SLAC SNAC wrists Management Results Satyam Patel January





- Slides: 44
SLAC & SNAC wrists Management & Results Satyam Patel January 19 th, 2007
Overview • • Definitions Natural history Treatment Options Results
Definition • SLAC = Scapho-Lunate Advanced Collapse • SNAC = Scaphoid Nonunion Advanced Collapse • PRC = proximal row carpectomy • 4 CF = 4 corner (Capito. Hamate-Lunate-Triquetrum) Fusion
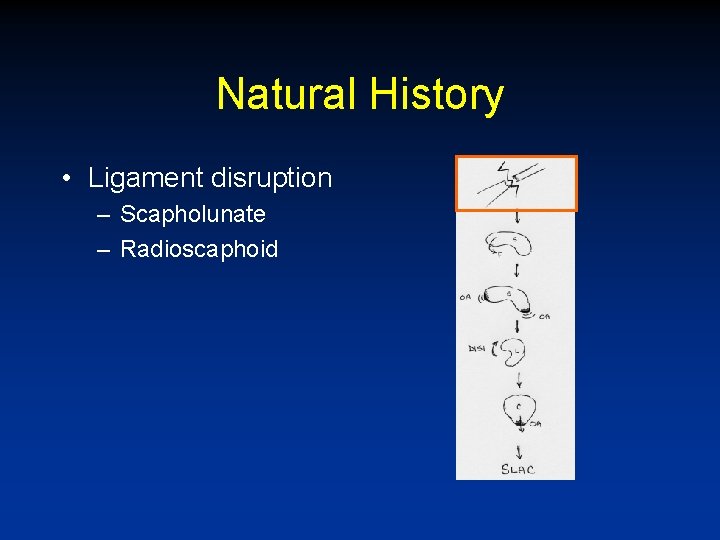
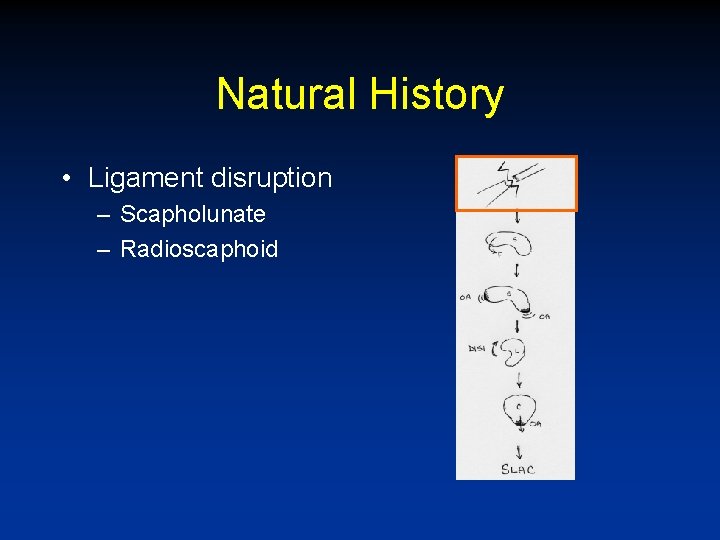
Natural History • Ligament disruption – Scapholunate – Radioscaphoid
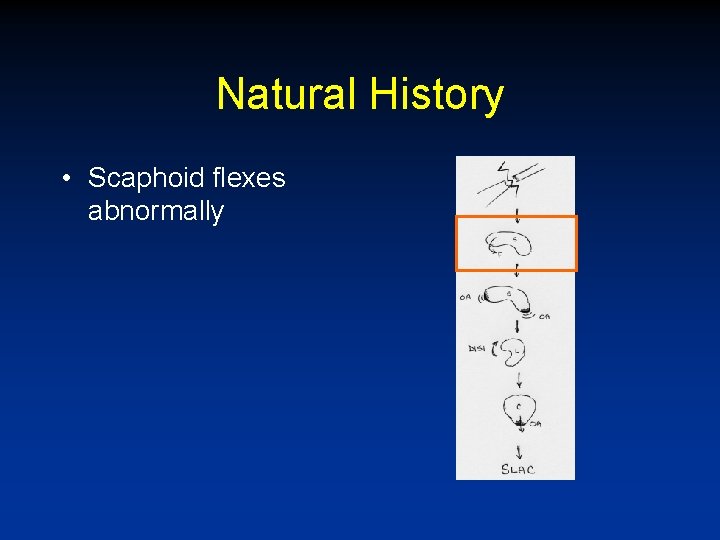
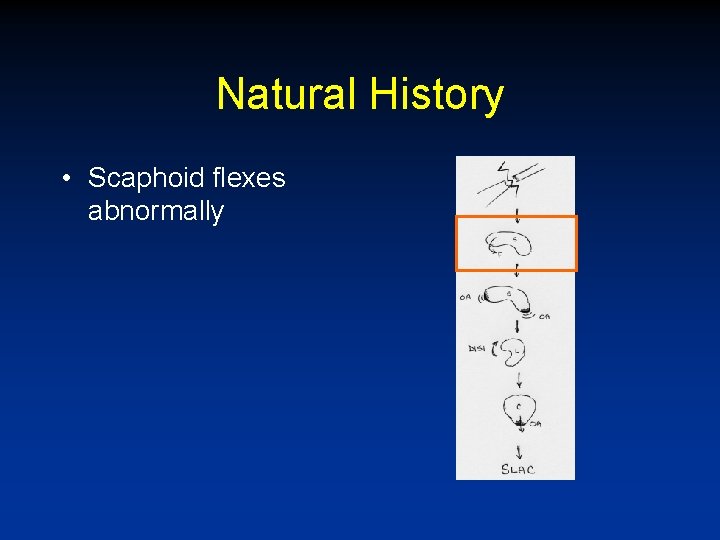
Natural History • Scaphoid flexes abnormally
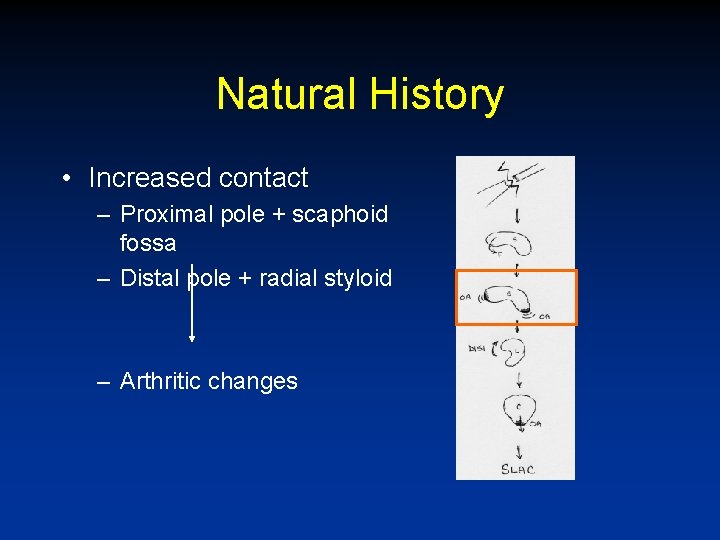
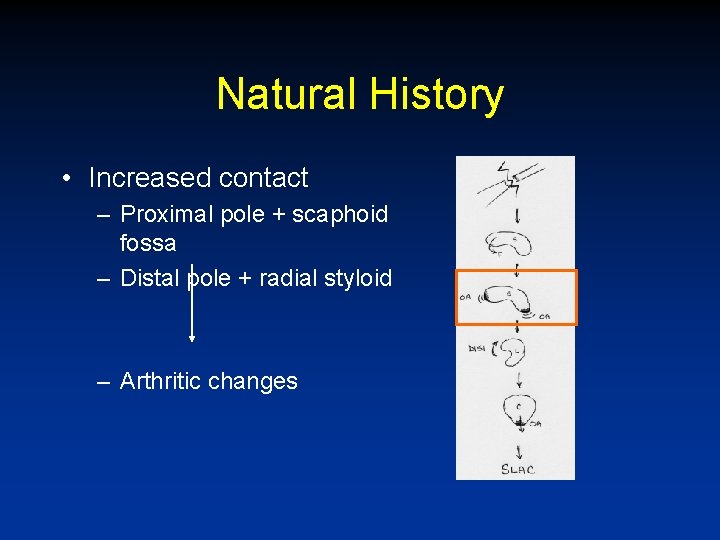
Natural History • Increased contact – Proximal pole + scaphoid fossa – Distal pole + radial styloid – Arthritic changes
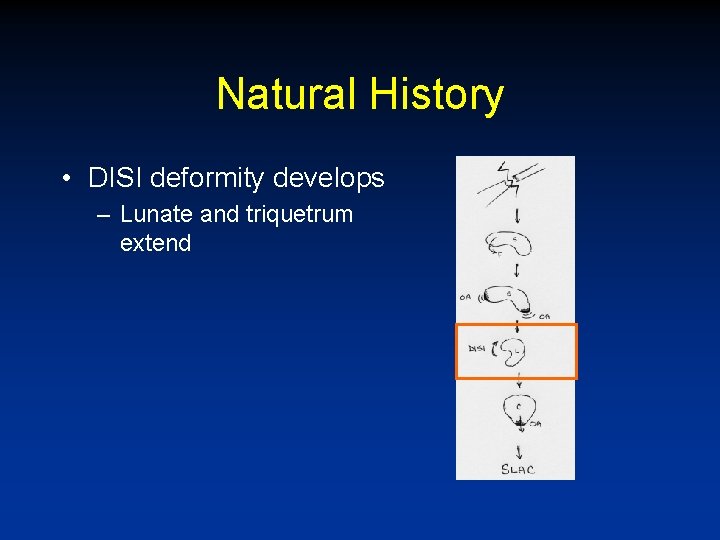
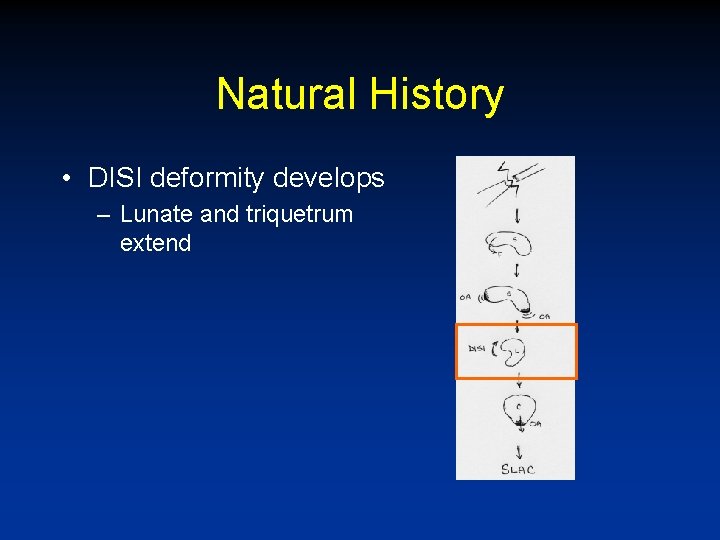
Natural History • DISI deformity develops – Lunate and triquetrum extend
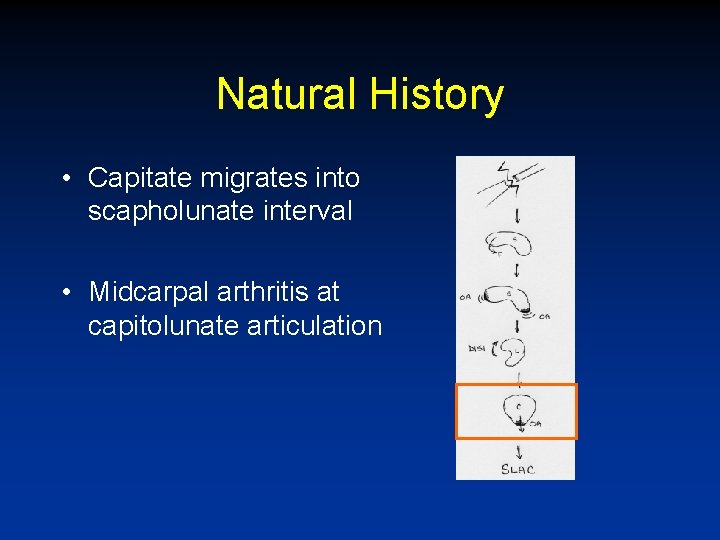
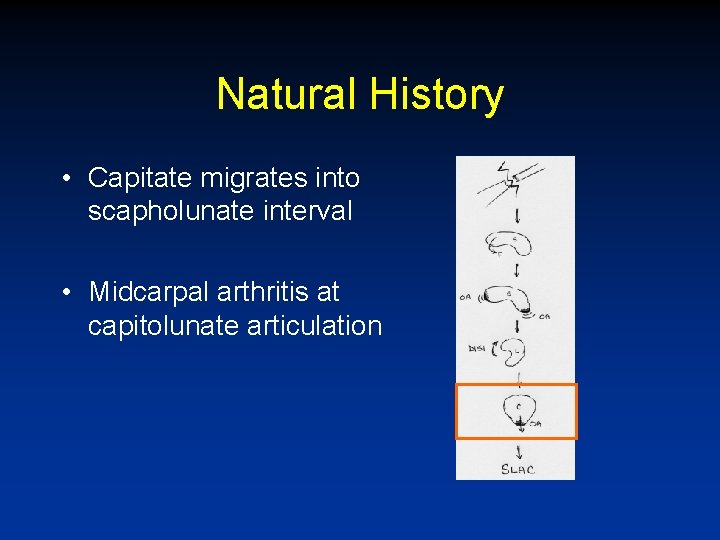
Natural History • Capitate migrates into scapholunate interval • Midcarpal arthritis at capitolunate articulation
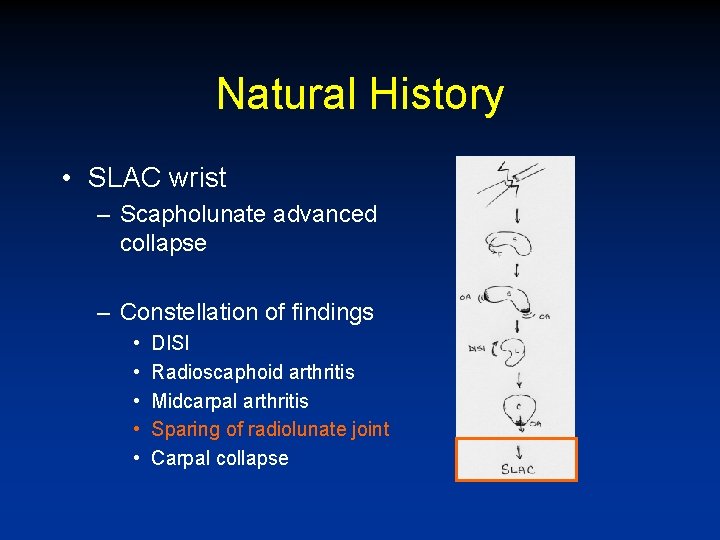
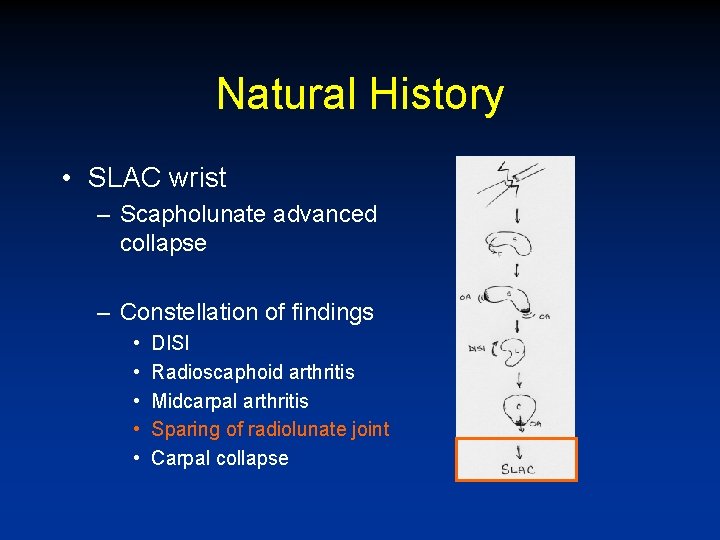
Natural History • SLAC wrist – Scapholunate advanced collapse – Constellation of findings • • • DISI Radioscaphoid arthritis Midcarpal arthritis Sparing of radiolunate joint Carpal collapse
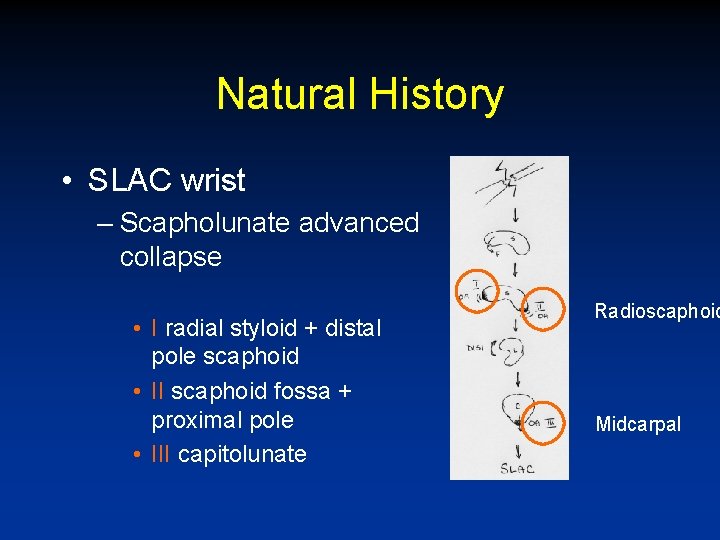
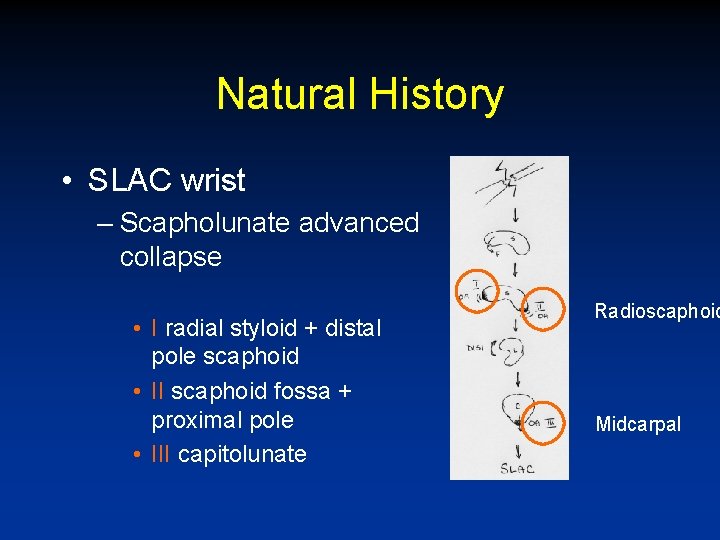
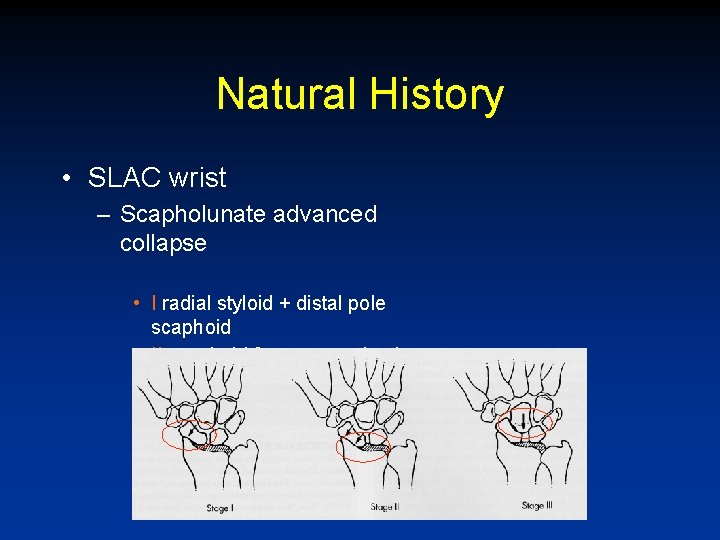
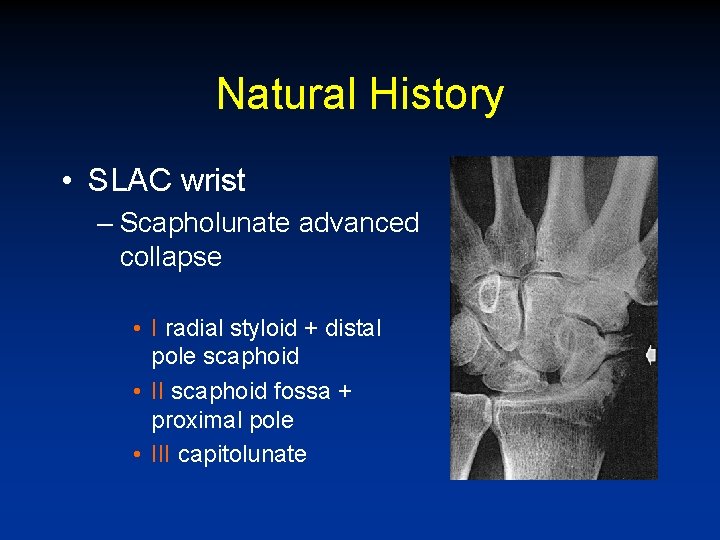
Natural History • SLAC wrist – Scapholunate advanced collapse • I radial styloid + distal pole scaphoid • II scaphoid fossa + proximal pole • III capitolunate Radioscaphoid Midcarpal
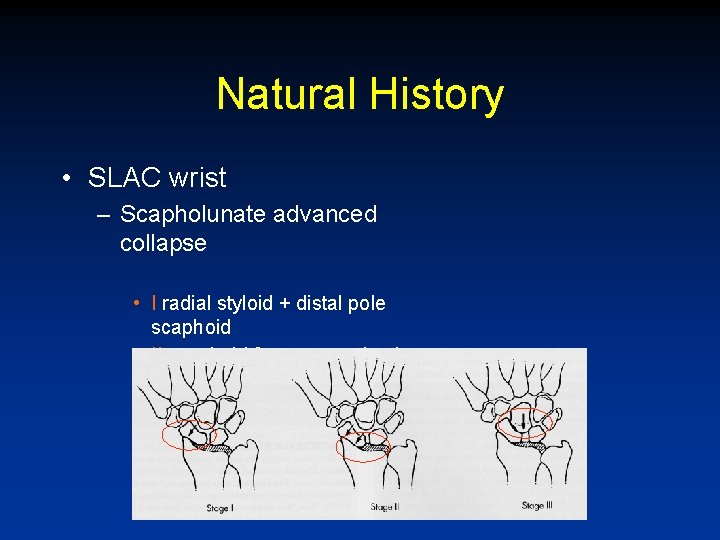
Natural History • SLAC wrist – Scapholunate advanced collapse • I radial styloid + distal pole scaphoid • II scaphoid fossa + proximal pole • III capitolunate
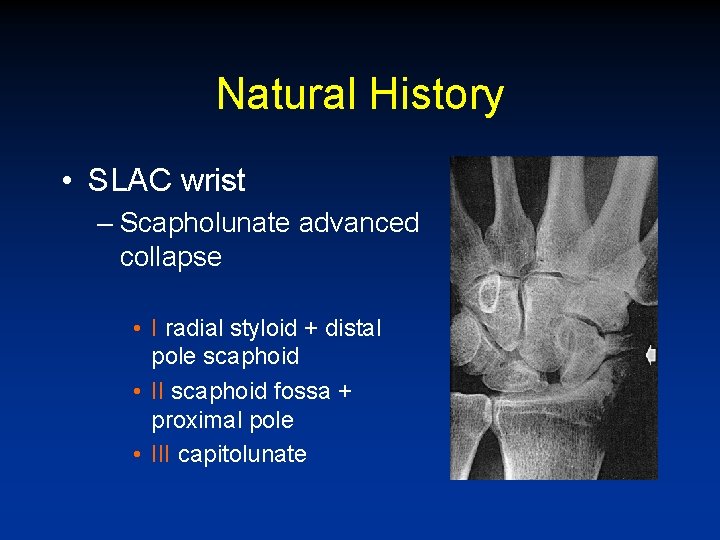
Natural History • SLAC wrist – Scapholunate advanced collapse • I radial styloid + distal pole scaphoid • II scaphoid fossa + proximal pole • III capitolunate
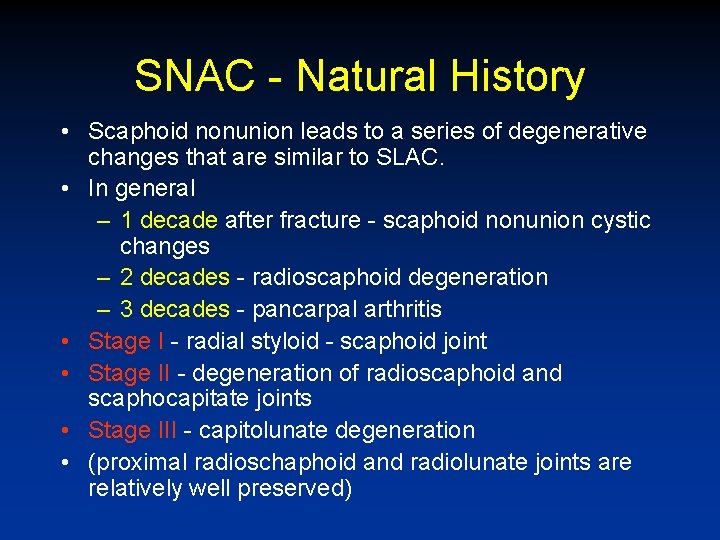
SNAC - Natural History • Scaphoid nonunion leads to a series of degenerative changes that are similar to SLAC. • In general – 1 decade after fracture - scaphoid nonunion cystic changes – 2 decades - radioscaphoid degeneration – 3 decades - pancarpal arthritis • Stage I - radial styloid - scaphoid joint • Stage II - degeneration of radioscaphoid and scaphocapitate joints • Stage III - capitolunate degeneration • (proximal radioschaphoid and radiolunate joints are relatively well preserved)
Treatment Options • Relevant factors – Patient age – Activity Level – State of Degeneration

Treatment Options • Conservative – – Activity modification Splinting Steroid injection NSAIDs
Treatment Options • Surgical – PIN neurectomy – Total or partial wrist arthrodesis – Proximal row carpectomy – Distraction arthroplasty – Total wrist arthroplasty
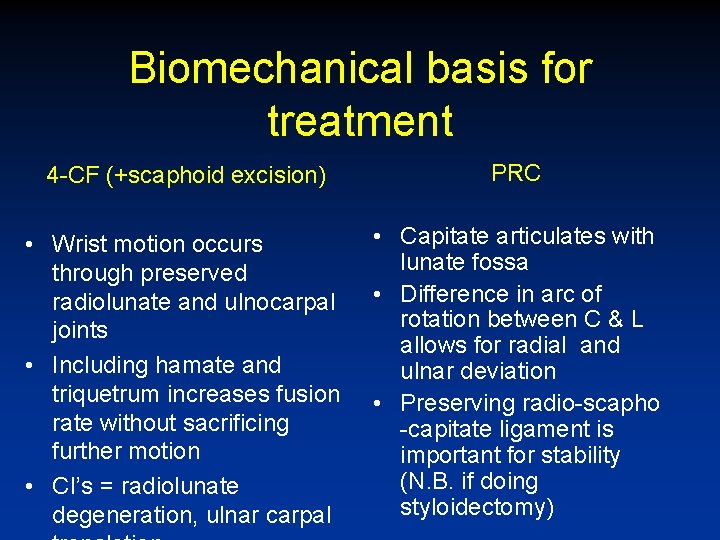
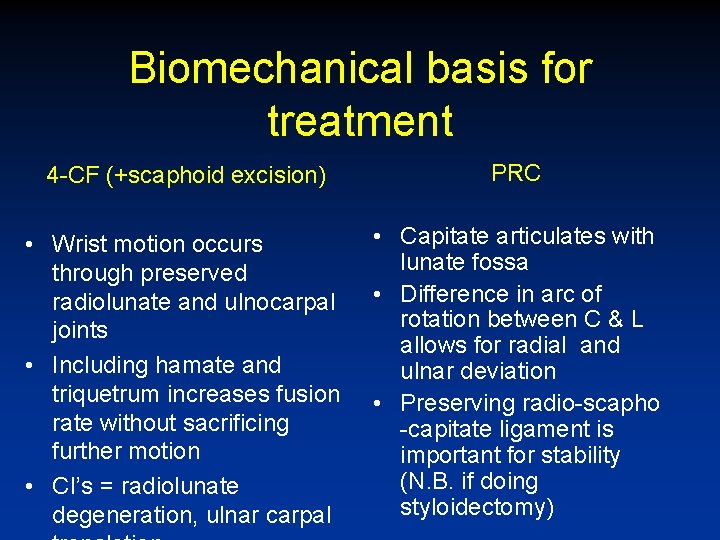
Biomechanical basis for treatment 4 -CF (+scaphoid excision) PRC • Wrist motion occurs through preserved radiolunate and ulnocarpal joints • Including hamate and triquetrum increases fusion rate without sacrificing further motion • CI’s = radiolunate degeneration, ulnar carpal • Capitate articulates with lunate fossa • Difference in arc of rotation between C & L allows for radial and ulnar deviation • Preserving radio-scapho -capitate ligament is important for stability (N. B. if doing styloidectomy)

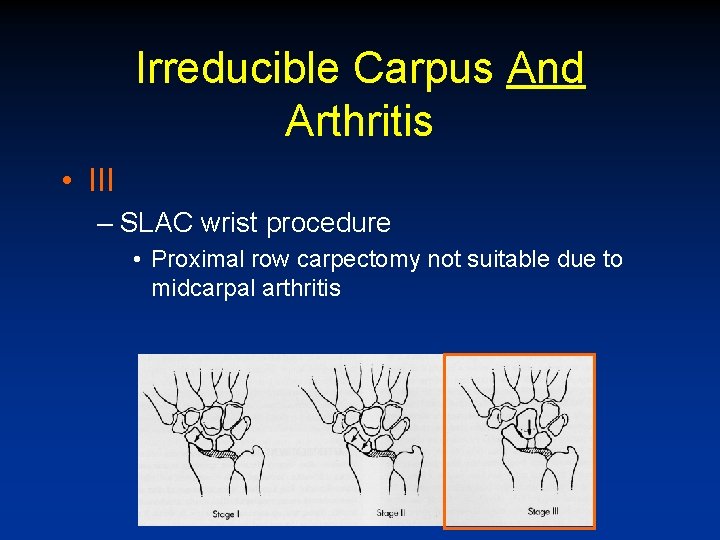
Irreducible Carpus And Arthritis • RECALL: • SLAC wrist – Scapholunate advanced collapse • I radial styloid + distal pole scaphoid • II scaphoid fossa + proximal pole • III capitolunate
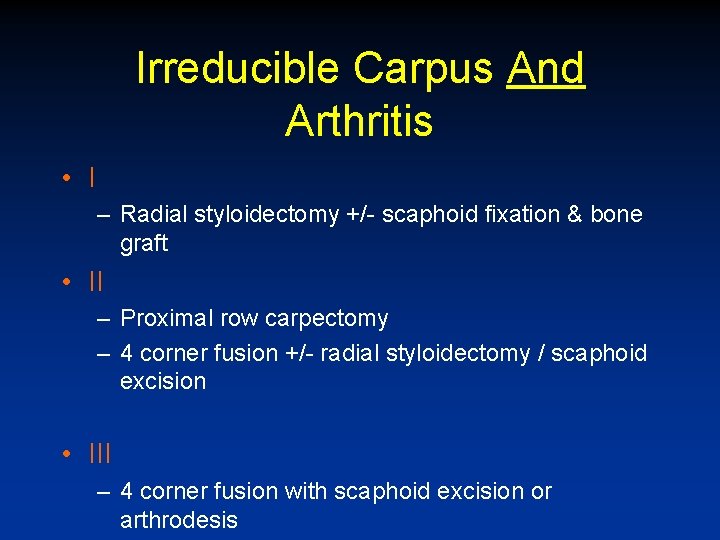
Irreducible Carpus And Arthritis • I – Radial styloidectomy +/- scaphoid fixation & bone graft • II – Proximal row carpectomy – 4 corner fusion +/- radial styloidectomy / scaphoid excision • III – 4 corner fusion with scaphoid excision or arthrodesis
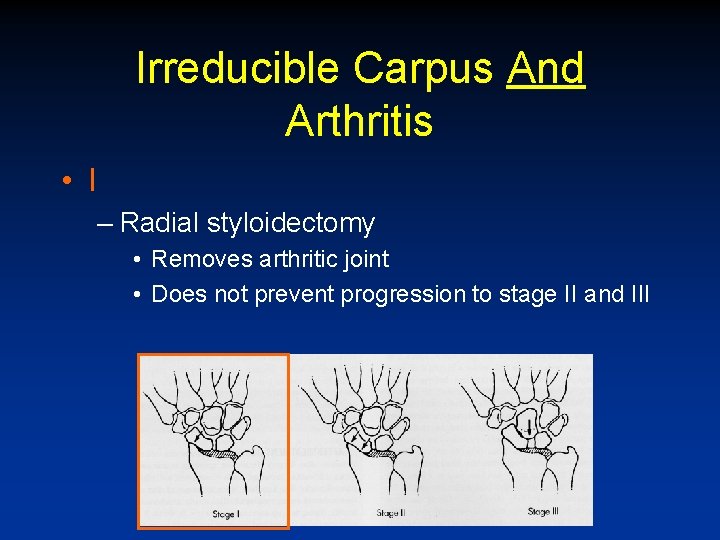
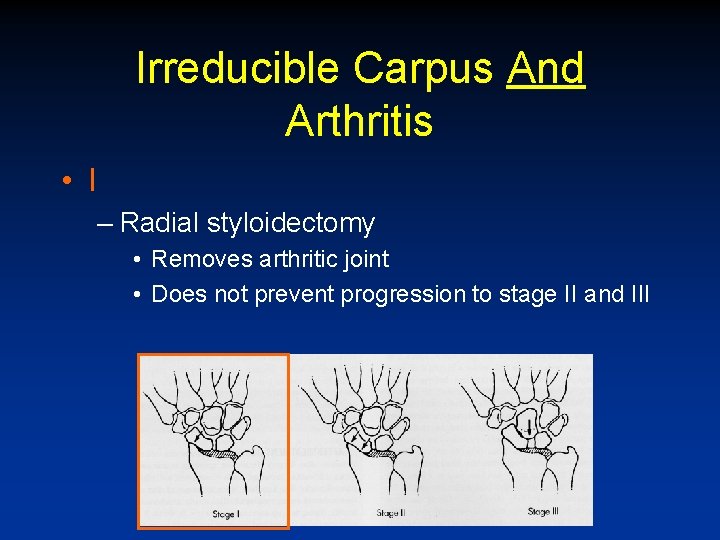
Irreducible Carpus And Arthritis • I – Radial styloidectomy • Removes arthritic joint • Does not prevent progression to stage II and III
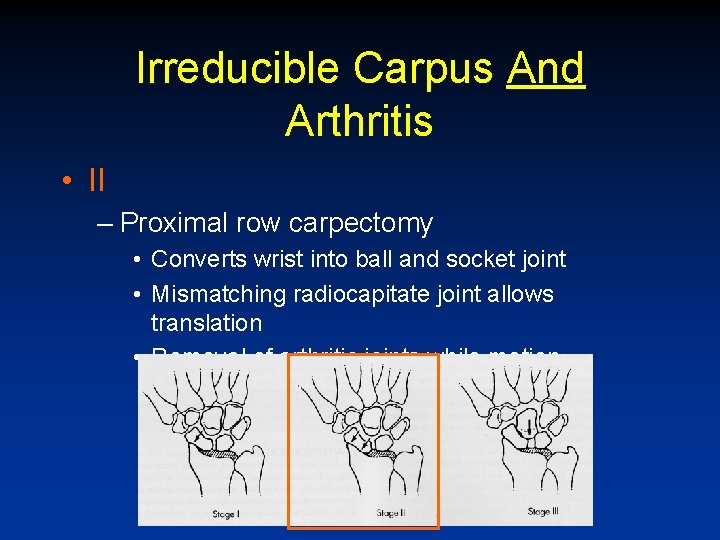
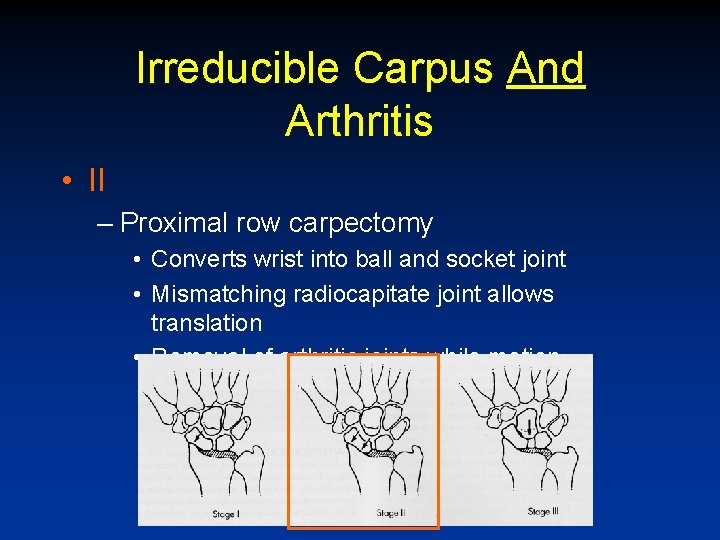
Irreducible Carpus And Arthritis • II – Proximal row carpectomy • Converts wrist into ball and socket joint • Mismatching radiocapitate joint allows translation • Removal of arthritic joints while motion maintained
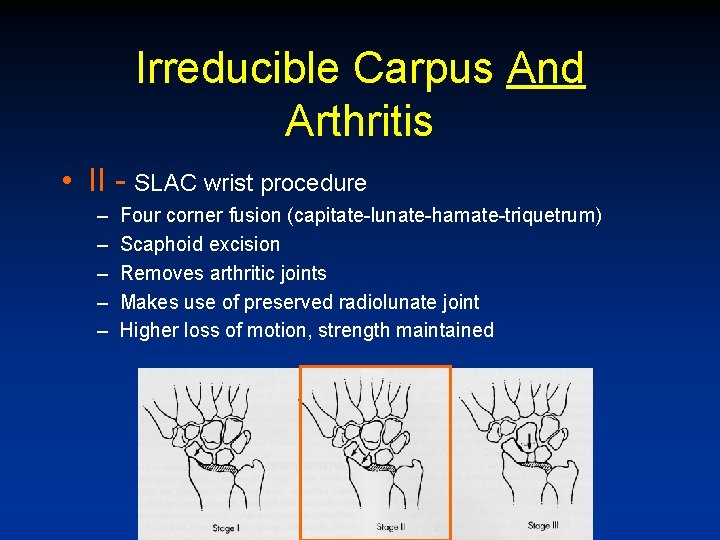
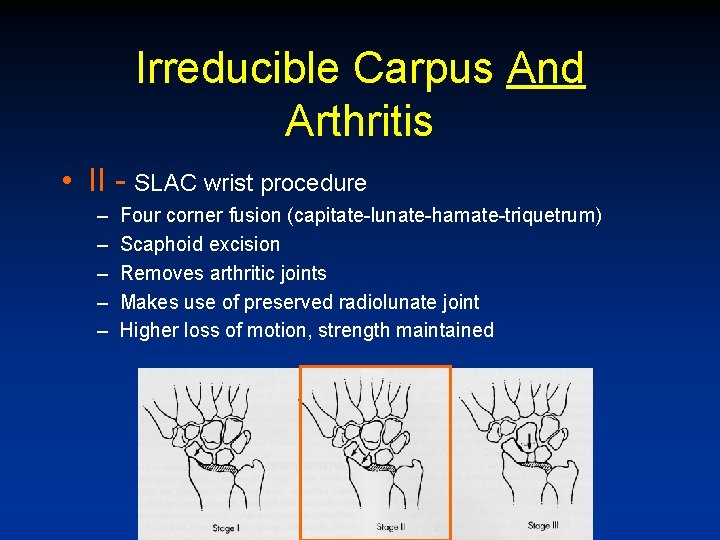
Irreducible Carpus And Arthritis • II - SLAC wrist procedure – – – Four corner fusion (capitate-lunate-hamate-triquetrum) Scaphoid excision Removes arthritic joints Makes use of preserved radiolunate joint Higher loss of motion, strength maintained
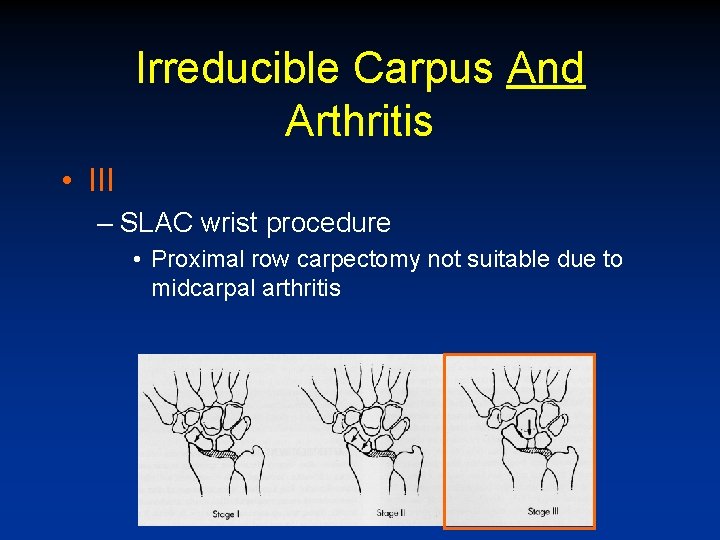
Irreducible Carpus And Arthritis • III – SLAC wrist procedure • Proximal row carpectomy not suitable due to midcarpal arthritis
Indications for total wrist arthrodesis • Diffuse arthritic change (capitate or lunate fossa involved) • Motion less than 30 / 30 • Contraindication = if wrist dorsiflexion is required for tenodesis (e. g. tetraplegic patients)
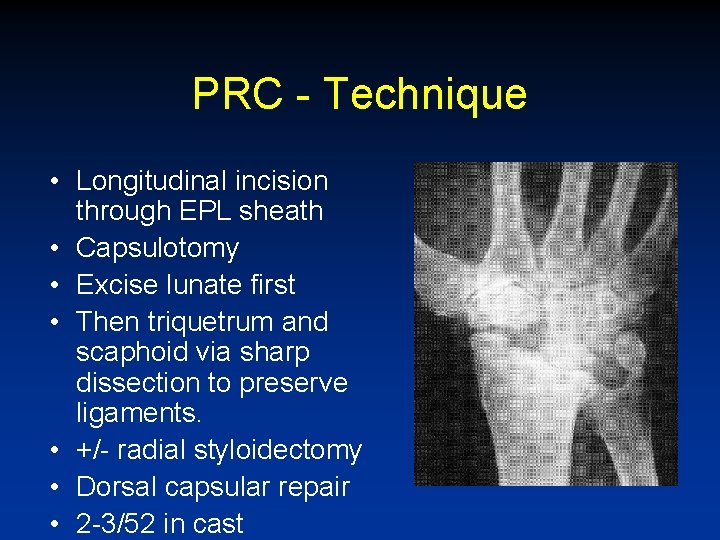
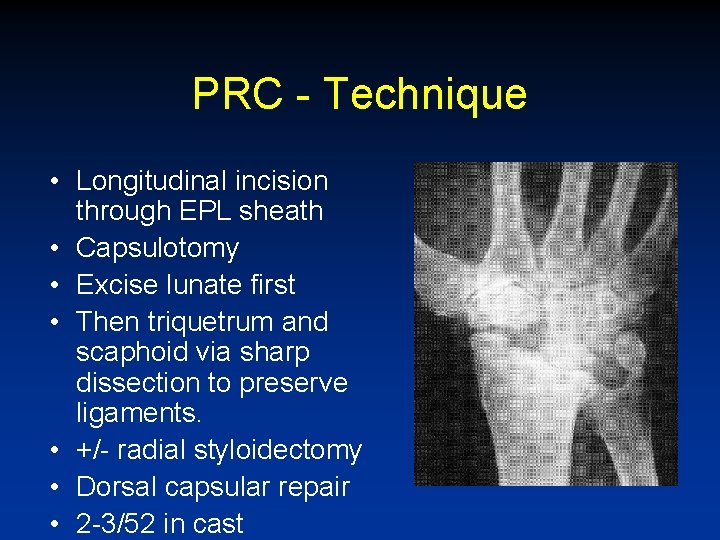
PRC - Technique • Longitudinal incision through EPL sheath • Capsulotomy • Excise lunate first • Then triquetrum and scaphoid via sharp dissection to preserve ligaments. • +/- radial styloidectomy • Dorsal capsular repair • 2 -3/52 in cast
PRC - variations • Pre-op arthroscopy to evaluate condition of cartilage • Temporary internal fixation with K-wires • dorsal capsule interposition • Radial styloidectomy • Proximal capitate excision (? ) • N. B. caution in pts < 35 y. o. , rheumatoid patients

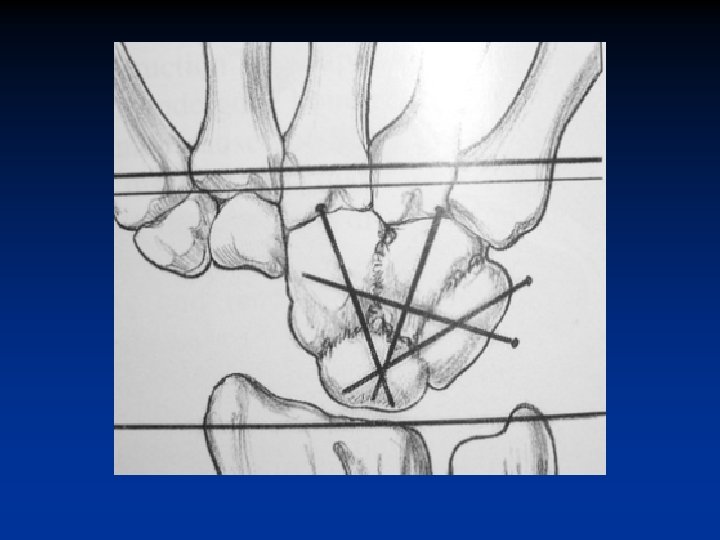
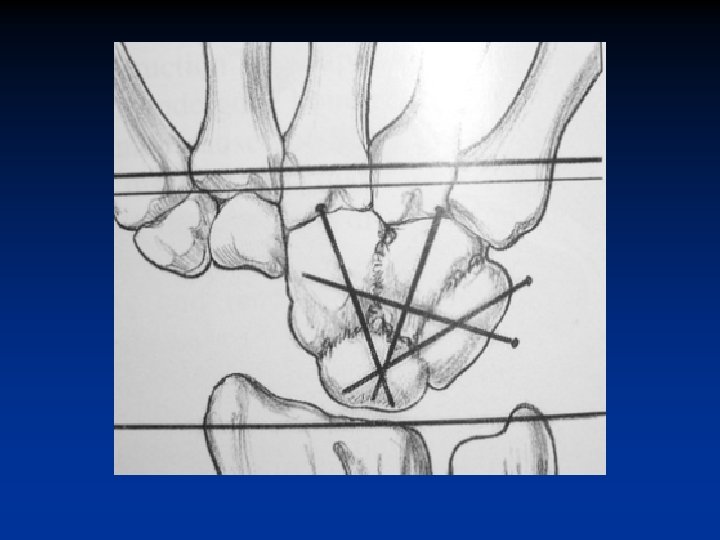
Technique SLAC Wrist Procedure Four-Corner-Fusion With Scaphoid Excision • Exposure as in PRC • Scaphoid excision • Radioscaphocapitate ligament preserved • Joints decorticated • ICBG or distal radius bone graft • Lunate reduced to capitate (slight flexion) • K-wires, staples, screws, “spider” plate • Avoid silastic scaphoid (synovitis)
Variations of 4 -corner fusion • Use of k-wires vs. use of spider plate – Trade-off between increased fusion rate and incidence of dorsal impingement – P. Stern • Excision of triquetrum (3 corner fusion / Capito-lunate fusion) – Better dorsiflexion in cadaveric study, no significant increase in ROM clinically thus far. – G. Bain, J. Calandruccio, R. Gelberman
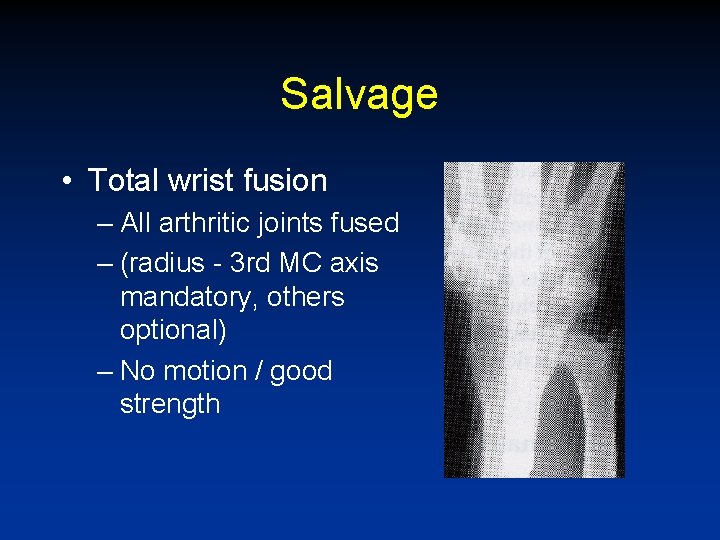
Salvage • Total wrist fusion – All arthritic joints fused – (radius - 3 rd MC axis mandatory, others optional) – No motion / good strength
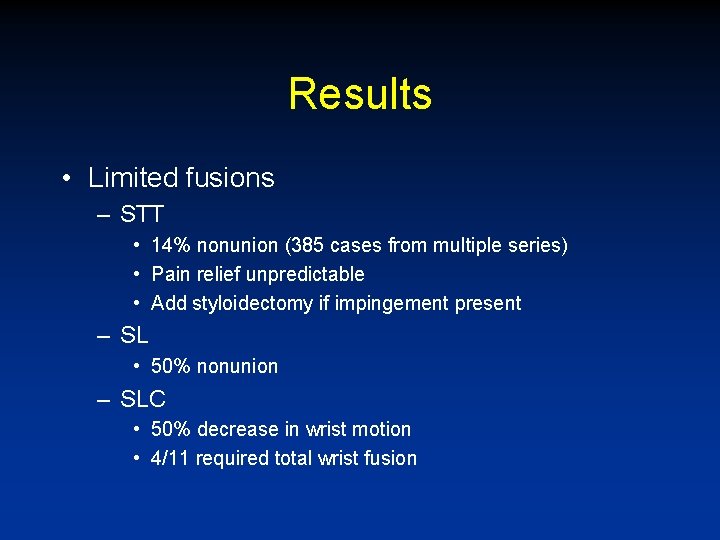
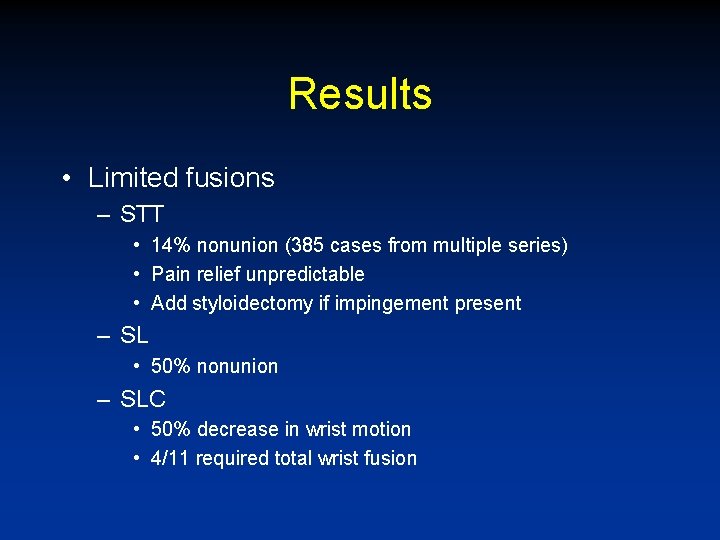
Results • Limited fusions – STT • 14% nonunion (385 cases from multiple series) • Pain relief unpredictable • Add styloidectomy if impingement present – SL • 50% nonunion – SLC • 50% decrease in wrist motion • 4/11 required total wrist fusion
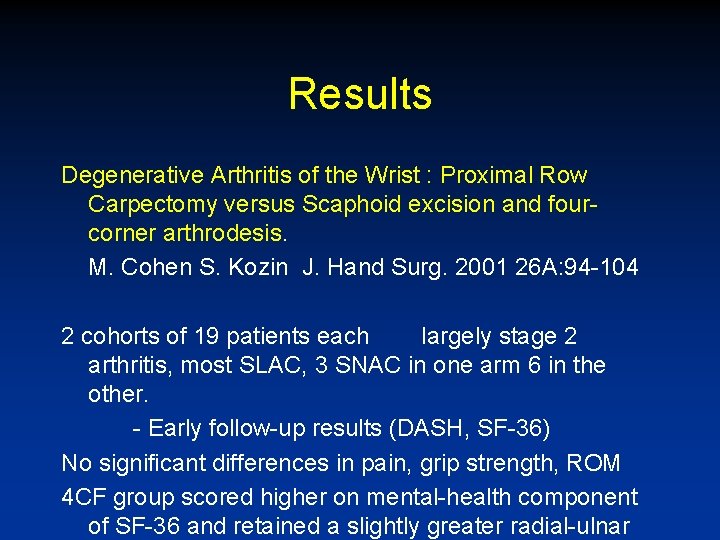
Results Degenerative Arthritis of the Wrist : Proximal Row Carpectomy versus Scaphoid excision and fourcorner arthrodesis. M. Cohen S. Kozin J. Hand Surg. 2001 26 A: 94 -104 2 cohorts of 19 patients each largely stage 2 arthritis, most SLAC, 3 SNAC in one arm 6 in the other. - Early follow-up results (DASH, SF-36) No significant differences in pain, grip strength, ROM 4 CF group scored higher on mental-health component of SF-36 and retained a slightly greater radial-ulnar
Results • Acta Orthop Belg 2006 – Salvage procedures for degenerative osteoarthritis of the wrist due to advanced carpal collapse – 63 patients - 19 fused, PRC 26, scaphoidectomy +4 CF 18 – PRC significantly better (DASH =16) – No significant differences between 4 CF and arthrodesis (DASH = 39, 45)
PRC - results • Jorgenson 22 PRC cases over 20 years • Increased ROM, subjective feeling of weakness • Scand J Plast Reconstr Surg & Hand Surg 2006 • 51 patients PRC between 1992 & 2002 11% required arthrodesis (9 patients) • 34 returned to work (avg. 6/12) • F 66% E 73% RD 74% • Grip 70% UD 76%
Results of 4 CF & scaphoidectomy • • • Ashmead et. al 44/12 100 patients E 32 deg F 42 deg (53%) Grip strength 80% 78/85 satisfied (would undergo operation again) • 3% nonunion rate • Dorsal impingement 13%
Results • Wrist fusion – 85% total pain relief – 65% return to former occupation Hastings and Silver
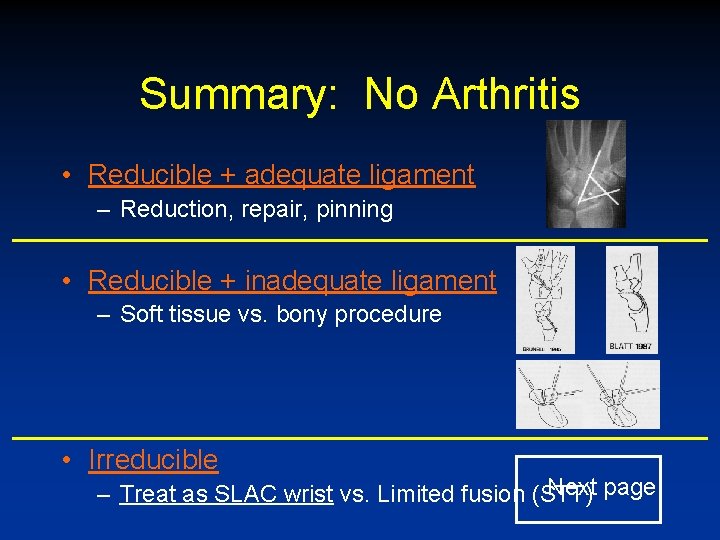
Summary: No Arthritis • Reducible + adequate ligament – Reduction, repair, pinning • Reducible + inadequate ligament – Soft tissue vs. bony procedure • Irreducible Next page – Treat as SLAC wrist vs. Limited fusion (STT)
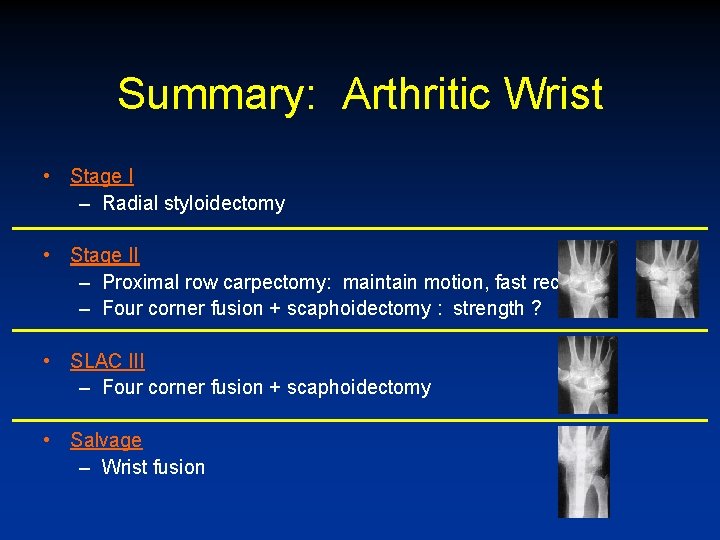
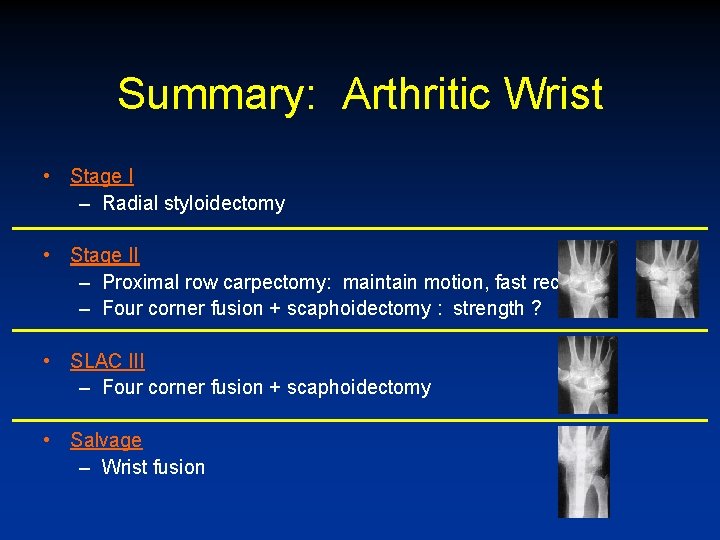
Summary: Arthritic Wrist • Stage I – Radial styloidectomy • Stage II – Proximal row carpectomy: maintain motion, fast recovery – Four corner fusion + scaphoidectomy : strength ? • SLAC III – Four corner fusion + scaphoidectomy • Salvage – Wrist fusion


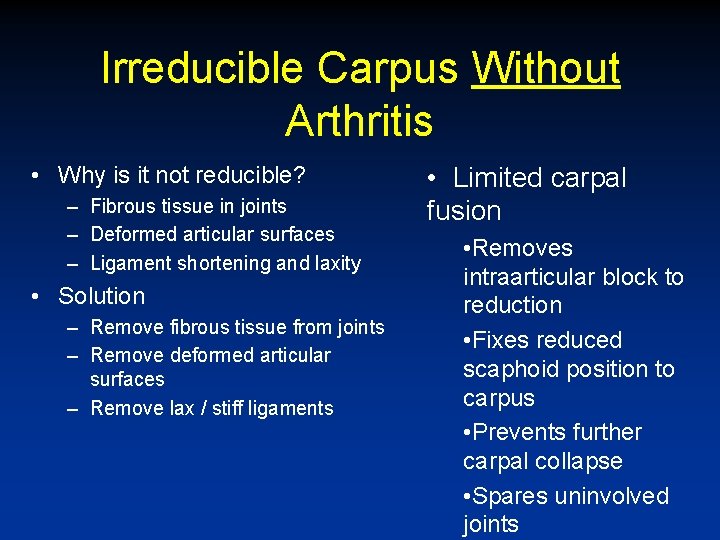
Irreducible Carpus Without Arthritis • Why is it not reducible? – Fibrous tissue in joints – Deformed articular surfaces – Ligament shortening and laxity • Solution – Remove fibrous tissue from joints – Remove deformed articular surfaces – Remove lax / stiff ligaments • Limited carpal fusion • Removes intraarticular block to reduction • Fixes reduced scaphoid position to carpus • Prevents further carpal collapse • Spares uninvolved joints
Irreducible Carpus Without Arthritis • STT fusion + dorsolateral styloidectomy • SL / SC / SLC fusion • Without reduction of deformity, progression to SLAC wrist • Results of limited wrist carpal fusions may not be good enough or predictable enough to justify using them -- safer option is to treat as SLAC wrist
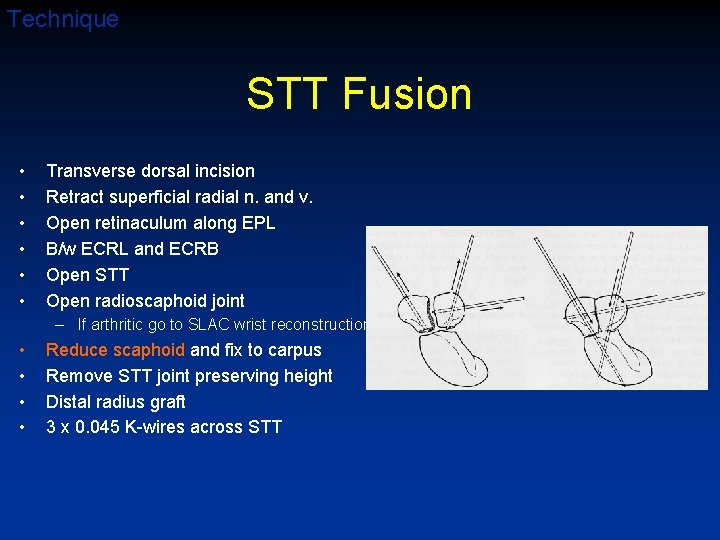
Technique STT Fusion • • • Transverse dorsal incision Retract superficial radial n. and v. Open retinaculum along EPL B/w ECRL and ECRB Open STT Open radioscaphoid joint – If arthritic go to SLAC wrist reconstruction • • Reduce scaphoid and fix to carpus Remove STT joint preserving height Distal radius graft 3 x 0. 045 K-wires across STT
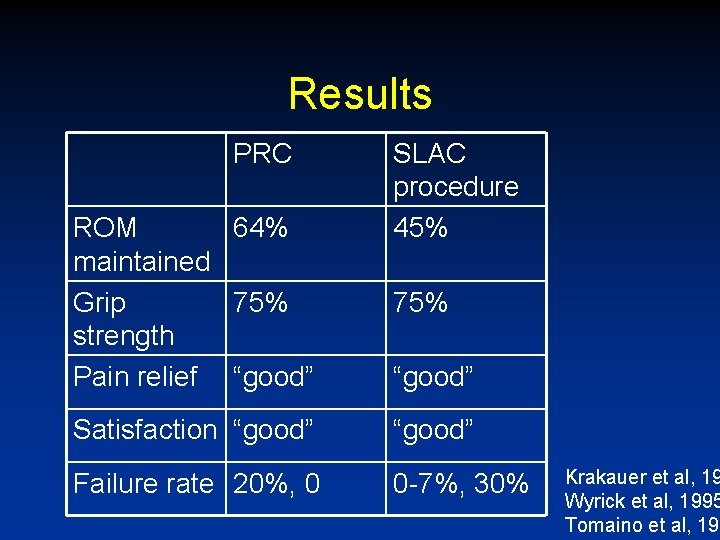
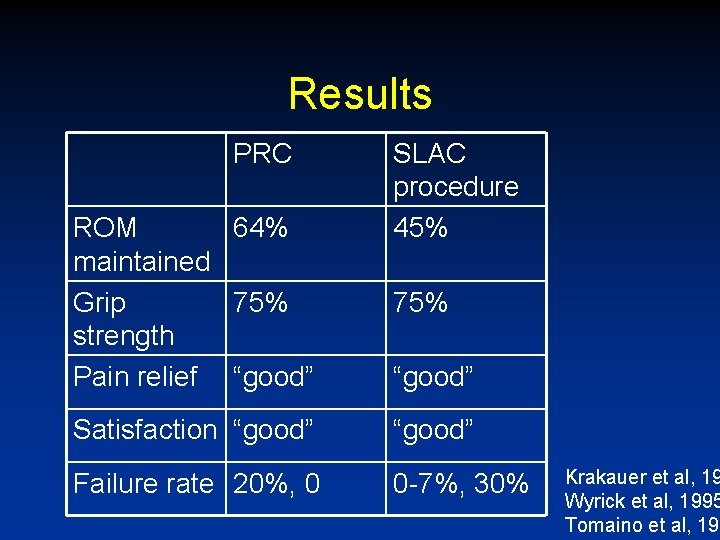
Results PRC ROM 64% maintained Grip 75% strength Pain relief “good” SLAC procedure 45% 75% “good” Satisfaction “good” Failure rate 20%, 0 0 -7%, 30% Krakauer et al, 19 Wyrick et al, 1995 Tomaino et al, 199