Sore throat Dr duaa Hiasat Clinical objectives 1
Sore throat Dr. duaa Hiasat
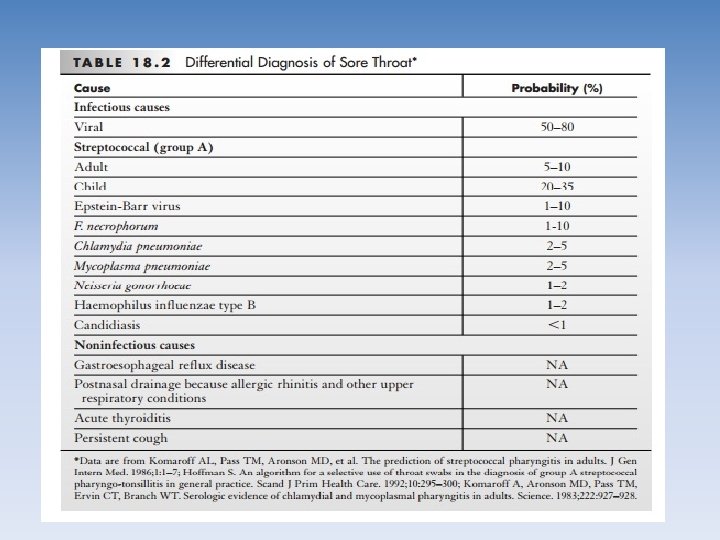
Clinical objectives 1. Describe the differential diagnosis of sore throat for patients of different ages. 2. Describe an evidence-based approach to diagnosis of strep throat and infectious mononucleosis that integrates the history and physical with judicious use of the laboratory. 3. Choose appropriate treatment for various causes of sore throat.
Definition • A sore throat is pain, scratchiness or irritation of the throat that often worsens with swallowing • About 4% of patient seeing a family physician report “sore throat “as the primary reason for causes. • It is the second –most common reason for an office visit.
Aetiology Infectious causes § Bacterial(GABHS) § Viral (most) § Fungal Noninfectious causes § Gastroesophageal reflux § Postnasal drainage because allergic rhinitis and other upper respiratory conditions § acute thyroiditis § Persistent cough § Trauma 1. External 2. Internal § Referred dental pain
Viral infection Most episodes of pharyngitis are caused by viruses , including § Adenoviruses § Influenza viruses § Paraifluenza virus § Respiratory syncytial virus
• Not necessary or important to determine the specific viruses responsible for the infection. • An exception Epstein-Barr virus infection, infectious mononucleosis, because of the protracted course and potentially serious complications of this illness such as : • (splenic rupture, respiratory compromise because severe tonsillar hypertrophy and cervical adenopathy)
Bacterial infections may be due to • GABHS most important of bacterial infection(because of it is rare but serious complication ) • Group B and group C • Chlamydia pneumoniae • Branhamella species • Haemophilus species • Mycoplasma pneumoniae
CLINICAL EVALUATION HISTORY AND PHYSICAL EXAMINATION
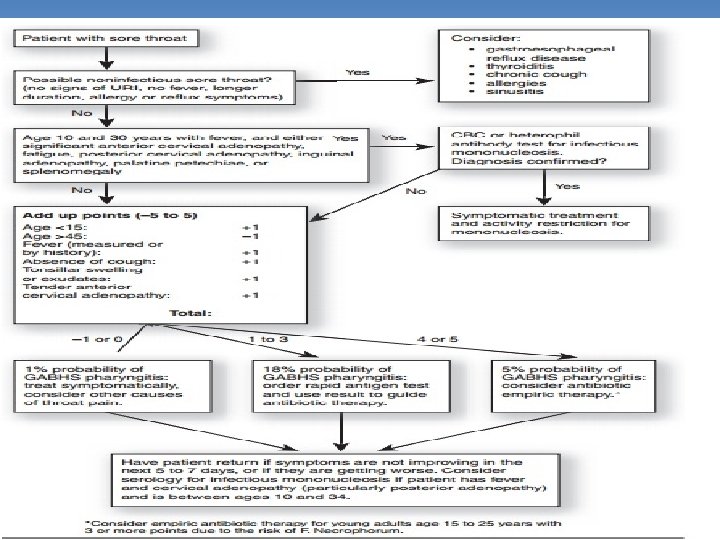
• Should determine whether it is infectious or noninfectious : • noninfectious should be suspected in : • Afebrile • No other sign of upper respiratory tract infection • Longer duration than 1 -2 weeks • And associated symptom with hurtburn , itchy eyes , postnasal drip • History of use antiacid • Symptome get worse late at night or early morning
Viral pharyngitis • • Fever Malaise Myalgias Headache A runny or congested nose Irritation or redness of the eyes Cough, hoarseness, soreness in the roof of the mouth
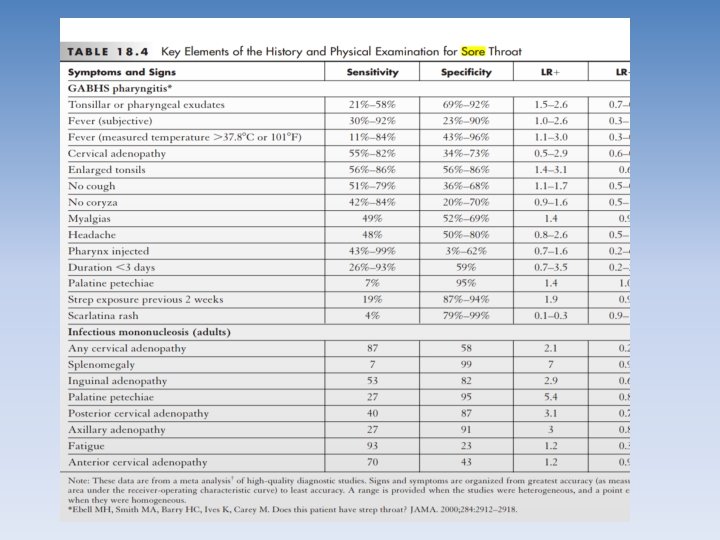
Bacteria –GABHS- Streptococcal pharyngitis • • • Fever>3 8 NOcough, Tonsillar enlargement Tonsillar or pharyngeal exudate, Anterior cervical adenopathy Myalgias, Recent strep exposure, Brief duration of illness before presentation, Headache also

Bacteria –GABHS- Streptococcal pharyngitis Pharyngeal injection pharynx looks red. Scarlatina rash (a fine sandpapery eruption)
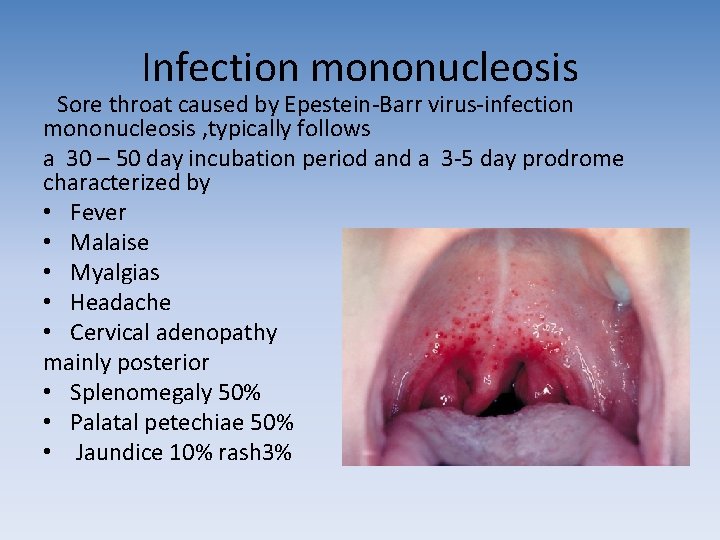
Infection mononucleosis Sore throat caused by Epestein-Barr virus-infection mononucleosis , typically follows a 30 – 50 day incubation period and a 3 -5 day prodrome characterized by • Fever • Malaise • Myalgias • Headache • Cervical adenopathy mainly posterior • Splenomegaly 50% • Palatal petechiae 50% • Jaundice 10% rash 3%
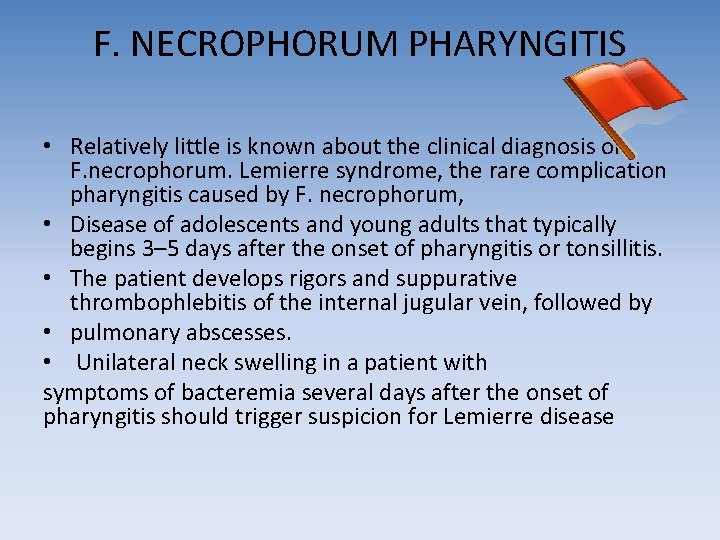
F. NECROPHORUM PHARYNGITIS • Relatively little is known about the clinical diagnosis of F. necrophorum. Lemierre syndrome, the rare complication pharyngitis caused by F. necrophorum, • Disease of adolescents and young adults that typically begins 3– 5 days after the onset of pharyngitis or tonsillitis. • The patient develops rigors and suppurative thrombophlebitis of the internal jugular vein, followed by • pulmonary abscesses. • Unilateral neck swelling in a patient with symptoms of bacteremia several days after the onset of pharyngitis should trigger suspicion for Lemierre disease
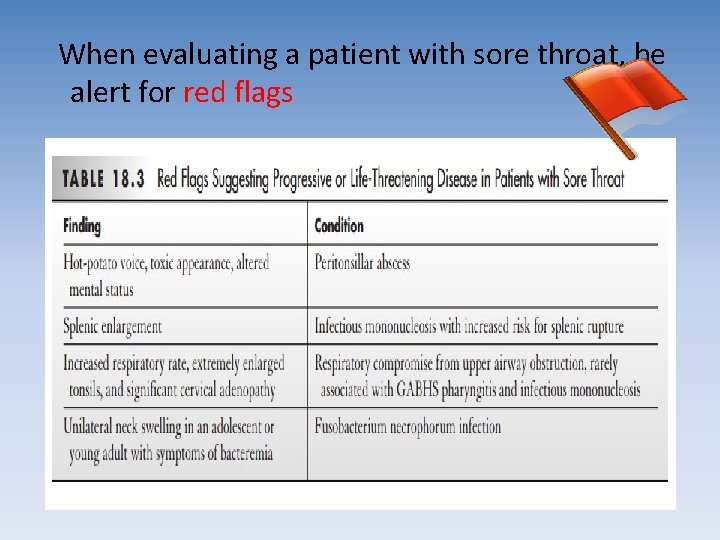
When evaluating a patient with sore throat, be alert for red flags
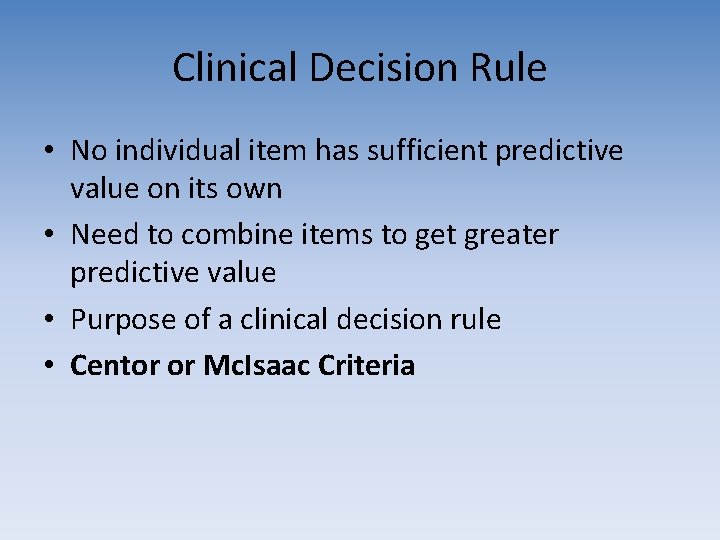
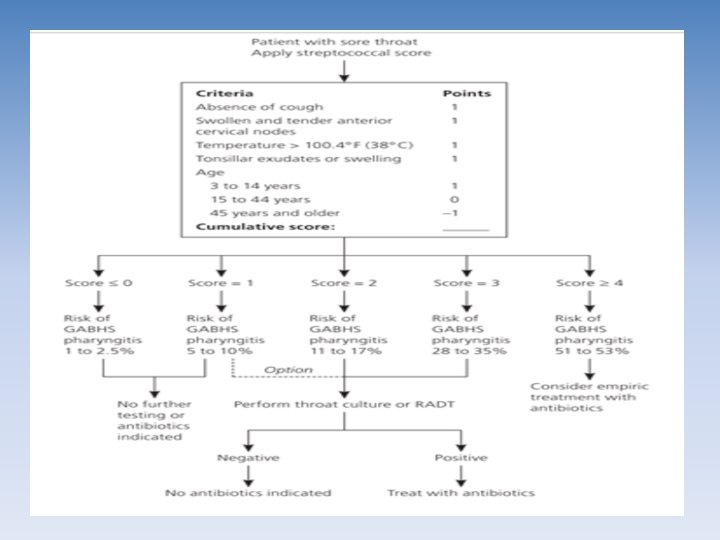
Clinical Decision Rule • No individual item has sufficient predictive value on its own • Need to combine items to get greater predictive value • Purpose of a clinical decision rule • Centor or Mc. Isaac Criteria
Diagnostic Testing
GABHS- Streptococcal pharyngitis • A variety of rapid antigen tests and cultures are available to test for the presence of GABHS bacteria in the pharynx. • Rapid antigen tests include enzyme immunoassays, latex agglutination tests, liposomal assays. • Although the throat culture test is often considered a gold standard.
Mononucleosis Two types of laboratory tests are useful for confirming the diagnosis of infectious mononucleosis: 1. The complete blood-CBC count with differential, 2. A variety of serologic tests.
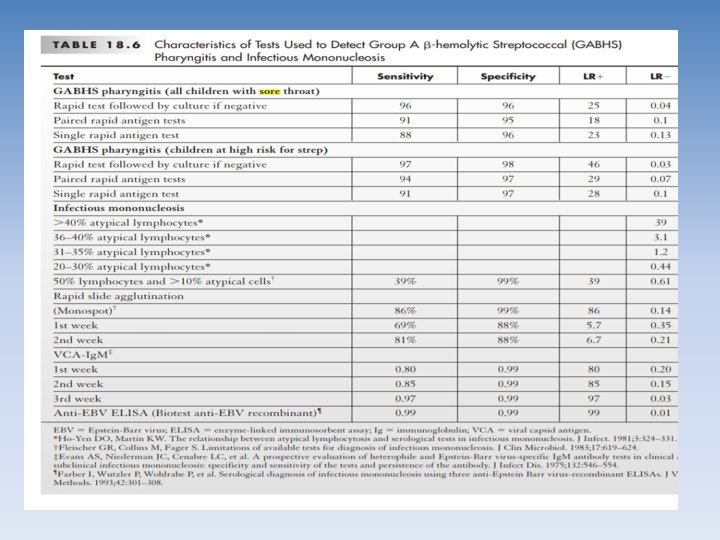
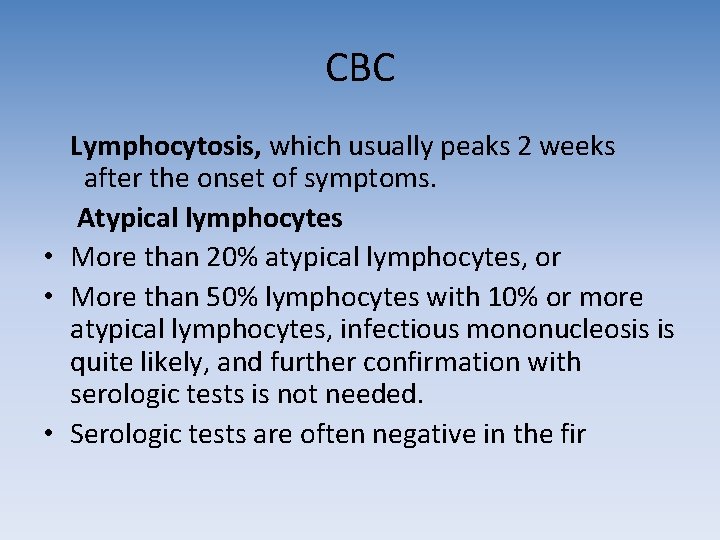
CBC Lymphocytosis, which usually peaks 2 weeks after the onset of symptoms. Atypical lymphocytes • More than 20% atypical lymphocytes, or • More than 50% lymphocytes with 10% or more atypical lymphocytes, infectious mononucleosis is quite likely, and further confirmation with serologic tests is not needed. • Serologic tests are often negative in the fir
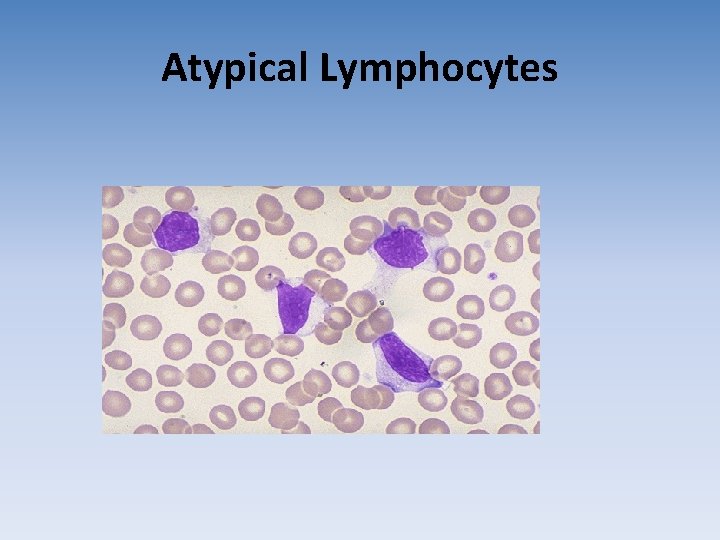
Atypical Lymphocytes
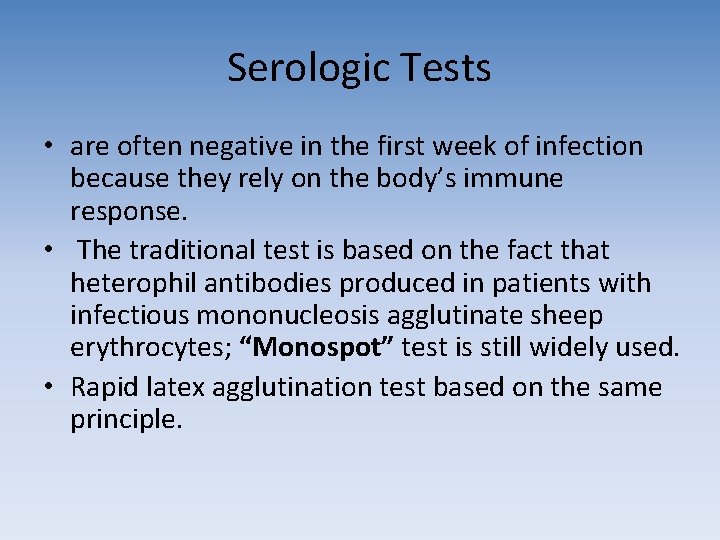
Serologic Tests • are often negative in the first week of infection because they rely on the body’s immune response. • The traditional test is based on the fact that heterophil antibodies produced in patients with infectious mononucleosis agglutinate sheep erythrocytes; “Monospot” test is still widely used. • Rapid latex agglutination test based on the same principle.
• Viral capsid antigen immunoglobulin M antibodies : ü produced relatively early in infection and do not persist once the acute infection is over. ü This test is quite sensitive and specific, ü the sensitivity improves during the second week of the illness. • Other laboratory tests ü aspartate aminotransferase (40 /L in 76% of patients) ü alkaline phosphatase (elevated in 71% of patients)

MANAGEMENT
![Viral pharyngitis Symptomatic treatment • Nonsteroidal anti-inflammatory drugs [NSAIDs] or Acetaminophen for fever and Viral pharyngitis Symptomatic treatment • Nonsteroidal anti-inflammatory drugs [NSAIDs] or Acetaminophen for fever and](http://slidetodoc.com/presentation_image_h2/7dd613a05ed1fece59adb09d21677c91/image-33.jpg)
Viral pharyngitis Symptomatic treatment • Nonsteroidal anti-inflammatory drugs [NSAIDs] or Acetaminophen for fever and throat pain • Gargling with 2% viscous lidocaine for patients with severe throat pain, • Over-the-counter (OTC) topical sprays (e. g. , Chloraseptic spray) • Herbal tea has been shown in a randomized trial to be more effective than placebo
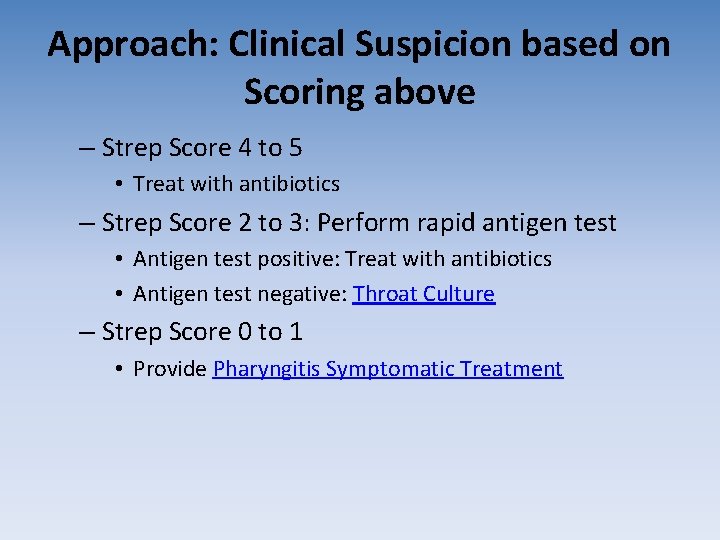
Approach: Clinical Suspicion based on Scoring above – Strep Score 4 to 5 • Treat with antibiotics – Strep Score 2 to 3: Perform rapid antigen test • Antigen test positive: Treat with antibiotics • Antigen test negative: Throat Culture – Strep Score 0 to 1 • Provide Pharyngitis Symptomatic Treatment
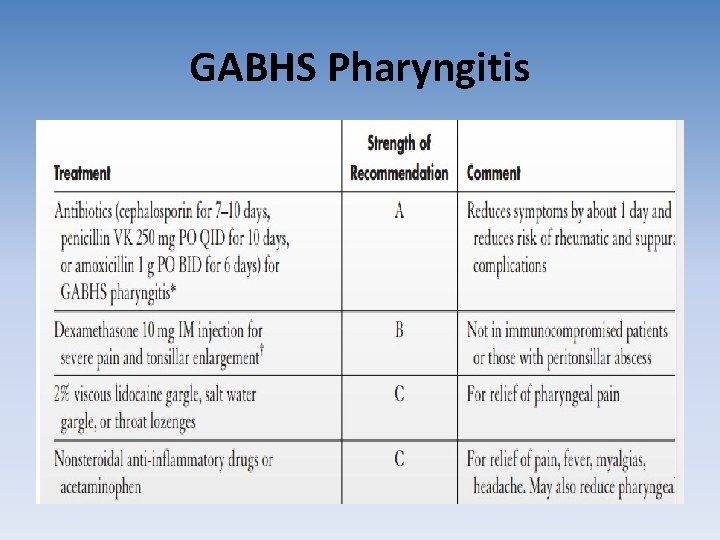
GABHS Pharyngitis
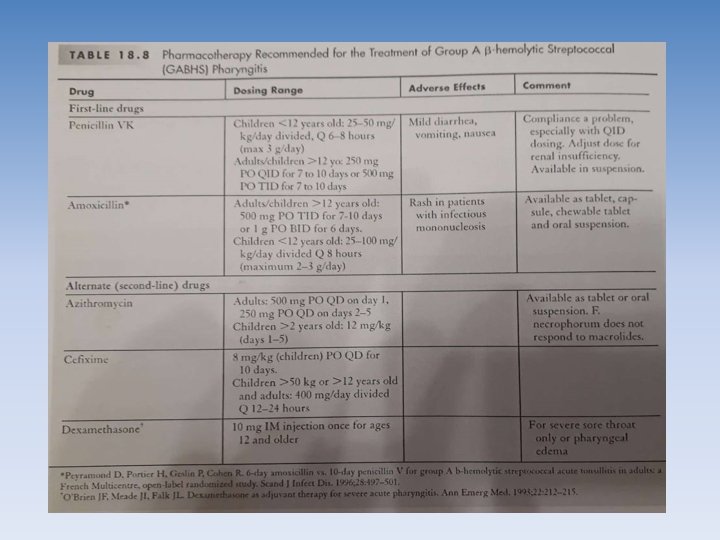
Child can return to school on the second day after the office visit.
Infectious Mononucleosis • Symptomatical treatment • Rest, • Oral fluids, and NSAIDs or acetaminophen for fever and myalgias. • Aspirin should be avoided because Of Reye syndrome has been reported in association with IM. • Corticosteroids for significant pharyngeal edema that causes or threatens respiratory compromise.

• Participation in contact sports (e. g. , cheerleading, basketball, hockey, football, soccer) should be restricted during the acute phase of the illness and cont to be restricted at least 4 weeks and as long as the spleen is palpable • patient with coexisting strep pharyngitis based on sign and symptom should start AB other than amoxicillin
F. NECROPHORUM PHARYNGITIS • NO diagnostic test available to identify this agent. • So any patient adolescent or young adult with 3 or more of centor criteria should start empirically AB other than macraloids.
Complications
GABHS Pharyngitis 1. Suppurative • bacteremia, • cervical lymphadenitis, • endocarditis, • mastoiditis, meningitis, otitis media, peritonsillar or retropharyngeal abscess, and/or pneumonia 2. Non-Suppurative Poststreptococcal • Glomerulonephritis • Rheumatic fever.
Scarlet fever • Scarlet fever is associated with GABHS pharyngitis • punctate, erythematous, blanchable, sandpaperlike exanthem. • The rash is found in the neck, groin, and axillae, and is accentuated in body folds and creases (Pastia’s lines). • The pharynx and tonsils are erythematous and covered with exudates. • The tongue may be bright red with a white coating (strawberry tongue)

Scarlet fever
Infectious Mononucleosis • Splenomegaly- In extreme cases spleen rupture • Hepatitis. You may experience mild liver inflammation (hepatitis). • Jaundice. : • Anemia -Thrombocytopenia — • Heart problems — (myocarditis) • Complications involving the nervous system — meningitis, encephalitis and Guillain-Barre syndrome • Enlarged tonsils -Respiratory compromise
PATIENT EDUCATION Several goals. • Patients should understand that only a minority of sore throats are caused by streptococcal pharyngitis or other bacteria, • Symptomatic treatment is usually sufficient. • They should also be told to relieve the symptoms of sore throat, using salt water gargles, NSAIDs, OTC throat sprays, and OTC lozenges (e. g. , Chloraseptic ).
Case 1 • A 7 -year-old male presents with a 3 -day history of sore throat, hoarseness, fever to 100°F (38°C), and cough. Your examination reveals injection of his tonsils, no exudates, shotty lymphadenopathy, and normal breath sounds. Which one of the following would be most appropriate? A) Symptomatic treatment only B) Empiric treatment for streptococcal pharyngitis C) A rapid antigen test for streptococcal pharyngitis D) A throat culture for streptococcal pharyngitis E) An office test for mononucleosis

• Thanks
- Slides: 48