Skeletal System Functions Support Protection Assist in movement
- Slides: 27
Skeletal System
Functions • • • Support Protection Assist in movement Mineral homeostasis Blood cell production (hemopoesis) Triglyceride storage
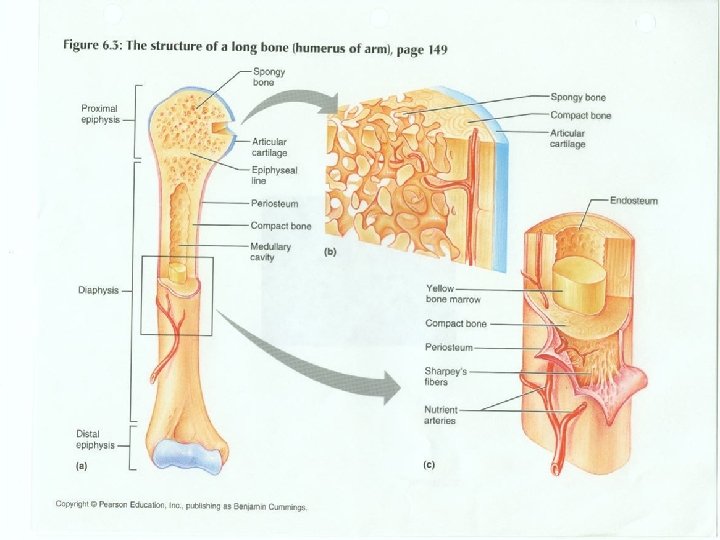
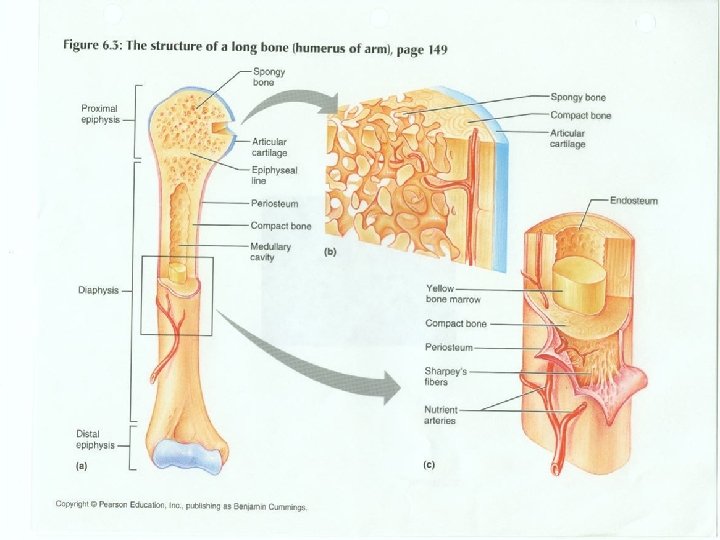
Bone Structure • Diaphysis – (long, cylindrical, main portion of bone) • Epiphysis – (distal and proximal ends of bone) • Articular Cartilage – (thin layer of hyline cartilage covering the epiphysis where bones form articulation) • Periosteum – (connective tissue that covers bone where there is no articular cartilage)
Bone structure continued • Medullary cavity – ( space within diaphysis that contains fatty yellow bone marrow) • Endosteum – ( lines medullary cavity and contains bone forming cells)
Composition of bone • 25% water • 25% Protein fibers • 50% mineral salts
Histology of bone Bone cells
Osteogenic Cells • Only bone cell that can undergo mitosis • Develop into osteoblasts
Osteoblasts • Bone building cells • Secrete collagen and other organic components
Osteocytes • Derived from osteoblasts • Form when osteoblasts become entrapped in matrix secretions • “House Keeping” cells
Osteoclasts • Derived from white blood cells • Maintain normal development, growth, maintenance, and repair of bone
Calcification or mineralization • Mineral salts crystallize in the microscopic spaces between collagen fibers • After spaces are filled, mineral crystals crystallize around collagen fibers • Mineral salts include: Calcium phosphate and Calcium carbonate • Collagen and mineral salts make bone rigid yet flexible
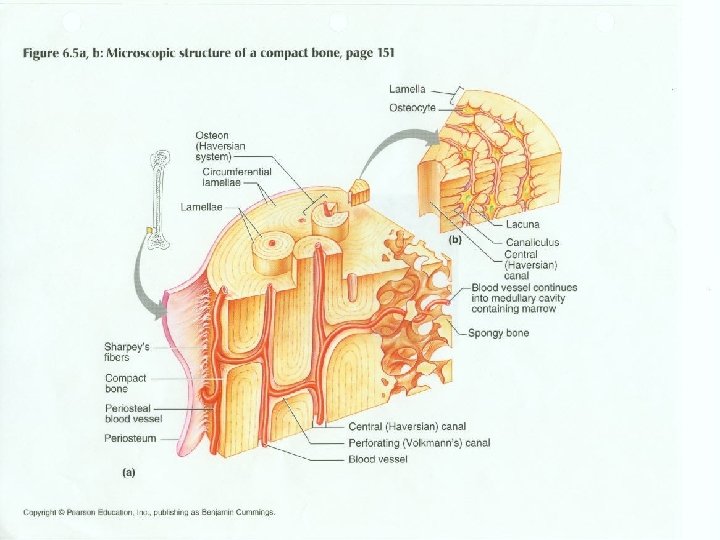
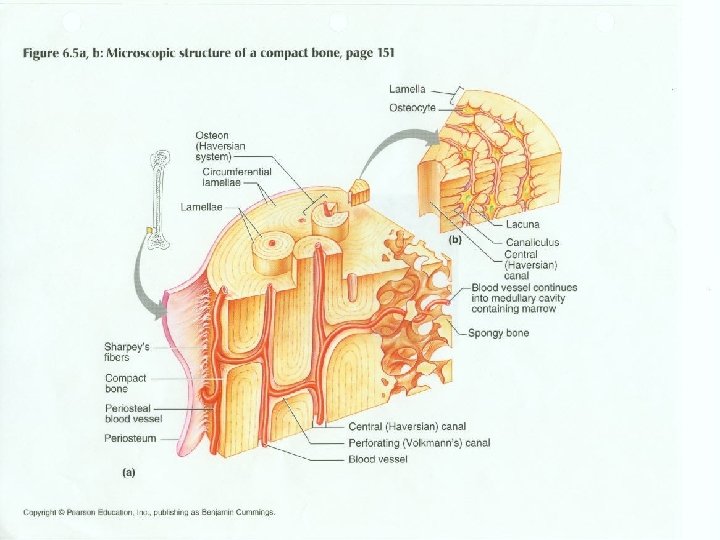
Compact bone tissue • Haversian system (osteons) make up unit of compact bone • Perforating canals allow blood vessels, lymphatic vessels, and nerves to penetrate bone tissue (run laterally) • Central (Haversian) canals – Run longitudinally and connect to perforating canals • Concentric Lamellae – Hard rings of bone matrix that form around central canals
Compact bone tissue continued • Lacunae – Holes that contain osteocytes and are found in lamellae • Canuliculi – Channels filled with extracellular fluid and projections of osteocytes which allow osteocytes to connect with each other and pass blood born nutrients and wastes)
Spongy bone • Trabeculae – Irregular lattice of thin columns of bone • Spaces between trabeculae are filled with marrow • Makes up most of the tissue of short, flat, and irregular shaped bones; most of the epiphysis of long bones and lines diaphysis • The spongy bone tissue in the hip bones, ribs, breastbone, backbones, and ends of long bones is the only sites of hemopoesis in adults
Endochondrial Ossification
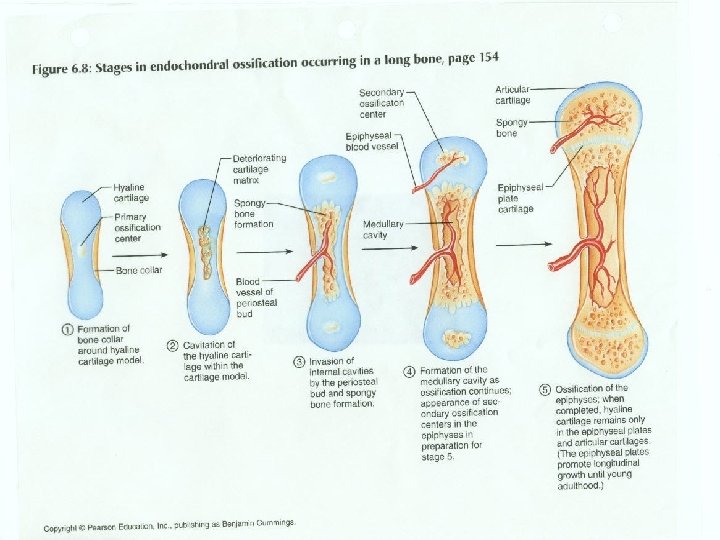
Development of cartilage model • Mesenchymal cells crowd together in shape of future bone • Mesenchymal cells differentiate into chondrocytes
Growth of cartilage model • Model grows in length by chondrocyte cell division • More cartilage is secreted and chondrocytes die
Development of primary ossification • Nutrient artery penetrates into model • Osteoblasts move in from periosteum • Osteoblasts deposit bone matrix over calcified cartilage forming spongy bone
Development of secondary ossification • The hyaline cartilage of diaphysis is replaced by bone • When nutrient artery penetrates into epiphysis secondary centers form
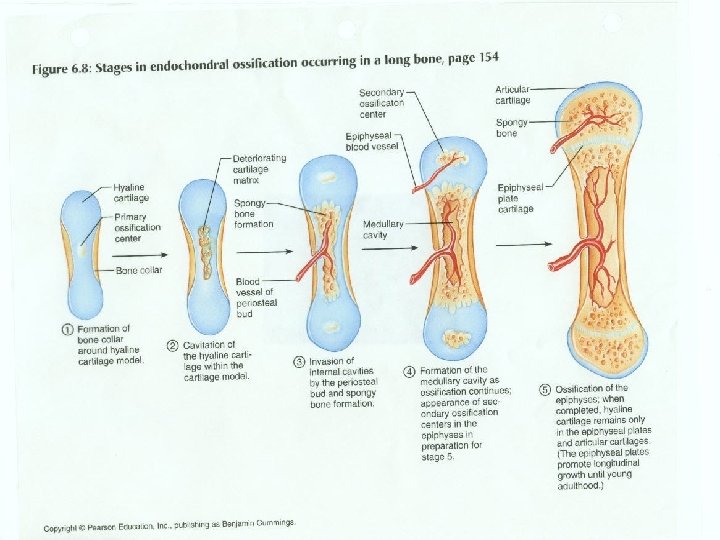
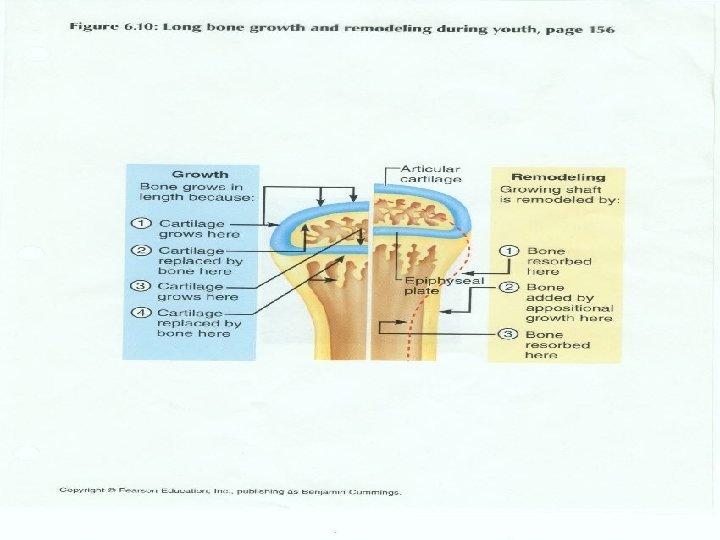
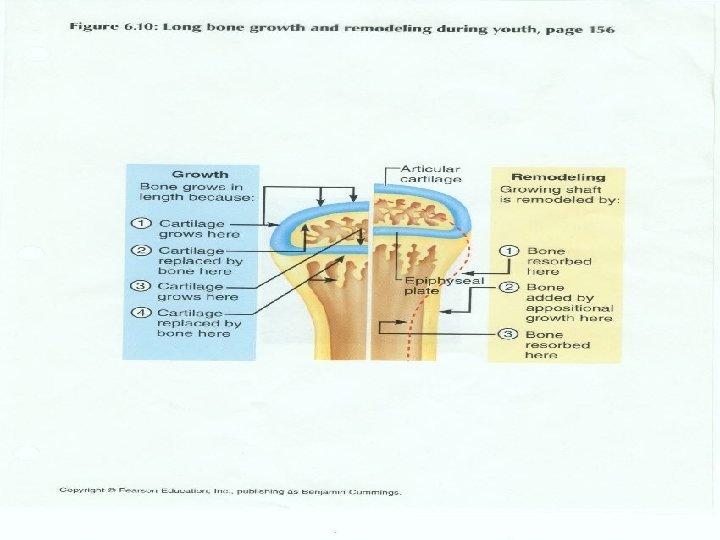
Formation of articular cartilage and epiphyseal plate • Hyaline cartilage becomes articular cartilage • Hyaline cartilage remains between diaphysis and epiphysis as epiphyseal plate which is responsible for lengthwise growth of long bones
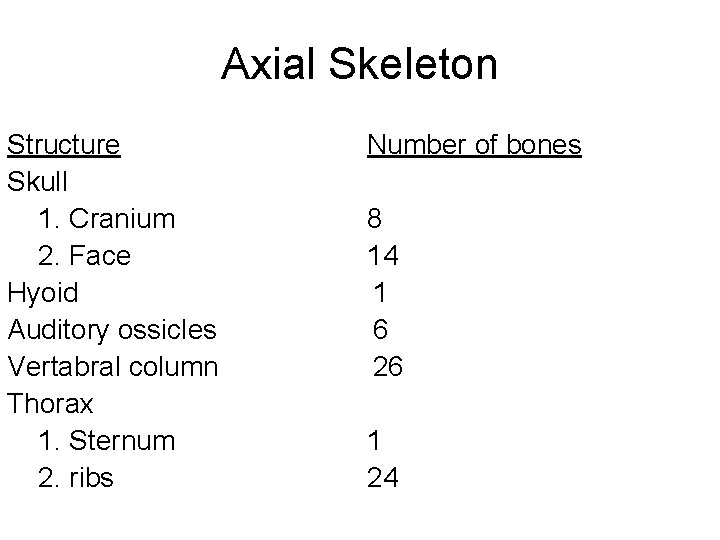
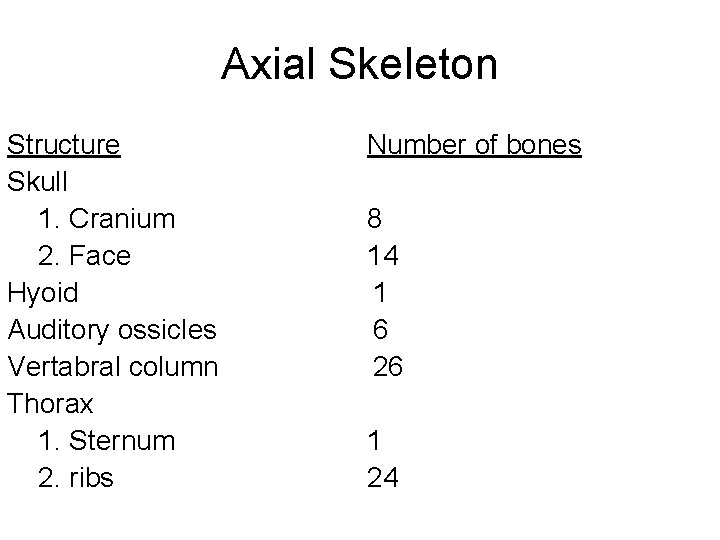
Axial Skeleton Structure Skull 1. Cranium 2. Face Hyoid Auditory ossicles Vertabral column Thorax 1. Sternum 2. ribs Number of bones 8 14 1 6 26 1 24
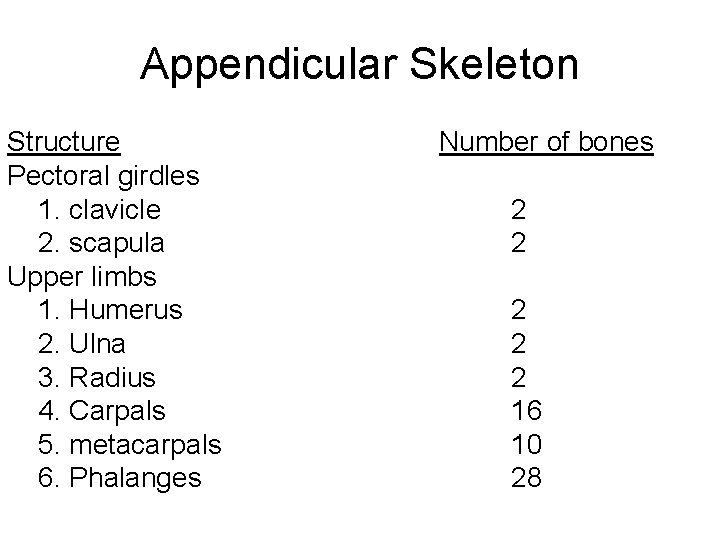
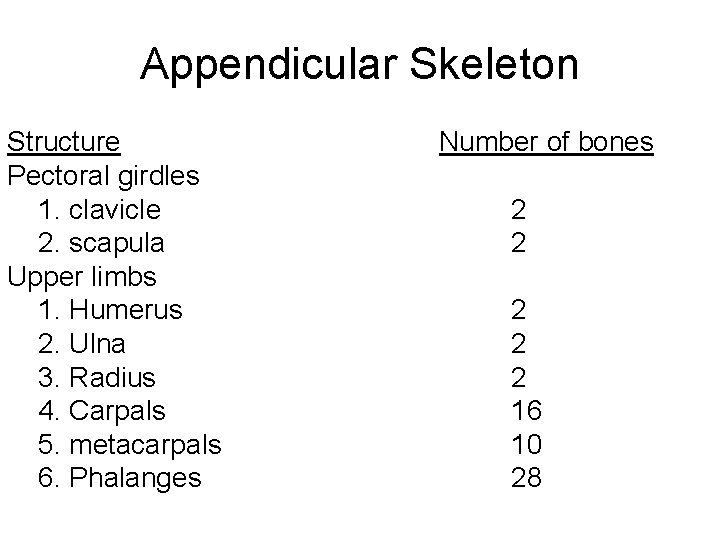
Appendicular Skeleton Structure Pectoral girdles 1. clavicle 2. scapula Upper limbs 1. Humerus 2. Ulna 3. Radius 4. Carpals 5. metacarpals 6. Phalanges Number of bones 2 2 2 16 10 28
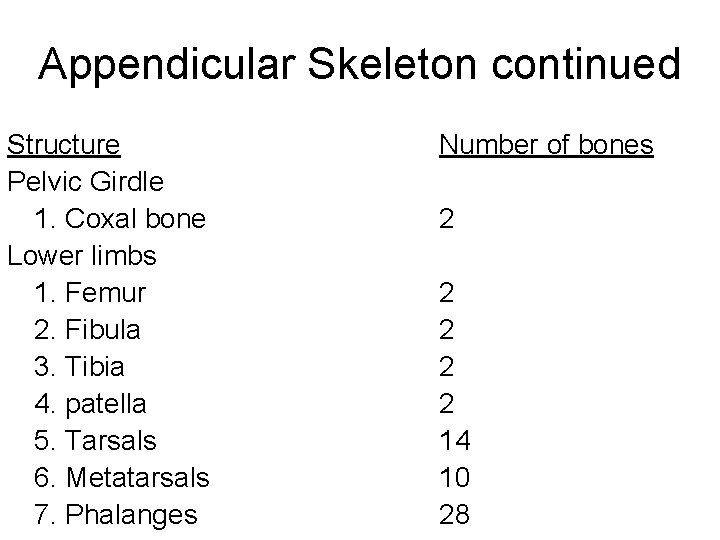
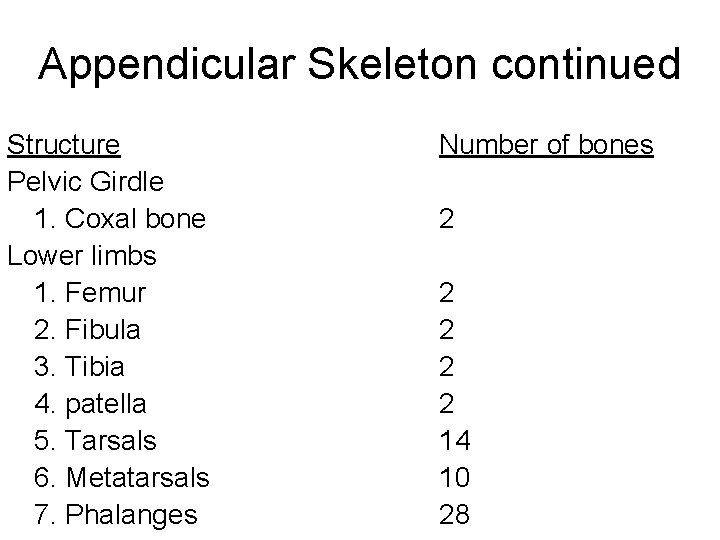
Appendicular Skeleton continued Structure Pelvic Girdle 1. Coxal bone Lower limbs 1. Femur 2. Fibula 3. Tibia 4. patella 5. Tarsals 6. Metatarsals 7. Phalanges Number of bones 2 2 2 14 10 28