SKIN CANCER Jody Gooding Linsey Sekulich Brandi Kusumoto

SKIN CANCER Jody Gooding Linsey Sekulich Brandi Kusumoto
PRE Questions 1. What are three MOST COMMON types of skin cancer? (select all that apply) a. Basal cell carcinoma b. Merkel cell carcinoma c. Squamous cell carcinoma d. Melanoma 2. Which of the following is NOT included in the ABCDE method for self assessing lesions? a. Consistency

Disease characterized by uncontrolled growth of abnormal skin cells As cells become more abnormal, old or damaged cells survive when they should have died Exposure to ultraviolet radiation of the sun, irritating chemicals, recurrent trauma, and irradiation Overexposure to sunlight is the major cause of skin cancer Extra cells divide without stopping and may form tumors People with light complexions have a higher rate of skin cancer than those with dark complexions Males are more likely to develop skin cancer than females
https: //infograph. venngage. com/p/107403/skin-cancer-cc
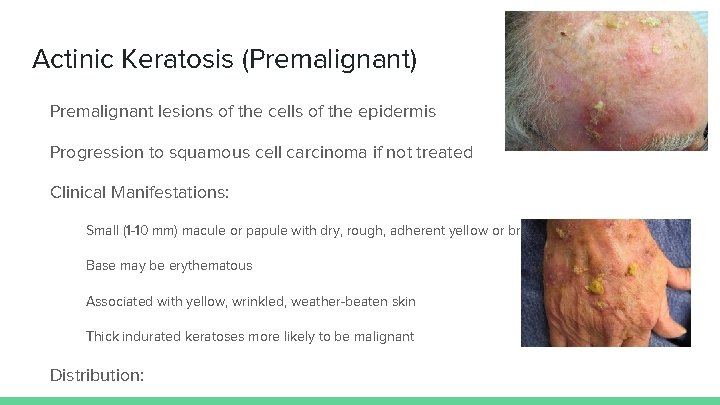
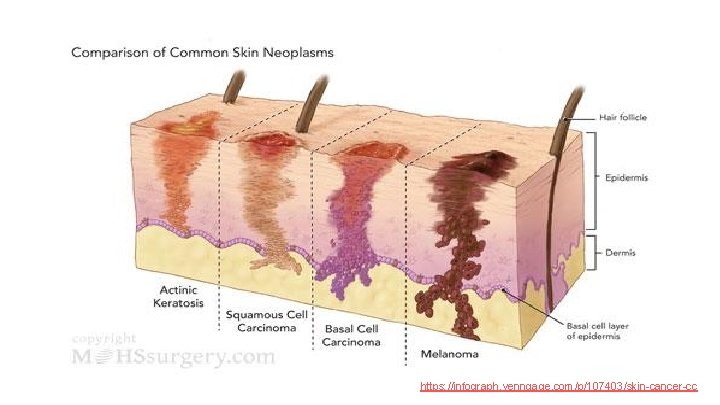
Actinic Keratosis (Premalignant) Premalignant lesions of the cells of the epidermis Progression to squamous cell carcinoma if not treated Clinical Manifestations: Small (1 -10 mm) macule or papule with dry, rough, adherent yellow or brown scales Base may be erythematous Associated with yellow, wrinkled, weather-beaten skin Thick indurated keratoses more likely to be malignant Distribution:
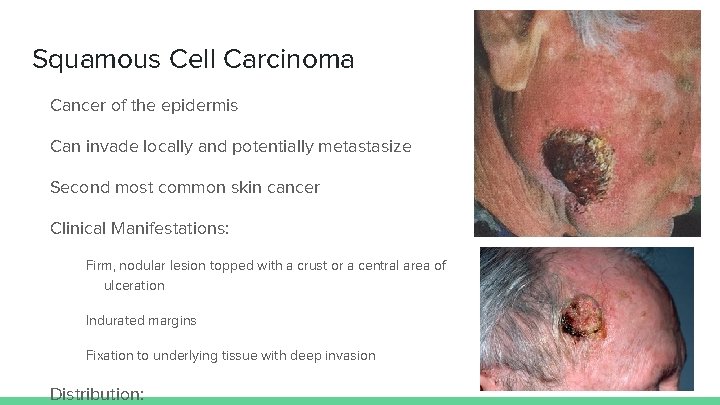
Squamous Cell Carcinoma Cancer of the epidermis Can invade locally and potentially metastasize Second most common skin cancer Clinical Manifestations: Firm, nodular lesion topped with a crust or a central area of ulceration Indurated margins Fixation to underlying tissue with deep invasion Distribution:
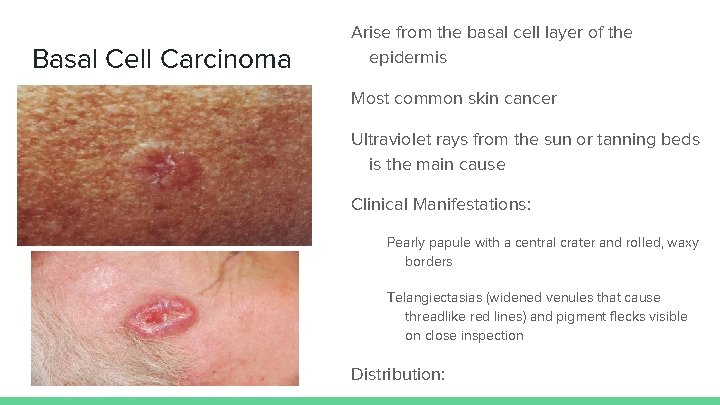
Basal Cell Carcinoma Arise from the basal cell layer of the epidermis Most common skin cancer Ultraviolet rays from the sun or tanning beds is the main cause Clinical Manifestations: Pearly papule with a central crater and rolled, waxy borders Telangiectasias (widened venules that cause threadlike red lines) and pigment flecks visible on close inspection Distribution:
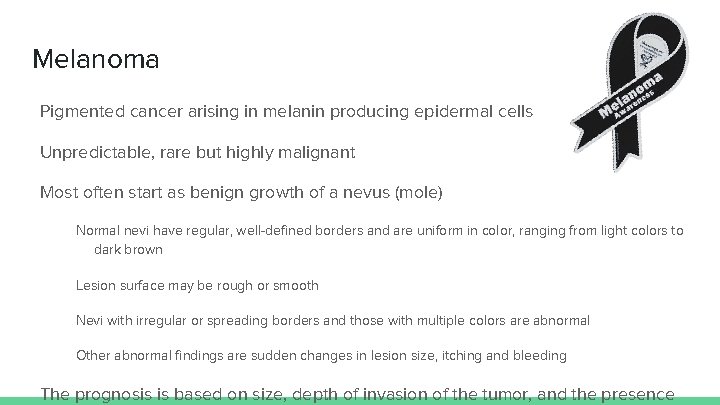
Melanoma Pigmented cancer arising in melanin producing epidermal cells Unpredictable, rare but highly malignant Most often start as benign growth of a nevus (mole) Normal nevi have regular, well-defined borders and are uniform in color, ranging from light colors to dark brown Lesion surface may be rough or smooth Nevi with irregular or spreading borders and those with multiple colors are abnormal Other abnormal findings are sudden changes in lesion size, itching and bleeding The prognosis is based on size, depth of invasion of the tumor, and the presence

Melanoma Cont. Clinical Manifestations: Irregularly shaped, pigmented papule or plaque Variegated colors, with red, white and blue tones Distribution: Can occur anywhere on the body, especially where nevi (moles) or birthmarks are evident Commonly found on upper back, lower legs, soles of feet and palms in dark-skinned people Course
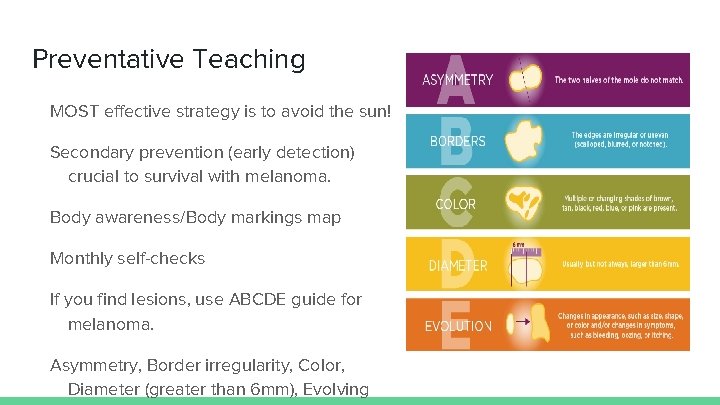
Preventative Teaching MOST effective strategy is to avoid the sun! Secondary prevention (early detection) crucial to survival with melanoma. Body awareness/Body markings map Monthly self-checks If you find lesions, use ABCDE guide for melanoma. Asymmetry, Border irregularity, Color, Diameter (greater than 6 mm), Evolving
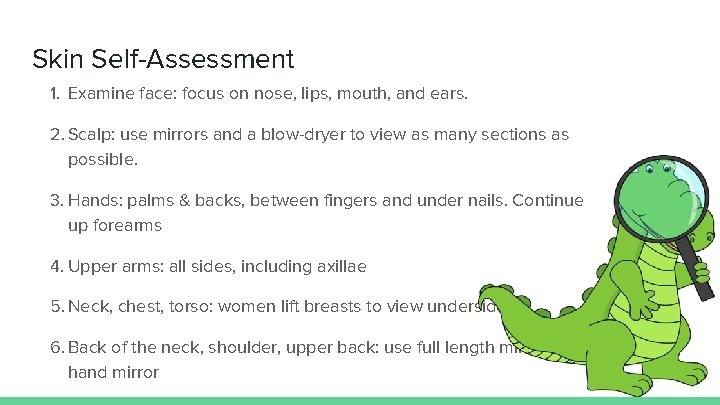
Skin Self-Assessment 1. Examine face: focus on nose, lips, mouth, and ears. 2. Scalp: use mirrors and a blow-dryer to view as many sections as possible. 3. Hands: palms & backs, between fingers and under nails. Continue up forearms 4. Upper arms: all sides, including axillae 5. Neck, chest, torso: women lift breasts to view underside 6. Back of the neck, shoulder, upper back: use full length mirror and hand mirror
Seek Medical Advice if you note any of these: A change in color of a lesion, especially if it darkens or shows evidence of spreading A change in the size of a lesion, especially rapid growth A change in the shape of a lesion, such as a sharp border becoming irregular or a flat lesion becoming raised Redness or swelling of the skin around a lesion A change in sensation, especially itching or increased tenderness of a lesion A change in the character of a lesion, such as oozing, crusting, bleeding, or scaling
Interventions Surgical and Nonsurgical interventions are combined for effective treatment in skin cancer. Treatment is determined by the size and severity of the malignancy, the location of the lesion, and the age and general health of the patient.
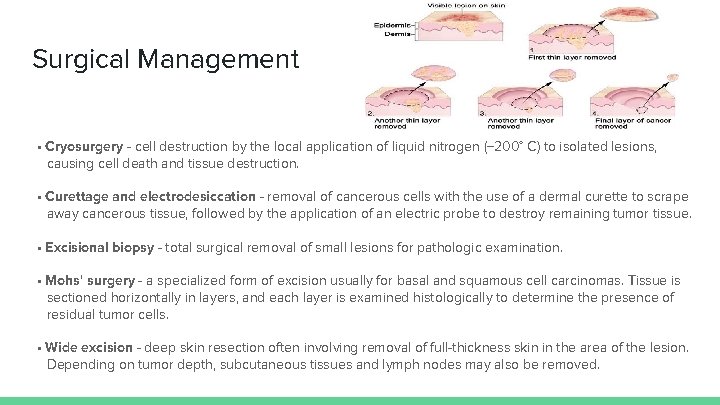
Surgical Management • Cryosurgery - cell destruction by the local application of liquid nitrogen (− 200° C) to isolated lesions, causing cell death and tissue destruction. • Curettage and electrodesiccation - removal of cancerous cells with the use of a dermal curette to scrape away cancerous tissue, followed by the application of an electric probe to destroy remaining tumor tissue. • Excisional biopsy - total surgical removal of small lesions for pathologic examination. • Mohs' surgery - a specialized form of excision usually for basal and squamous cell carcinomas. Tissue is sectioned horizontally in layers, and each layer is examined histologically to determine the presence of residual tumor cells. • Wide excision - deep skin resection often involving removal of full-thickness skin in the area of the lesion. Depending on tumor depth, subcutaneous tissues and lymph nodes may also be removed.
Nonsurgical Management Topical Therapy - Used to treat multiple actinic keratosis or for widespread superficial basal cell carcinoma. Therapy is continued for several weeks, and treated areas become increasingly tender and inflamed as lesions crust, ooze, and erode. Prepare patient for an unsightly appearance during therapy, and reassure them that cosmetic result will be positive. Systemic Chemotherapy - Systemic chemotherapeutic agents are used in treatment of locally advanced or metastatic squamous cell skin cancer.
Nonsurgical Management Cont. Biotherapy - Biotherapy with interferon, monoclonal antibodies, and targeted therapy are now accepted treatment for melanoma after surgical removal. Interferon is used for melanomas that are at stage III or higher. Monoclonal antibody therapy leads to greater T-cell lymphocyte activity. Targeted therapy is available for melanomas with specific mutation in the BRAF gene. Radiation Therapy - When used for skin cancer is limited to older patients with large, deeply invasive basal cell tumors and to those who are poor risks for surgery. Melanoma is relatively resistant to radiation therapy.
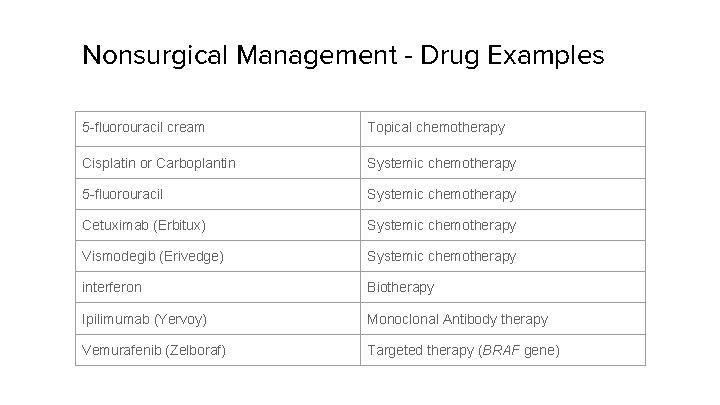
Nonsurgical Management - Drug Examples 5 -fluorouracil cream Topical chemotherapy Cisplatin or Carboplantin Systemic chemotherapy 5 -fluorouracil Systemic chemotherapy Cetuximab (Erbitux) Systemic chemotherapy Vismodegib (Erivedge) Systemic chemotherapy interferon Biotherapy Ipilimumab (Yervoy) Monoclonal Antibody therapy Vemurafenib (Zelboraf) Targeted therapy (BRAF gene)
POST Questions 1. What are three MOST COMMON types of skin cancer? (select all that apply) a. Basal cell carcinoma b. Merkel cell carcinoma c. Squamous cell carcinoma d. Melanoma 2. Which of the following is NOT included in the ABCDE method for self assessing lesions? a. Consistency b. Diameter
References Copstead, L. C. , & Banasik, J. L. (2013). Pathophysiology (5 th ed. ). St. Louis, MO: Elsevier. Ignatavicius, D. D. , & Workman, M. L. (2016). Medical-surgical nursing: patientcentered collaborative care (8 th ed. ). St. Louis, MO: Elsevier. National Cancer institute (https: //www. cancer. gov/)
- Slides: 19