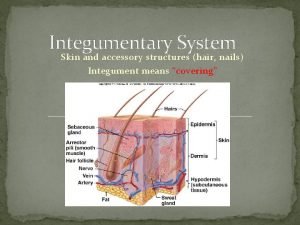
Skin and skin organs Integumentum commune David Kachlk


























- Slides: 96
Skin and skin organs Integumentum commune David Kachlík
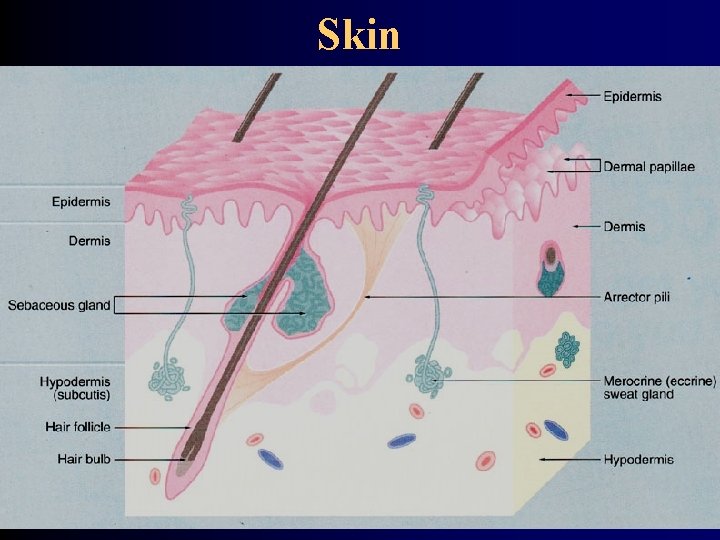
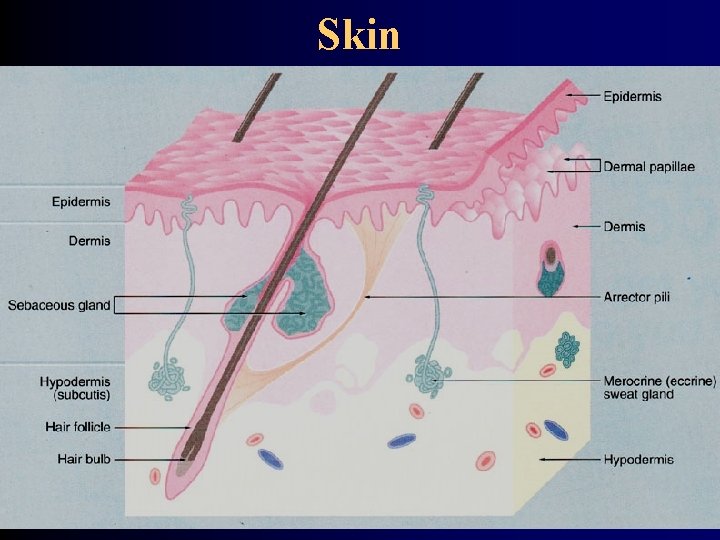
Skin
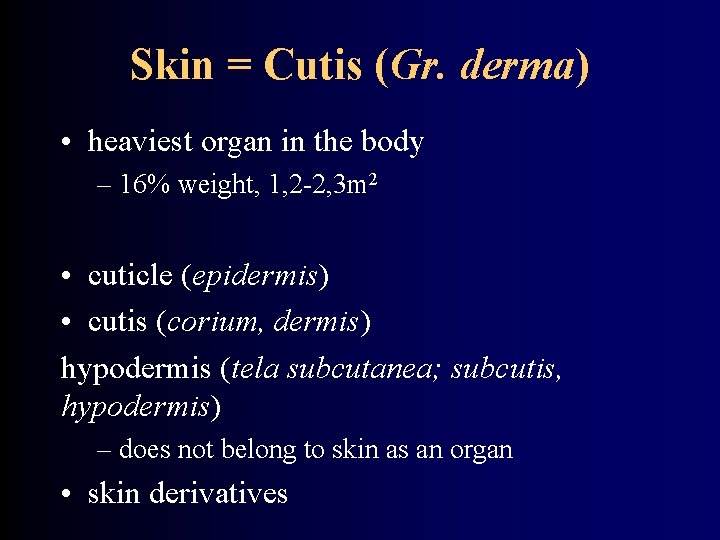
Skin = Cutis (Gr. derma) • heaviest organ in the body – 16% weight, 1, 2 -2, 3 m 2 • cuticle (epidermis) • cutis (corium, dermis) hypodermis (tela subcutanea; subcutis, hypodermis) – does not belong to skin as an organ • skin derivatives

Skin - function protection termoregulation Sudorific glands Changes in the blood flow (respiration) – perspiratio insensibilis excretion Absorption of medicaments immunity metabolism (ergosterol → vitamin D) Emotions and psychic
Skin - relief • skin grooves (sulci cutis) – in between of them rhomboid skin fields • Tactile crests (cristae cutis) – 9 types according to Purkynje → dactyloscopy • Tactile pillows (toruli tactiles) – 10 on hand (ce thenar) • Bending sulci (lineae distractiones) • Skin vincula (retinacula cutis) – (retinaculum caudale) • striae (striae cutaneae) – growth, gravidity, obesity

Bending sulci (lineae distractiones) • Sulci at joints, wrinkles • sulcus mentolabialis, nasolabialis, suprapalpebralis, infrapalpebralis • sulcus gluteus, crena ani • hand – Purkynje - chiromantia – linea oppositionis pollicis (vitalis) – linea manus clausae (cephalica, naturalis) – linea occlusionis dig. trium ulnarium (mensalis) – sulcus cutaneus intercarpalis (linea rasceta) – most proximal carpal – linea restricta – middle carpal
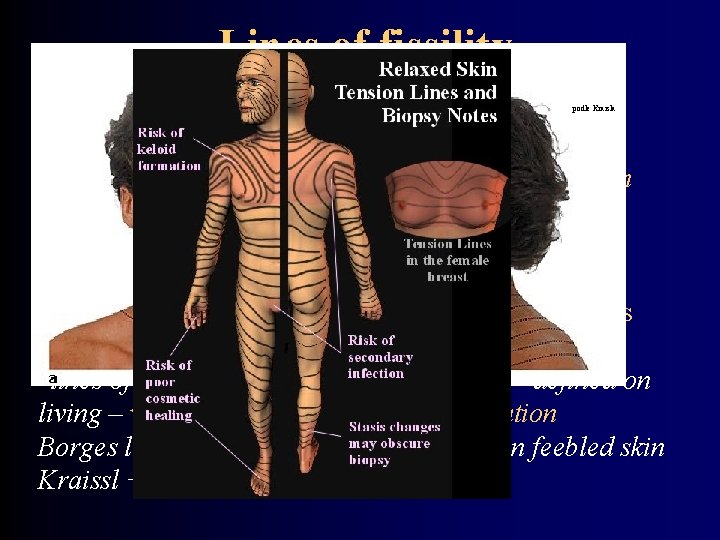
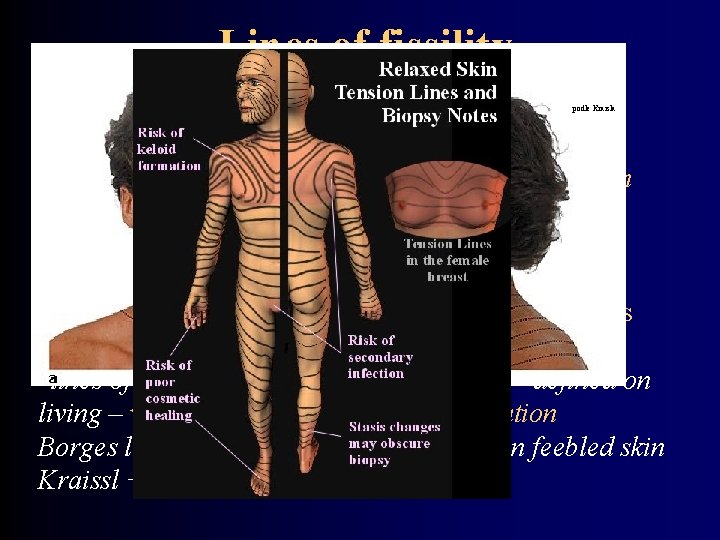
Lines of fissility podle Kraisla = Langers skin lines; cleavage lines; tension lines Runs in direction of fibril bundles in dermis (stratum reticulare) Vertical to direction of strongest pull Correspond to wrinkles on surface of skin Important in plastic surgery and for surgery incisions "lines of greatest tension" (Kraissls lines) – defined on living – vertical to muscle position orientation Borges lines – according to lines present in feebled skin Kraissl + Borges lines better effect
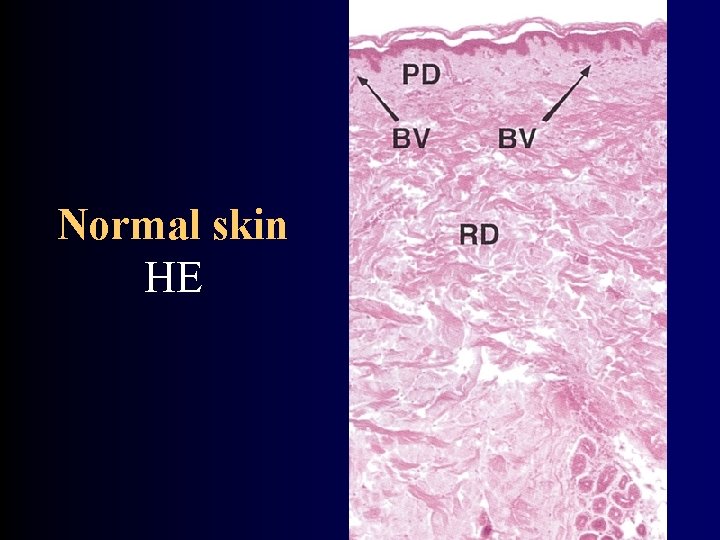
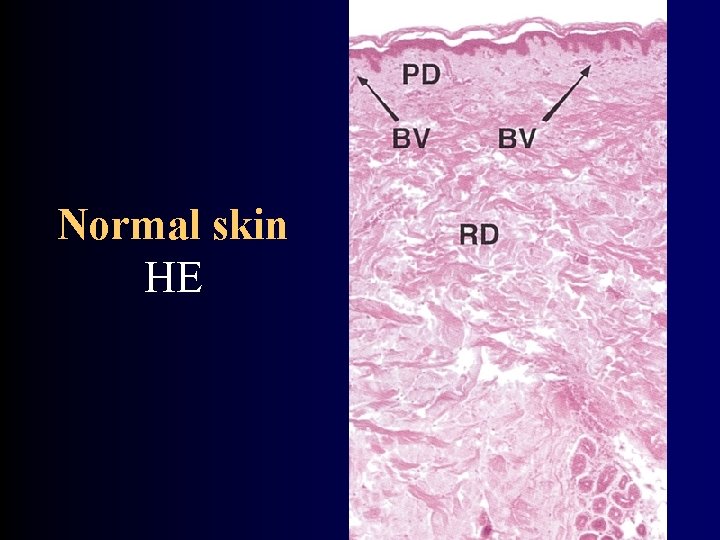
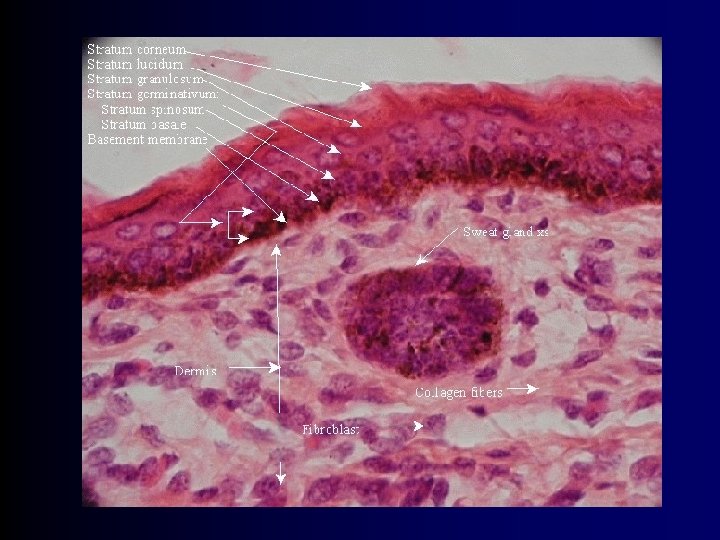
Normal skin HE

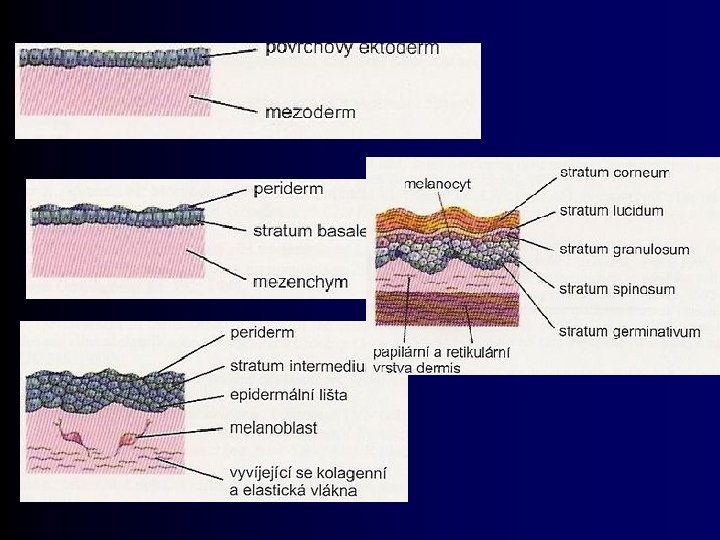
Skin - development ectoderm → epidermis (surface) mesoderm → dermis → Langerhans cells Neural crest → melanocytes → Merkels cells
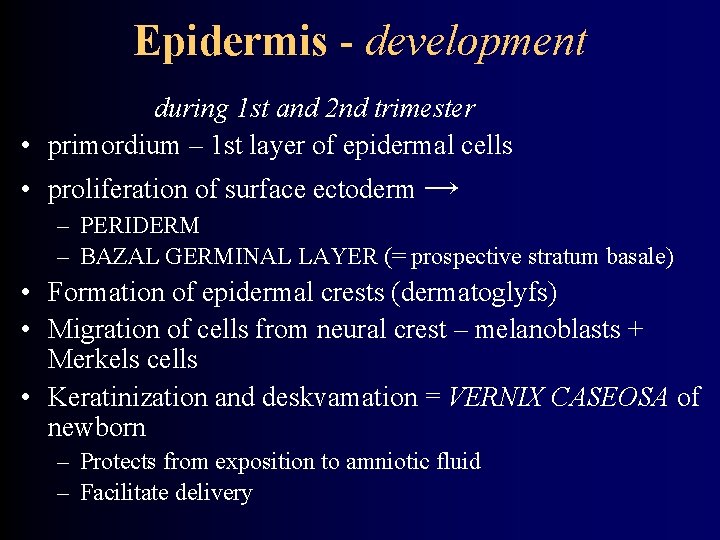
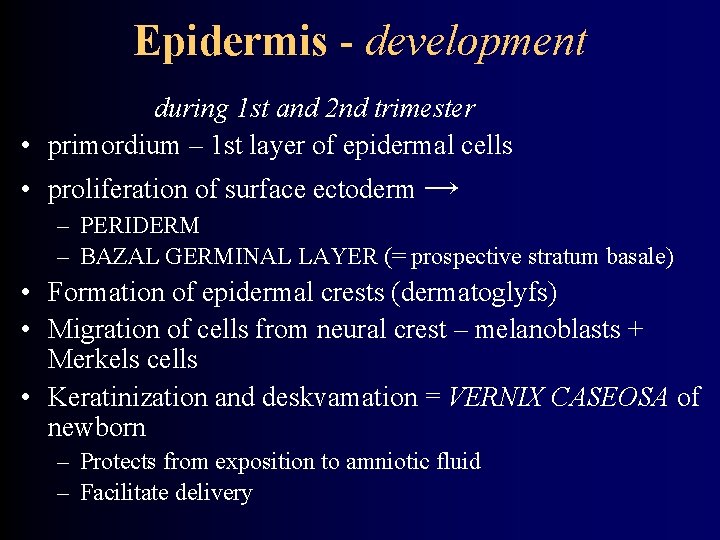
Epidermis - development during 1 st and 2 nd trimester • primordium – 1 st layer of epidermal cells • proliferation of surface ectoderm → – PERIDERM – BAZAL GERMINAL LAYER (= prospective stratum basale) • Formation of epidermal crests (dermatoglyfs) • Migration of cells from neural crest – melanoblasts + Merkels cells • Keratinization and deskvamation = VERNIX CASEOSA of newborn – Protects from exposition to amniotic fluid – Facilitate delivery
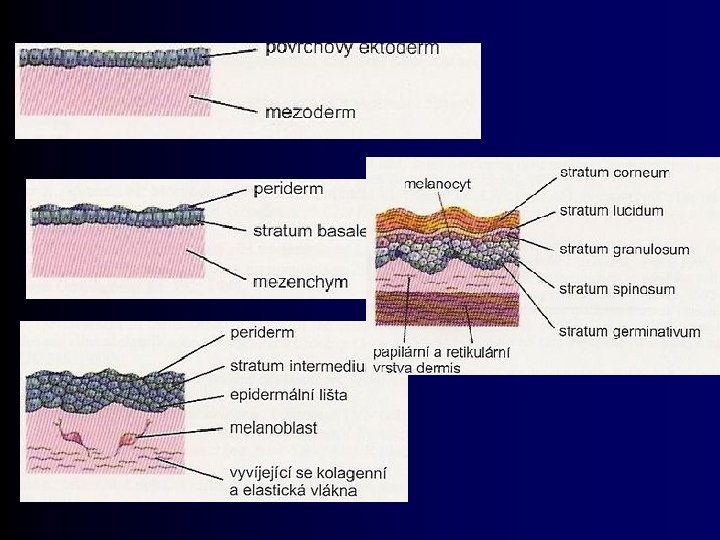
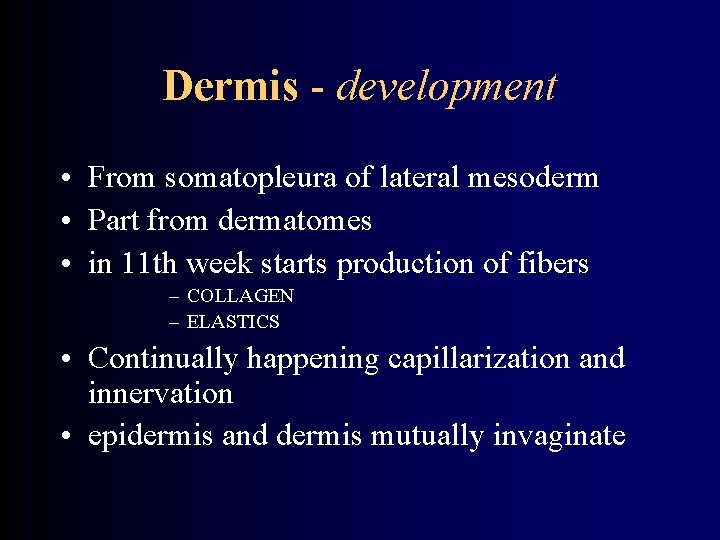
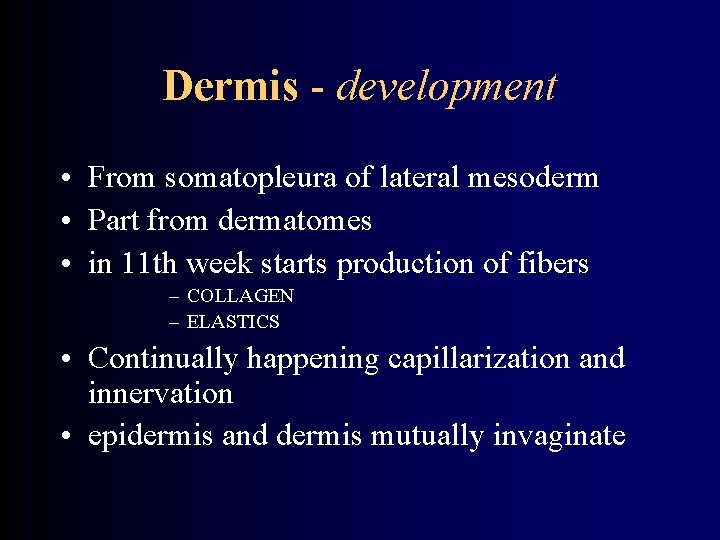
Dermis - development • From somatopleura of lateral mesoderm • Part from dermatomes • in 11 th week starts production of fibers – COLLAGEN – ELASTICS • Continually happening capillarization and innervation • epidermis and dermis mutually invaginate

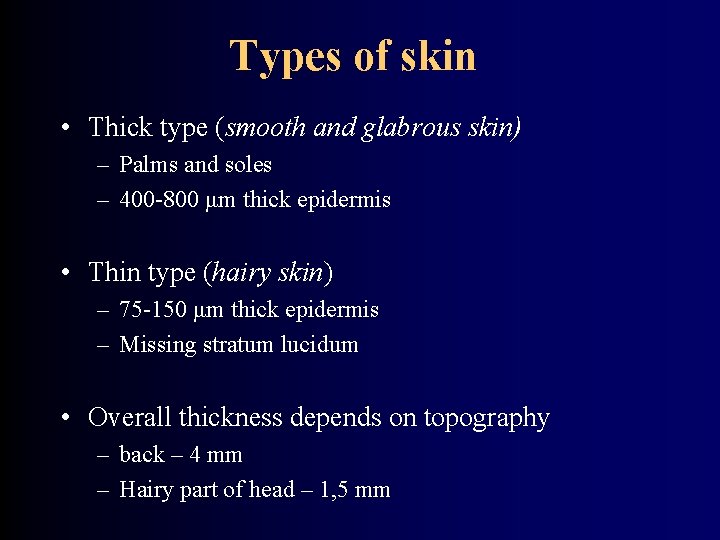
Types of skin • Thick type (smooth and glabrous skin) – Palms and soles – 400 -800 μm thick epidermis • Thin type (hairy skin) – 75 -150 μm thick epidermis – Missing stratum lucidum • Overall thickness depends on topography – back – 4 mm – Hairy part of head – 1, 5 mm
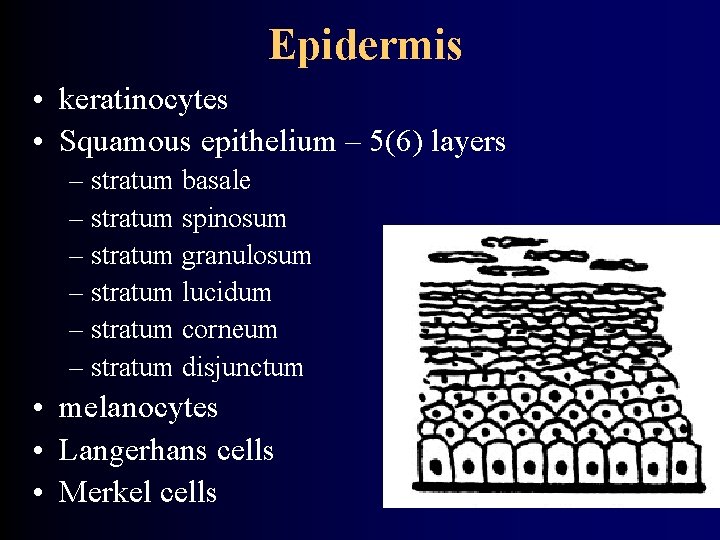
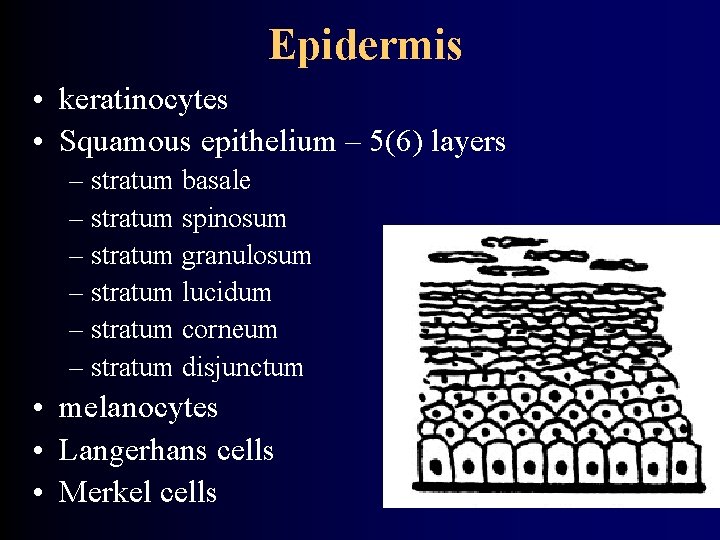
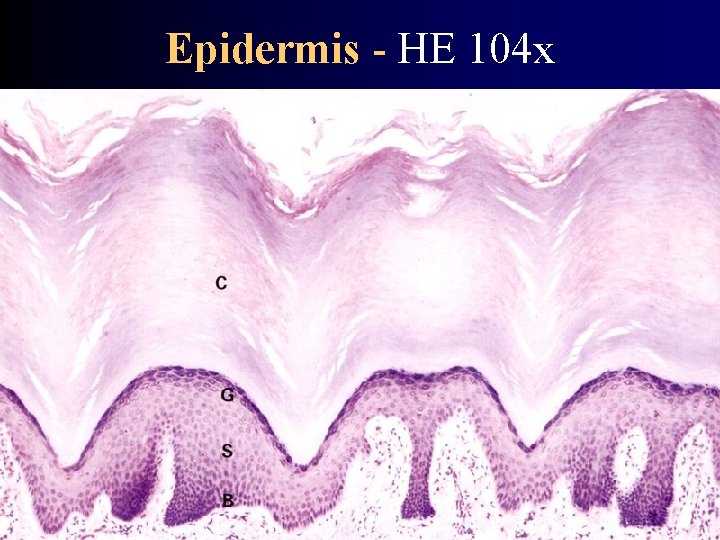
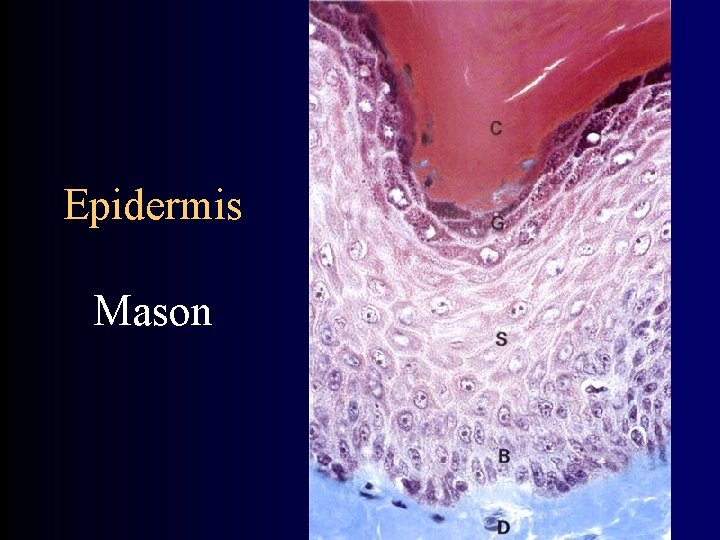
Epidermis • keratinocytes • Squamous epithelium – 5(6) layers – stratum basale – stratum spinosum – stratum granulosum – stratum lucidum – stratum corneum – stratum disjunctum • melanocytes • Langerhans cells • Merkel cells
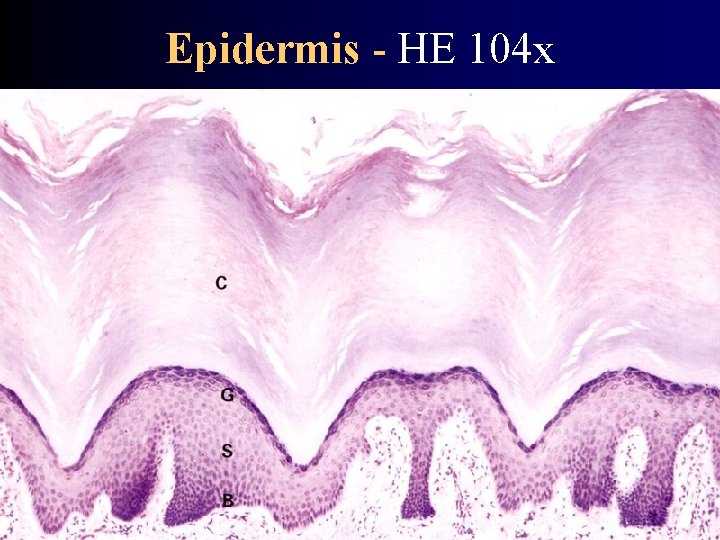
Epidermis - HE 104 x
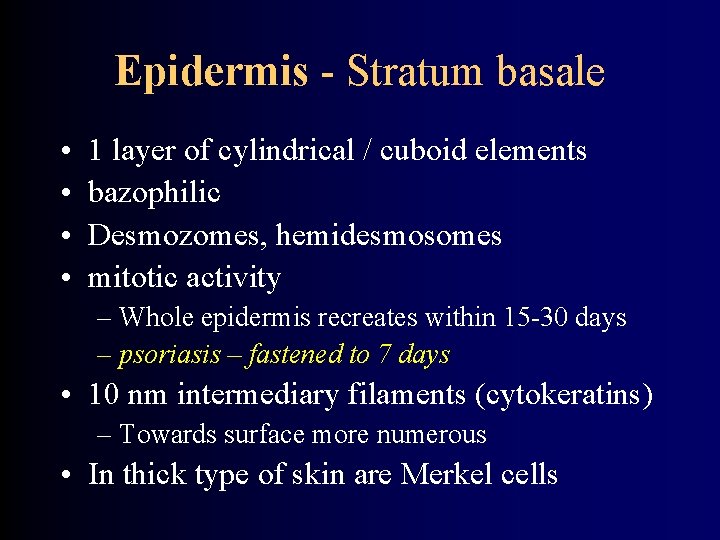
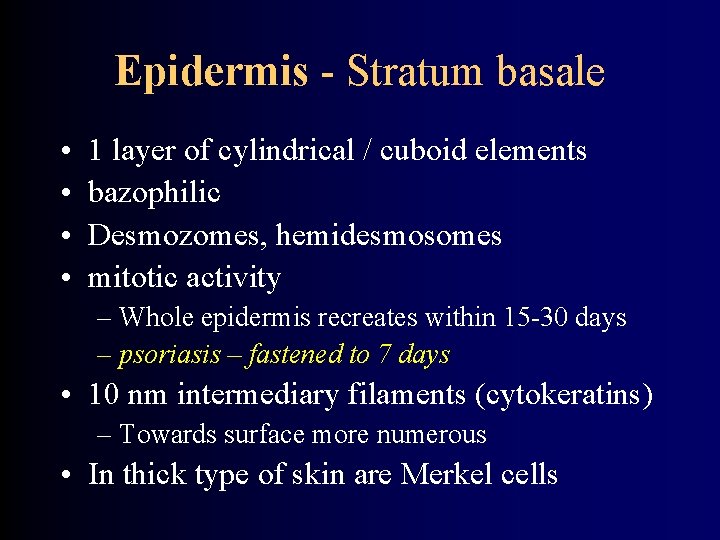
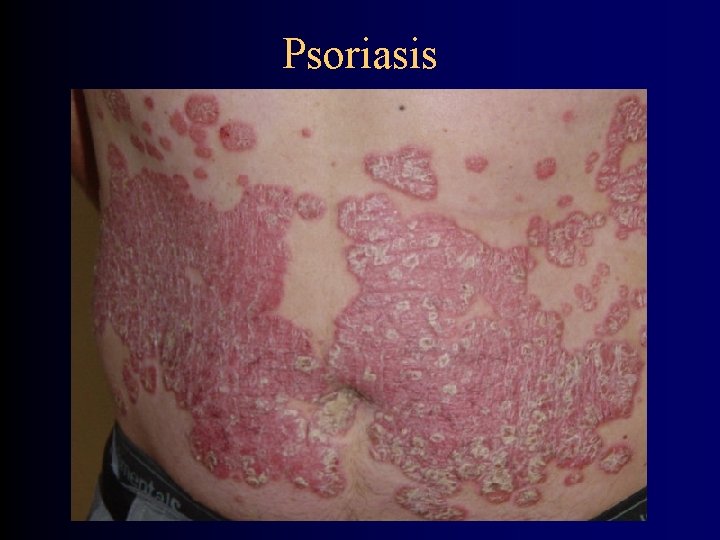
Epidermis - Stratum basale • • 1 layer of cylindrical / cuboid elements bazophilic Desmozomes, hemidesmosomes mitotic activity – Whole epidermis recreates within 15 -30 days – psoriasis – fastened to 7 days • 10 nm intermediary filaments (cytokeratins) – Towards surface more numerous • In thick type of skin are Merkel cells
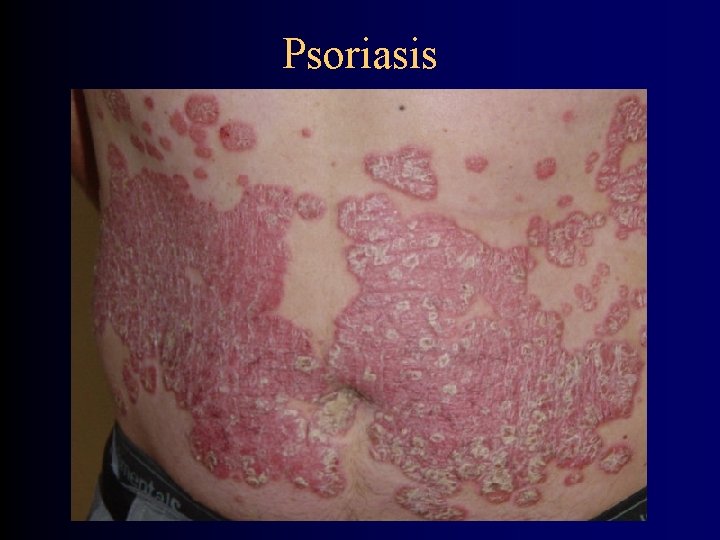
Psoriasis
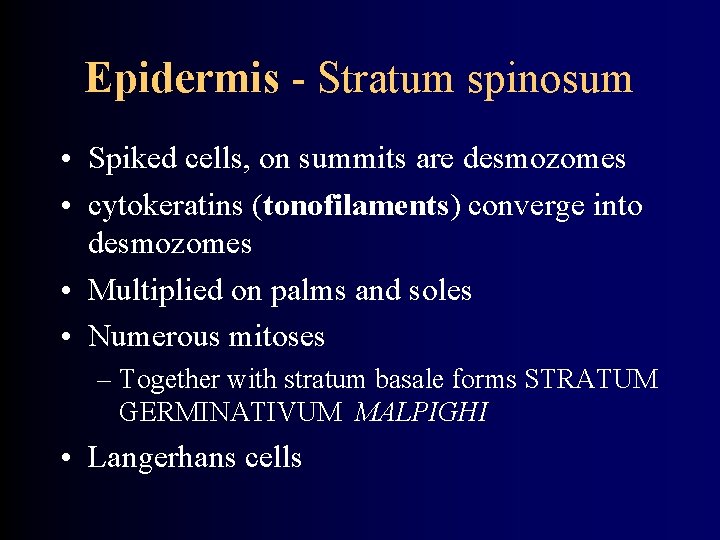
Epidermis - Stratum spinosum • Spiked cells, on summits are desmozomes • cytokeratins (tonofilaments) converge into desmozomes • Multiplied on palms and soles • Numerous mitoses – Together with stratum basale forms STRATUM GERMINATIVUM MALPIGHI • Langerhans cells
Epidermis - Stratum granulosum • 3 -5 layers of cells • Polygonal with centrally located nucleus • 2 types of granules: – BAZOFILIC granules = keratohyalin – LAMELAR granules = Odland corpuscles (content excreted into intercellular space serves as cement against pass of foreign bodies)
Epidermis - Stratum lucidum • • • thin Flat eosinophilic cells Nucleus and organels not well visible Mostly filaments in electrondense matrix Visible desmozomes ELEIDIN (very structurated)
Epidermis - Stratum corneum • 15 -20 layers of flat cells = cells of the corneal layer • Nuclei and organels not present – Effect of lyzosomal enzymes • cytoplazm filled by KERATIN – Composed scleroprotein cemented by basic substance from keratohyalin granules • stratum disjunctum – releasing cells
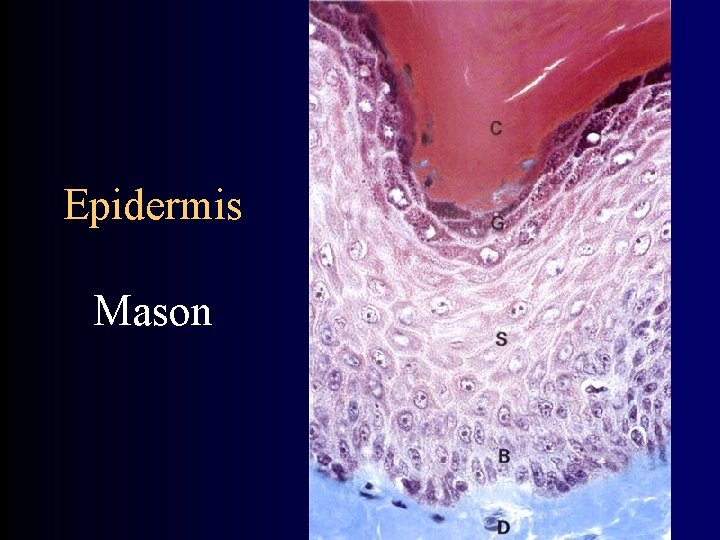
Epidermis Mason

Epidermis - HE 1000 x
Coloring of skin • • melanin (melanocytes) karoten Number of vessels in dermis Color of blood in vessels of dermis
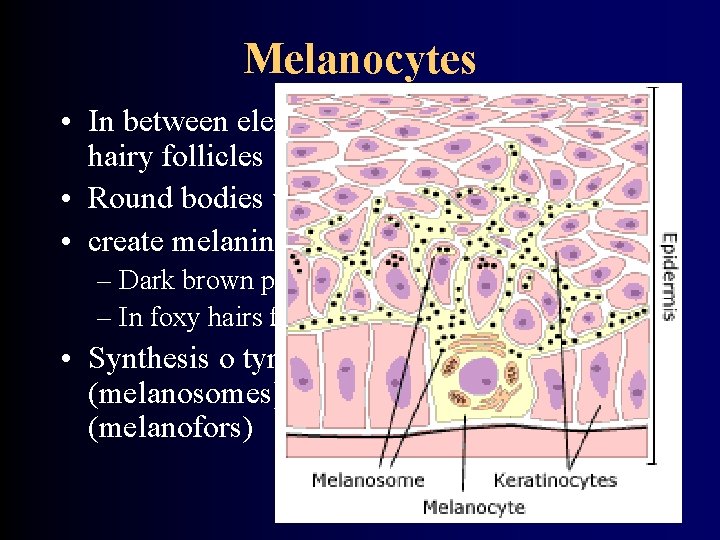
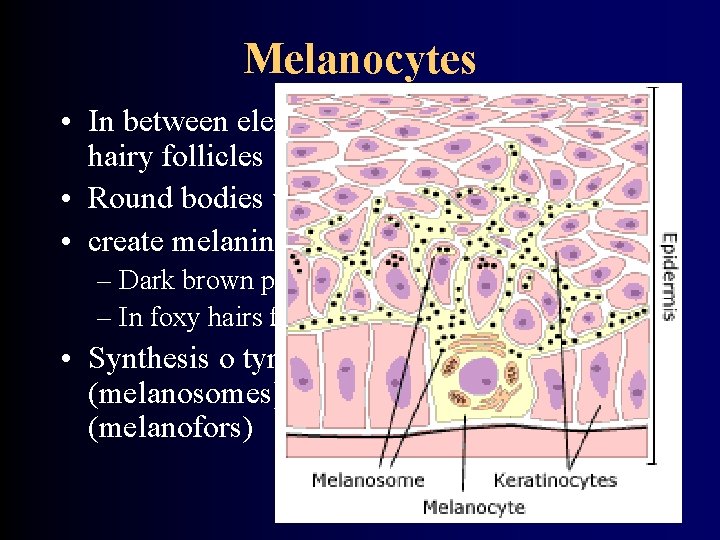
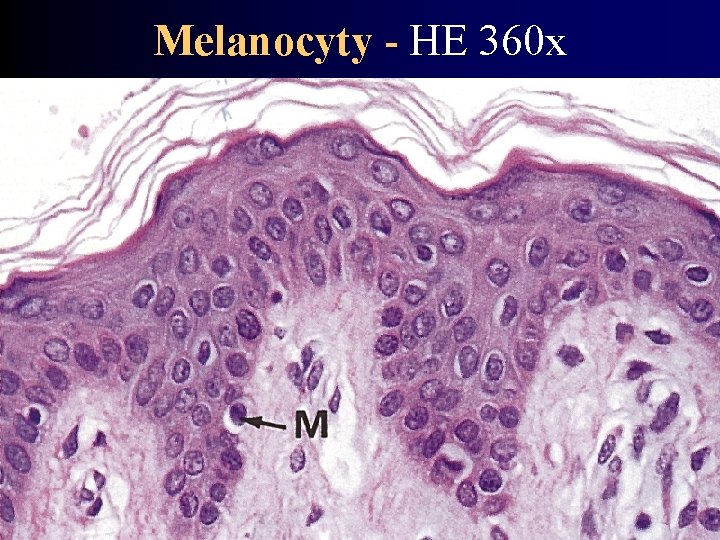
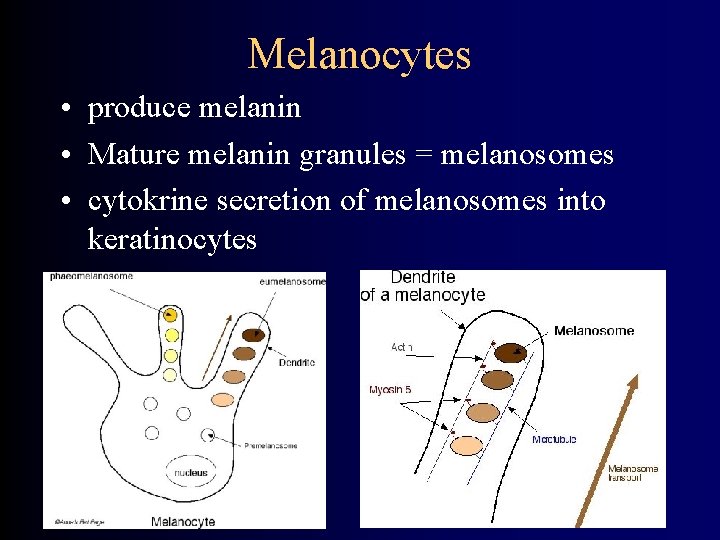
Melanocytes • In between elements of stratum basale, in hairy follicles • Round bodies with extensions into epidermis • create melanin (eumelanin) – Dark brown pigment – In foxy hairs feomelanin • Synthesis o tyrosinase and deposition in sacs (melanosomes) injected into keratinocytes (melanofors)
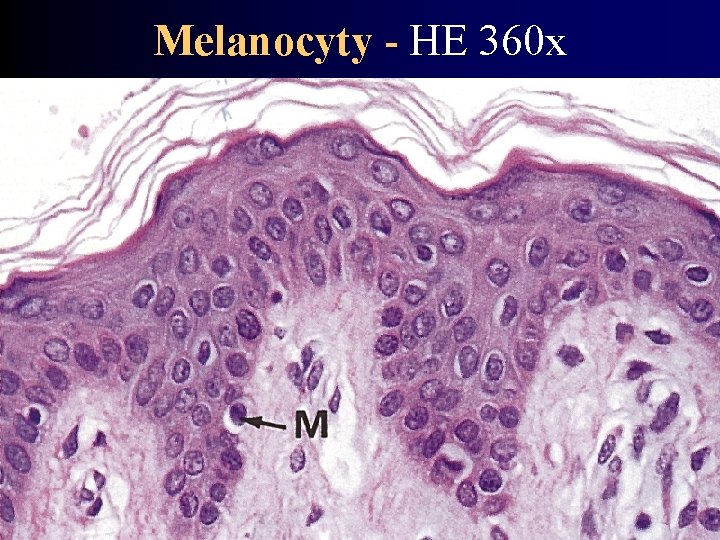
Melanocyty - HE 360 x
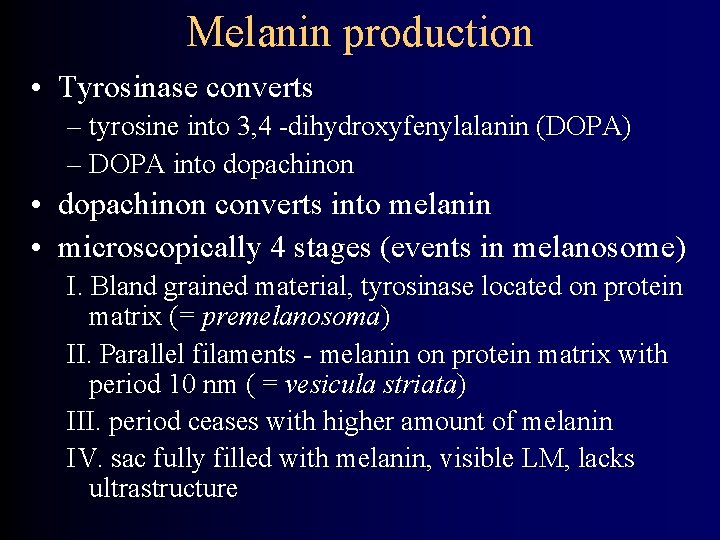
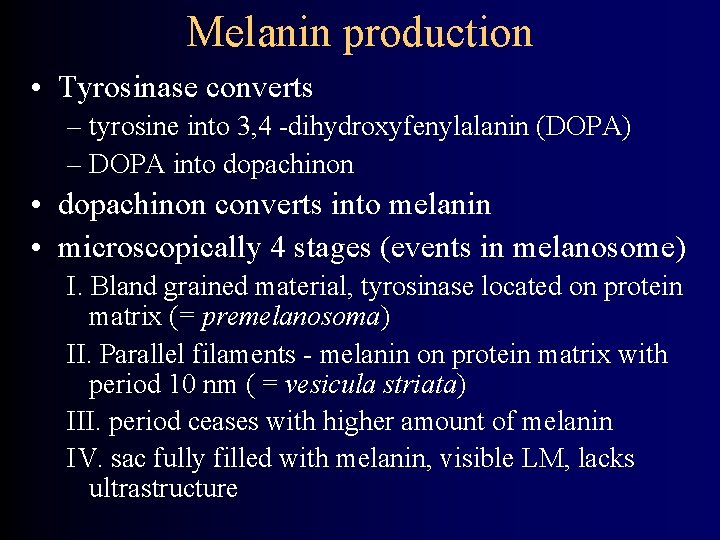
Melanin production • Tyrosinase converts – tyrosine into 3, 4 -dihydroxyfenylalanin (DOPA) – DOPA into dopachinon • dopachinon converts into melanin • microscopically 4 stages (events in melanosome) I. Bland grained material, tyrosinase located on protein matrix (= premelanosoma) II. Parallel filaments - melanin on protein matrix with period 10 nm ( = vesicula striata) III. period ceases with higher amount of melanin IV. sac fully filled with melanin, visible LM, lacks ultrastructure
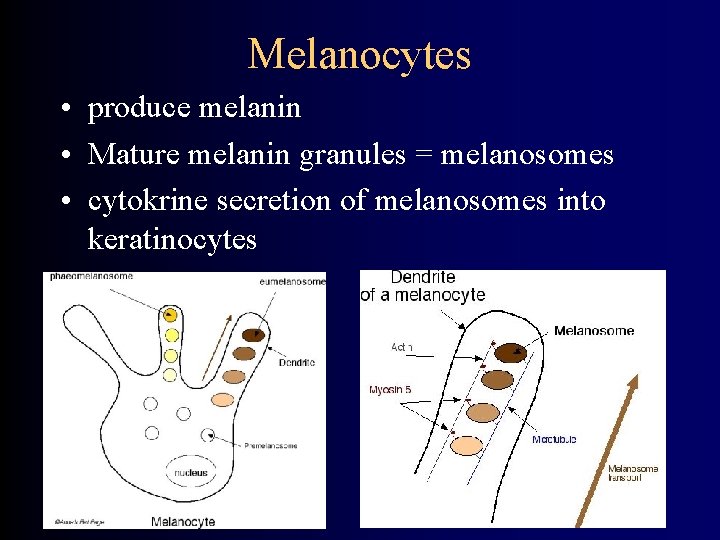
Melanocytes • produce melanin • Mature melanin granules = melanosomes • cytokrine secretion of melanosomes into keratinocytes
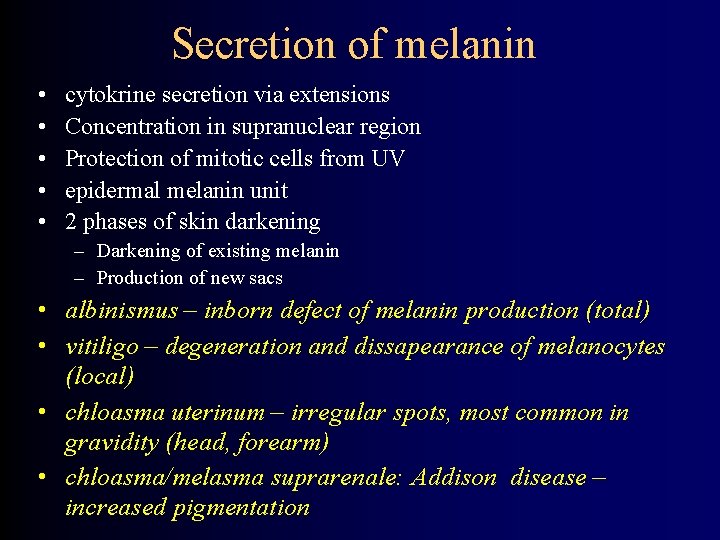
Secretion of melanin • • • cytokrine secretion via extensions Concentration in supranuclear region Protection of mitotic cells from UV epidermal melanin unit 2 phases of skin darkening – Darkening of existing melanin – Production of new sacs • albinismus – inborn defect of melanin production (total) • vitiligo – degeneration and dissapearance of melanocytes (local) • chloasma uterinum – irregular spots, most common in gravidity (head, forearm) • chloasma/melasma suprarenale: Addison disease – increased pigmentation

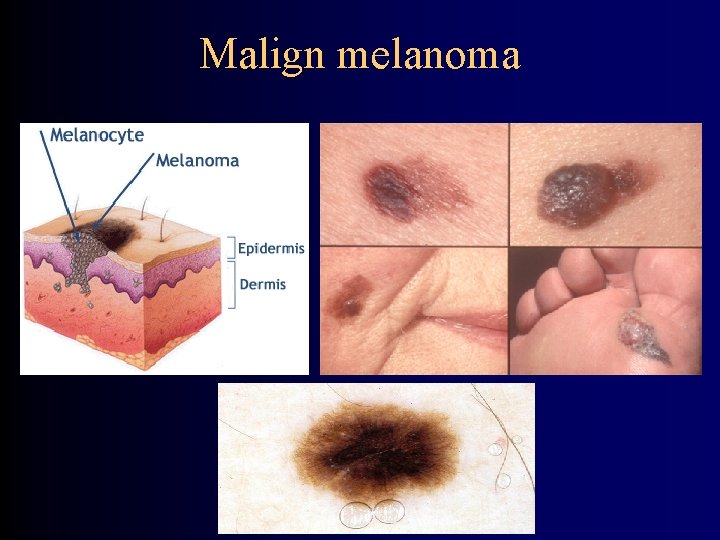
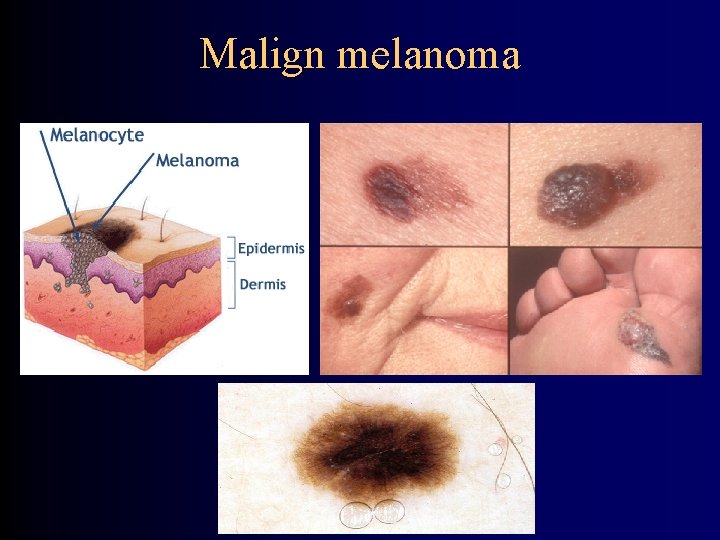
Malign melanoma
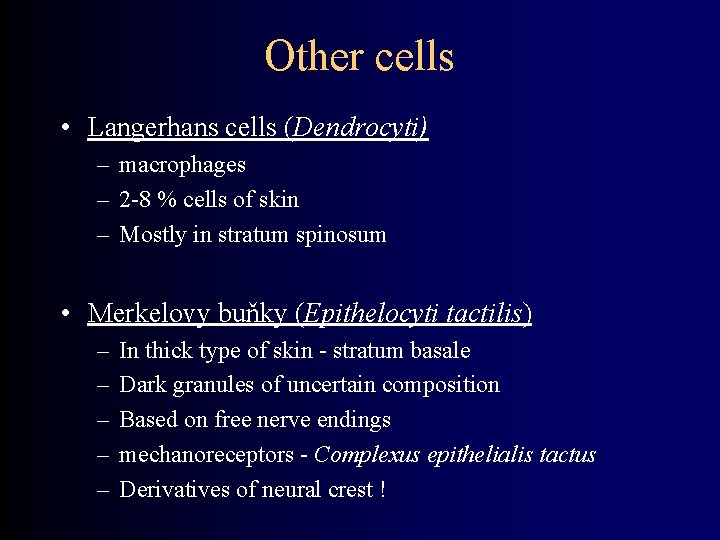
Other cells • Langerhans cells (Dendrocyti) – macrophages – 2 -8 % cells of skin – Mostly in stratum spinosum • Merkelovy buňky (Epithelocyti tactilis) – – – In thick type of skin - stratum basale Dark granules of uncertain composition Based on free nerve endings mechanoreceptors - Complexus epithelialis tactus Derivatives of neural crest !

Langerhansovy buňky - HE 700 x
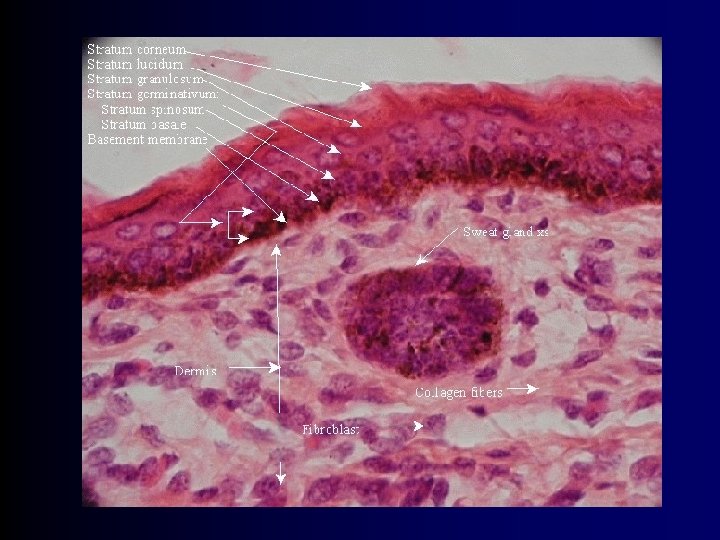

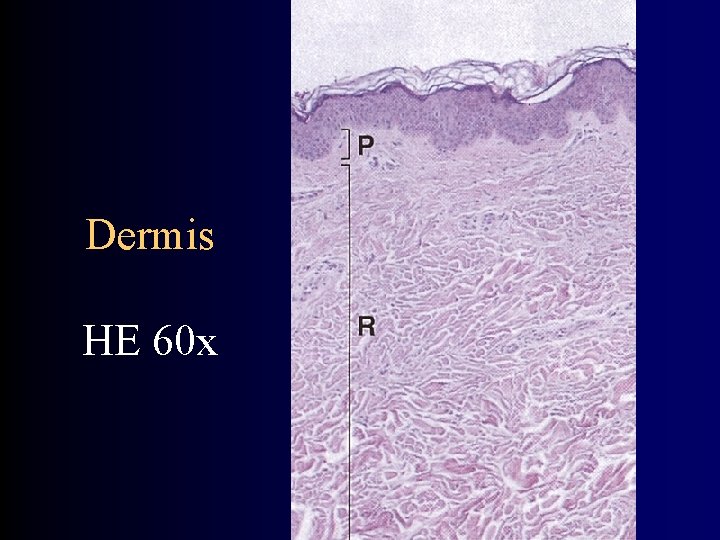
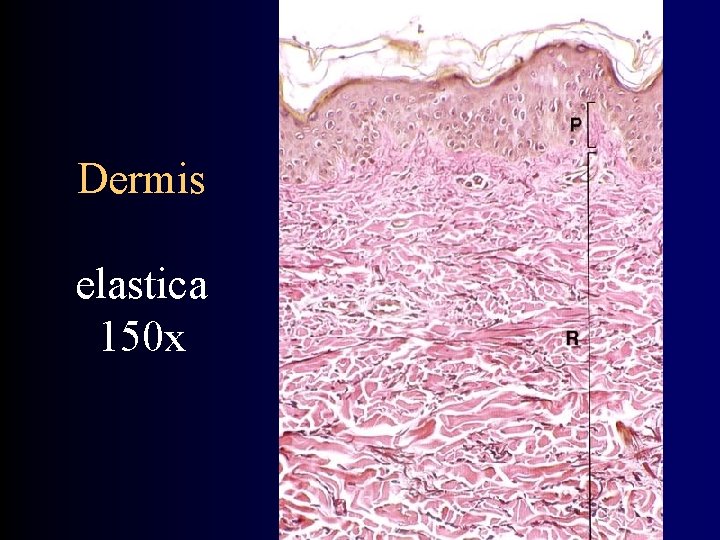
Dermis - composition • Fibrous layer under basal membrane of epidermis • thickness up to 4 mm (back) • extensions - dermal papillas – Correlates with epidermal pegs • 2 slurry bordered layers – stratum papillare and reticulare • Rich capillary bedstream • Presence of skin derivatives

Dermis - Stratum papillare • • Forms great part of papills Thin tissue Common fibrous components ANCHORING FIBERS inserting into basal membrane
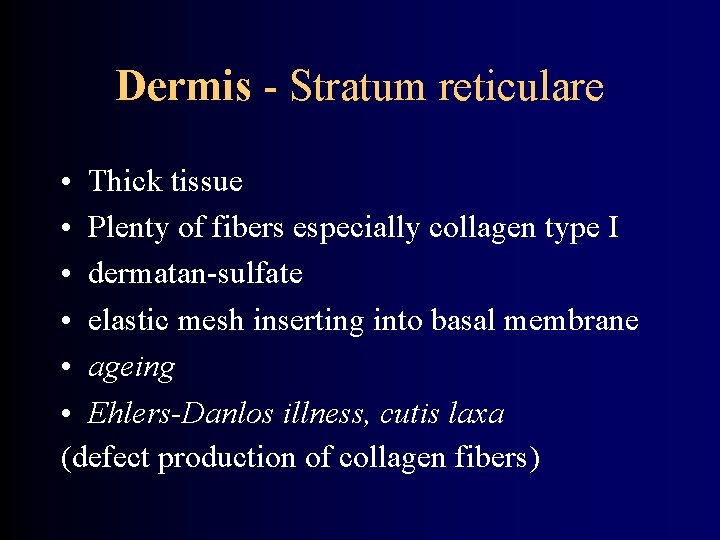
Dermis - Stratum reticulare • Thick tissue • Plenty of fibers especially collagen type I • dermatan-sulfate • elastic mesh inserting into basal membrane • ageing • Ehlers-Danlos illness, cutis laxa (defect production of collagen fibers)
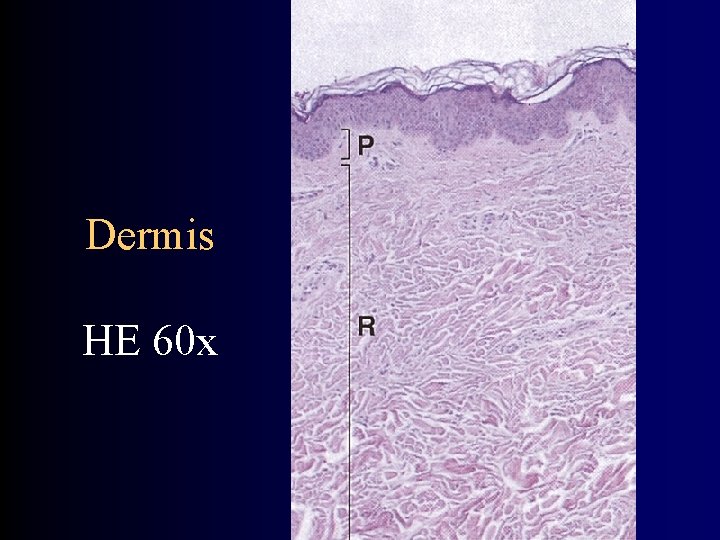
Dermis HE 60 x

Dermis HE 20 x
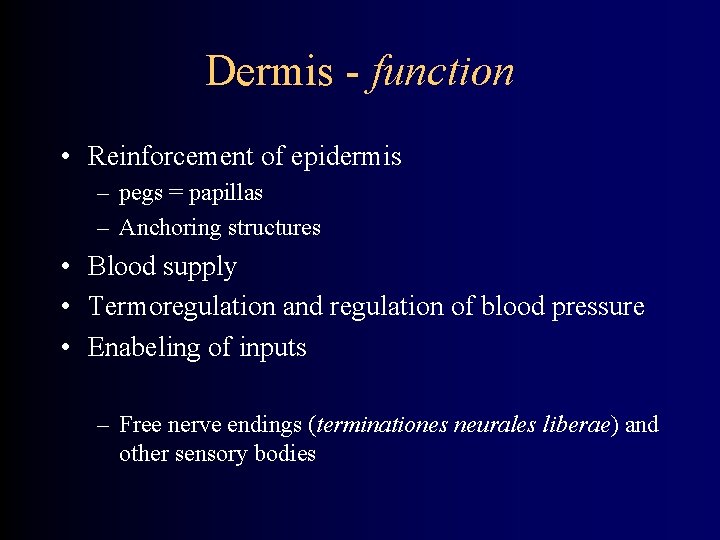
Dermis - function • Reinforcement of epidermis – pegs = papillas – Anchoring structures • Blood supply • Termoregulation and regulation of blood pressure • Enabeling of inputs – Free nerve endings (terminationes neurales liberae) and other sensory bodies
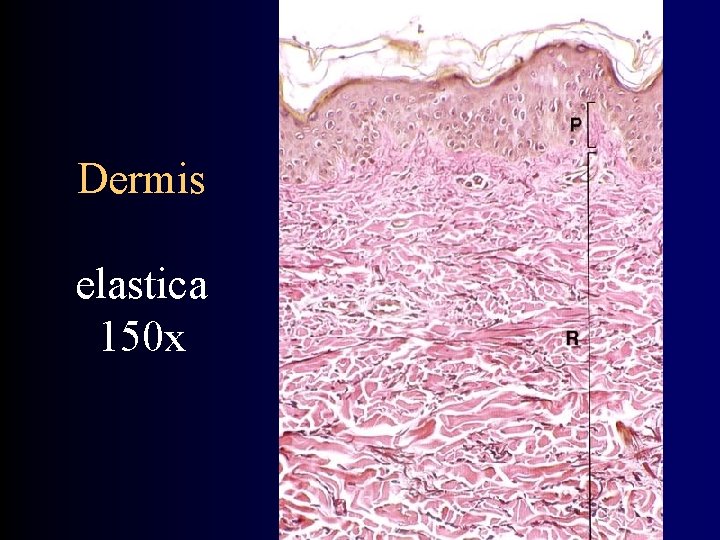
Dermis elastica 150 x

Abdominal skin - Mason 12 x

Skin - supply • arteries – deep and superficial net – Always constant stalk for particular area skin folds for replantations – capillaries - a-v anastomoses • veins – the same • lymph – capillaries subcapillary mesh collectors • nerves – missing parasympaticus ! – Nerve endings (free x corpuscles) – 5 th sense = touch – somatosensory fibers – sympatic postganglionic vasomotoric fibers – adrenergic – visceromotor fibers – sympatic fibers for sudoriferous glands – cholinergic !
Skin diseases I. Pemphigus vulgaris • Autoimmune illness • Circulating Ig. G anti bodies against surface antigens of cuboid epithelium associated with desmozomes • Binding of antibody causes activation of proteases, breakdown of epidermis and formation of blisters • Intraepidermal blisters – Located suprabazally
Skin diseases II. Bulous pemfigoid • autoimmune illness: circulating Ig. G anti bodies binding to antigens BP 1 and BP 2 in basal membrane area • Binding of anti bodies leads to complement activation, defect of tissue and blisters • Subepidermal blisters with cover formed by relatively normal epidermis
Skin diseases II. Skin tumors • 1/3 of all tumors • Originate from keratinocytes of stratum germinativum • bazalioma • spinocellular carcinoma • - are recognized early • Originate from melanocytes – melanoma • growth through BL, penetrates into vessels, metastasing
Skin derivatives • hairs (pili) – lanugo /flumina, vortices/ – hairs (capilli), eyebrow (supercilia), eyelashes (cilia), beard (barba), tragi (external auditory canal), vibrissae (nose), hirci (armpit), pubes, tactile (sinusoids) • nails (ungues) • Skin glands (glandulae cutis) – Are derivatives of epidermis
Hairs (pili) • Everywhere except for palms, soles, lips, glans penis and labia minora • Allocation, density and color depends on: – Sex, age, race and body area – Effect of hormones (androgens, T 3, T 4, corticoids) • Growth periods (anagen) • Quiescent periods (katagen, telogen)

Hair growth • anagen - 3 years/ 1000 days • katagen - 3 weeks/ 10 days • telogen - 3 month/ 100 days Perish of bulb and its renewal 0, 4 mm/day Falling out – up to 100 hairs per day – if more effluvium areas w/o hairs - alopecia Influence of: hormones, nutrition, toxic (infections,
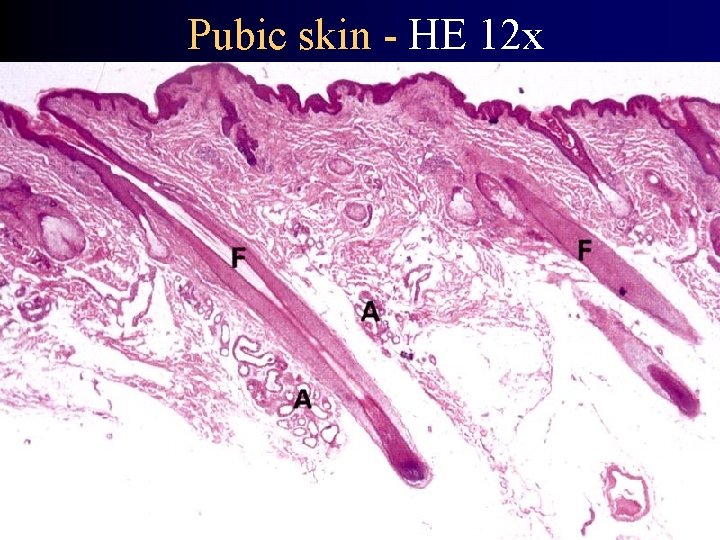
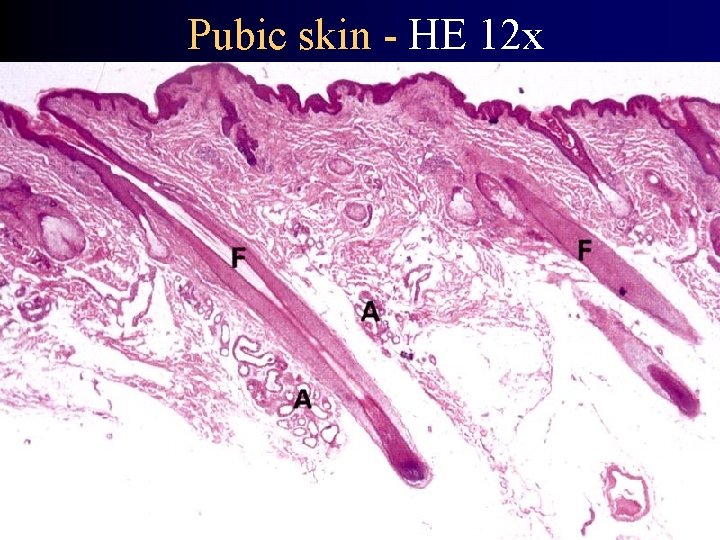
Pubic skin - HE 12 x

Hairs (Pili) – structure I. • Hairy sheath (folliculus pili) - invaginated epidermis • Hairy bulb (bulbus pili) – equivalent to stratum germinativum • Dermal papilla (based on bulb, capillary mesh) • Cells around papilla → root of hair – medulla – from central cells above papilla • Big, vacuolised elements – Cortex – from central cells around papilla • keratinized, spindle elements – From other cellular layer originate cuticula
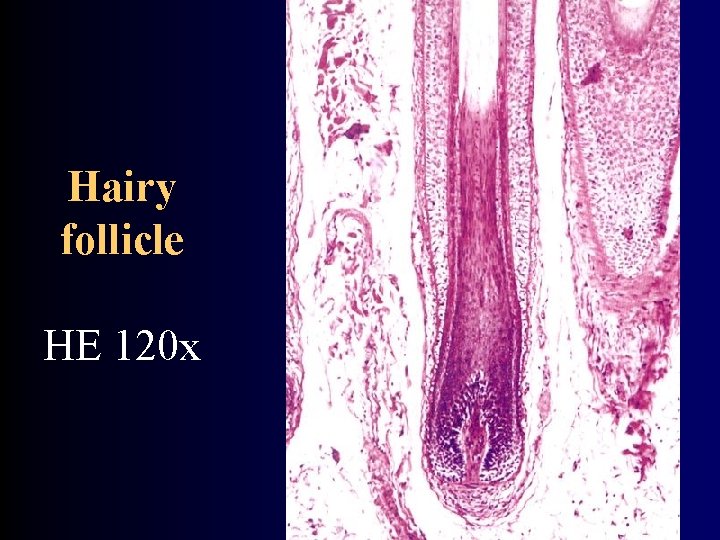
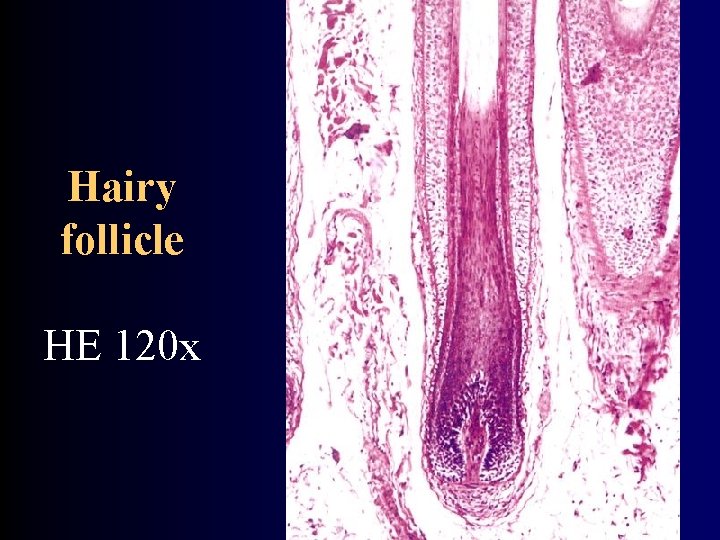
Hairy follicle HE 120 x
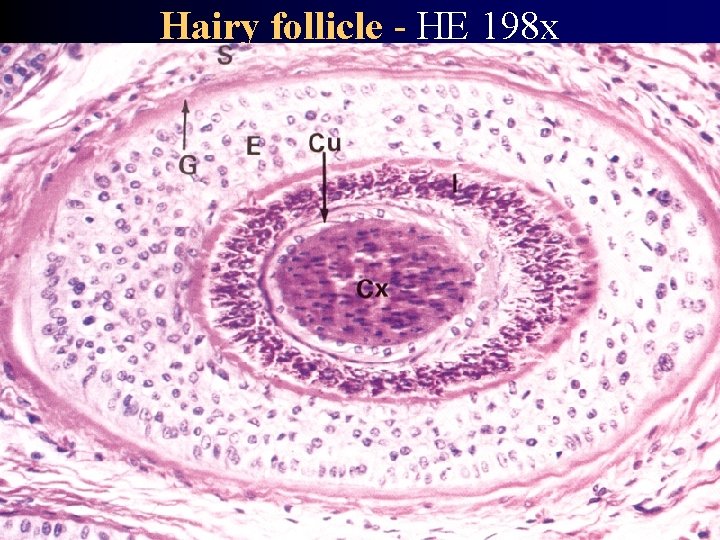
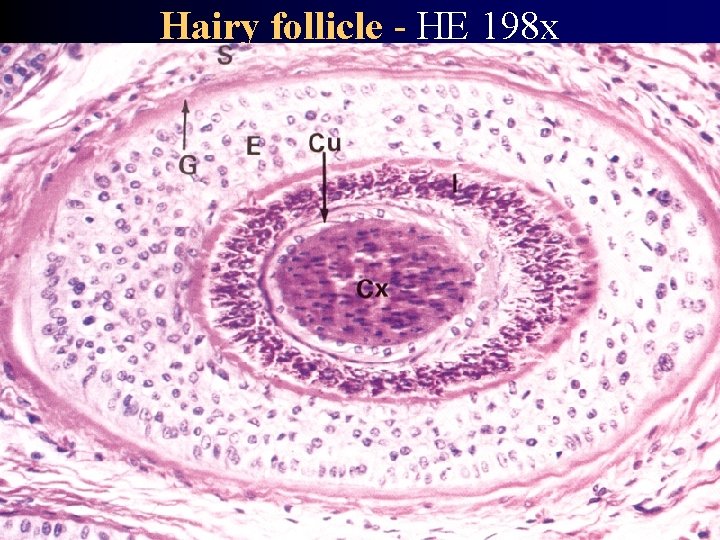
Hairy follicle - HE 198 x • medulla • cortex • cuticula • inner and outer bulbar sheath (vagina radicularis epithelialis int. +ext. ) • glassy membrane (membrana vitrea) • fibrous sheath (vagina radicularis dermalis)
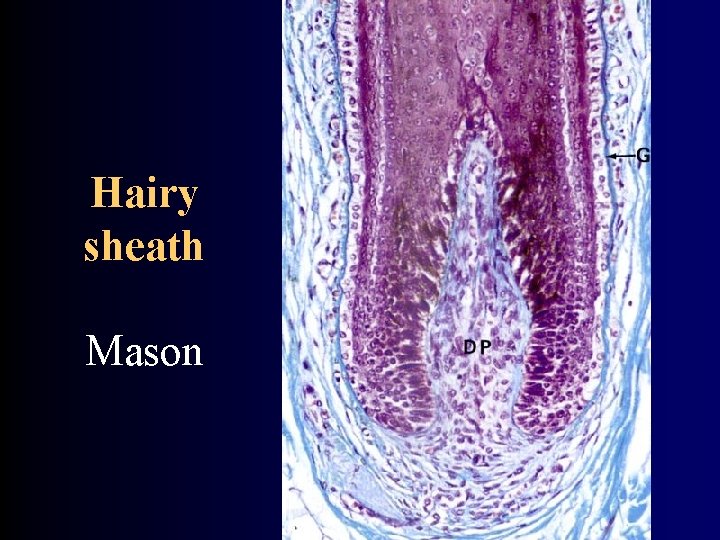
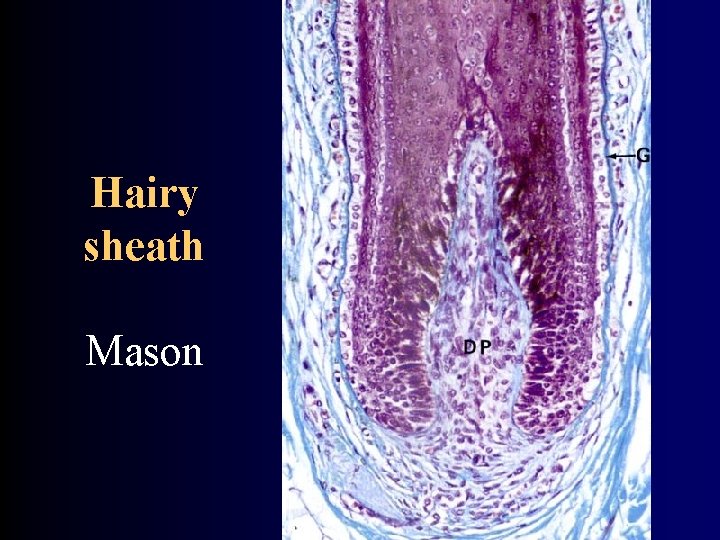
Hairy sheath Mason
Hairs (Pili) - structure II. • From peripheral cells originate – Inner bulb pouch – Outer bulb pouch (→ continues into epithelium) • Glassy membrane separates pouch from dermis • dermis around pouch is dense → fibrous pouch • Erector of pilli (musculus arrector pili) – Inserts into fibrous pouch – Originate in papillary layer of dermis – Erects pillus → anserina cutis

Unguis Pictures – 1. LF UK
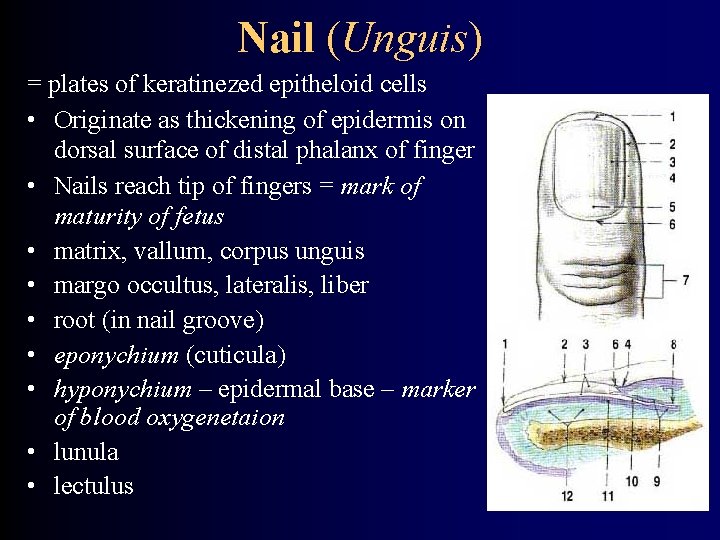
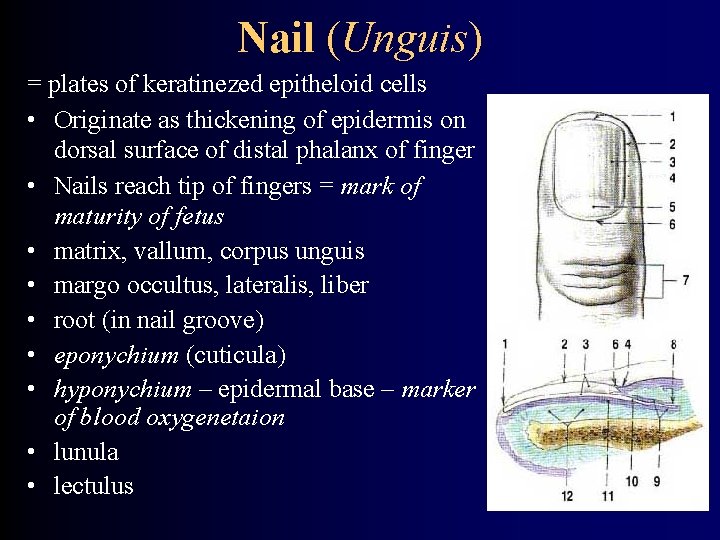
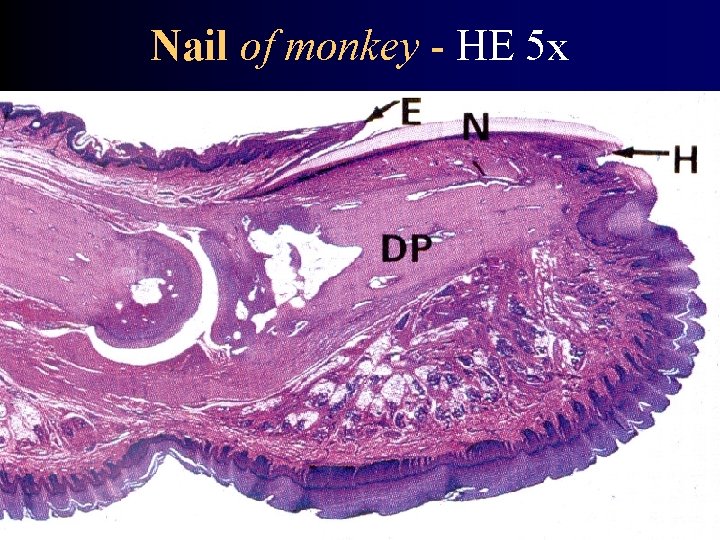
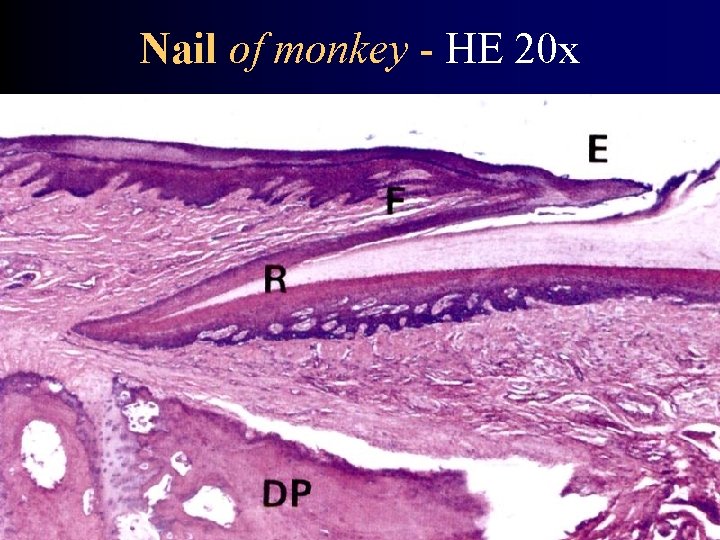
Nail (Unguis) = plates of keratinezed epitheloid cells • Originate as thickening of epidermis on dorsal surface of distal phalanx of finger • Nails reach tip of fingers = mark of maturity of fetus • matrix, vallum, corpus unguis • margo occultus, lateralis, liber • root (in nail groove) • eponychium (cuticula) • hyponychium – epidermal base – marker of blood oxygenetaion • lunula • lectulus
Nails - development • Nails originate as thickening of epidermis on tips of fingers – Nails overhanging tips of fingers are one mark of fetal maturity
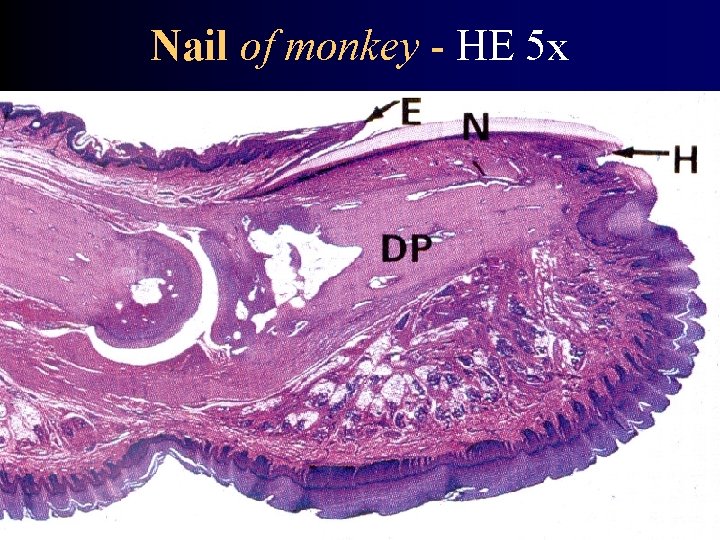
Nail of monkey - HE 5 x
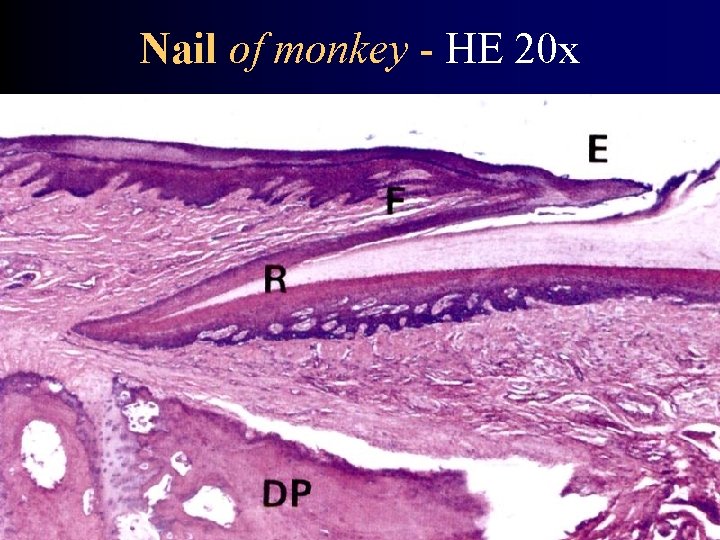
Nail of monkey - HE 20 x
Skin glands • sebaceous • sudorific • effluvial
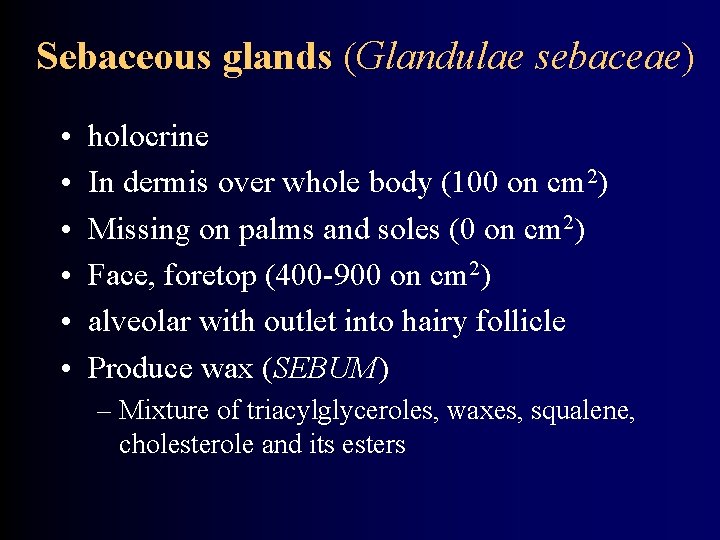
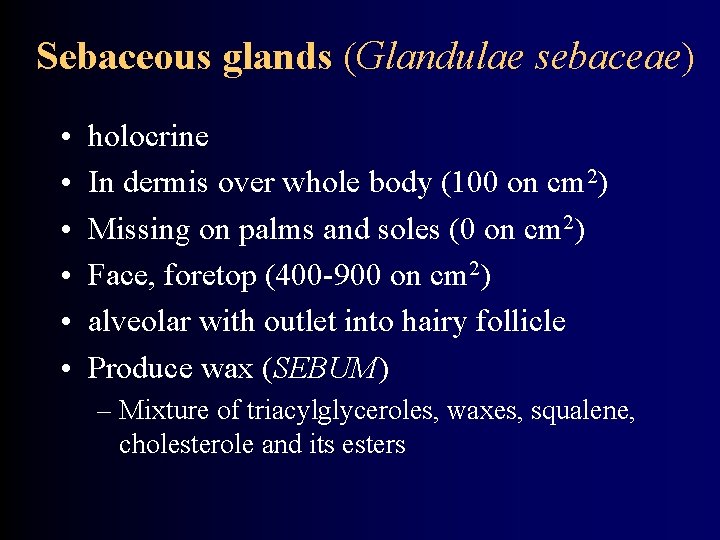
Sebaceous glands (Glandulae sebaceae) • • • holocrine In dermis over whole body (100 on cm 2) Missing on palms and soles (0 on cm 2) Face, foretop (400 -900 on cm 2) alveolar with outlet into hairy follicle Produce wax (SEBUM) – Mixture of triacylglyceroles, waxes, squalene, cholesterole and its esters

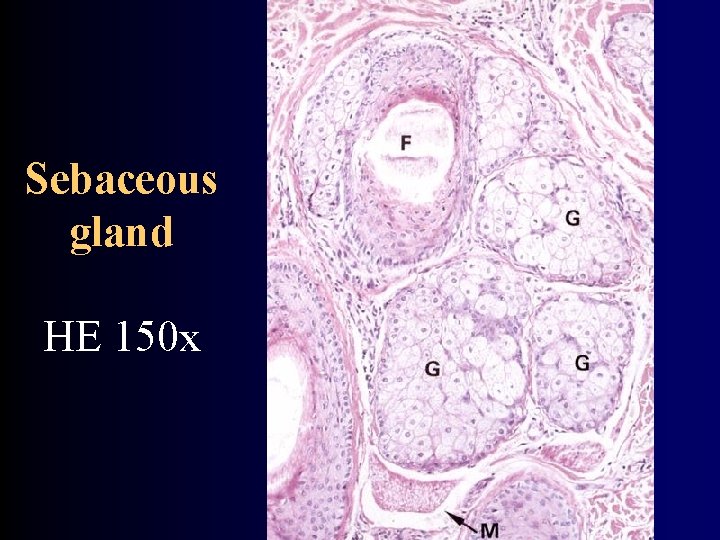
Sebaceous gland HE 33 x
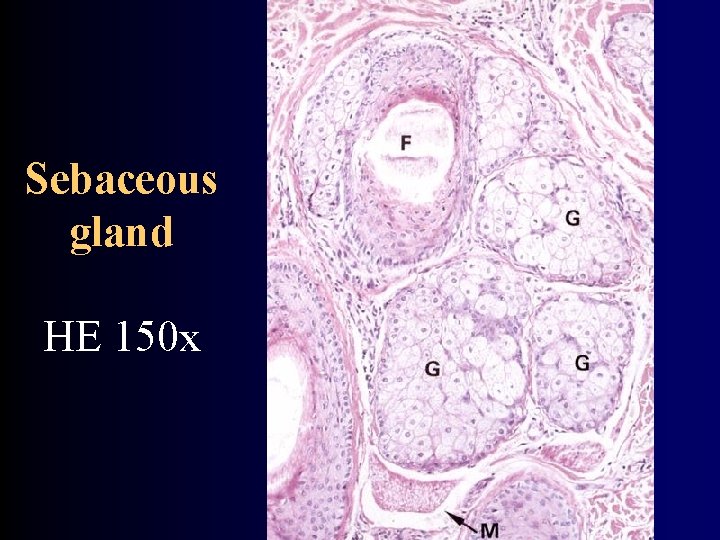
Sebaceous gland HE 150 x
Sudoriferic glands (Glandulae sudorifereae) Merocrine secretion • eccrine (glandula sudorifera merocrina / eccrina) • apocrine (glandula sudorifera apocrinna) – axilla, pubic area, labia minora – gll. mammariae, gll. areolares Montgomeryi – gll. ciliares Molli - eyelid – gll. ceruminosae – external auditory tube → EAR WAX (CERUMEN) – gll. sudoriferae nasales – gll. circumanales
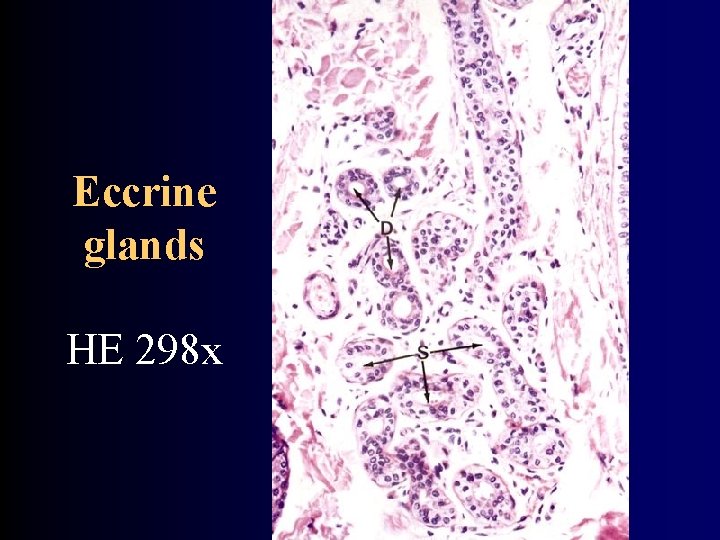
Eccrine glands = sudoriferous • Simple, convoluted, tubulous • Opening aside of pilli pouch • Everywhere, thickest on palm, sole and forehead • Missing on glans penis and inner side of preputium – Dark cells (mucoid) – Light cells (transport of ions) • Produce non tenacious fluid – water, Na. Cl, urea, amoniac, uric acid – Ultrafiltrate of blood plasma
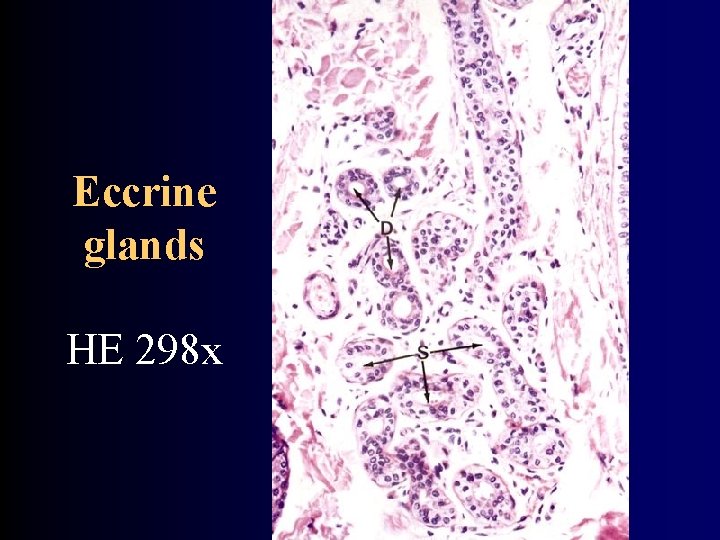
Eccrine glands HE 298 x

Apocrine glands = effluvial • • • 3 -5 mm in diameter In subcutaneous fat Open into pouches of hairy follicles Viscous secret w/o smell aromatic stink – infulence of bacteria Adrenergic innervation

Apocrine glands HE 128 x
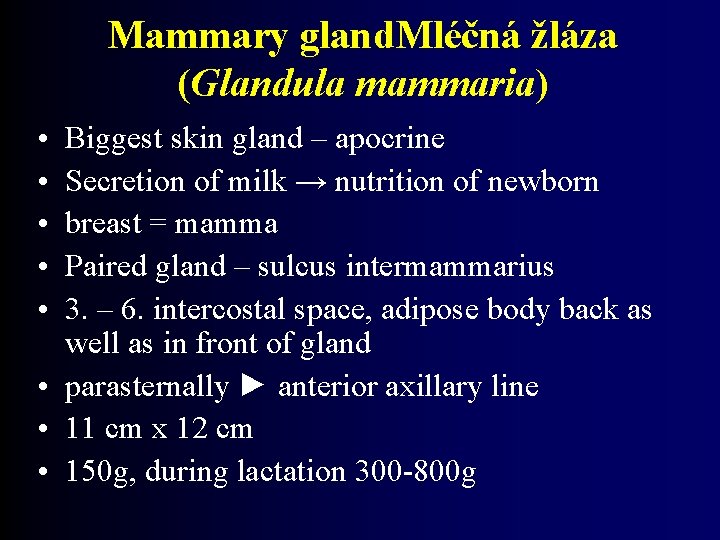
Mammary gland. Mléčná žláza (Glandula mammaria) • • • Biggest skin gland – apocrine Secretion of milk → nutrition of newborn breast = mamma Paired gland – sulcus intermammarius 3. – 6. intercostal space, adipose body back as well as in front of gland • parasternally ► anterior axillary line • 11 cm x 12 cm • 150 g, during lactation 300 -800 g

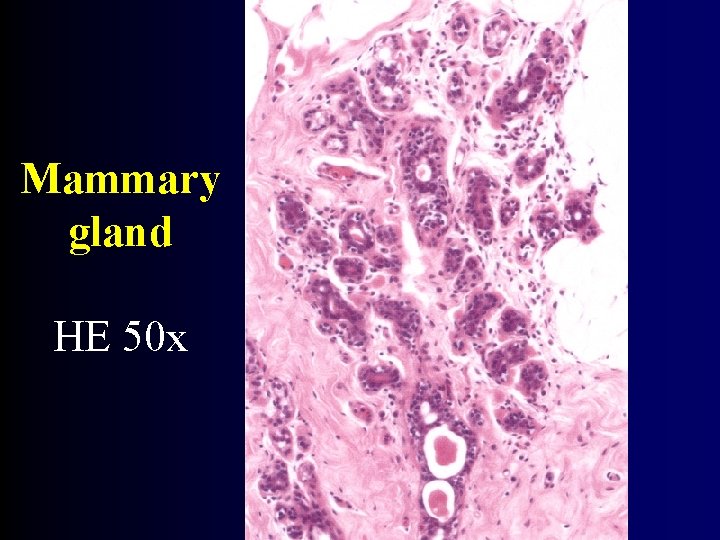
Mammary gland (Glandula mammaria) • Body of gland (corpus mammae) – processus axillaris • lobes → lobuli → glandular alveoles (glandular epithelium, myoepithelial cells) • 15 -20 complex tuboalveolar glands • Each having own excretory duct = lactiferous duct (ductus lactifer) → sinus lactiferi /only during lactation/ → papilla (papillae mammae) • Separated by thick tissue and adipose tissue • retinaculum cutis mammae = ligg. suspensoria mammaria Cooperi
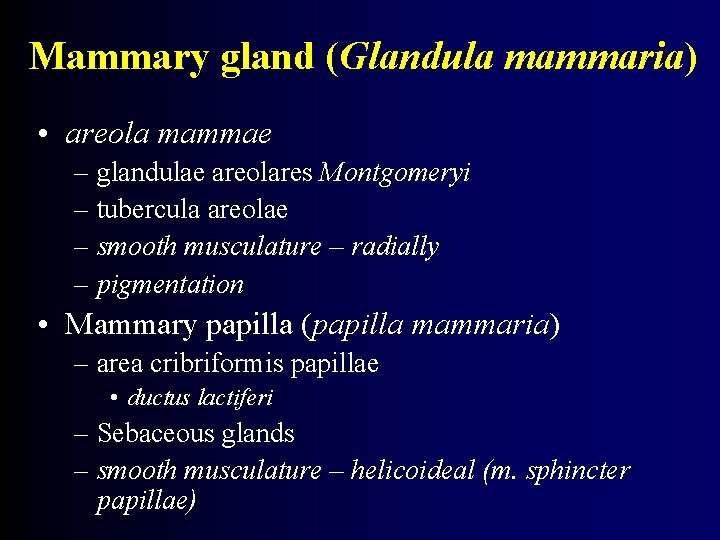
Mammary gland (Glandula mammaria) • areola mammae – glandulae areolares Montgomeryi – tubercula areolae – smooth musculature – radially – pigmentation • Mammary papilla (papilla mammaria) – area cribriformis papillae • ductus lactiferi – Sebaceous glands – smooth musculature – helicoideal (m. sphincter papillae)


Mammary gland - development • 6. week: MILKY CRESTS (= thickening of epidermis) from axilla to umbilicus • 2. trimester: 15 -20 epitelial pegs – foundation of lactiferous ducts • Newborns of both sexes – diameter: 3, 5 - 9 – Outlets bulged by accumulated secret – Excretion of secret (influence of maternal hormones = „Hexenmilch“)

Mammary gland - pubertas • In girls enlargement due to – Accumulation of adipose and fibrous tissue – Proliferation and branching of ductus lactiferi – Both under influence of ovarial estrogens • In males breasts remaining flat
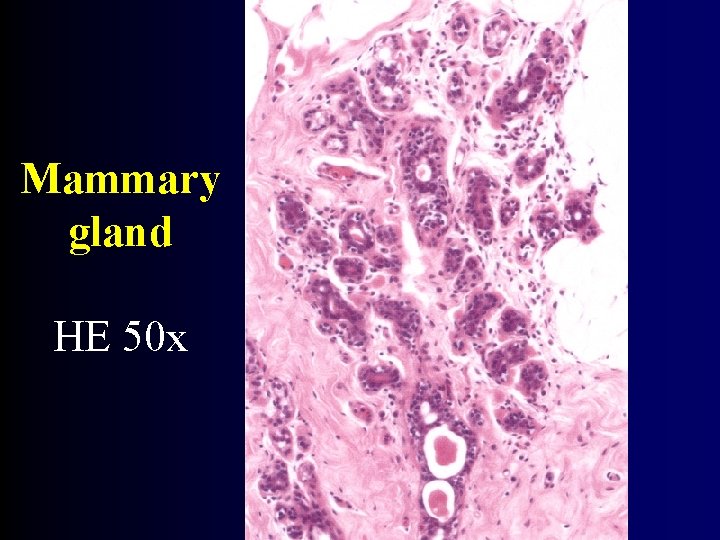
Mammary gland HE 50 x
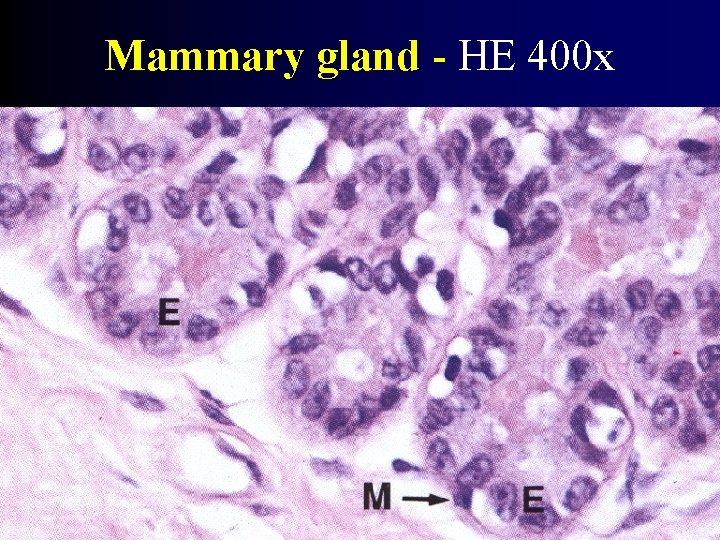
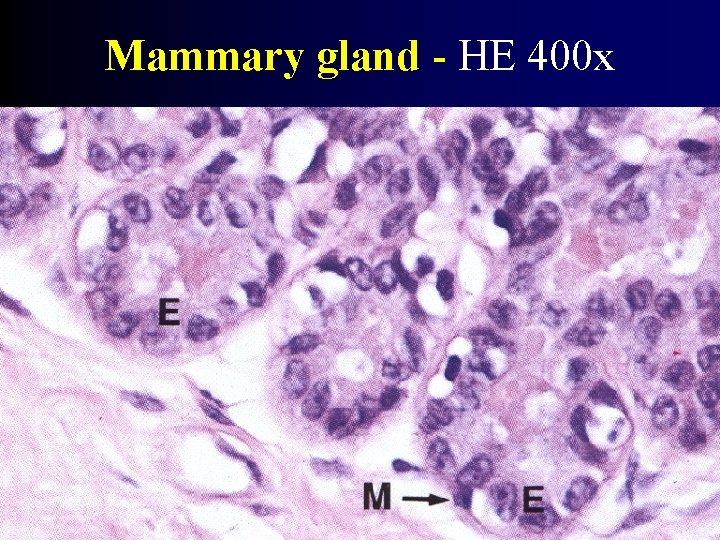
Mammary gland - HE 400 x
Mammary gland – gravidity and lactation • Proliferation of alveoles in lobules • Cells with excretory vacuols and adipose globules • 4 -6 myoepitelial cells around alveoles • synergic influence of hormones → growth of secretory part • Secretion into lumen of alveoles • water, lipids, proteins (caseins), lactose, Ig A • foremilk (colostrum), suckling, oxytocin
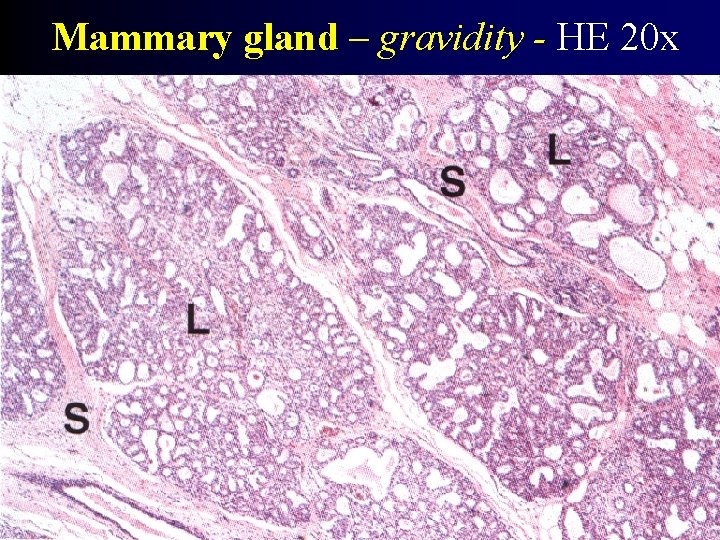
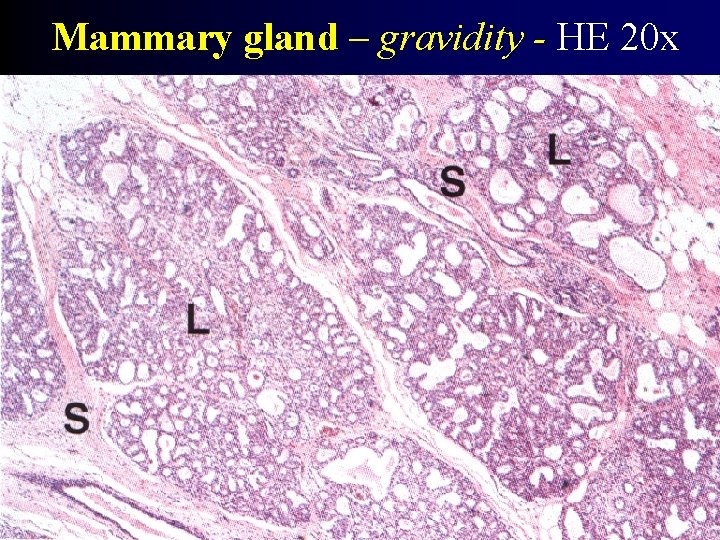
Mammary gland – gravidity - HE 20 x
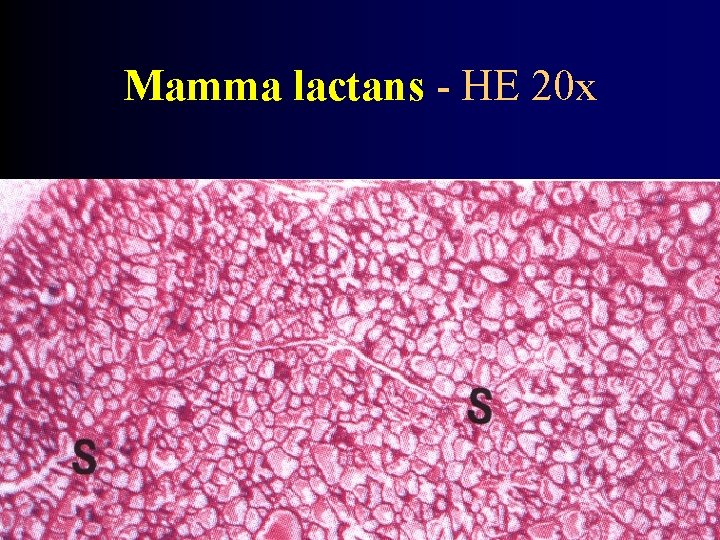
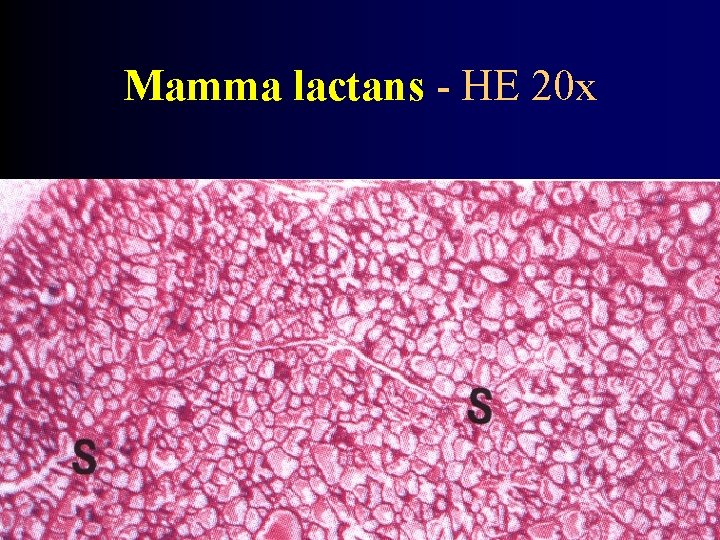
Mamma lactans - HE 20 x
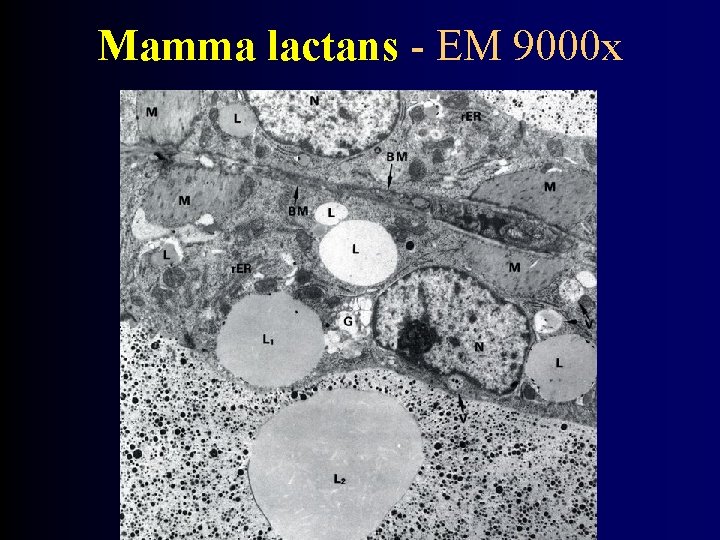
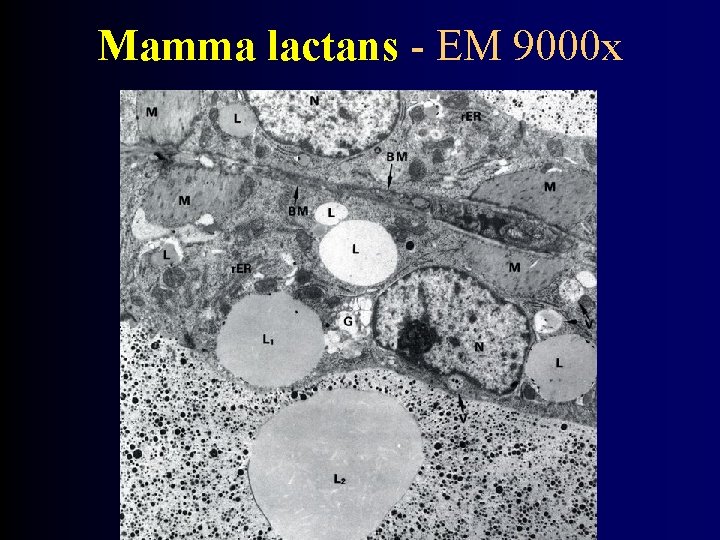
Mamma lactans - EM 9000 x
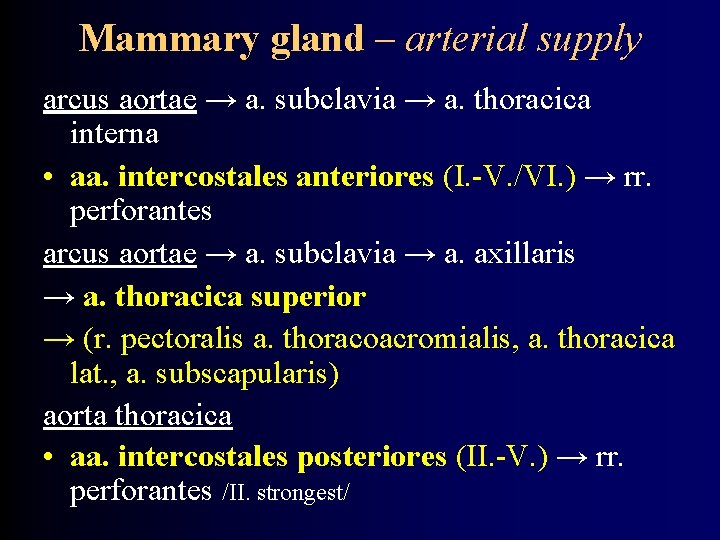
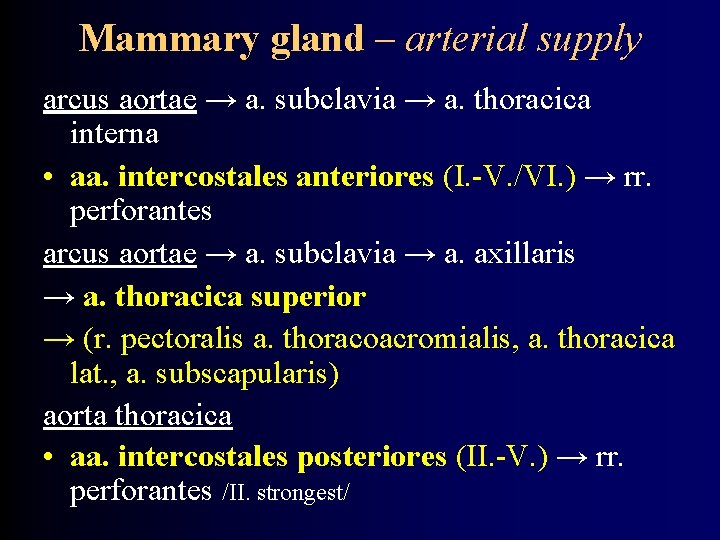
Mammary gland – arterial supply arcus aortae → a. subclavia → a. thoracica interna • aa. intercostales anteriores (I. -V. /VI. ) → rr. perforantes arcus aortae → a. subclavia → a. axillaris → a. thoracica superior → (r. pectoralis a. thoracoacromialis, a. thoracica lat. , a. subscapularis) aorta thoracica • aa. intercostales posteriores (II. -V. ) → rr. perforantes /II. strongest/
Mammary gland – venous drainage • plexus venosus Halleri – under areola mammae v. axillaris v. thoracica interna vv. intercostales posteriores
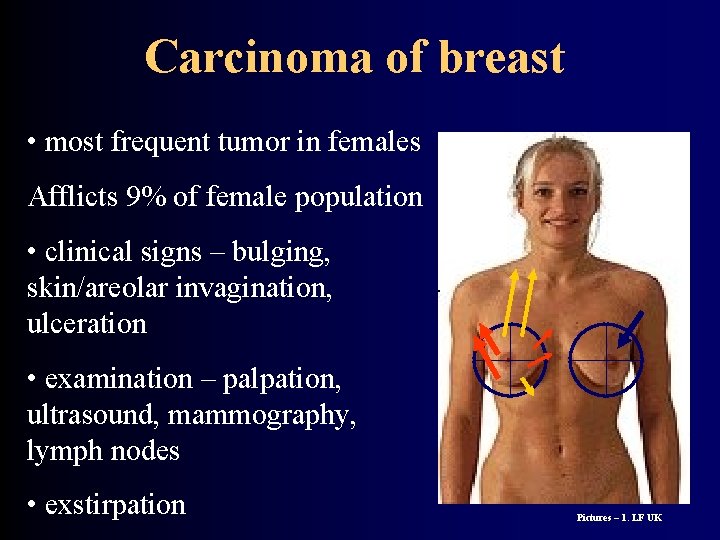
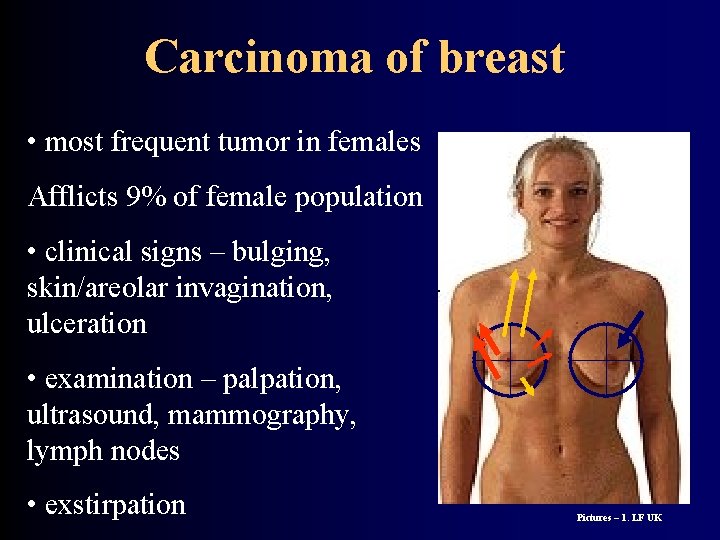
Carcinoma of breast • most frequent tumor in females Afflicts 9% of female population • clinical signs – bulging, skin/areolar invagination, ulceration • examination – palpation, ultrasound, mammography, lymph nodes • exstirpation Pictures – 1. LF UK
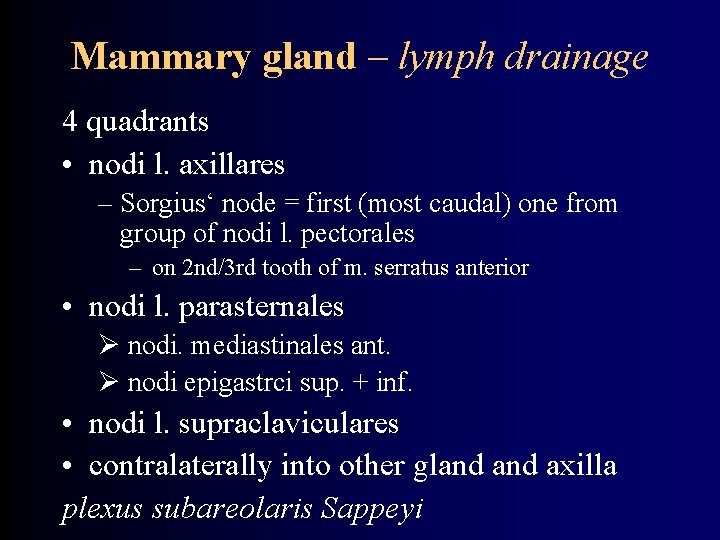
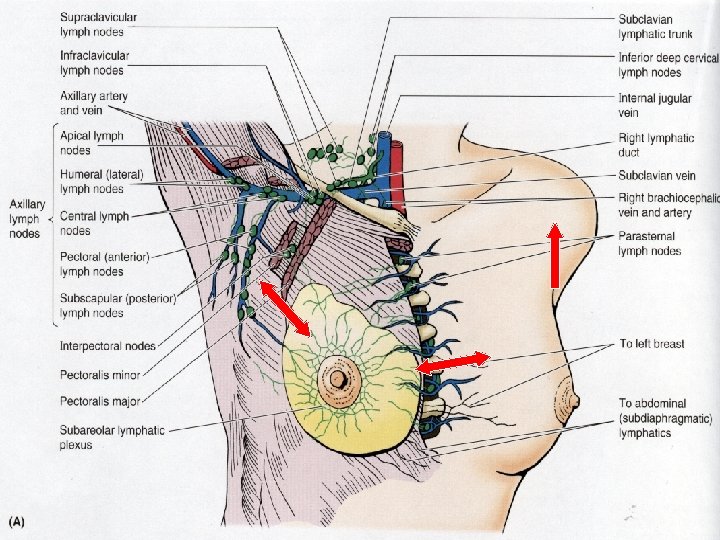
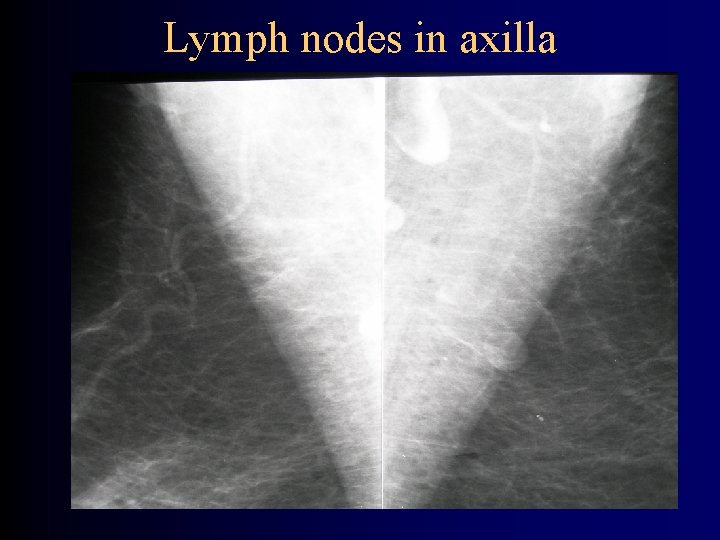
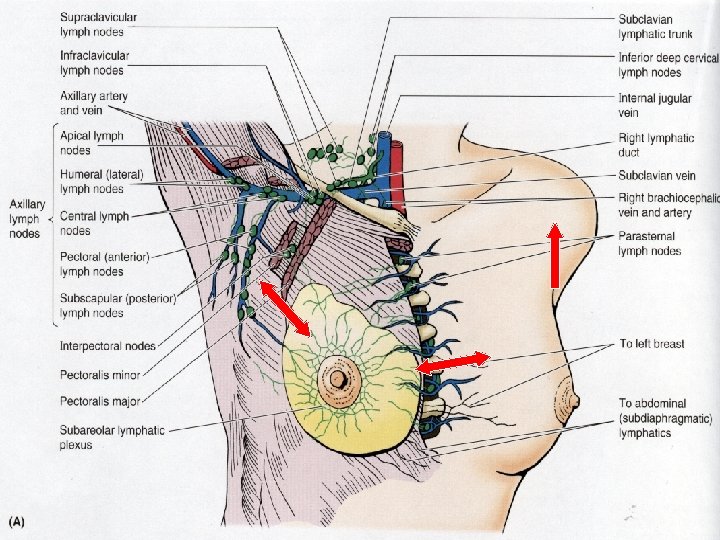
Mammary gland – lymph drainage 4 quadrants • nodi l. axillares – Sorgius‘ node = first (most caudal) one from group of nodi l. pectorales – on 2 nd/3 rd tooth of m. serratus anterior • nodi l. parasternales nodi. mediastinales ant. nodi epigastrci sup. + inf. • nodi l. supraclaviculares • contralaterally into other gland axilla plexus subareolaris Sappeyi
END
Mammary gland – nerves nn. intercostales IV. - VI. rami ant. + lat. Sensitive plexus around areola mammae (T 4)

END
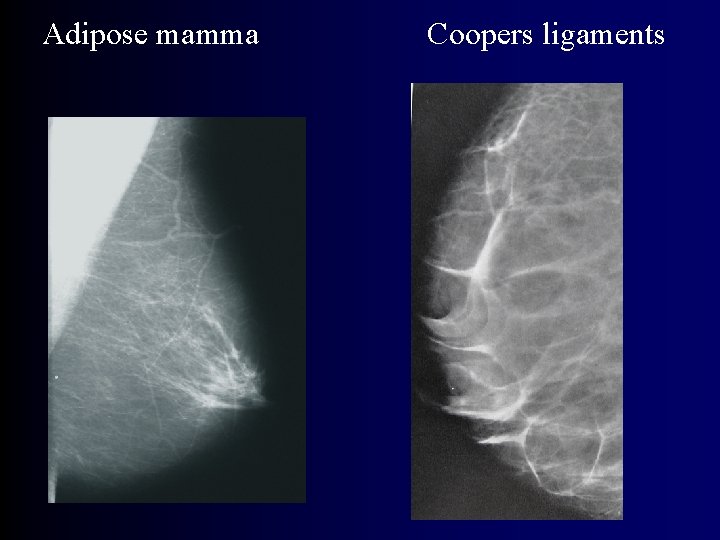
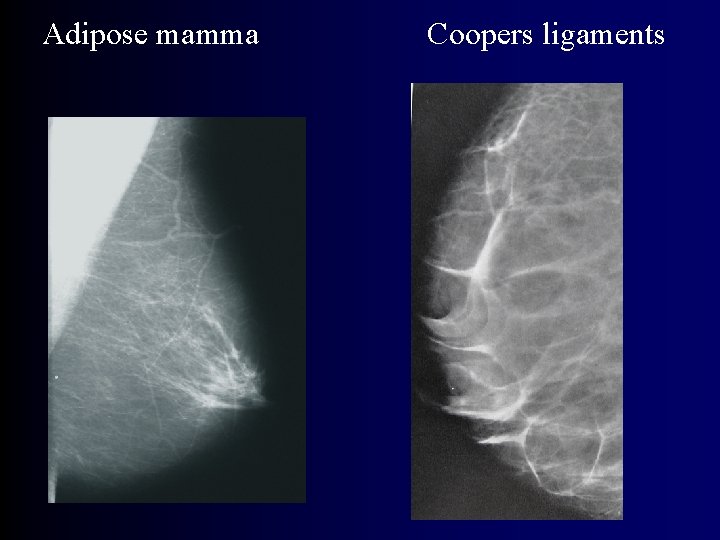
Adipose mamma Coopers ligaments
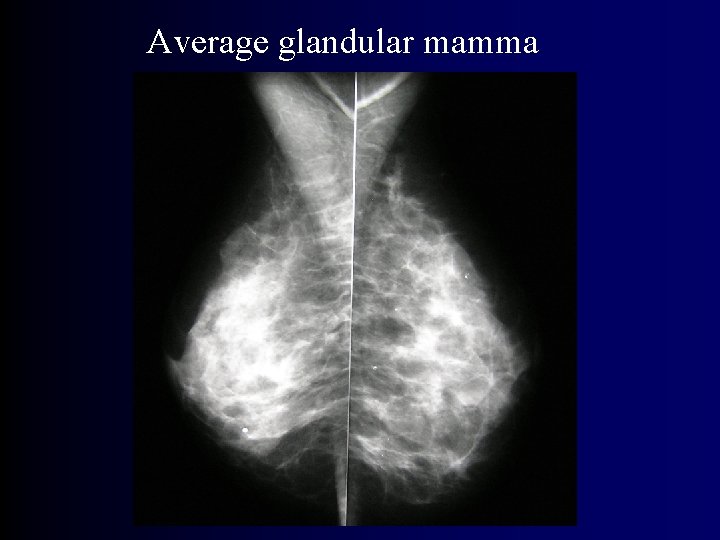
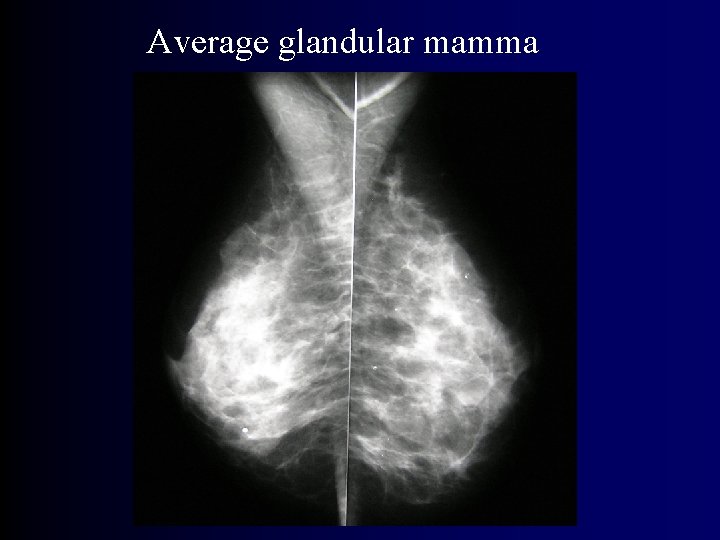
Average glandular mamma
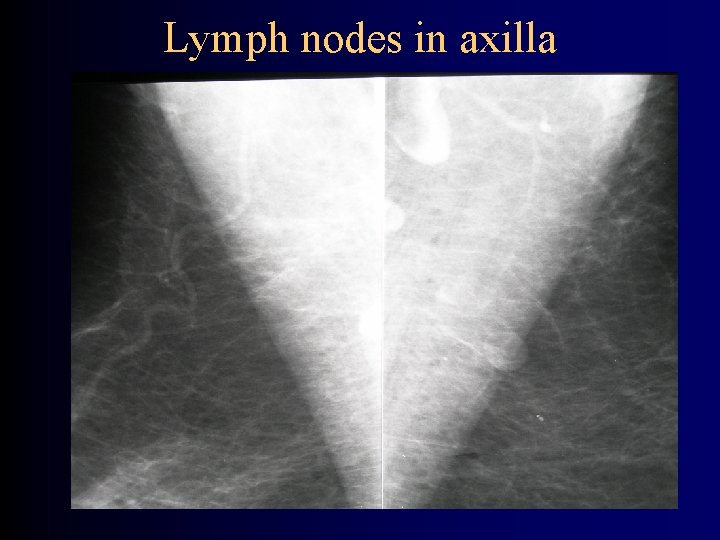
Lymph nodes in axilla


Anogenital adnexal glands • • • van der Putte 1991 Compositionally similar to mamma Transition between eccrine and apocrine hormonal receptors cyclic changes sulcus interlabialis, perianally ? function – perhaps sexual function

Hypodermis (Tela subcutanea) • retinacula cutis – retinaculum caudale • panniculus adiposus – stratum musculorum – stratum fibrosum • stratum membranosum • textus connectivus laxus • bursae synoviales subcutaneae
 Tubercula areolae
Tubercula areolae Lactating female
Lactating female Systema integumentum
Systema integumentum Systema integumentum
Systema integumentum Communion of the holy spirit
Communion of the holy spirit Cognitive therapy ap psychology
Cognitive therapy ap psychology Couplage par impédance commune
Couplage par impédance commune échéance moyenne formule
échéance moyenne formule Transistor bipolaire en régime dynamique
Transistor bipolaire en régime dynamique Suger
Suger Which city established itself as a free commune in 1125?
Which city established itself as a free commune in 1125? Caput commune extensorum
Caput commune extensorum Definition commune
Definition commune Membrana tectoria ohr
Membrana tectoria ohr Definition commune
Definition commune Ius commune definition
Ius commune definition Stratum lucidum
Stratum lucidum Thin skin vs thick skin
Thin skin vs thick skin Milady chapter 23 pdf
Milady chapter 23 pdf Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs What is rebound tenderness in appendicitis
What is rebound tenderness in appendicitis Human excretory system function
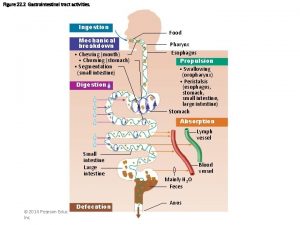
Human excretory system function Accessory organ of the digestive system
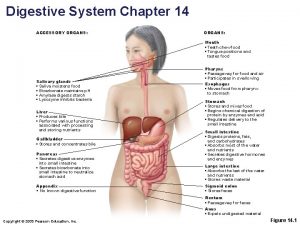
Accessory organ of the digestive system Manus region
Manus region Biomaterials artificial organs and tissue engineering
Biomaterials artificial organs and tissue engineering Accessory organs
Accessory organs Posterior abdominal wall
Posterior abdominal wall Red and white blood cells difference
Red and white blood cells difference Akar dikotil
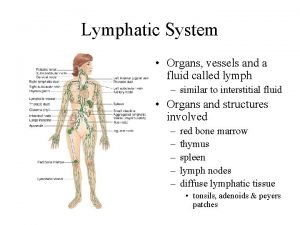
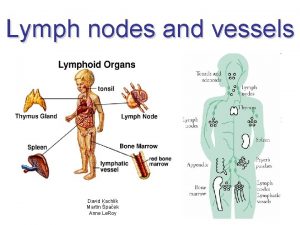
Akar dikotil Function of lymphatic system
Function of lymphatic system Plant tissue and organs
Plant tissue and organs Change of gases
Change of gases Frog
Frog Organs of wto
Organs of wto Analogous homologous and vestigial structures
Analogous homologous and vestigial structures English vowel sounds
English vowel sounds Ligaments of the stomach
Ligaments of the stomach Ligament of stomach
Ligament of stomach Superior duodenal recess
Superior duodenal recess Adh release
Adh release Bee organs
Bee organs Urinary structure
Urinary structure What moves the food in the digestive organs
What moves the food in the digestive organs Sense organs
Sense organs Proves anatòmiques
Proves anatòmiques Sensory system organs
Sensory system organs Description of the larynx
Description of the larynx Plant organs
Plant organs Articulators theatre definition
Articulators theatre definition Articulatory organs
Articulatory organs A.k.a. little organs.
A.k.a. little organs. Plant organs
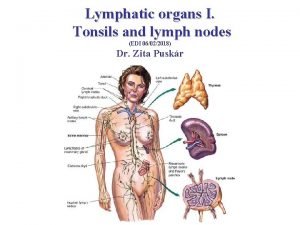
Plant organs Malt tonsils
Malt tonsils Invertebrate digestive system
Invertebrate digestive system Respiratory organs of invertebrates
Respiratory organs of invertebrates Nails integumentary system
Nails integumentary system Central lymphoid organs
Central lymphoid organs Articulatory organs
Articulatory organs Images of sense organs with names
Images of sense organs with names Frog organs
Frog organs Urinary bladder with peritoneum
Urinary bladder with peritoneum Excretory organ?
Excretory organ? Vestigial organs
Vestigial organs Name the three organs of the government
Name the three organs of the government Directional term
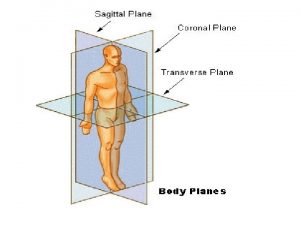
Directional term Internal organs
Internal organs Plica sublingualis
Plica sublingualis Types of salivary glands
Types of salivary glands Little nicky (cat)
Little nicky (cat) Posterior view of the female reproductive organs
Posterior view of the female reproductive organs Plant organs
Plant organs Female reproductive organs sagittal section
Female reproductive organs sagittal section Accessory organs of the digestive system
Accessory organs of the digestive system Otolithic organs
Otolithic organs Abdominopelvic organs
Abdominopelvic organs Umbilical regions
Umbilical regions Organs in each quadrant
Organs in each quadrant Hollow organs
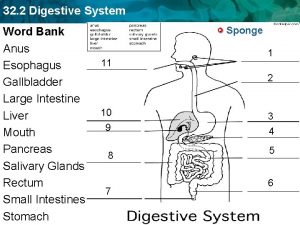
Hollow organs Digestive system word bank
Digestive system word bank Organs forming the respiratory passageway
Organs forming the respiratory passageway Torso organs
Torso organs Reptiles organs for locomotion
Reptiles organs for locomotion Generative lymphoid organs
Generative lymphoid organs Six main organs of the united nations
Six main organs of the united nations Excretory organs in mammals
Excretory organs in mammals Pulmonary ventilation
Pulmonary ventilation Rat dissection quiz
Rat dissection quiz Aphi sada u rat yaya
Aphi sada u rat yaya Organs xxx
Organs xxx Organs of speech presentation
Organs of speech presentation Sense organs for class 1
Sense organs for class 1 A group of organs working together
A group of organs working together Lymphatic system organs
Lymphatic system organs Lingual tonsil
Lingual tonsil Frog
Frog Osteichthyes locomotion
Osteichthyes locomotion Main function of major organs
Main function of major organs