Solute Transport across the Peritoneum By diffusion and
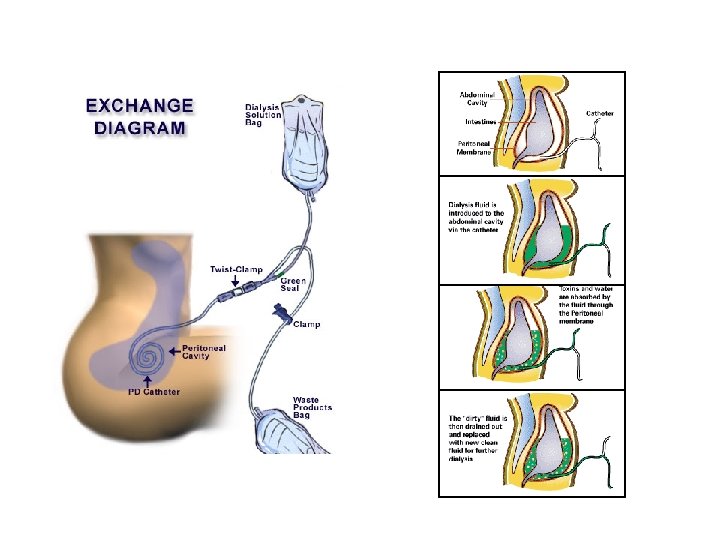
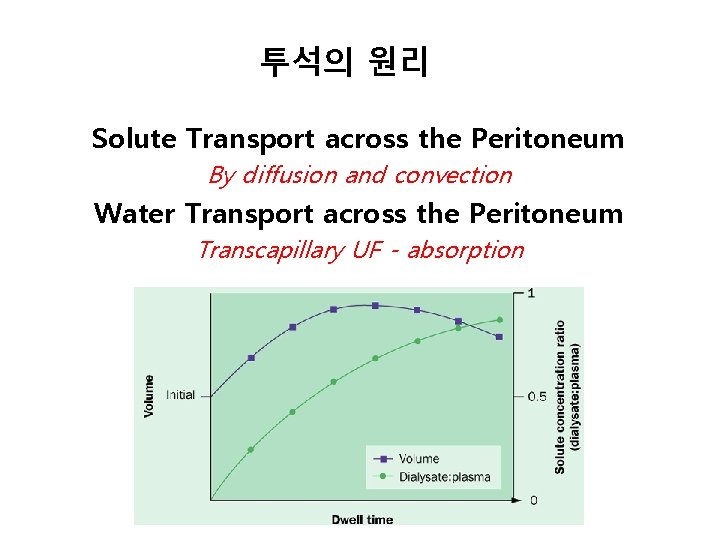
투석의 원리 Solute Transport across the Peritoneum By diffusion and convection Water Transport across the Peritoneum Transcapillary UF - absorption
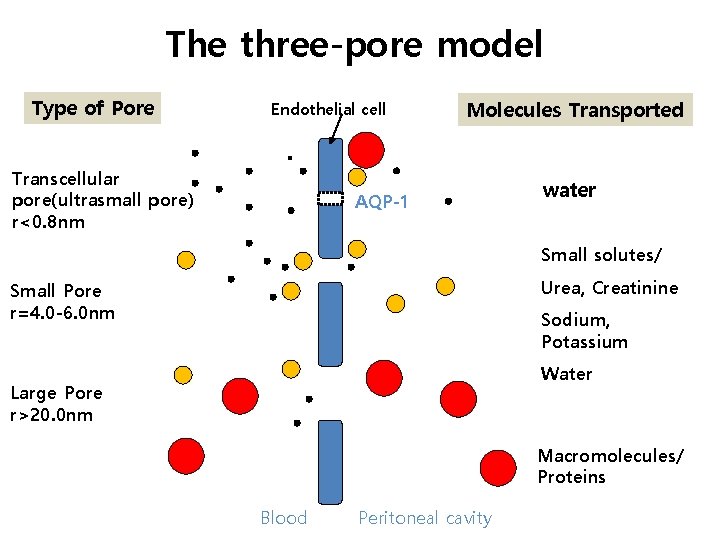
The three-pore model Type of Pore Endothelial cell Transcellular pore(ultrasmall pore) r<0. 8 nm Molecules Transported AQP-1 water Small solutes/ Urea, Creatinine Small Pore r=4. 0 -6. 0 nm Sodium, Potassium Water Large Pore r>20. 0 nm Macromolecules/ Proteins Blood Peritoneal cavity
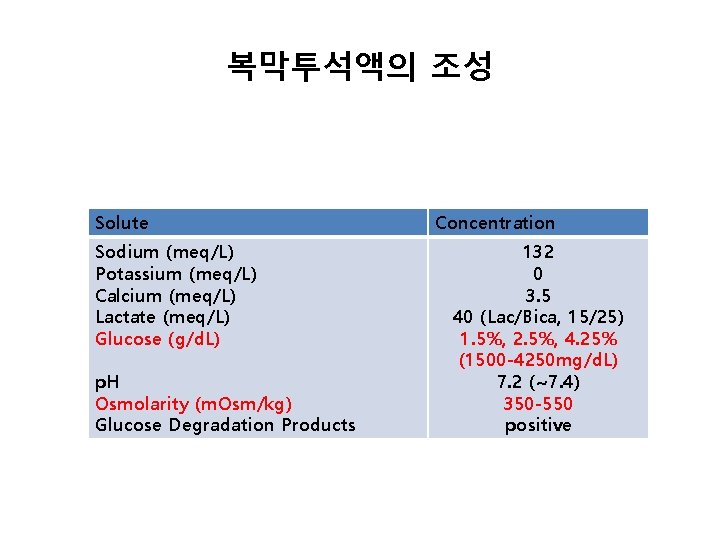
복막투석액의 조성 Solute Sodium (meq/L) Potassium (meq/L) Calcium (meq/L) Lactate (meq/L) Glucose (g/d. L) p. H Osmolarity (m. Osm/kg) Glucose Degradation Products Concentration 132 0 3. 5 40 (Lac/Bica, 15/25) 1. 5%, 2. 5%, 4. 25% (1500 -4250 mg/d. L) 7. 2 (~7. 4) 350 -550 positive
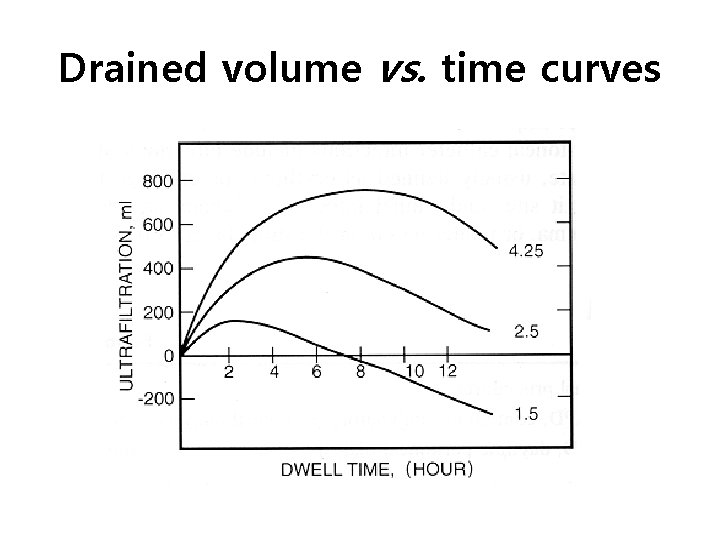
Drained volume vs. time curves
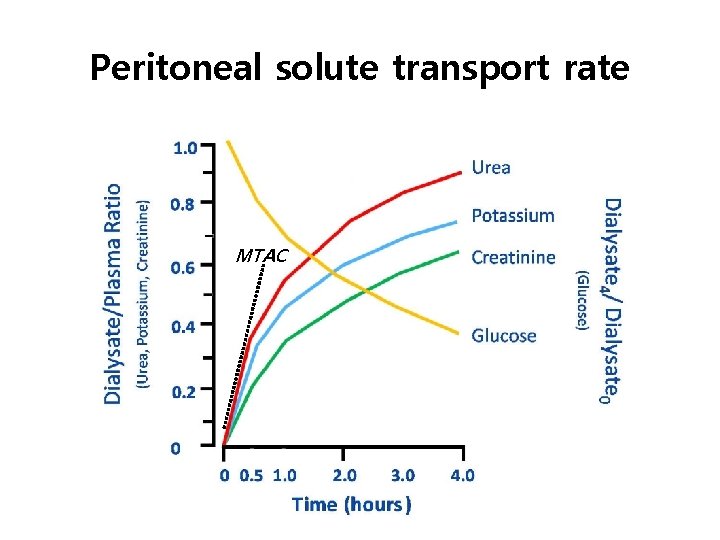
Peritoneal solute transport rate MTAC
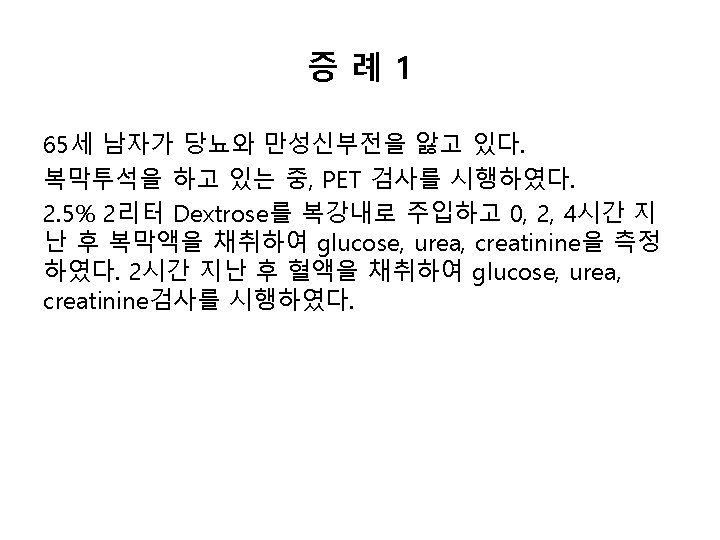
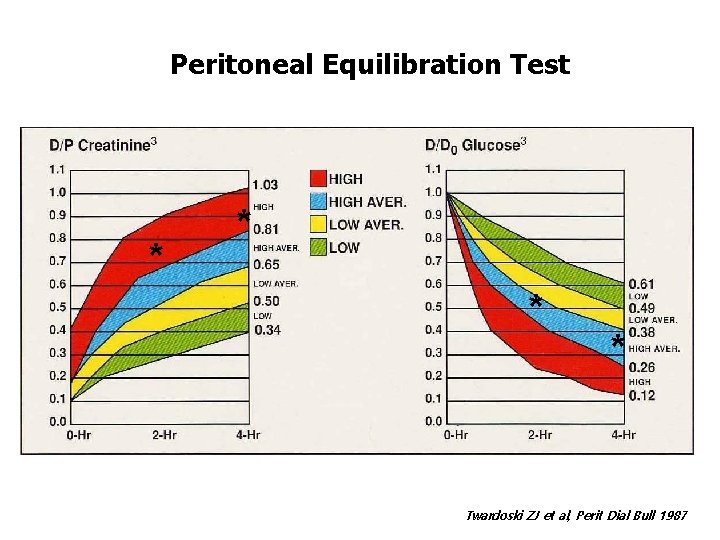
Peritoneal Equilibration Test * * Twardoski ZJ et al, Perit Dial Bull 1987
질문 2 • 앞의 PET 검사에 대한 내용으로 옳은 것을 고르시오. (1) (2) (3) (4) (5) Low transporter type 이다. High transporter type 이다. Low clearance type 이다. High clearance type 이다. 모두 다 정답이 아니다.
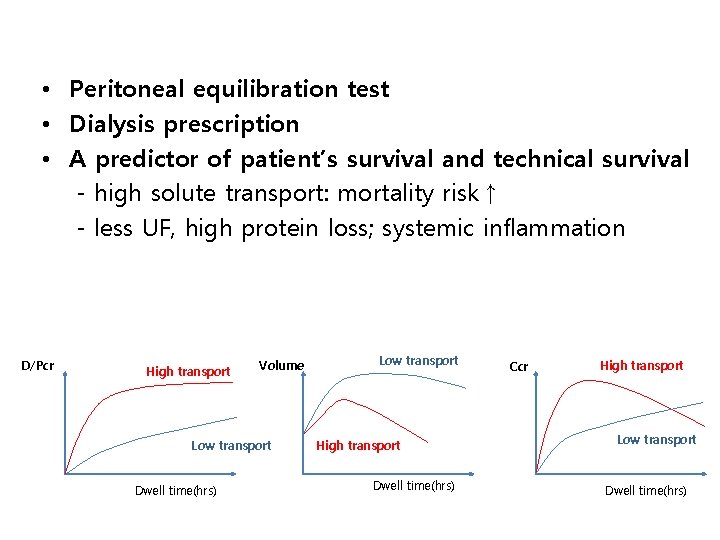
• Peritoneal equilibration test • Dialysis prescription • A predictor of patient’s survival and technical survival - high solute transport: mortality risk↑ - less UF, high protein loss; systemic inflammation D/Pcr High transport Volume Low transport Dwell time(hrs) Low transport High transport Dwell time(hrs) Ccr High transport Low transport Dwell time(hrs)
수분제거 Ultrafltration failure; 3ⅹ 4 rules (UFV< 400 ml after a dwell of 4 -h with 3. 86/4. 25%) • • Rapid solute transport Slow solute transport High peritoneal reabsorption Decreased free water transport(aquaporin failure)
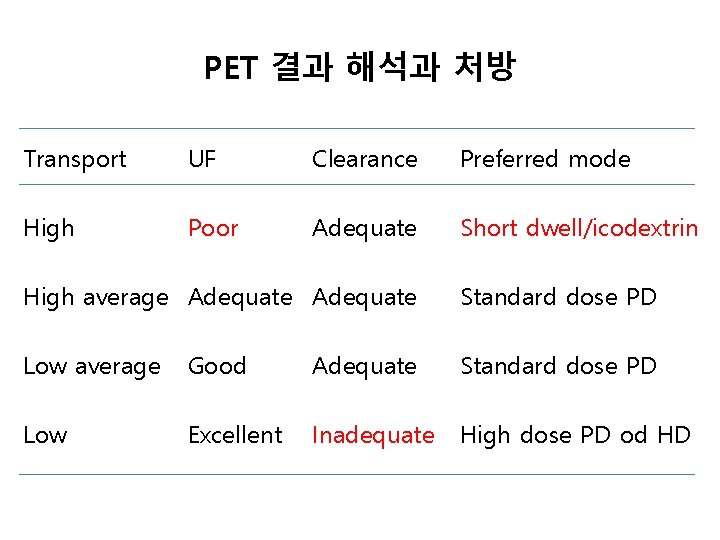
PET 결과 해석과 처방 Transport UF Clearance Preferred mode High Poor Adequate Short dwell/icodextrin High average Adequate Standard dose PD Low average Good Adequate Standard dose PD Low Excellent Inadequate High dose PD od HD
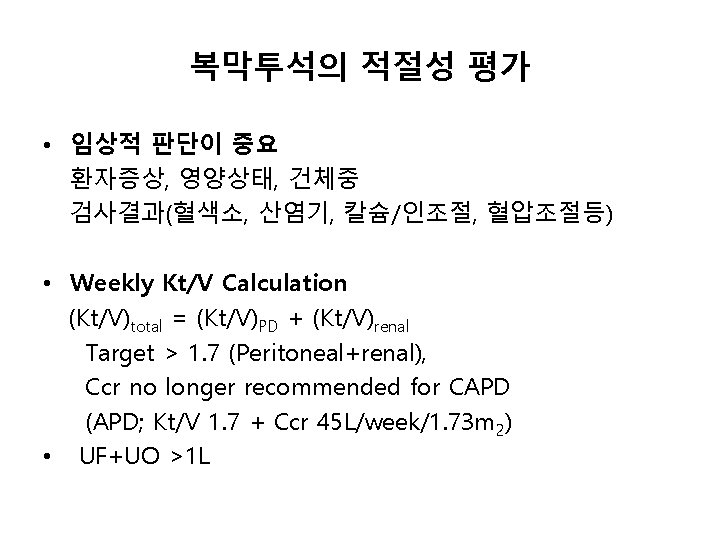
복막투석의 적절성 평가 • 임상적 판단이 중요 환자증상, 영양상태, 건체중 검사결과(혈색소, 산염기, 칼슘/인조절, 혈압조절등) • Weekly Kt/V Calculation (Kt/V)total = (Kt/V)PD + (Kt/V)renal Target > 1. 7 (Peritoneal+renal), Ccr no longer recommended for CAPD (APD; Kt/V 1. 7 + Ccr 45 L/week/1. 73 m 2) • UF+UO >1 L
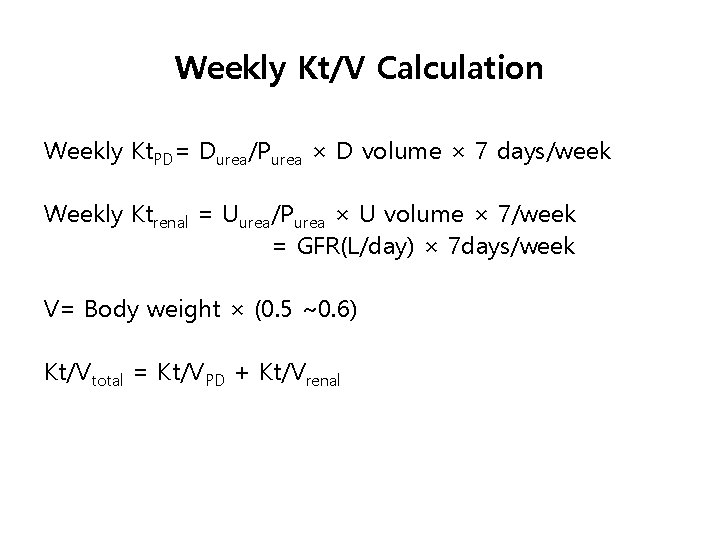
Weekly Kt/V Calculation Weekly Kt. PD= Durea/Purea × D volume × 7 days/week Weekly Ktrenal = Uurea/Purea × U volume × 7/week = GFR(L/day) × 7 days/week V= Body weight × (0. 5 ~0. 6) Kt/Vtotal = Kt/VPD + Kt/Vrenal
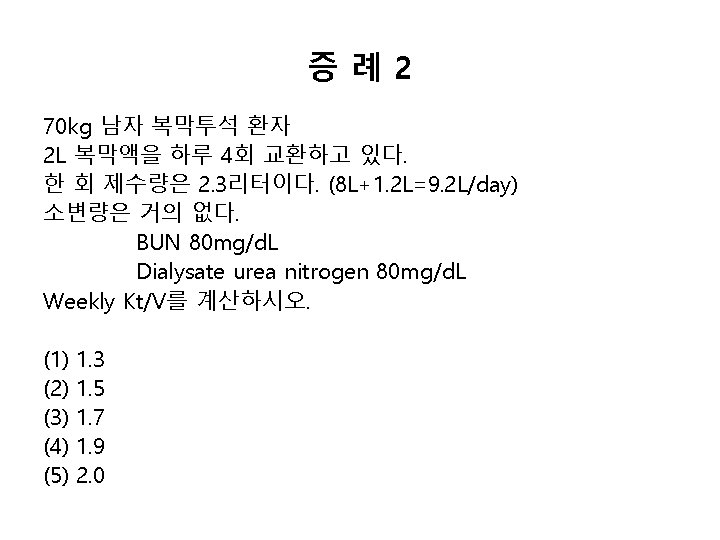
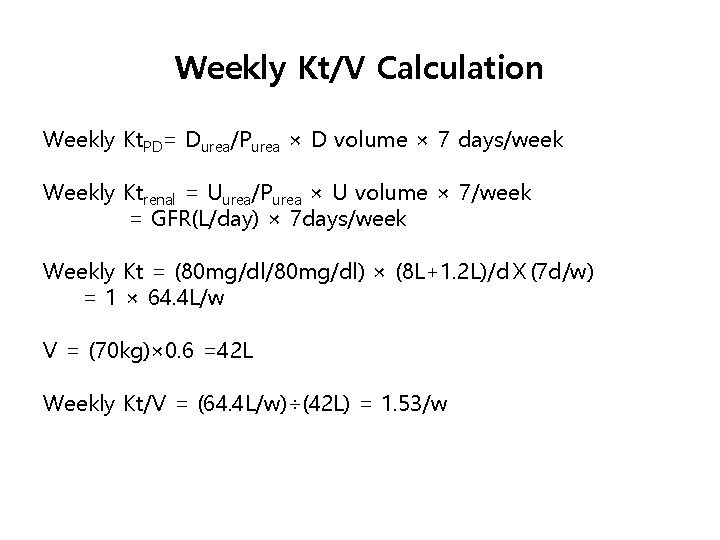
Weekly Kt/V Calculation Weekly Kt. PD= Durea/Purea × D volume × 7 days/week Weekly Ktrenal = Uurea/Purea × U volume × 7/week = GFR(L/day) × 7 days/week Weekly Kt = (80 mg/dl/80 mg/dl) × (8 L+1. 2 L)/dⅩ(7 d/w) = 1 × 64. 4 L/w V = (70 kg)× 0. 6 =42 L Weekly Kt/V = (64. 4 L/w)÷(42 L) = 1. 53/w
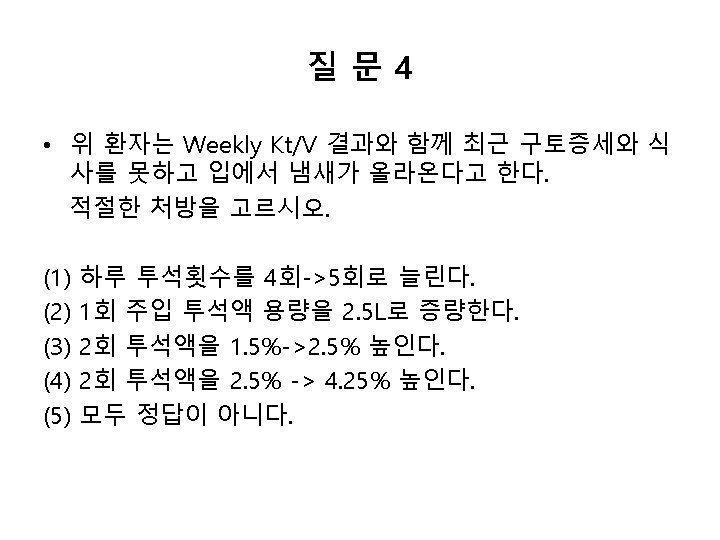
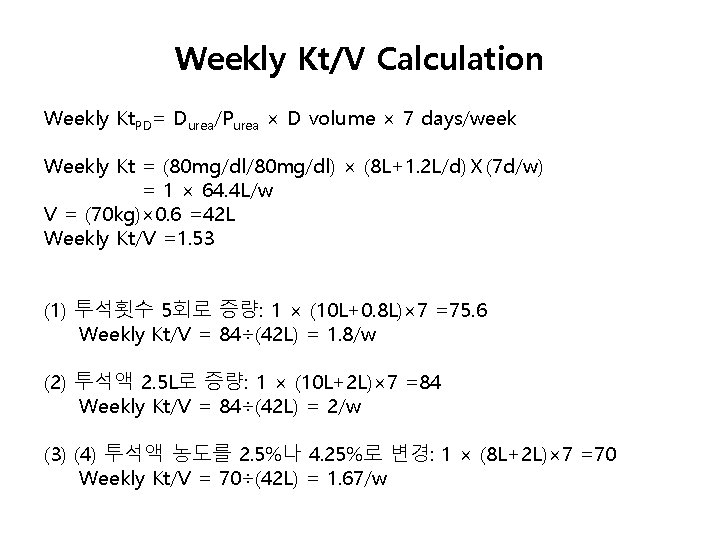
Weekly Kt/V Calculation Weekly Kt. PD= Durea/Purea × D volume × 7 days/week Weekly Kt = (80 mg/dl/80 mg/dl) × (8 L+1. 2 L/d)Ⅹ(7 d/w) = 1 × 64. 4 L/w V = (70 kg)× 0. 6 =42 L Weekly Kt/V =1. 53 (1) 투석횟수 5회로 증량: 1 × (10 L+0. 8 L)× 7 =75. 6 Weekly Kt/V = 84÷(42 L) = 1. 8/w (2) 투석액 2. 5 L로 증량: 1 × (10 L+2 L)× 7 =84 Weekly Kt/V = 84÷(42 L) = 2/w (3) (4) 투석액 농도를 2. 5%나 4. 25%로 변경: 1 × (8 L+2 L)× 7 =70 Weekly Kt/V = 70÷(42 L) = 1. 67/w
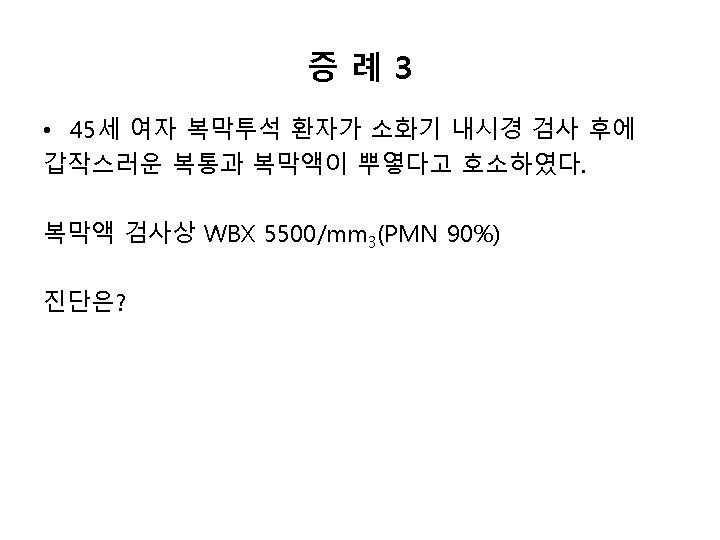
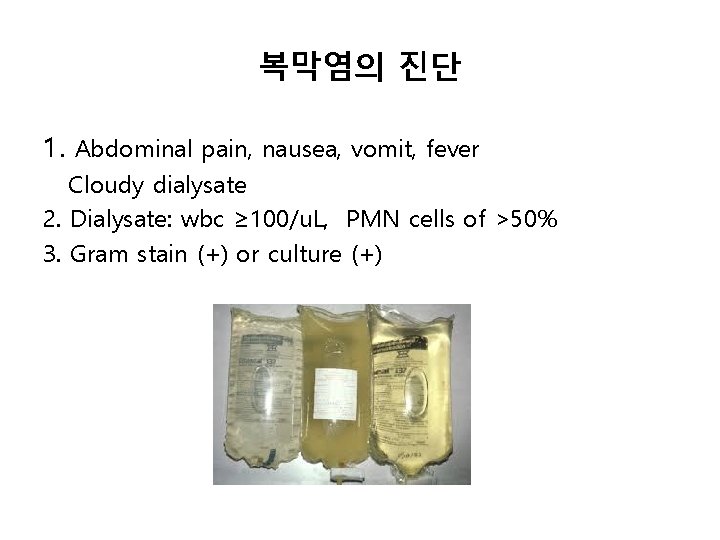
복막염의 진단 1. Abdominal pain, nausea, vomit, fever Cloudy dialysate 2. Dialysate: wbc ≥ 100/u. L, PMN cells of >50% 3. Gram stain (+) or culture (+)
질문 5 • 위 복막투석 환자는 하루 소변량은 거의 없다. 균배양 검 사 결과 보고 이전 경험적으로 사용할 수 있는 항생제를 고르시오 (1) (2) (3) (4) (5) cefazolin + quinolone cefazolin + aminoglycoside cefazolin + ceftazidime vancomycin +quinolone vancomycin +aminoglycoside
Diagnosis of EPS • Clinical symptoms Repeatedly and/or progressive bowel obstruction ( pain, vomiting, distension) • Exclude other possible causes of obstruction • Image findings; Abdominal CT • Surgical findings, Laparoscopy • Histology
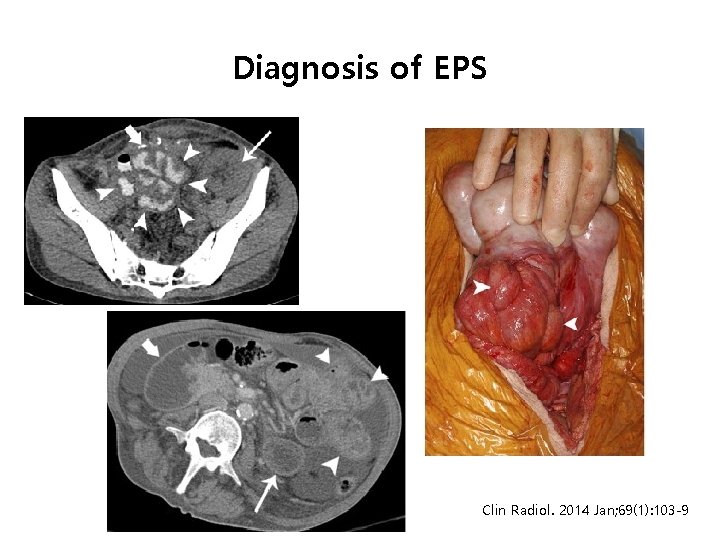
Diagnosis of EPS Clin Radiol. 2014 Jan; 69(1): 103 -9
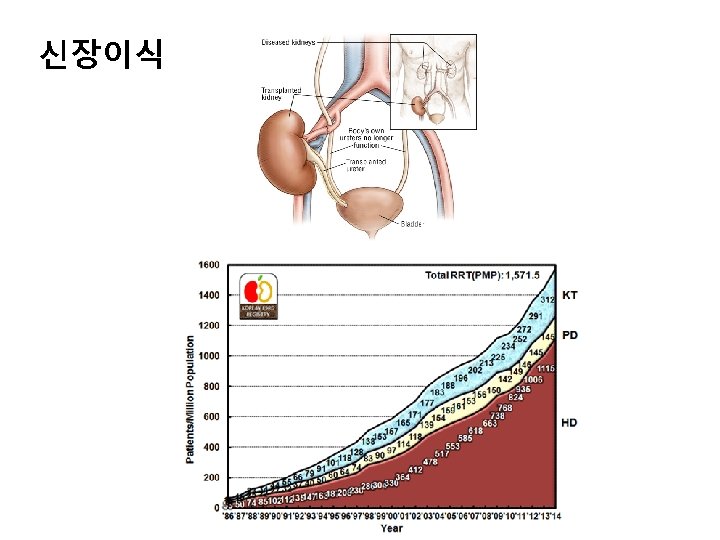
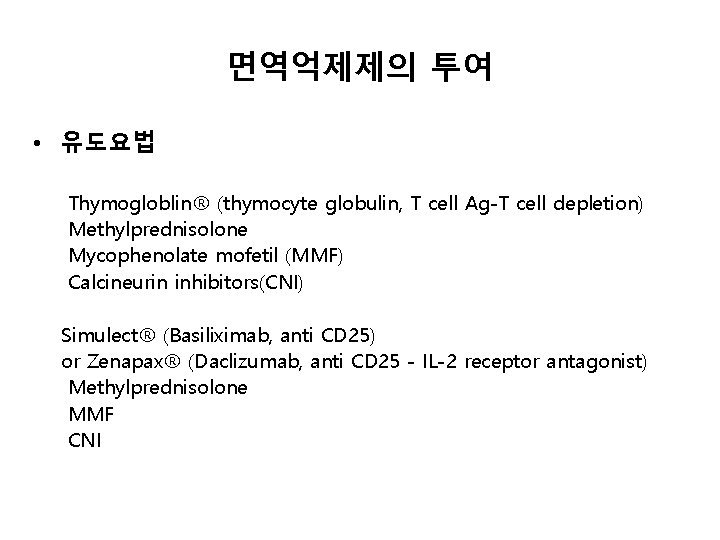
면역억제제의 투여 • 유도요법 Thymogloblin® (thymocyte globulin, T cell Ag-T cell depletion) Methylprednisolone Mycophenolate mofetil (MMF) Calcineurin inhibitors(CNI) Simulect® (Basiliximab, anti CD 25) or Zenapax® (Daclizumab, anti CD 25 - IL-2 receptor antagonist) Methylprednisolone MMF CNI
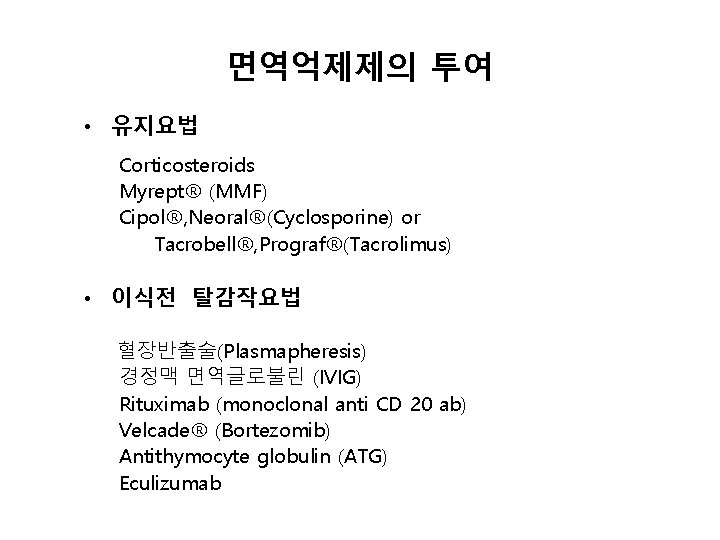
면역억제제의 투여 • 유지요법 Corticosteroids Myrept® (MMF) Cipol®, Neoral®(Cyclosporine) or Tacrobell®, Prograf®(Tacrolimus) • 이식전 탈감작요법 혈장반출술(Plasmapheresis) 경정맥 면역글로불린 (IVIG) Rituximab (monoclonal anti CD 20 ab) Velcade® (Bortezomib) Antithymocyte globulin (ATG) Eculizumab
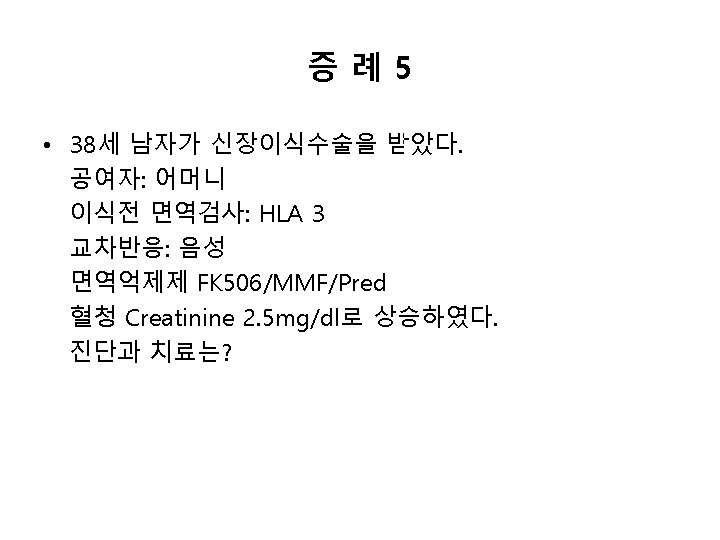
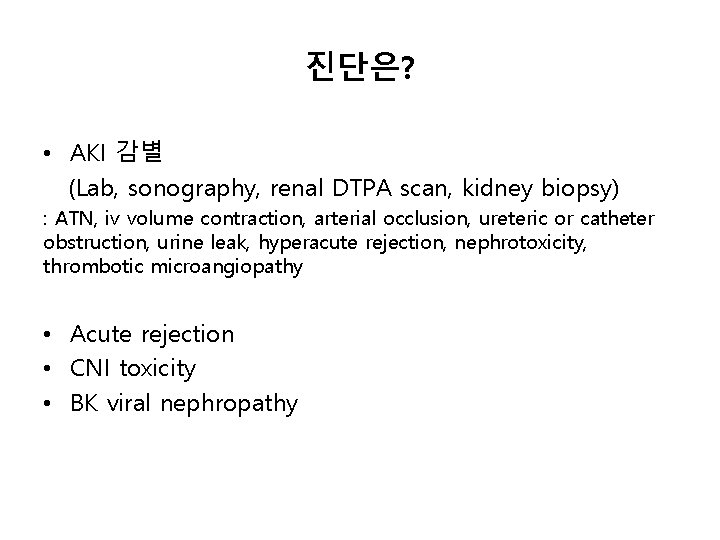
진단은? • AKI 감별 (Lab, sonography, renal DTPA scan, kidney biopsy) : ATN, iv volume contraction, arterial occlusion, ureteric or catheter obstruction, urine leak, hyperacute rejection, nephrotoxicity, thrombotic microangiopathy • Acute rejection • CNI toxicity • BK viral nephropathy
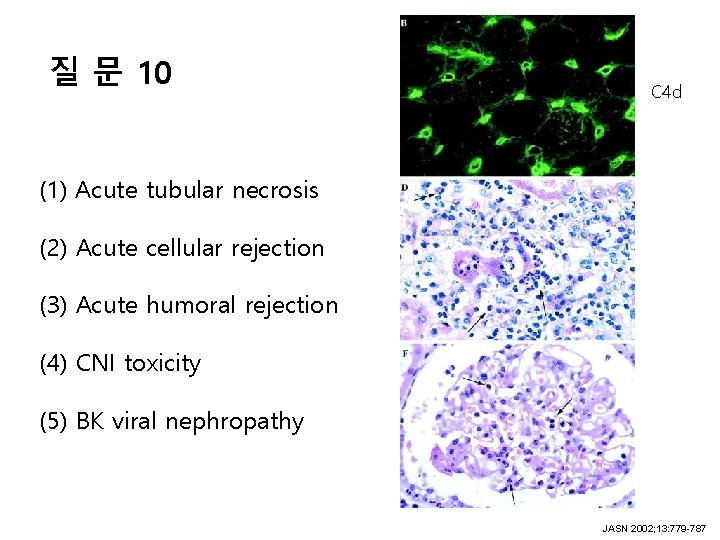
질 문 10 C 4 d (1) Acute tubular necrosis (2) Acute cellular rejection (3) Acute humoral rejection (4) CNI toxicity (5) BK viral nephropathy JASN 2002; 13: 779 -787
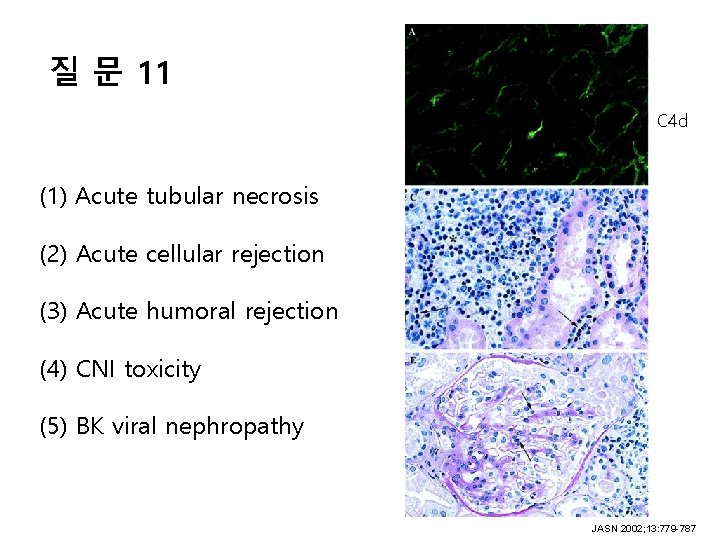
질 문 11 C 4 d (1) Acute tubular necrosis (2) Acute cellular rejection (3) Acute humoral rejection (4) CNI toxicity (5) BK viral nephropathy JASN 2002; 13: 779 -787
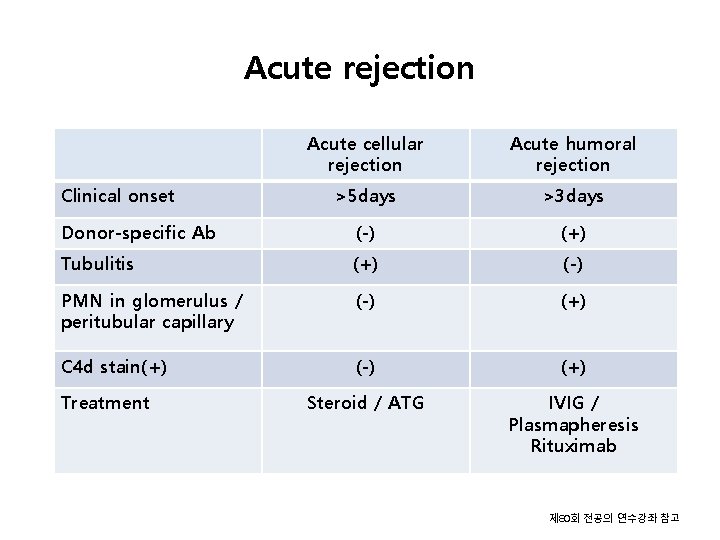
Acute rejection Acute cellular rejection Acute humoral rejection >5 days >3 days Donor-specific Ab (-) (+) Tubulitis (+) (-) PMN in glomerulus / peritubular capillary (-) (+) C 4 d stain(+) (-) (+) Steroid / ATG IVIG / Plasmapheresis Rituximab Clinical onset Treatment 제 80회 전공의 연수강좌 참고
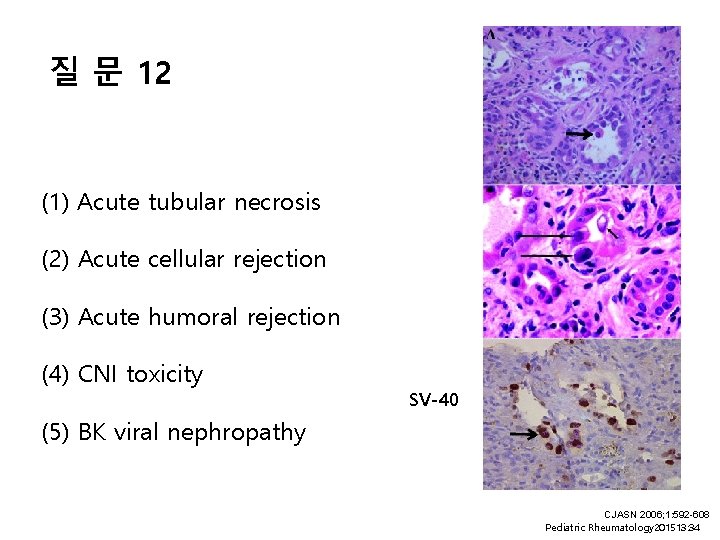
질 문 12 (1) Acute tubular necrosis (2) Acute cellular rejection (3) Acute humoral rejection (4) CNI toxicity SV-40 (5) BK viral nephropathy CJASN 2006; 1: 592 -608 Pediatric Rheumatology 201513: 34
BK virus nephropathy • 신장이식 1년 후 • Tubulointerstitial nephritis, ureteral stricture, hemorrhagic cystisis • Urine cytology; Decoy cell Urine and plasma BKV DNA • 진단: Renal biopsy • 특별한 치료방법이 없다: 면역억제제 감량
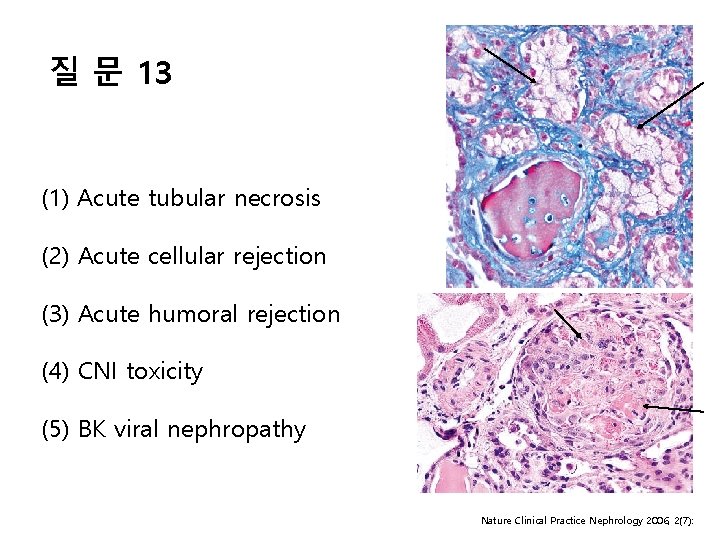
질 문 13 (1) Acute tubular necrosis (2) Acute cellular rejection (3) Acute humoral rejection (4) CNI toxicity (5) BK viral nephropathy Nature Clinical Practice Nephrology 2006, 2(7):
CNI induced nephropathy • Acute nephropathy Toxic tubulopathy Toxic vasculopathy Acute arteriopathy Thrombotic microaniopathy • Chronic nephropathy Hyaline arteriopathy Interstitial fibrosis and tubular atrophy Glomerular changes
- Slides: 50