Small for gestational age SGA or IUGR Definition




- Slides: 24
Small for gestational age (SGA) or IUGR
Definition; SGA or IUGR is considered when the weight of baby is below the 5 th percentile of growth for gestational age. IUGR is present when fetal growth stops and, with time, falls below the 5 th percentile of growth for gestational age or when growth proceeds slowly but the absolute size remains less than the 5 th percentile.
Causes: I. Fetal causes: 1. Chromosomal abnormalities (Trisomies). 2. Chronic fetal infections (syphilis, rubella). 3. Congenital abnormalities. 4. Radiation. 5. Multiple gestation.
II. Placental causes: 1. Placental tumors. 2. Placental separation. 3. Twin-twin transfusion syndrome. 4. Placental infarction.
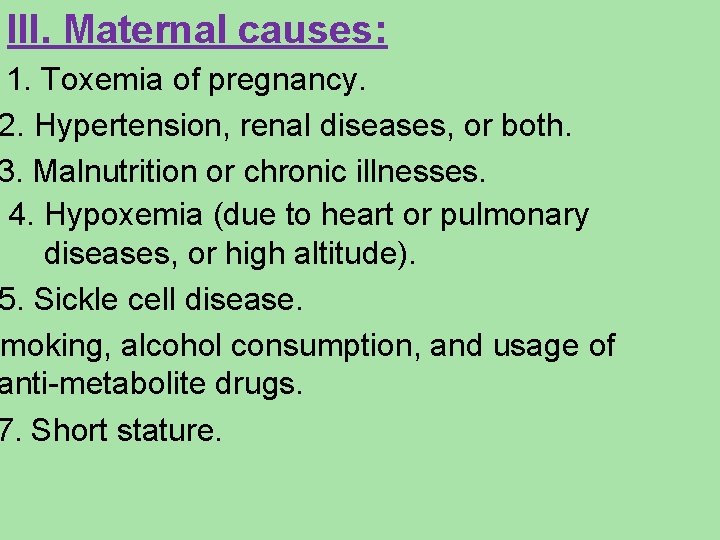
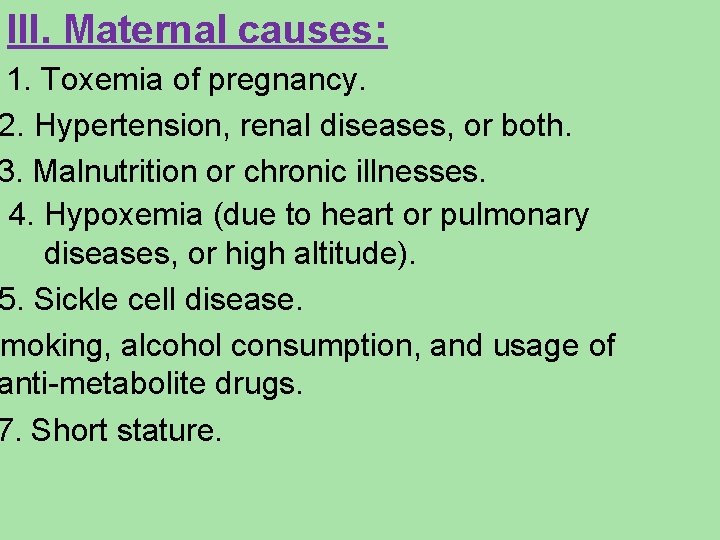
III. Maternal causes: 1. Toxemia of pregnancy. 2. Hypertension, renal diseases, or both. 3. Malnutrition or chronic illnesses. 4. Hypoxemia (due to heart or pulmonary diseases, or high altitude). 5. Sickle cell disease. Smoking, alcohol consumption, and usage of anti-metabolite drugs. 7. Short stature.
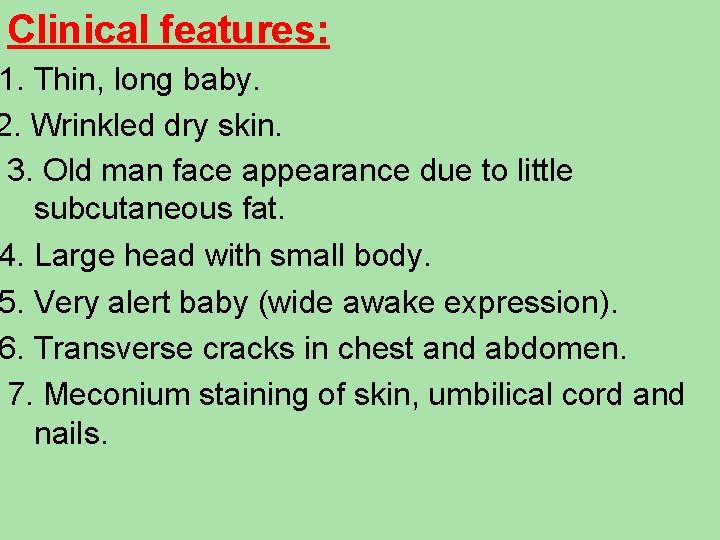
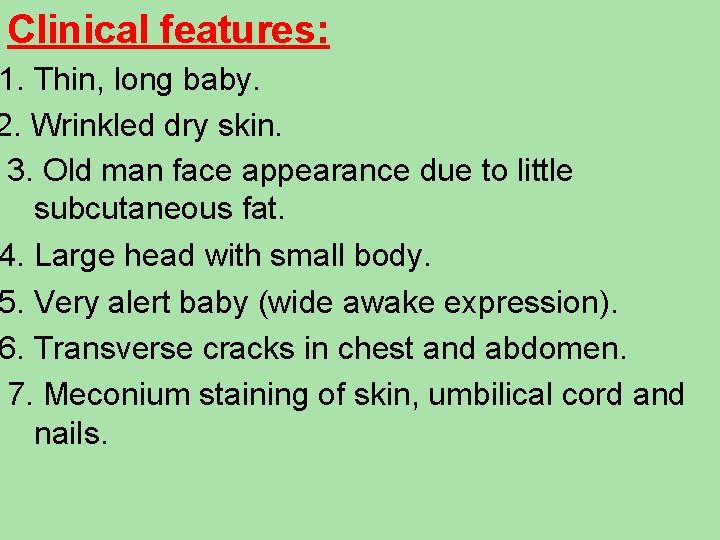
Clinical features: 1. Thin, long baby. 2. Wrinkled dry skin. 3. Old man face appearance due to little subcutaneous fat. 4. Large head with small body. 5. Very alert baby (wide awake expression). 6. Transverse cracks in chest and abdomen. 7. Meconium staining of skin, umbilical cord and nails.



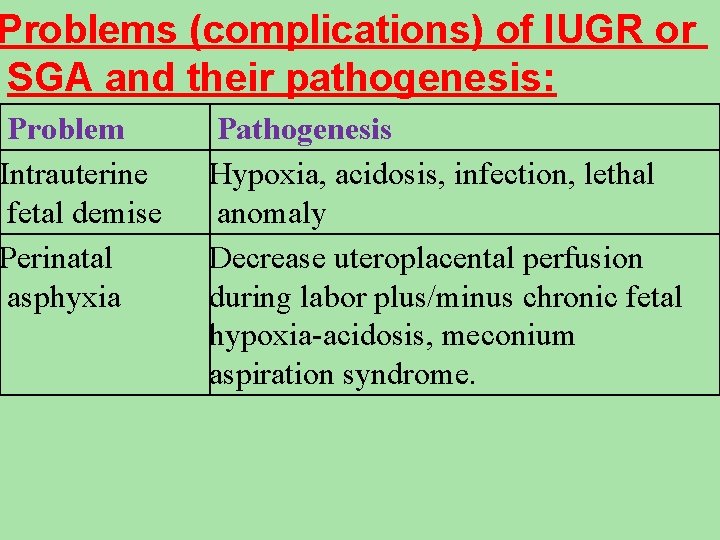
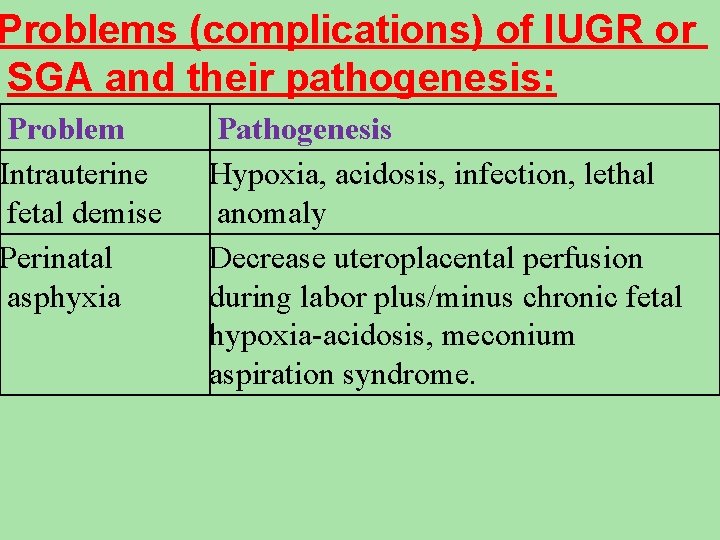
Problems (complications) of IUGR or SGA and their pathogenesis: Problem Intrauterine fetal demise Perinatal asphyxia Pathogenesis Hypoxia, acidosis, infection, lethal anomaly Decrease uteroplacental perfusion during labor plus/minus chronic fetal hypoxia-acidosis, meconium aspiration syndrome.
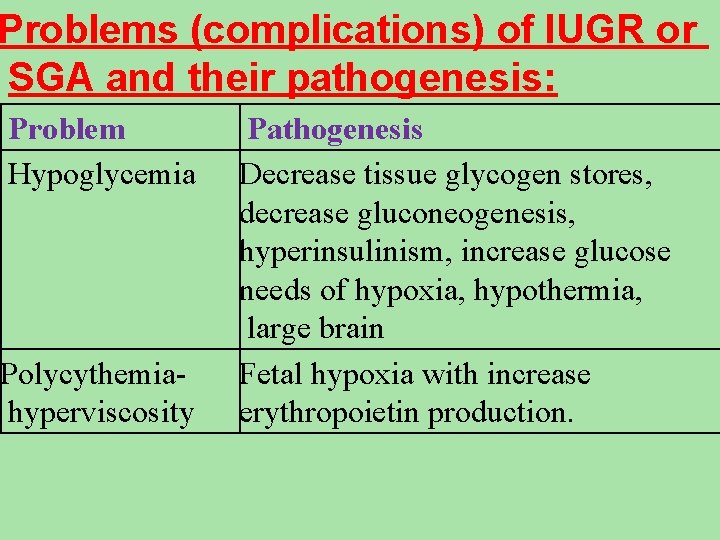
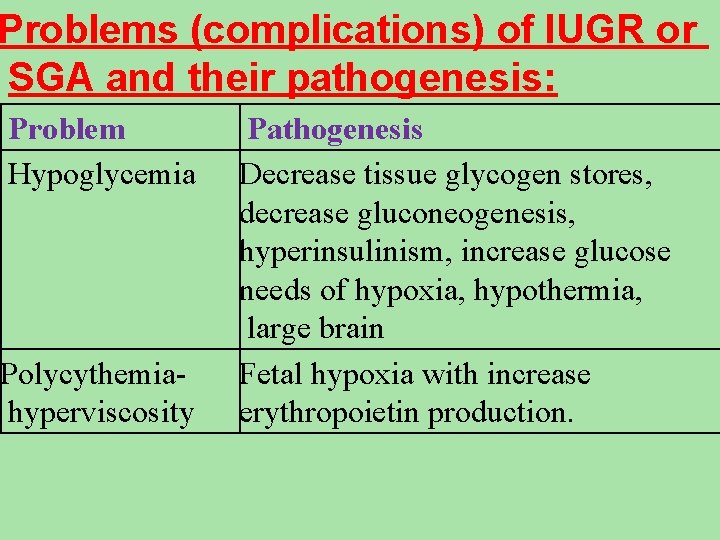
Problems (complications) of IUGR or SGA and their pathogenesis: Problem Hypoglycemia Polycythemiahyperviscosity Pathogenesis Decrease tissue glycogen stores, decrease gluconeogenesis, hyperinsulinism, increase glucose needs of hypoxia, hypothermia, large brain Fetal hypoxia with increase erythropoietin production.
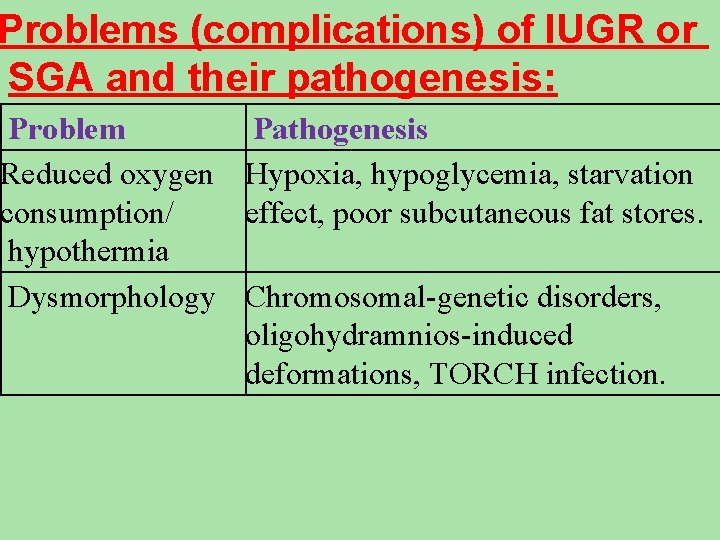
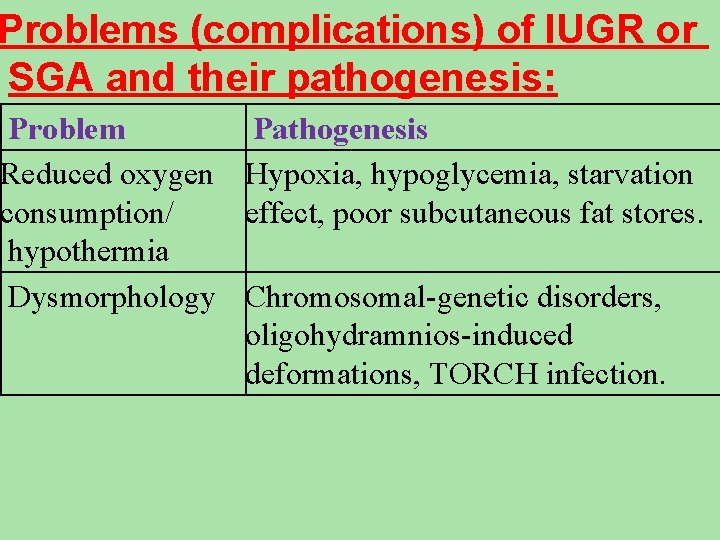
Problems (complications) of IUGR or SGA and their pathogenesis: Problem Pathogenesis Reduced oxygen Hypoxia, hypoglycemia, starvation consumption/ effect, poor subcutaneous fat stores. hypothermia Dysmorphology Chromosomal-genetic disorders, oligohydramnios-induced deformations, TORCH infection.
Management of IUGR: Its directed to the complications of IUGR especially perinatal asphyxia, polycythemia, hypoglycemia, and hypothermia in addition to the nutritional support.
Outcome (prognosis) of IUGR or SGA Its depend on the cause of IUGR and associated complications after birth. Fetuses subjected to chronic intrauterine hypoxia as a result of uteroplacental insufficiency are at an increased risk of birth asphyxia, polycythemia and hypoglycemia. Fetuses with IUGR resulting from chromosomal or multiple congenital anomaly syndromes have poor outcomes depend on the prognosis of these syndromes.
Fetuses born to small mothers or fetuses with poor nutritional intake usually do well and may catch-up growth after birth.
Large for gestational age Is birth weight above the 90 th centile or 2 standard deviations above the mean body weight for gestational age (> 4000 g). These infants are usually born at term, but they might be preterm with weight high for gestational age.
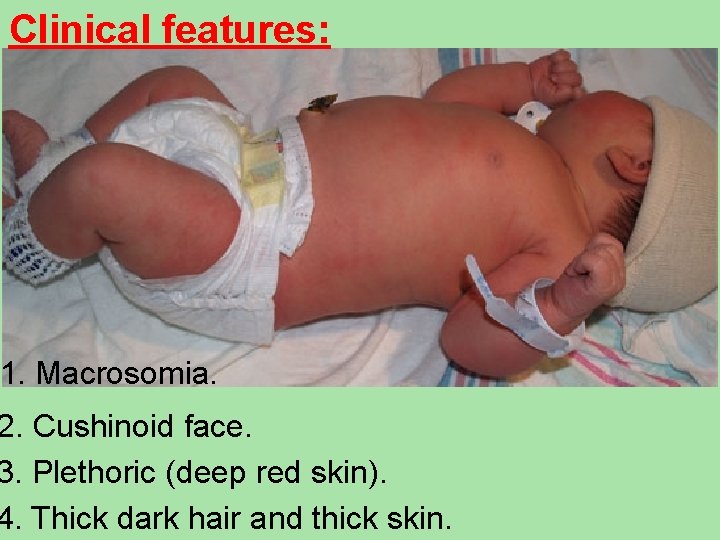
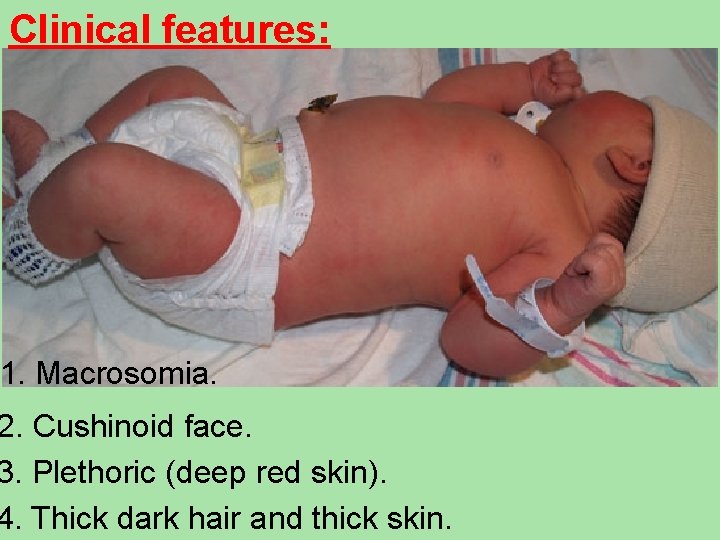
Clinical features: 1. Macrosomia. 2. Cushinoid face. 3. Plethoric (deep red skin). 4. Thick dark hair and thick skin.
Predisposing factors: 1. Maternal diabetes mellitus. 2. Maternal obesity. 3. Old age mothers. Complications; ncreased incidence of birth injuries especially vical and brachial plexus injuries, fractures icle, subdural hemorrhage, phrenic nerve h diaphragmatic paralysis, and ecchymosis of face and head.
2. Intellectual and mental retardations. 3. Congenital anomalies (especially of the heart). Severe hypoglycemia due to exposure to high cose in utero which causes ia of islets cells of pancrease ding to hyperinsulinism. 5. Hyperbilirubinemia.
Management: heck blood glucose levels and start feeding. glucose as early as possible to avoid glycemia and treat hypoglycemia when present. 2. Check serum calcium and treat hypocalcaemia when present. 3. Detect any congenital anomalies. 4. Treat jaundice. 5. Careful examination for birth injuries.
Post-term infants "postmaturity" Definition: Post-term infants are those born after 42 wk of gestation regardless of birth wt. Causes are unknown.
Clinical features: 1. Increased birth weight. 2. Absence of lanugo hair. 3. Decreased or absent vernix caseosa. 4. Long nails, abundant scalp hair, with white desquamating skin. 5. Increased alertness. 6. Meconium stained skin, umbilical cord and amniotic fluid.

Treatment: 1. Careful obstetric monitoring. n of labor or cesarean section ated in old primigravidas who go more than 2 -4 wk beyond term. matic treatment for meconium aspiration pneumonia or HIE Prognosis: Significant increase in the mrtality rate (3 times more than term infants) if delivery doelayed 3 wk or more beyond term.