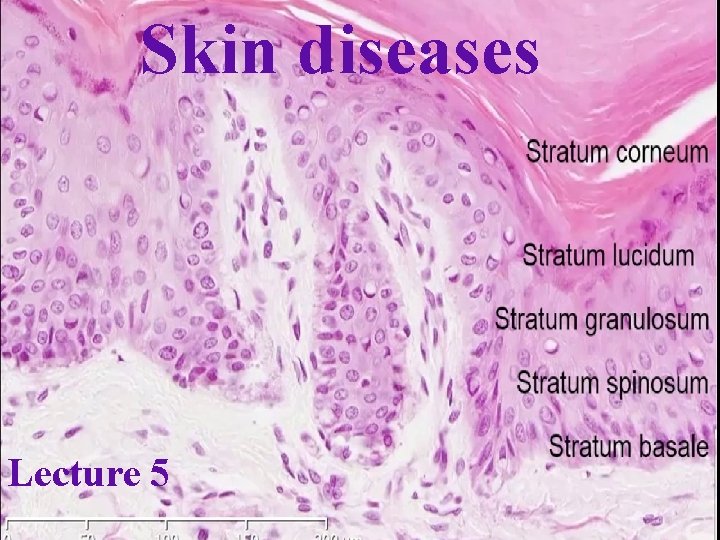
Skin diseases Lecture 5 Skin diseases Skin Complex








- Slides: 42
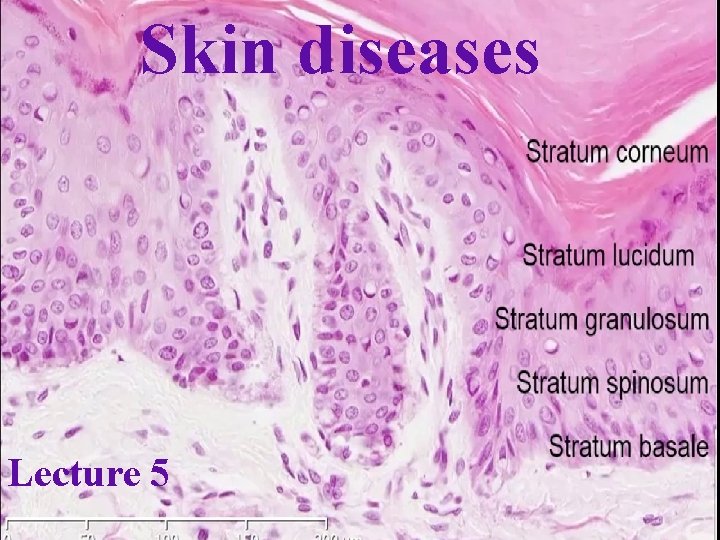
Skin diseases Lecture 5
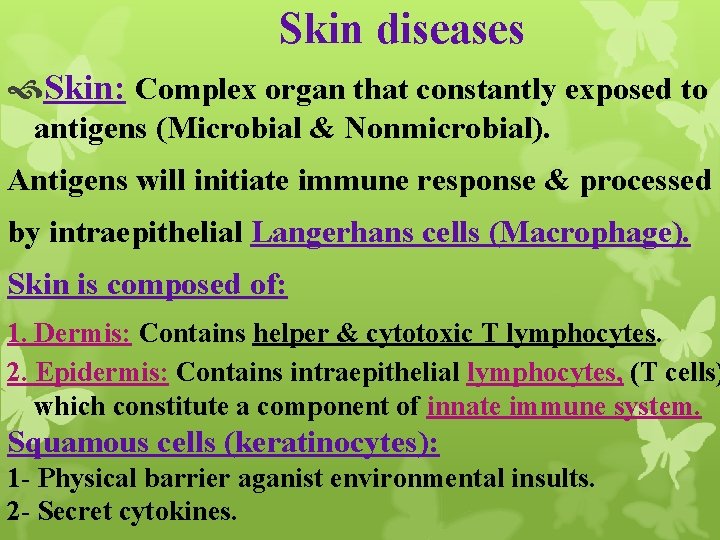
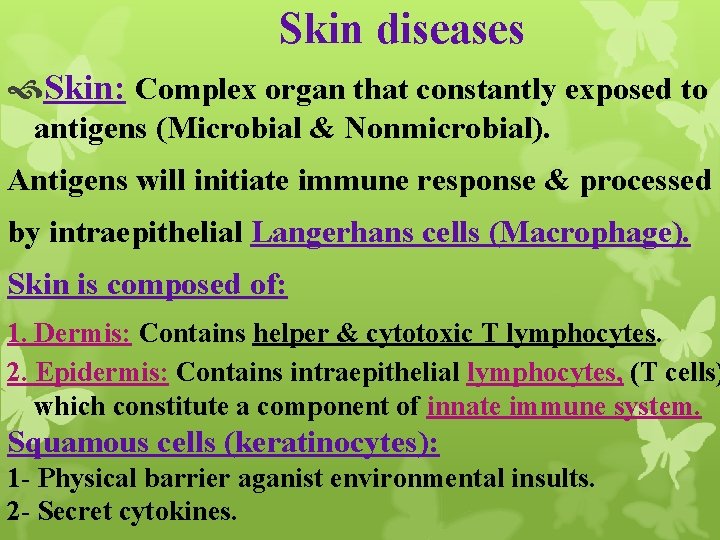
Skin diseases Skin: Complex organ that constantly exposed to antigens (Microbial & Nonmicrobial). Antigens will initiate immune response & processed by intraepithelial Langerhans cells (Macrophage). Skin is composed of: 1. Dermis: Contains helper & cytotoxic T lymphocytes. 2. Epidermis: Contains intraepithelial lymphocytes, (T cells) which constitute a component of innate immune system. Squamous cells (keratinocytes): 1 - Physical barrier aganist environmental insults. 2 - Secret cytokines.
Microscopic & clinical manifestations of cutaneous inflammatory & infectious diseases are due to this local immune responses (Immune cells & cytokines) Skin diseases: q. Common & diverse group of diseases ranging from 1. Irritating acne (pimples). 2. Life-threatening melanoma. q. Skin manifestations of diseases are intrinsic to skin q. Or involves many tissues: (Systemic lupus erythematosus) q. Genetic syndromes such as neurofibromatosis.

Terms used for Macroscopic Lesions: Excoriation: Broken epidermis due to trauma Red linear mark (deep scratch); often self-inflicted. Lichenification: Thickened & rough skin with prominent markings result from repeated rubbing.

Macule: Flat circumscribed colored area, 5 mm or less in diameter. Patch: Macule greater than 5 mm.

Papule: Elevated dome- or flat-topped lesion, 5 mm or less. Nodule: Papule greater than 5 mm.

Plaque: Elevated flat-topped lesion, greater than 5 mm. Pustule: Small, pus-filled raised lesion.

Scale: Dry, horny, platelike lesion result of imperfect cornification.
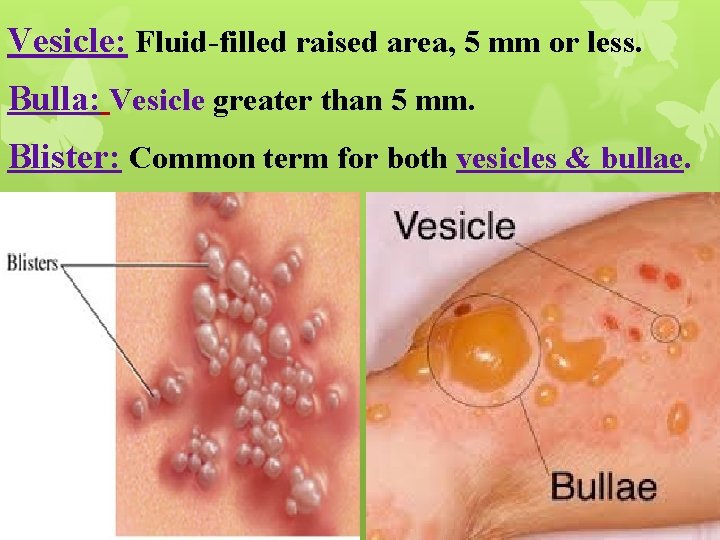
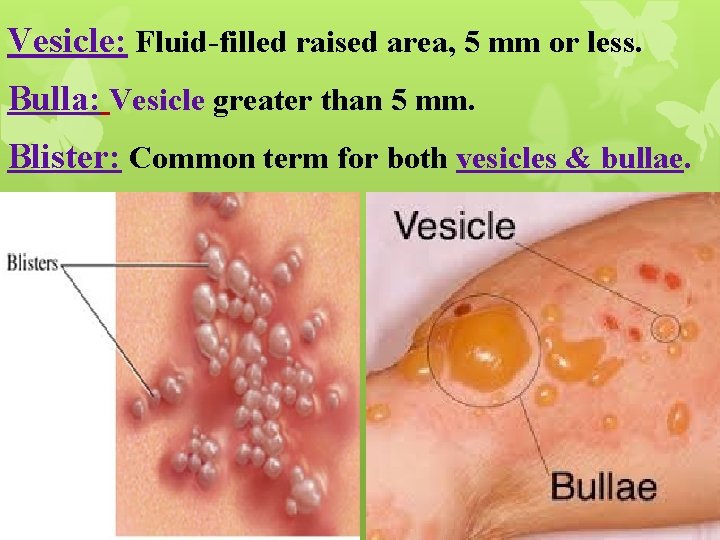
Vesicle: Fluid-filled raised area, 5 mm or less. Bulla: Vesicle greater than 5 mm. Blister: Common term for both vesicles & bullae.
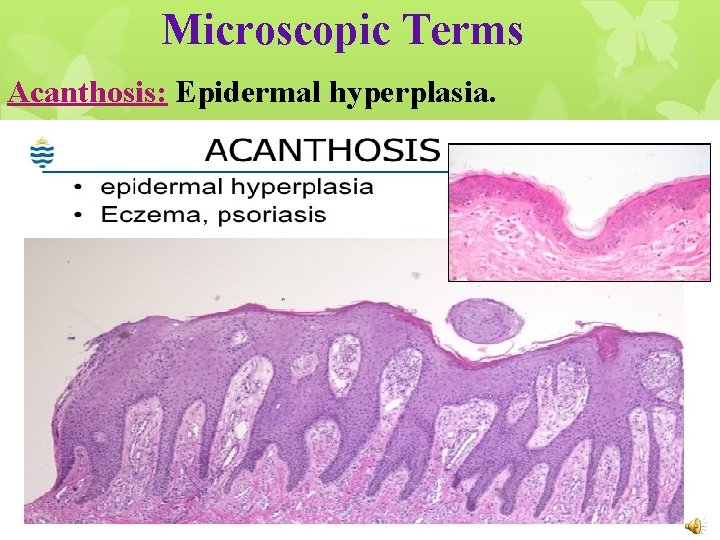
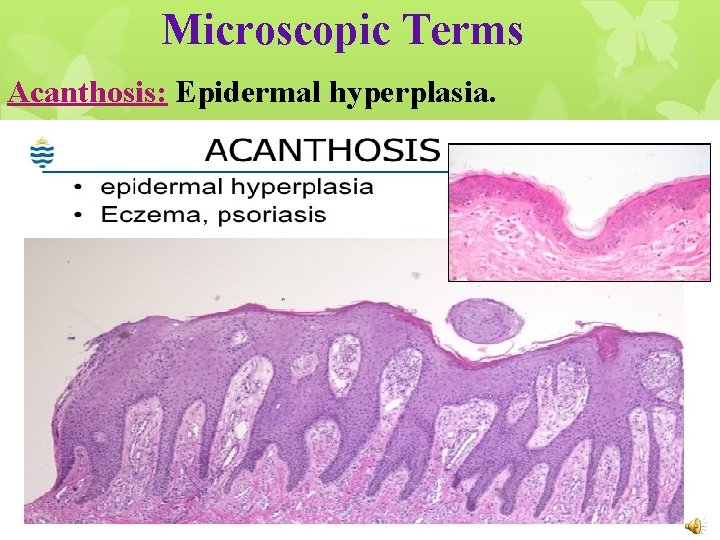
Microscopic Terms Acanthosis: Epidermal hyperplasia.
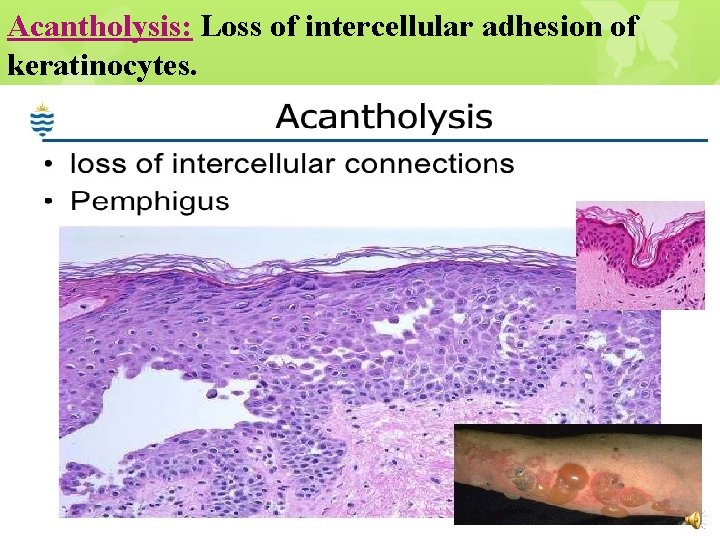
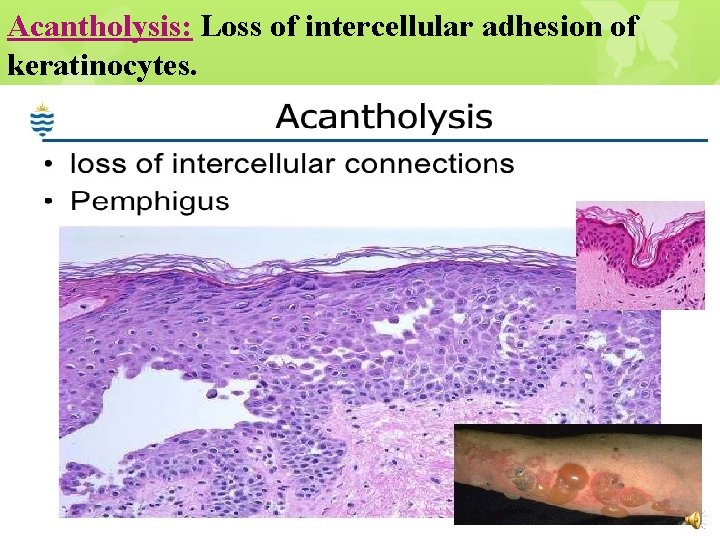
Acantholysis: Loss of intercellular adhesion of keratinocytes.
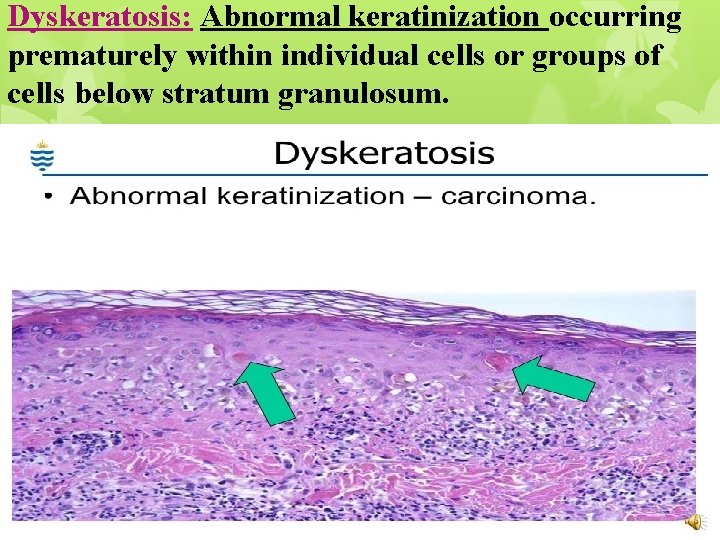
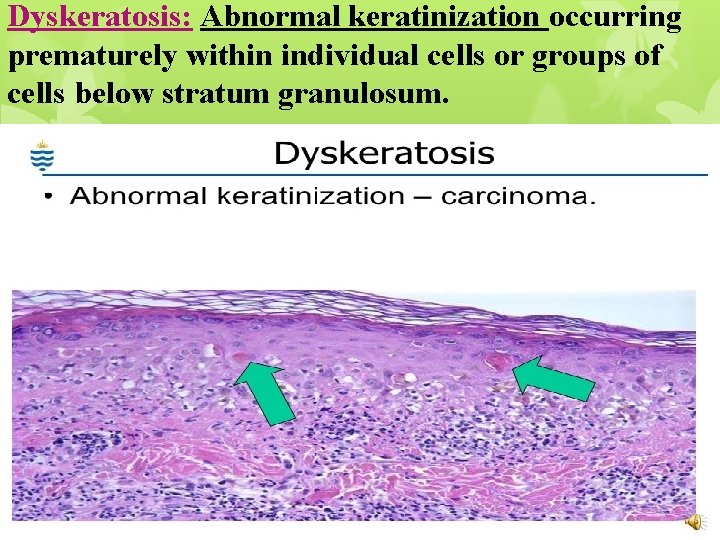
Dyskeratosis: Abnormal keratinization occurring prematurely within individual cells or groups of cells below stratum granulosum.
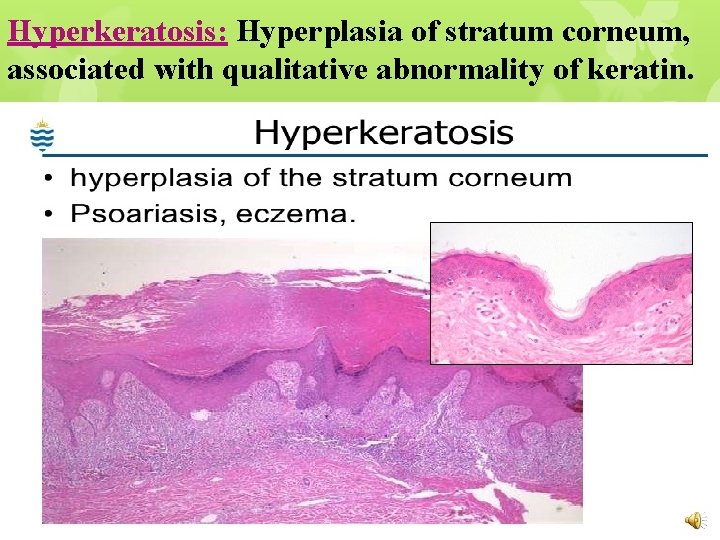
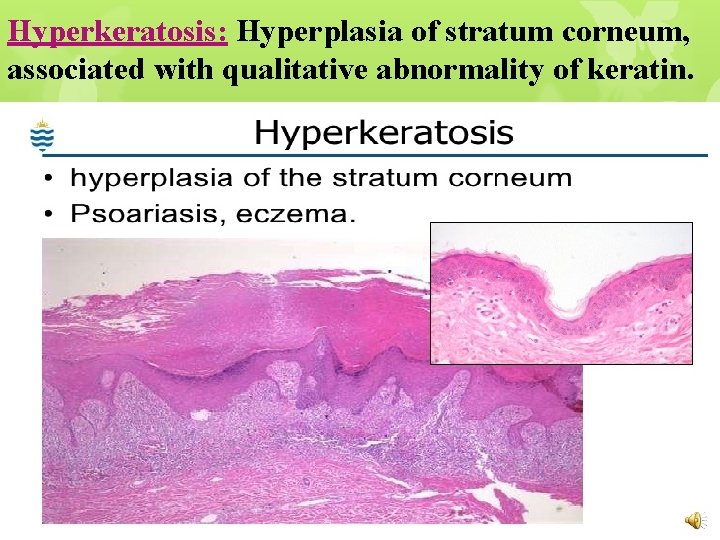
Hyperkeratosis: Hyperplasia of stratum corneum, associated with qualitative abnormality of keratin.
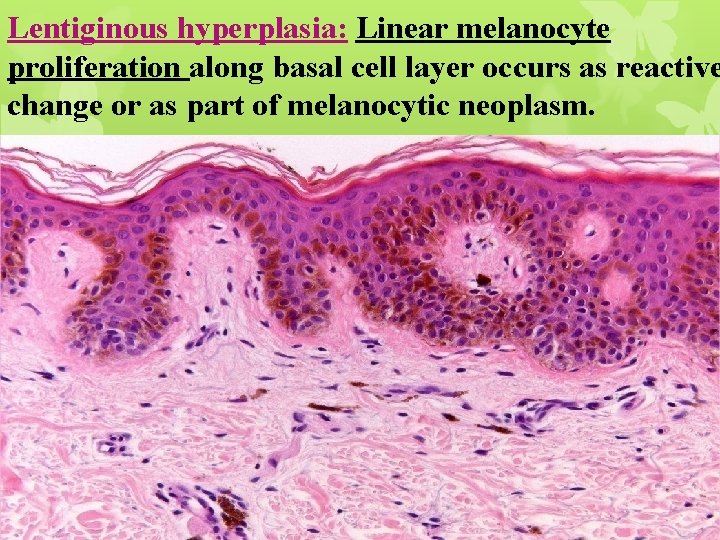
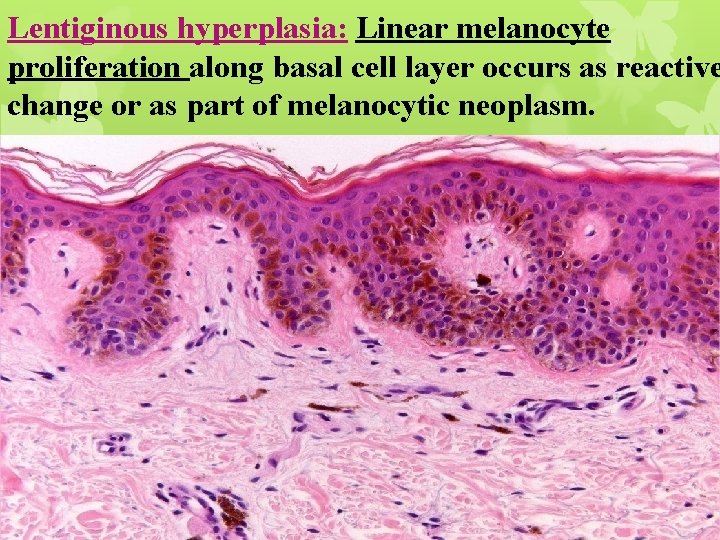
Lentiginous hyperplasia: Linear melanocyte proliferation along basal cell layer occurs as reactive change or as part of melanocytic neoplasm.
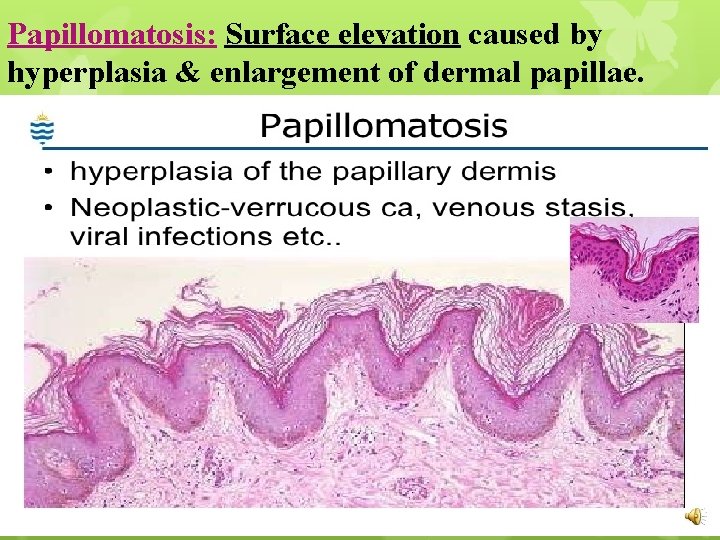
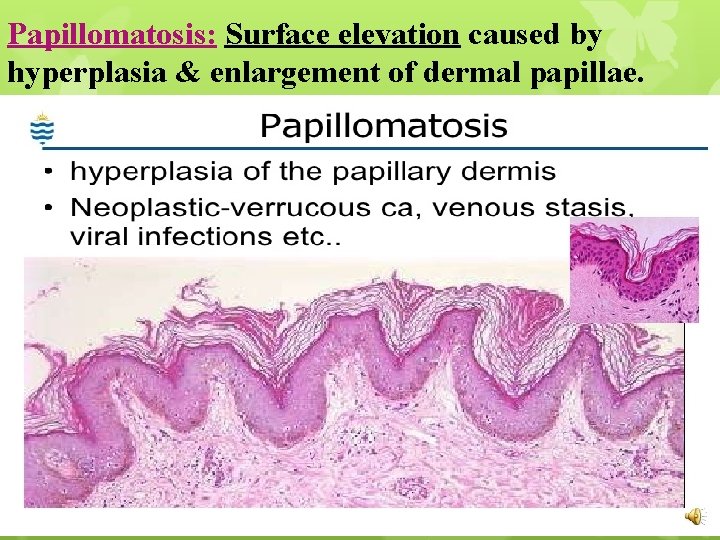
Papillomatosis: Surface elevation caused by hyperplasia & enlargement of dermal papillae.
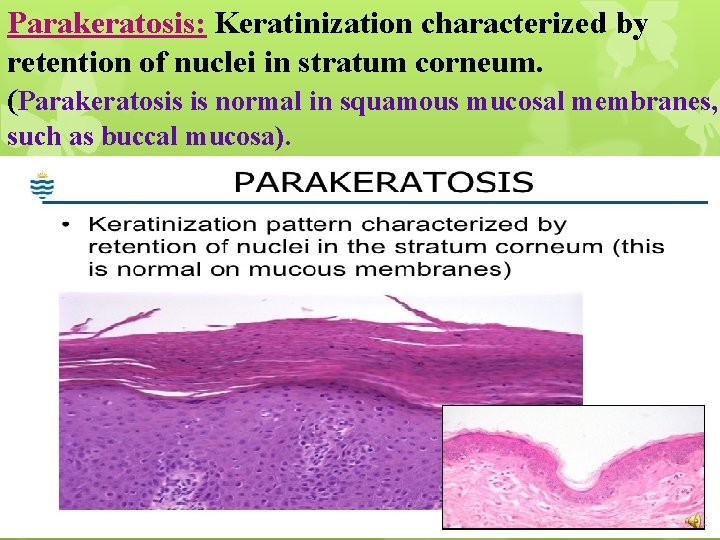
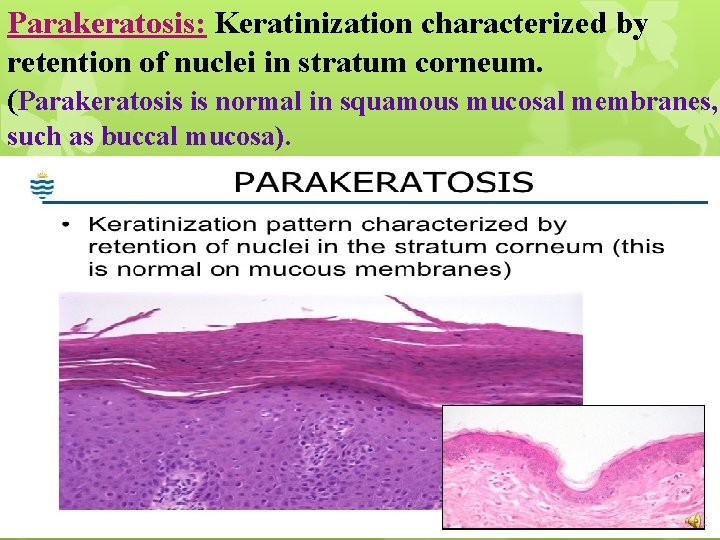
Parakeratosis: Keratinization characterized by retention of nuclei in stratum corneum. (Parakeratosis is normal in squamous mucosal membranes, such as buccal mucosa).
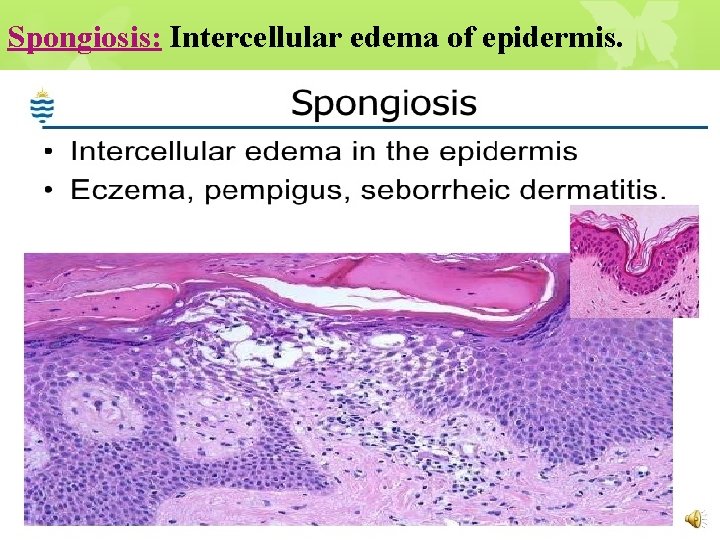
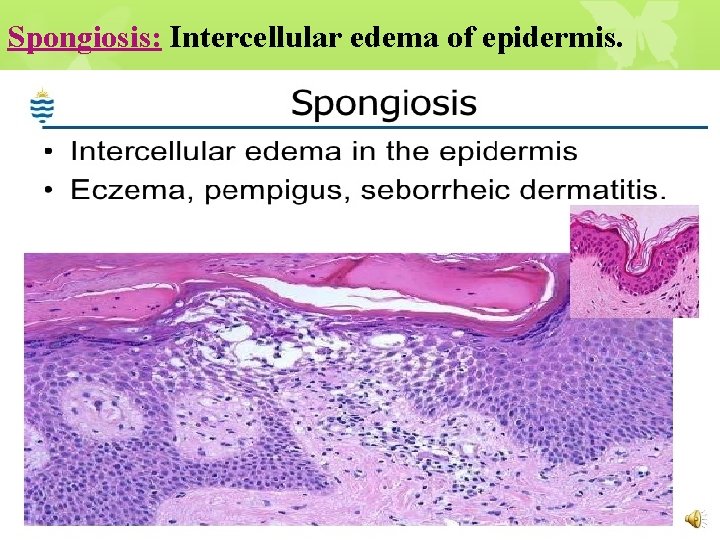
Spongiosis: Intercellular edema of epidermis.
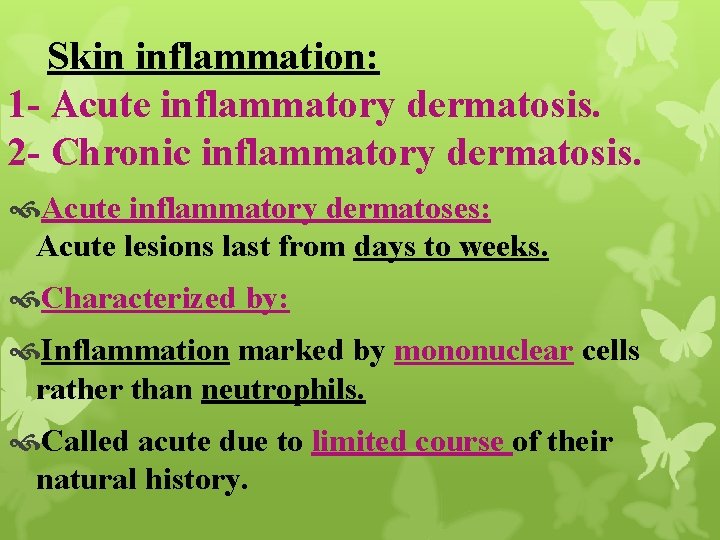
Skin inflammation: 1 - Acute inflammatory dermatosis. 2 - Chronic inflammatory dermatosis. Acute inflammatory dermatoses: Acute lesions last from days to weeks. Characterized by: Inflammation marked by mononuclear cells rather than neutrophils. Called acute due to limited course of their natural history.
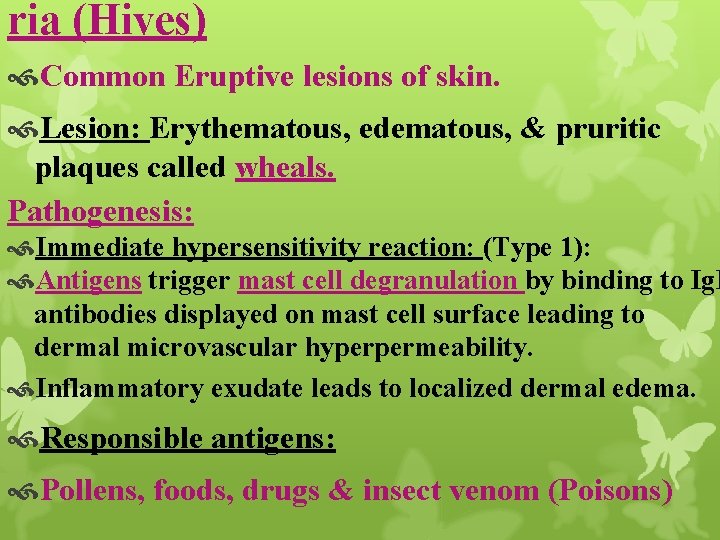
ria (Hives) Common Eruptive lesions of skin. Lesion: Erythematous, edematous, & pruritic plaques called wheals. Pathogenesis: Immediate hypersensitivity reaction: (Type 1): Antigens trigger mast cell degranulation by binding to Ig. E antibodies displayed on mast cell surface leading to dermal microvascular hyperpermeability. Inflammatory exudate leads to localized dermal edema. Responsible antigens: Pollens, foods, drugs & insect venom (Poisons)
Clinical Features: Ø Lesions develop & fade within hours. Ø Or persists for days or months due to: Urticarial vasculitis. Lesions of urticaria: Small pruritic papules. Large, edematous, erythematous plaques. Urticaria is not life-threatening but can causes severe pruritus & social embarrassment.

Urticaria (Hives)
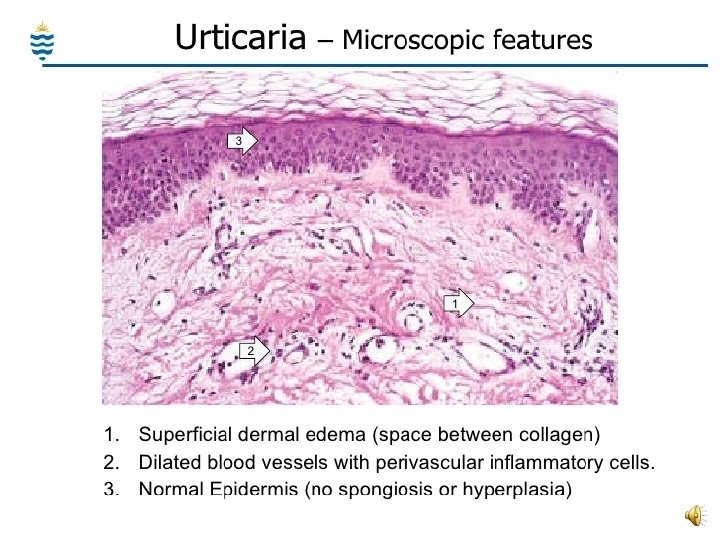
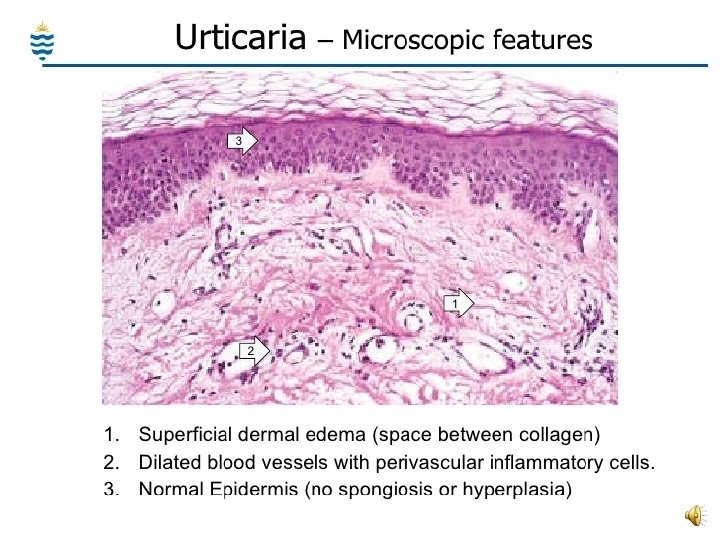
Morphology Superficial perivenular infiltrate of mononuclear cells, rare neutrophils, & sometimes eosinophils. Superficial dermal edema creates more widely spaced collagen bundles.
Acute Eczematous Dermatitis Eczema is clinical term include: A number of conditions with different causes. New lesions: Red papules, with overlying vesicles, which ooze & become crusted. Persistent lesions: Raised scaling plaques. Skin lesions resolve completely when the offending stimulus is removed or exposure is limited
Clinical subtypes of eczema: 1 • Allergic contact dermatitis: Topical exposure to allergen. 2 • Atopic dermatitis: Due to: #. Allergen exposure. #. Defects in keratinocyte function as a barrier, many with genetic basis. 3 • Drug-related eczematous dermatitis: Hypersensitivity reaction to a drug. 4 • Photoeczematous dermatitis: Abnormal reaction to UV or visible light. 5 • Primary irritant dermatitis: Exposure to substances damaging the skin. Chemical, physical, or mechanical.
Contact dermatitis: Delayed-type hypersensitivity reaction (Type IV) (Cell mediated). Exposure to environmental allergens (Poison ivy) reacts with self-proteins, processed by epidermal langerhans cells, which migrate to draining lymph nodes & present the antigen to naive T cells. Sensitization event Immunologic memory. On reexposure to antigen: Activated memory T lymphocytes migrate to affected skin sites releasing cytokines recruiting additional inflammatory cells & also mediate epidermal damage, as in any delayed-type hypersensitivity reaction.
Clinical Features Pruritic (itchy), edematous, oozing plaques, containing vesicles & bullae. With persistent antigen exposure: Lesions become scaly (hyperkeratotic) due to epidermis acanthosis. (Thicking) Clinical causes of eczema: 1. Reaction to internal circulating Ag. (Ingested food or drug). 2. Contact with external antigen: Poison ivy.
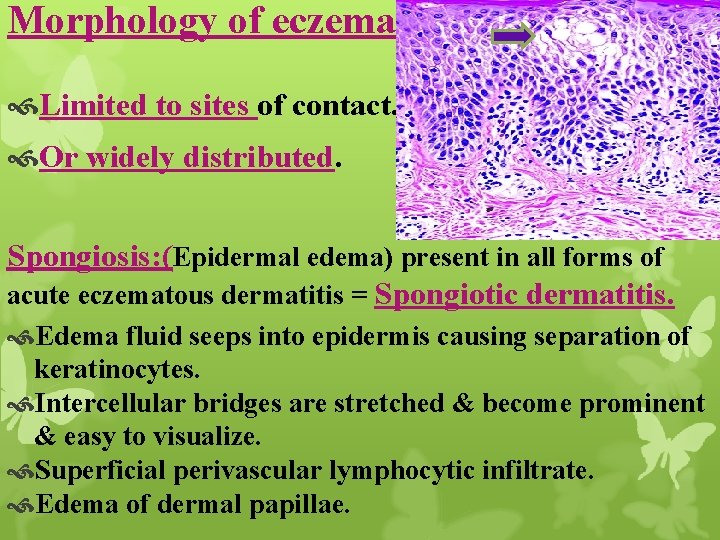
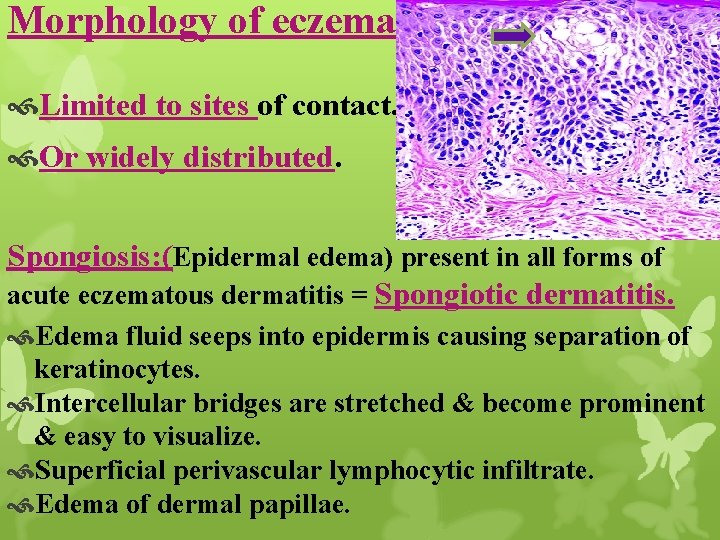
Morphology of eczema: Limited to sites of contact. Or widely distributed. Spongiosis: (Epidermal edema) present in all forms of acute eczematous dermatitis = Spongiotic dermatitis. Edema fluid seeps into epidermis causing separation of keratinocytes. Intercellular bridges are stretched & become prominent & easy to visualize. Superficial perivascular lymphocytic infiltrate. Edema of dermal papillae.
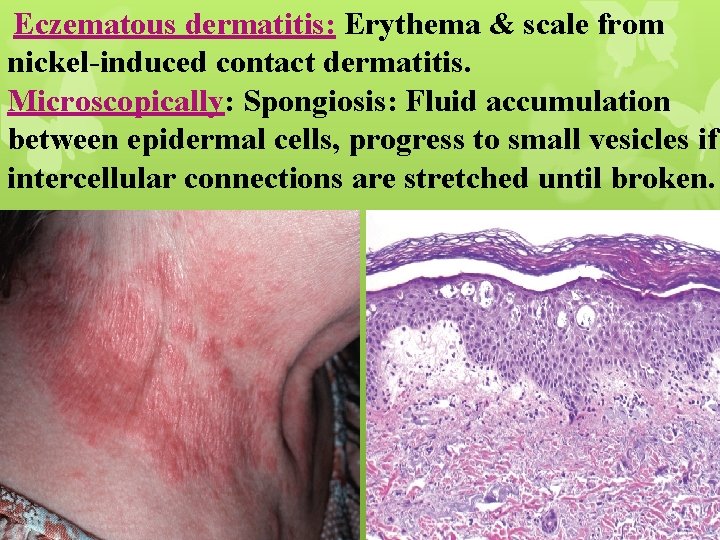
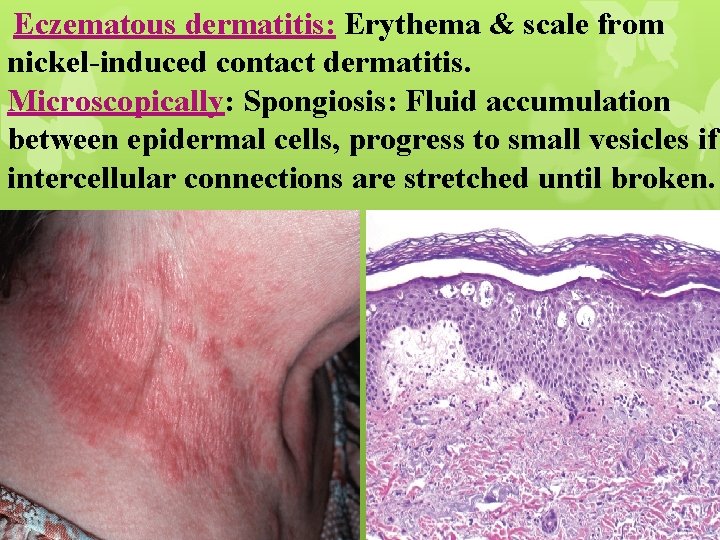
Eczematous dermatitis: Erythema & scale from nickel-induced contact dermatitis. Microscopically: Spongiosis: Fluid accumulation between epidermal cells, progress to small vesicles if intercellular connections are stretched until broken.
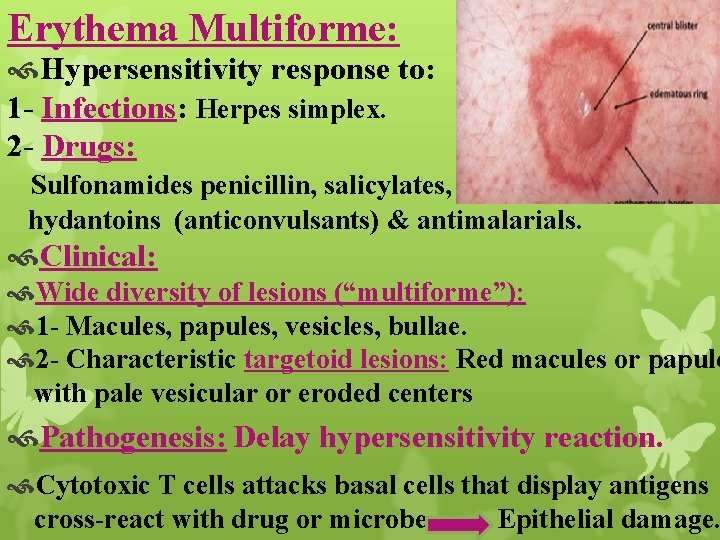
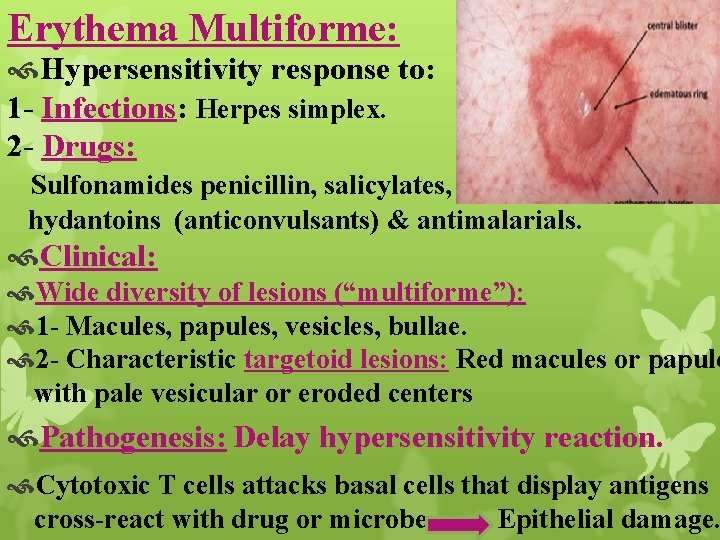
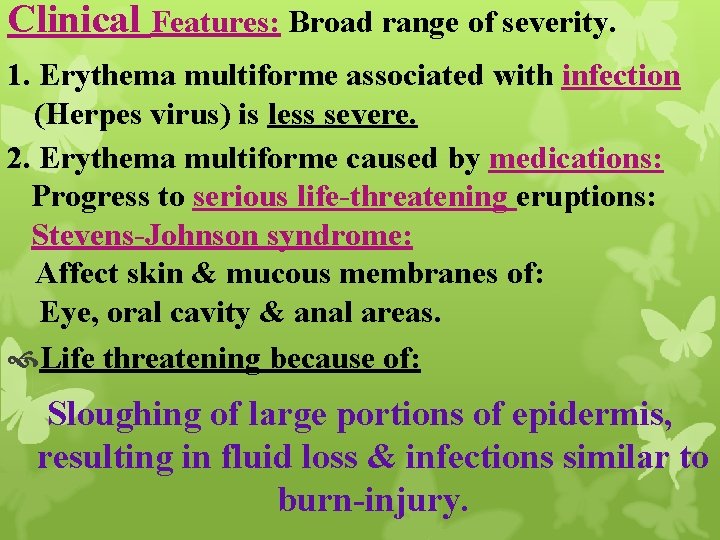
Erythema Multiforme: Hypersensitivity response to: 1 - Infections: Herpes simplex. 2 - Drugs: Sulfonamides penicillin, salicylates, hydantoins (anticonvulsants) & antimalarials. Clinical: Wide diversity of lesions (“multiforme”): 1 - Macules, papules, vesicles, bullae. 2 - Characteristic targetoid lesions: Red macules or papule with pale vesicular or eroded centers Pathogenesis: Delay hypersensitivity reaction. Cytotoxic T cells attacks basal cells that display antigens cross-react with drug or microbe Epithelial damage.
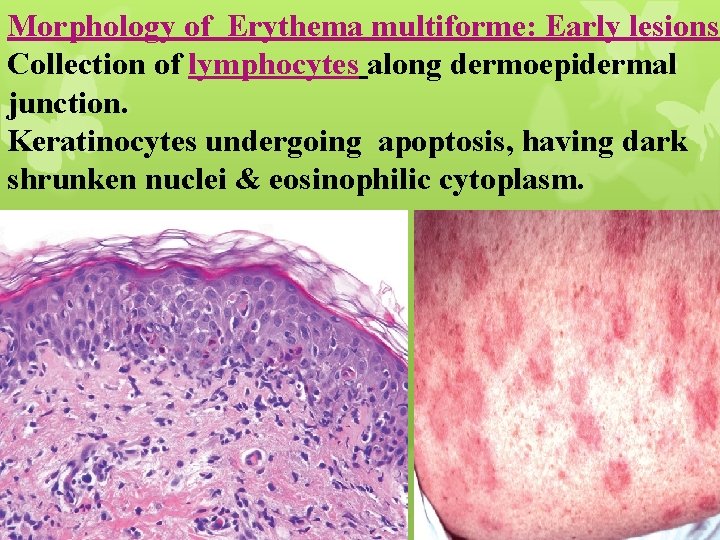
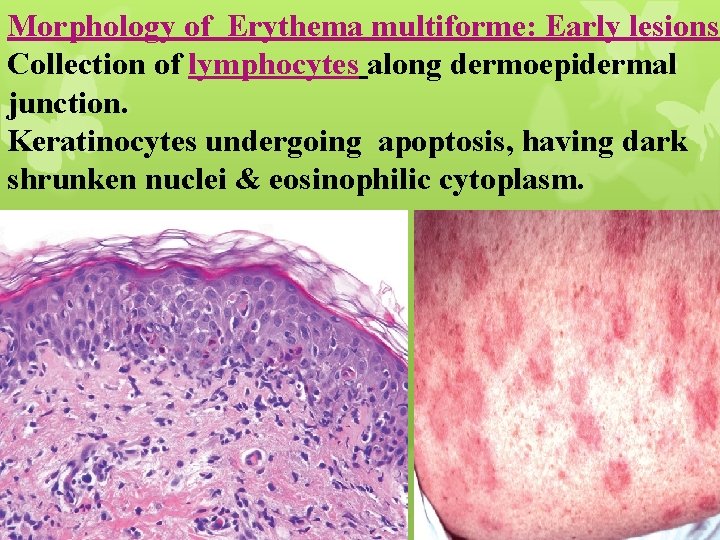
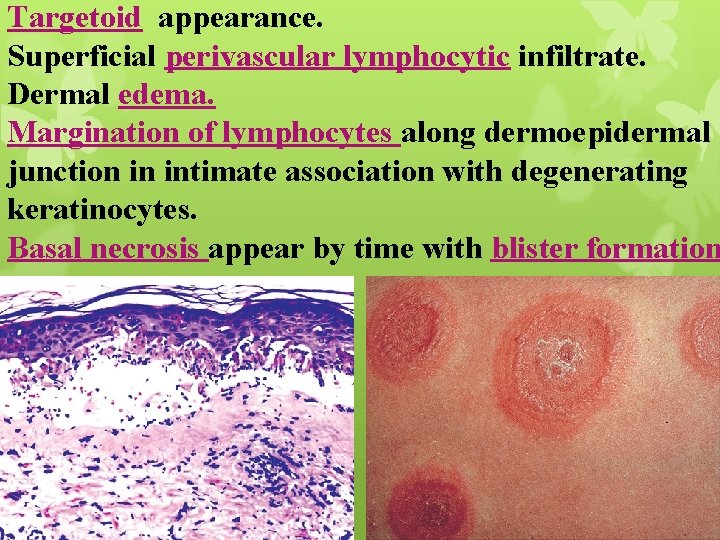
Morphology of Erythema multiforme: Early lesions Collection of lymphocytes along dermoepidermal junction. Keratinocytes undergoing apoptosis, having dark shrunken nuclei & eosinophilic cytoplasm.
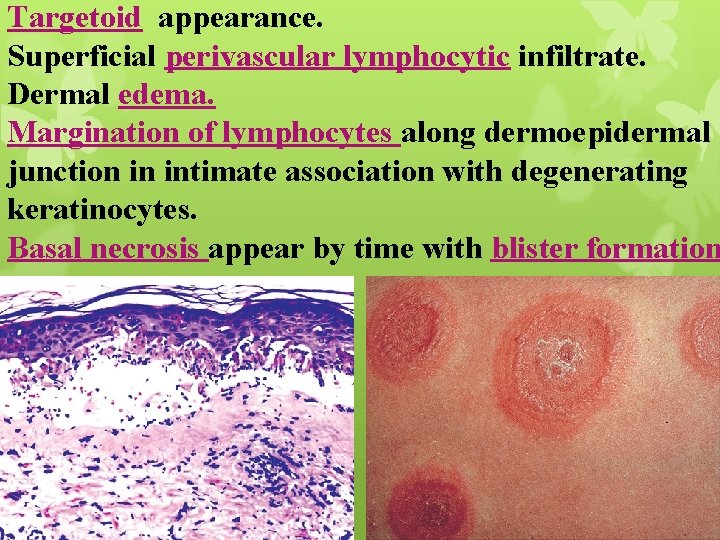
Targetoid appearance. Superficial perivascular lymphocytic infiltrate. Dermal edema. Margination of lymphocytes along dermoepidermal junction in intimate association with degenerating keratinocytes. Basal necrosis appear by time with blister formation
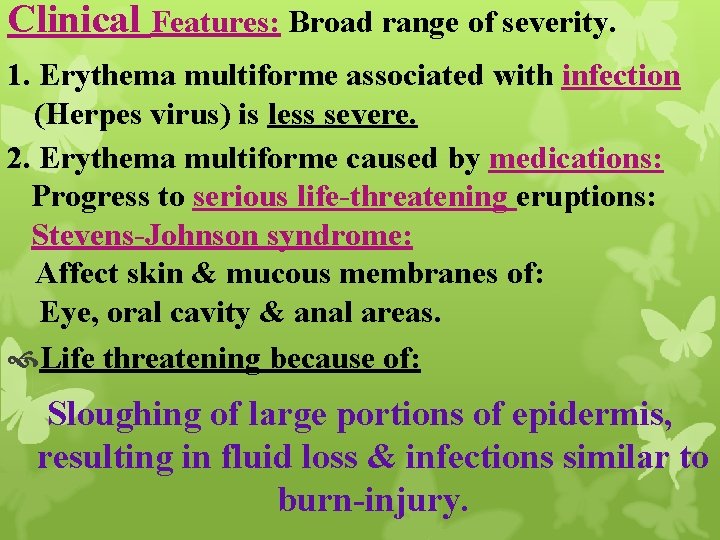
Clinical Features: Broad range of severity. 1. Erythema multiforme associated with infection (Herpes virus) is less severe. 2. Erythema multiforme caused by medications: Progress to serious life-threatening eruptions: Stevens-Johnson syndrome: Affect skin & mucous membranes of: Eye, oral cavity & anal areas. Life threatening because of: Sloughing of large portions of epidermis, resulting in fluid loss & infections similar to burn-injury.
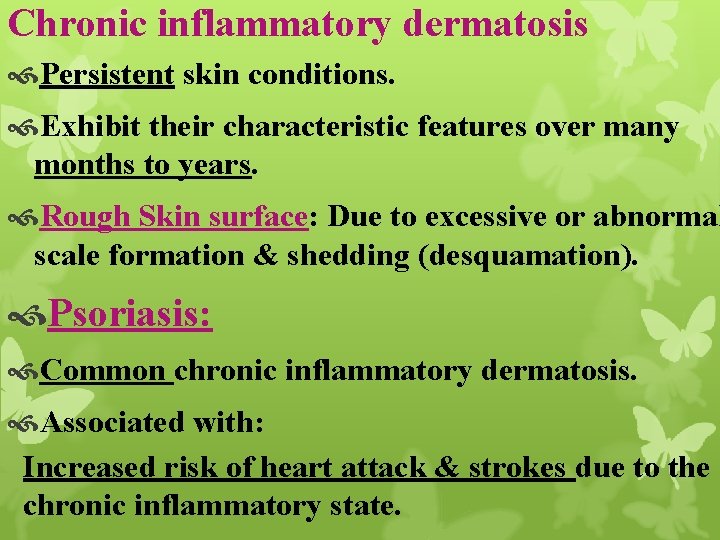
Chronic inflammatory dermatosis Persistent skin conditions. Exhibit their characteristic features over many months to years. Rough Skin surface: Due to excessive or abnormal scale formation & shedding (desquamation). Psoriasis: Common chronic inflammatory dermatosis. Associated with: Increased risk of heart attack & strokes due to the chronic inflammatory state.
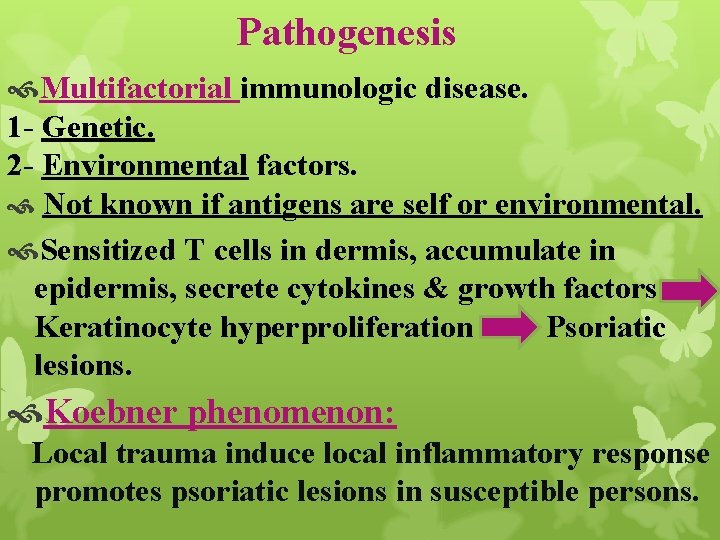
Pathogenesis Multifactorial immunologic disease. 1 - Genetic. 2 - Environmental factors. Not known if antigens are self or environmental. Sensitized T cells in dermis, accumulate in epidermis, secrete cytokines & growth factors Keratinocyte hyperproliferation Psoriatic lesions. Koebner phenomenon: Local trauma induce local inflammatory response promotes psoriatic lesions in susceptible persons.

Morphology Clinical: Well-demarcated, pink to salmon–colored plaque covered by loosely adherent silvery-white scale. Microscopy: Acanthosis (epidermal thickening). Downward elongation of rete ridges. Increased epidermal cell turnover & lack of maturation will lead to: 1 - Loss of stratum granulosum. 2 - Extensive parakeratotic scale.
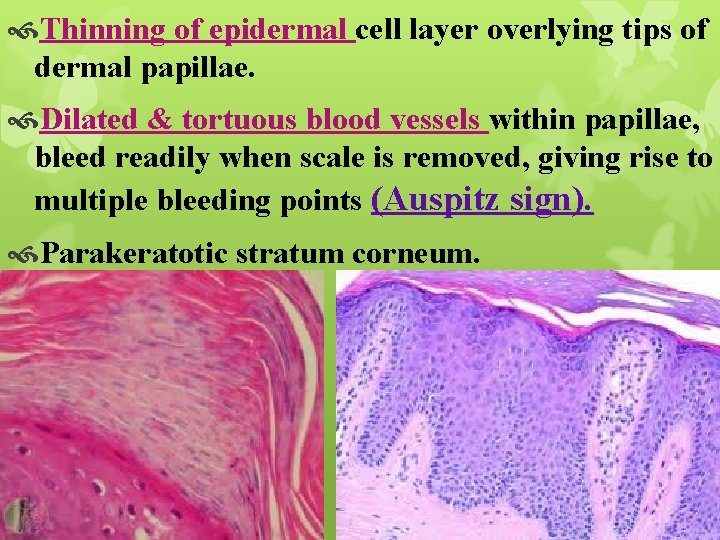
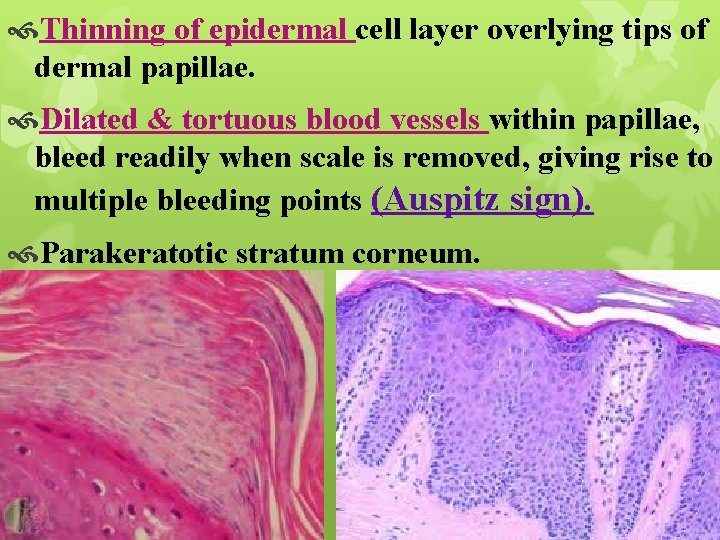
Thinning of epidermal cell layer overlying tips of dermal papillae. Dilated & tortuous blood vessels within papillae, bleed readily when scale is removed, giving rise to multiple bleeding points (Auspitz sign). Parakeratotic stratum corneum.
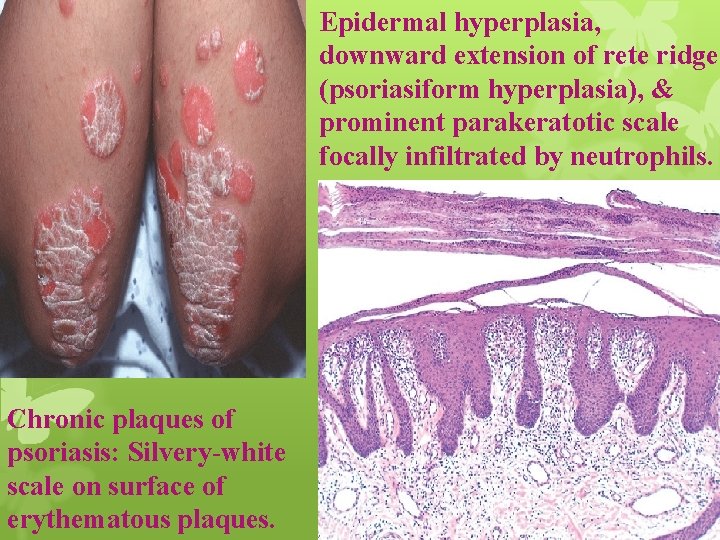
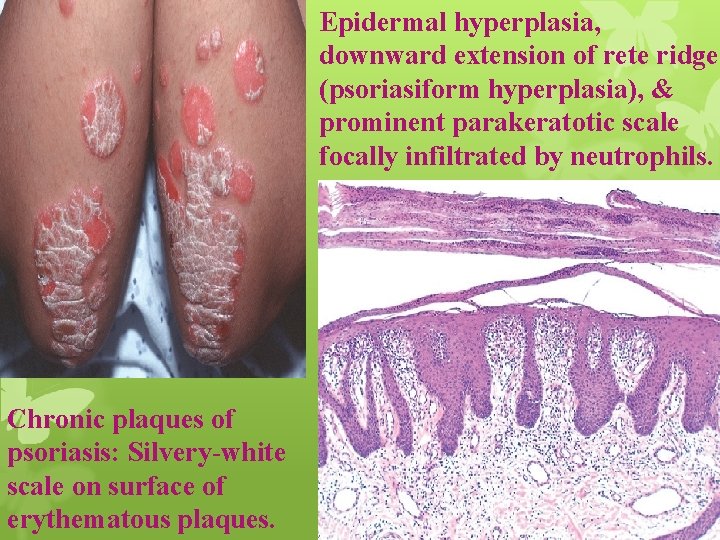
Epidermal hyperplasia, downward extension of rete ridges (psoriasiform hyperplasia), & prominent parakeratotic scale focally infiltrated by neutrophils. Chronic plaques of psoriasis: Silvery-white scale on surface of erythematous plaques.
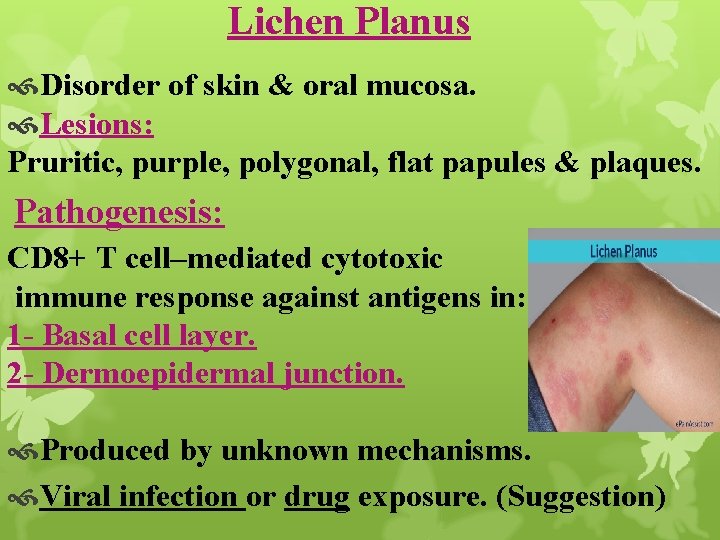
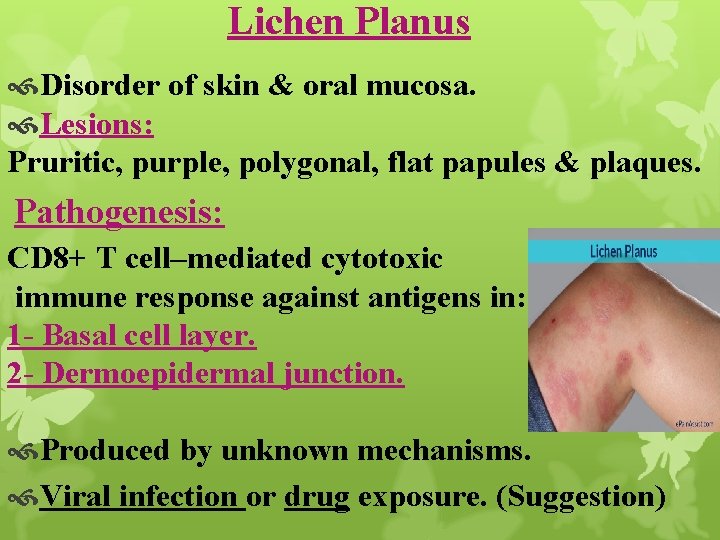
Lichen Planus Disorder of skin & oral mucosa. Lesions: Pruritic, purple, polygonal, flat papules & plaques. Pathogenesis: CD 8+ T cell–mediated cytotoxic immune response against antigens in: 1 - Basal cell layer. 2 - Dermoepidermal junction. Produced by unknown mechanisms. Viral infection or drug exposure. (Suggestion)

Morphology Cutaneous lesions: Pruritic, violaceous, flat-topped papules, may coalesce focally to form plaques. Papules are highlighted by white dots or lacelike lines called Wickham striae.
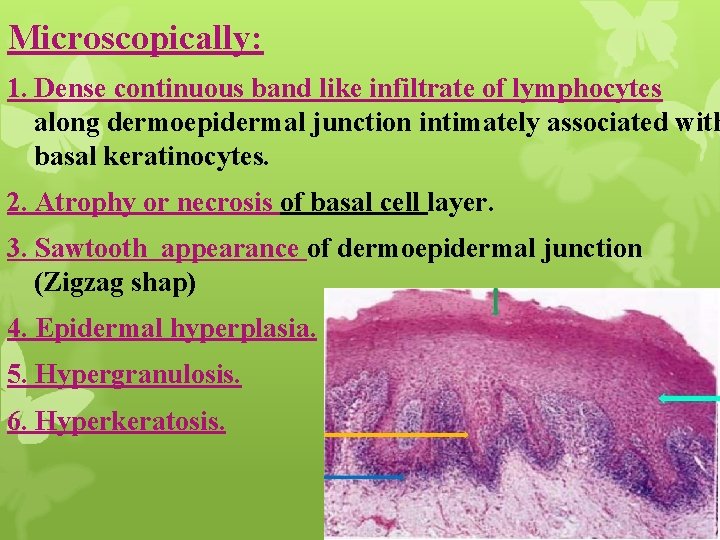
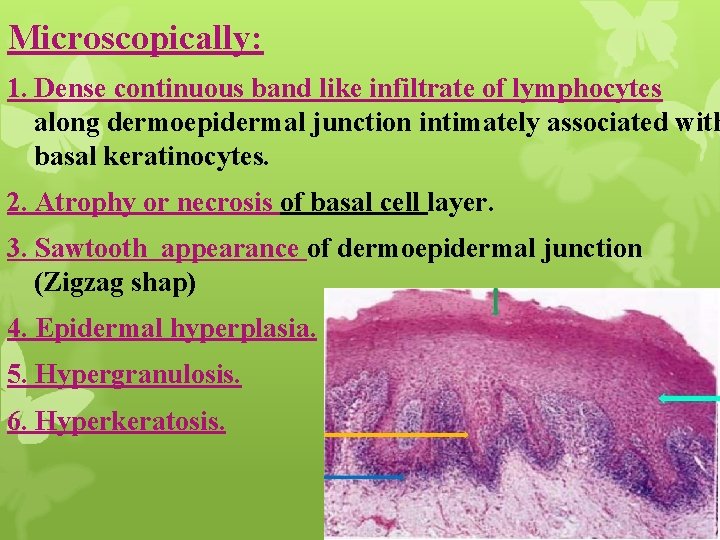
Microscopically: 1. Dense continuous band like infiltrate of lymphocytes along dermoepidermal junction intimately associated with basal keratinocytes. 2. Atrophy or necrosis of basal cell layer. 3. Sawtooth appearance of dermoepidermal junction (Zigzag shap) 4. Epidermal hyperplasia. 5. Hypergranulosis. 6. Hyperkeratosis.
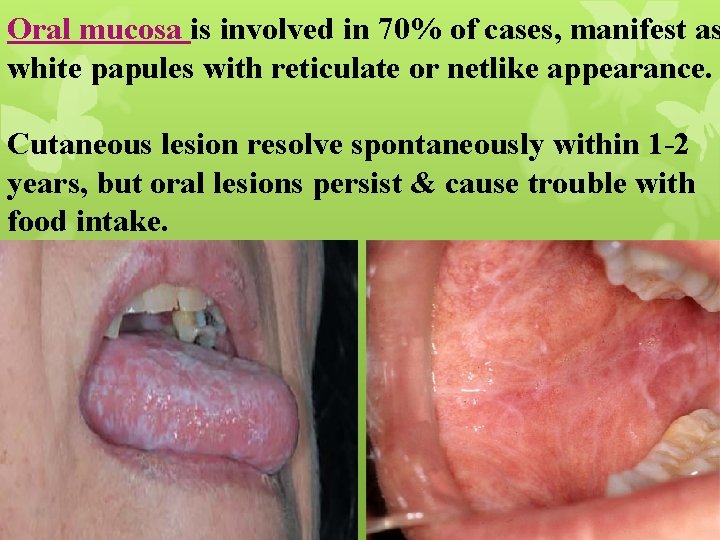
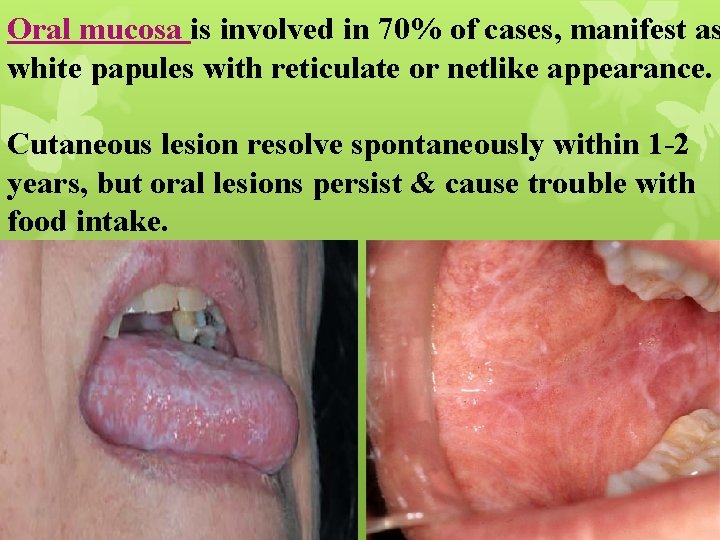
Oral mucosa is involved in 70% of cases, manifest as white papules with reticulate or netlike appearance. Cutaneous lesion resolve spontaneously within 1 -2 years, but oral lesions persist & cause trouble with food intake.
Thank you