Soft Tissue Reconstruction Dr Saleh Abualhaj Plastic surgeon
Soft Tissue Reconstruction Dr. Saleh Abualhaj Plastic surgeon
SKIN: Physiology & Function • Epidermis: § protective barrier (against mechanical damage, microbe invasion, & water loss) § high regenerative capacity § Producer of skin appendages (hair, nails, sweat & sebaceous glands)
SKIN: Physiology & Function Dermis: – mechanical strength (collagen & elastin) – Barrier to microbe invasion – Sensation (point, temp, pressure, proprioception) – Thermoregulation (vasomotor activity of blood vessels and sweat gland activity)
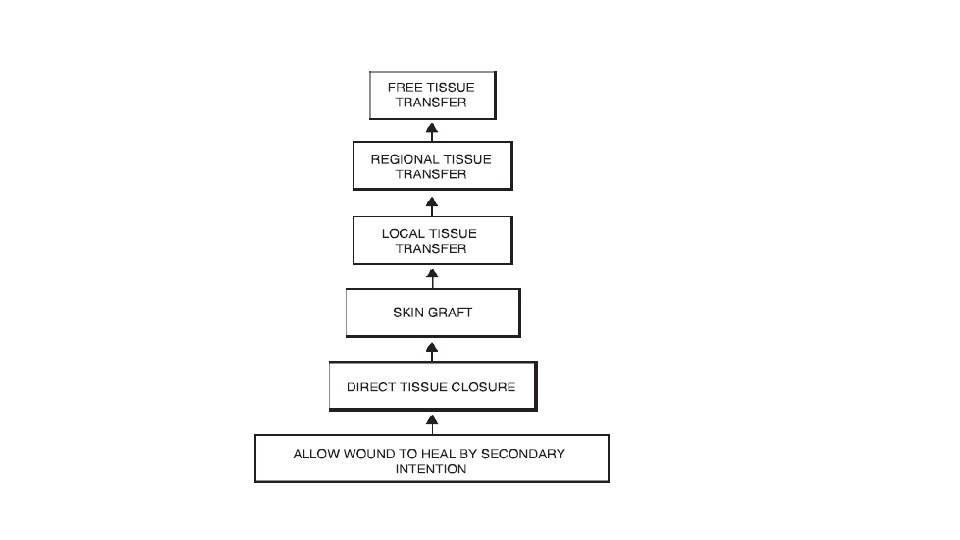
Step 1: Dressings • Adjunct applied to a wound to promote healing and prevent further harm • Allow the wound to heal by secondary intention • Aim – maintain a moist environment without excess exudate
Step 2: Primary (or delayed) closure • Primary closure – appose + secure incised wound edges • Traumatic/dirty wounds – may require debridement + delayed closure
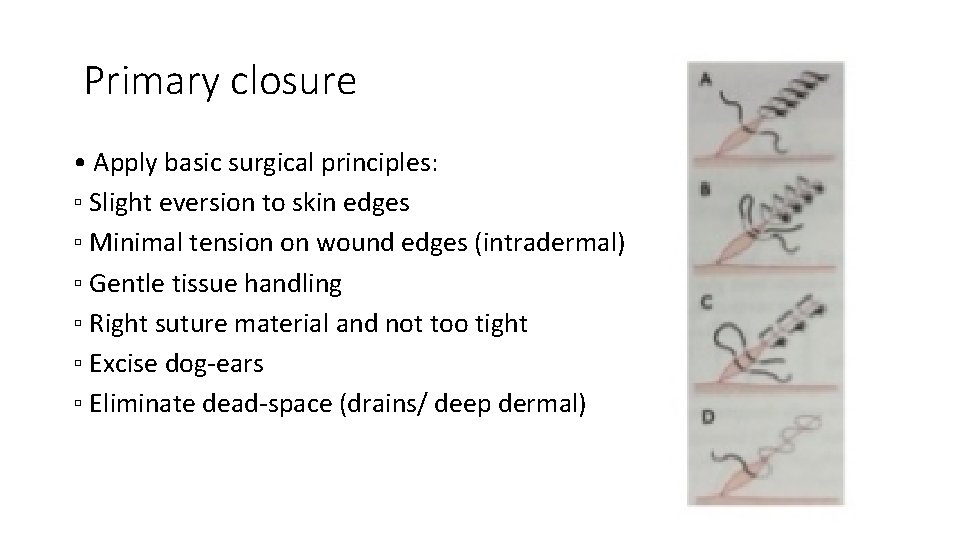
Primary closure • Apply basic surgical principles: ▫ Slight eversion to skin edges ▫ Minimal tension on wound edges (intradermal) ▫ Gentle tissue handling ▫ Right suture material and not too tight ▫ Excise dog-ears ▫ Eliminate dead-space (drains/ deep dermal)
Delayed closure • Indicated when wounds are dirty, contaminated or at high risk of sepsis (e. g. bites) • The first option following debridement • Wounds can be also left to heal by secondary intention
Step 3: Skin grafting • Block of tissue transferred without blood supply • Classified according to tissue of origin: ▫ Autograft ▫ Allograft ▫ Xenograft
Step 3: Skin grafting • Either split-thickness or full-thickness • Graft survival dependent on graft quality AND the graft bed Muscle/fascia (proper) Bare cortical bone/tendon(improper)
Skin graft survival and healing 1. *Imbibition (first 24 to 48 hours): Plasma imbibition (diffusion) responsible for skin graft survival until angiogenesis occurs → thinner grafts more likely to survive. 2. *Inosculation (48 to 72 hours): Process of capillaries joining between skin graft and recipient bed. 3. Revascularization (4 to 7 days): Ingrowth of capillaries into graft
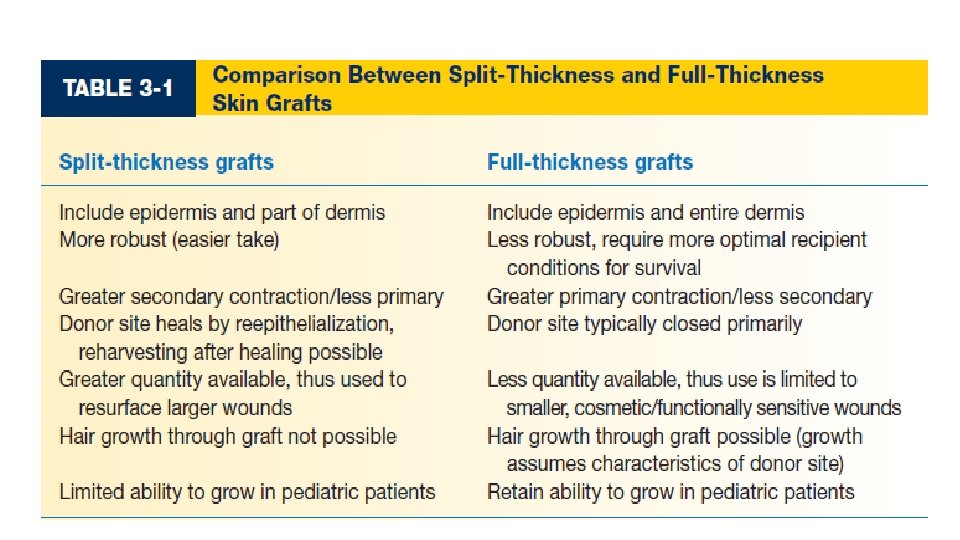
4. Primary contraction a. Occurs at the time of graft harvest/application b. Due to elastin fibers in dermis c. Greater in FTSGs (>40%) compared with STSGs (<20%) 5. Secondary contraction a. Occurs after graft take b. During healing phase of graft over 6 to 18 months c. greater in STSGs d. Dermal components of FTSGs suppress myofibroblast activities responsible for secondary contraction
6. Regeneration of dermal appendages a. More likely to regenerate in thicker grafts b. Sweating assumes characteristics of recipient site when glands are reinnervated c. Sebaceous glands retain characteristics of donor site 7. Reinnervation a. Begins 2 to 4 weeks after grafting b. Process takes several months to years c. Assumes characteristics of recipient site d. Reinnervation incomplete and some degree of decreased sensation will persist e. STSGs regain sensation quicker, but FTSGs regain more complete innervation. f. Pain returns first, then touch, then temperature.
8. Hair growth: Assumes characteristics of donor site, but only has potential to return after FTSGs. 9. Pigmentation a. More predictable in FTSGs b. Permanent hyperpigmentation may result from early sun exposure before full maturation. 10. Growth potential: STSGs have limited ability to grow in pediatric patients, FTSGs have potential to grow.
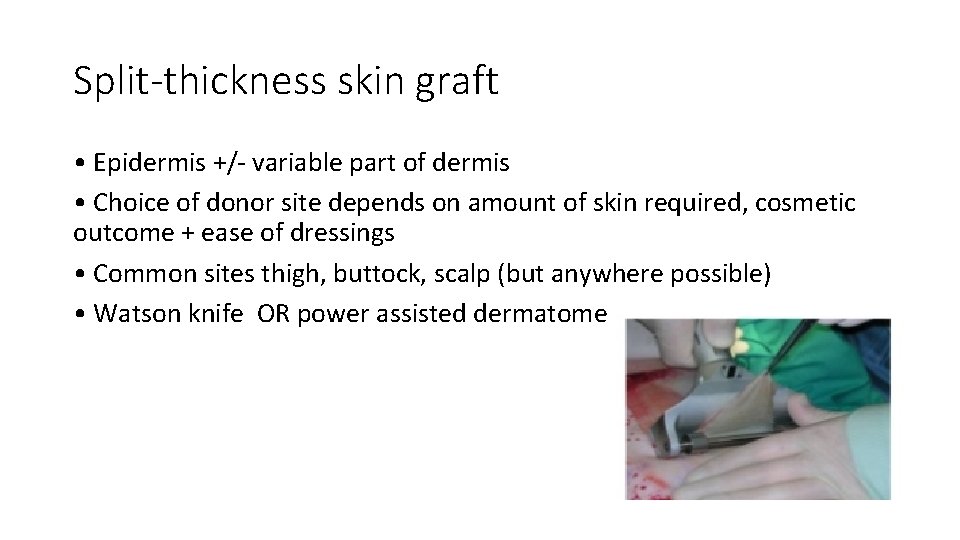
Split-thickness skin graft • Epidermis +/- variable part of dermis • Choice of donor site depends on amount of skin required, cosmetic outcome + ease of dressings • Common sites thigh, buttock, scalp (but anywhere possible) • Watson knife OR power assisted dermatome
Full-thickness graft • Entire epidermis & dermis • Limited in size – leave defect with no healing potential • Donor site needs direct closure or SSG • Chose donor site for good colour and texture match
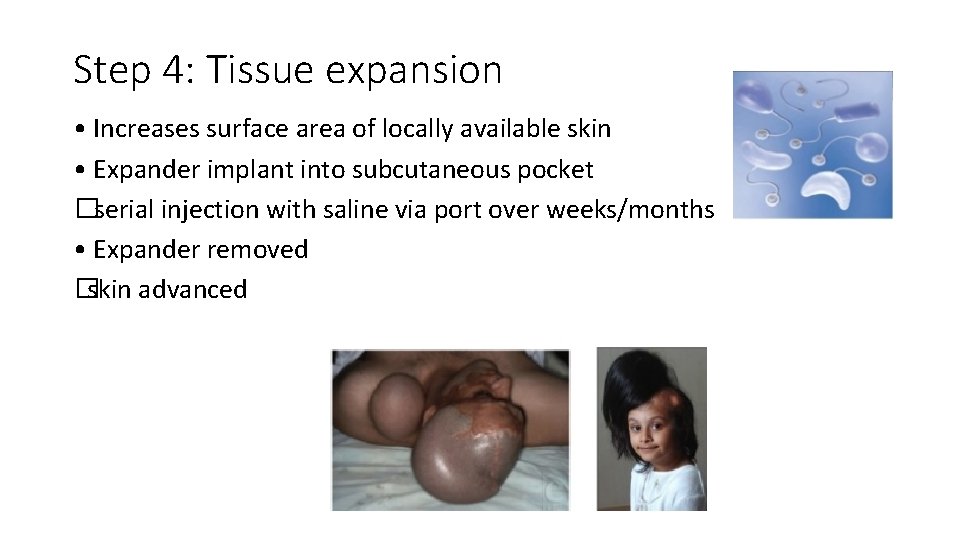
Step 4: Tissue expansion • Increases surface area of locally available skin • Expander implant into subcutaneous pocket �serial injection with saline via port over weeks/months • Expander removed �skin advanced
Tissue Expansion Advantages • Reconstructed tissue is a similar colour & texture to defect • Allows reconstruction with sensate skin with appendages • Limited donor site morbidity Disadvantages: • Painful • Prolonged • Multiple procedures and clinic attendances • No role in acute injury Contra-indications: • Immature scars • Presence of infection • Use underneath skin grafts or irradiated tissues
Step 5: Flaps • Flap = “a unit of tissue which maintains its own blood vessels whilst being transferred from a donor site to a recipient site” • 3 broad types – random pattern, pedicled and free • Numerous classification systems • Simplified = The three C’s: ▫ Circulation – blood supply �named vs unamed/random vessel ▫ Contiguity – donor site �local vs distant, pedicled vs free ▫ Composition – type of tissue �single vs composite
Flap classification: Composition • Flaps are composed of single or multiple tissue types (composite) ▫ Cutaneous ▫ Fasciocutaneous ▫ Fascial ▫ Muscle ▫ Musculocutaneous ▫ Osseocutaneous ▫ Composite
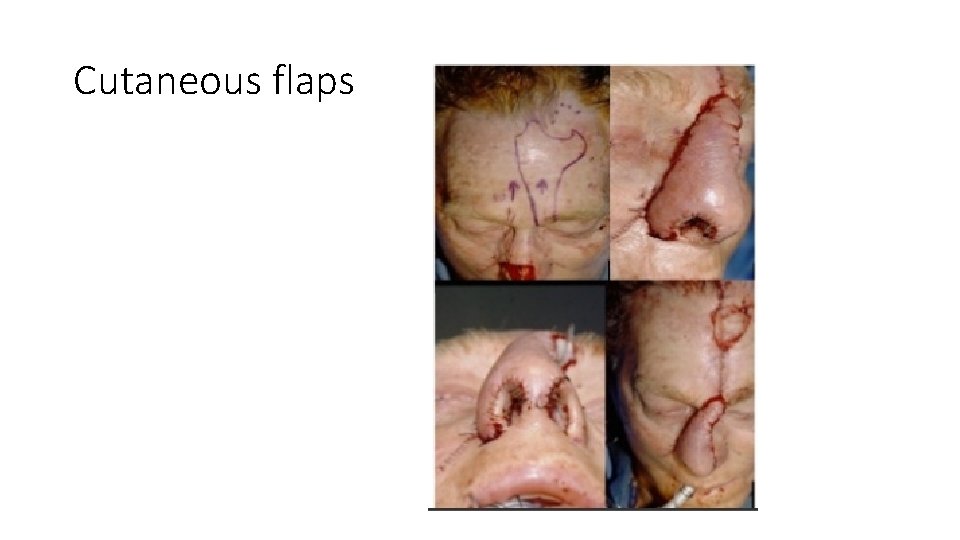
Cutaneous flaps

Fascial , Muscle , Composite

Osseous

Muscle
Flap classification: Circulation • Random pattern flaps: ▫ No directional blood flow, no named vessel ▫ Rely on dermal/subdermal plexus ▫ Limited length to breadth ratio (1: 1)
Flap classification: Circulation • Axial pattern flaps: ▫ Named depending on course of vessel ▫ Direct, fasciocutaneous, musculocutaneous
Flap classification: Circulation • Perforator flaps: ▫ Improved understanding of anatomy/physiology = custom made flap designs based on specific vessels
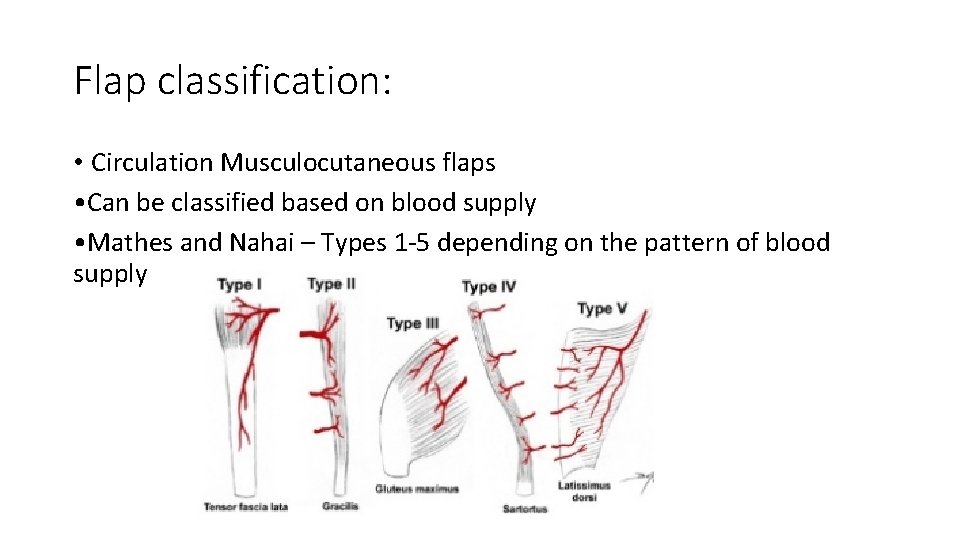
Flap classification: • Circulation Musculocutaneous flaps • Can be classified based on blood supply • Mathes and Nahai – Types 1 -5 depending on the pattern of blood supply
Flap classification: Contiguity • Local –donor site next to recipient site • Regional • Distant – pedicled or free
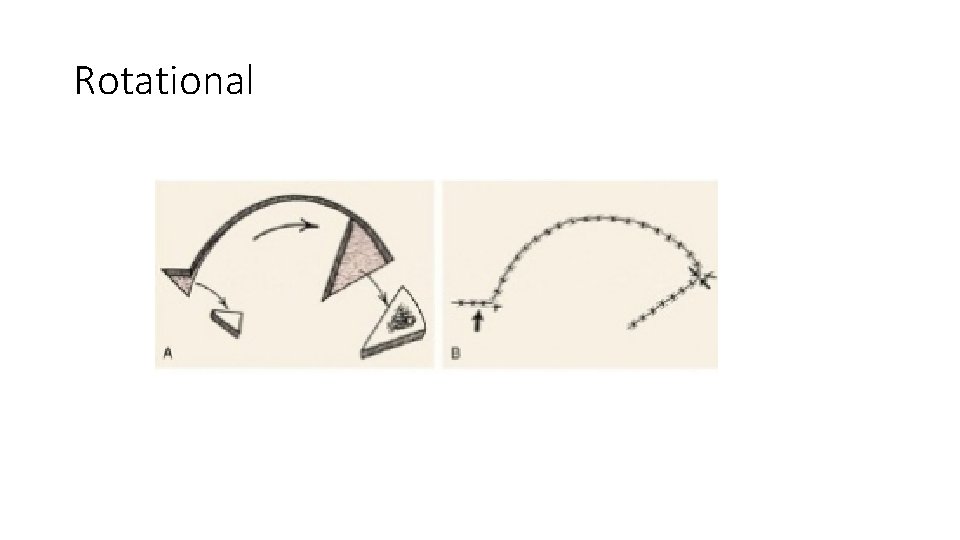
Rotational
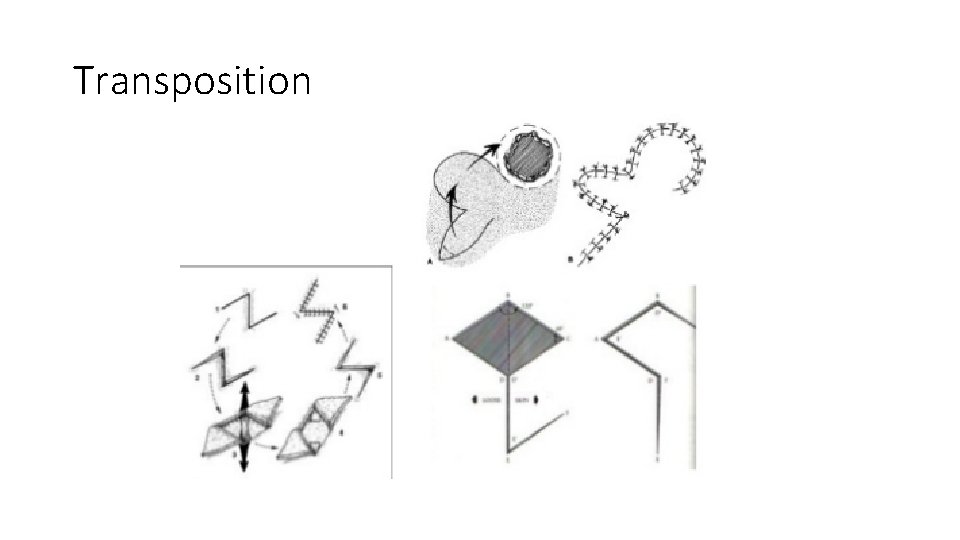
Transposition
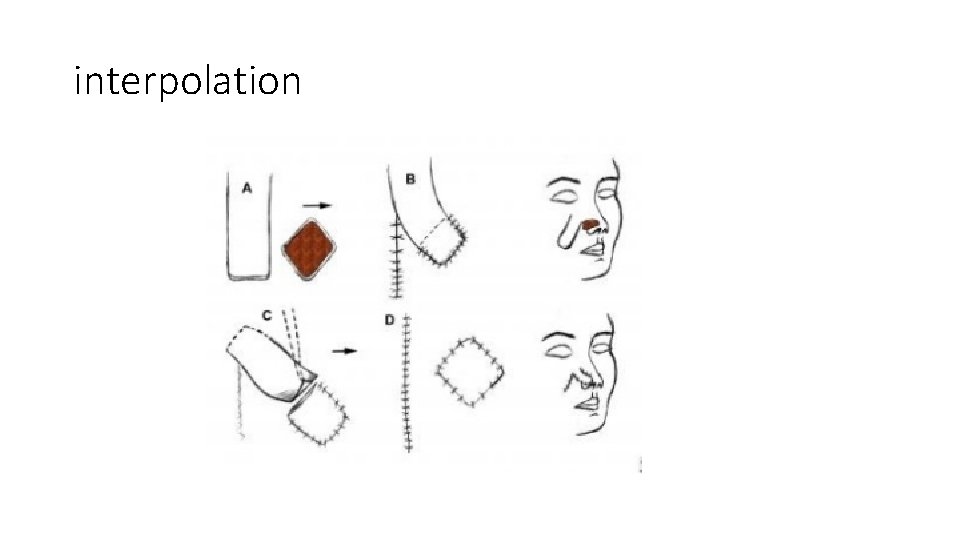
interpolation
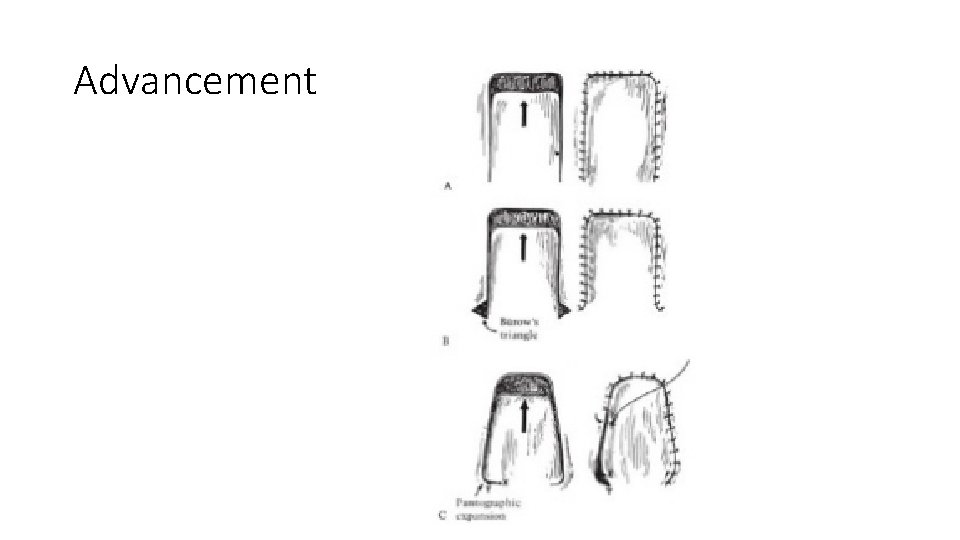
Advancement
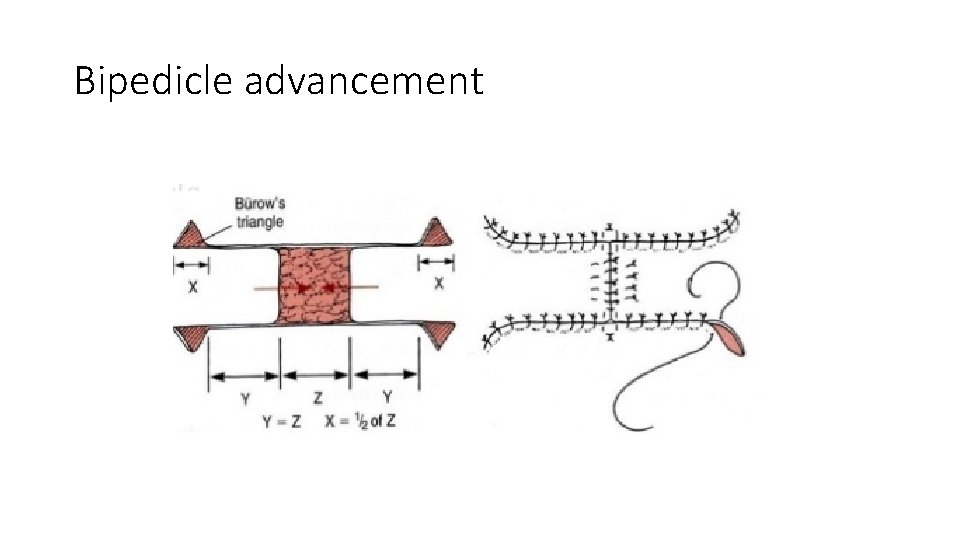
Bipedicle advancement
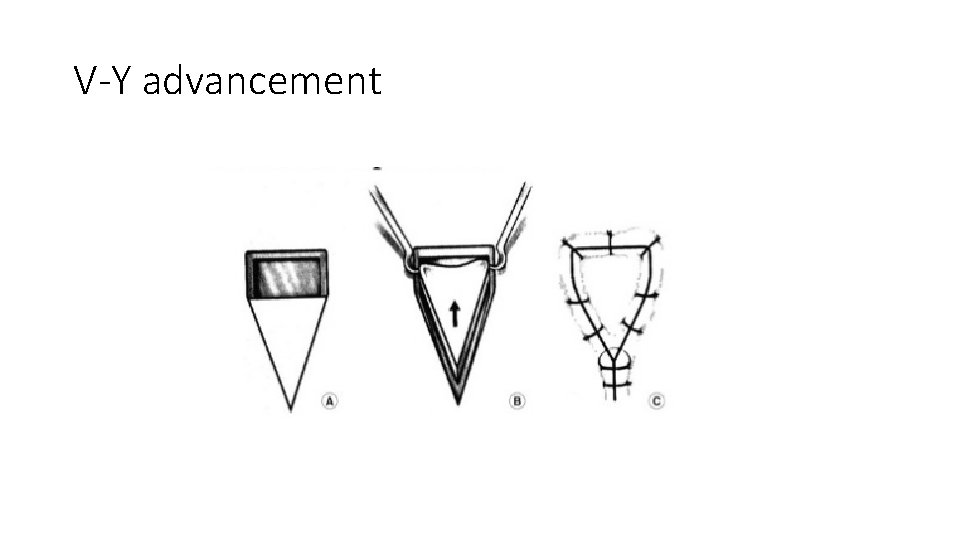
V-Y advancement
Flap classification: Contiguity • Distant – pedicled or free • Pedicled flaps - based on a named vessel (axial flaps) • Flap remains attached to pedicled vessel (which is not detached from the donor site)
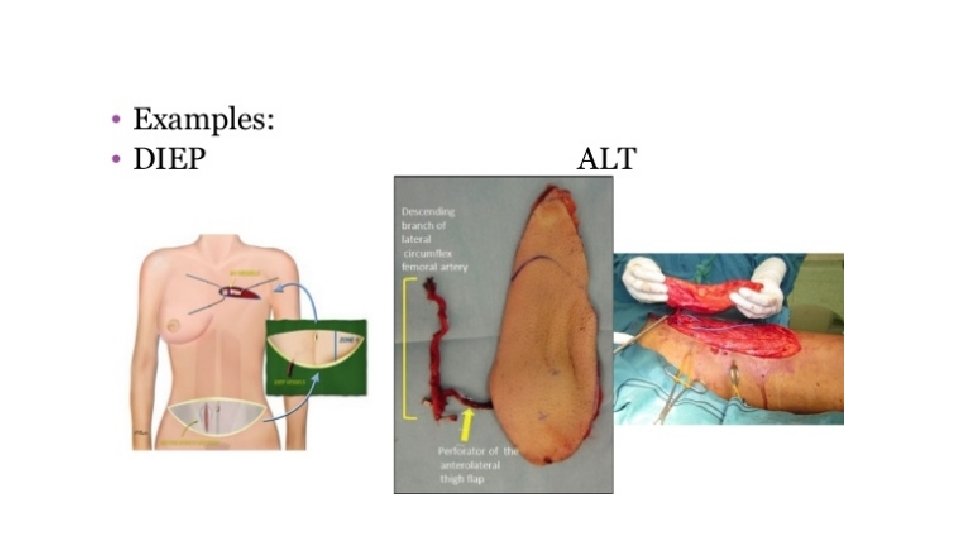
5 Flap classification: Contiguity • Distant – pedicled or free • Free flaps – tissue moved from area of the body to another with disconnection then re- anastomosis of their blood supply • Based on known axial flaps • Involves tissue ischaemia, hypoxia and reperfusion • Highest Step of reconstructive ladder • Riskiest reconstructive option
• Indications of Free flaps ▫ Need for a certain tissue at recipient site ▫ No local options (foot, distal 1/3 leg, head and neck) ▫ Massive defects ▫ Areas that need reconstruction with multiple different tissue types (head and neck/ breast) ▫ Areas requiring freshly vascularised tissue
• Advantages of free flap : ▫ Single-stage procedure ▫ Choice of donor tissues ▫ Large volume of tissue can be transferred ▫ Can optimise vascularity (recipient and donor) ▫ Less immobilisation cf. pedicled flaps ▫ Can choose and hide donor defects (esp. breast)

• Disadvantages of free flap : ▫ Long and specialised ▫ High-risk (flap-loss can occur) ▫ Quality of recipient vessel may be poor ▫ Donor site morbidity (varies according to flap) �Scar, hernia, loss of function
Thank you
- Slides: 44