SLEEP DISORDERS contents What is sleep Why is



















- Slides: 58
SLEEP DISORDERS

contents • What is sleep? • Why is sleep important? • Quick sleep facts • Cycle of sleep • Biological rhythms • Dreaming • Sleep disorders • Treatment of sleep disorders • Sleep hygiene • Resources

What is sleep? • Sleep is a dynamic and regulated set of behavioral and physiological states during which many processes vital to health and well-being take place.
Why is sleep important? • Sufficient sleep is essential for maintaining optimal physical health, mental and emotional functioning, and cognitive performance. • Inadequate sleep time and poor quality sleep interfere with quality of life and can be hazardous to health
Quick sleep facts • There are 5 phases of sleep: 1, 2, 3, 4, and REM, which is when we experience dreams. We spend about 50% of our sleep time in stage 2, 20% in REM sleep, and the other 30% in the other stages • Neurotransmitters control whether we are asleep or awake. • Experts say if you feel drowsy during the day, you haven’t had enough sleep. • Most adults need 7 -8 hours of sleep, teenagers about 9, and infants require about 16 hours a day.
Quick Sleep Facts • Sleep gives neurons that are used when we are awake a chance to shut down and repair themselves. Without sleep those neurons would be depleted of energy, polluted with byproducts, and normal cellular activities would begin to malfunction. • Sleeping may also help learning because it gives the brain a chance to exercise neural connections that might deteriorate otherwise.
Sleep cycle
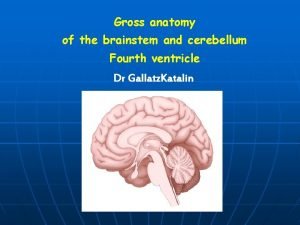
8 STAGES OF SLEEP • Sleep is characterized by two distinct cycles, • NREM sleep. Non-Rapid Eye Movement Sleep (NREM) is further classified into 4 stages: • Stage 1, • Stage 2, • Stage 3 and • Stage 4. • Rapid Eye Movement Sleep (REM) sleep • A normal human sleep cycle starts with NREM stage 1, stage 2, stage 3, stage 4 and progresses to REM. This cycle is repeated several times throughout the night (between 4 to 5 cycles). The duration for each cycle has been identified ranging between 60 to 90 minutes. The next section explains the characteristics of each of the four stages in detail.

9
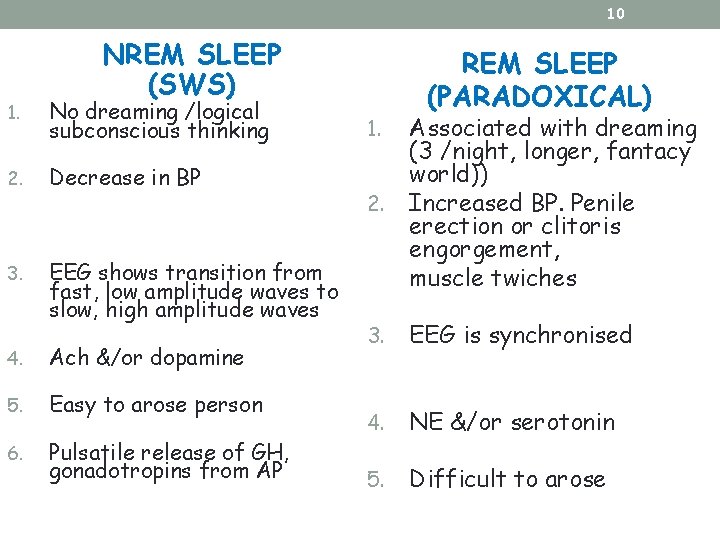
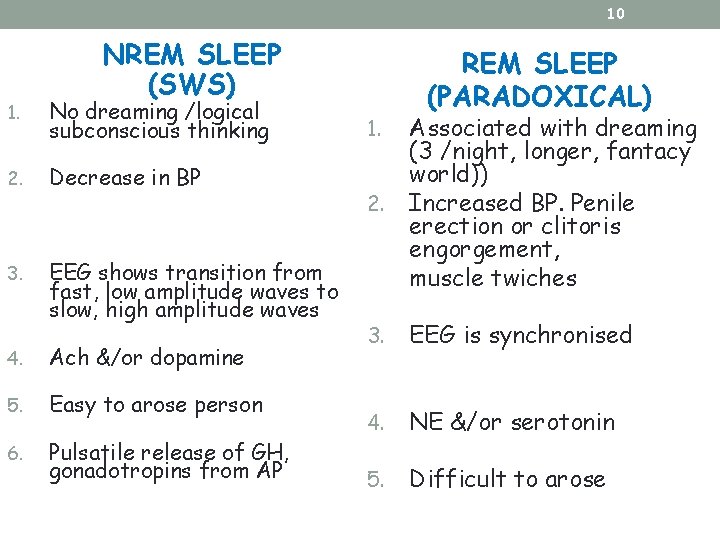
10 NREM SLEEP (SWS) 1. No dreaming /logical subconscious thinking 2. Decrease in BP 3. EEG shows transition from fast, low amplitude waves to slow, high amplitude waves 4. Ach &/or dopamine 5. Easy to arose person 6. Pulsatile release of GH, gonadotropins from AP REM SLEEP (PARADOXICAL) 2. Associated with dreaming (3 /night, longer, fantacy world)) Increased BP. Penile erection or clitoris engorgement, muscle twiches 3. EEG is synchronised 4. NE &/or serotonin 5. Difficult to arose 1.

EEG Sleep Patterns
12 Biological Rhythms • Biological processes related to sleep are influenced by the circadian rhythm and other biology rhythms. Homeostatic factors (factor S) and circadian factors (factor C) are both interact to determine the timing and quality of sleep.
13 Circadian Rhythms • Circadian Rhythm is one of the several intrinsic body rhythms modulated by the hypothalamus. • Circadian rhythm allows the brain to regulate periods of rest during sleep (equivalent to battery re-charging) and periods of high activity during the wakefulness (equivalent to battery discharging.
14 Other Biological Rhythms • The hypothalamus controls the body temperature cycles. Body temperature will increase during the course of the day and decrease during the night. • Melatonin secretion by the pineal gland controlled by the suprachiamastic nucleus is light-modulated. It is secreted maximally during the night. Prolactin, testosterone, and growth hormone also demonstrate circadian rhythms, with maximal secretion during the night. Melatonin influences sleep timing by modulating the amplitude of circadian signal and neuronal firing. Melatonin has multiple functions throughout the body, including regulation of immune function, hormone secretion, reproductive rhythms.

15 DREAMING • Dreams are the images, sounds, thoughts and feelings experienced during sleeping. There is a strong association with REM sleep. Scientific studies of dreams, also known as ONEIROLOGY, have shown that a person spends a total of six years dreaming (estimated at 2 hrs each night).
Dreams & Memory 16 • Study have shown that illogical locations, characters and dream flow may help the brain strengthen the linking and consolidation of semantic memories. These occur during REM sleep when the flow of information between the hippocampus and neocortex is reduced. One stage of memory consolidation is the linking of distant but related memories. • It is found that people all over the world dream of mostly the same things. Personal experiences from the last day or week are frequently incorporated into dreams • Emotions • Sexual content • Recurring dreams • Common themes • Relationship with mental illness
Sleep disorders

A sleep disorder is a medical condition of the sleep patterns of a person. ■ Sleep disorders are common serious under diagnosed treatable
Sleep problems can be associated with many conditions including: • Stress and environmental factors • Pregnancy • Menopause • Chronic pain • Major depression • Chronic illnesses such as cancer, cardio-pulmonary disease, and Alzheimer’s
Impaired Sleep and Adverse Health Outcomes • Adverse health outcomes resulting from insufficient sleep include physiological, behavioral / cognitive, emotional, and/or social responses. • Physiological outcomes include increased risk for obesity, hypertension, and impaired immune system functioning
Impaired Sleep and Adverse Health Outcomes • Inadequate sleep impacts behavior in children and adults and may result in impaired daytime functioning, including decreased school or work place performance due to decreased alertness, poor memory, and impaired problem solving. • Insufficient sleep may be a factor in sports related and automobile accidents. • Not enough sleep may lead to use of caffeine and other stimulants to maintain wakefulness

Sleep Disorders DSM-IV-TR • Primary Sleep Disorders- 1 -Dyssomnia 2 -Parasomnia • Secondary Sleep Disorders- - Sleep Disorder Related to Another Mental Disorder - Sleep Disorder Due to a General Medical Condition - Substance- Induced Sleep Disorder
Primary sleep disorders • DYSSOMNIA: Difficulty getting enough sleep or Problems in the timing of sleep “either too awake at night or too sleepy in the day. ” Subtypes: • Intrinsic (physiological or psychological cause): insomnia, narcolepsy, sleep apnea, PLMD. • Extrinsic (cause is outside the body): altitude, allergy, alcohol, noise, sleep deprivation. • Circadian Rhythm Disturbance: delayed sleep phase. jet travel, shift work,

• PARASOMNIA: Abnormal behavioral & physiological events during sleep • • Arousal Disorders: sleepwalking, sleep terrors (“night terrors”), confusional arousals • Sleep-Wake Transition Disorders: somniloquy, hypnic jerks, rhythmic movement disorder (pediatrics) • REM Parasomnias: RBD, nightmares, sleep paralysis • Other: bruxism, enuresis, SIDS
Secondary sleep disorder • MEDICAL-PSYCHIATRIC disorders: a sleep abnormality is a major symptom of the disorder, but not the primary problem: • Depression (short RL, high RD, insomnia) • Schizophrenia (long initial insomnia) • Alcoholism (REMS and SWS suppression) • Dementias (“sundowning”, RBD) • Infection (sleeping sickness, encephalitis)
Insomnia • Difficulty initiating sleep, maintaining sleep, &/or nonrestorative sleep for at least 1 month • Primary: insomnia is not related to other medical or psychiatric problems • Insomnia can be acute (short-term) or chronic (ongoing). • 60 million Americans report having insomnia frequently or for long periods of time. Insomnia increases with age and affects 40% of women and 30% of men

• Contributing Factors: • Medical factors, such as pain & physical discomfort and respiratory problems • High body temperature • Inactivity during the day • Psychological disorders • Stress • Unrealistic expectations regarding sleep • Poor bedtime habits or sleep hygiene • Rebound insomnia (sleeping pills)

• Treatments: • Prescription drugs (benzodiazepines) & Other drug options: antihistamines, Remeron, Trazedone • Relaxation training • Stimulus control procedures • Setting regular bedtime routines • Sleep restriction • Confronting unrealistic expectations about sleep • Vigorous daytime exercise, not exercising before sleep

Hypersomnia sleeping too much • Characteristics • Excessive sleepiness • Persists for 1 month or longer • prolonged sleep episodes or daytime sleep episodes occur almost daily
• Often due to: • Major Depressive Episode, Dysthymic Disorder with atypical features • Use of substances is less likely to produce hypersomnia than insomnia, but it can happen (e. g. , sleeping pills overdose) • causes • The cause sometimes can not be identified. • Treatment • Exercise when becoming sleepy

Restless Leg Syndrome • Neurological disorder characterized by unpleasant sensations in the legs and an uncontrollable urge to move when resting as an attempt to relieve these feelings. • Causes difficulty falling asleep • Cause unknown, difficult to treat
Narcolepsy • People affected by narcolepsy may experience several sleep “attacks” per day. These attacks may occur at any time of day, including during activities such as driving or even during a conversation. • Nacrolapsy is a neurological disorder that can begin at any age, but usually develops between the ages of 10 and 25 years old.

• Characteristics Sleep intrudes into wakefulness, causing clients to fall asleep almost instantly • Sleep is brief but refreshing • May also have sleep paralysis, sudden loss of strength, and hallucinations as fall asleep or awaken. • • Treatments: • Stimulants • Provigil • Antidepressants
Cataplexy • Neurological condition in which the person experiences sudden bilateral loss of muscle tone and falls, usually experienced right after a strong emotion (anger, fear, or excitement). Can last from seconds to minutes. • Can be a symptom of Narcolepsy (60 -100%) • Treatment: • Treated with antidepressants; imipramine or desipramine

Breathing-Related Sleep Disorder • Sleep is disrupted by a sleep-related breathing condition • Breathing is interrupted during sleep, producing numerous brief arousals during the night • Leads to excessive sleepiness during the day Characteristics Sleep disruption (excessive sleepiness or insomnia) • • Due to sleep-related breathing condition (e. g. , Obstructive Sleep Apnea Syndrome)
Treatment • In mild cases: weight loss, sleeping on one’s side, and avoiding hypnotics and alcohol • In more serious cases: a machine that provides continuous positive airway pressure • Surgery: Few benefits
Sleep Paralysis • A condition either at on set of sleep or at awaking when a person is aware of their surroundings, but not able to move. • Often associated with Narcolepsy. • Treatment: • Treated with antidepressants

Sleep Apnea • Sleep disorder that occurs when a person’s breathing is interrupted during sleep. They stop breathing repeatedly during their sleep, sometimes hundreds of times. • This means that the brain, and the rest of the body, may not get enough oxygen. • . Animal studies have shown that the lack of oxygen to the brain causes learning and memory impairment and neuronal death
• Signs: loud snoring, heavy sweating during the night, morning headaches, sleep attacks during the day Two types: • Obstructive Sleep Apnea (OSA), caused by blockage of the airway, usually when the soft tissue in the back of throat collapses during sleep. • Central Sleep Apnea (CSA), the brain fails to signal the muscles to breathe due to instability in the respiratory control center. Contributing Factors: more common in males, the obese, & middle to older age Prevalence: occurs in 10 -20% of population
Treatment of Sleep Apnea • Weight loss • Sleep on sides (and stomach) • CPAP (Continuous Positive Airway Pressure) prevents obstruction by soft-tissue and keeps airway open • Surgical intervention (e. g. , enlarged tonsils, deviated septum) • Avoid sedatives (which can prevent reawakening to breathe)

Circadian Rhythm Sleep Disorders • Inability to synchronize one’s circadian sleep-wake pattern with the sleep-wake schedule of the surrounding environment • Results in disrupted sleep – either insomnia or excessive sleepiness during the day • 2 types: • Jet lag type – sleep problems caused by rapidly crossing multiple time zones • Shift work type – sleep problems associated with night shift work or frequently changing shift work
Circadian Rhythm Sleep Disorders • Phase Shifts: • Delayed Sleep Phase Type – late sleep onset & late awakening • Advanced Sleep Phase Type – early sleep onset & early awakening • Treatments • Phase delays – moving bedtime later • Phase advances – moving bedtime earlier • Use of a bright light
Parasomnias • Disturbances in arousal and sleep stage transition that intrude into the sleep process • 2 types: • Those that occur during rapid eye movement (REM) sleep • Those that occur during non-rapid eye movement (NREM) sleep
Nightmares • Occurs during REM (dream) sleep • Extremely frightening dreams that interrupt sleep and interfere with daily functioning • Person readily awakens from dreams, has detailed recall, and rapidly becomes oriented and alert • Common in children (10 -50%), but not adults (5 -10%)
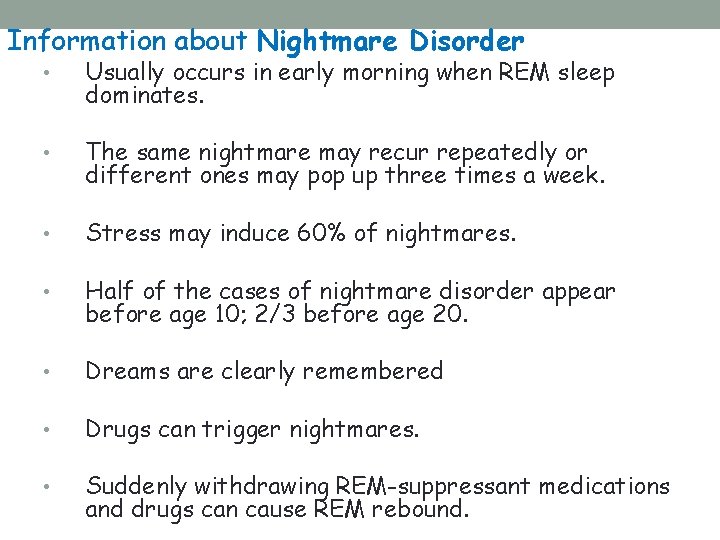
Information about Nightmare Disorder • Usually occurs in early morning when REM sleep dominates. • The same nightmare may recur repeatedly or different ones may pop up three times a week. • Stress may induce 60% of nightmares. • Half of the cases of nightmare disorder appear before age 10; 2/3 before age 20. • Dreams are clearly remembered • Drugs can trigger nightmares. • Suddenly withdrawing REM-suppressant medications and drugs can cause REM rebound.
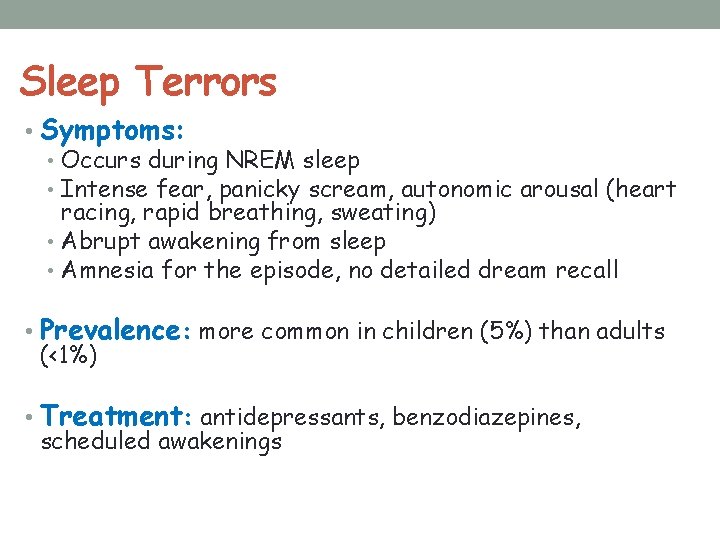
Sleep Terrors • Symptoms: • Occurs during NREM sleep • Intense fear, panicky scream, autonomic arousal (heart racing, rapid breathing, sweating) • Abrupt awakening from sleep • Amnesia for the episode, no detailed dream recall • Prevalence: more common in children (5%) than adults (<1%) • Treatment: antidepressants, benzodiazepines, scheduled awakenings
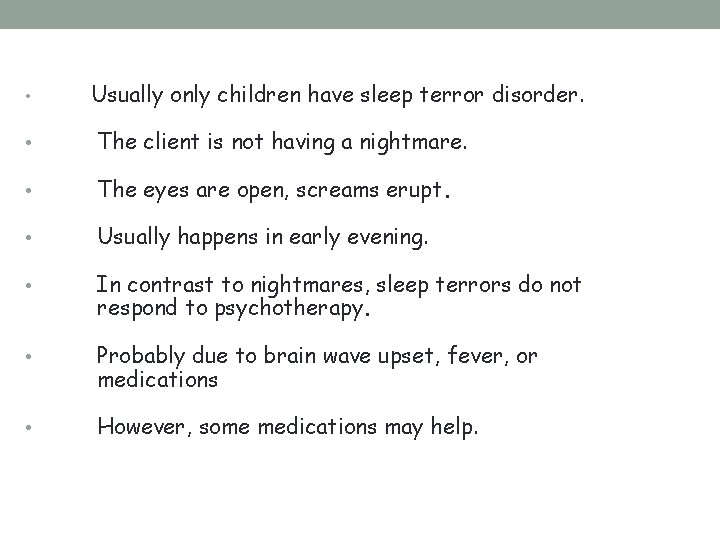
• Usually only children have sleep terror disorder. • The client is not having a nightmare. • The eyes are open, screams erupt. • Usually happens in early evening. • In contrast to nightmares, sleep terrors do not respond to psychotherapy. • Probably due to brain wave upset, fever, or medications • However, some medications may help.
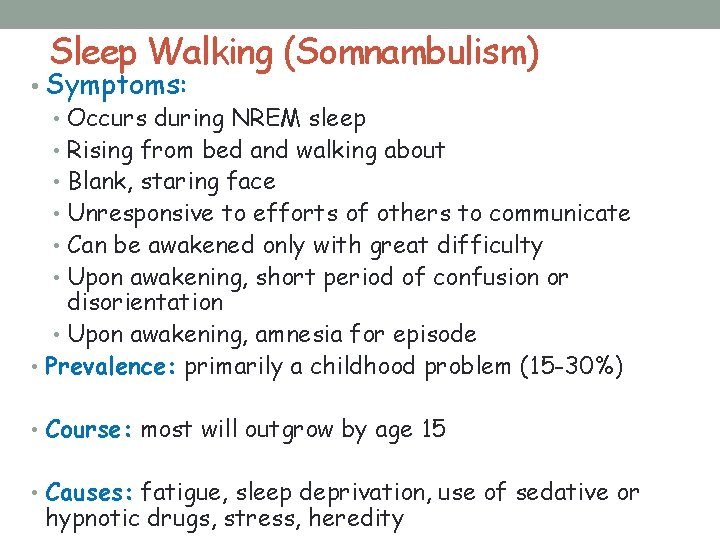
Sleep Walking (Somnambulism) • Symptoms: • Occurs during NREM sleep • Rising from bed and walking about • Blank, staring face • Unresponsive to efforts of others to communicate • Can be awakened only with great difficulty • Upon awakening, short period of confusion or disorientation • Upon awakening, amnesia for episode • Prevalence: primarily a childhood problem (15 -30%) • Course: most will outgrow by age 15 • Causes: fatigue, sleep deprivation, use of sedative or hypnotic drugs, stress, heredity
• Most sleepwalking children are psychologically normal. • Runs in families. • Begins between ages 6 and 12 and may be stressrelated. • Customarily sleepwalkers exhibit other delta-sleep interruptions. • At some time 1 -6% of children sleepwalk; of these, 15% do so occasionally. • Adult sleepwalking is far less common, usually worse and more chronic.
Treatment: • Relaxation techniques • Biofeedback training • Hypnosis. May need to sleep on the ground floor, have outside doors securely locked, and have car keys unavailable.

Other NREM Parasomnias • Sleep Talking • Bruxism (teeth grinding) • Nocturnal Eating Syndrome
Treatment of Sleep Problems • Behavior modification programs, hypnosis, or meditation may be effective • Self-prescribed over-the-counter sleep aids • Prescription medications
Sleep Medications Over the counter medications include: 1. antihistamines or drugs containing diphenhydramamine hydrochloride 2. diphenhydramine citrate 3. doxylamine succinate
Prescription Medications • Must be used at the direction of a physician • Often do not cure the cause of sleeping problems, just help alleviate the symptoms • Can be addictive / become drug dependent • May cause physical side effects • May interact with other medications or alcohol
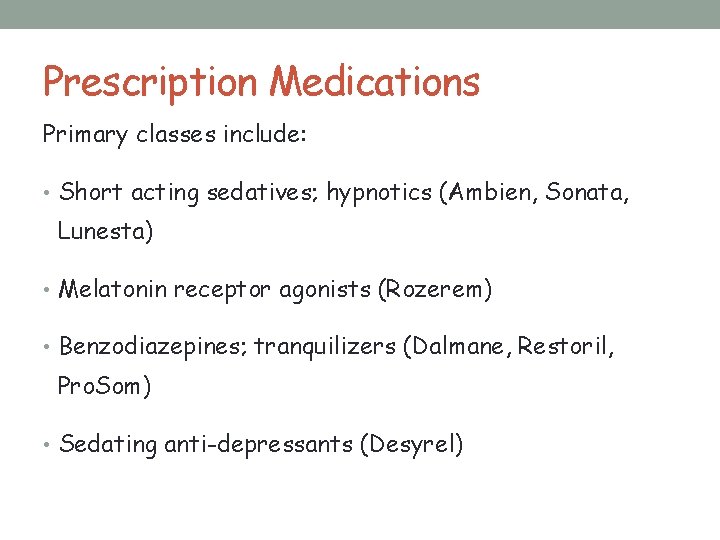
Prescription Medications Primary classes include: • Short acting sedatives; hypnotics (Ambien, Sonata, Lunesta) • Melatonin receptor agonists (Rozerem) • Benzodiazepines; tranquilizers (Dalmane, Restoril, Pro. Som) • Sedating anti-depressants (Desyrel)

Sleep Hygiene • Establish a set bedtime routine • Set a regular sleep and wake time • Go to bed when tired & get out of bed if unable to sleep within 15 minutes • Reduce noise, light, stimulation, & temperature in bedroom • Restrict activities in bed to those that help induce sleep • Avoid using caffeine & nicotine 6 hours before bedtime • Limit use of alcohol or tobacco • Do not exercise or participate in vigorous activities in the evening • Exercise during the day • Eat a balanced diet • Increase exposure to natural and bright light during the day • Educate self about normal sleep and sleep behavior

Resources • www. sleepfoundation. org • www. aasmnet. org • www. bettersleep. org • www. sleepresearchsociety. org • www. sleepandhealth. com • www. kidzzzsleep. org
 Hey bye bye
Hey bye bye Sleep disorders
Sleep disorders Remalteon
Remalteon Sleep disorders
Sleep disorders Dyssomnias
Dyssomnias Who analgesic ladder
Who analgesic ladder Dont ask why why why
Dont ask why why why Come sleep o sleep the certain knot of peace
Come sleep o sleep the certain knot of peace Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories David swan theme
David swan theme Why is sleep necessary
Why is sleep necessary Why we need sleep
Why we need sleep Career portfolio definition
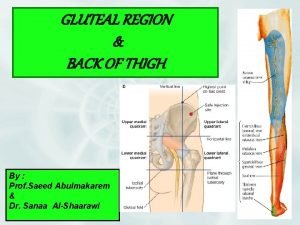
Career portfolio definition Deep perineal pouch contents
Deep perineal pouch contents Febrile non hemolytic transfusion reaction
Febrile non hemolytic transfusion reaction Ffp
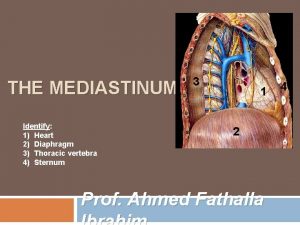
Ffp Middle mediastinum: contents mnemonic
Middle mediastinum: contents mnemonic Diagram of adductor canal
Diagram of adductor canal Superior mediastinum contents
Superior mediastinum contents The immortal life of henrietta lacks table of contents
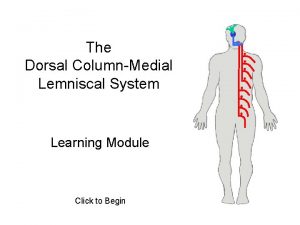
The immortal life of henrietta lacks table of contents Medial lemniscus
Medial lemniscus Posterior scapular region
Posterior scapular region Ark
Ark Comic book table of contents
Comic book table of contents Omental tuberosity of liver
Omental tuberosity of liver Mla table of contents
Mla table of contents Stylistic synonyms lexicology
Stylistic synonyms lexicology Cover page of school magazine
Cover page of school magazine Examples of continuous variables
Examples of continuous variables How to write an appendix
How to write an appendix Fresh frozen plasma contents
Fresh frozen plasma contents Posterior mediastinum contents
Posterior mediastinum contents Pericardium and mediastinum
Pericardium and mediastinum Indicative and informative verbs
Indicative and informative verbs Persepolis table of contents with page numbers
Persepolis table of contents with page numbers Persepolis table of contents
Persepolis table of contents Interactive notebook table of contents
Interactive notebook table of contents Cryoprecipitate
Cryoprecipitate Contents of interpeduncular fossa
Contents of interpeduncular fossa Spermatic cord
Spermatic cord Greater sciatic foramen
Greater sciatic foramen 5 ws of event management
5 ws of event management Contents of the middle mediastinum
Contents of the middle mediastinum Definition of mediastinum
Definition of mediastinum Carotid triangle contents
Carotid triangle contents Triangular space contents
Triangular space contents Curriculum vitaem
Curriculum vitaem Ctd module 3
Ctd module 3 Conclusion of cost audit
Conclusion of cost audit Civics interactive notebook
Civics interactive notebook City of ember poppy
City of ember poppy Fresh frozen plasma transfusion time
Fresh frozen plasma transfusion time Contents of air pollution
Contents of air pollution Magazine contents page analysis
Magazine contents page analysis Biceps brachii
Biceps brachii Relations of elbow joint
Relations of elbow joint