Skeletal Tissues Chapter 7 Anatomy Bone Tissue Compact
Skeletal Tissues Chapter 7 Anatomy
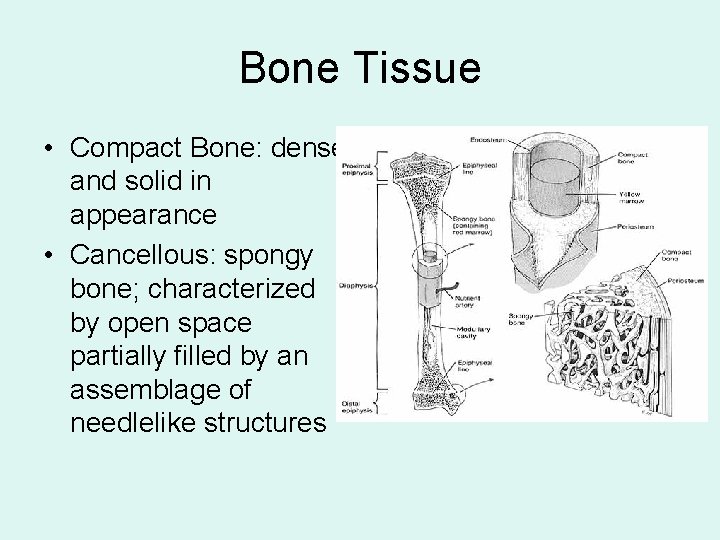
Bone Tissue • Compact Bone: dense and solid in appearance • Cancellous: spongy bone; characterized by open space partially filled by an assemblage of needlelike structures

Types of Bones 1. Long Bones: longitudinal axes and uniquely shaped articular ends 2. Short Bones: cube or box shaped bones 3. Flat Bones: generally broad and thin with flattened and often curved surfaces • Red marrow found in the compact bone on the inside; used to diagnose certain diseases 4. Irregular Bones: clustered in groups and come in various sizes and shapes
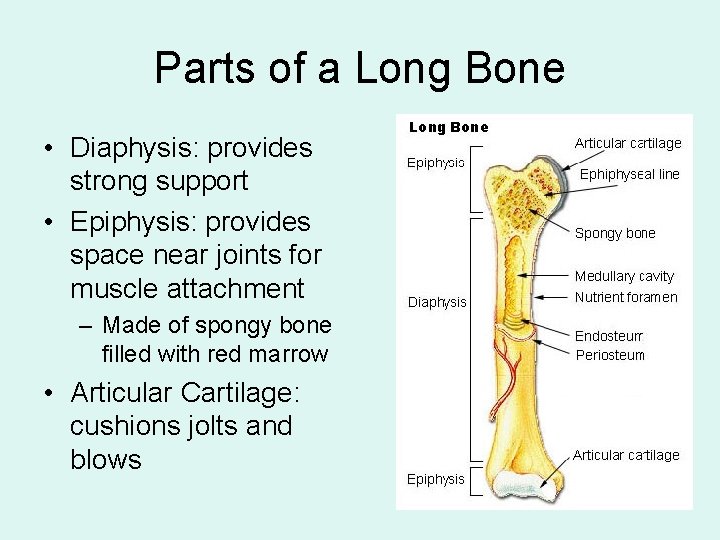
Parts of a Long Bone • Diaphysis: provides strong support • Epiphysis: provides space near joints for muscle attachment – Made of spongy bone filled with red marrow • Articular Cartilage: cushions jolts and blows
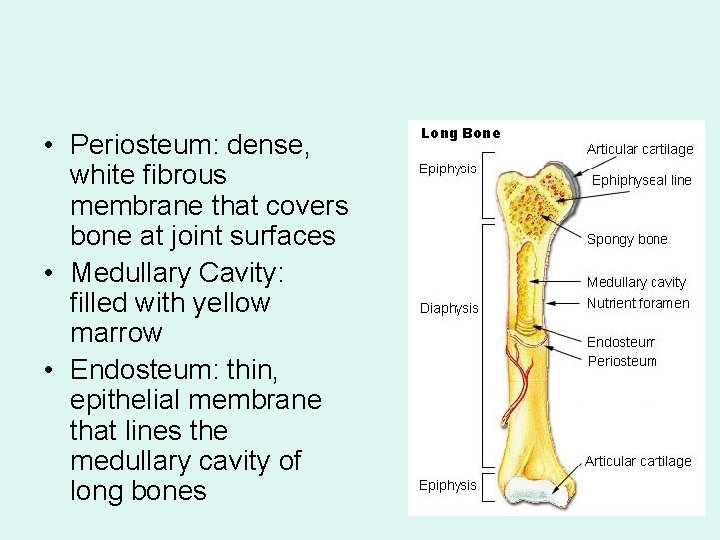
• Periosteum: dense, white fibrous membrane that covers bone at joint surfaces • Medullary Cavity: filled with yellow marrow • Endosteum: thin, epithelial membrane that lines the medullary cavity of long bones
Bone Tissue • Aka osseous tissue • Consists of cells, fibers, and primarily matrix – Matrix is hard and calcified

Bone Matrix • Two major components 1. Inorganic Salts: hydroxyapatite which are specialized chemical crystals of calcium and phosphate – Resistance to stress and mechanical deformation 2. Organic Matrix: composed of collagenous fibers and a mixture of protein and polysaccharides called ground substance – Gives bone plastic-like resilience
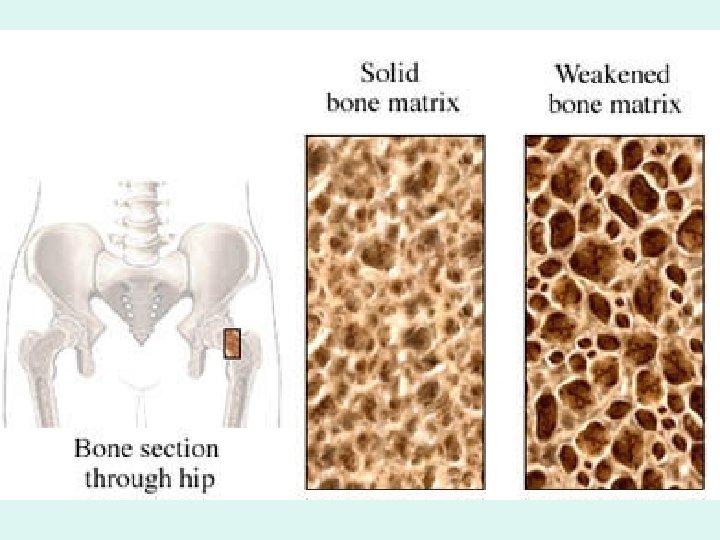
Measuring Bone Mineral Density • Osteoporosis: loss of bone mineral density, increased fragility, and susceptibility to fractures-especially of the spine, forearm, and hip. – Affects 45% of untreated women the first 10 years after menopause – Treated with estrogen or bone building drugs – Identified by radiographic absorptiometry
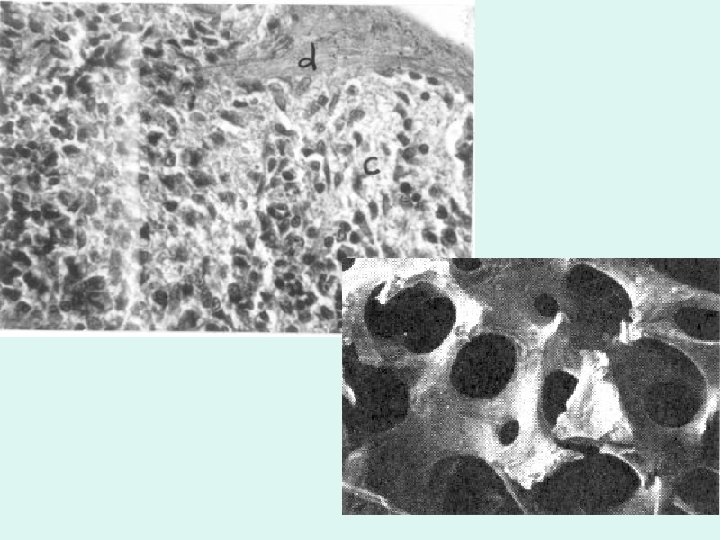
Compact Bone • Composed of Osteons or Haversian Systems – Osteons surround a canal – Living cells are cemented together – Allows for delivery of nutrients and removal of wastes
Structures of an Osteon • Lamellae: concentric, cylindrical-shaped layers of calcified matrix • Lacunae: small spaces containing tissue fluid in which bone cells lie imprisoned between the hard layers of the lamellae • Canaliculi: small canals radiating in all directions from the lacunae and connecting them to each other into a larger canal, the Haversian canal:
• Haversian Canal: extends lengthwise through the center of each Haversian System; contains blood vessels, lymphatic vessels and nerves • Volkman’s Canals: connects haversian canals allowing communication and containing nerves and vessels from the exterior to the osteons
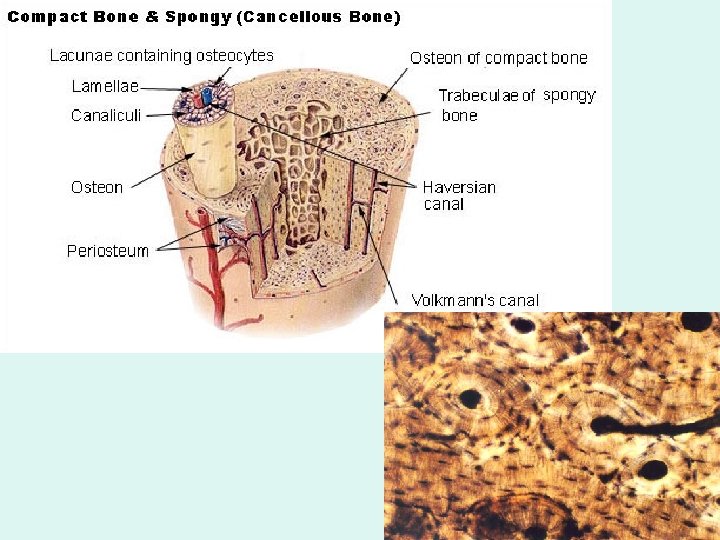
Cancellous Bone • Trabaculae: needlelike bony spicules that compose spongy bone – Arranged along lines of stress to enhance bone’s strength • Bone cells found within trabaculae • Nutrients are delivered and wastes removed through tiny canaliculi that extend to the surface of the very thin spicules
Bone Cells • Osteoblasts: “bone forming cells”; secrete specialized organic matrix called osteoid which serves as an important part of ground substance • Osteoclasts: “bone-reabsorbing cells”; responsible for active erosion of bone minerals, allows for continuous change and remodeling of bone tissue • Osteocytes: mature, nondividing osteoblasts that have become surrounded by matrix and now lie within lacunae
Bone Marrow • Soft, diffuse connective tissue called myeloid tissue • Found in the medullary cavity and spaces in spongy bone • Site of blood cell formation – Red marrow: site of red blood cell formation (more in children than adults unless of trauma) – Yellow marrow: no blood cell formation, contains fat (may convert to red marrow in times of need in adults)
Functions of Bone • Support: shape, alignment, and position of body parts • Protection: skull, rib cage protect organs • Movement: along with muscles act as levers for movement • Mineral Storage: of calcium, phosphorus, and other minerals • Hematopoiesis: blood cell formation
Regulation of Blood Calcium Levels • Bones are a reservoir for 98% of the bodies calcium – Maintains blood calcium levels – Calcium is controlled by the remodeling of bone by the osteoblasts and osteoclasts • Calcium is necessary for bone formation, blood clotting, transmission of nerve impulses, and maintenance of muscle contractions
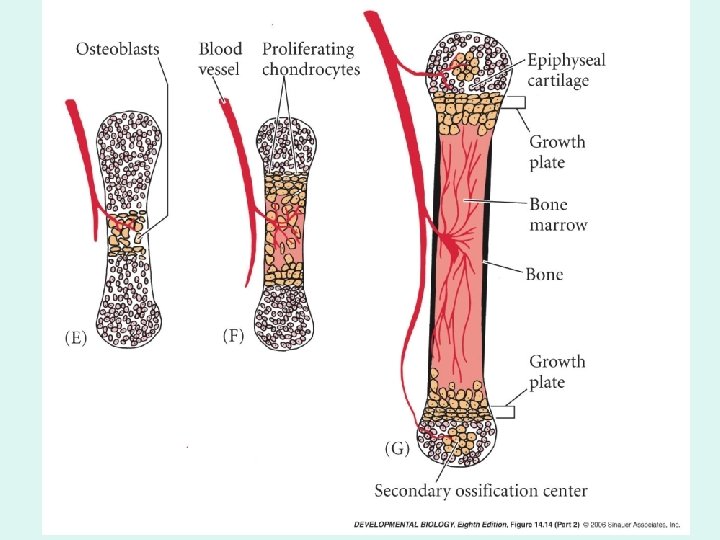
Development of Bone • As infants, bone starts as cartilage and goes through a calcification process to result in adult bone formation • Osteogenesis: combined action of osteoblasts and osteoclasts sculpting bone into their adult shapes – Allows bones to respond to injury (athletes normally have denser bones than nonathletes)
Types of Bone Formation 1. Intramembranous Ossification: process by which most flat bones are formed within connective tissue membranes 2. Endochondral Ossification: process by which bones are formed by replacement of cartilage ends
Bone Growth and Resorption • Growth in diameter of bone results when osteoblasts build new bone around the outside and osteoclasts enlarge the diameter of the medullary cavity • In adults ossification = resorption (until you reach about 40 years)
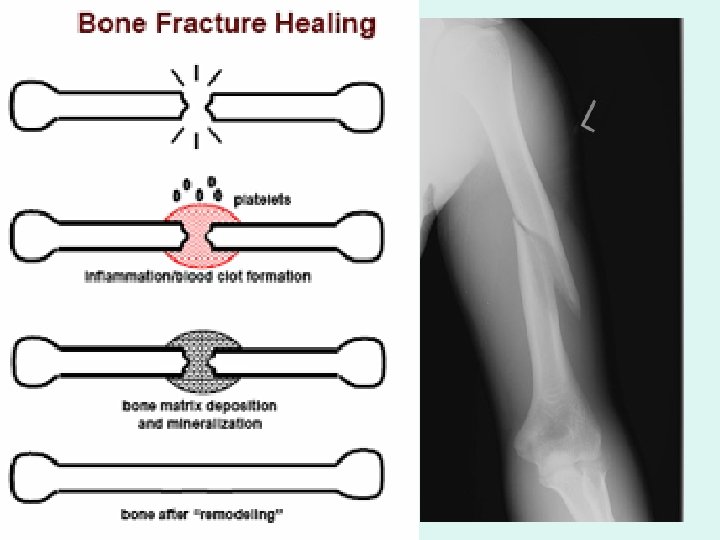
Repair of Fractures • Fracture: a break in continuity of the bone – Tears and destroys blood vessels – Fracture healing: the prototype of bone repair 1. Hemorrhaging and pooling of blood at the point of injury: fracture hematoma 2. Hematoma is resorbed and callus tissue forms to bone the broken ends of the fracture on the outside and in the inside of bone 3. Callus will be replaced with normal bone tissue
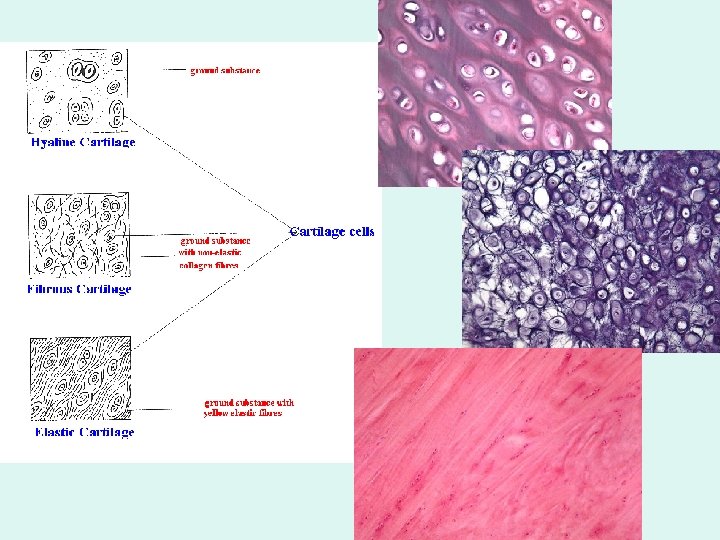
Cartilage • • Connective Tissue Fibers reinforced by matrix that is gel-like Mostly extracellular substance (few cells) No canal system or blood vessels (avascular) – Nutrients and oxygen reach cells (chondrocytes) via diffusion from capillaries in the covering of cartilage (perichondrium) • Three Types of Cartilage: differ in the amount of matrix and the amounts of elastic and collagenous fibers present
Types of Cartilage 1. Hyaline: most abundant 2. Elastic: very elastic (fewer collagenous fibers) • External ear, epiglottis, eustachian tubes 3. Fibrocartilage: most collagenous fibers; greatest tensile strength, little matrix • Symphysis pubis, intervertebral disks, points of attachment of some tendons to bones
Cartilage Growth • Two Types 1. Interstitial Growth: common in children: growth from within 2. Appositional Growth: common in adults: new matrix deposited on the surface of cartilage
- Slides: 29