SMFM Clinical Practice Guidelines Isolated fetal choroid plexus
- Slides: 8
SMFM Clinical Practice Guidelines Isolated fetal choroid plexus cysts Society of Maternal Fetal Medicine with the assistance of Karin M. Fuchs MD Published in Contemporary OB/GYN / April 2013
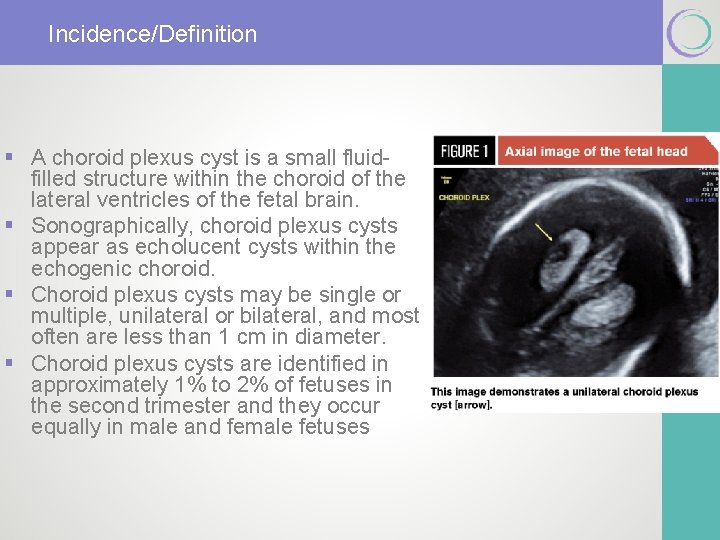
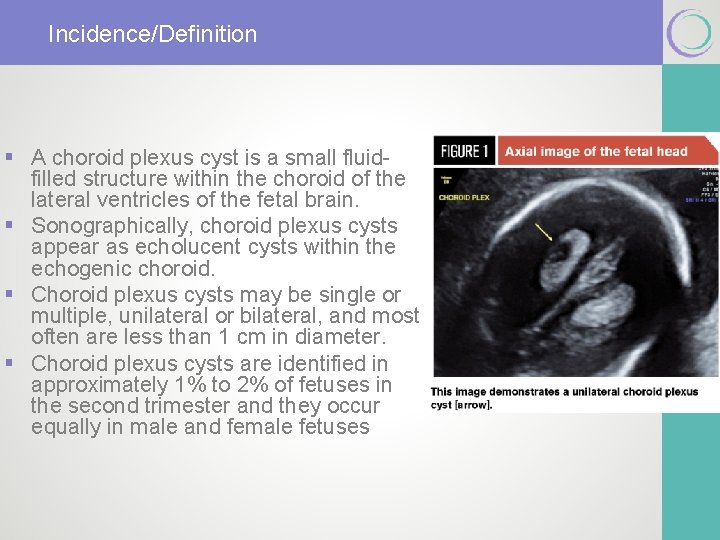
Incidence/Definition § A choroid plexus cyst is a small fluidfilled structure within the choroid of the lateral ventricles of the fetal brain. § Sonographically, choroid plexus cysts appear as echolucent cysts within the echogenic choroid. § Choroid plexus cysts may be single or multiple, unilateral or bilateral, and most often are less than 1 cm in diameter. § Choroid plexus cysts are identified in approximately 1% to 2% of fetuses in the second trimester and they occur equally in male and female fetuses
Major clinical implications of an isolated choroid plexus § When a choroid plexus cyst is identified, the presence of structural malformations and other sonographic markers of aneuploidy should be assessed with a detailed fetal anatomic survey. § Detailed examination of the fetal heart (4 -chamber view and outflow tracts view) and hands (for “clenching” or other abnormal positioning) should be included, as well as fetal biometry for assessment of intrauterine growth restriction.
Major clinical implications of an isolated choroid plexus § A choroid plexus cyst is not considered a structural or functional brain abnormality. § Most choroid plexus cysts are isolated and occur in otherwise lowrisk pregnancies. § The only association of some significance between an isolated choroid plexus cyst and a possible fetal problem is with trisomy 18. § Choroid plexus cysts are present in 30% to 50% of fetuses with trisomy 18. § When a fetus is affected by trisomy 18, multiple structural anomalies are almost always evident, including structural heart defects, clenched hands, talipes deformity of the feet, growth restriction, and polyhydramnios. § When a structural anomaly is present in addition to choroid plexus cysts, the probability of trisomy 18 is 37%. § In the absence of associated sonographic abnormalities, the likelihood of trisomy 18 is extremely low in otherwise low-risk pregnancies.
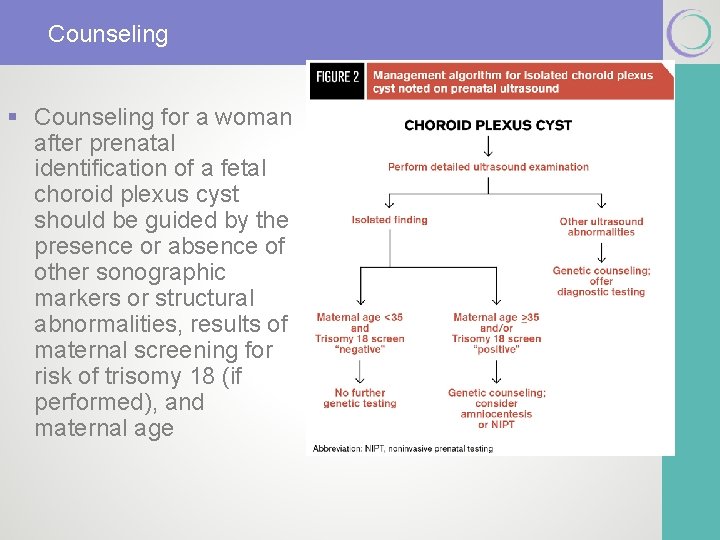
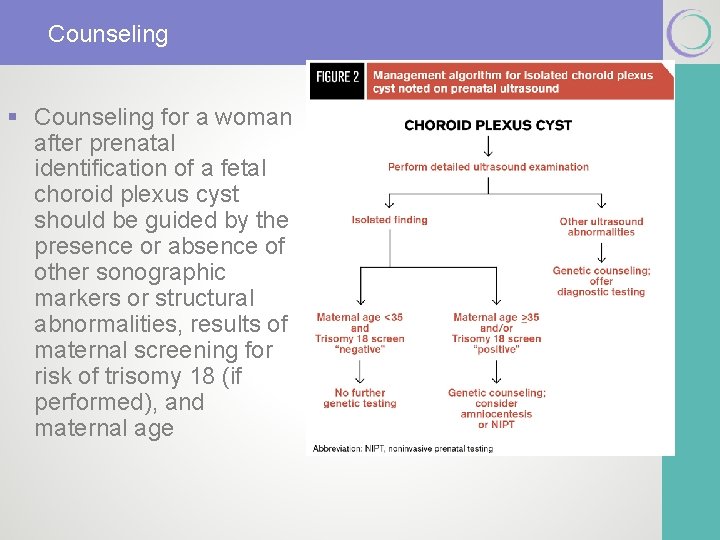
Counseling § Counseling for a woman after prenatal identification of a fetal choroid plexus cyst should be guided by the presence or absence of other sonographic markers or structural abnormalities, results of maternal screening for risk of trisomy 18 (if performed), and maternal age
Follow up § More than 90% of choroid plexus cysts resolve, most often by 28 weeks. § Studies evaluating neurodevelopmental outcomes in euploid children born after a prenatal diagnosis of choroid plexus cysts have not shown differences in neurocognitive ability, motor function, or behavior. § Therefore, neither serial antenatal ultrasounds nor post -natal evaluation are clinically useful.
Disclaimer § The practice of medicine continues to evolve, and individual circumstances will vary. This opinion reflects information available at the time of its submission for publication and is neither designed nor intended to establish an exclusive standard of perinatal care. This presentation is not expected to reflect the opinions of all members of the Society for Maternal-Fetal Medicine. § These slides are for personal, non-commercial and educational use only
Disclosures § This opinion was developed by the Publications Committee of the Society for Maternal Fetal Medicine with the assistance of Stanley M. Berry, MD, Joanne Stone, MD, Mary Norton, MD, Donna Johnson, MD, and Vincenzo Berghella, MD, and was approved by the executive committee of the society on March 11, 2012. Dr Berghella and each member of the publications committee (Vincenzo Berghella, MD [chair], Sean Blackwell, MD [vice-chair], Brenna Anderson, MD, Suneet P. Chauhan, MD, Jodi Dashe, MD, Cynthia Gyamfi-Bannerman, MD, Donna Johnson, MD, Sarah Little, MD, Kate Menard, MD, Mary Norton, MD, George Saade, MD, Neil Silverman, MD, Hyagriv Simhan, MD, Joanne Stone, MD, Alan Tita, MD, Michael Varner, MD) have submitted a conflict of interest disclosure delineating personal, professional, and/or business interests that might be perceived as a real or potential conflict of interest in relation to this publication.