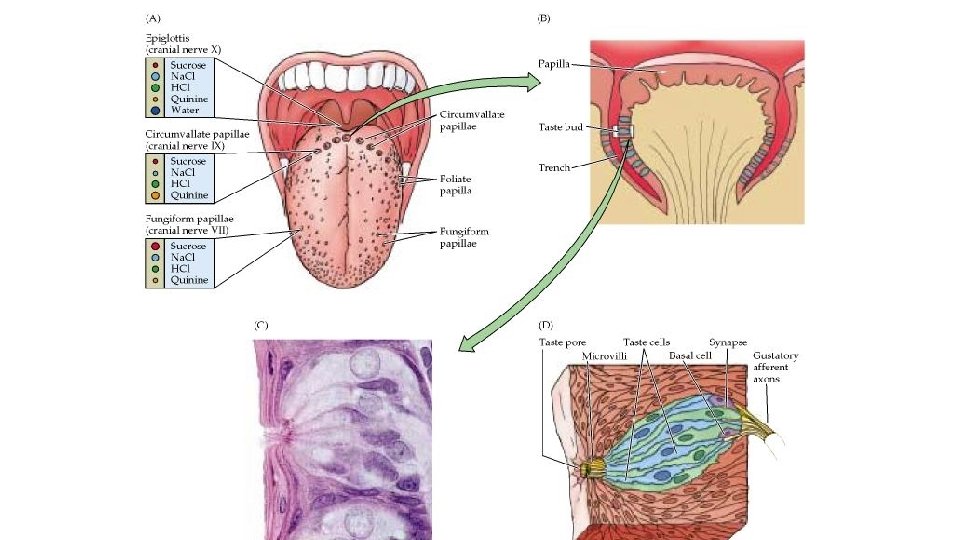
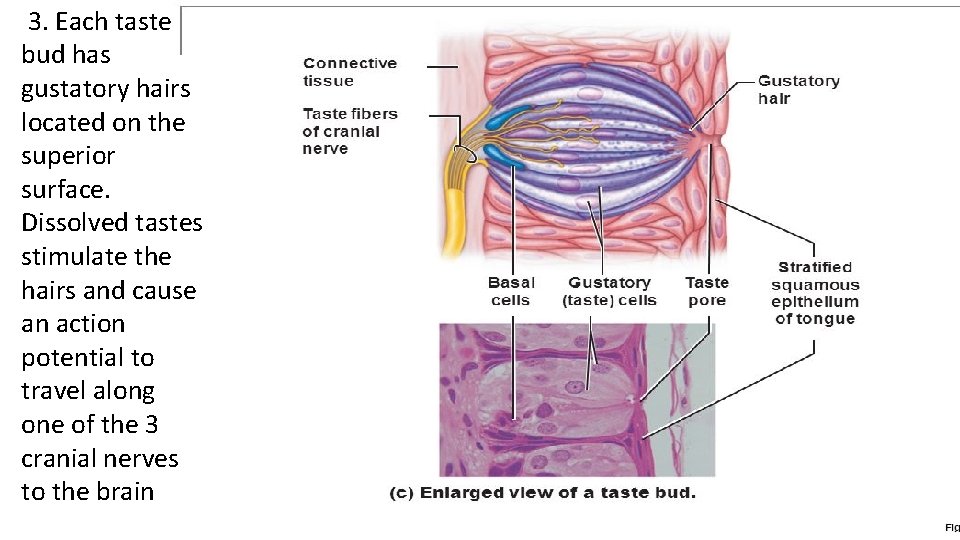
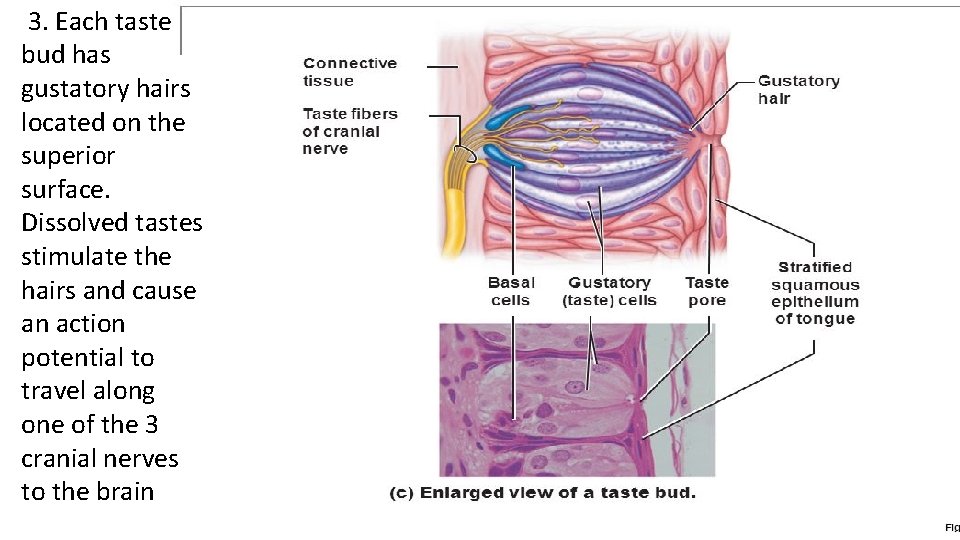
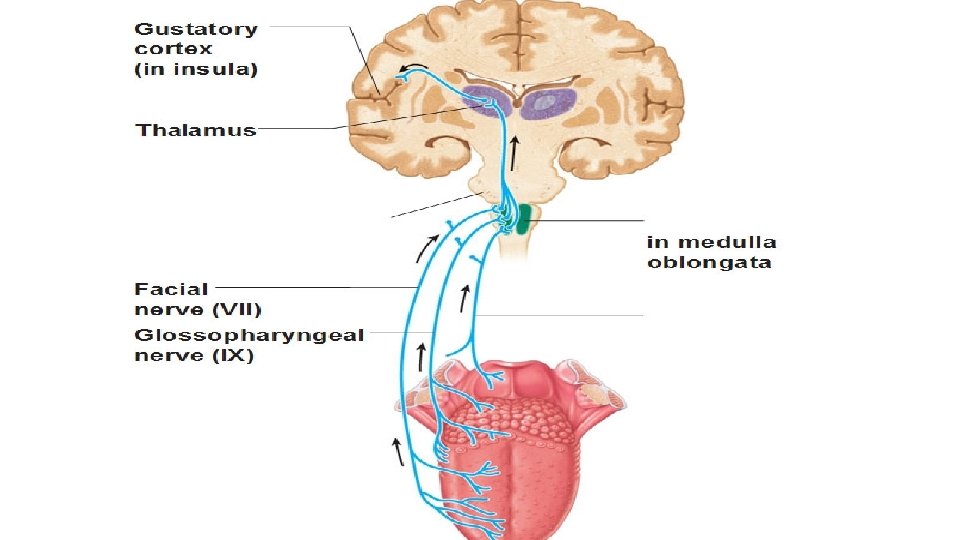
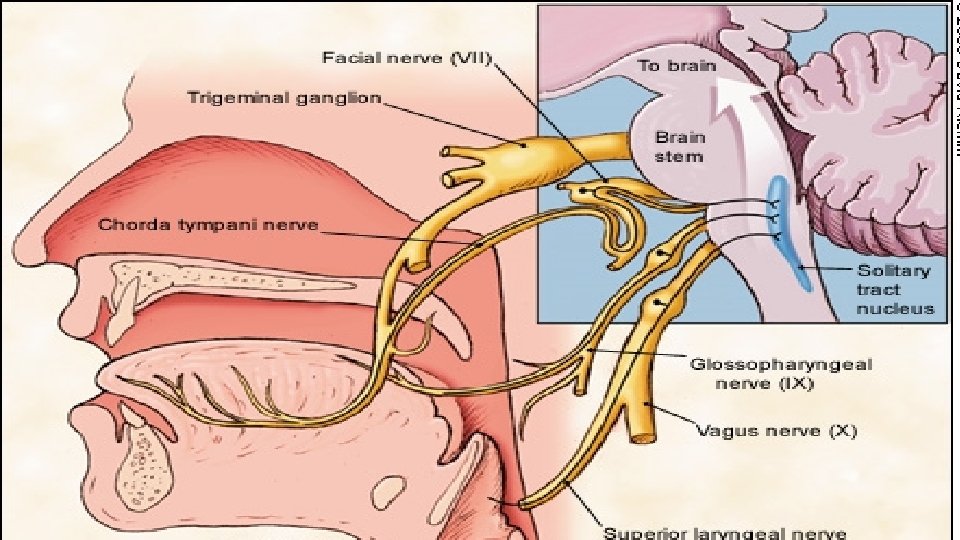
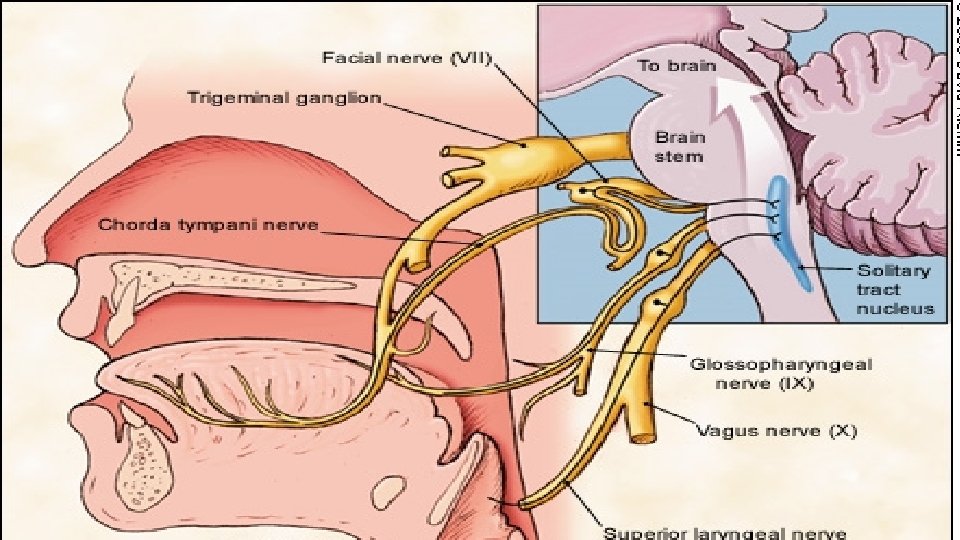
3. Each taste bud has gustatory hairs located on the superior surface. Dissolved tastes stimulate the hairs and cause an action potential to travel along one of the 3 cranial nerves to the brain
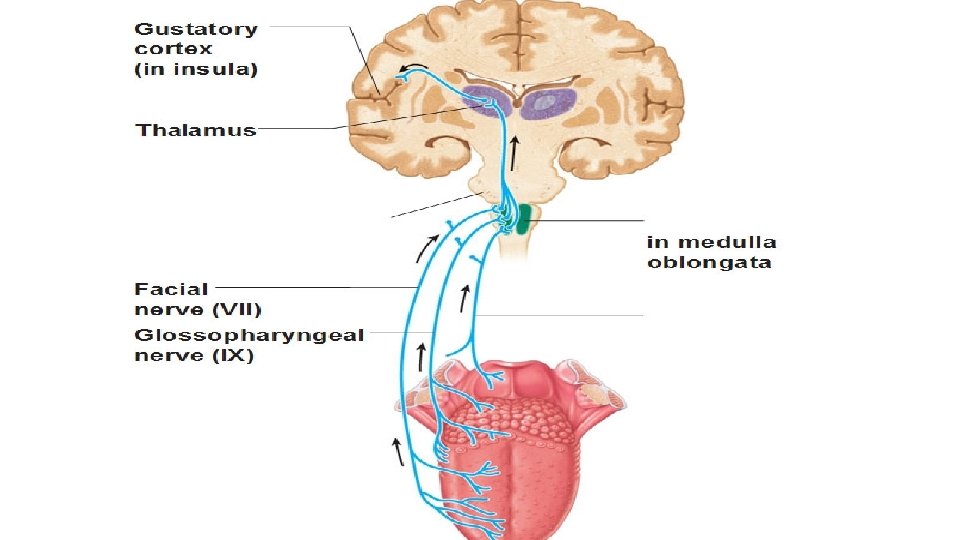
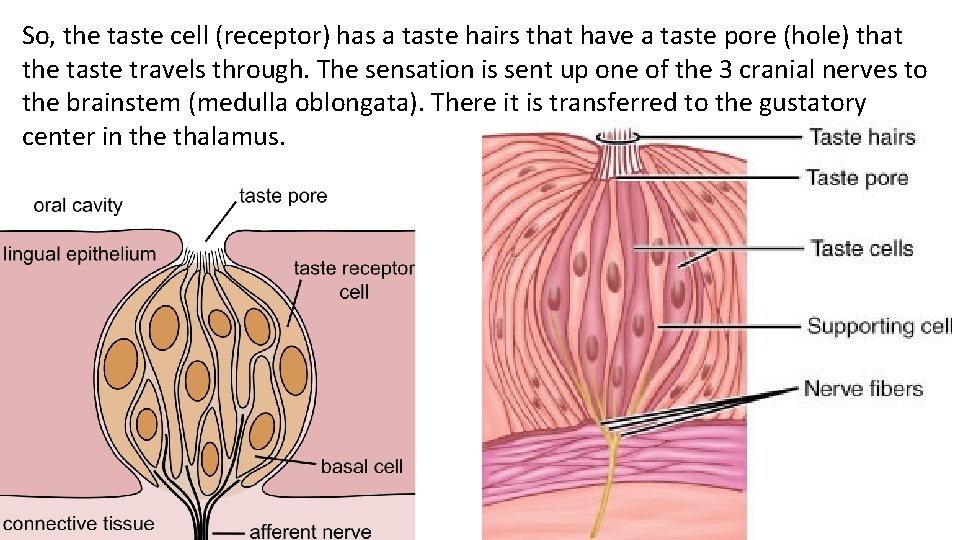
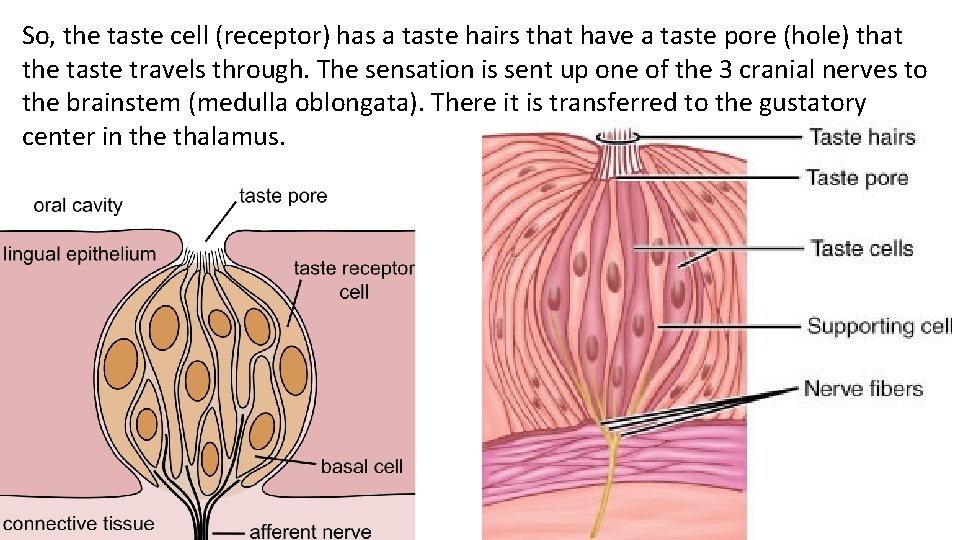
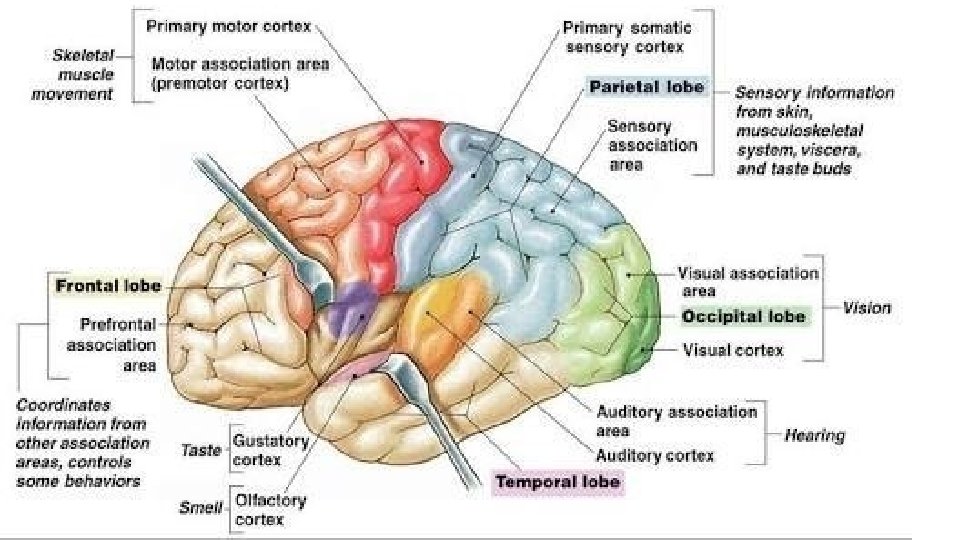
So, the taste cell (receptor) has a taste hairs that have a taste pore (hole) that the taste travels through. The sensation is sent up one of the 3 cranial nerves to the brainstem (medulla oblongata). There it is transferred to the gustatory center in the thalamus.
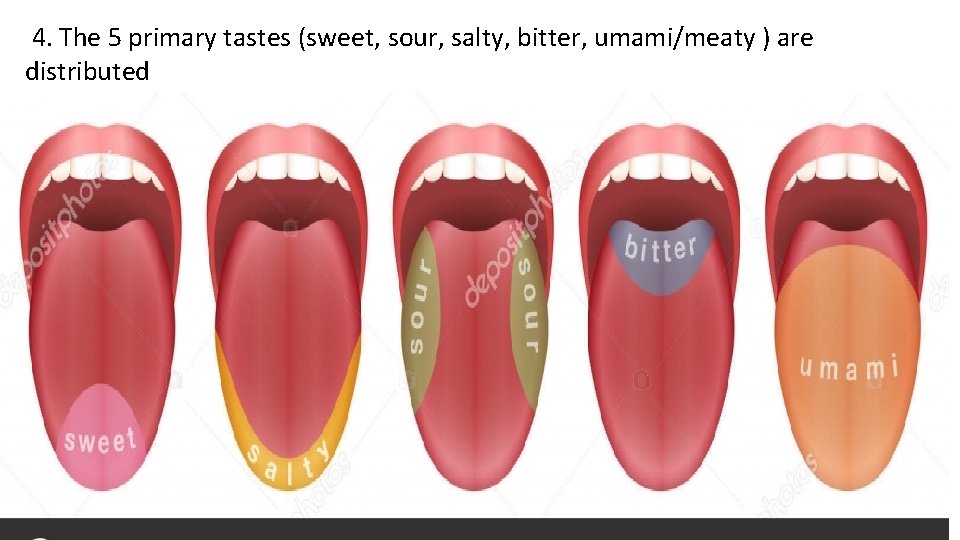
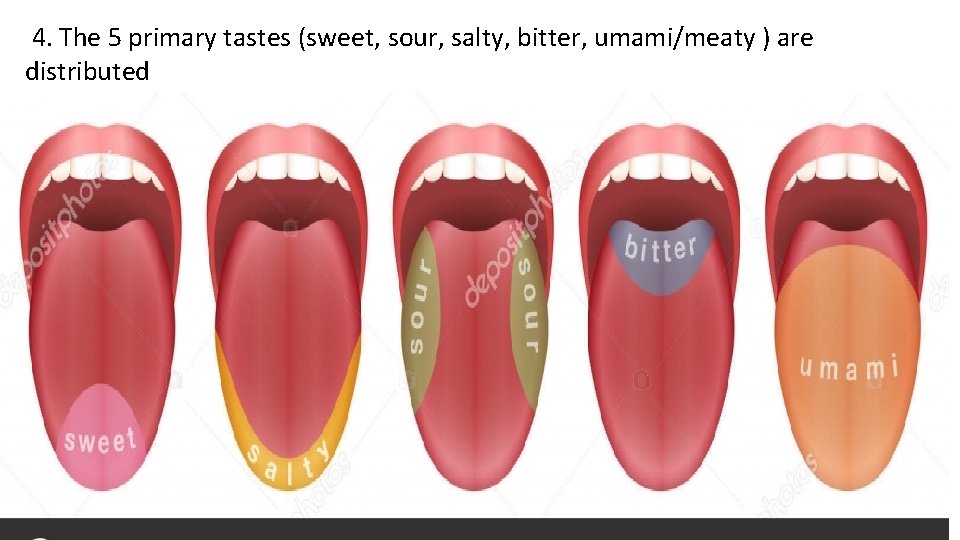
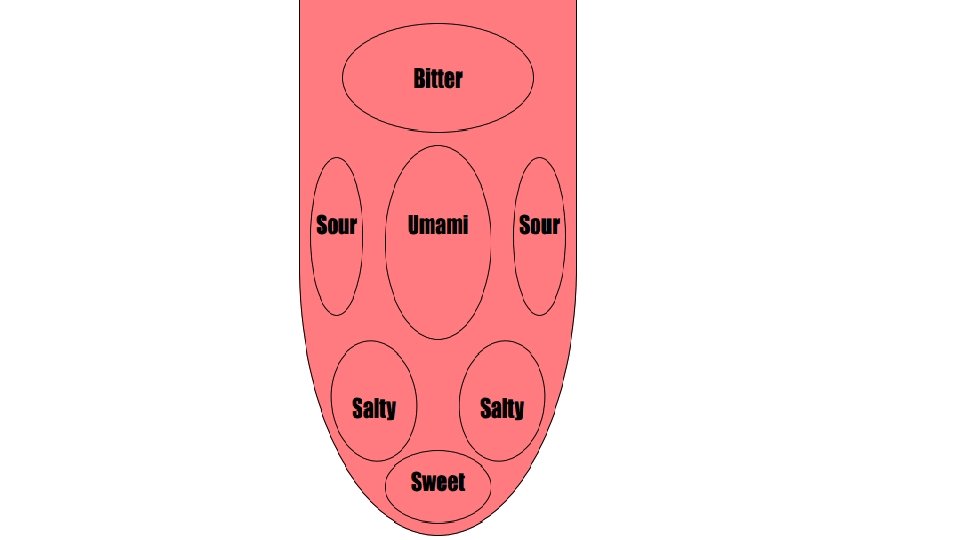
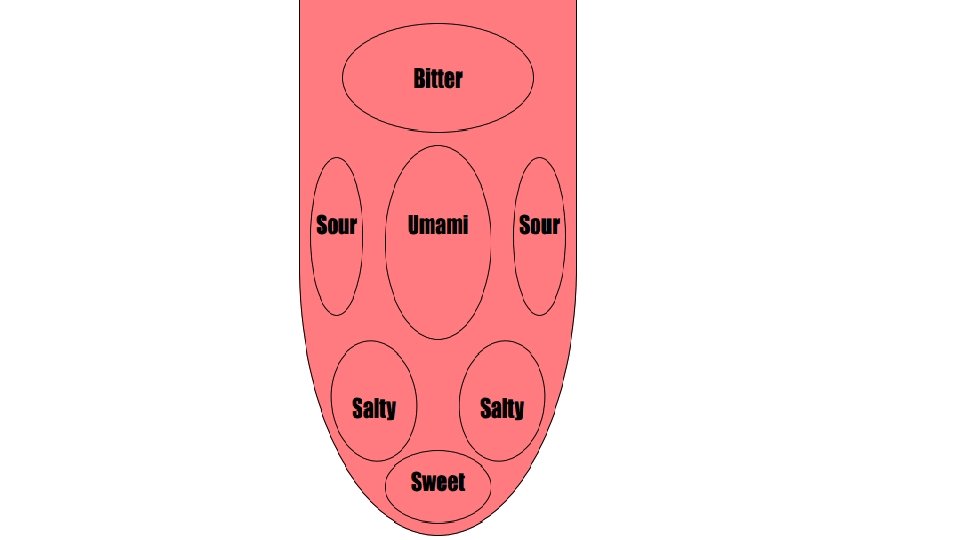
4. The 5 primary tastes (sweet, sour, salty, bitter, umami/meaty ) are distributed unevenly along the tongue’s surface.
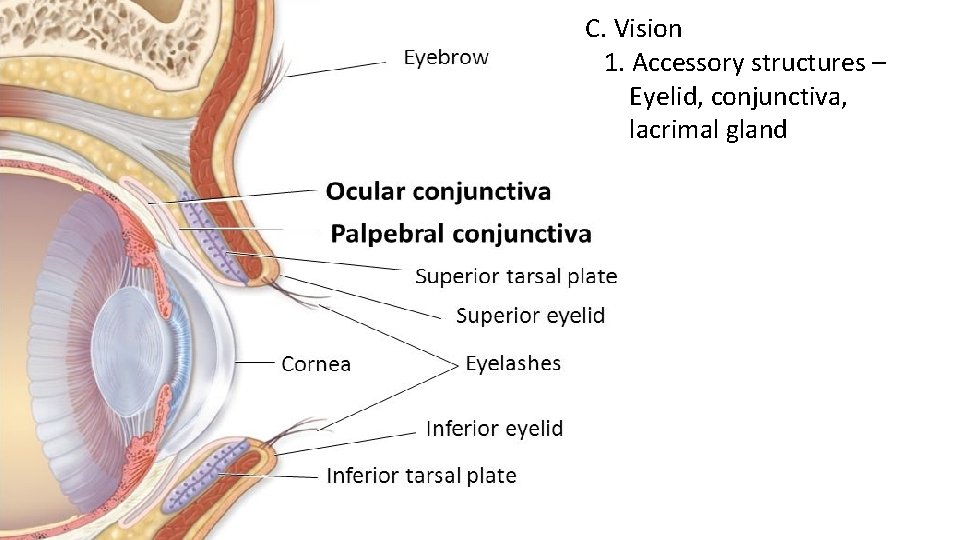
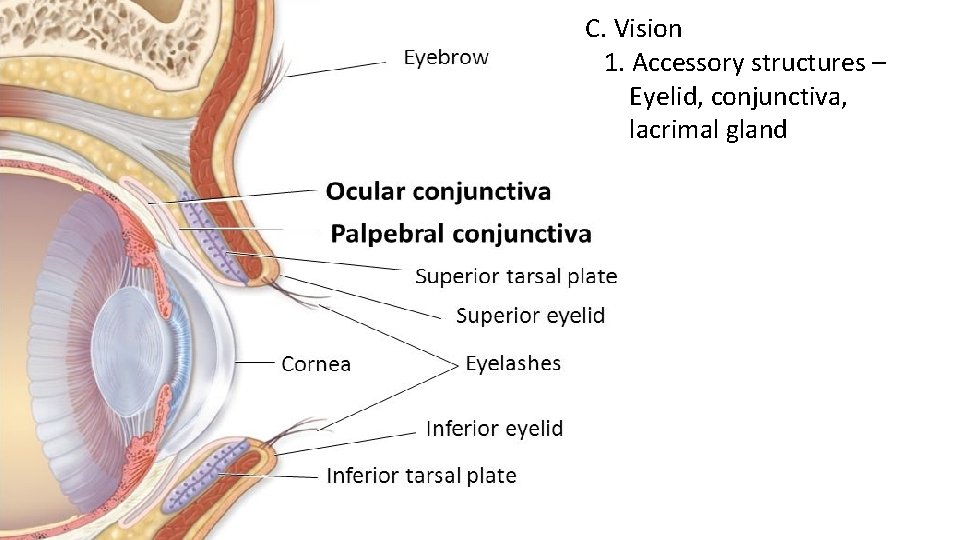
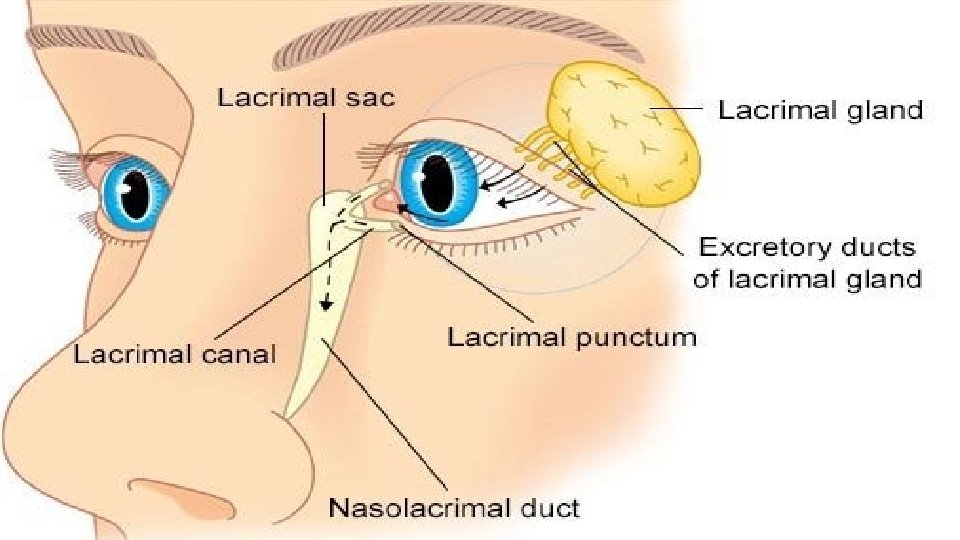
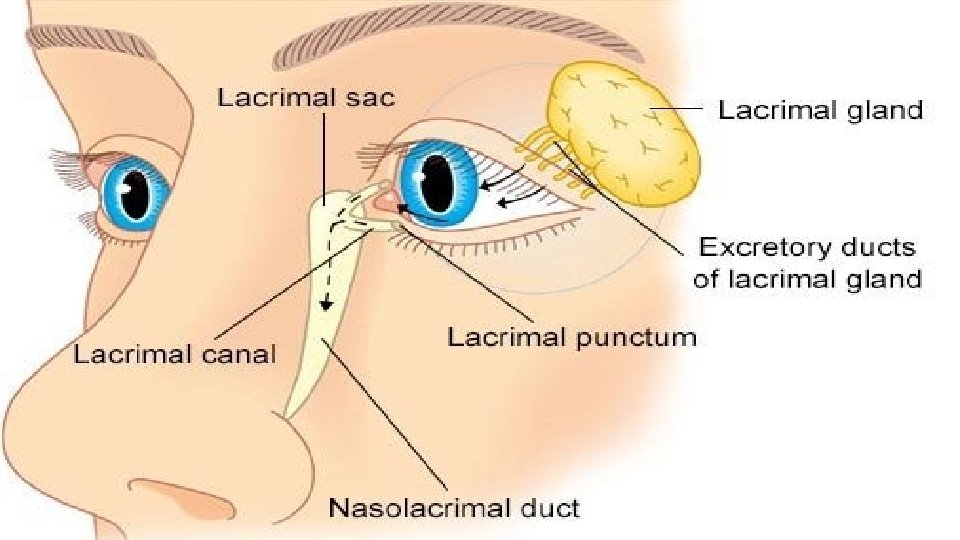
C. Vision 1. Accessory structures – Eyelid, conjunctiva, lacrimal gland
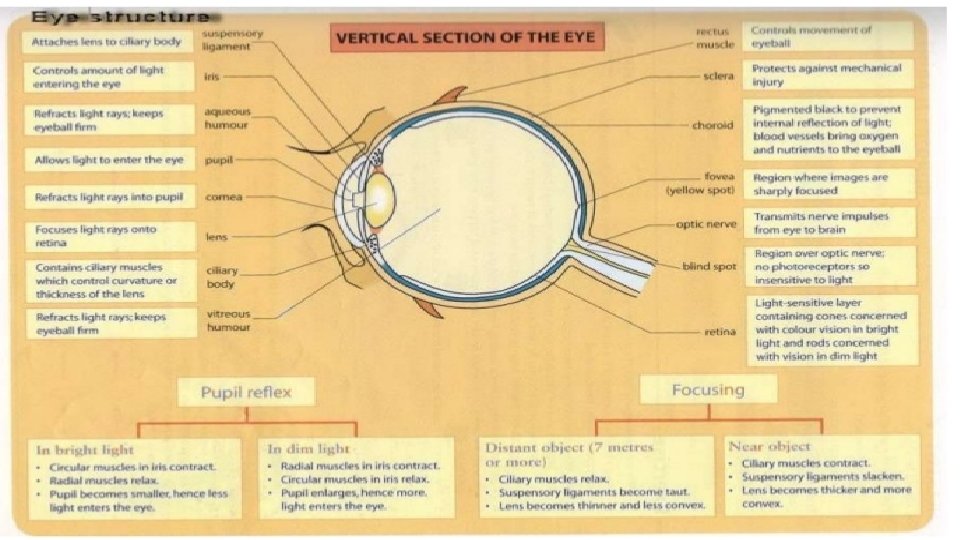
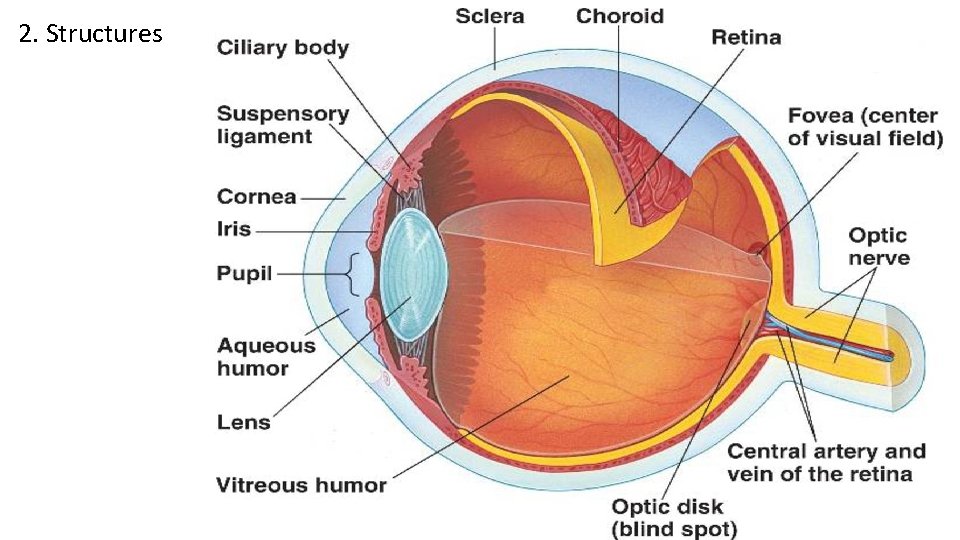
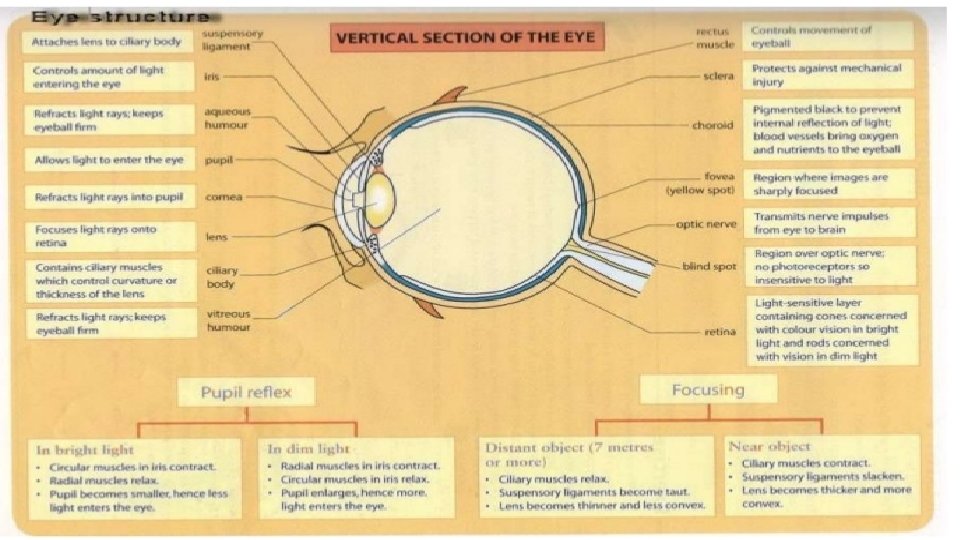
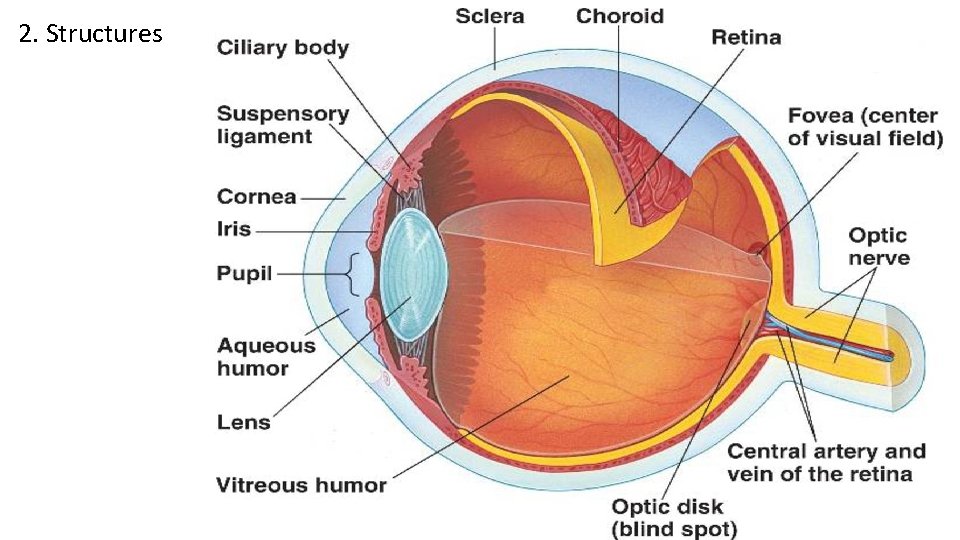
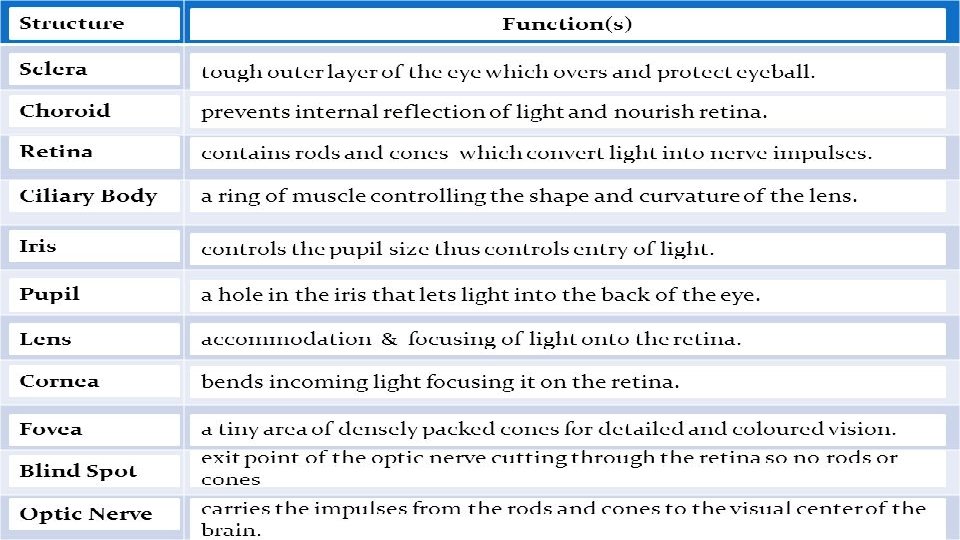
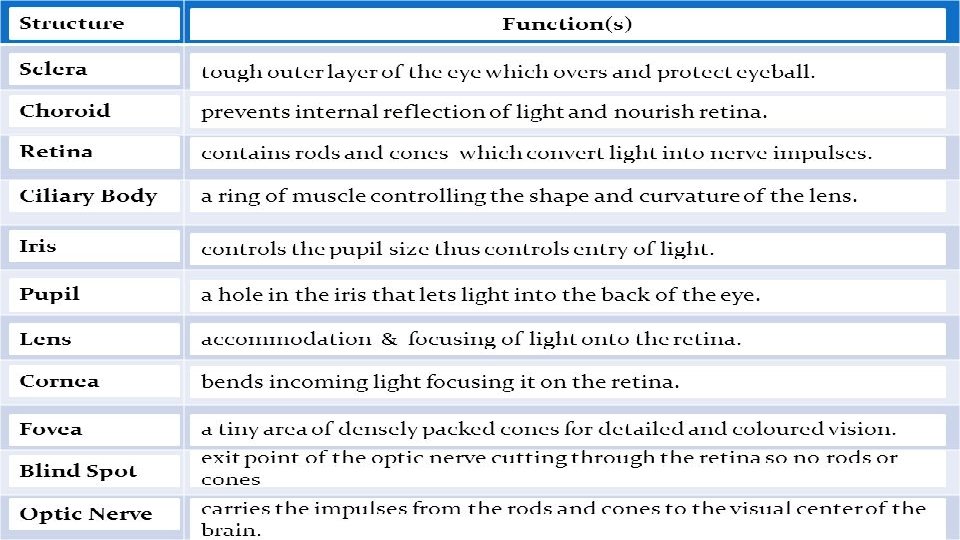
2. Structures
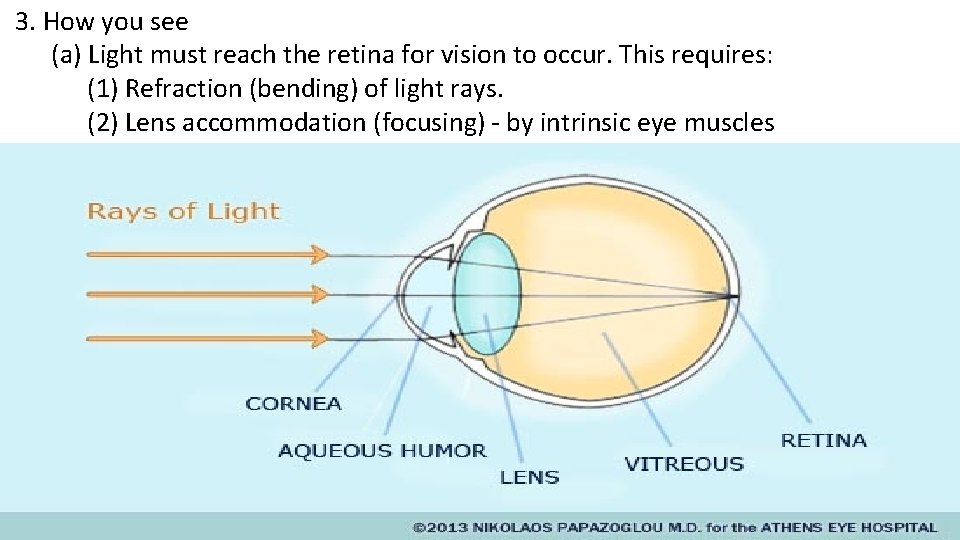
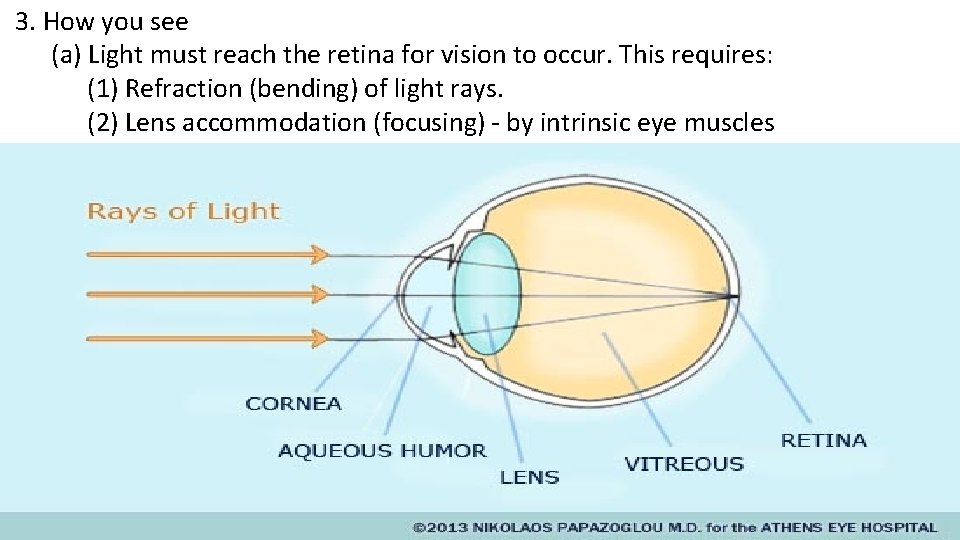
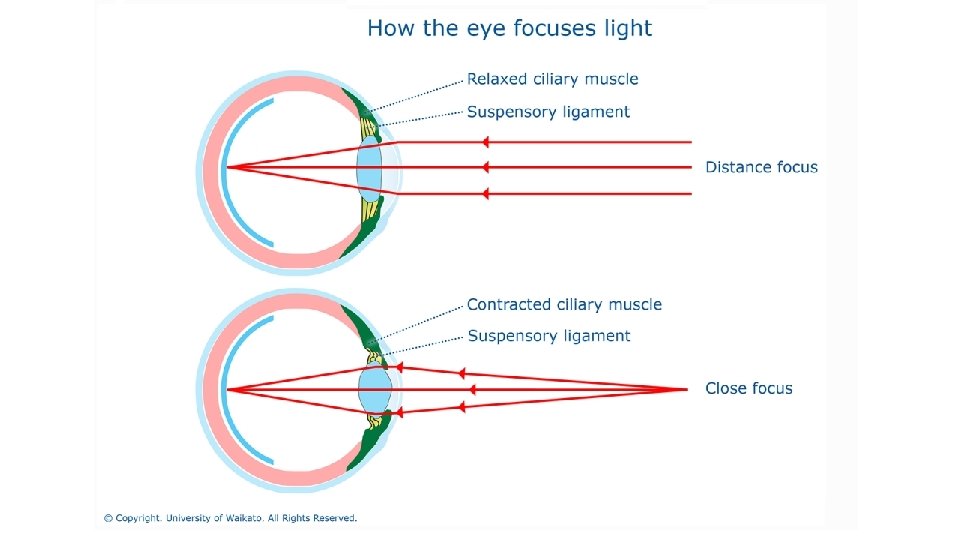
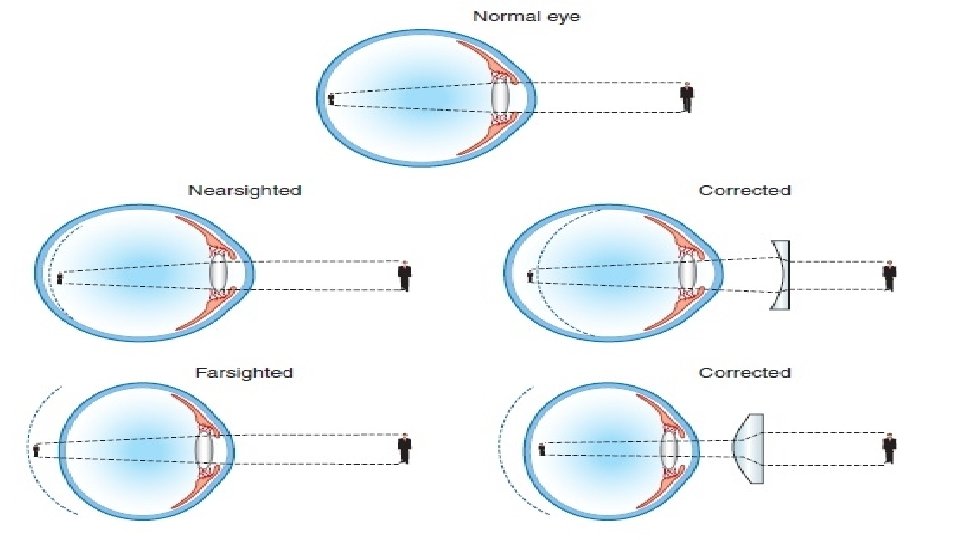
3. How you see (a) Light must reach the retina for vision to occur. This requires: (1) Refraction (bending) of light rays. (2) Lens accommodation (focusing) - by intrinsic eye muscles
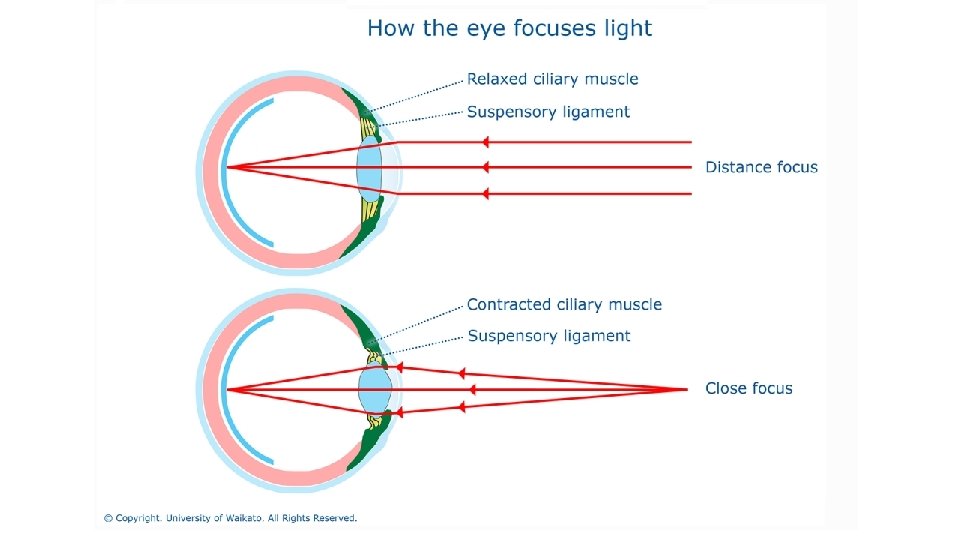
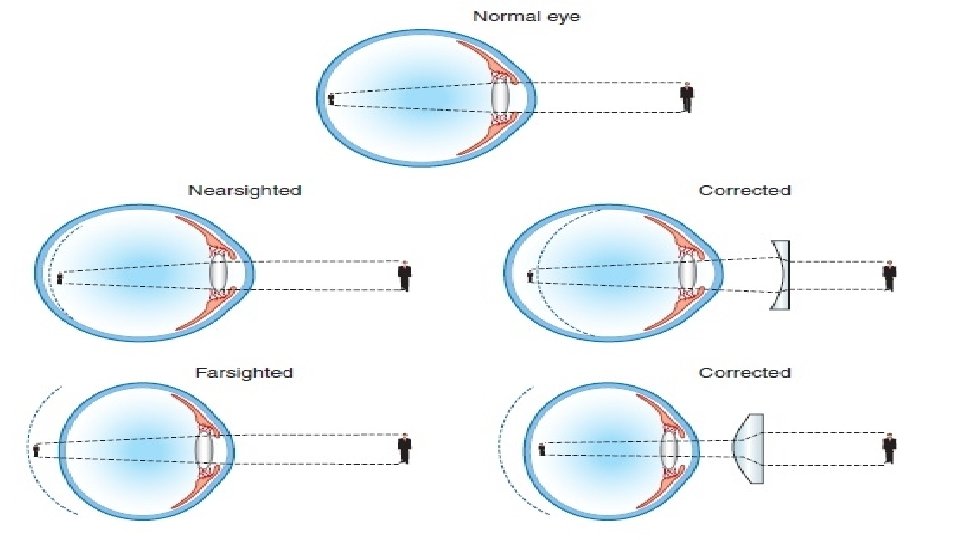
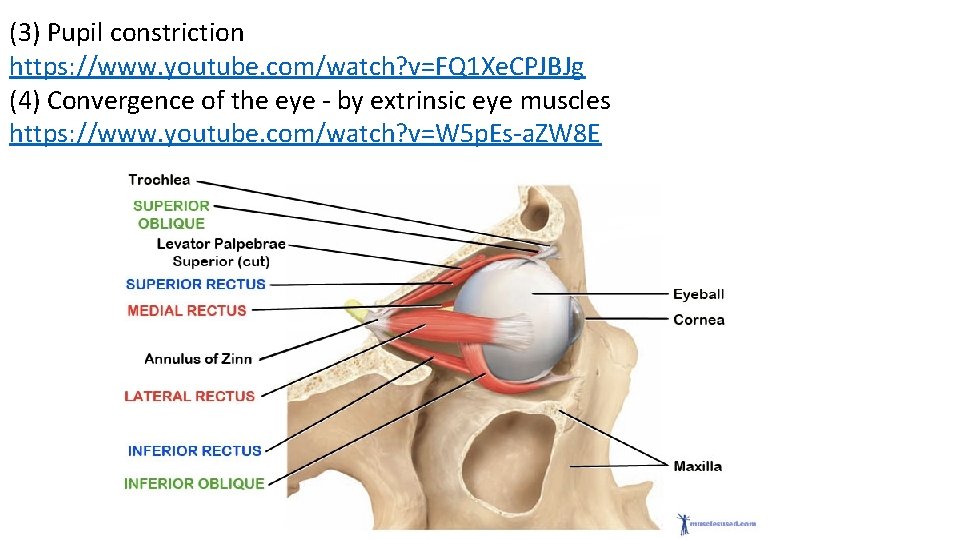
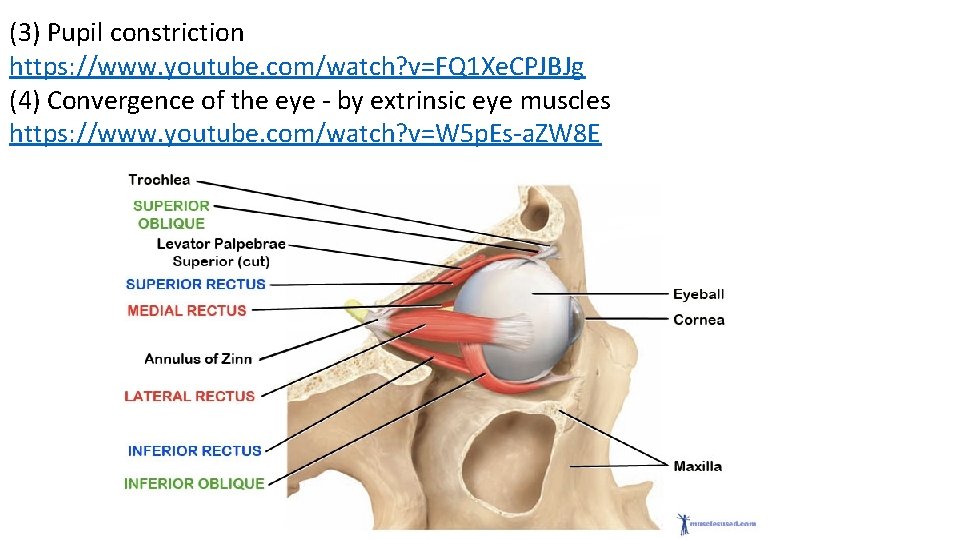
(3) Pupil constriction https: //www. youtube. com/watch? v=FQ 1 Xe. CPJBJg (4) Convergence of the eye - by extrinsic eye muscles https: //www. youtube. com/watch? v=W 5 p. Es-a. ZW 8 E
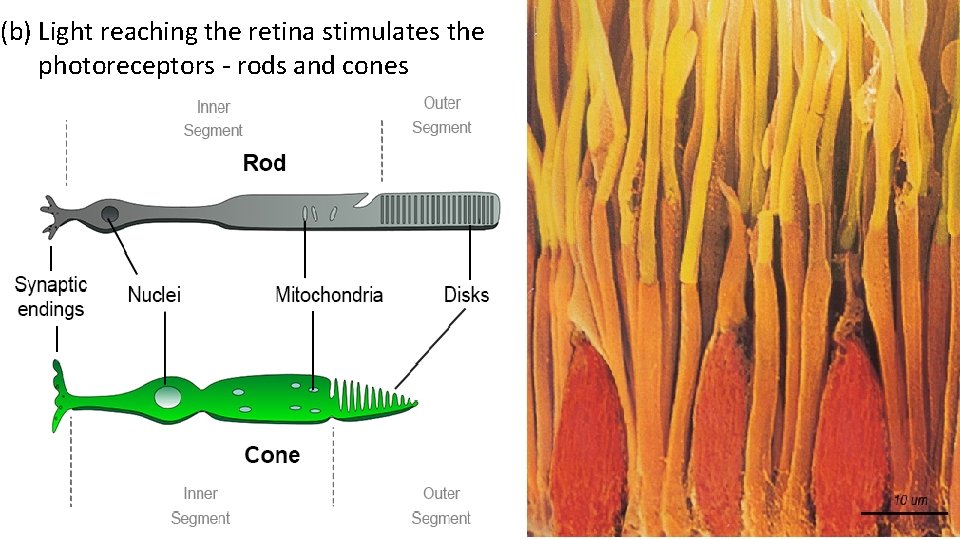
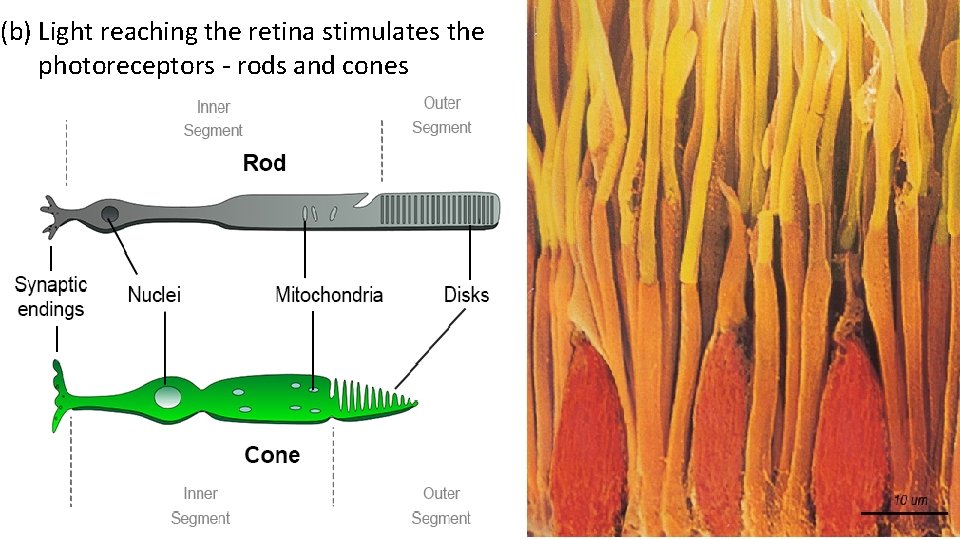
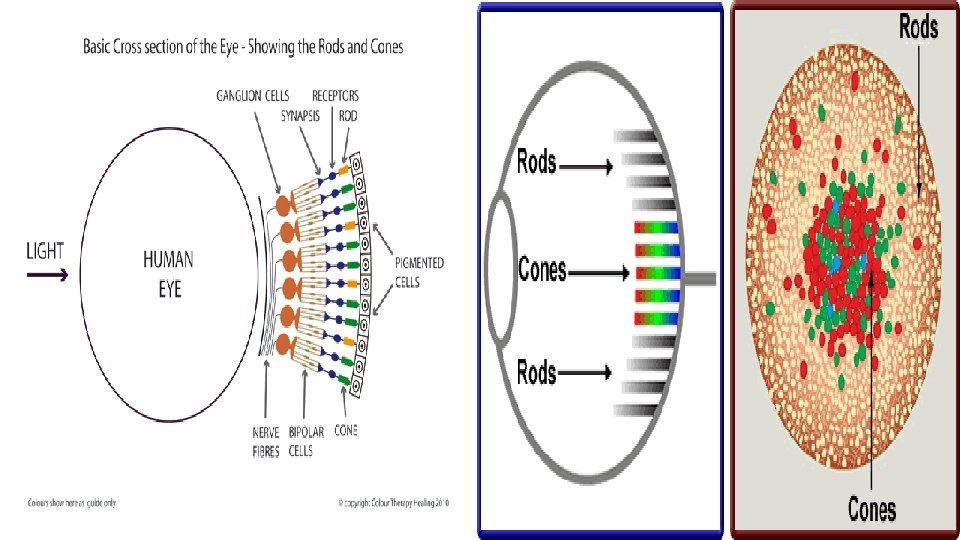
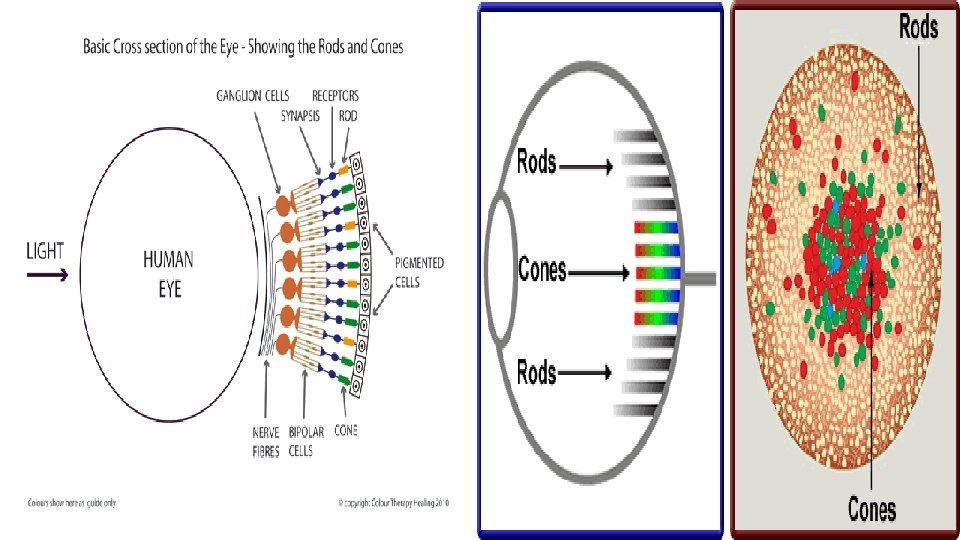
(b) Light reaching the retina stimulates the photoreceptors - rods and cones
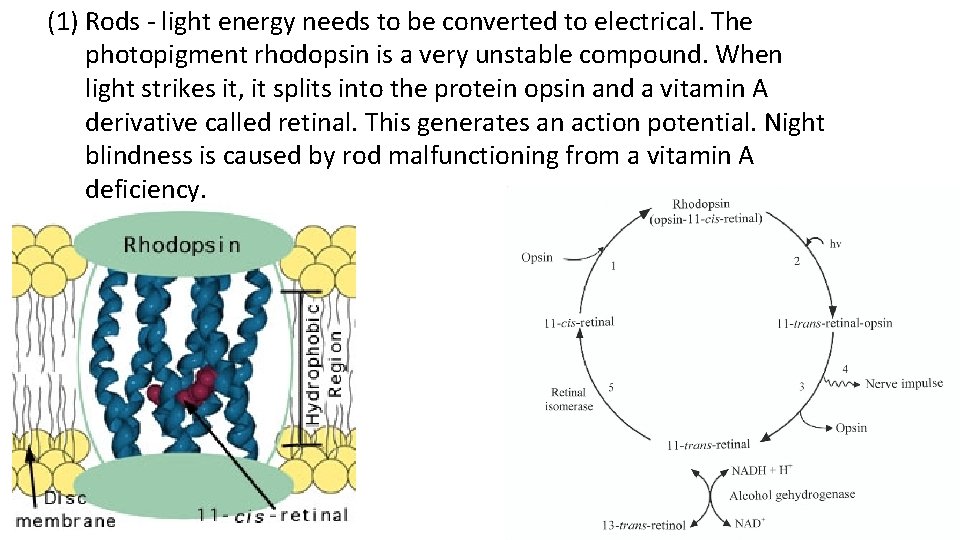
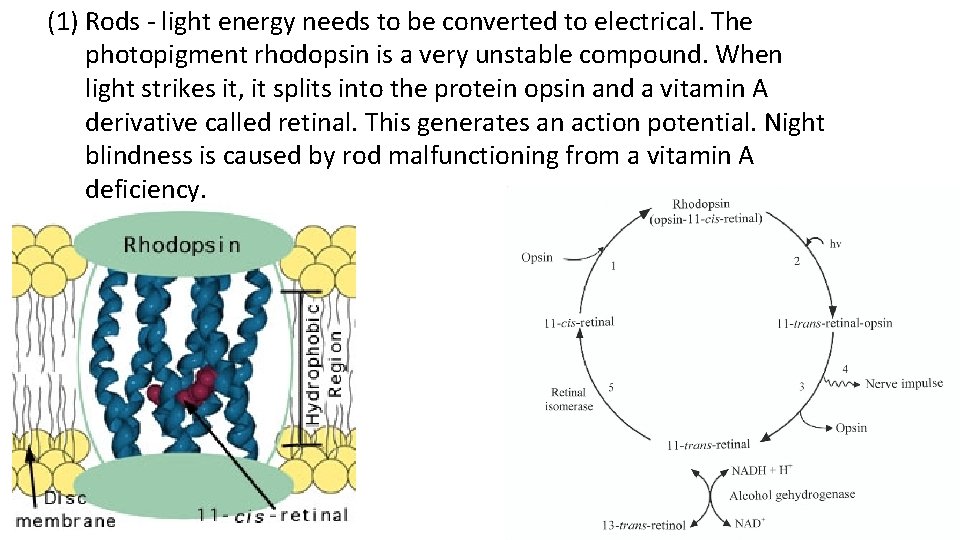
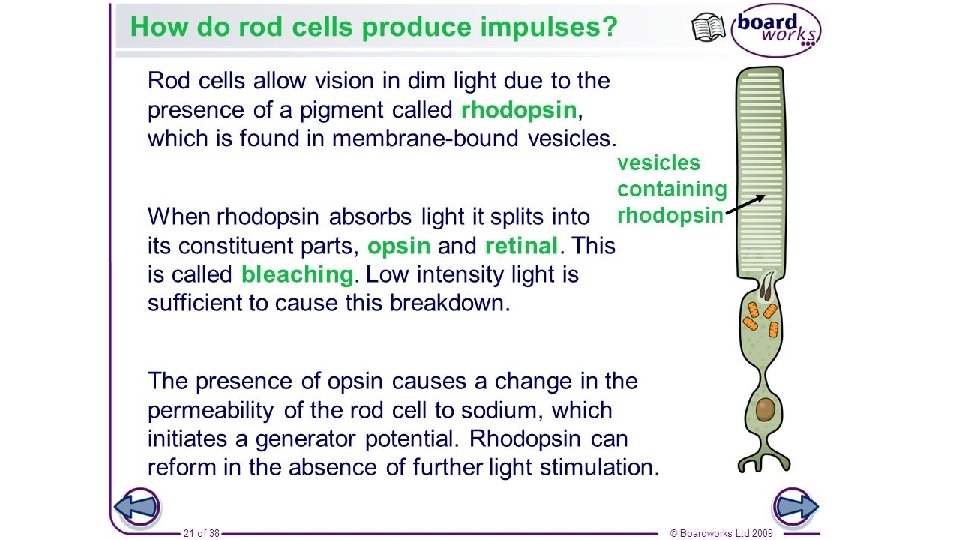
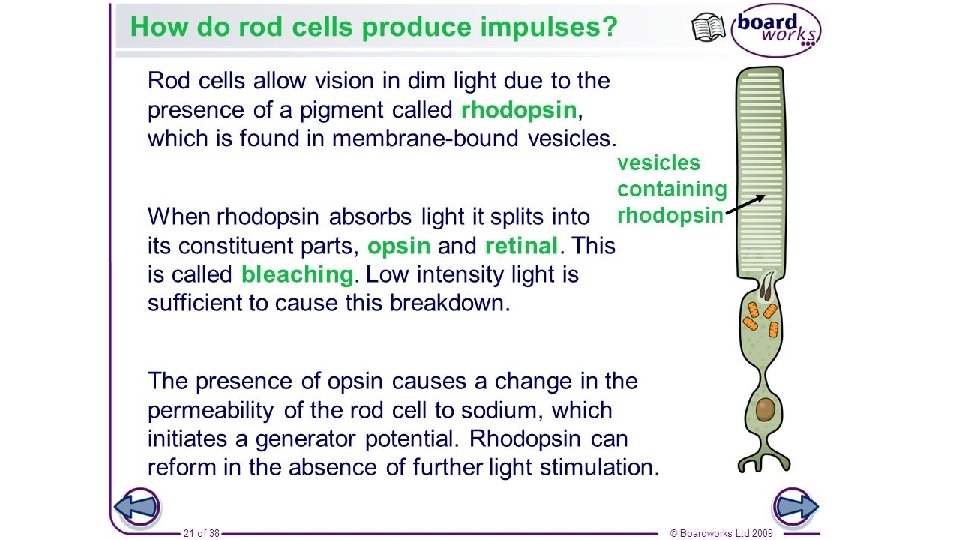
(1) Rods - light energy needs to be converted to electrical. The photopigment rhodopsin is a very unstable compound. When light strikes it, it splits into the protein opsin and a vitamin A derivative called retinal. This generates an action potential. Night blindness is caused by rod malfunctioning from a vitamin A deficiency.
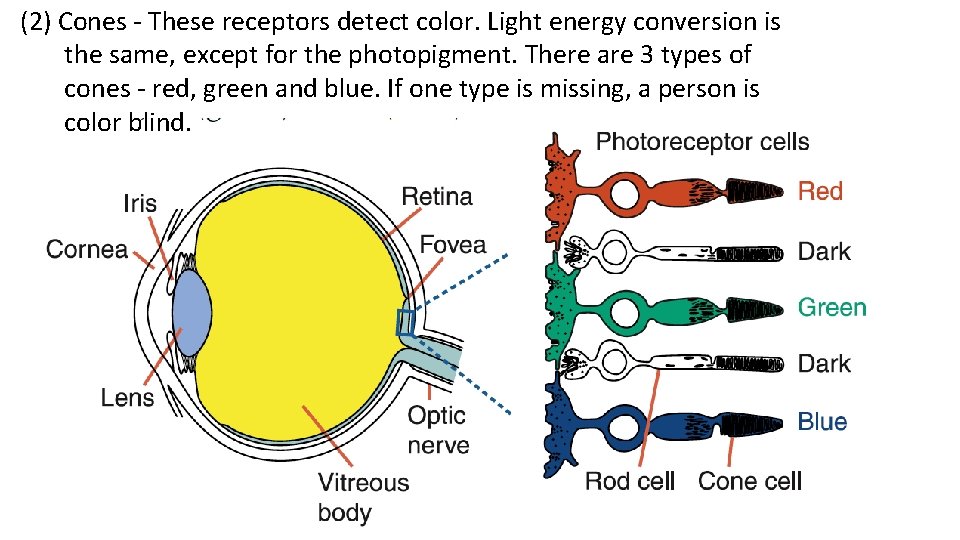
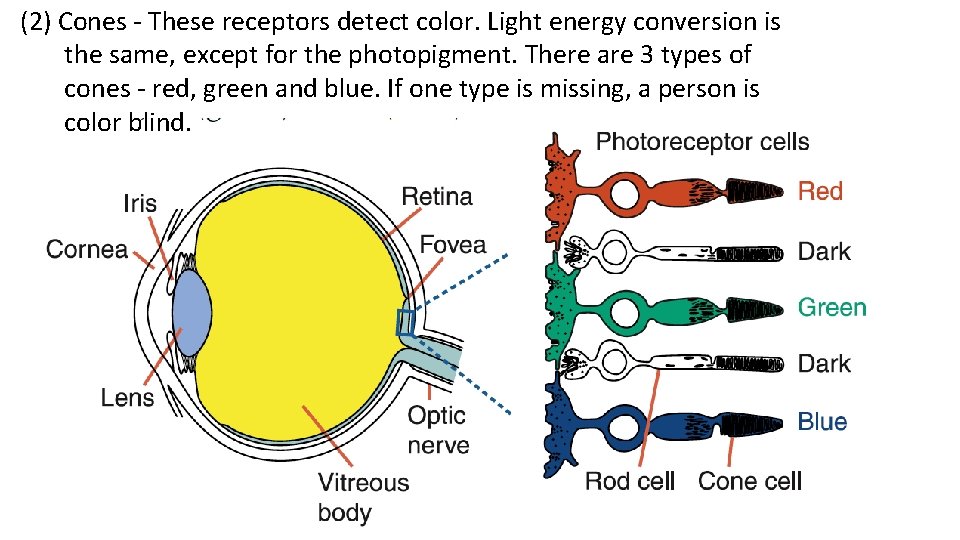
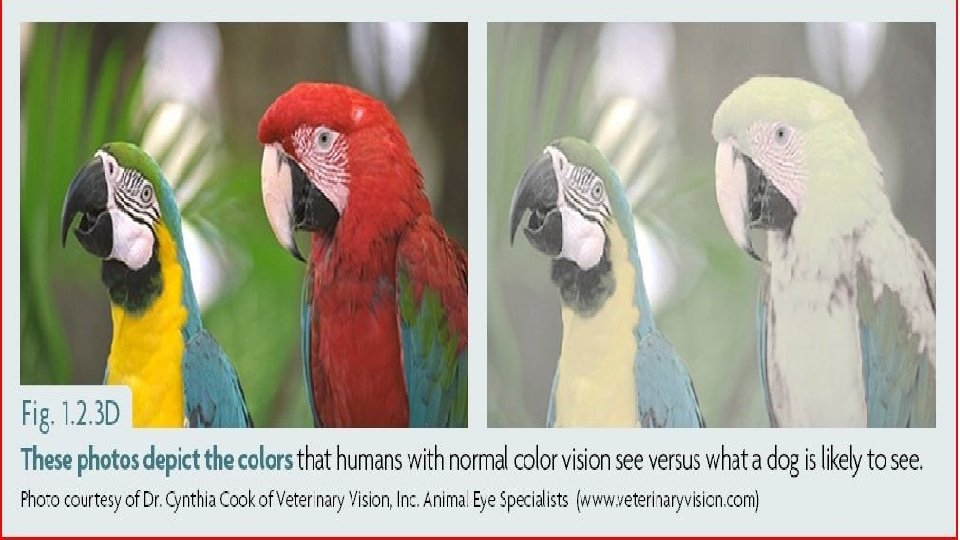
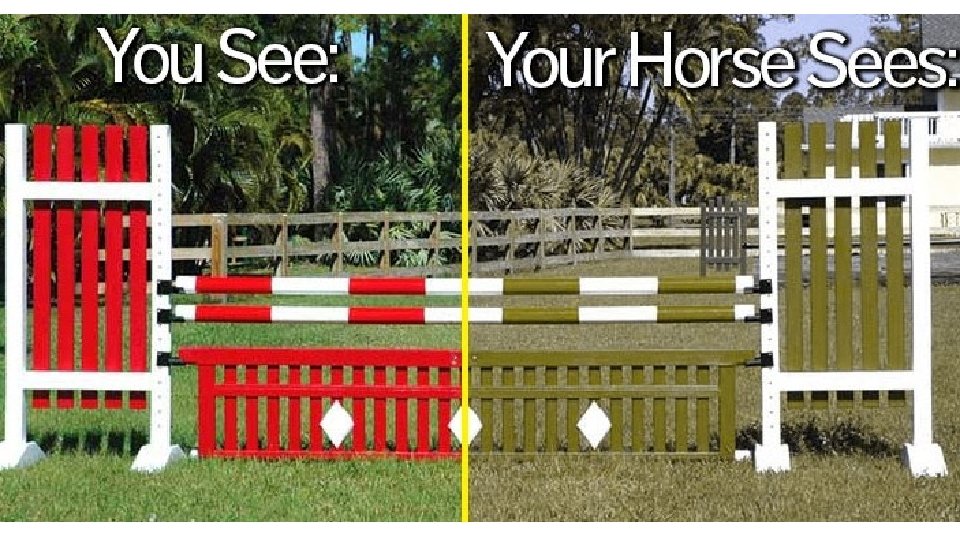
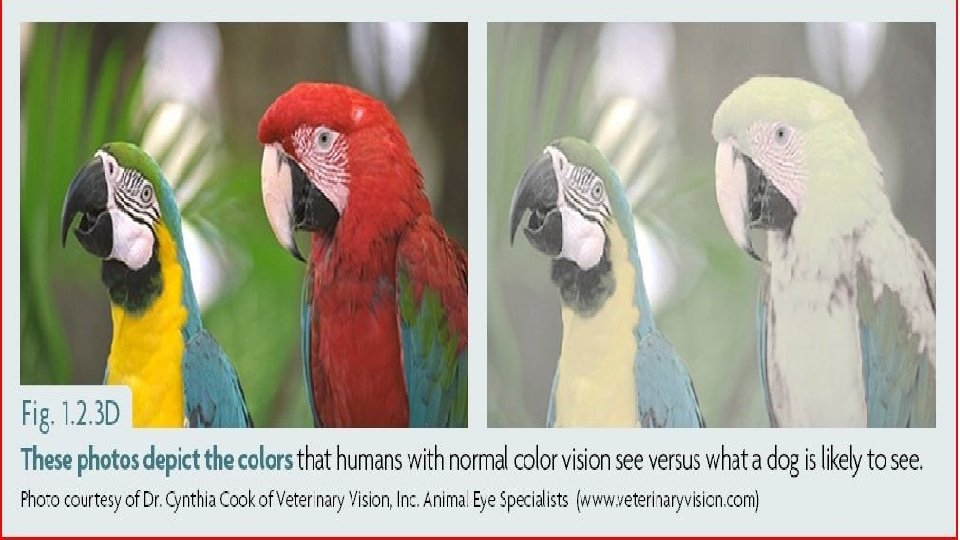
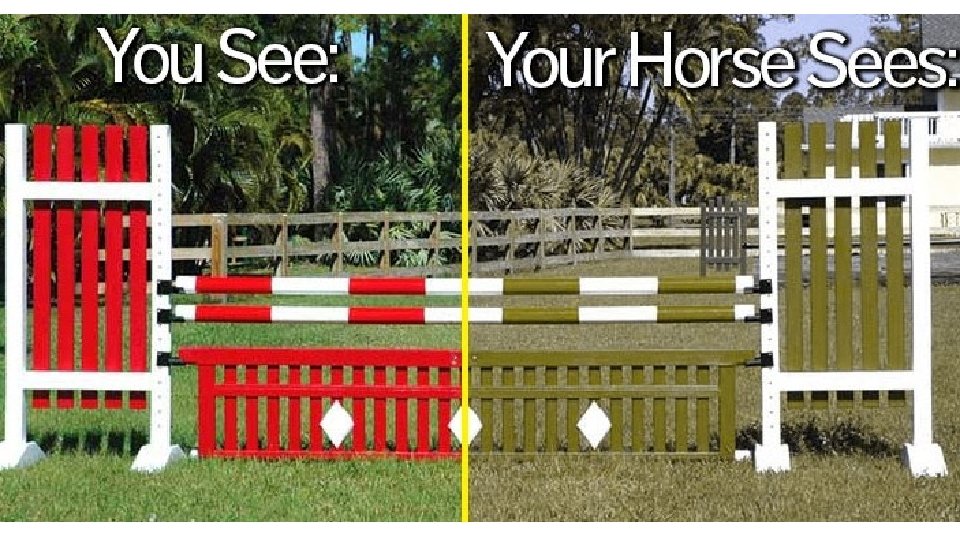
(2) Cones - These receptors detect color. Light energy conversion is the same, except for the photopigment. There are 3 types of cones - red, green and blue. If one type is missing, a person is color blind.

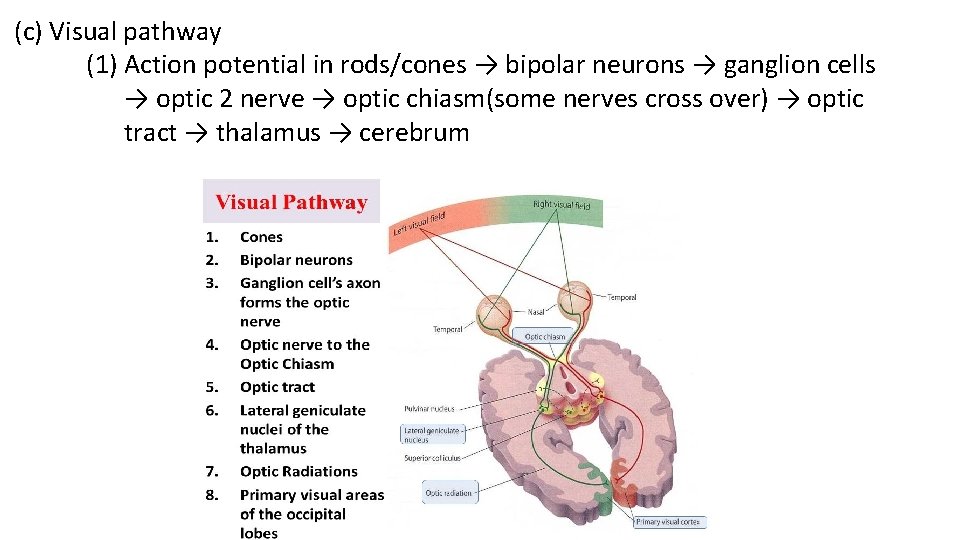
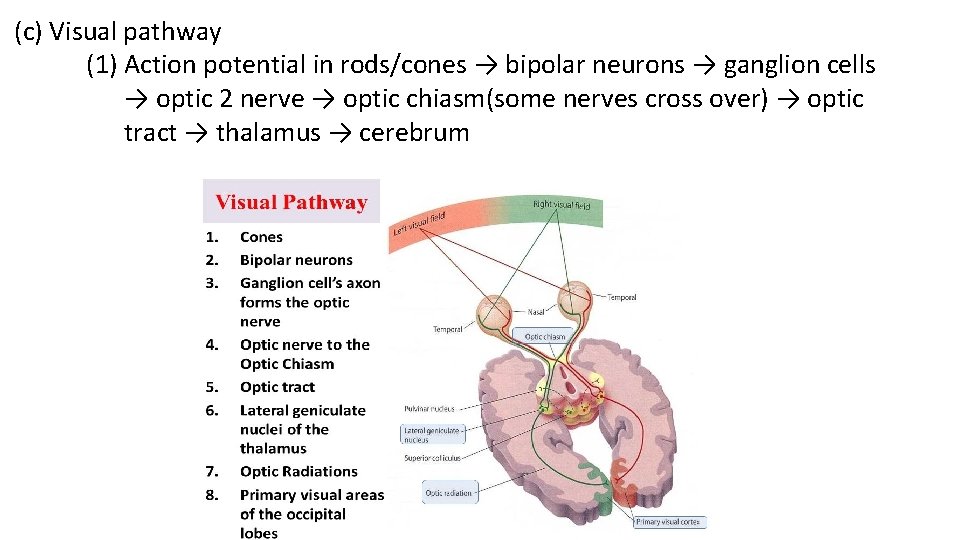
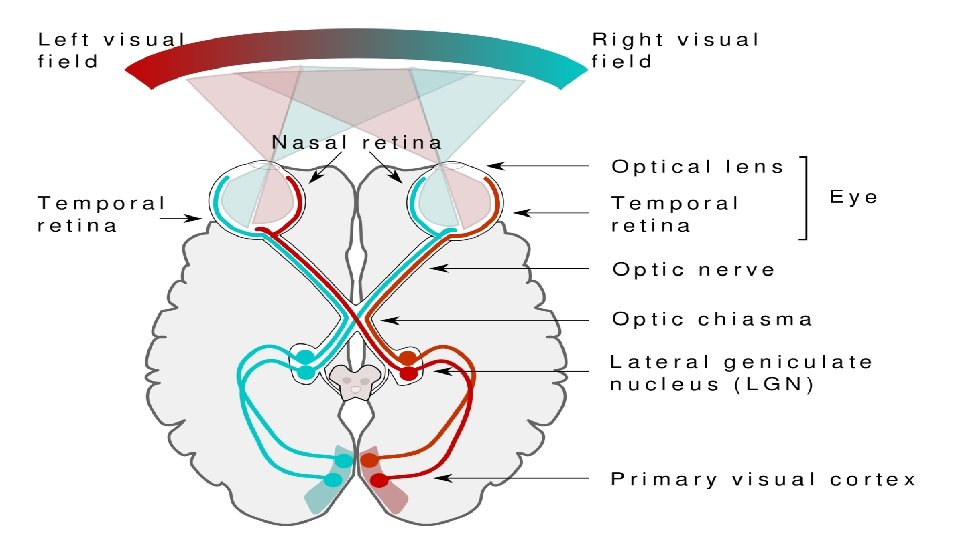
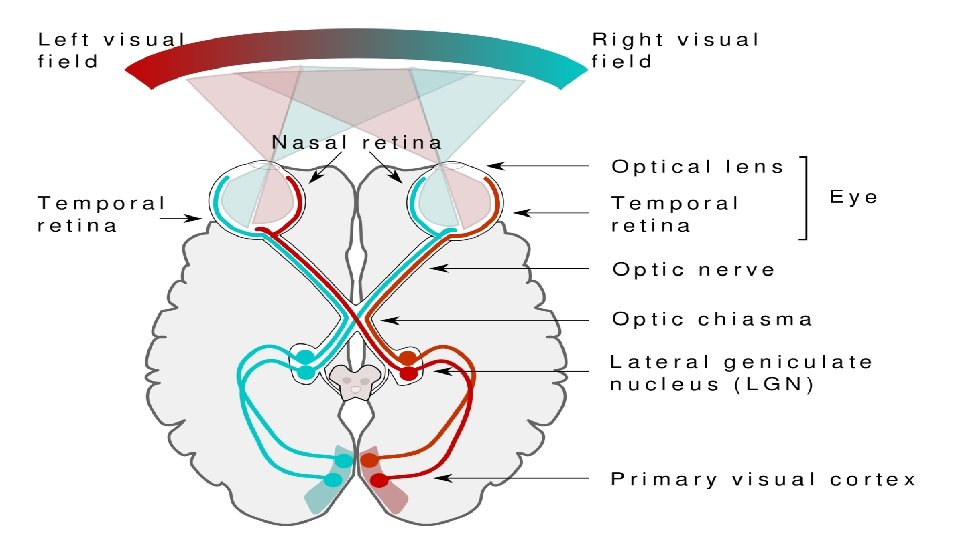
(c) Visual pathway (1) Action potential in rods/cones → bipolar neurons → ganglion cells → optic 2 nerve → optic chiasm(some nerves cross over) → optic tract → thalamus → cerebrum
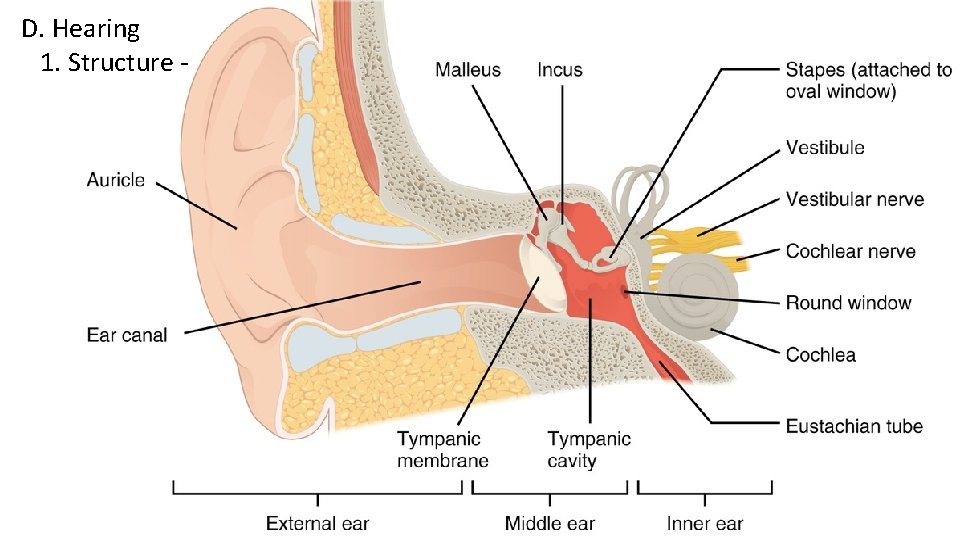
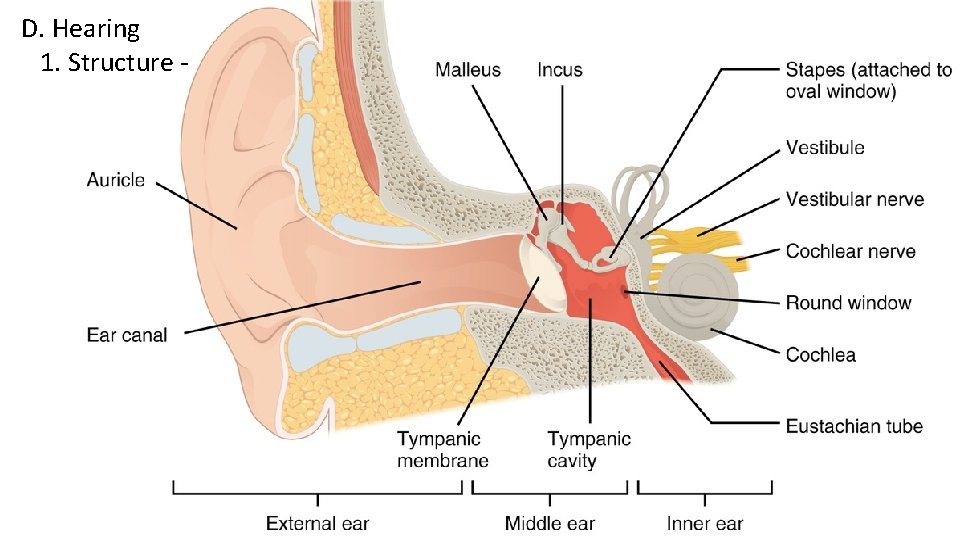
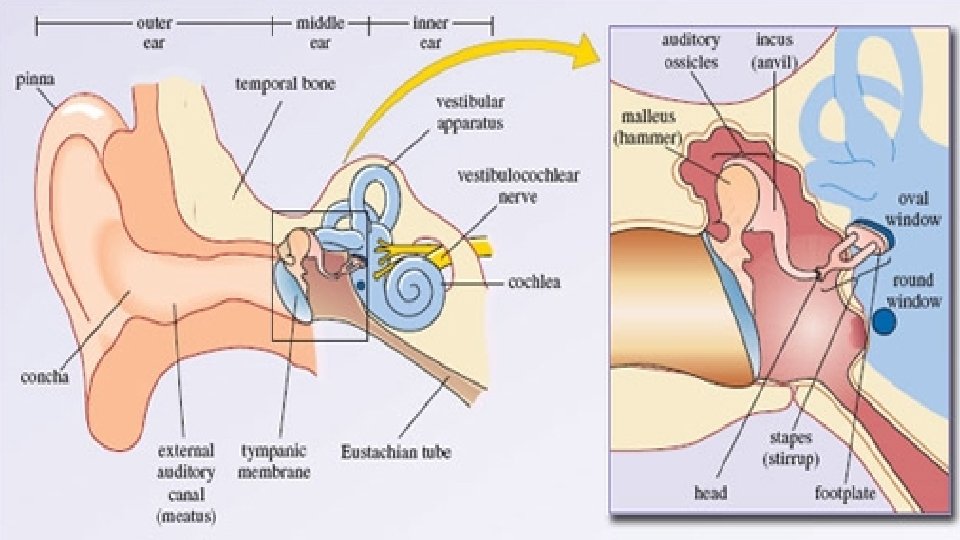
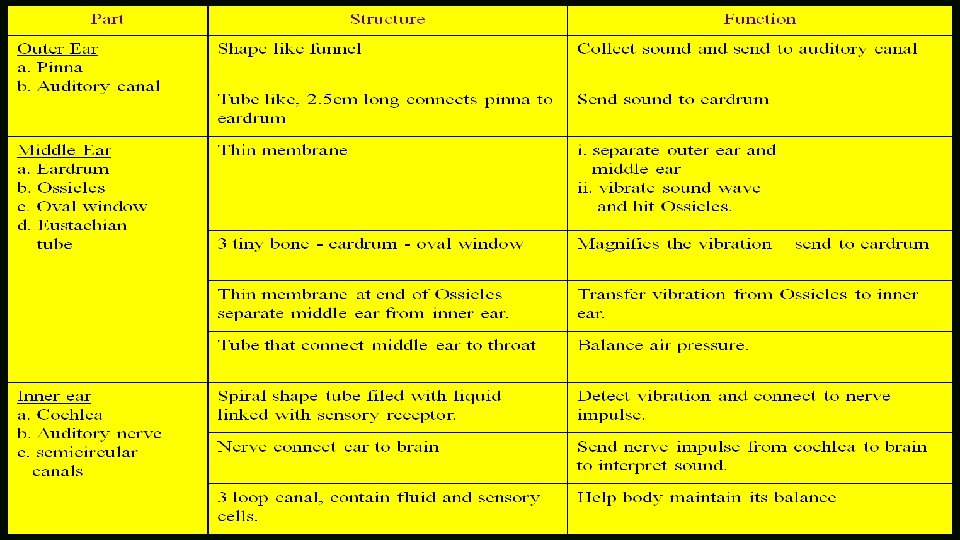
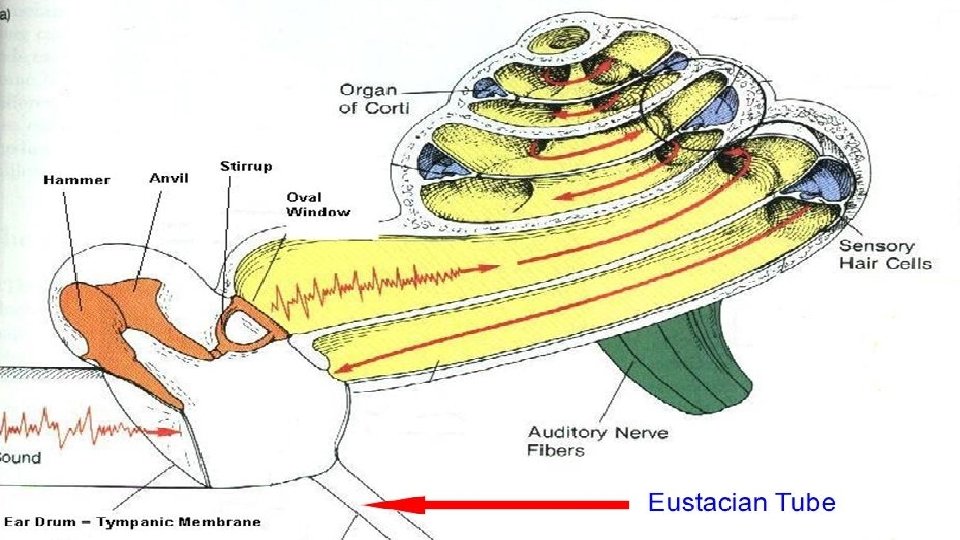
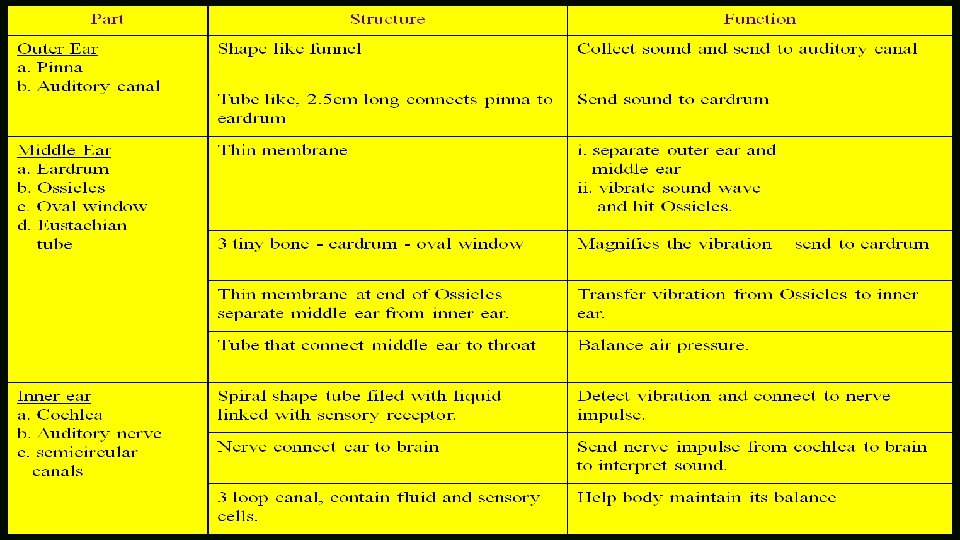
D. Hearing 1. Structure -
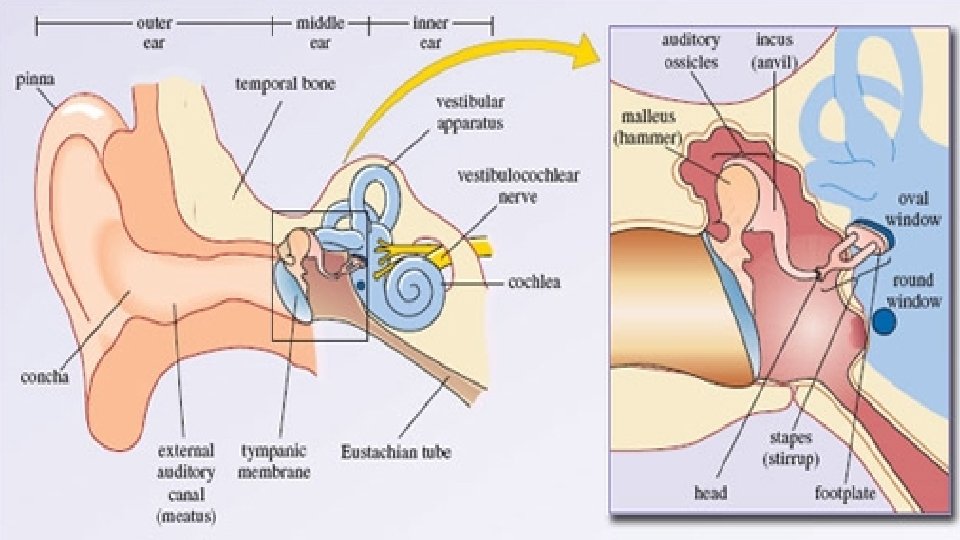
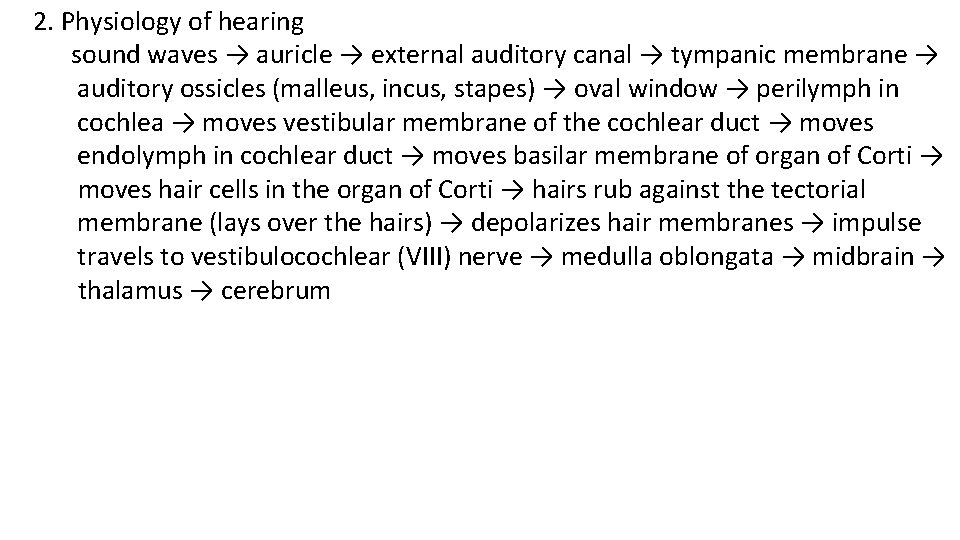
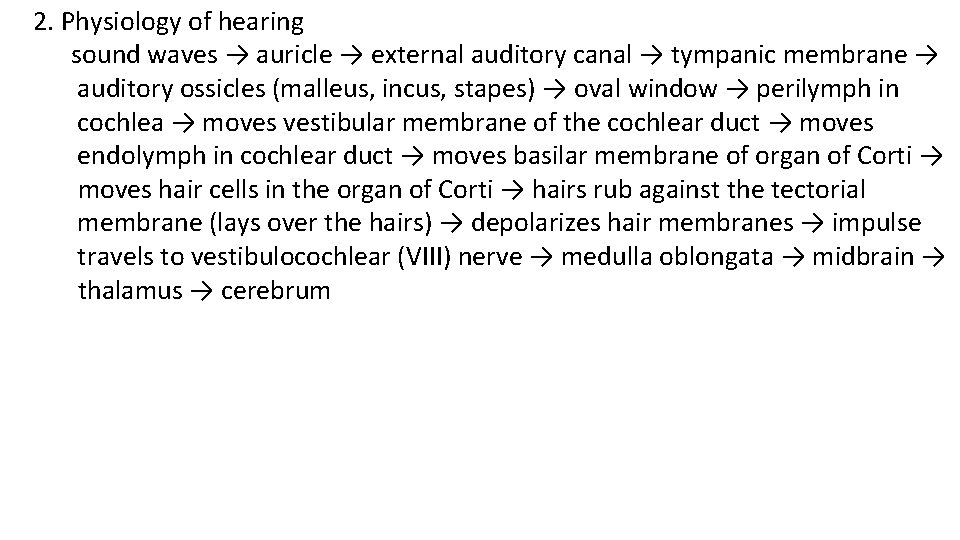
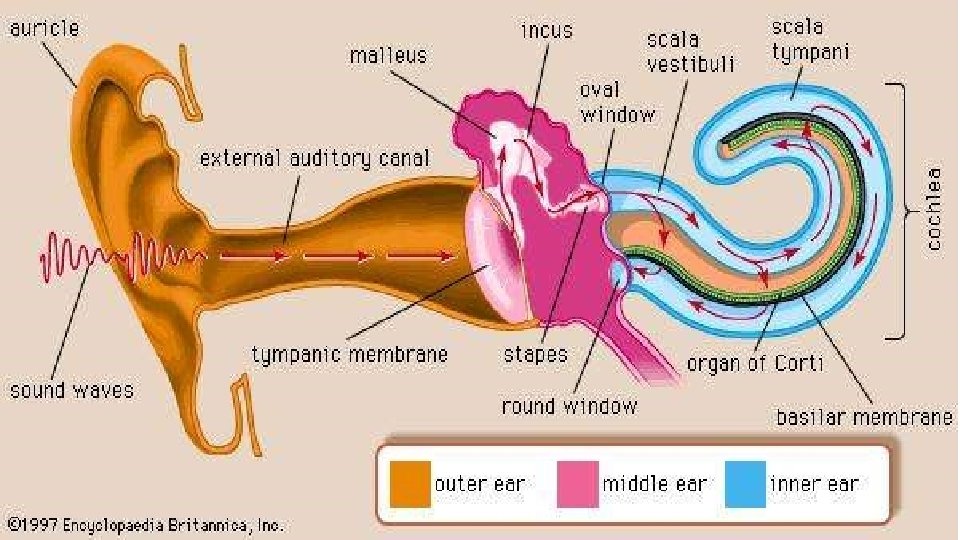
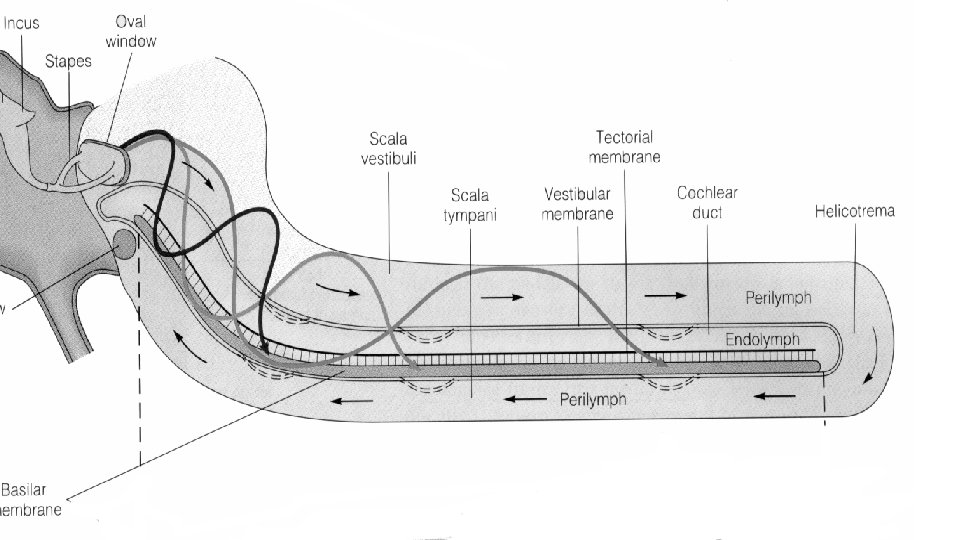
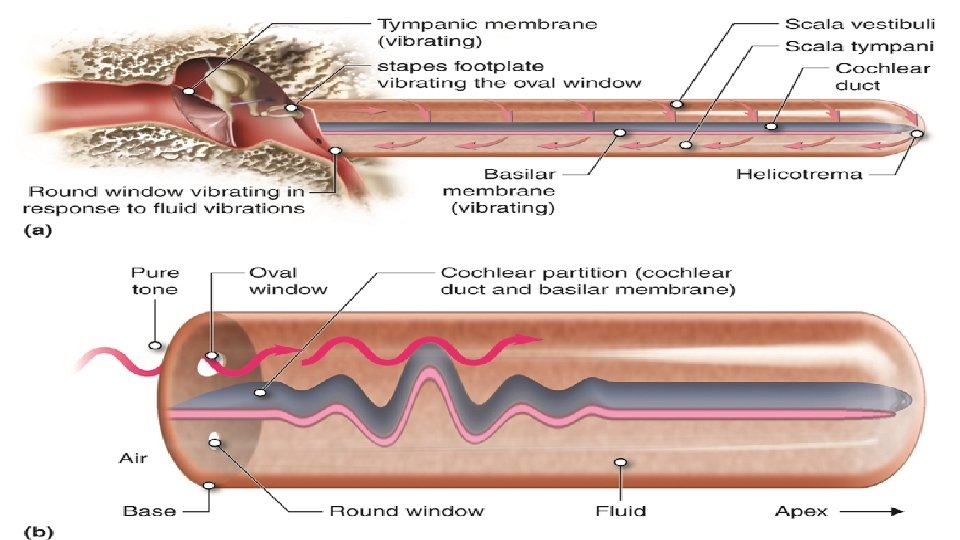
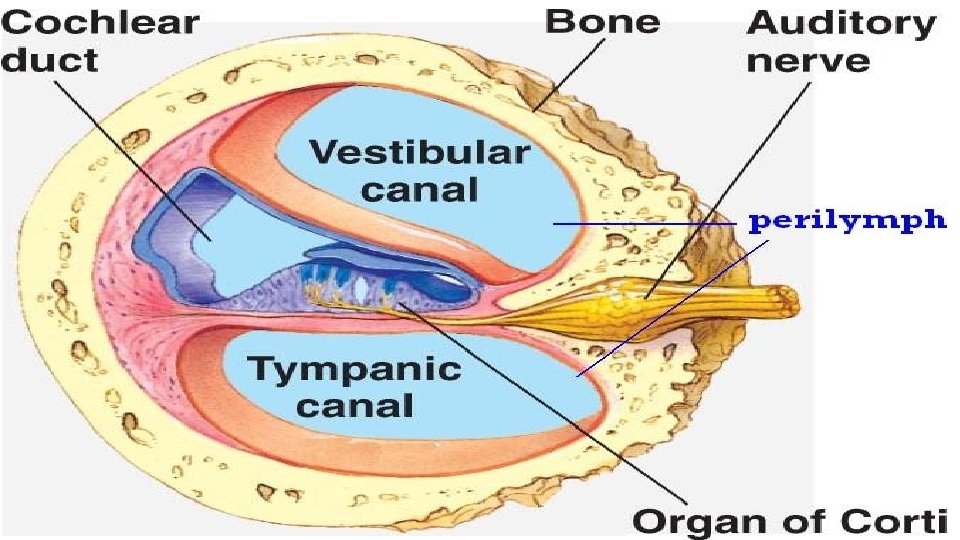
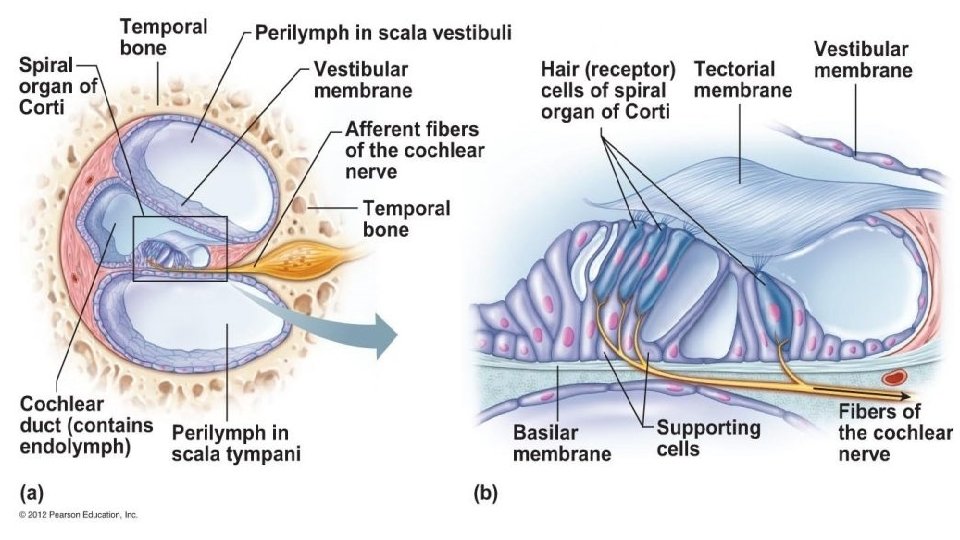
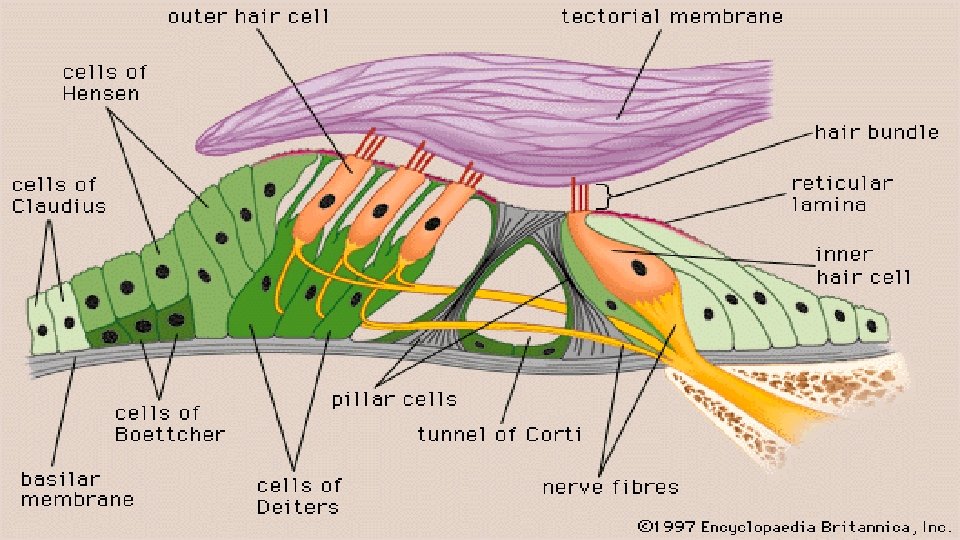
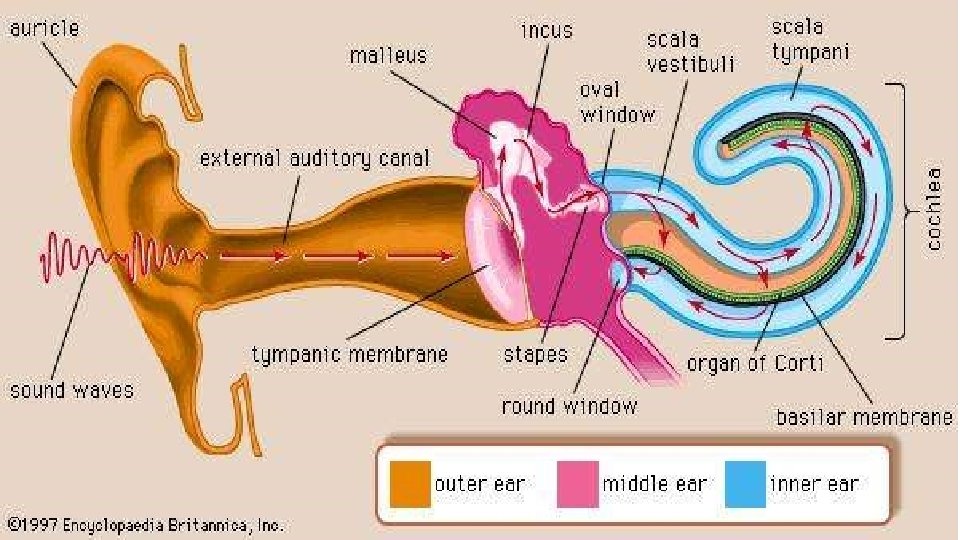
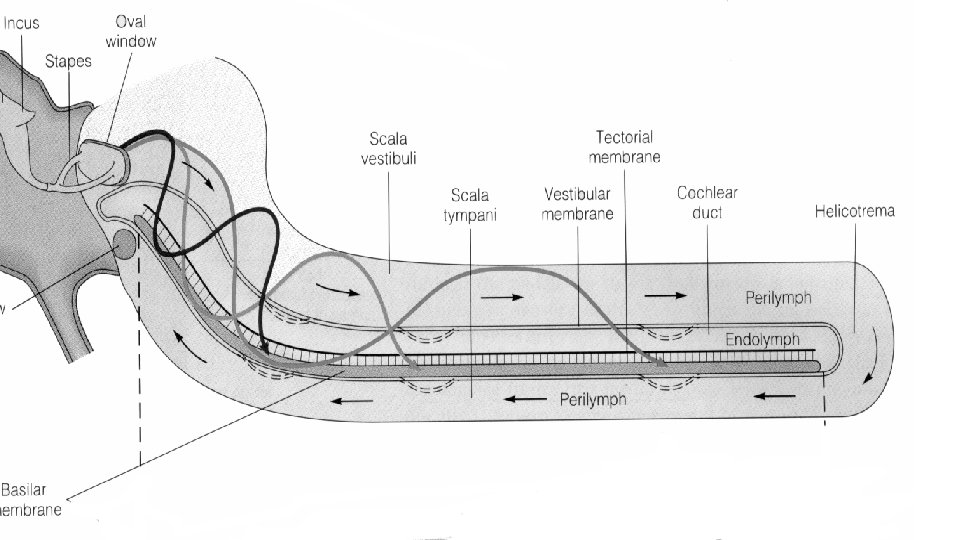
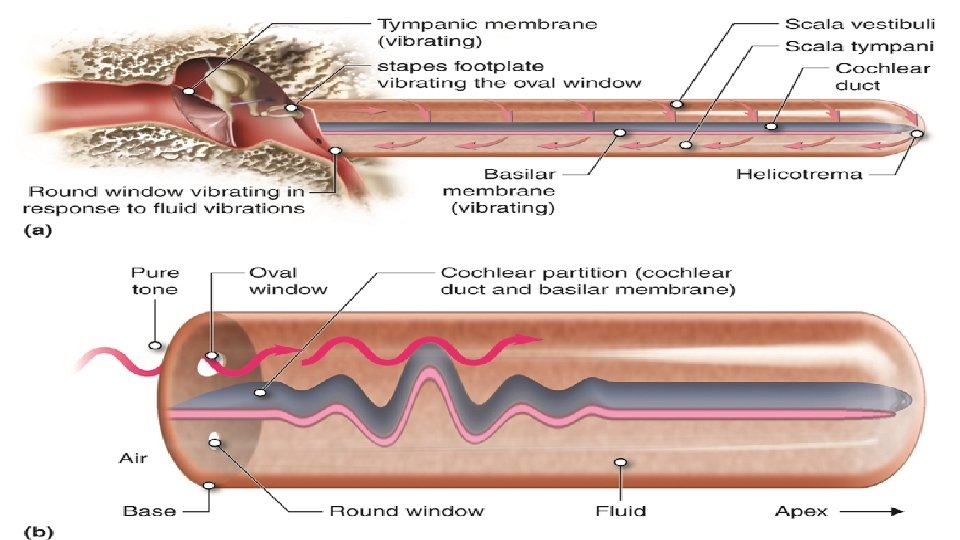
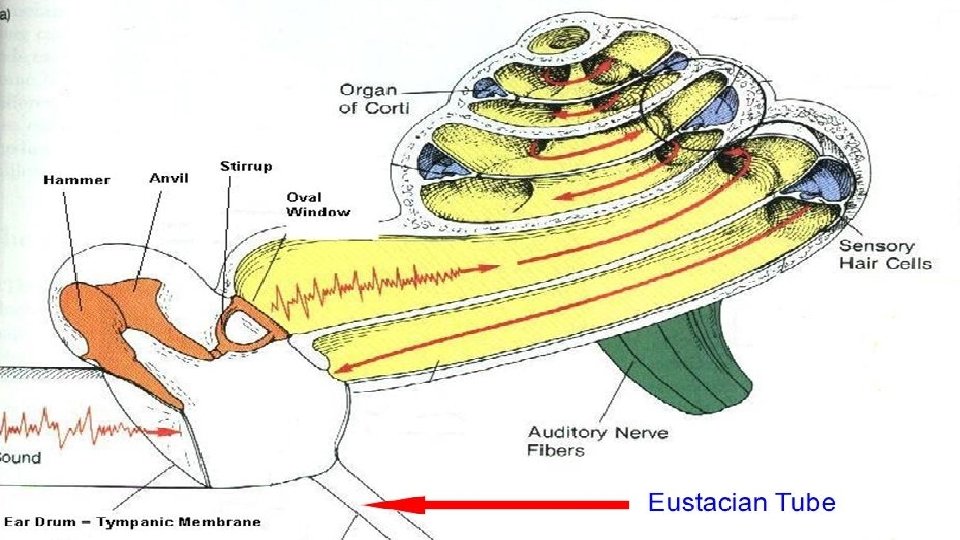
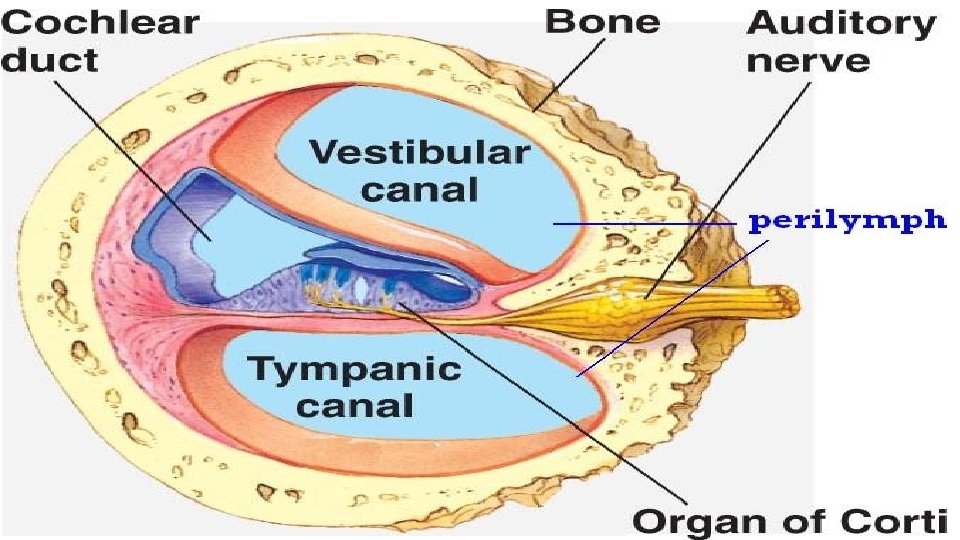
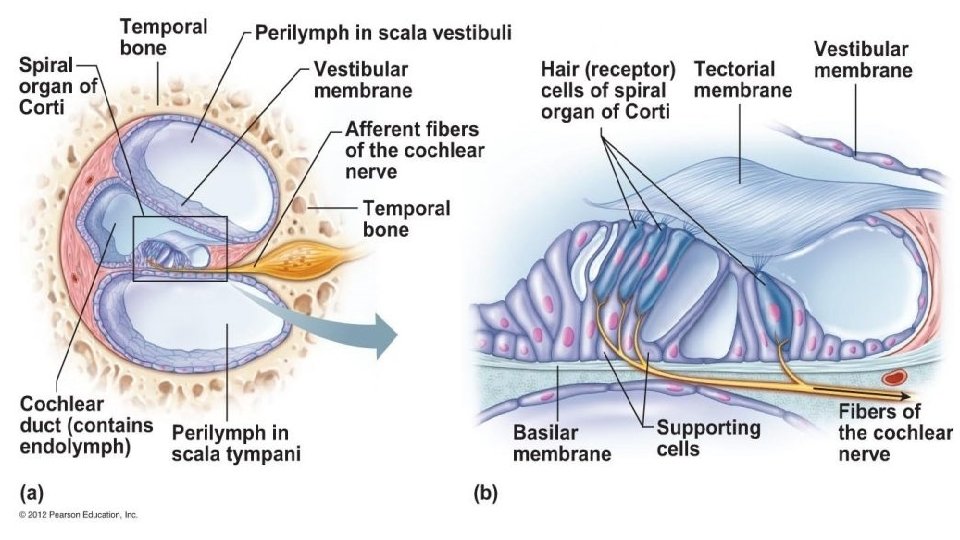
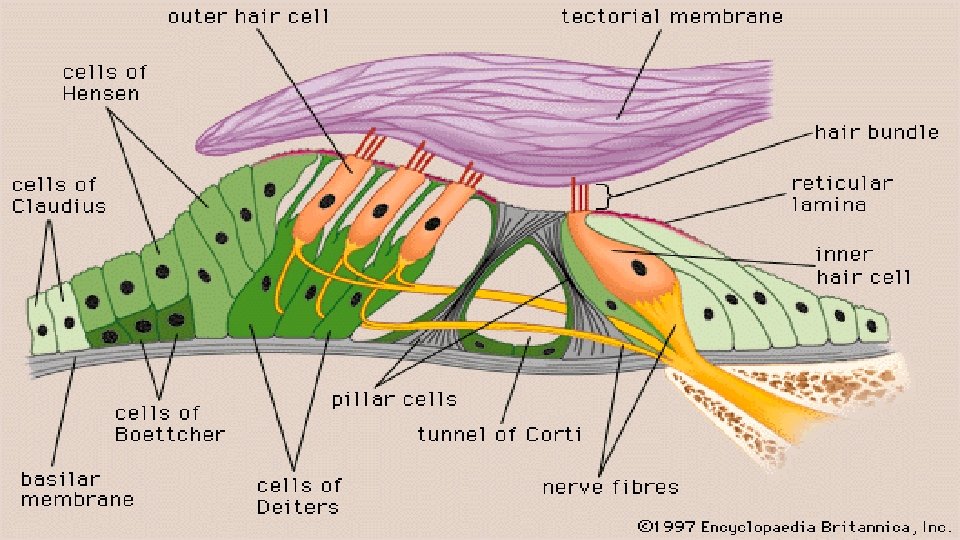
2. Physiology of hearing sound waves → auricle → external auditory canal → tympanic membrane → auditory ossicles (malleus, incus, stapes) → oval window → perilymph in cochlea → moves vestibular membrane of the cochlear duct → moves endolymph in cochlear duct → moves basilar membrane of organ of Corti → moves hair cells in the organ of Corti → hairs rub against the tectorial membrane (lays over the hairs) → depolarizes hair membranes → impulse travels to vestibulocochlear (VIII) nerve → medulla oblongata → midbrain → thalamus → cerebrum
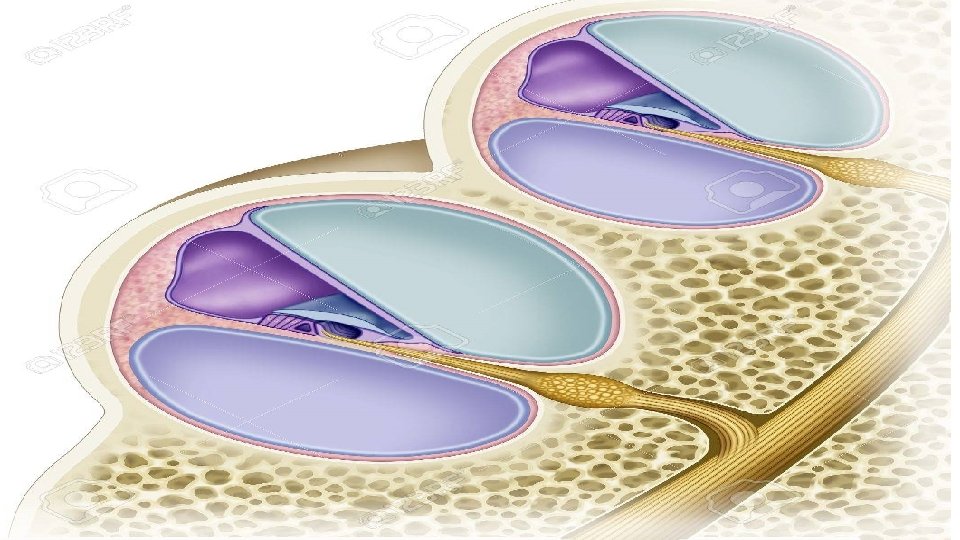
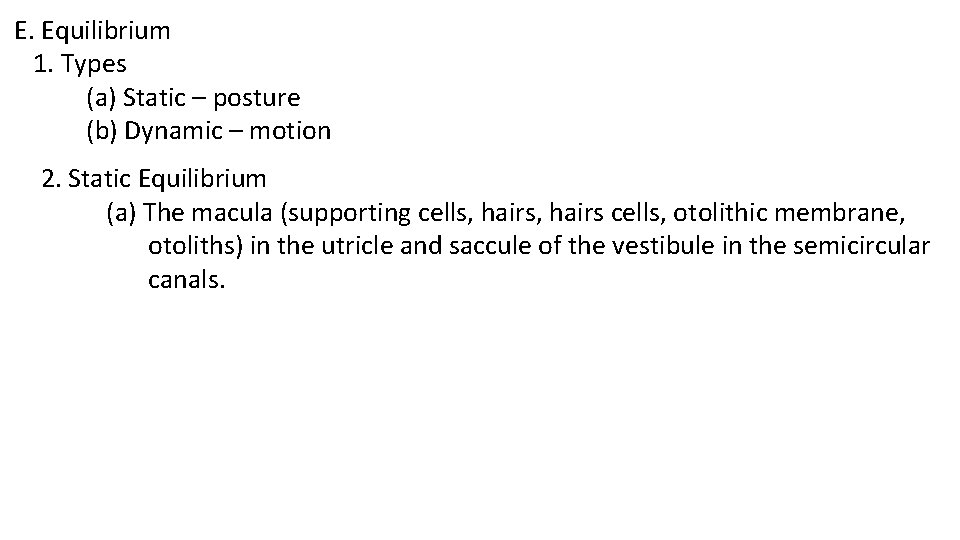
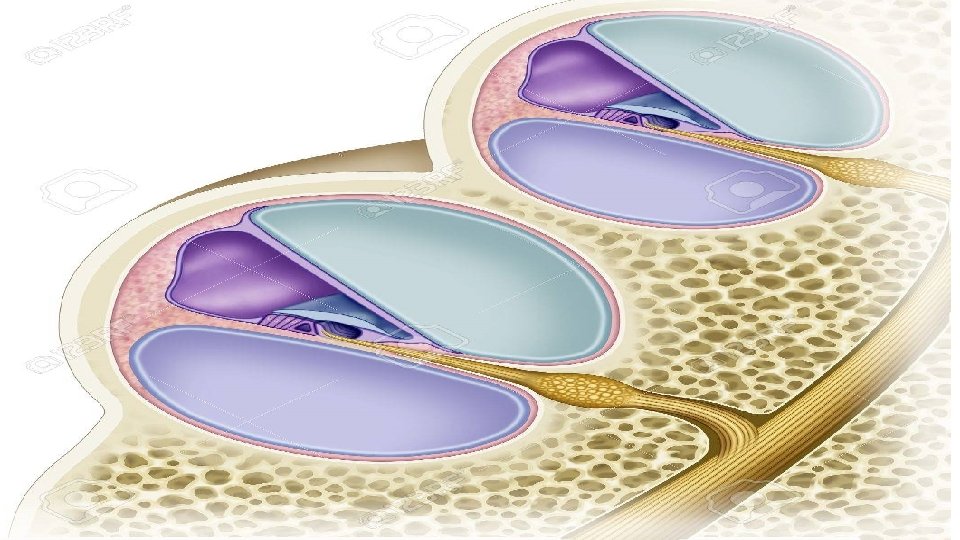
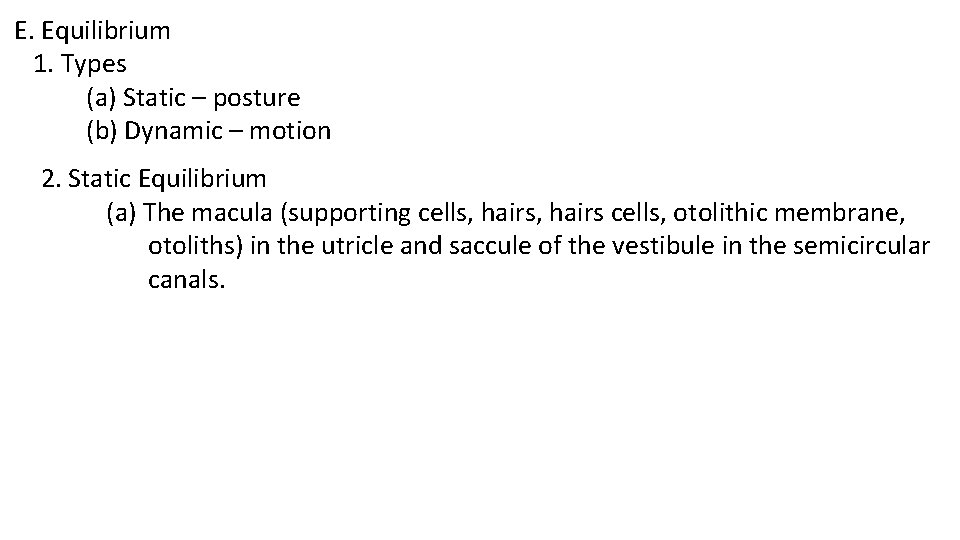
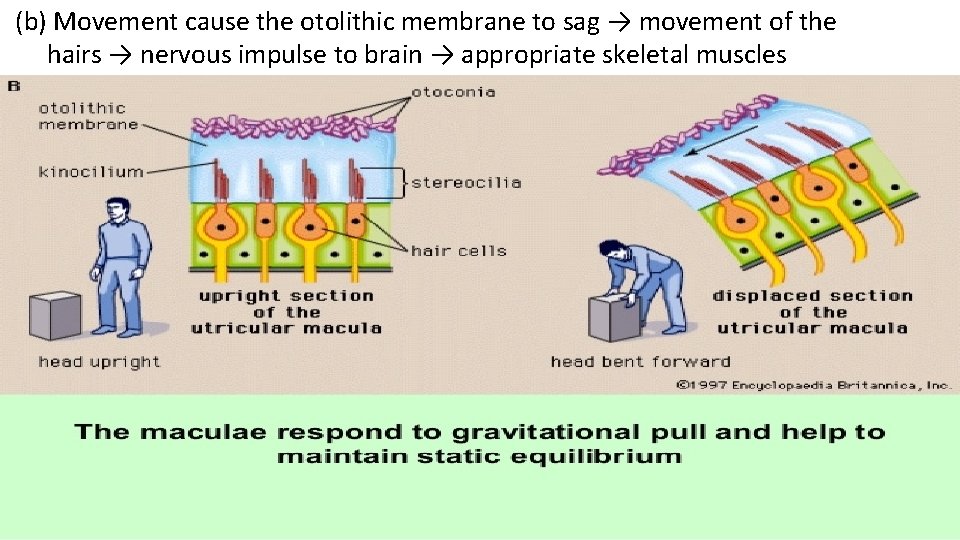
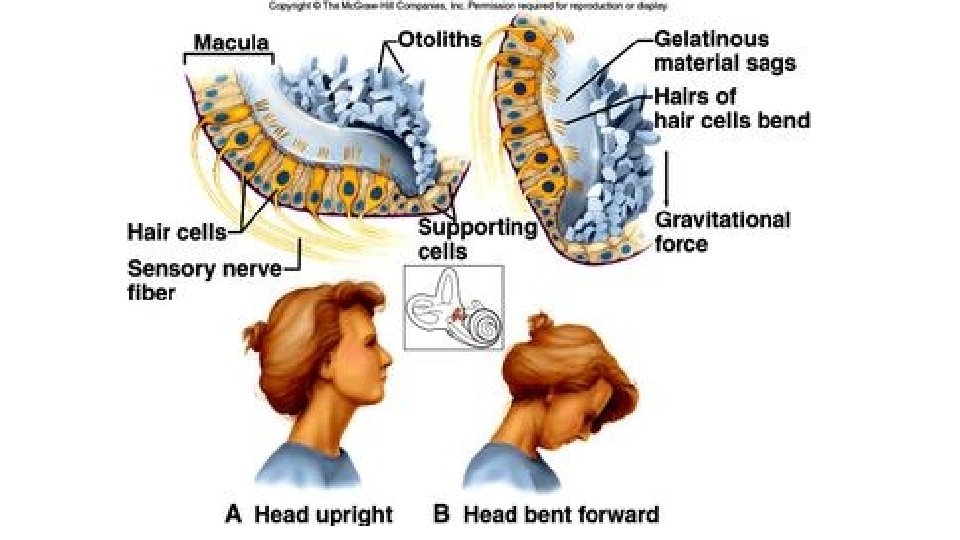
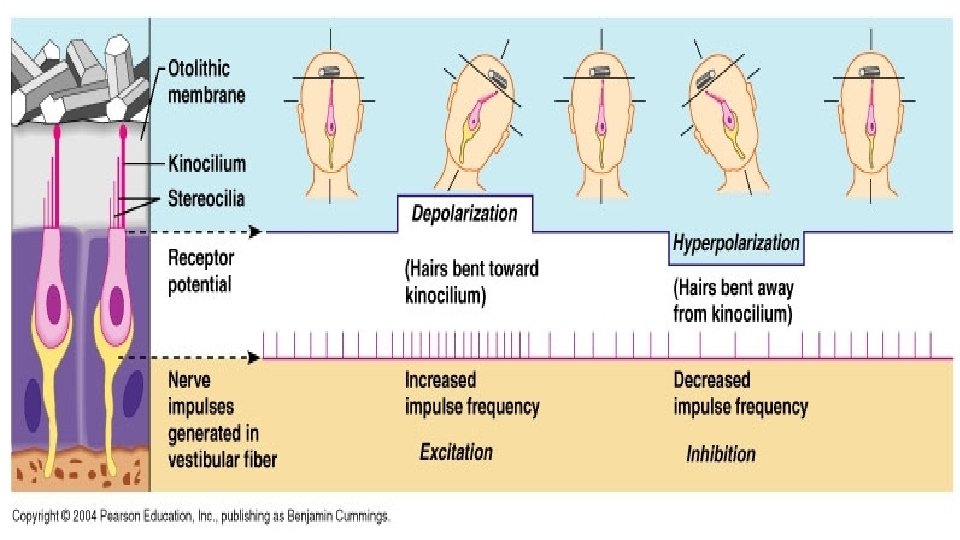
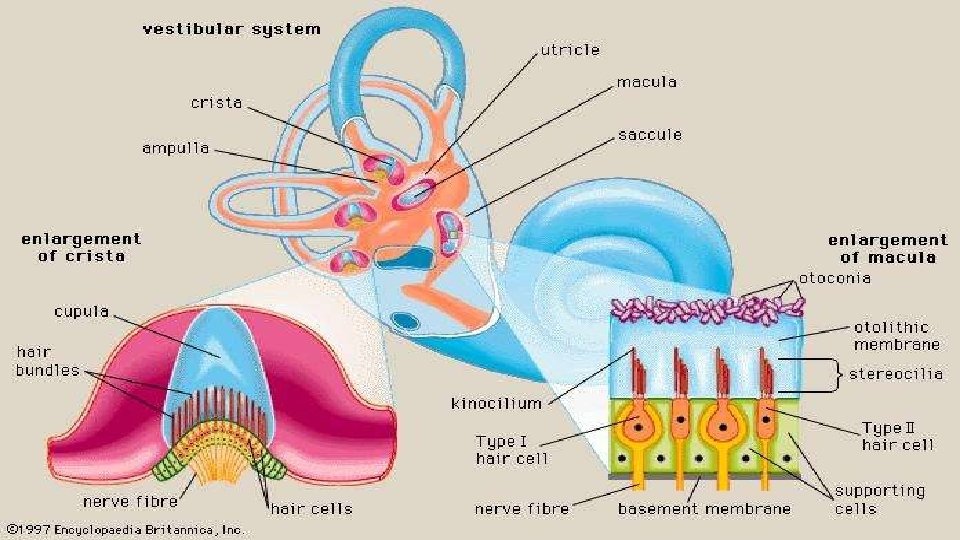
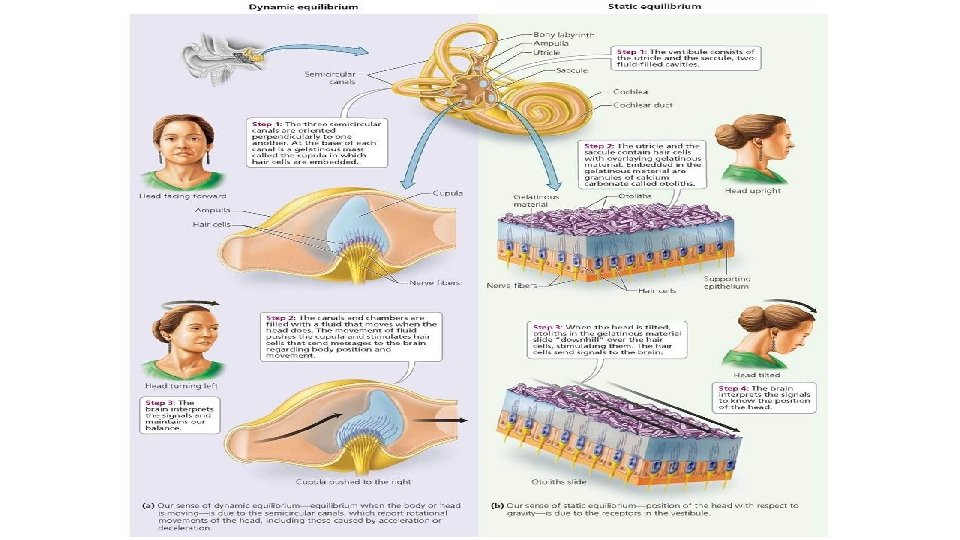
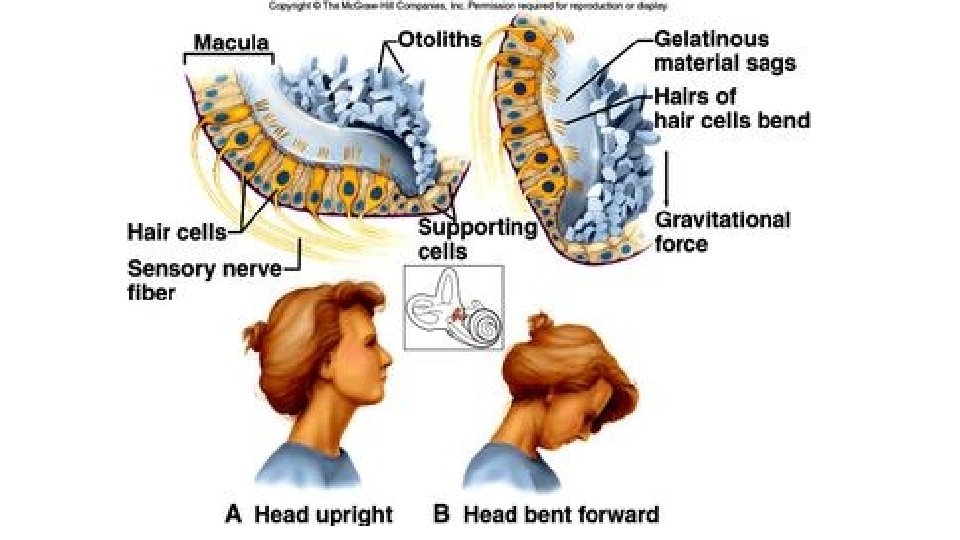
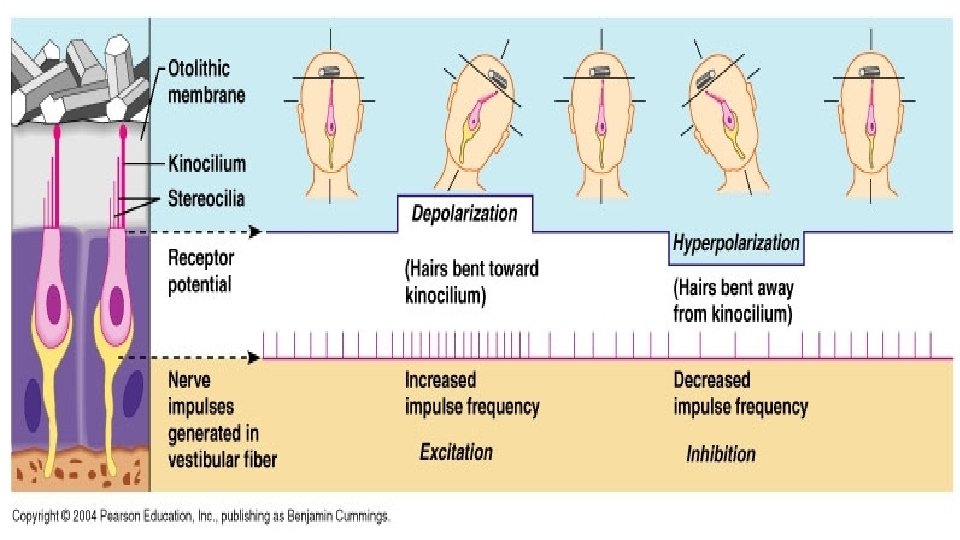
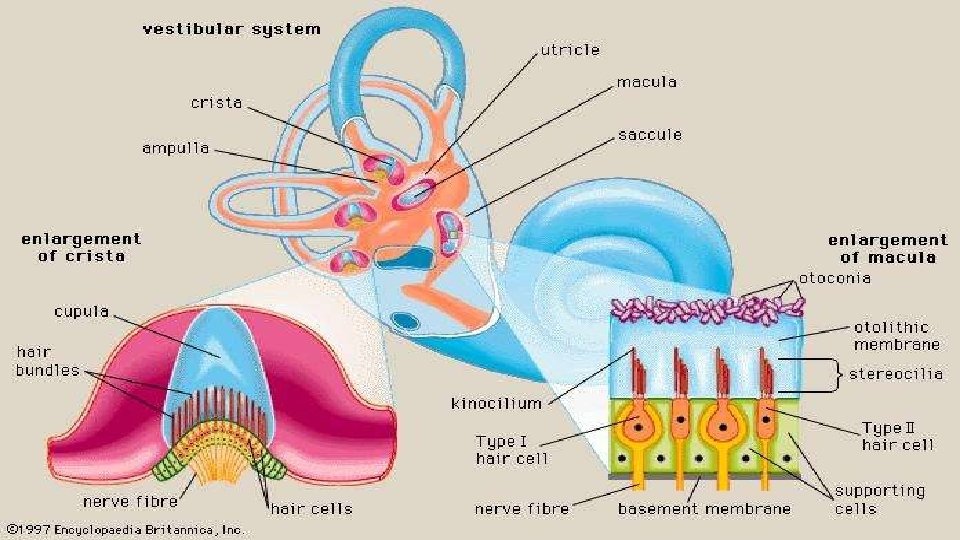
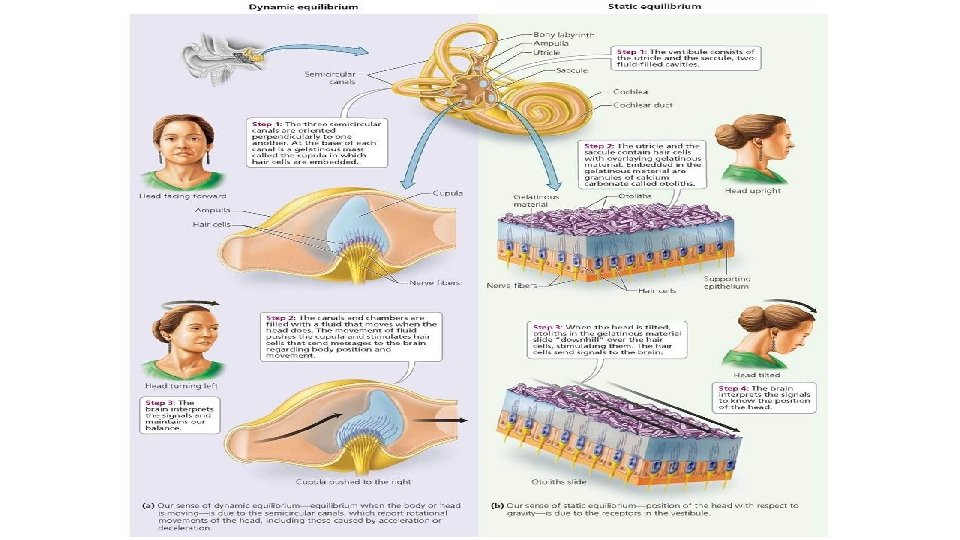
E. Equilibrium 1. Types (a) Static – posture (b) Dynamic – motion 2. Static Equilibrium (a) The macula (supporting cells, hairs cells, otolithic membrane, otoliths) in the utricle and saccule of the vestibule in the semicircular canals.
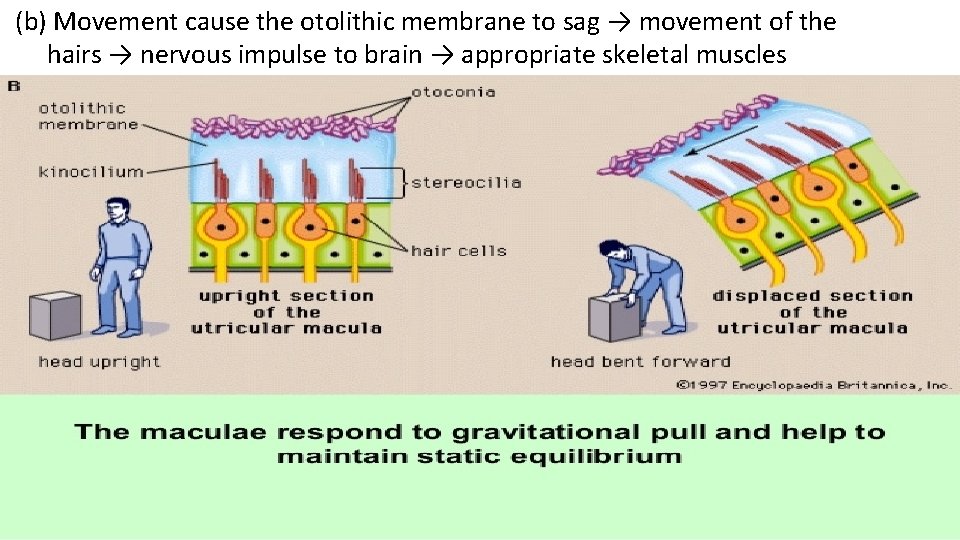
(b) Movement cause the otolithic membrane to sag → movement of the hairs → nervous impulse to brain → appropriate skeletal muscles
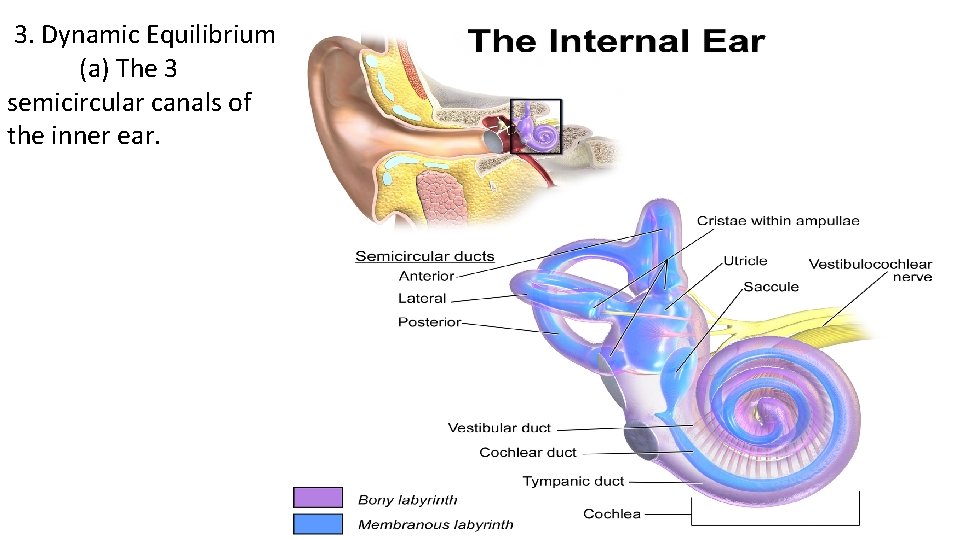
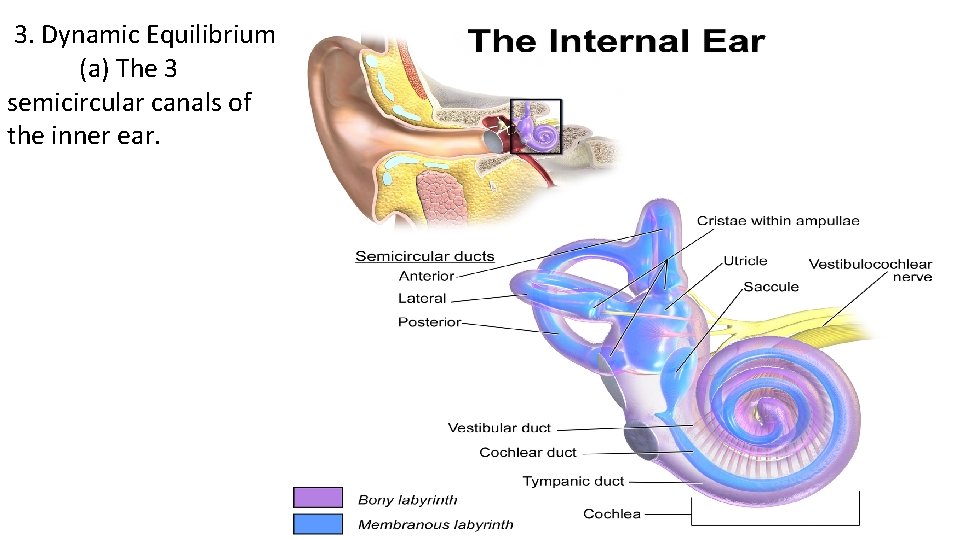
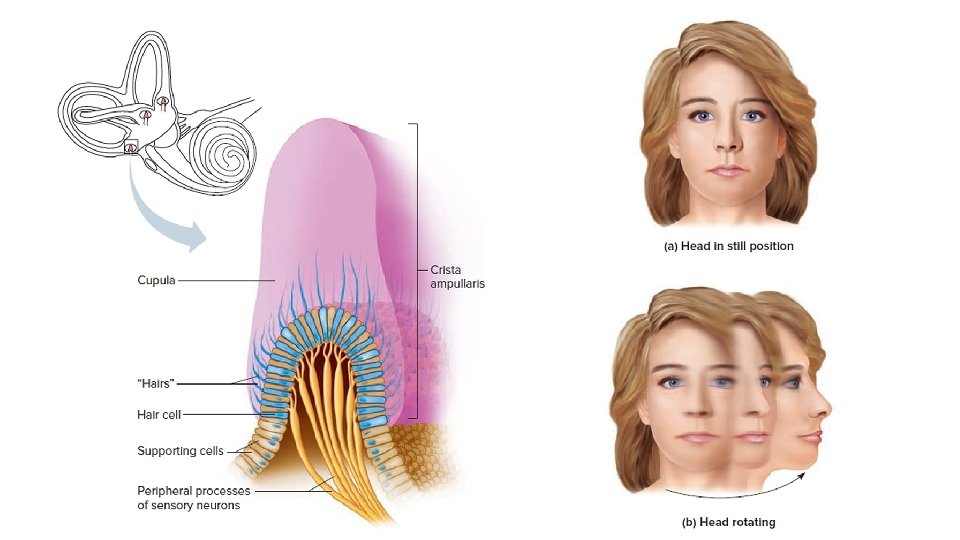
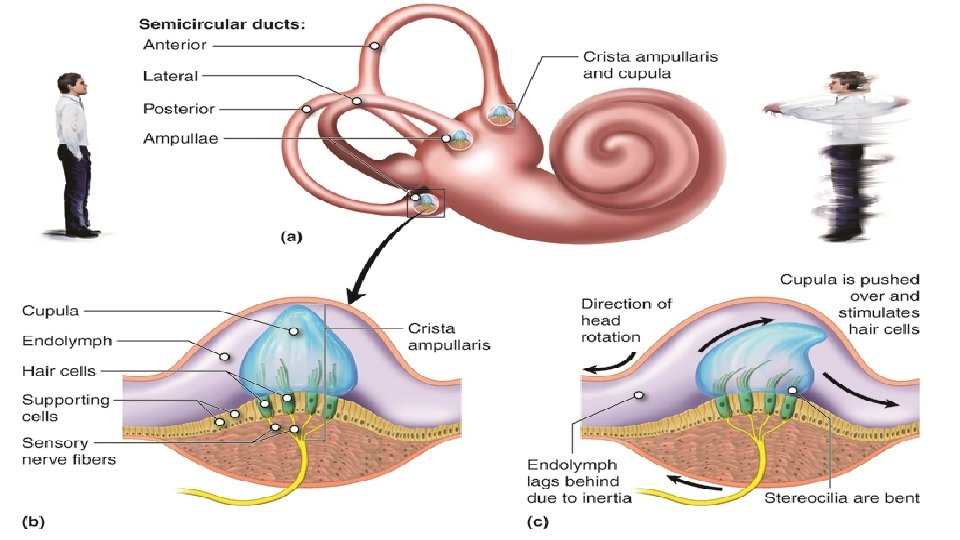
3. Dynamic Equilibrium (a) The 3 semicircular canals of the inner ear.
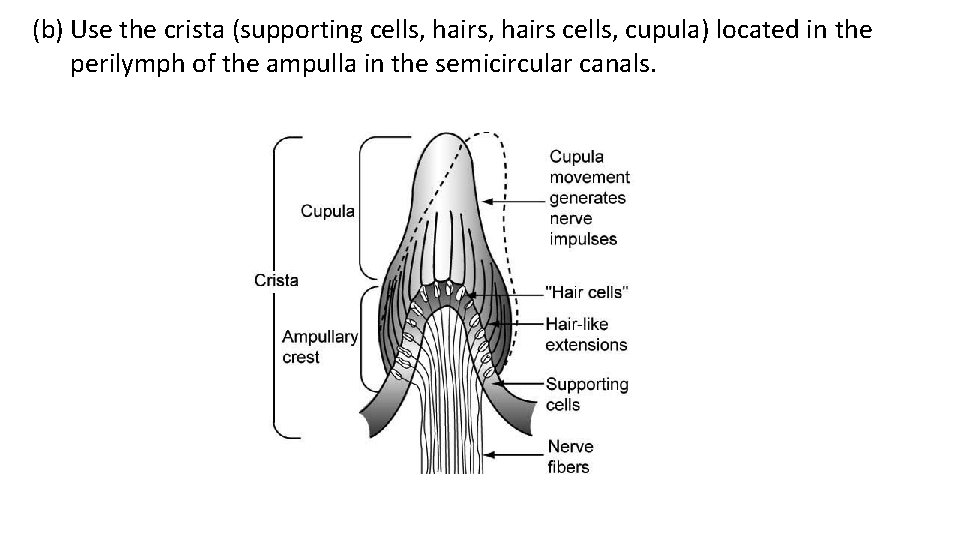
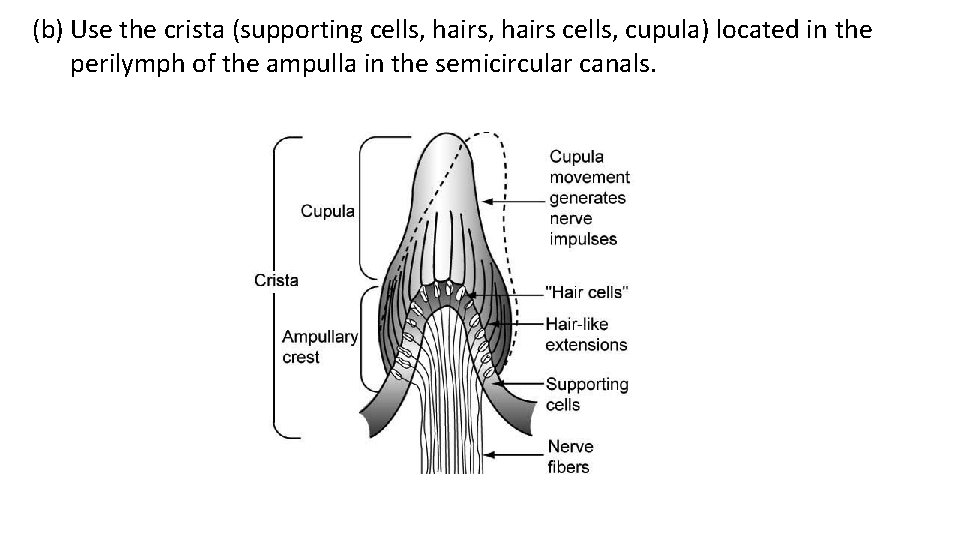
(b) Use the crista (supporting cells, hairs cells, cupula) located in the perilymph of the ampulla in the semicircular canals.
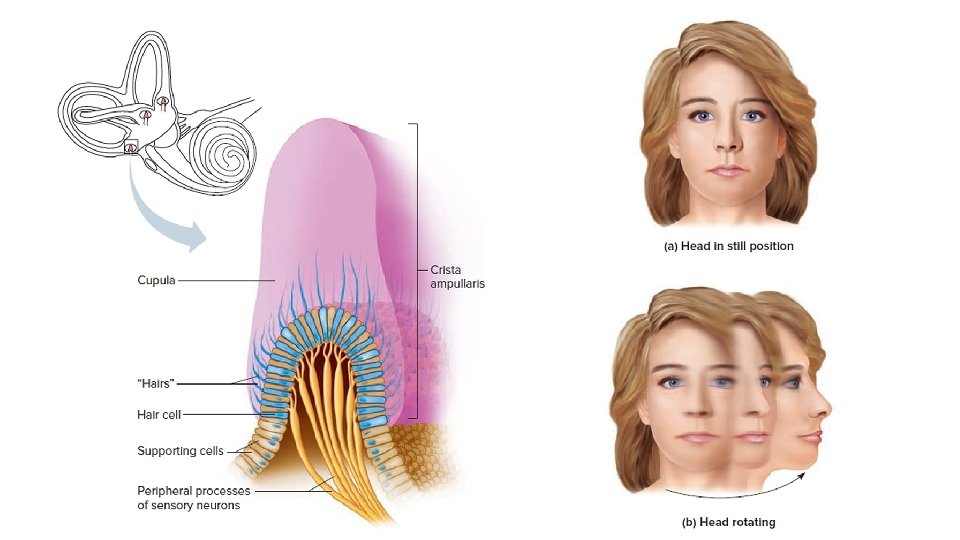
(c) Movement cause the perilymph to move → movement of the crista → nervous impulse to cerebellum → appropriate skeletal muscles
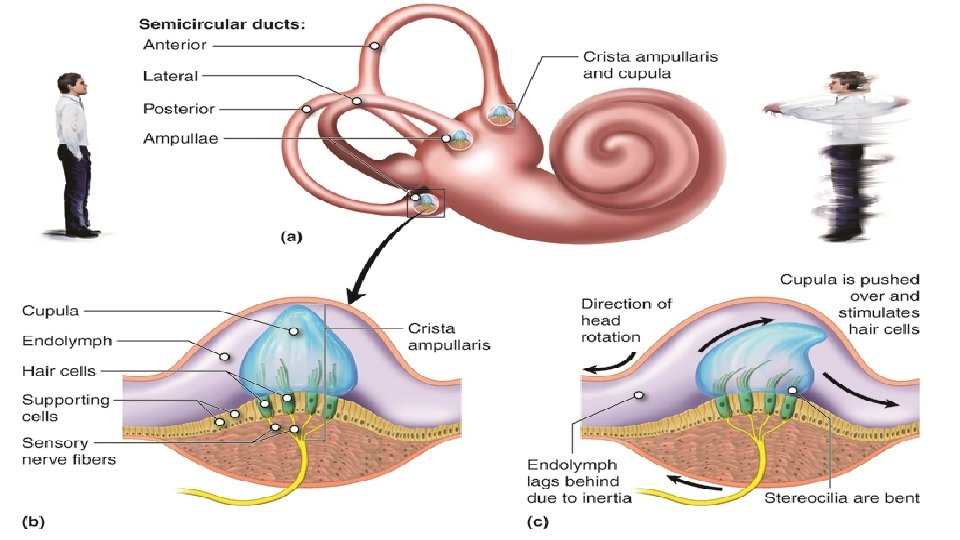
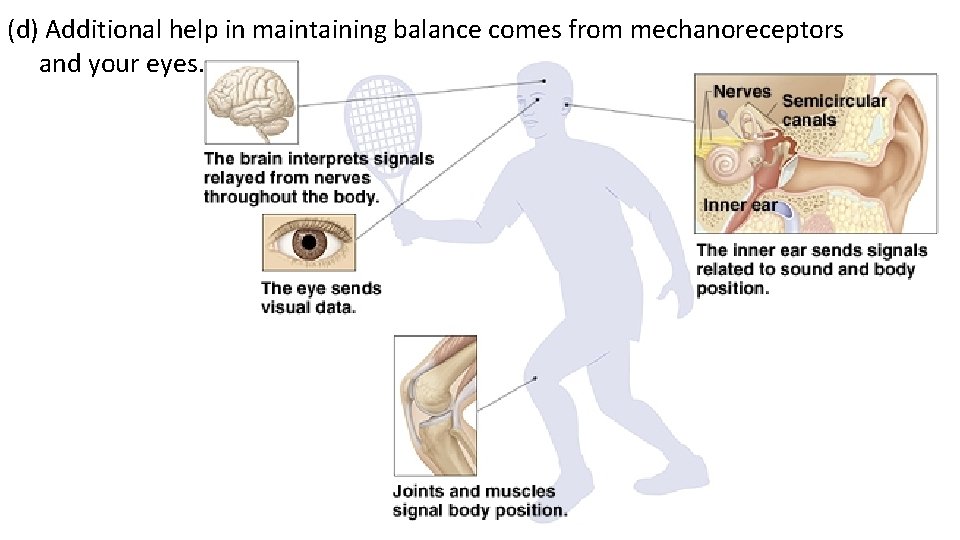
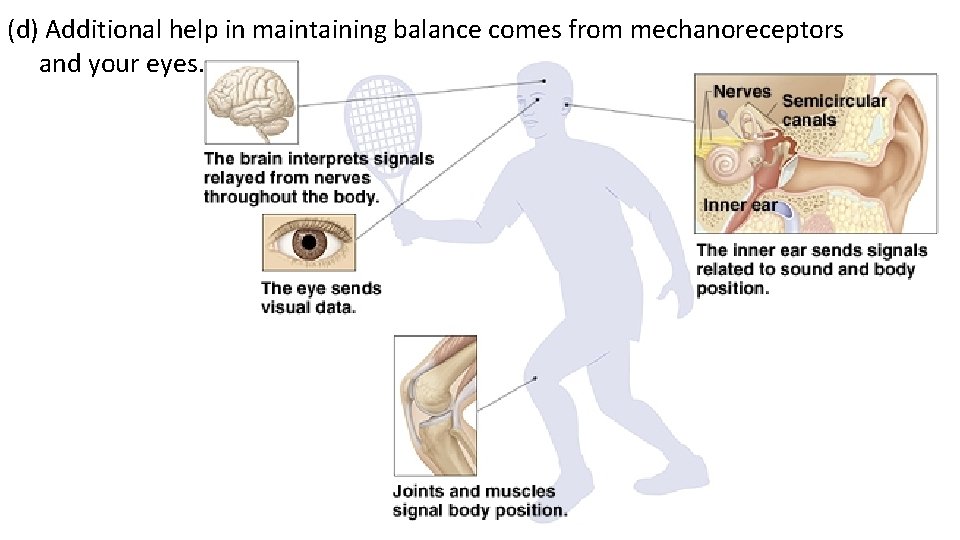
(d) Additional help in maintaining balance comes from mechanoreceptors and your eyes.