Skin and SoftTissue Infections Superficial lesions vs Deadly
- Slides: 18
Skin and Soft-Tissue Infections Superficial lesions vs Deadly disease Outpatient Management and Indications for Hospitalization Nayef El-Daher, MD, Ph. D Richard Magnussen, MD J Crit Illness, 1998; 13(3): 151 -160 3/98 medslides. com 1
Skin and soft-tissue Infections • Localized infections – cellulitis – erysipelas • Potentially lethal infections – necrotizing fascitis – myonecrosis – pyomyositis 3/98 medslides. com 2
Cellulitis and Erysipelas pathogenesis • Cellulitis – group A streptococci typically follows an innocuous or unrecognized injury; inflammation is diffuse, spreading along tissue planes – staphylococcus aureus usually associated with wound or penetrating trauma; localized abscess become surrounded by cellulitis 3/98 medslides. com 3
Cellulitis and Erysipelas pathogenesis • Erysipelas – caused most often by group A streptococci – rarely cased by ß-hemolytic streptococci of the B, C, or G serologic group 3/98 medslides. com 4
Cellulitis and Erysipelas diagnosis • General features – varying degrees of skin or soft-tissue erythema, warmth, edema, and pain – associated fever and leukocytosis – history of trauma, abrasion, or skin ulceration (not reported by every patient) 3/98 medslides. com 5
Cellulitis and Erysipelas diagnosis • physical exam – cellulitis has an ill-defined border that merge smoothly with adjacent skin; usually pinkish to redish – erysipelas has an elevated and sharply demarcated border with a fiery-red appearance 3/98 medslides. com 6
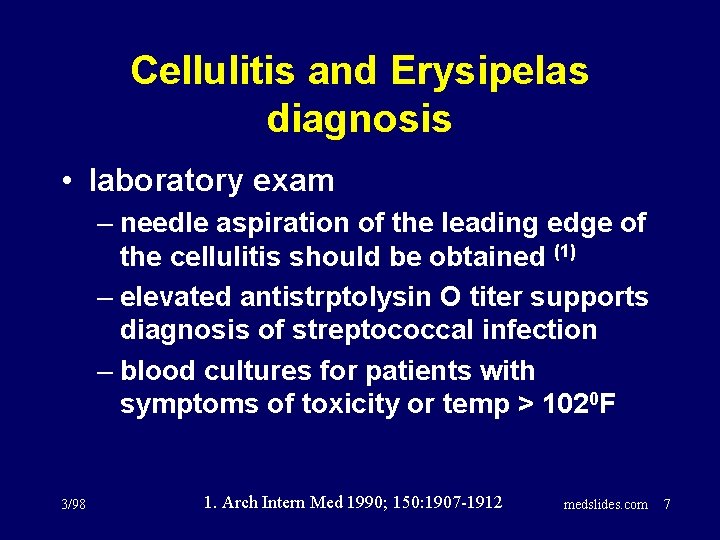
Cellulitis and Erysipelas diagnosis • laboratory exam – needle aspiration of the leading edge of the cellulitis should be obtained (1) – elevated antistrptolysin O titer supports diagnosis of streptococcal infection – blood cultures for patients with symptoms of toxicity or temp > 1020 F 3/98 1. Arch Intern Med 1990; 150: 1907 -1912 medslides. com 7
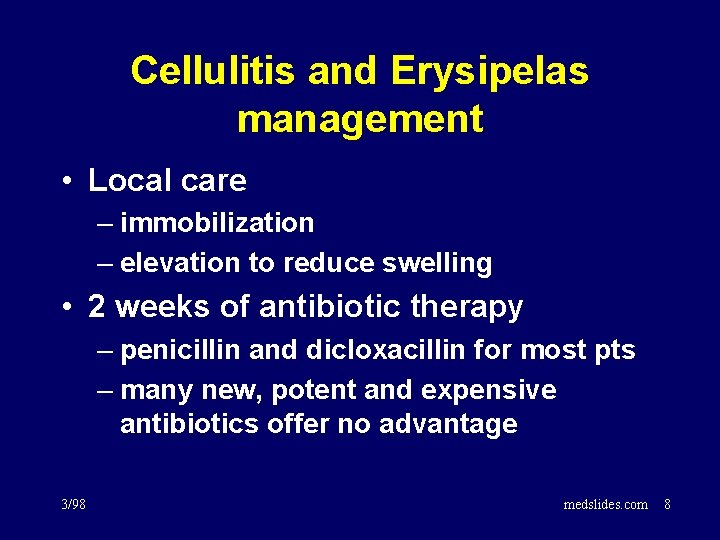
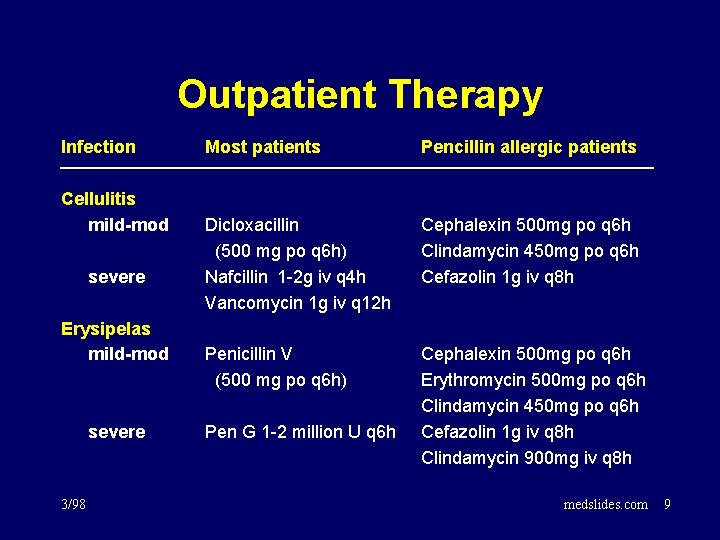
Cellulitis and Erysipelas management • Local care – immobilization – elevation to reduce swelling • 2 weeks of antibiotic therapy – penicillin and dicloxacillin for most pts – many new, potent and expensive antibiotics offer no advantage 3/98 medslides. com 8
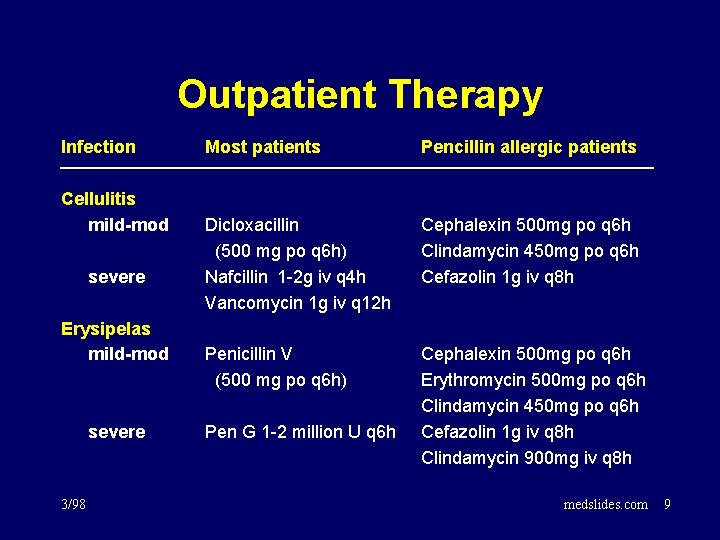
Outpatient Therapy Infection Cellulitis mild-mod severe Erysipelas mild-mod severe 3/98 Most patients Pencillin allergic patients Dicloxacillin (500 mg po q 6 h) Nafcillin 1 -2 g iv q 4 h Vancomycin 1 g iv q 12 h Cephalexin 500 mg po q 6 h Clindamycin 450 mg po q 6 h Cefazolin 1 g iv q 8 h Penicillin V (500 mg po q 6 h) Cephalexin 500 mg po q 6 h Erythromycin 500 mg po q 6 h Clindamycin 450 mg po q 6 h Cefazolin 1 g iv q 8 h Clindamycin 900 mg iv q 8 h Pen G 1 -2 million U q 6 h medslides. com 9
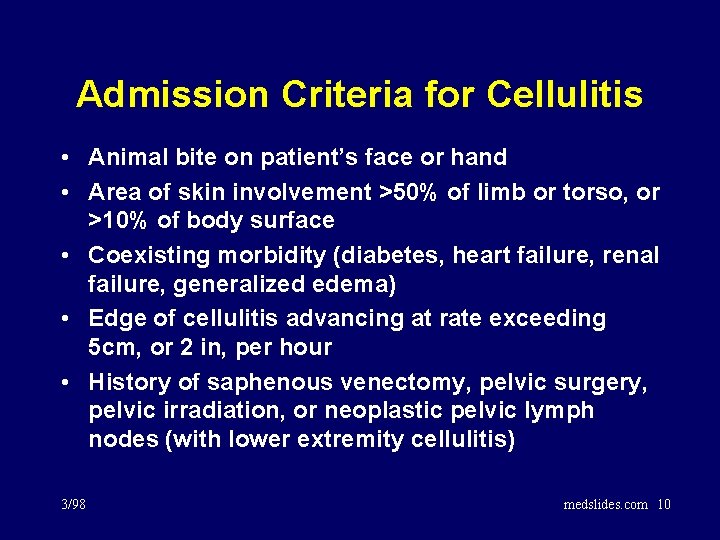
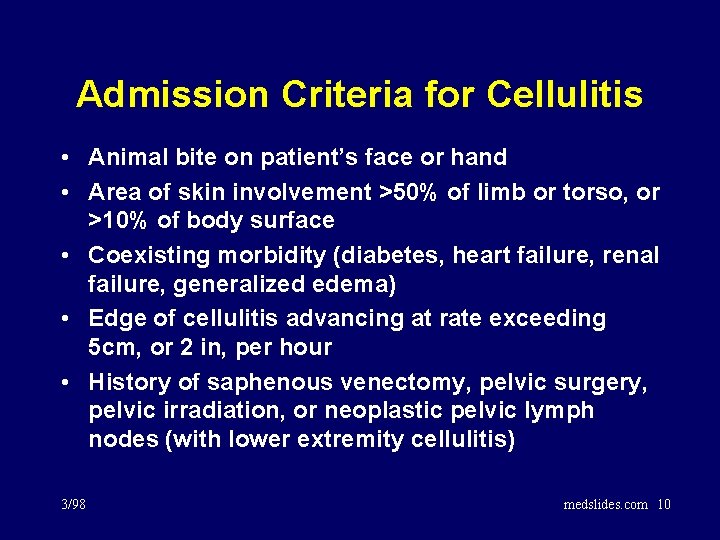
Admission Criteria for Cellulitis • Animal bite on patient’s face or hand • Area of skin involvement >50% of limb or torso, or >10% of body surface • Coexisting morbidity (diabetes, heart failure, renal failure, generalized edema) • Edge of cellulitis advancing at rate exceeding 5 cm, or 2 in, per hour • History of saphenous venectomy, pelvic surgery, pelvic irradiation, or neoplastic pelvic lymph nodes (with lower extremity cellulitis) 3/98 medslides. com 10
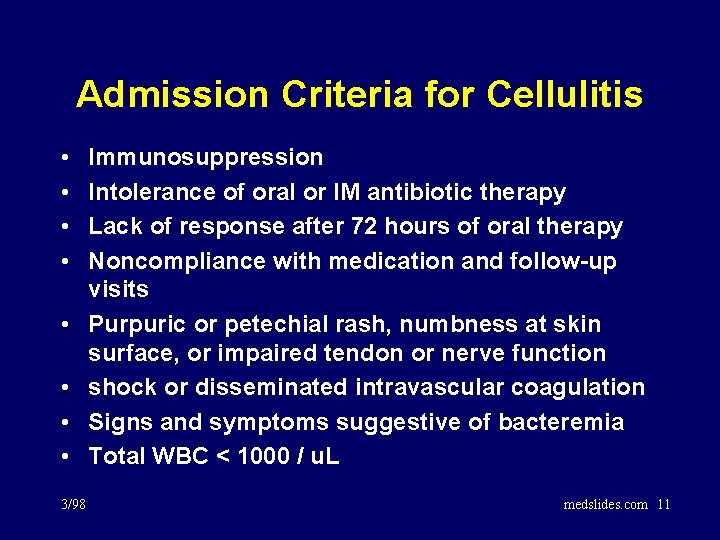
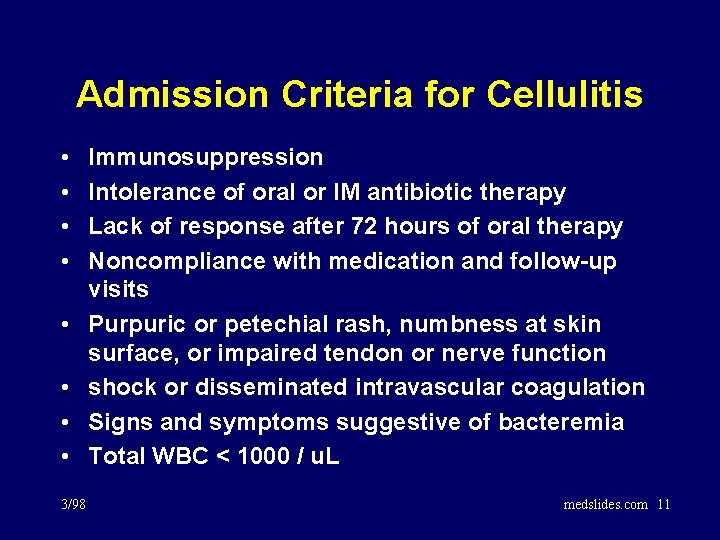
Admission Criteria for Cellulitis • • 3/98 Immunosuppression Intolerance of oral or IM antibiotic therapy Lack of response after 72 hours of oral therapy Noncompliance with medication and follow-up visits Purpuric or petechial rash, numbness at skin surface, or impaired tendon or nerve function shock or disseminated intravascular coagulation Signs and symptoms suggestive of bacteremia Total WBC < 1000 / u. L medslides. com 11
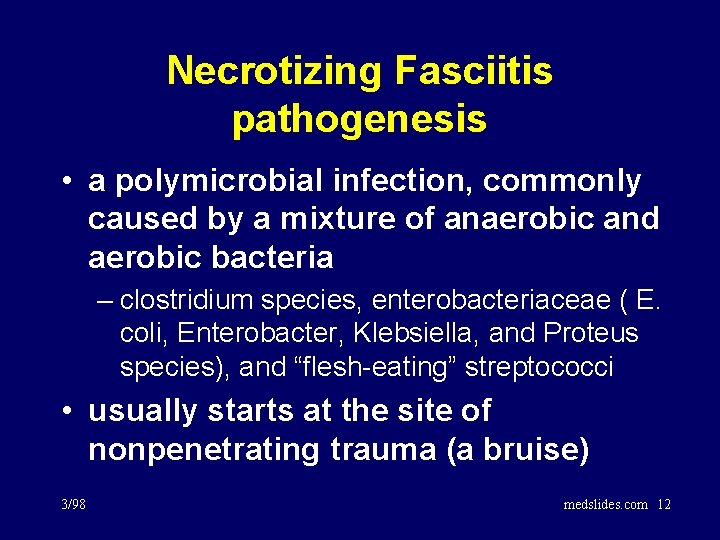
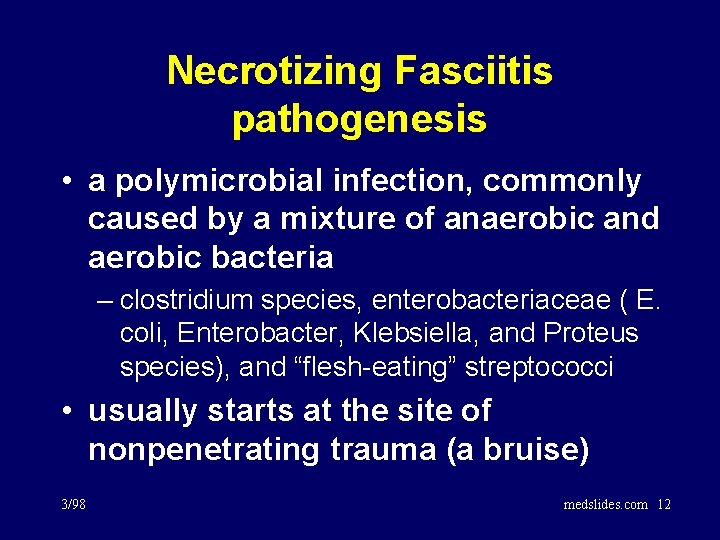
Necrotizing Fasciitis pathogenesis • a polymicrobial infection, commonly caused by a mixture of anaerobic and aerobic bacteria – clostridium species, enterobacteriaceae ( E. coli, Enterobacter, Klebsiella, and Proteus species), and “flesh-eating” streptococci • usually starts at the site of nonpenetrating trauma (a bruise) 3/98 medslides. com 12
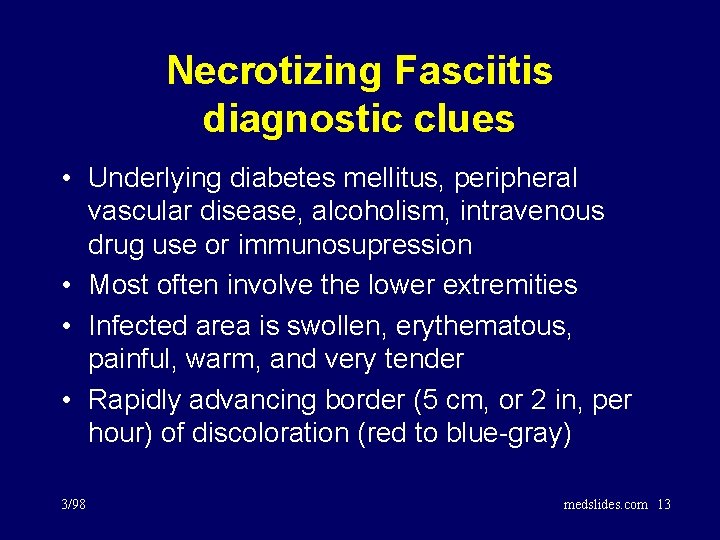
Necrotizing Fasciitis diagnostic clues • Underlying diabetes mellitus, peripheral vascular disease, alcoholism, intravenous drug use or immunosupression • Most often involve the lower extremities • Infected area is swollen, erythematous, painful, warm, and very tender • Rapidly advancing border (5 cm, or 2 in, per hour) of discoloration (red to blue-gray) 3/98 medslides. com 13
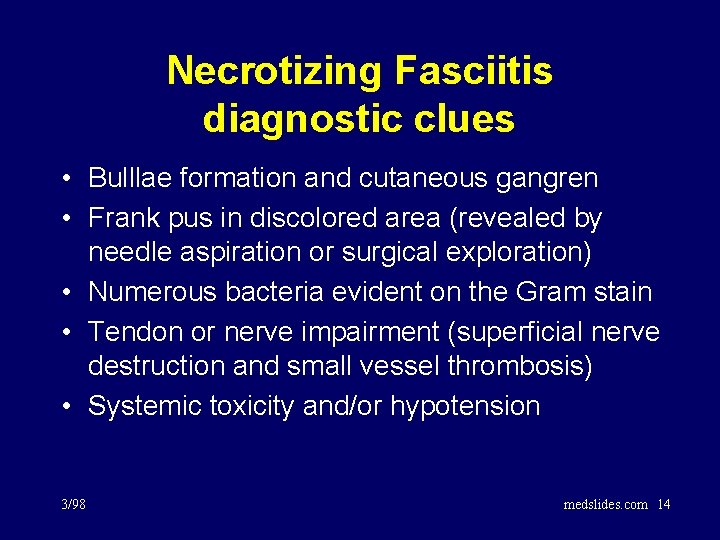
Necrotizing Fasciitis diagnostic clues • Bulllae formation and cutaneous gangren • Frank pus in discolored area (revealed by needle aspiration or surgical exploration) • Numerous bacteria evident on the Gram stain • Tendon or nerve impairment (superficial nerve destruction and small vessel thrombosis) • Systemic toxicity and/or hypotension 3/98 medslides. com 14
Necrotizing Fasciitis management • Immediate surgical debridement is critical and life saving • empiric antibiotics to cover anaerobes, gram negative bacilli, streptococci, and Staph aureus – pen+metronidazole+clindamycin+ceftriaxone – vancomycin+chloramphenicol – monotherapy with imipenem • antibiotics for a minimum of 3 wks 3/98 medslides. com 15
Myonecrosis (Gas Gangrene) • • a pure Clostridium perfringens infection gas in a gangrenous muscle group incubation period of hours to days local edema and pain accompanied by fever and tachycardia • discharge is serosanguinous, dirty, and foul • pen G (3 -4 million U q 4 h) or chloramphenicol • surgical removal of infected muscle 3/98 medslides. com 16
Pyomyositis (tropical myositis) • 50% with co-morbidity (diabetes, alcoholic liver disease, concurrent corticosteroid therapy, immunosuppression) • endemic in the tropics • area is indurated with a “woody” consistency; erythema and tenderness is minimal initially • fever and marked muscle tenderness may develop in 1 -3 weeks 3/98 medslides. com 17
Pyomyositis (tropical myositis) • Rhabdomyolysis - along with myoglobinuria and acute renal failure - may develop • Staph aureus is the most common organism • MRI or CT may show muscle enlargement • surgical drainage is essential • empiric antibiotics directed against Staph – nafcillin 2 g iv q 4 h – vancomycin 1 g iv q 12 h or cefazolin 1 g iv q 8 h 3/98 medslides. com 18