Somatic Symptom Disorder in Primary Care Setting Part



![Somatic Symptom Scale – 8 [SSS-8] (Table is hyperlinked) Somatic Symptom Scale – 8 [SSS-8] (Table is hyperlinked)](https://slidetodoc.com/presentation_image_h2/a151397dc1a5b712939e02f673783d5e/image-20.jpg)


- Slides: 26
Somatic Symptom Disorder in Primary Care Setting - Part II Presented by: Ruth Tadesse, MS, RN Date: 5/21/2015
Disclosures and Learning Objectives: • Review DSM 5 criteria used to diagnose somatic symptom disorders. • Identify best practice treatment methods used to manage somatic symptom disorders. • Know how to provide patient education to increase insight about mind-body dichotomy. Disclosures: Ruth Tadesse has nothing to disclose.
Background: Why should we care? • One in three people who come to primary care setting have medically unexplained physical symptoms (MUPS) that have no clear cause. • Somatic symptom disorders and MUPS may lead to: - Functional impairment - High levels of psychological distress - Troubled doctor-patient relationship - Fragmented care - High utilization and cost of health care - Reduced quality of life (Konnopka, 2012).
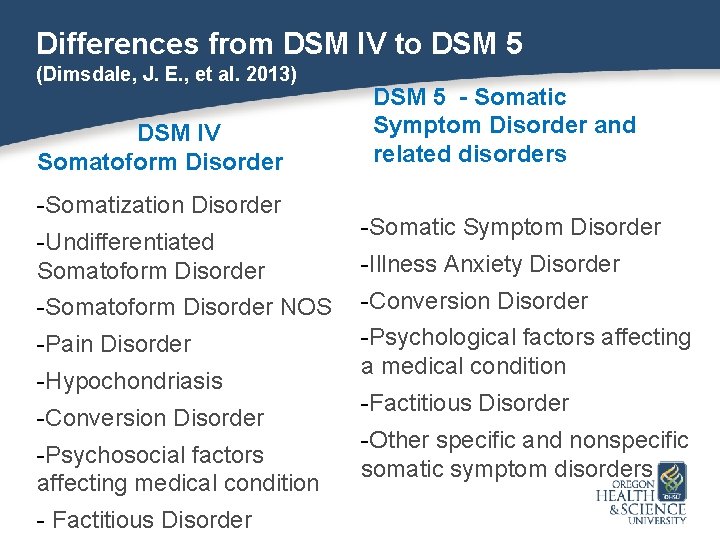
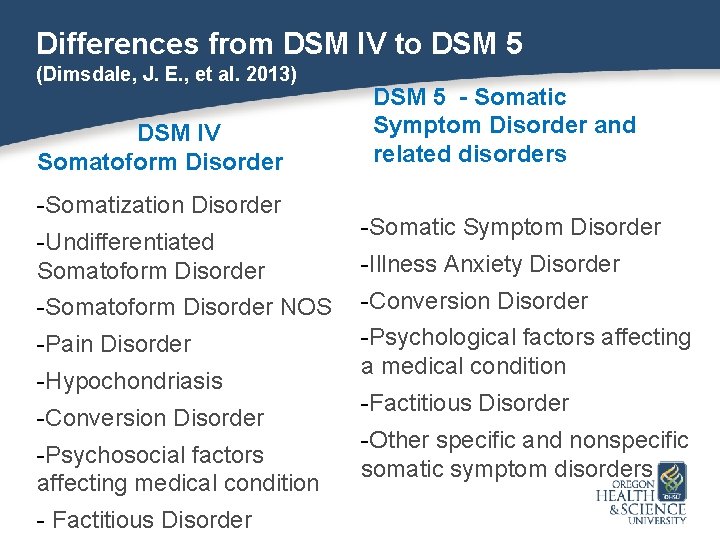
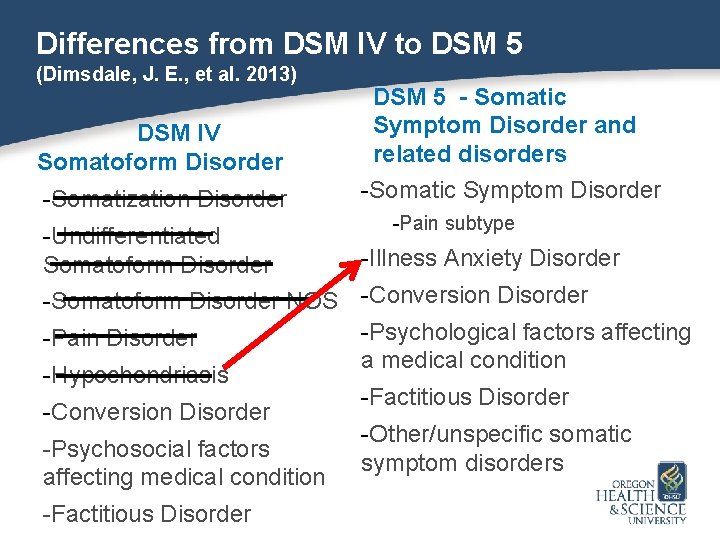
Differences from DSM IV to DSM 5 (Dimsdale, J. E. , et al. 2013) DSM IV Somatoform Disorder -Somatization Disorder -Undifferentiated Somatoform Disorder DSM 5 - Somatic Symptom Disorder and related disorders -Somatic Symptom Disorder -Illness Anxiety Disorder -Somatoform Disorder NOS -Conversion Disorder -Pain Disorder -Psychological factors affecting a medical condition -Hypochondriasis -Conversion Disorder -Psychosocial factors affecting medical condition - Factitious Disorder -Other specific and nonspecific somatic symptom disorders
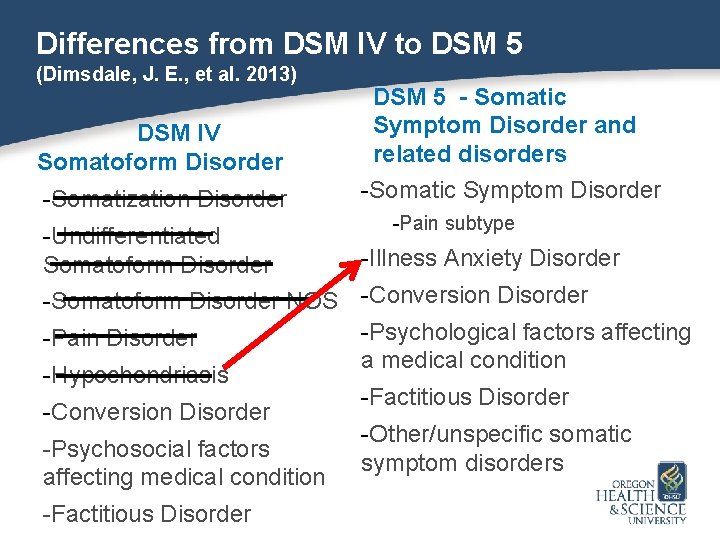
Differences from DSM IV to DSM 5 (Dimsdale, J. E. , et al. 2013) DSM IV Somatoform Disorder DSM 5 - Somatic Symptom Disorder and related disorders -Somatization Disorder -Somatic Symptom Disorder -Undifferentiated Somatoform Disorder -Illness Anxiety Disorder -Pain subtype -Somatoform Disorder NOS -Conversion Disorder -Psychological factors affecting -Pain Disorder a medical condition -Hypochondriasis -Factitious Disorder -Conversion Disorder -Other/unspecific somatic -Psychosocial factors symptom disorders affecting medical condition -Factitious Disorder

From negative to positive symptoms - DSM-IV – defines symptoms negatively – by absence of core features Medically unexplained conditions - DSM-5 – defines symptoms positively – by presence of core features The symptoms may or may not be medically unexplained. http: //www. dsm 5. org/documents/somatic%20 symptom%20 disorder%20 fact%20 sheet. pdf Somatic Symptom Disorder Fact Sheet. pdf
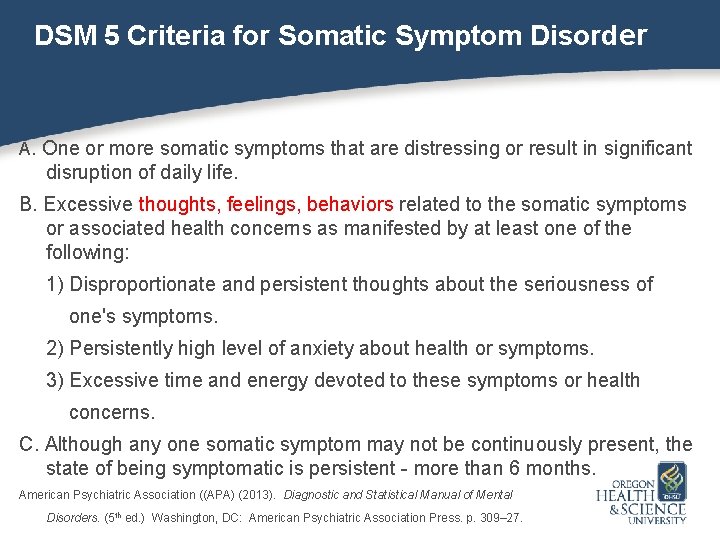
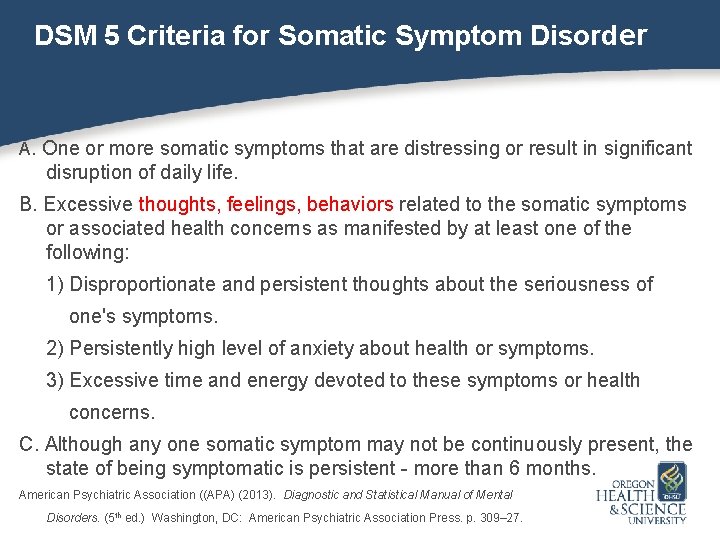
DSM 5 Criteria for Somatic Symptom Disorder A. One or more somatic symptoms that are distressing or result in significant disruption of daily life. B. Excessive thoughts, feelings, behaviors related to the somatic symptoms or associated health concerns as manifested by at least one of the following: 1) Disproportionate and persistent thoughts about the seriousness of one's symptoms. 2) Persistently high level of anxiety about health or symptoms. 3) Excessive time and energy devoted to these symptoms or health concerns. C. Although any one somatic symptom may not be continuously present, the state of being symptomatic is persistent - more than 6 months. American Psychiatric Association ((APA) (2013). Diagnostic and Statistical Manual of Mental Disorders. (5 th ed. ) Washington, DC: American Psychiatric Association Press. p. 309– 27.
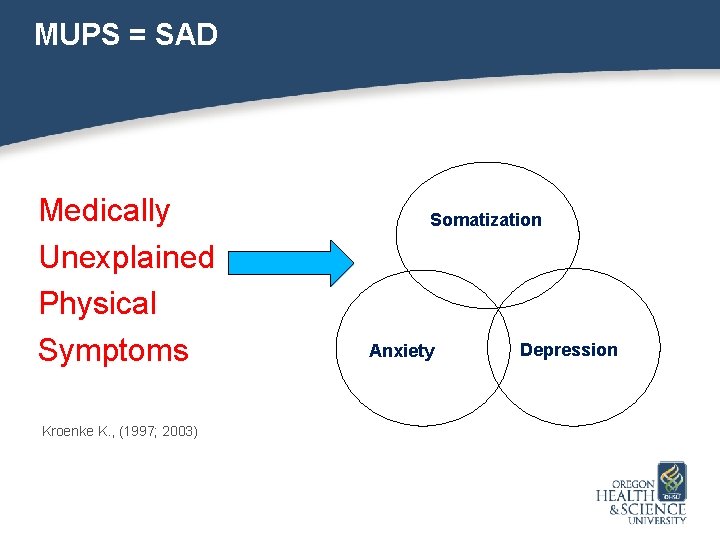
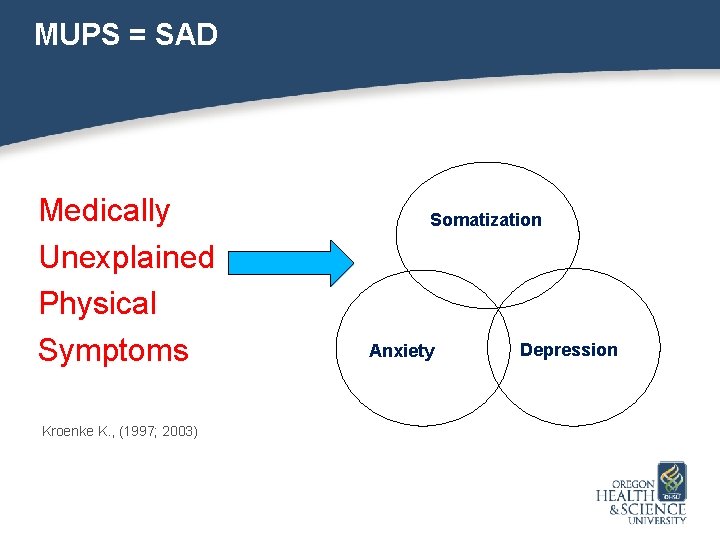
MUPS = SAD Medically Unexplained Physical Symptoms Kroenke K. , (1997; 2003) Somatization Anxiety Depression
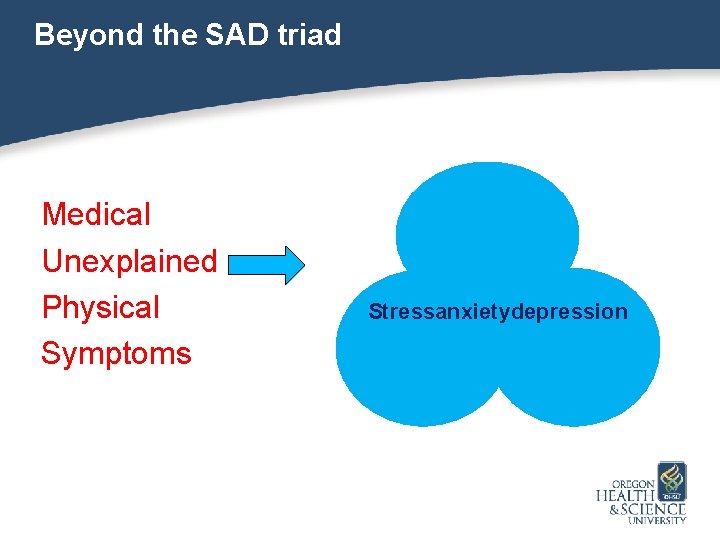
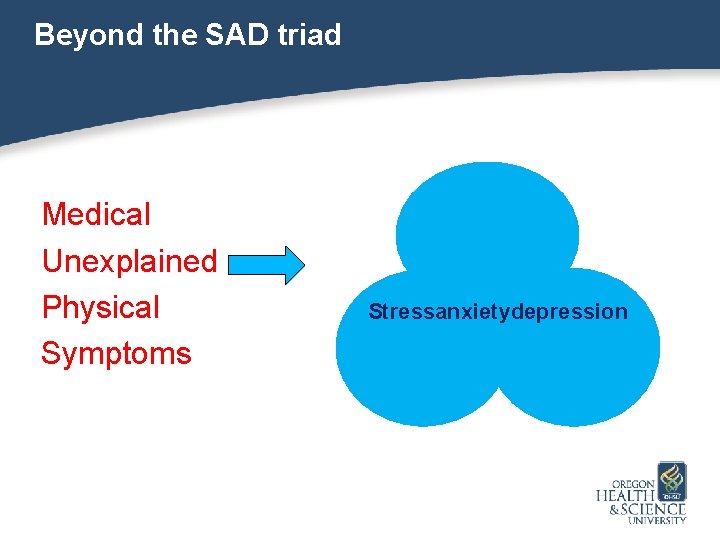
Beyond the SAD triad Medical Unexplained Physical Symptoms Stressanxietydepression
Somatic Symptom Disorder – Essential Features Somatic Symptom Disorder Essential features – Somatic symptom burden Illness Anxiety Disorder Essential features – preoccupation with being ill Conversion Disorder Essential features - functional pattern of sensory-motor symptoms & signs - Still incompatibility with neurologic disorder - Not psychological or presumed trauma

Core Features of Somatic Symptom Disorder - Somatic symptom burden - Total number of symptoms - Continuous number, no threshold Explained vs unexplained doesn’t matter - Distress and impairment - Associated with several adverse outcomes - Disability Increased health care utilization http: //medprofvideos. mayoclinic. org/videos/somatic-symptom-disorders-part-ii-corefeatures-and-treatment

Identifying Somatic Symptom Disorder (Croicu C, et al. 2014) • Do a thorough history and detailed physical assessment • Rule out medical illness • Consider medication side effects • Identify ability to meet basic needs • Identify secondary gains • Identify ability to communicate emotional needs • Determine substance use • Build therapeutic alliance with the patient • Use screening tools appropriate for somatic symptom disorder: SSS-8 and PHQ-15 Approach to the patient with multiple somatic symptoms. pdf
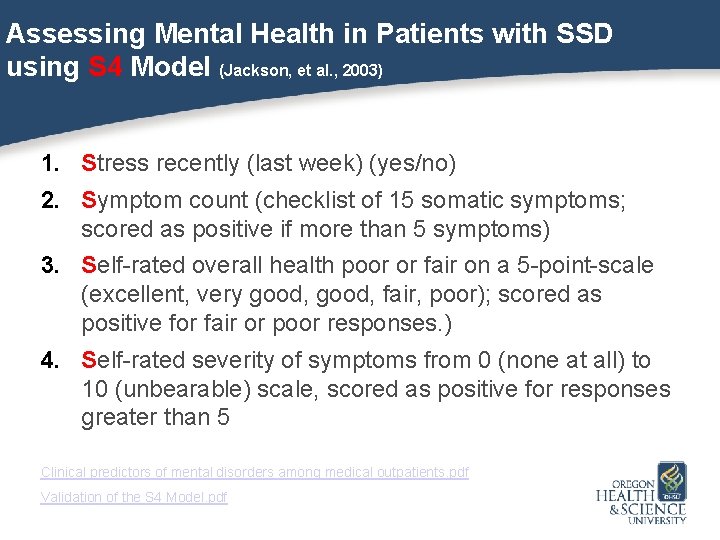
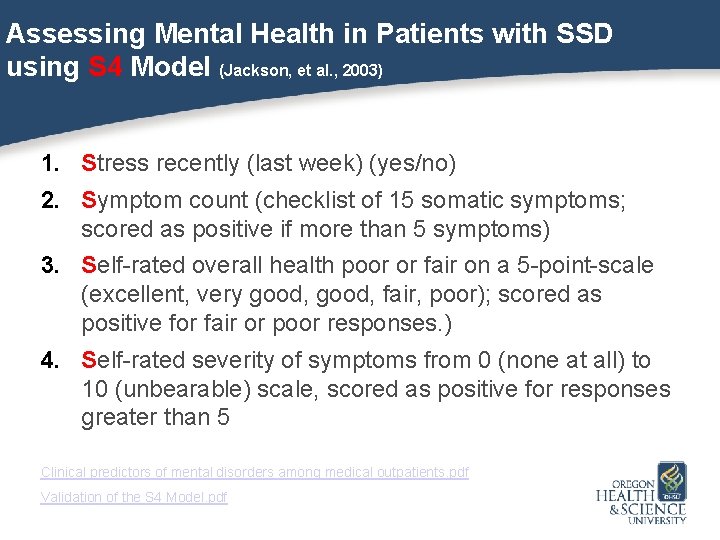
Assessing Mental Health in Patients with SSD using S 4 Model (Jackson, et al. , 2003) 1. Stress recently (last week) (yes/no) 2. Symptom count (checklist of 15 somatic symptoms; scored as positive if more than 5 symptoms) 3. Self-rated overall health poor or fair on a 5 -point-scale (excellent, very good, fair, poor); scored as positive for fair or poor responses. ) 4. Self-rated severity of symptoms from 0 (none at all) to 10 (unbearable) scale, scored as positive for responses greater than 5 Clinical predictors of mental disorders among medical outpatients. pdf Validation of the S 4 Model. pdf
Treatment for Somatic Symptom Disorder
Treatment for Somatic Symptom Disorder Specific DX=Specific Intervention=Better Outcome Review of 34 Controlled Trials; Variable Size and Quality -** Identifying and diagnosing somatic symptom disorder makes a difference - CBT – decreases symptoms and disability - Antidepressants – TCA/SNRIs - greater than SSRIs (Stabb, 2014)
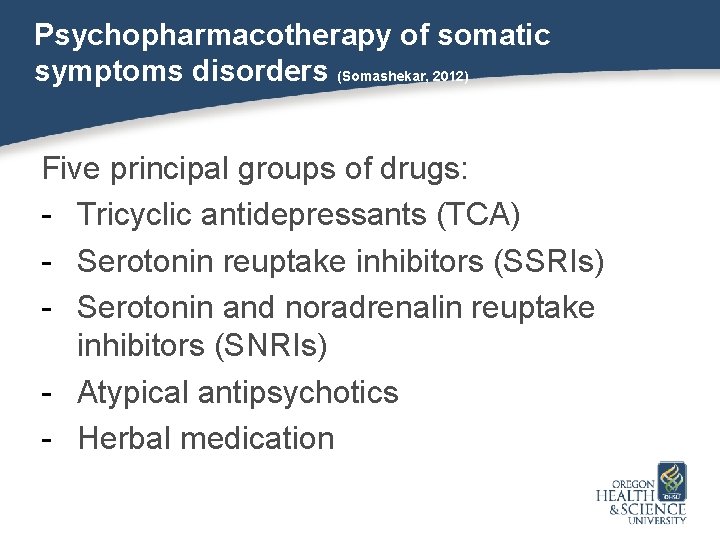
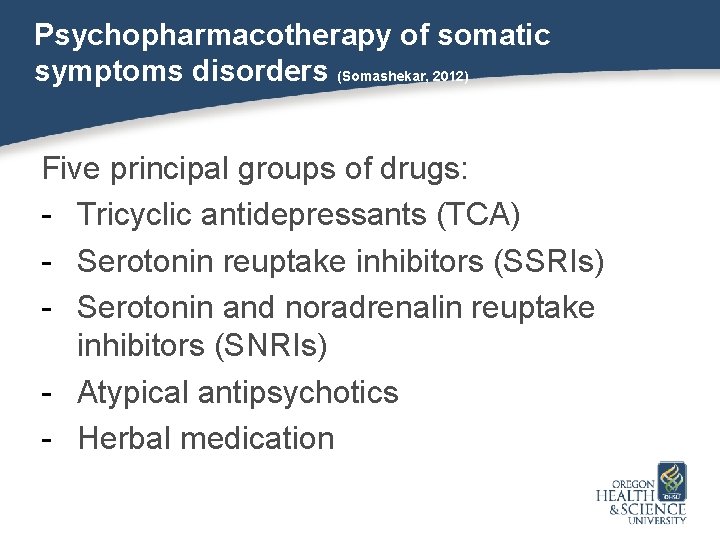
Psychopharmacotherapy of somatic symptoms disorders (Somashekar, 2012) Five principal groups of drugs: - Tricyclic antidepressants (TCA) - Serotonin reuptake inhibitors (SSRIs) - Serotonin and noradrenalin reuptake inhibitors (SNRIs) - Atypical antipsychotics - Herbal medication
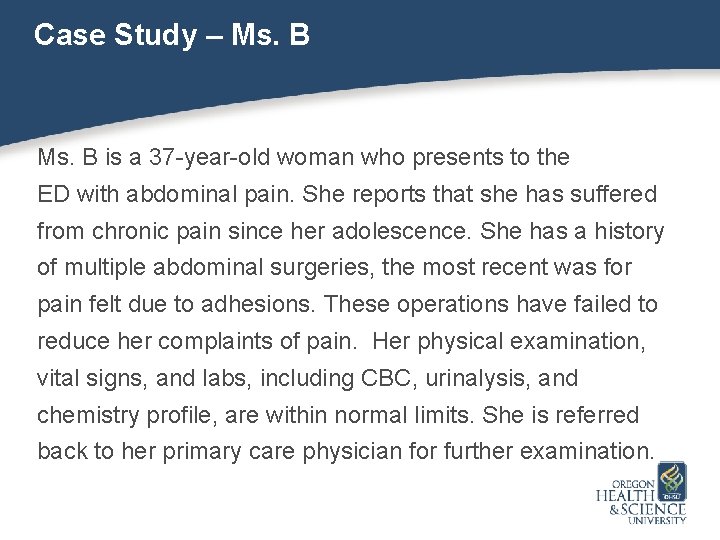
Case Study – Ms. B is a 37 -year-old woman who presents to the ED with abdominal pain. She reports that she has suffered from chronic pain since her adolescence. She has a history of multiple abdominal surgeries, the most recent was for pain felt due to adhesions. These operations have failed to reduce her complaints of pain. Her physical examination, vital signs, and labs, including CBC, urinalysis, and chemistry profile, are within normal limits. She is referred back to her primary care physician for further examination.
Case Study – Ms. B • If you are her PCP, what more would you like to know? • What additional tests/screenings would you like to do? • What will you include under your differential diagnosis? • What do you think her full mental status examination would look like? • What will you prescribe to treat Ms. B’s chronic pain?
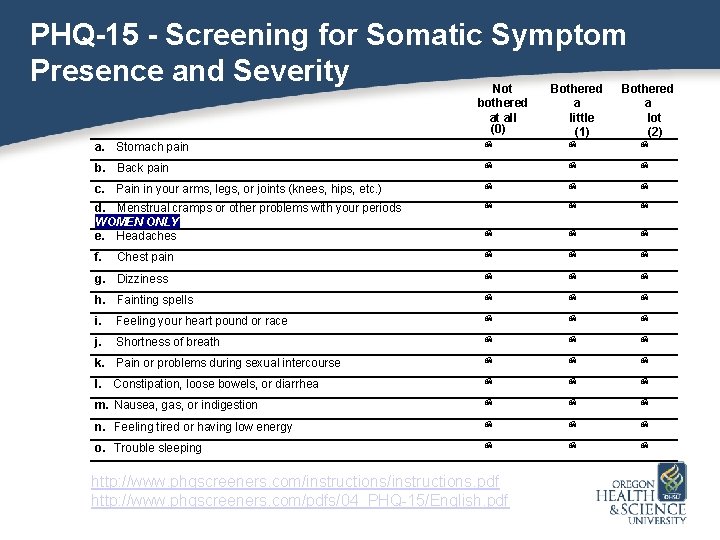
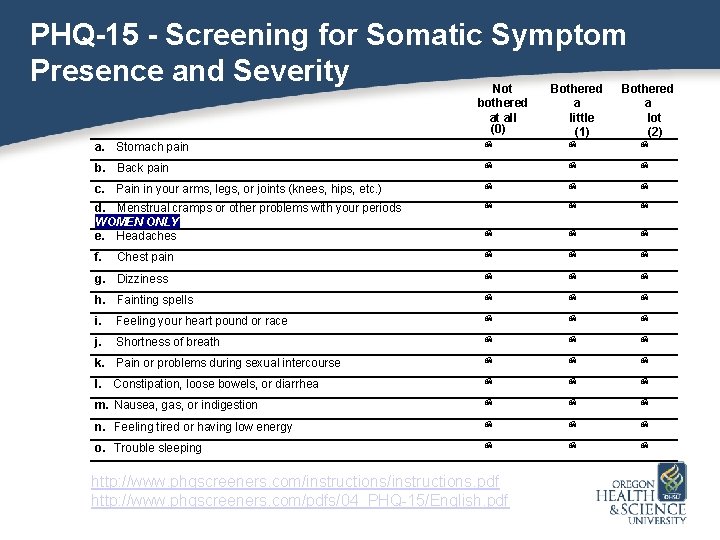
PHQ-15 - Screening for Somatic Symptom Presence and Severity Not bothered at all (0) Bothered a little (1) Bothered a lot (2) a. Stomach pain b. Back pain c. Pain in your arms, legs, or joints (knees, hips, etc. ) d. Menstrual cramps or other problems with your periods WOMEN ONLY e. Headaches f. g. Dizziness h. Fainting spells i. Feeling your heart pound or race j. Shortness of breath k. Pain or problems during sexual intercourse l. Constipation, loose bowels, or diarrhea m. Nausea, gas, or indigestion n. Feeling tired or having low energy o. Trouble sleeping Chest pain http: //www. phqscreeners. com/instructions. pdf http: //www. phqscreeners. com/pdfs/04_PHQ-15/English. pdf
![Somatic Symptom Scale 8 SSS8 Table is hyperlinked Somatic Symptom Scale – 8 [SSS-8] (Table is hyperlinked)](https://slidetodoc.com/presentation_image_h2/a151397dc1a5b712939e02f673783d5e/image-20.jpg)
Somatic Symptom Scale – 8 [SSS-8] (Table is hyperlinked)

Essential Treatment Approaches for Patients with Somatic Symptom Disorder (Croicu, C. , et al. 2014) • Schedule time-limited regular appointments (e. g. 4 -6 weeks) to address complaints • Explain that although there may not be a reason for their symptoms, you will work together to improve their functioning as much as possible • Educate patients how psychosocial stressors and symptoms interact • Avoid comments like “Your symptoms are all psychological. ” or “There is nothing wrong with you medically. ” Approach to the patient with multiple somatic symptoms. pdf

Essential Treatment Approaches for Patients with Somatic Symptom Disorder (Croicu, C. , et al. 2014) • Avoid the temptation to order unnecessary, repetitive, or invasive investigations • Educate the patient on how to cope with their symptoms instead of focusing on a cure • Evaluate somatic symptom burden • Collaborate with the patient in setting treatment goals • Screen for common psychiatric conditions associated with somatic complaints such as depression and anxiety • Treat identified comorbid psychiatric disorders Approach to the patient with multiple somatic symptoms. pdf
Summary • Scheduling a regular visit with the patient reduces or eliminates unnecessary ED visits. • Identifying risks such as childhood trauma can suggest screening for somatic symptom disorders using appropriate assessment tools (PHQ-15 & SSS-8). • Identifying, screening for and treating common psychiatric comorbidities such as depression (PHQ-9) and anxiety (GAD-7) can decrease somatic symptom burden. • Non-pharmacological interventions such as CBT has shown evidence in decreasing somatic symptom disorder. • Therapeutic alliance with the patient with somatic complaints improves outcomes.
References American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. 5 th edition. American Psychiatric Association Press. Croicu, C. , Chwastiak, L. , & Katon, W. (2014). Approach to the patient with multiple somatic symptoms. Medical Clinics of North America. 98(5): 1079 -1095. Dimsdale, J. E. , Creed F. , Escobar, J. , …Levenson, J. (2013). Somatic symptom disorder: An important change in DSM. Journal of Pscyhosomatic Research. 75(3): 223 -228. DSM V Somatic Symptom Disorder Fact Sheet available online http: //www. dsm 5. org/documents/somatic%20 symptom%20 disorder%20 fact%20 sheet. pdf Glerk, B. , Kohlmann, S. , Kroenke, K. , …Lowe, B. (2014). The Somatic Symptom Scale-8 (SSS 8). A Brief Measure of somatic symptom burden. JAMA Internal Medicine. 174(3): 399 -407. Gierk, B. , Kohlmann, S. , Toussaint, A. …Lowe, B. (2014). Assessing somatic symptom burden. A psychometric comparison of the Patient Health Questionnaire – 15 (PHQ-15) and the Somatic Symptom Scale- 8(SSS-8)
References Cont. Jackson, J. L. , O’Malley, P. , & Kroenke, K. (1998). Clinical Predictors of Mental Disorders Among Medical Outpatients: Validation of the S 4 Model. The Journal of Consultation and Liaison Psychiatry. 39(5): 431– 436. Kroenke K. , (2003). Patients presenting with somatic complaints epidemiology, psychiatric comorbidity and management. International journal of methods in psychiatric research. 12(1): 34 -43 Kroenke, K. , Jackson, J. L. , & Chamberlin, J. (1997). Depressive and anxiety disorders in patients presenting with physical complaints. The American Journal of Medicine. 103(5): 339– 347. Martin, A. , Rauh, E. , Fichter, M. , & Rief, W. (2007). A One-session treatment for patients suffering from medically unexplained symptoms in primary care: A randomized clinical trial. Psychosomatics. 48(4): 294 -303. Ravesteign, H. , Wittkampf, K. , Lucassen, P. , …, Weel, C. (2009). Detecting somatoform disorders in primary care with the PHQ-15. Annals of Family Medicine. 7: 232 -238. Van Dessel, N. , den Boeft, van der Wouden, J. C. …van Marwijk, H. (2014). Nonpharmacological interventions for somatoform disorders and medically unexplained physical symptoms (MUPS) in adults. Cochrane Database Systematic Review. 11(1): Vol. 11, p. CD 011142 -CD 011142
The End! Next Week Topic TBD 05/28/15