Smiling matters Oral Health care in care homes















- Slides: 29
Smiling matters Oral Health care in care homes Kent Community Dental Service
Aims Be able to provide oral health education to the carers to improve knowledge on oral health To be able to build carers confidence in completing oral health assessment Objectives ● ● To understand the importance of brushing To understand what dry mouth is and how to manage it. To provide information on denture care To demonstrated how to assess oral health
Why is this training being provided? CQC report “Smiling matters: oral health care in care homes” June 2019. 52% care homes did not have policy to promote and protect people’s oral health, 73% of care plan reviews did not cover oral health 47% of the staff members had never received training in oral health care. CQC stated that “it wants care home to embrace oral health and ensure that it receives the same priority ad physical and mental health”.

Why is it important…? ? We use our mouth to: chew, swallow, taste food, communicate/talk, express emotions Some bacteria associated with general health- pneumonia, cardiovascular disease, Alzheimer's, Diabetes How can dental pain affect our daily life? ? Unable to eat/drink: lack of nutrition, affect on general health- immune system Affects mood: grumpy, angry, tearful, unresponsive Unable to sleep Trouble talking Cost- travelling to/for appointments, payments for the treatment Depend on carers or family members for self care

Why is this training important? Holistic care Prevention: reduce risk of caries, gum disease, keep the teeth longer Older people are more at risk of oral disease o Medication side effects o Frail and dependent due to reduced manual dexterity o Inadequate oral hygiene care

Topics Plaque Tooth decay (caries) Gum disease Brushing Dry mouth Denture care Assessing oral health

Gum disease Inflammation of the gingiva (gum) Gingivitis: early stage, short duration characterised as inflammation of the gum and its reversible. Periodontitis: irreversible, long duration characterised by inflammation of the gums and the supporting periodontium; periodontal ligament and the bones which are destroyed/lost. Diabetic has increases risk of developing periodontal disease Sign and symptoms: Bleeding Bad breath Red and sore gums Loose teeth Sensitivity Recession Plaque and calculus present

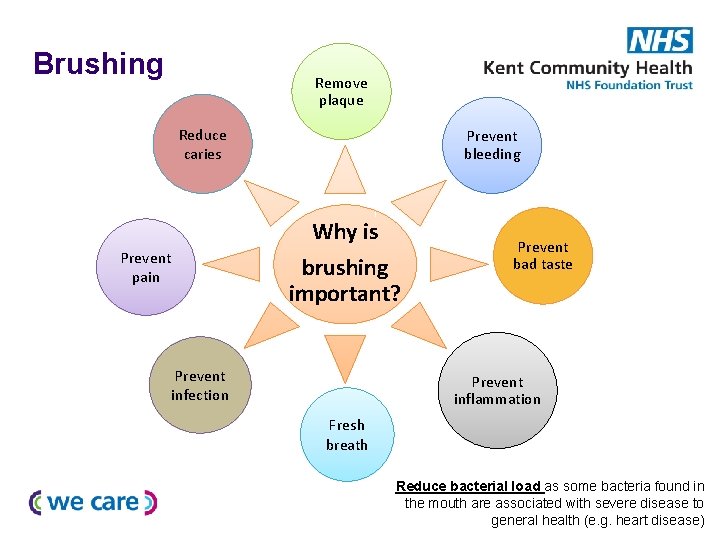
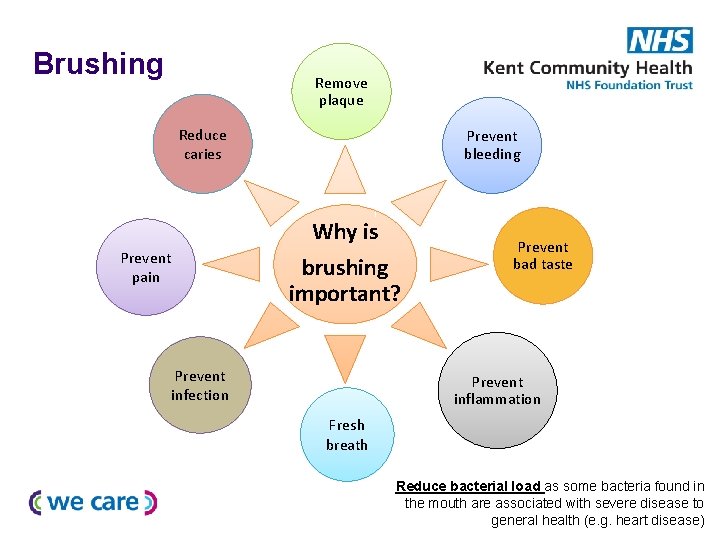
Brushing Remove plaque Reduce caries Prevent bleeding Why is brushing important? Prevent pain Prevent infection Prevent bad taste Prevent inflammation Fresh breath Reduce bacterial load as some bacteria found in the mouth are associated with severe disease to general health (e. g. heart disease)
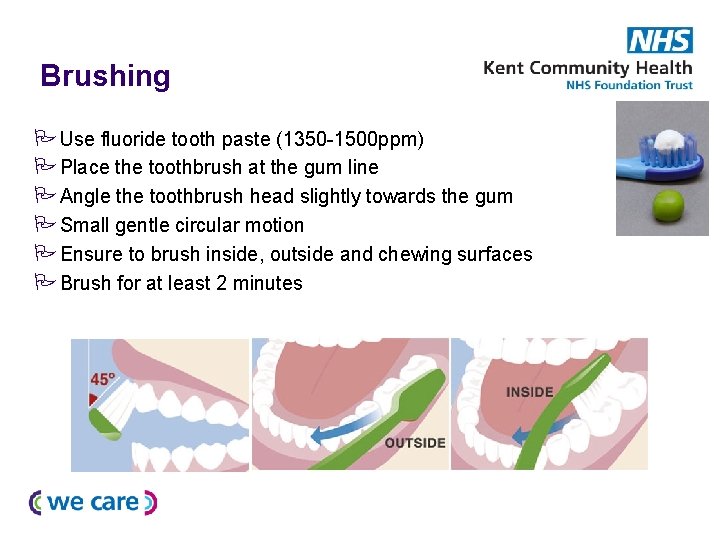
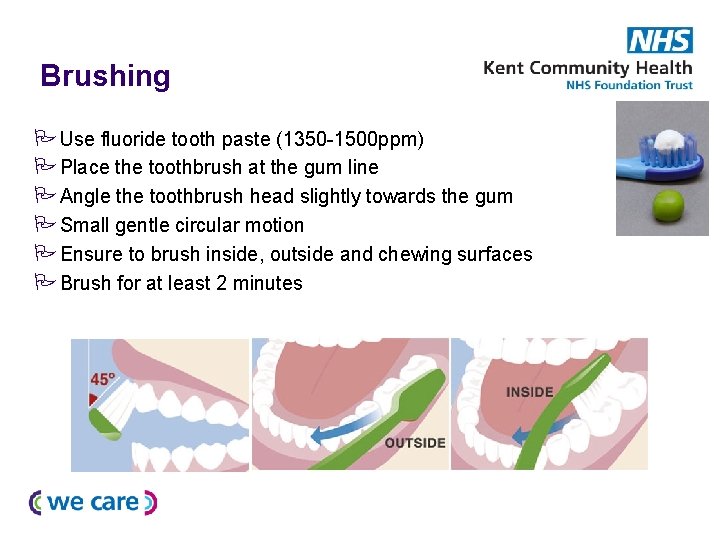
Brushing Use fluoride tooth paste (1350 -1500 ppm) Place the toothbrush at the gum line Angle the toothbrush head slightly towards the gum Small gentle circular motion Ensure to brush inside, outside and chewing surfaces Brush for at least 2 minutes

Most important to brush Before bed time- reduced saliva production, increased bacterial activity due to reduced saliva antibacterial/buffering properties Any time during the day Spit no rinse Requires a lot of patience and time Ask the residents how they would like to brush and what form of help they want

What type of tooth brush. . ? Electric or manual Small headed Tooth brush adaptors - Tennis ball - Putty/clay grip - Super brush - Use of weight to control muscle movements

Where to look for fluoride content in a toothpaste package 1350 -1500 ppm Fluoride Sodium fluoride Stannous fluoride
Dry mouth Absence or reduction of saliva production/flow, this could be due to age, reduced salivary glands function, diabetes, side effects of medication, post radiotherapy or chemotherapy, mouth breathing etc. Saliva acts as lubricant, has anti-microbial/bacterial properties, neutralised the oral cavity; p. H neutral Some medications that can cause dry mouth: § High blood pressure § Antihistamine § Antidepressant

How to identify it? Lips: looks very dry and chapped, sore and cracked corner of the lips Mouth red and shiny Unable or difficulties to eat/chew/swallowing food, taking very long time to eat Difficulties on talking Increased caries Bad breath Complaint about having thick and stringy saliva Burning/tingly sensation or sensitive to certain food; spicy, citric, alcohol Unable to wear the dentures

Management Drink plenty of water, sip plain water through out the day Salivary stimulants/substitutes: gel, spray, tablets, lozenges- consult with GP Sugar free sweets If breathing through mouth consult with GP to assess any issues with nasal passage Reduce alcohol, tea and coffee content Stop smoking If dry mouth is due to medications, consult with GP regarding alternative medications Avoid tooth paste containing Sodium Lauryl Sulphate (SLS) Avoid citrus and spicy food

Other conditions associated with poor oral hygiene Candida infections: white patch, e. g. thrush Ulcerations Stomatitis Angular chelitis; sore and cracking of the corner of the lips/mouth Oral cancer General health: Bacteria associated with: Cardiovascular (heart) disease; infective endocarditisbacteria causing infection, increases risk of Alzheimer’s, Pneumonia If in doubt book an urgent appointment with GP or dentist

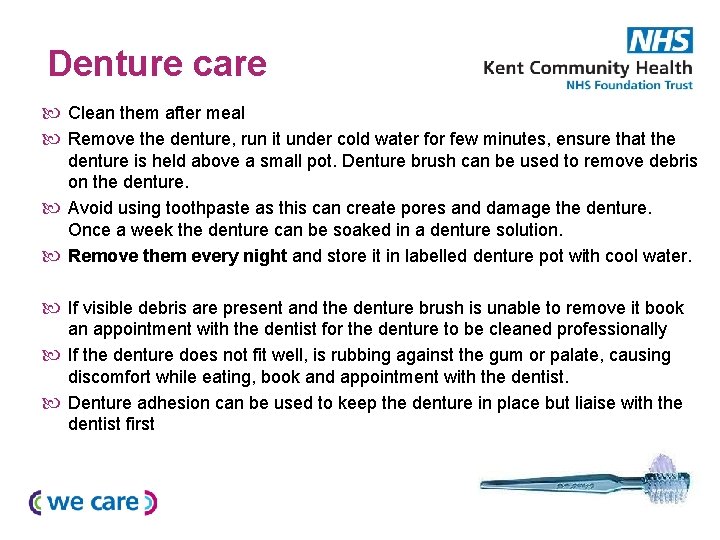
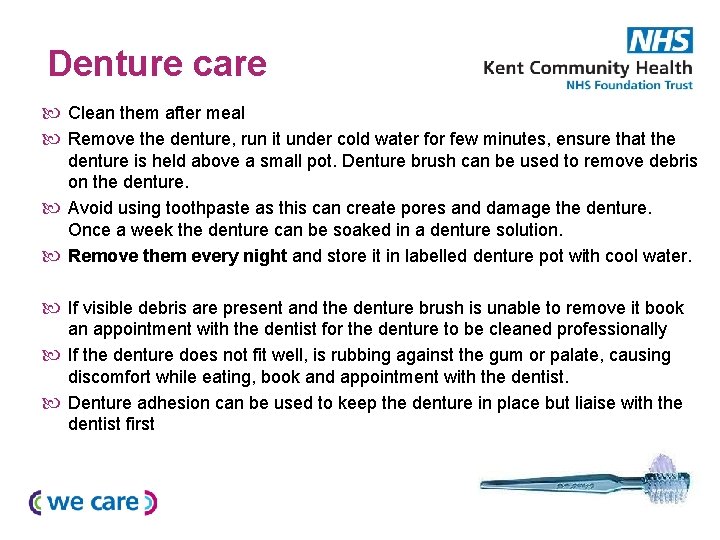
Denture care Clean them after meal Remove the denture, run it under cold water for few minutes, ensure that the denture is held above a small pot. Denture brush can be used to remove debris on the denture. Avoid using toothpaste as this can create pores and damage the denture. Once a week the denture can be soaked in a denture solution. Remove them every night and store it in labelled denture pot with cool water. If visible debris are present and the denture brush is unable to remove it book an appointment with the dentist for the denture to be cleaned professionally If the denture does not fit well, is rubbing against the gum or palate, causing discomfort while eating, book and appointment with the dentist. Denture adhesion can be used to keep the denture in place but liaise with the dentist first

Oral Health Foundation: Denture care guidelines
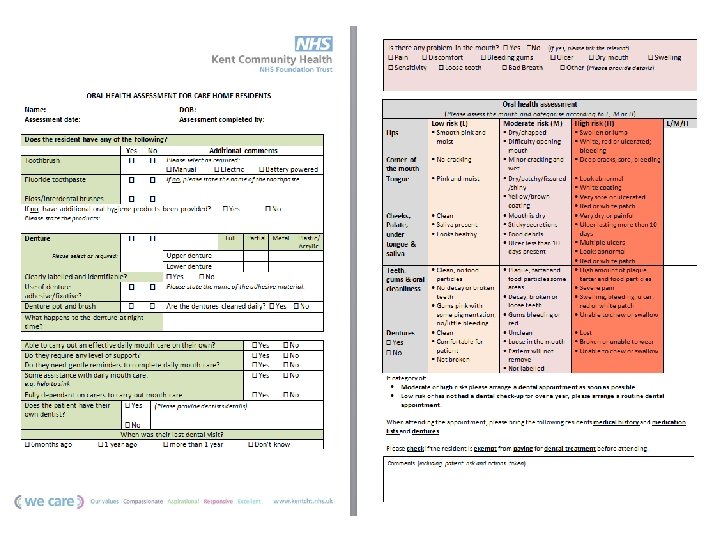
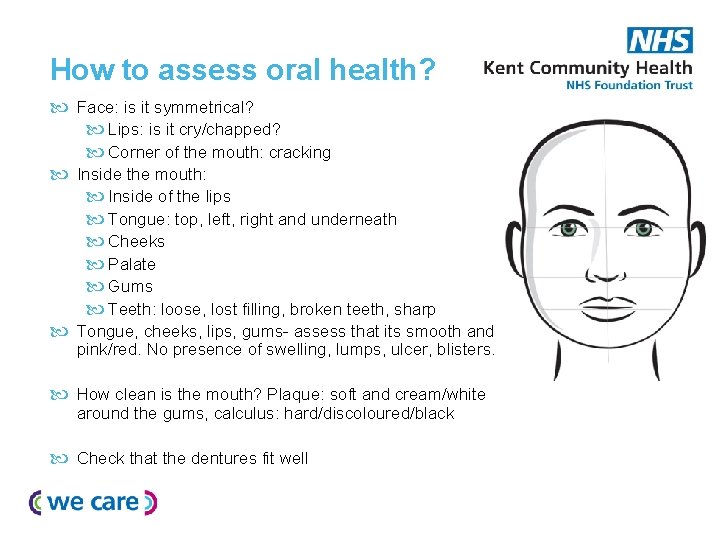
How to assess oral health? Face: is it symmetrical? Lips: is it cry/chapped? Corner of the mouth: cracking Inside the mouth: Inside of the lips Tongue: top, left, right and underneath Cheeks Palate Gums Teeth: loose, lost filling, broken teeth, sharp Tongue, cheeks, lips, gums- assess that its smooth and pink/red. No presence of swelling, lumps, ulcer, blisters. How clean is the mouth? Plaque: soft and cream/white around the gums, calculus: hard/discoloured/black Check that the dentures fit well


Medication that can have an effect on oral health Common examples are: Antihypertension (high blood pressure); calcium channel blockers Anti depressants Antihistamines Anti-epileptic drug: phenytoin Immunosuppressant: cyclosporine If unsure about the presence of the signs please liaise with the GP. Alternative medication can be requested to prevent or reduce the sideeffects of the medications on the oral health.
Seeing a dentist Ensure that all resident registered to the dentist and having a regular check-up. NHS choice- search for dental practice near the care home Local general dental practice: some dental practice have few emergency slots available but this does not mean they will see them as there might be other patients who is in need of the dentist more Out of hour dental service: Dentaline Home visits Complex cases: referral to community dental service
www. kentcht. nhs. uk/services/dental Domiciliary Service Download packs Online referral form Referral Management team: 0330 123 9438
Resources CQC report: June 2019 “Smiling matters- Oral health care in care homes” Oral Health Foundation: Denture care guidelines https: //www. dentalhealth. org/denturecareguidelines Dent-O-Care: OH aids NHS choice Delivering better oral health: an evidence-based toolkit for prevention Mouth care matters Alzheimer’s society: https: //www. alzheimers. org. uk/get-support/dailyliving/dental-care
 Enhanced health in care homes
Enhanced health in care homes Hhs
Hhs Infant oral health care
Infant oral health care Health matters paragraph
Health matters paragraph Health matters amesbury
Health matters amesbury Holston homes foster care
Holston homes foster care Homely remedies care homes
Homely remedies care homes Nationwide care matters
Nationwide care matters Aged care matters
Aged care matters Palliative care matters
Palliative care matters Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Smiling faces beautiful places
Smiling faces beautiful places Bursting through the door the flustered mother
Bursting through the door the flustered mother Limerick lady from niger
Limerick lady from niger Smiling vs frowning
Smiling vs frowning I just kept on smiling full text
I just kept on smiling full text Diction refers to
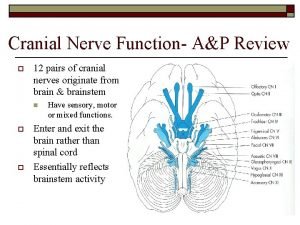
Diction refers to 12 cranial nerve test
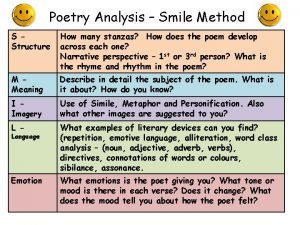
12 cranial nerve test Structure of the poem
Structure of the poem Smiling adverb
Smiling adverb Gently smiling the mother tenderly
Gently smiling the mother tenderly Identifying tone and mood bouncing into the room
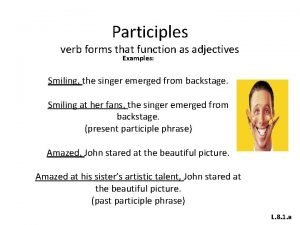
Identifying tone and mood bouncing into the room Participle phrase
Participle phrase On one corner of my dresser sits a smiling toy clown
On one corner of my dresser sits a smiling toy clown Smiling umbilicus
Smiling umbilicus Albert camus smiling
Albert camus smiling Smiling is adjective
Smiling is adjective Gently smiling the mother tenderly
Gently smiling the mother tenderly Purpose
Purpose Echelle smiling faces
Echelle smiling faces