Skin Lesion James Warneke MD University of Arizona












- Slides: 38
Skin Lesion James Warneke, MD University of Arizona

Mr. Smith § Patient is a 64 year-old man with a history of a mole on his chest that has been present for years, but has recently grown is size. The mole has not bleed.
History What other points of the history do you want to know?
History, Mr. Smith Consider the Following § Characterization of symptoms § Temporal sequence § Alleviating / Exacerbating factors: § Pertinent PMH, ROS, MEDS. § Relevant family hx. § Associated signs and symptoms
History, Mr Smith § Characteristics of mole • Change in color • Nodular areas § Family History of melanoma § History of sun exposure and sunburns § History of previous atypical moles

What is your Differential Diagnosis?

Differential Diagnosis Based on History § § § Dysplastic Nevus Malignant Melanoma Basal Cell Carcinoma Squamous Cell Carcinoma Junctional Nevus Actinic Keratosis
Physical Examination What would you look for?
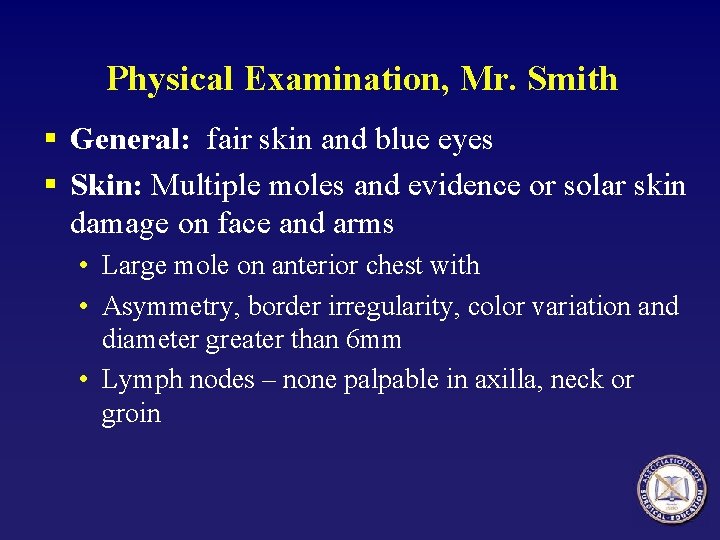
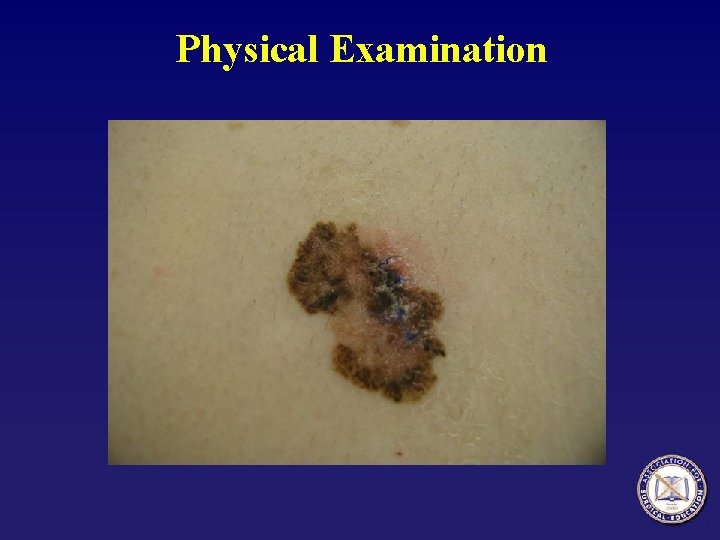
Physical Examination, Mr. Smith § General: fair skin and blue eyes § Skin: Multiple moles and evidence or solar skin damage on face and arms • Large mole on anterior chest with • Asymmetry, border irregularity, color variation and diameter greater than 6 mm • Lymph nodes – none palpable in axilla, neck or groin
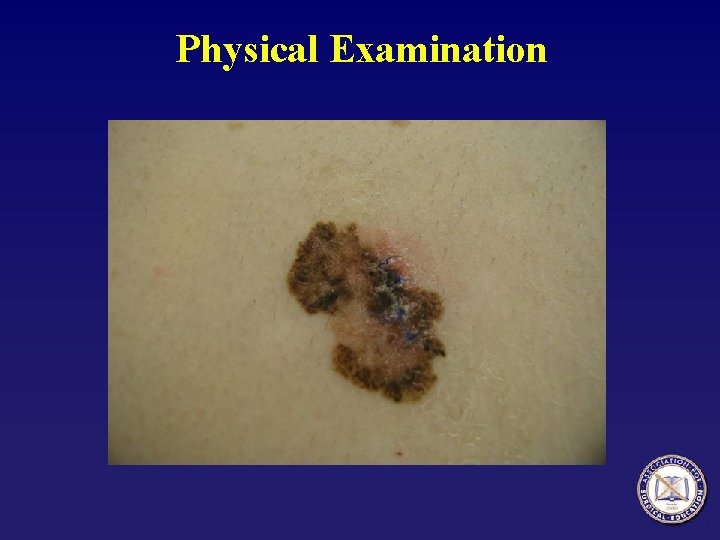
Physical Examination
Interventions at this point?
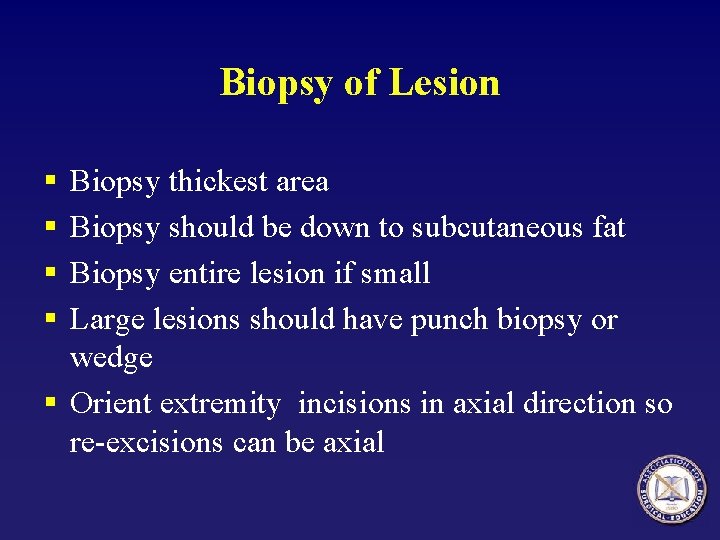
Biopsy of Lesion § § Biopsy thickest area Biopsy should be down to subcutaneous fat Biopsy entire lesion if small Large lesions should have punch biopsy or wedge § Orient extremity incisions in axial direction so re-excisions can be axial

Would you like to revise your Differential Diagnosis?
Results of Biopsy § Melanoma What is important to check on the pathology report?
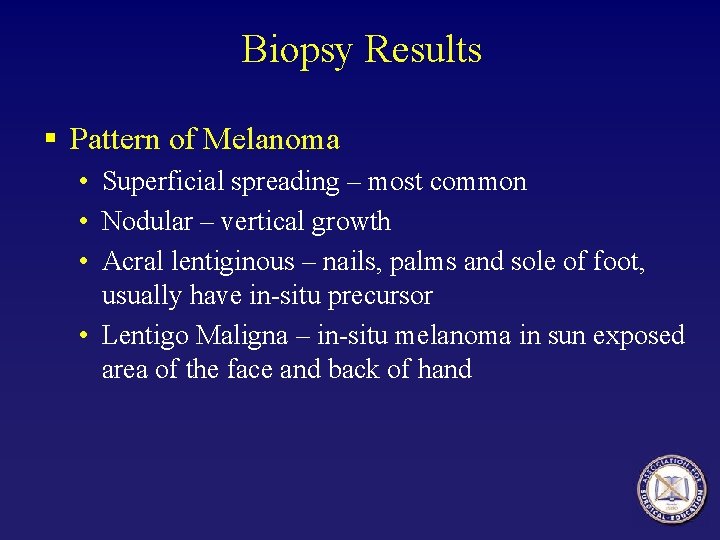
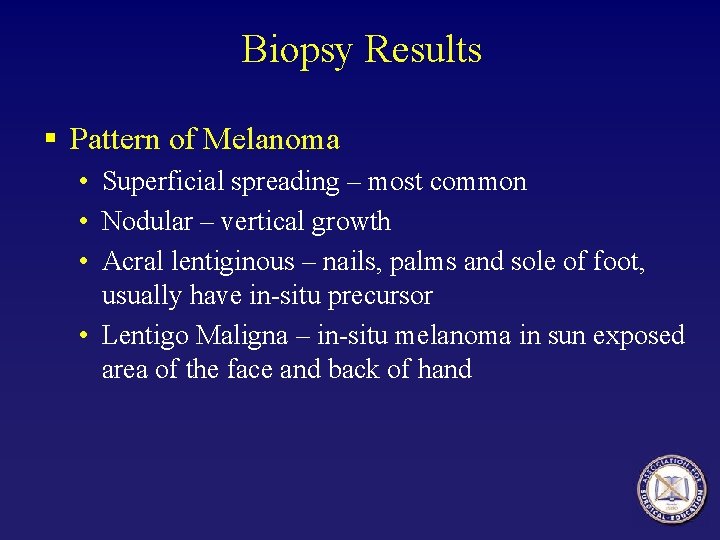
Biopsy Results § Pattern of Melanoma • Superficial spreading – most common • Nodular – vertical growth • Acral lentiginous – nails, palms and sole of foot, usually have in-situ precursor • Lentigo Maligna – in-situ melanoma in sun exposed area of the face and back of hand
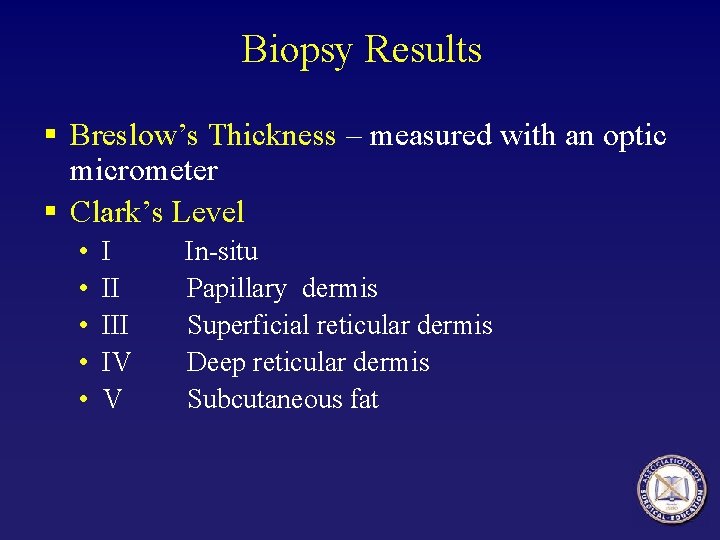
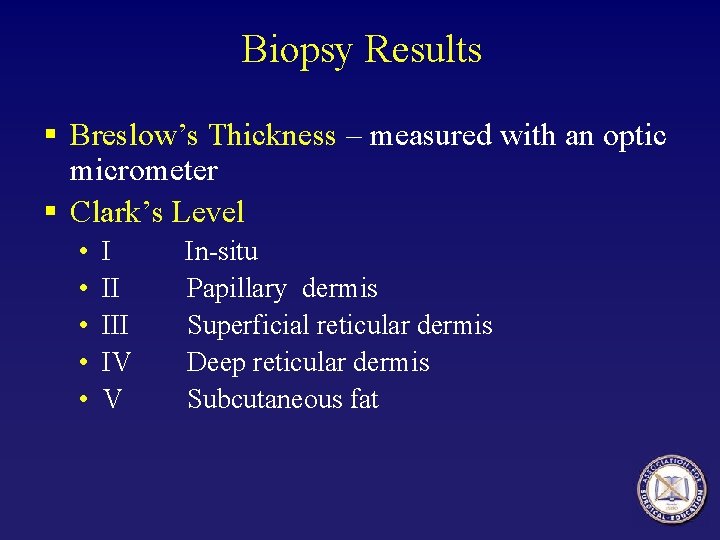
Biopsy Results § Breslow’s Thickness – measured with an optic micrometer § Clark’s Level • • • I II IV V In-situ Papillary dermis Superficial reticular dermis Deep reticular dermis Subcutaneous fat

Biopsy Results § Ulceration of Epithelium § Other Factors – deep margin involved with melanoma, regression, lymphocytic infiltration.
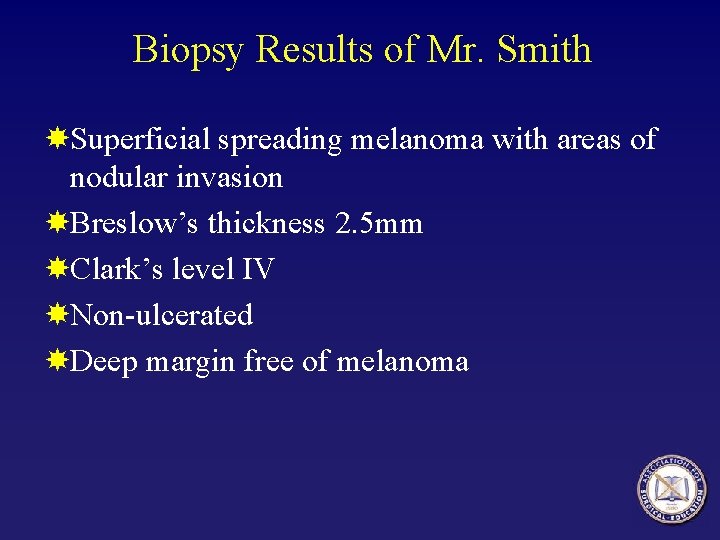
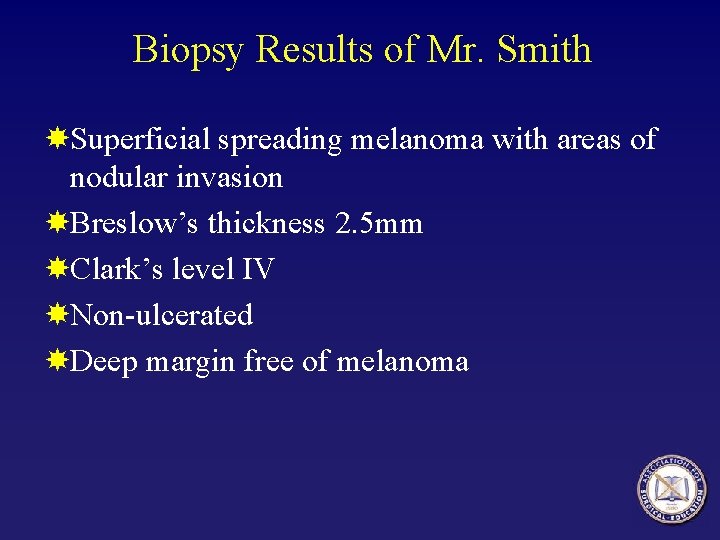
Biopsy Results of Mr. Smith Superficial spreading melanoma with areas of nodular invasion Breslow’s thickness 2. 5 mm Clark’s level IV Non-ulcerated Deep margin free of melanoma

Laboratory and X-ray What blood test should be ordered? What X-ray studies are indicated?
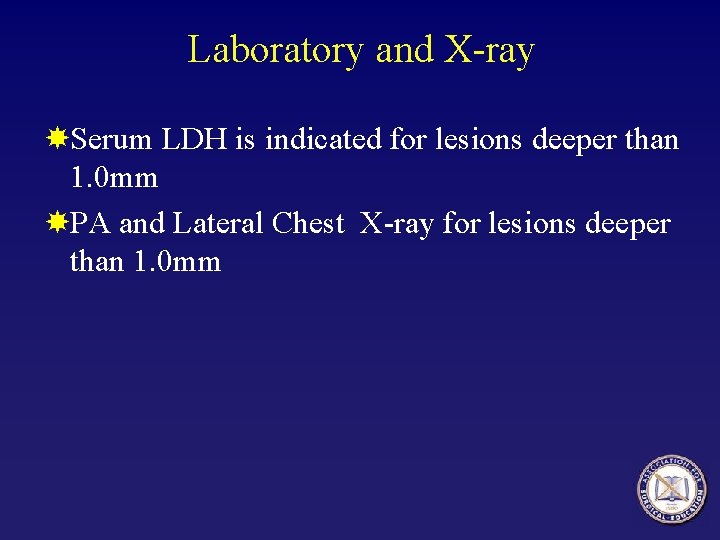
Laboratory and X-ray Serum LDH is indicated for lesions deeper than 1. 0 mm PA and Lateral Chest X-ray for lesions deeper than 1. 0 mm
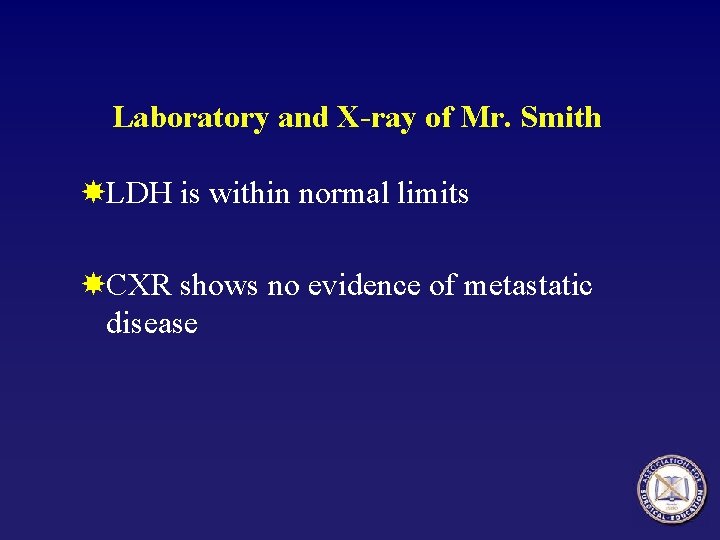
Laboratory and X-ray of Mr. Smith LDH is within normal limits CXR shows no evidence of metastatic disease
Further Management What should be done next?

Management Surgical Excision § How wide of an excision should be done? § When should a lymph node biopsy be planned?
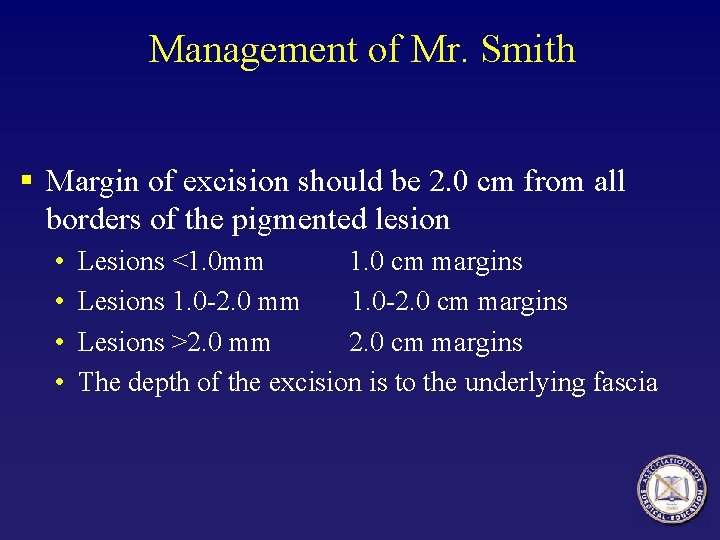
Management of Mr. Smith § Margin of excision should be 2. 0 cm from all borders of the pigmented lesion • • Lesions <1. 0 mm 1. 0 cm margins Lesions 1. 0 -2. 0 mm 1. 0 -2. 0 cm margins Lesions >2. 0 mm 2. 0 cm margins The depth of the excision is to the underlying fascia
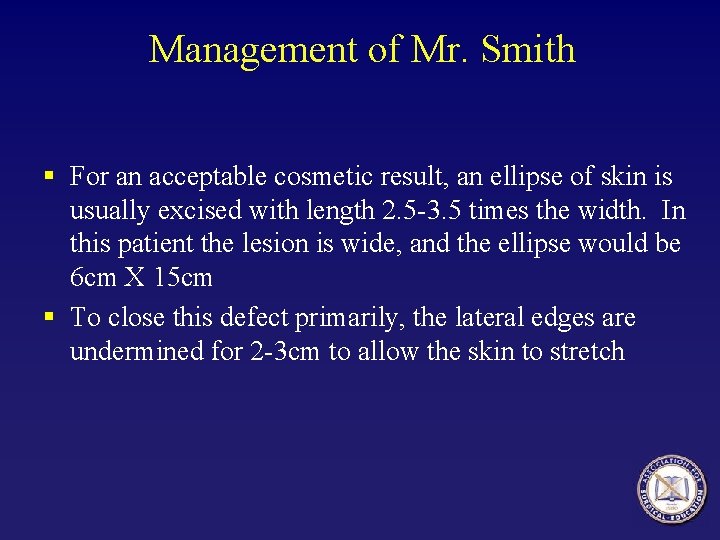
Management of Mr. Smith § For an acceptable cosmetic result, an ellipse of skin is usually excised with length 2. 5 -3. 5 times the width. In this patient the lesion is wide, and the ellipse would be 6 cm X 15 cm § To close this defect primarily, the lateral edges are undermined for 2 -3 cm to allow the skin to stretch
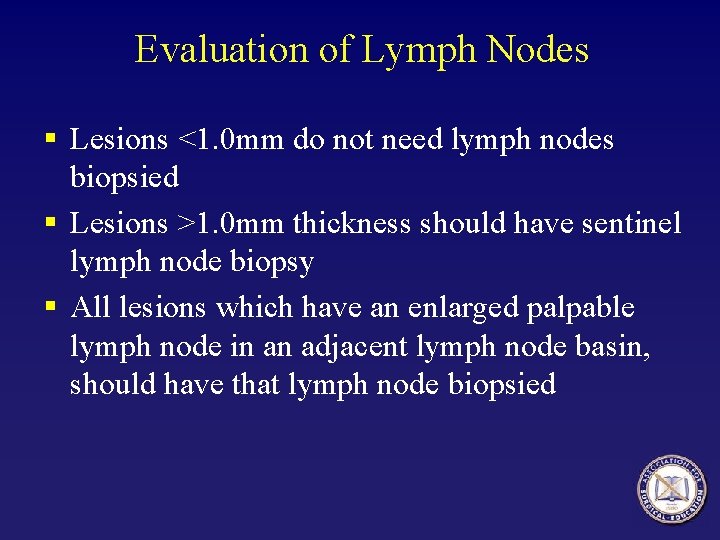
Evaluation of Lymph Nodes § Lesions <1. 0 mm do not need lymph nodes biopsied § Lesions >1. 0 mm thickness should have sentinel lymph node biopsy § All lesions which have an enlarged palpable lymph node in an adjacent lymph node basin, should have that lymph node biopsied
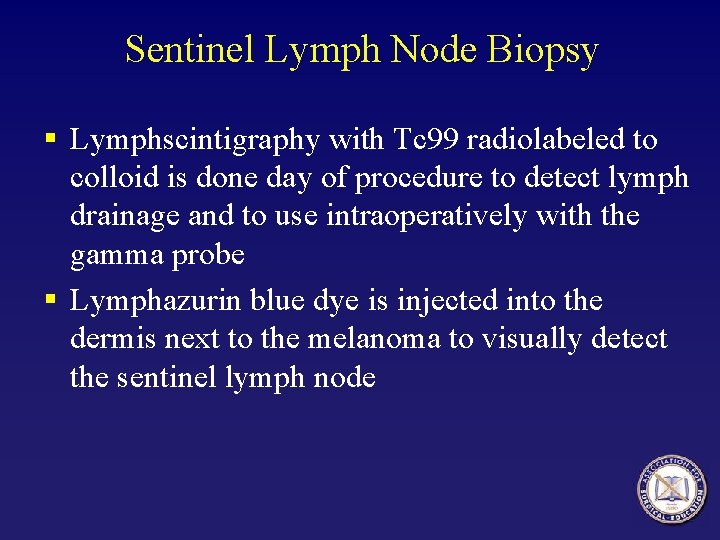
Sentinel Lymph Node Biopsy § Lymphscintigraphy with Tc 99 radiolabeled to colloid is done day of procedure to detect lymph drainage and to use intraoperatively with the gamma probe § Lymphazurin blue dye is injected into the dermis next to the melanoma to visually detect the sentinel lymph node
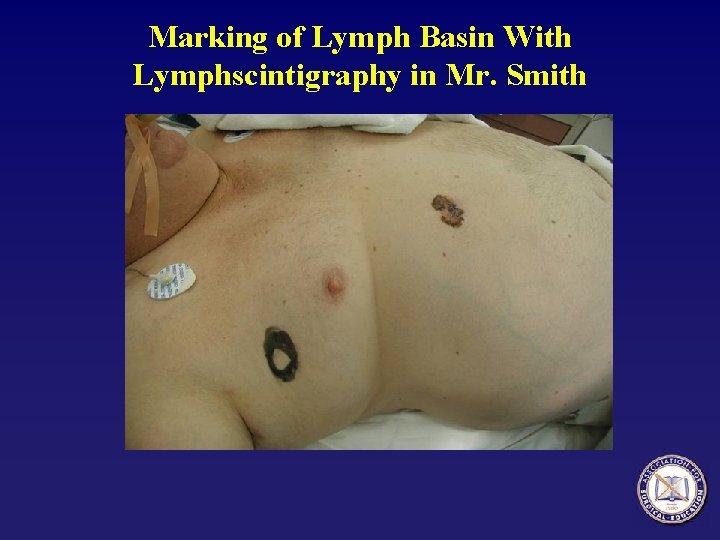
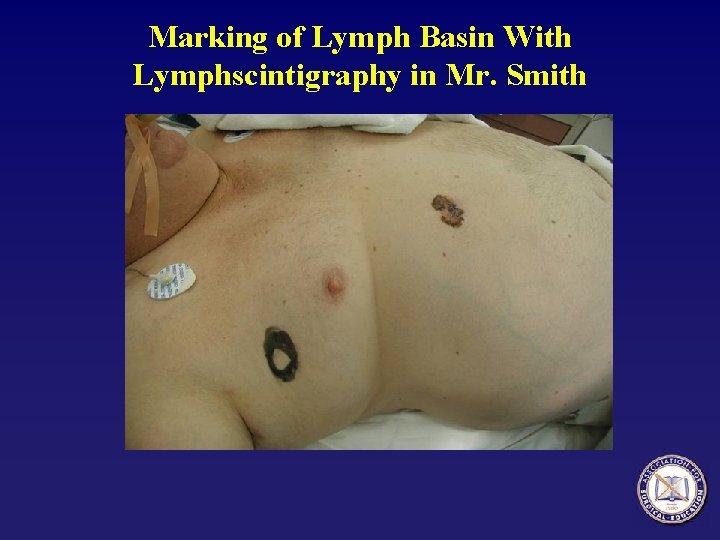
Marking of Lymph Basin With Lymphscintigraphy in Mr. Smith

Injection of Lymphazurin Blue Dye in Mr. Smith

Evaluation of Mr. Smith’s Lymph Nodes

Sentinel Lymph Nodes in Mr. Smith § Sentinel lymph node biopsy found two lymph nodes which where blue § Both blue lymph nodes were hot with the handheld gamma probe § Pathology by routine histology and immunohistochemistry did not detect any melanoma in the lymph nodes

What Stage is Mr. Smith’s Melanoma?
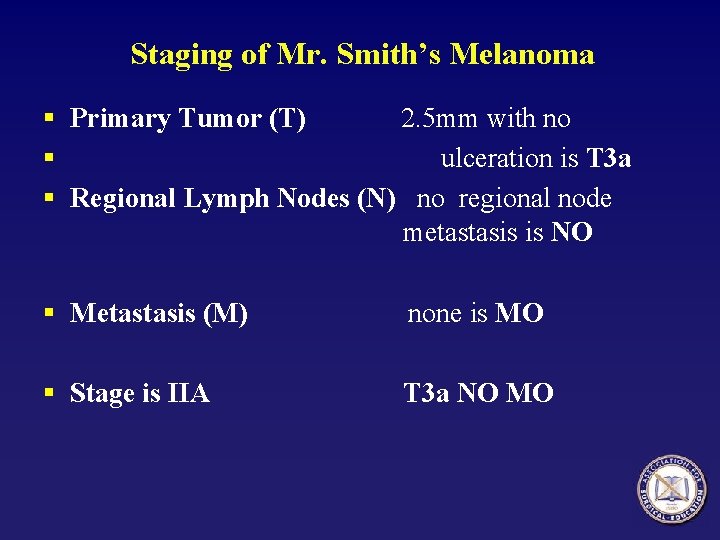
Staging of Mr. Smith’s Melanoma § Primary Tumor (T) 2. 5 mm with no § ulceration is T 3 a § Regional Lymph Nodes (N) no regional node metastasis is NO § Metastasis (M) none is MO § Stage is IIA T 3 a NO MO
Prognosis § What is the estimated 10 year survival of Mr. Smith?
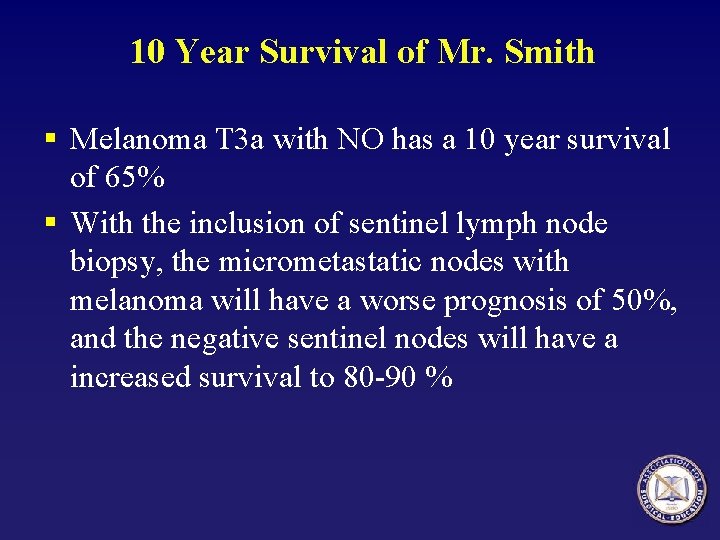
10 Year Survival of Mr. Smith § Melanoma T 3 a with NO has a 10 year survival of 65% § With the inclusion of sentinel lymph node biopsy, the micrometastatic nodes with melanoma will have a worse prognosis of 50%, and the negative sentinel nodes will have a increased survival to 80 -90 %
Questions?

Summary of Melanoma § § § 54, 200 new melanomas per year in US 7600 deaths from melanoma per year in US 1 in 57 white males 1 in 81 white females 89% 5 -year survival for 1992 -1998
Acknowledgment The preceding educational materials were made available through the ASSOCIATION FOR SURGICAL EDUCATION In order to improve our educational materials we welcome your comments/ suggestions at: feedback. PPTM@surgicaleducation. com
 Dr warneke tucson az
Dr warneke tucson az Chapter 8 skin disorders and diseases review questions
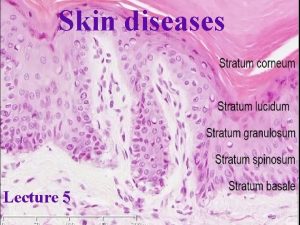
Chapter 8 skin disorders and diseases review questions Stratum lucidum
Stratum lucidum Thin skin vs thick skin
Thin skin vs thick skin Steps to a basic facial milady
Steps to a basic facial milady Arizona state university geology
Arizona state university geology Nau edulouie
Nau edulouie Infn genova
Infn genova Bblearnnau
Bblearnnau University of arizona emergency medicine
University of arizona emergency medicine Csc 110 university of arizona
Csc 110 university of arizona Bnad 276 university of arizona
Bnad 276 university of arizona Russell odom and clay lawson
Russell odom and clay lawson James russell odom
James russell odom Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Neospinothalamic pathway
Neospinothalamic pathway Tabes dorsalis gait
Tabes dorsalis gait Upper motor neuron lesion
Upper motor neuron lesion Pprf mlf pathway
Pprf mlf pathway Luxacion divergente de codo
Luxacion divergente de codo Lower motor neuron lesion
Lower motor neuron lesion Thalamus
Thalamus Lesions of vagus nerve
Lesions of vagus nerve Formatiune hipoecogena ficat
Formatiune hipoecogena ficat Optic tract lesions
Optic tract lesions Pirad 4 lesion prostate
Pirad 4 lesion prostate Signos duros y blandos de trauma vascular
Signos duros y blandos de trauma vascular Vascular
Vascular Citolítico
Citolítico Archicerebellum
Archicerebellum Lesion subepicardica
Lesion subepicardica Definicion de lesion celular
Definicion de lesion celular Molusco contagioso lesion elemental
Molusco contagioso lesion elemental Face nerve supply
Face nerve supply Tejido vitalizado
Tejido vitalizado Infarto subendocardico y subepicardico
Infarto subendocardico y subepicardico Archi paleo neo cerebellum
Archi paleo neo cerebellum Endo perio lesion
Endo perio lesion Ecg image en miroir
Ecg image en miroir