Sodium Disorders of sodium concentration reflect abnormalities in
Sodium Disorders of sodium concentration reflect abnormalities in water homeostasis n Serum sodium concentration does not provide any information about sodium content i. e. volume status It is only the ratio of sodium to extracellular fluid in which it is contained n
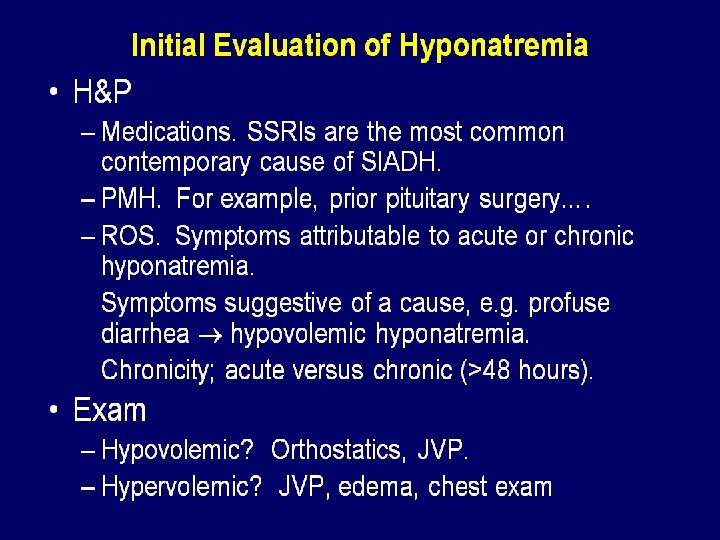
Hyponatremia Hx: duration of hyponatremia, presence of symptoms, ( change in mental status, lethargy, seizure, coma ) potential causes n PE: asses volume status, skin turgor, BP/orthostasis, pulmonary edema, peripheral edema n
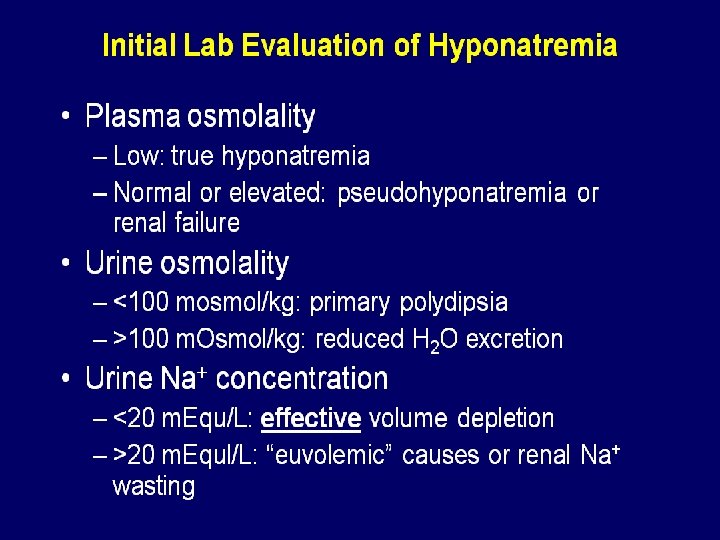
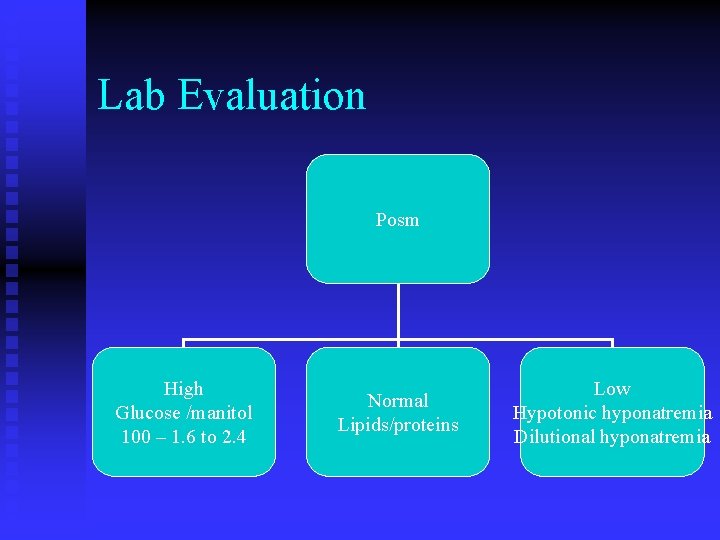
Lab Evaluation Posm High Glucose /manitol 100 – 1. 6 to 2. 4 Normal Lipids/proteins Low Hypotonic hyponatremia Dilutional hyponatremia
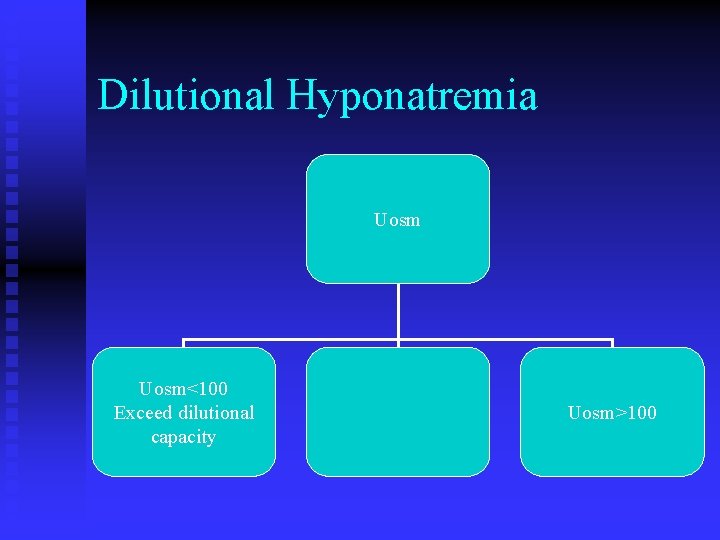
Dilutional Hyponatremia Uosm<100 Exceed dilutional capacity Uosm>100
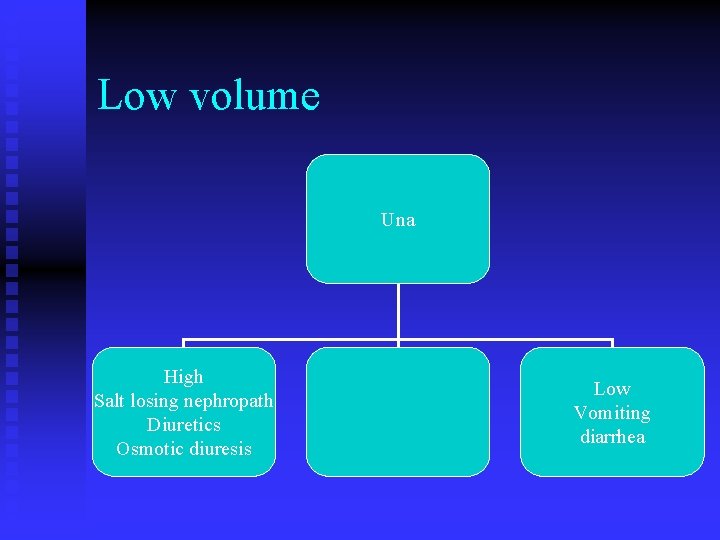
Low volume Una High Salt losing nephropath Diuretics Osmotic diuresis Low Vomiting diarrhea
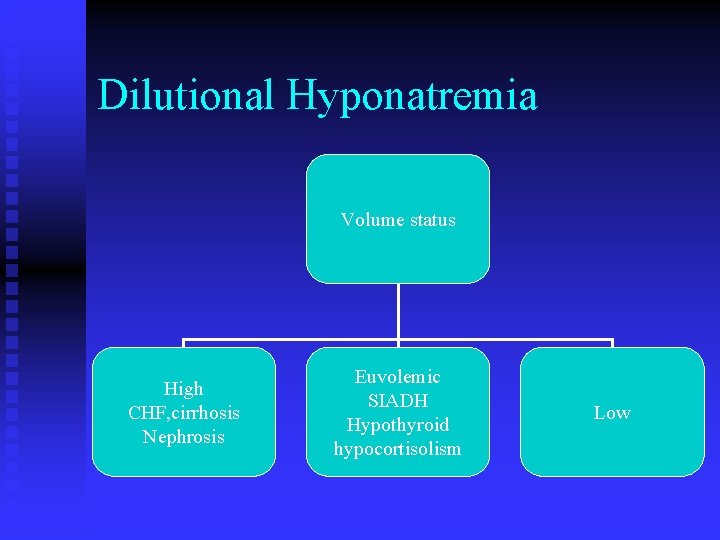
Dilutional Hyponatremia Volume status High CHF, cirrhosis Nephrosis Euvolemic SIADH Hypothyroid hypocortisolism Low

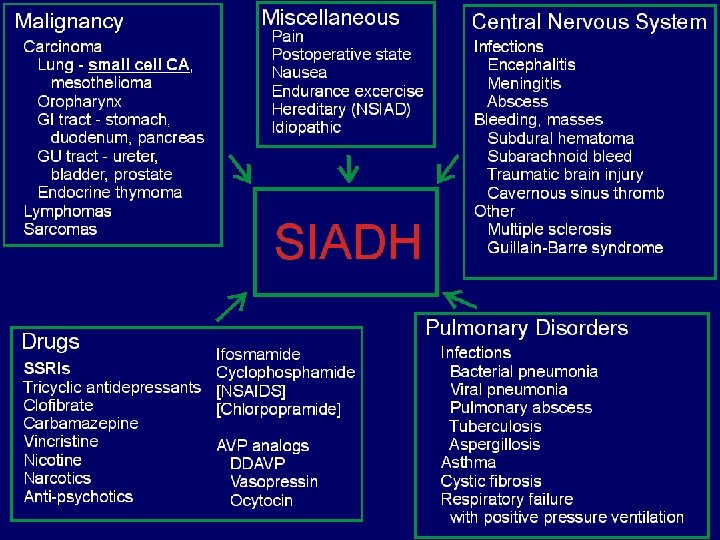
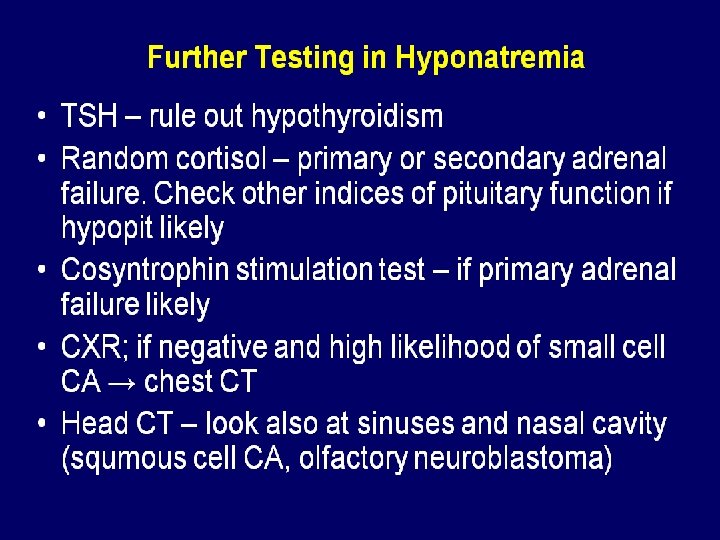
SIADH Inappropriate ADH response in a patient with hyponatremia. Urine is less than maximally dilute in the presence of relative euvolemia n Tx: free water restriction, loop diuretics, high protein and salt intake. Occasionally demeclocycline n
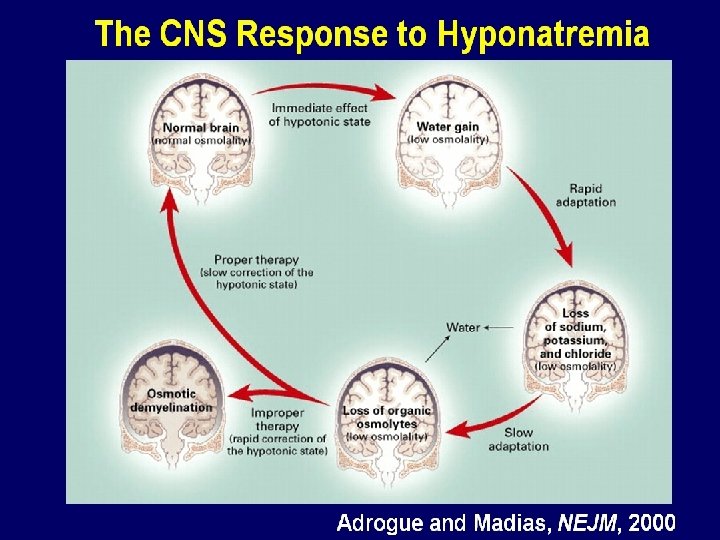
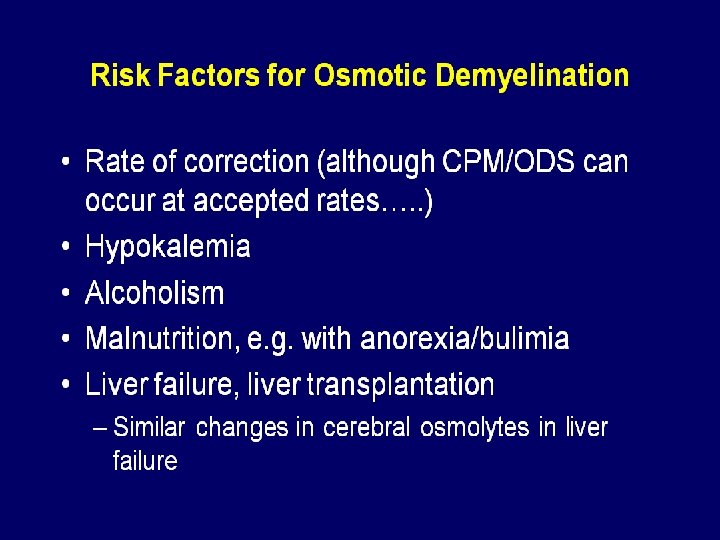
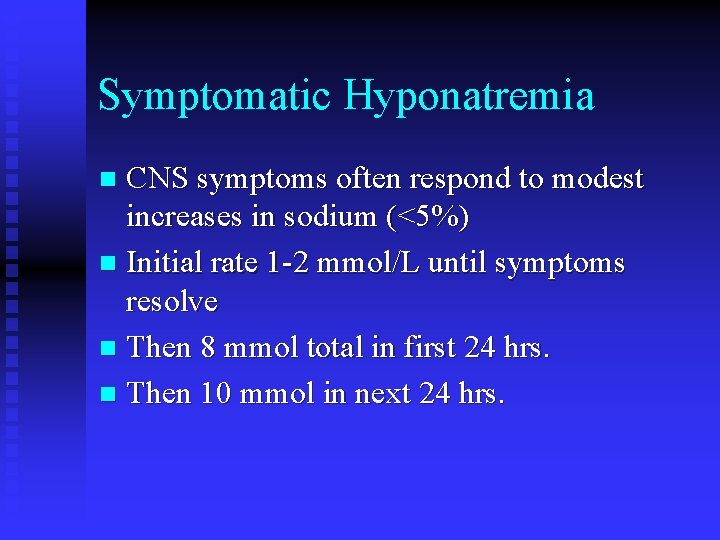
Symptomatic Hyponatremia CNS symptoms often respond to modest increases in sodium (<5%) n Initial rate 1 -2 mmol/L until symptoms resolve n Then 8 mmol total in first 24 hrs. n Then 10 mmol in next 24 hrs. n
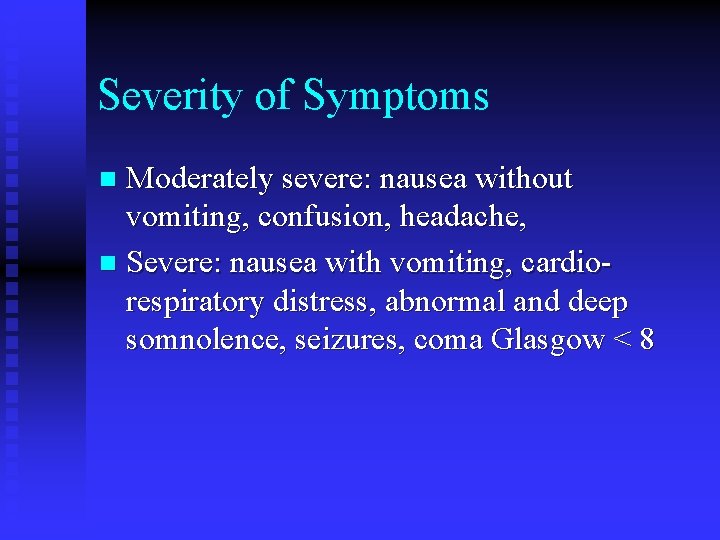
Severity of Symptoms Moderately severe: nausea without vomiting, confusion, headache, n Severe: nausea with vomiting, cardiorespiratory distress, abnormal and deep somnolence, seizures, coma Glasgow < 8 n
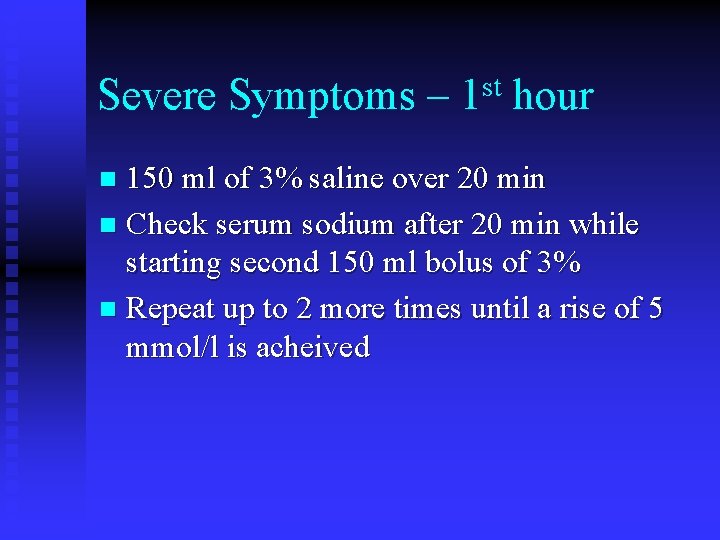
Severe Symptoms – st 1 hour 150 ml of 3% saline over 20 min n Check serum sodium after 20 min while starting second 150 ml bolus of 3% n Repeat up to 2 more times until a rise of 5 mmol/l is acheived n
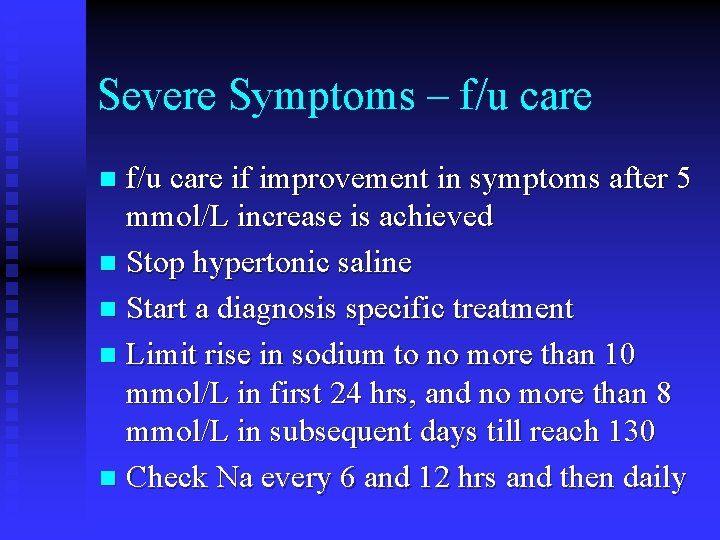
Severe Symptoms – f/u care if improvement in symptoms after 5 mmol/L increase is achieved n Stop hypertonic saline n Start a diagnosis specific treatment n Limit rise in sodium to no more than 10 mmol/L in first 24 hrs, and no more than 8 mmol/L in subsequent days till reach 130 n Check Na every 6 and 12 hrs and then daily n
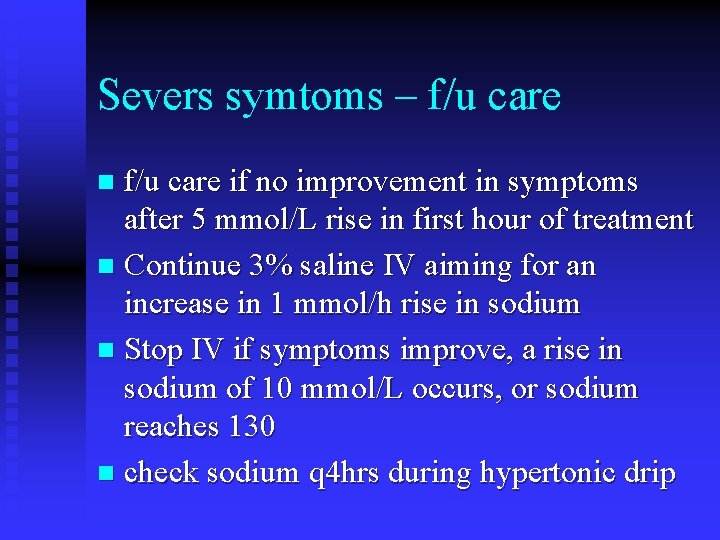
Severs symtoms – f/u care if no improvement in symptoms after 5 mmol/L rise in first hour of treatment n Continue 3% saline IV aiming for an increase in 1 mmol/h rise in sodium n Stop IV if symptoms improve, a rise in sodium of 10 mmol/L occurs, or sodium reaches 130 n check sodium q 4 hrs during hypertonic drip n

Rate of 3%– Adrogue-Madias To achieve 1 mmol/L per hr increase n Change Na = infusate Na – serum Na/TBW +1 n Include any potassium if in the infusate, i. e. infusate Na + infusate K n TBW =. 6 X body weight in men =. 5 X body weight in women n n

Correction Example Chg in Na/L of fluid=IV Na – Pna/TBW+1 n 3%saline = 513 mmol/L n Vol IV = desired change/expected chg 1 L n Rate infusion = Vol/time n
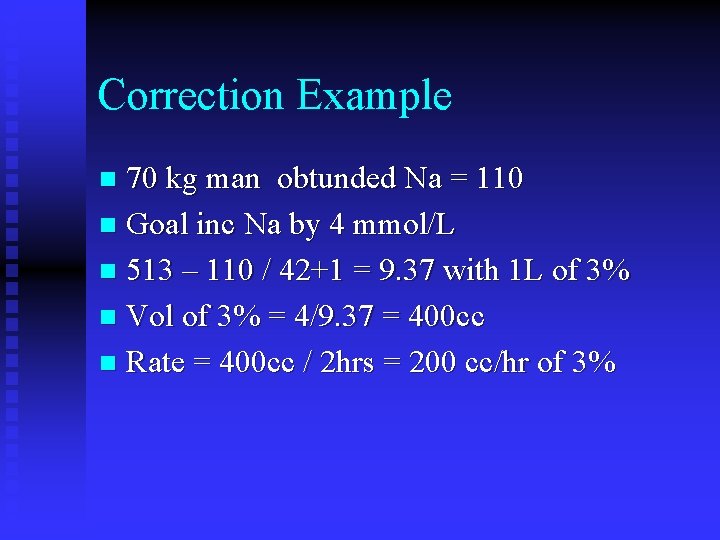
Correction Example 70 kg man obtunded Na = 110 n Goal inc Na by 4 mmol/L n 513 – 110 / 42+1 = 9. 37 with 1 L of 3% n Vol of 3% = 4/9. 37 = 400 cc n Rate = 400 cc / 2 hrs = 200 cc/hr of 3% n
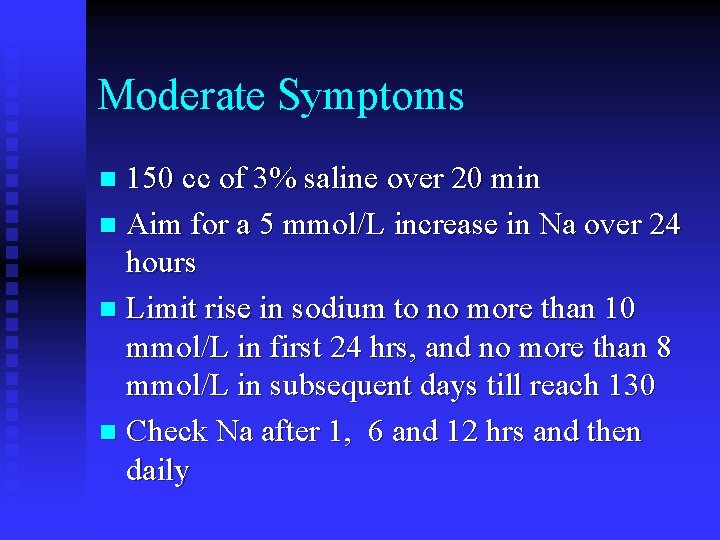
Moderate Symptoms 150 cc of 3% saline over 20 min n Aim for a 5 mmol/L increase in Na over 24 hours n Limit rise in sodium to no more than 10 mmol/L in first 24 hrs, and no more than 8 mmol/L in subsequent days till reach 130 n Check Na after 1, 6 and 12 hrs and then daily n
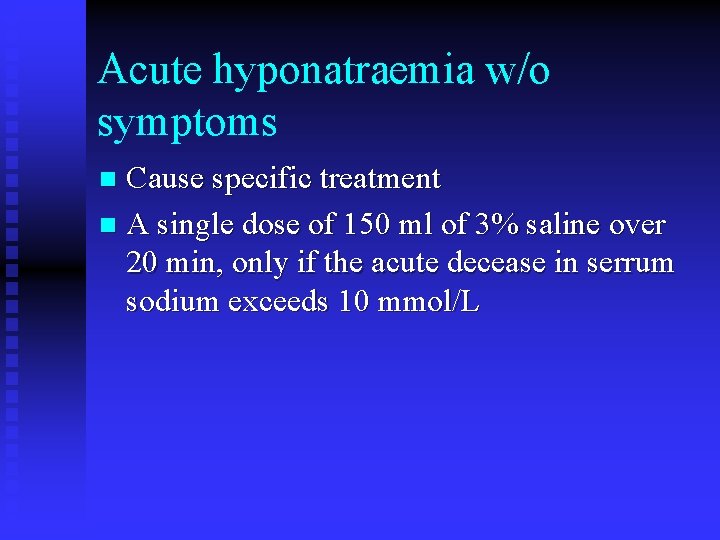
Acute hyponatraemia w/o symptoms Cause specific treatment n A single dose of 150 ml of 3% saline over 20 min, only if the acute decease in serrum sodium exceeds 10 mmol/L n
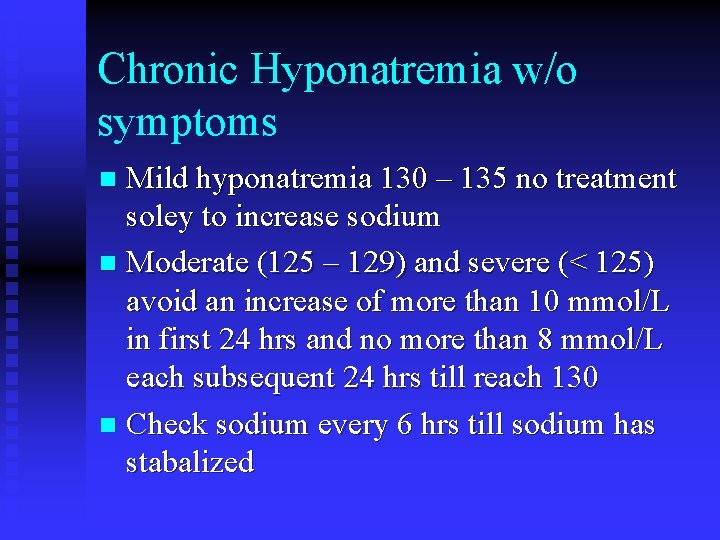
Chronic Hyponatremia w/o symptoms Mild hyponatremia 130 – 135 no treatment soley to increase sodium n Moderate (125 – 129) and severe (< 125) avoid an increase of more than 10 mmol/L in first 24 hrs and no more than 8 mmol/L each subsequent 24 hrs till reach 130 n Check sodium every 6 hrs till sodium has stabalized n
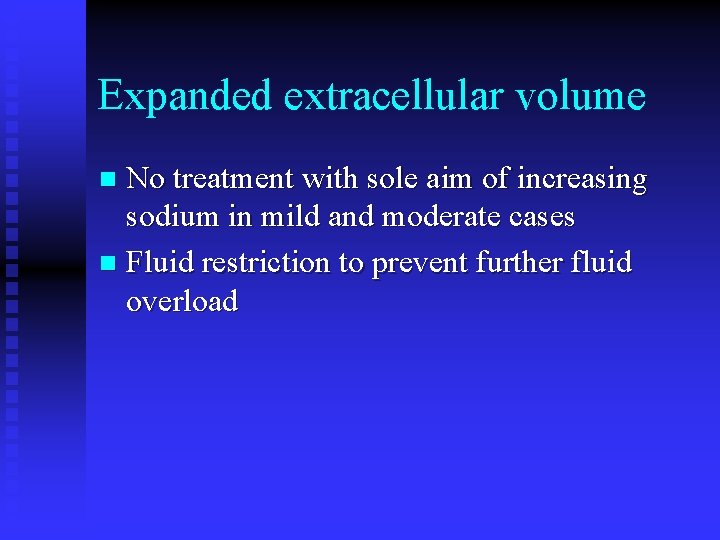
Expanded extracellular volume No treatment with sole aim of increasing sodium in mild and moderate cases n Fluid restriction to prevent further fluid overload n
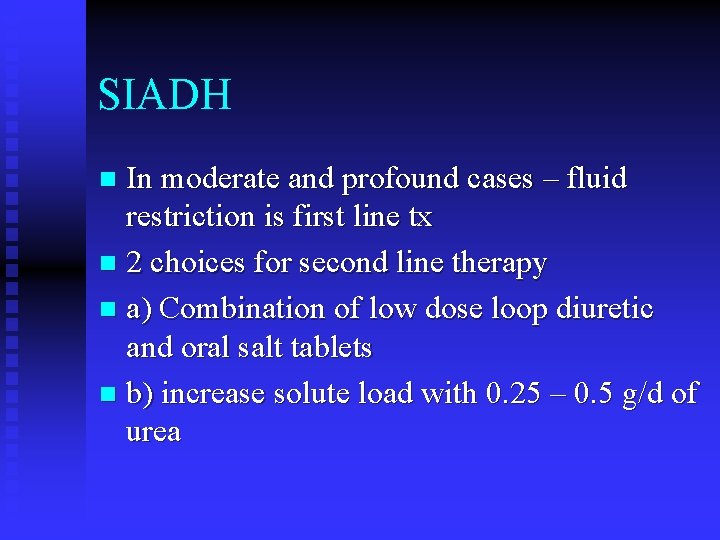
SIADH In moderate and profound cases – fluid restriction is first line tx n 2 choices for second line therapy n a) Combination of low dose loop diuretic and oral salt tablets n b) increase solute load with 0. 25 – 0. 5 g/d of urea n
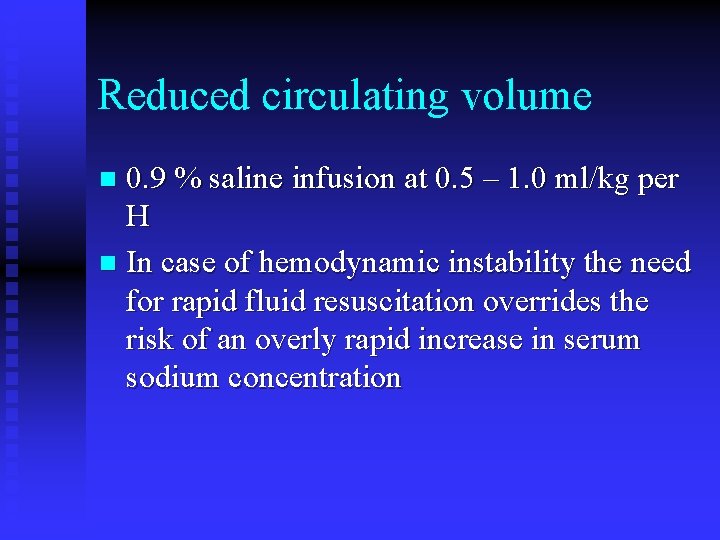
Reduced circulating volume 0. 9 % saline infusion at 0. 5 – 1. 0 ml/kg per H n In case of hemodynamic instability the need for rapid fluid resuscitation overrides the risk of an overly rapid increase in serum sodium concentration n
Overcorrection Prompt intervention for sodium rise > 10 mmol/L for the first day and 8 mmol/L for following days n Start an infusion of 10 ml/kg of free water over 1 hour n Consider IV desmporessin 2 micrograms, not more frequently than every 8 hours n
Correction n There is no substitute for frequent monitoring of the sodium response
Hypernatremia All forms of hypernatremia are associated with hyperosmolarity n Volume status cannot be inferred from the presence of hypernatremia n
Symptoms n CNS invovlement – lethargy, irritability, weakness, confusion – usually occur with sodium greater than 160
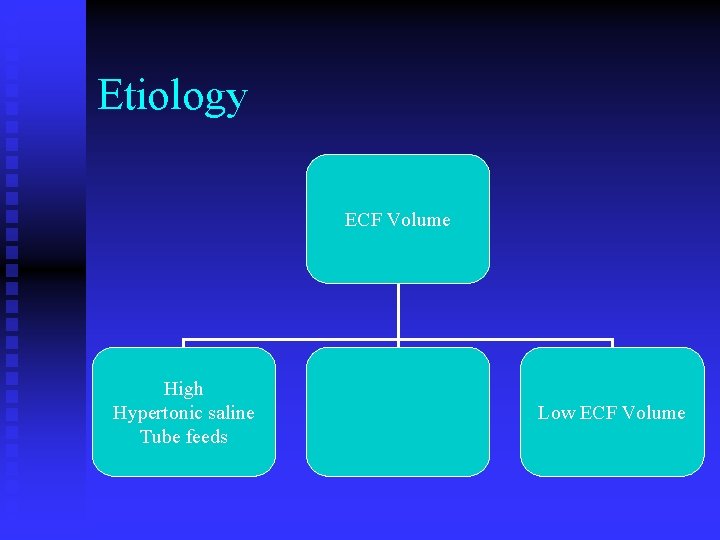
Etiology ECF Volume High Hypertonic saline Tube feeds Low ECF Volume
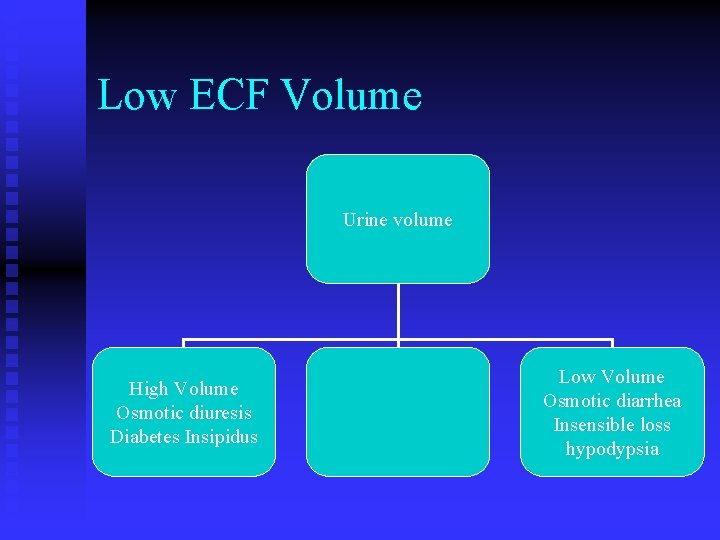
Low ECF Volume Urine volume High Volume Osmotic diuresis Diabetes Insipidus Low Volume Osmotic diarrhea Insensible loss hypodypsia
Correction of Hypernatremia Rate of correction. 5 mmol/L/hr n Severe Vol depletion or hemodynamic instability merits tx with. 9 NS n Lesser degrees of volume depletion can be treated with ½ or ¼ normal saline n Once volume is corrected can use D 5 W n
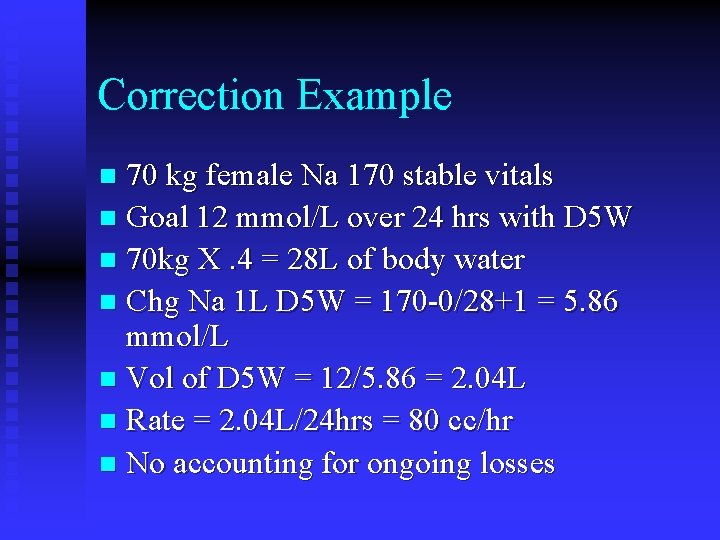
Correction Example 70 kg female Na 170 stable vitals n Goal 12 mmol/L over 24 hrs with D 5 W n 70 kg X. 4 = 28 L of body water n Chg Na 1 L D 5 W = 170 -0/28+1 = 5. 86 mmol/L n Vol of D 5 W = 12/5. 86 = 2. 04 L n Rate = 2. 04 L/24 hrs = 80 cc/hr n No accounting for ongoing losses n
Potassium n Hypo and hyper kalemia results from alterations in intake, cellular shifts or alterations in elimination
Hyperkalemia Etiology n Transcellular Shift Exercise, hyperchloremic metabolic acidosis, Insulin deficiency, hypertonicity, alpha adrenergic stimulation, tissue breakdown/ischemia (rhabdo, brain, gi)
etiology n Decreased renal excretion – CRF, Hypoaldo (meds i. e. ACE/ARB, NSAIDs, heparin. Type 4 RTA
Etiology n Pseudohyperkalemia ischemic/traumatic blood draw, increased wbc/plts (100, 000 400, 000)
Hyperkalemia Sx: neuromuscular weakness and cardiac conduction problems n Level of K at which problems occur is very variable between patients n
Etiology Increased Total Body K increased intake (rare as sole cause) decreased renal excretion Spurious – Thrombocytosis, Leukocytosis, ischemic blood draw n
Diagnosis Normal to High 24 hr urinary K >40 meq/d relative increase in K intake Low 24 hr urinary K < 20 – 40 meq/d Decreased renal K excretion GFR < 20 ml/min endogenous K load drugs that impair K excertion n
Diagnosis n Low 24 hr urine K – GFR > 20 ml/min decrease mineralcorticoid production/action Action – pseudohypoaldo type 1 or 2 Acquired ARB, aldactone, amiloride, sickle cell, obstruction Production - Hypoaldo, ACE, Heparin,
Diagnosis n Decreased distal nephron sodium delivery Heart failure, cirrhosis, volume depletion
hypokalemia Mild is asymptomatic (3. 0 – 3. 5) n Sever muscle weakness, pain cause rhabdo prominent U waves diminished or inverted T waves ST depression leads to vfib n
Hypokalemia - Etiology Shift Alkalemia, insulin, refeeding, thyrotoxicosis, Hypokalemic perodic paralysis, Barium Decreased Total Body K Decreased intake Increased Loss GI or Renal Spurious – Extreme leukocytosis n
Diagnosis n Low 24 hr K loss < 20 m. Eq/d Extrarenal metabolic acidosis – GI loss Diarrhea normal p. H – decreased intake metabolic alkalosis – GI Loss Vomiting
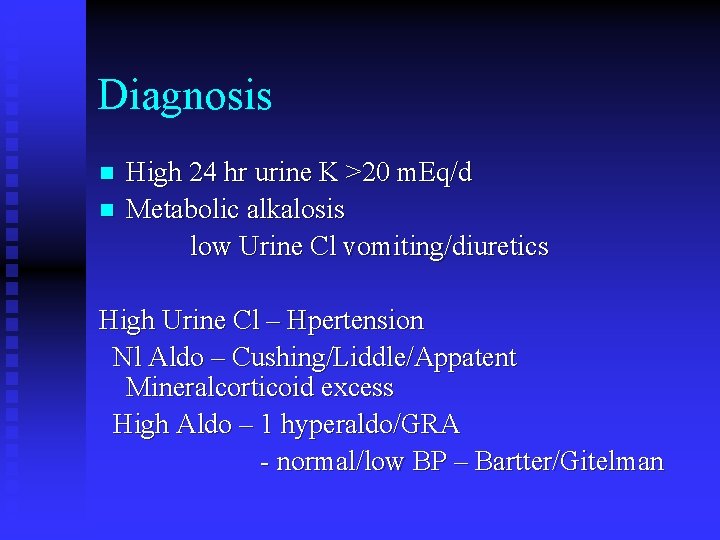
Diagnosis n n High 24 hr urine K >20 m. Eq/d Metabolic alkalosis low Urine Cl vomiting/diuretics High Urine Cl – Hpertension Nl Aldo – Cushing/Liddle/Appatent Mineralcorticoid excess High Aldo – 1 hyperaldo/GRA - normal/low BP – Bartter/Gitelman
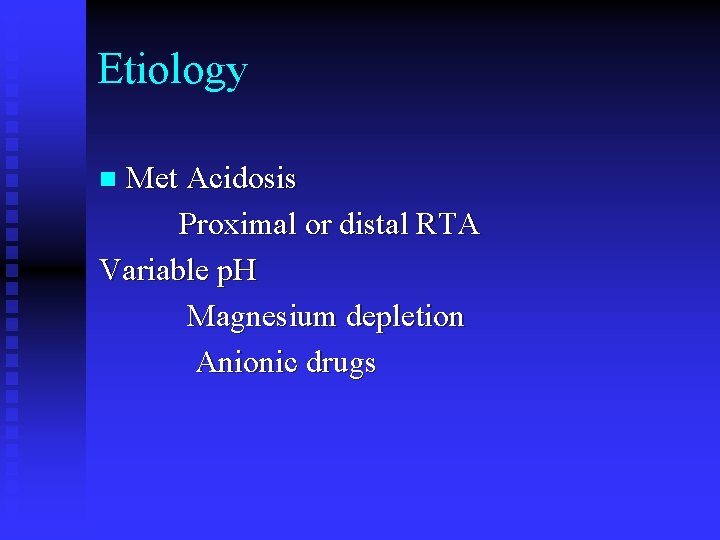
Etiology Met Acidosis Proximal or distal RTA Variable p. H Magnesium depletion Anionic drugs n
- Slides: 53