Somatoform and Sleep Disorders Nursing 201 characterized physical





- Slides: 44
Somatoform and Sleep Disorders Nursing 201
characterized • physical symptoms suggesting medical disease but without a demonstrable organic pathological condition or a known pathophysiological mechanism to account for them. • Somatoform disorders are more common – – In women than in men In those who are poorly educated In those who live in rural communities In those who are poor

Assessment • A syndrome of multiple somatic symptoms that cannot be explained medically and are associated with psychosocial distress and long-term seeking of assistance from health care professionals.
Predisposing Factors • Theory of family dynamics – “Psychosomatic families” – Role modeling • Cultural and environmental factors – Low socioeconomic, occupational, and educational status • Genetic factors – Possible inheritable predisposition • Transactional Model of Stress/Adaptation – The etiology of somatization disorder is more likely influenced by multiple factors
Nursing Diagnosis • Assessment
Outcomes
Planning/Implementation
Evaluation
Pain Disorder: Assessment • The predominant disturbance in pain disorder is severe and prolonged pain that causes – Clinically significant distress – Impairment in social, occupational, or other areas of functioning • Even when an organic pathological condition is detected, the pain complaint may be evidenced by correlation of a stressful situation with onset of symptoms.
• The disorder may be maintained by: – Primary gains: the symptom enables the client to avoid some unpleasant activity. – Secondary gains: the symptom promotes emotional support or attention for the client. • Psychodynamic theory – Symbolically expressing an intrapsychic conflict through the body • Behavior theory – Negative reinforcement results when the pain behavior prevents an undesirable phenomenon from occurring (i. e. , provides relief from responsibilities for the client)
• Theory of family dynamics – “Pain games” – Tertiary gain • Neurophysiological theory – Afferent pain fibers – Serotonin/endorphins
Nursing Diagnosis • Assessment
Outcomes
Planning/Implementation
Evaluation
Hypochondriasis: Assessment • Unrealistic or inaccurate interpretation of physical symptoms or sensations, leading to preoccupation and fear of having a serious disease • Even in the presence of medical disease, the symptoms grossly exceed extent of pathological condition. • Anxiety and depression are common findings, and obsessive-compulsive traits frequently accompany the disorder.
Predisposing Factors • Psychodynamic theory – Ego-defense mechanism – Transformation of aggressive and hostile wishes toward others into physical complaints about self to others – Defense against guilt • Cognitive theory – Hypochondriasis arises out of perceptual and cognitive abnormalities. • Social learning theory – Somatic complaints are often reinforced when the sick role relieves the client of the need to deal with a stressful situation.
• Past experience with physical illness – Previous experience can predispose to hypochondriasis. *Genetic influences • Transactional Model of Stress/Adaptation – The etiology of hypochondriasis is likely influenced by multiple factors.
Nursing Diagnosis • Assessment
Outcomes
Planning/Implementation
Evaluation
Conversion Disorder: Assessment • A loss of or change in body function resulting from a psychological conflict, the physical symptoms of which cannot be explained by any known medical disorder or pathophysiological mechanism • The client often expresses a relative lack of concern that is out of keeping with the severity of the impairment. This lack of concern is termed la belle indifference and may be a clue to the physician that the problem is psychological rather than physical.
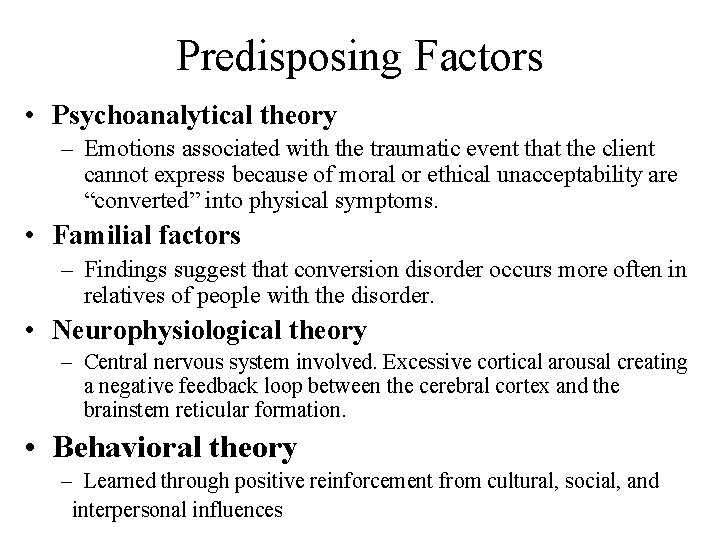
Predisposing Factors • Psychoanalytical theory – Emotions associated with the traumatic event that the client cannot express because of moral or ethical unacceptability are “converted” into physical symptoms. • Familial factors – Findings suggest that conversion disorder occurs more often in relatives of people with the disorder. • Neurophysiological theory – Central nervous system involved. Excessive cortical arousal creating a negative feedback loop between the cerebral cortex and the brainstem reticular formation. • Behavioral theory – Learned through positive reinforcement from cultural, social, and interpersonal influences
• Transactional Model of Stress/Adaptation – The etiology of conversion disorder is most likely influenced by multiple factors.

Nursing Diagnosis • Assessment
Outcomes
Planning/Implementation

Evaluation

Body Dysmorphic Disorder: Assessment • Characterized by the exaggerated belief that the body is deformed or defective in some specific way • Common complaints involve imagined or slight flaws of face or head • Symptoms of depression and characteristics associated with OCD common in people with body dysmorphic disorder
Predisposing Factors • Etiology unknown – In some clients, belief is result of another more pervasive psychiatric disorder, such as schizophrenia, major mood disorder, or anxiety disorder – Classified as one of several monosymptomatic hypochondriacal syndromes • Defined as the fear of some physical defect thought to be noticeable to others although the client appears normal.

Nursing Diagnosis • Assessment
Outcomes
Evaluation
Sleep Disorders: Introduction • About 75 percent of adult Americans suffer from a sleep problem. • 69% of all children experience sleep problems • The prevalence of sleep disorders increases with advancing age • Sleep disorders add an estimated $28 billion to the national health care bill. • Common types of sleep disorders include insomnia, hypersomnia, parasomnias, and circadian rhythm sleep disorders
Sleep Disorders: Assessment • Insomnia – Difficulty falling or staying sleep • Hypersomnia (somnolence) – Excessive sleepiness or seeking excessive amounts of sleep • Narcolepsy: Similar to hypersomnia – Characteristic manifestation: Sleep attacks; the person cannot prevent falling asleep • Parasomnias – Nightmares, sleep terrors, sleep walking
• Sleep terror disorder – Manifestations include abrupt arousal from sleep with a piercing scream or cry • Circadian rhythm sleep disorders – Shift-work type – Jet-lag type – Delayed sleep phase type
Predisposing Factors • Genetic or familial patterns are thought to play a contributing role in primary insomnia, primary hypersomnia, narcolepsy, sleep terror disorder, and sleepwalking. • Various medical conditions, as well as aging, have been implicated in the etiology of insomnia. • Psychiatric or environmental conditions can contribute to insomnia or hypersomnia. • Activities that interfere with the 24 -hour circadian rhythm hormonal and neurotransmitter functioning within the body predispose people to sleep-wake schedule disturbances.
Nursing Diagnosis • Assessment
Outcomes
Planning/Implementation
Client/Family Education
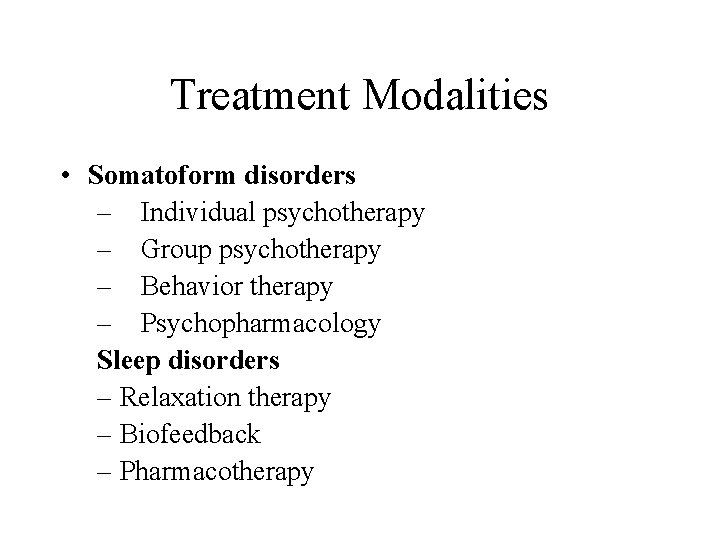
Treatment Modalities • Somatoform disorders – Individual psychotherapy – Group psychotherapy – Behavior therapy – Psychopharmacology Sleep disorders – Relaxation therapy – Biofeedback – Pharmacotherapy
• Primary hypersomnia/narcolepsy – Pharmacotherapy – CNS stimulants such as amphetamines • Parasomnias – Centers around measures to relieve obvious stress within the family – Individual or family therapy – Interventions to prevent injury
 Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders Neurosis
Neurosis Somatoform disorder nursing diagnosis
Somatoform disorder nursing diagnosis Somatization disorder
Somatization disorder Who analgesic ladder
Who analgesic ladder Inflexible personality
Inflexible personality Sleep disorders
Sleep disorders Psychiatric nursing theories
Psychiatric nursing theories Sleep disorders
Sleep disorders Sleep disorders
Sleep disorders Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Somatization disorder
Somatization disorder Gangguan somatoform
Gangguan somatoform What causes hyperventilation
What causes hyperventilation Epidemiologi gangguan somatoform
Epidemiologi gangguan somatoform Sir philip sidney sonnet 39
Sir philip sidney sonnet 39 Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Physical disorders and health psychology
Physical disorders and health psychology Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Nanda nursing diagnosis for eye disorders
Nanda nursing diagnosis for eye disorders Nursing care for gastrointestinal disorders
Nursing care for gastrointestinal disorders Borborygmi
Borborygmi Team nursing model advantages and disadvantages
Team nursing model advantages and disadvantages Math 201 bryant and stratton
Math 201 bryant and stratton Pricing tripod in service marketing
Pricing tripod in service marketing Physical fitness test grade 9
Physical fitness test grade 9 According to jung the unconscious mind is characterized by
According to jung the unconscious mind is characterized by The roaring '20s were characterized by
The roaring '20s were characterized by Diabetes mellitus is a metabolic disease characterized by
Diabetes mellitus is a metabolic disease characterized by Chaparral biomes are generally _______.
Chaparral biomes are generally _______. Workgroups are characterized by
Workgroups are characterized by 3e quick communication
3e quick communication A large geographic area characterized
A large geographic area characterized How are biomes characterized
How are biomes characterized Theme of the seventh man
Theme of the seventh man Subordinate defensiveness is characterized by
Subordinate defensiveness is characterized by Which trend characterized thomas jefferson's presidency?
Which trend characterized thomas jefferson's presidency? Characterization of the pardoner
Characterization of the pardoner Minoan architecture is characterized by fortified citadels.
Minoan architecture is characterized by fortified citadels. Asconoid definition
Asconoid definition Ocd is characterized by
Ocd is characterized by Characterized
Characterized Anorexia nervosa is characterized
Anorexia nervosa is characterized