Sinonasal Tumours Dr Mohammad aloulah Classification Malignant Benign
Sino-nasal Tumours Dr. Mohammad aloulah
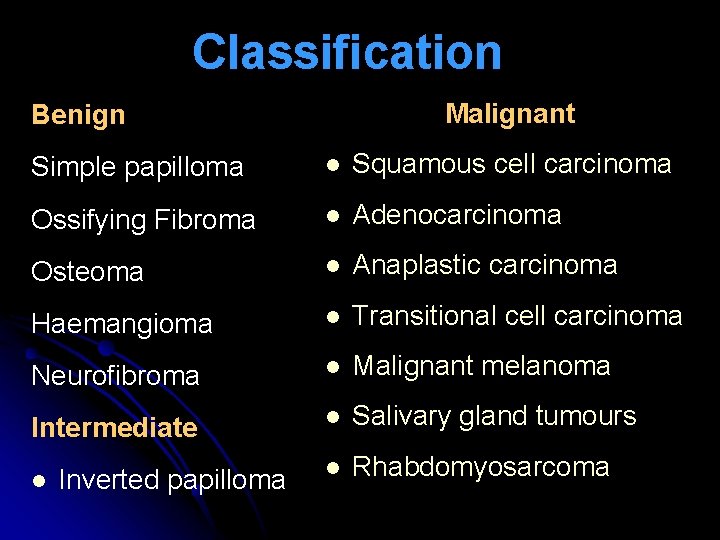
Classification Malignant Benign Simple papilloma l Squamous cell carcinoma Ossifying Fibroma l Adenocarcinoma Osteoma l Anaplastic carcinoma Haemangioma l Transitional cell carcinoma Neurofibroma l Malignant melanoma Intermediate l Salivary gland tumours l Rhabdomyosarcoma l Inverted papilloma
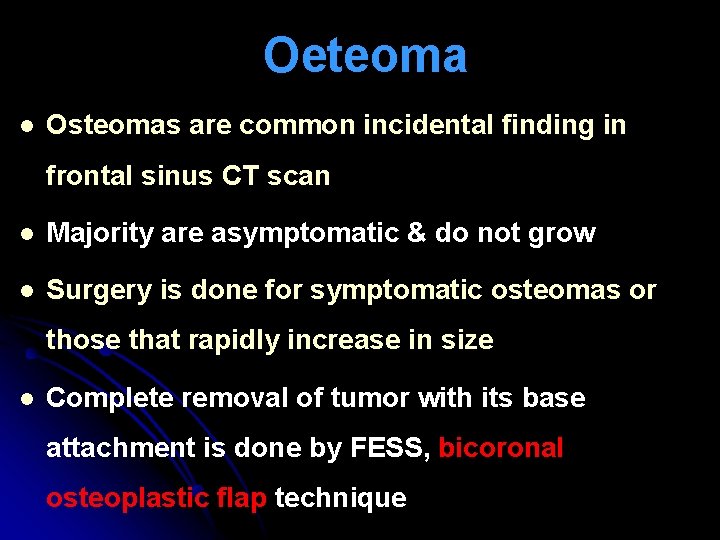
Oeteoma l Osteomas are common incidental finding in frontal sinus CT scan l Majority are asymptomatic & do not grow l Surgery is done for symptomatic osteomas or those that rapidly increase in size l Complete removal of tumor with its base attachment is done by FESS, bicoronal osteoplastic flap technique
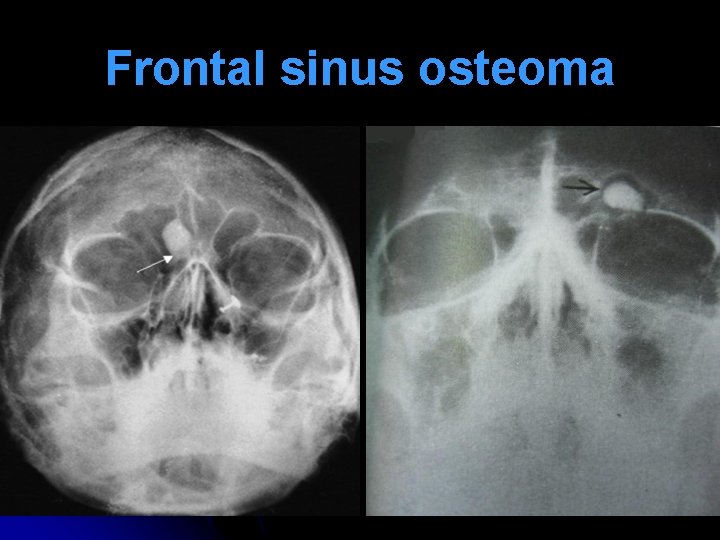
Frontal sinus osteoma

Bicoronal osteoplastic flap
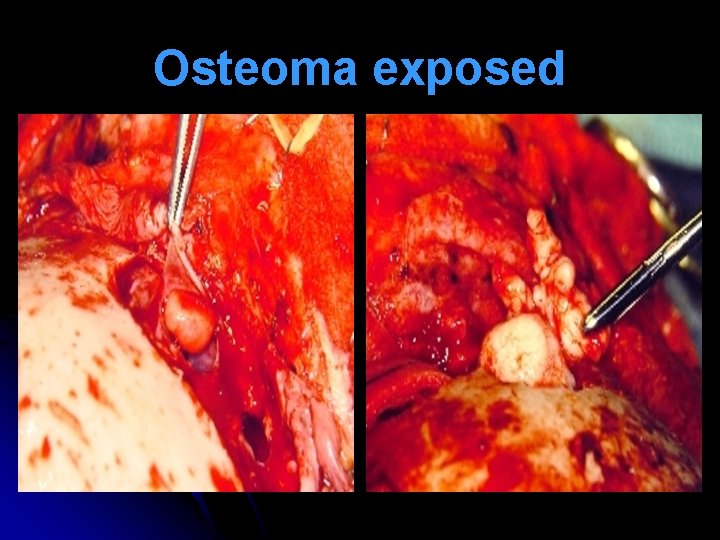
Osteoma exposed
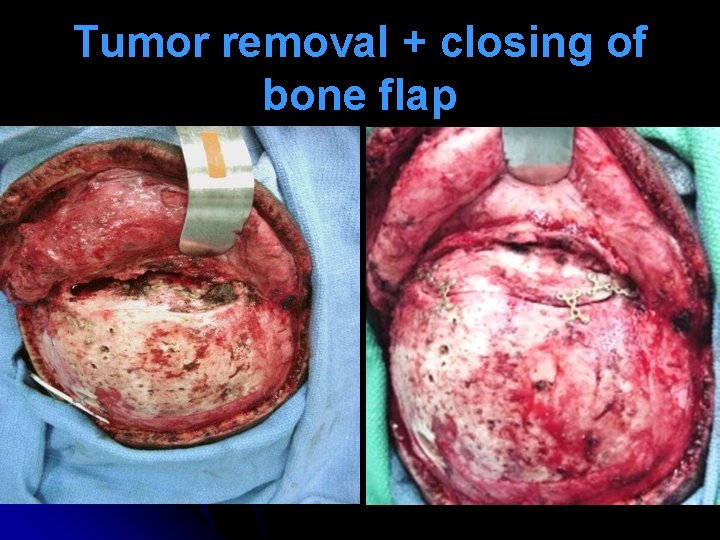
Tumor removal + closing of bone flap
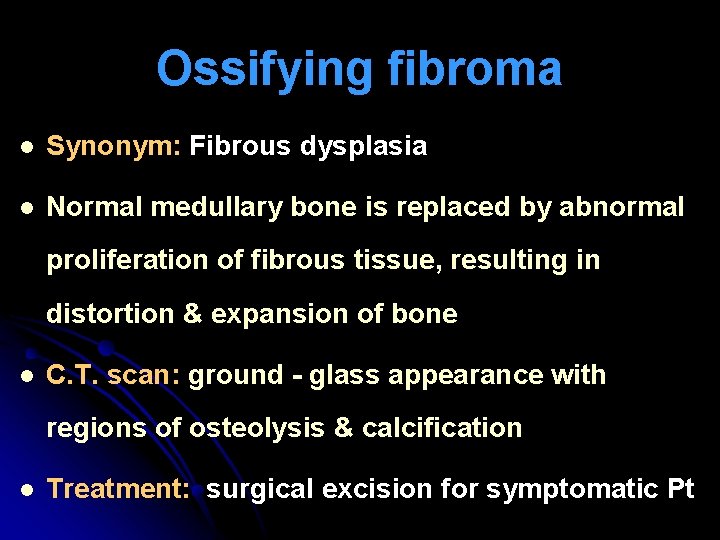
Ossifying fibroma l Synonym: Fibrous dysplasia l Normal medullary bone is replaced by abnormal proliferation of fibrous tissue, resulting in distortion & expansion of bone l C. T. scan: ground - glass appearance with regions of osteolysis & calcification l Treatment: surgical excision for symptomatic Pt
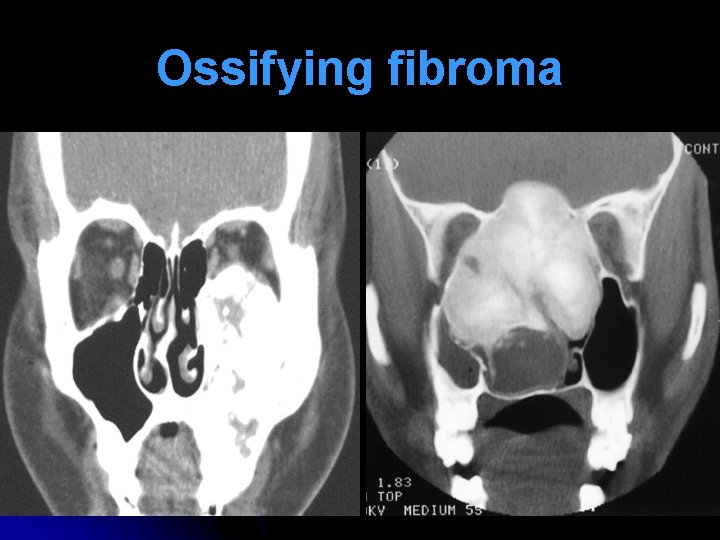
Ossifying fibroma
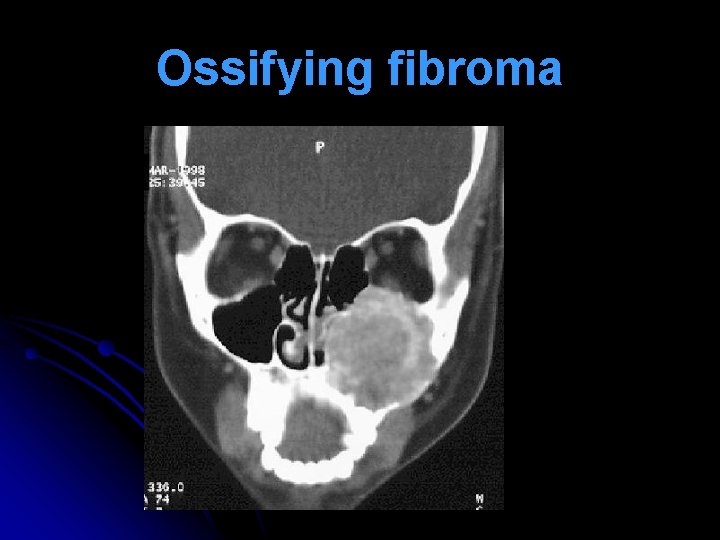
Ossifying fibroma
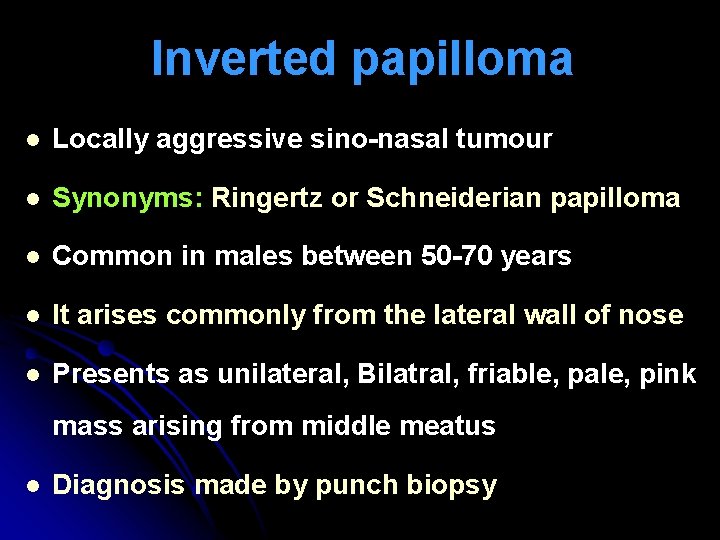
Inverted papilloma l Locally aggressive sino-nasal tumour l Synonyms: Ringertz or Schneiderian papilloma l Common in males between 50 -70 years l It arises commonly from the lateral wall of nose l Presents as unilateral, Bilatral, friable, pale, pink mass arising from middle meatus l Diagnosis made by punch biopsy

Inverted papilloma l Treatment: Endscopic medial maxillectomy and en bloc ethmoidectomy by lateral rhinotomy or midfacial degloving. l Inverted papilloma has a marked tendency to recur after surgical removal. l Squamous cell ca is present in 5 – 10 % cases.
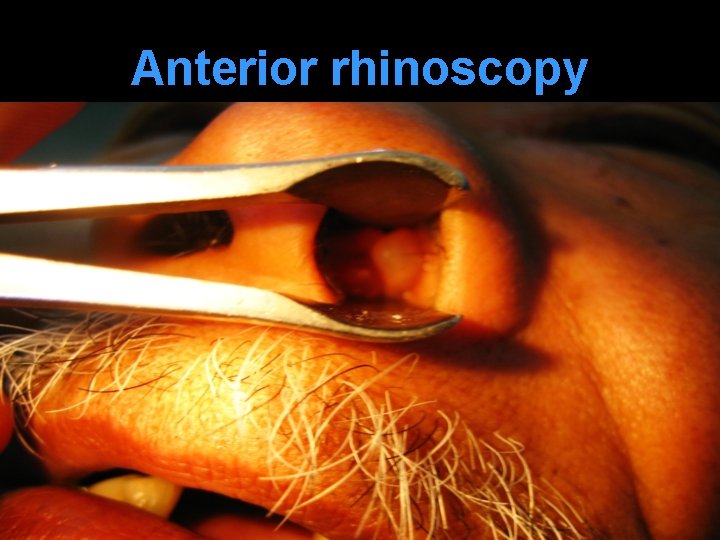
Anterior rhinoscopy
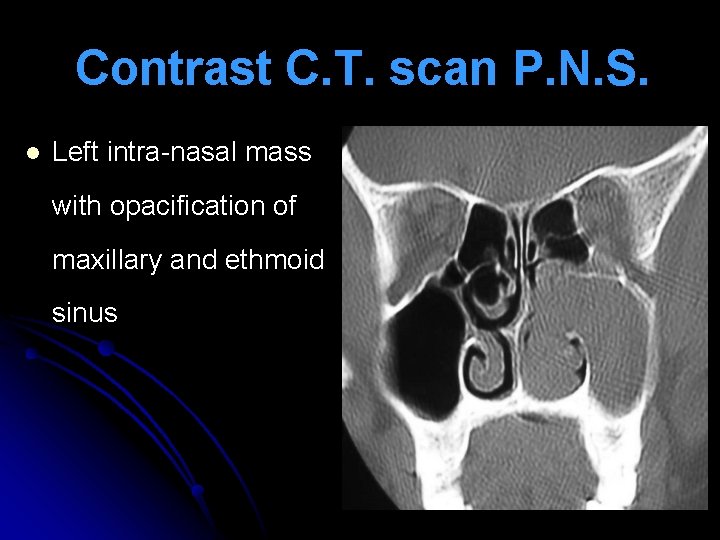
Contrast C. T. scan P. N. S. l Left intra-nasal mass with opacification of maxillary and ethmoid sinus
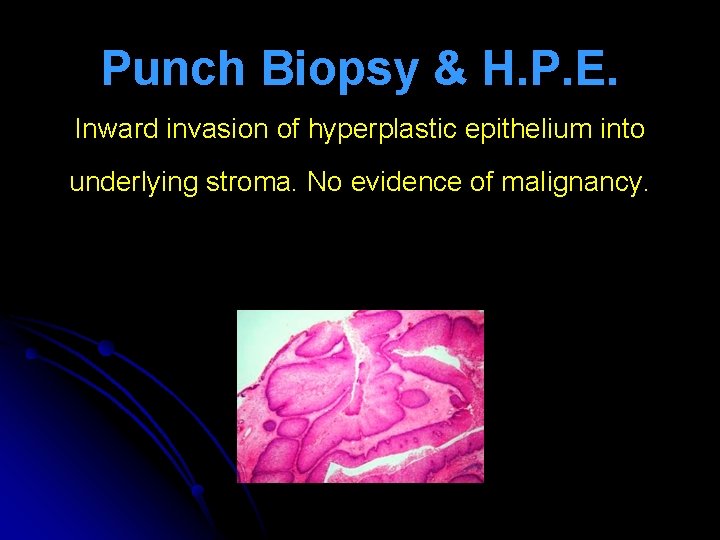
Punch Biopsy & H. P. E. Inward invasion of hyperplastic epithelium into underlying stroma. No evidence of malignancy.

lateral rhinotomy
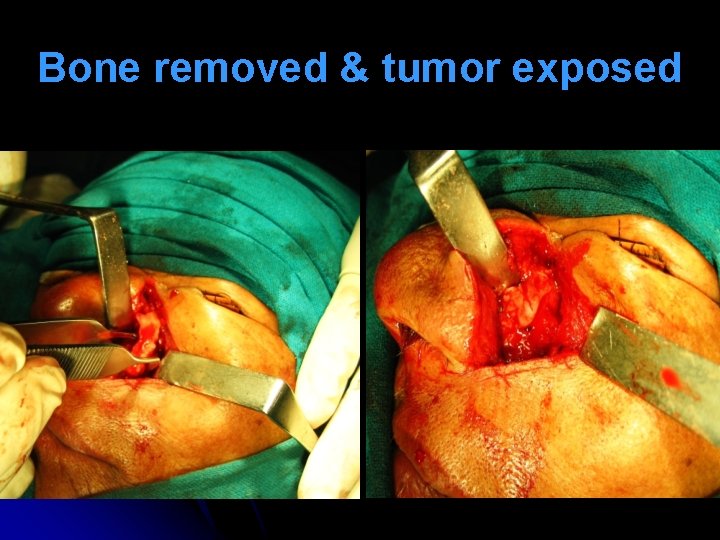
Bone removed & tumor exposed

Tumour removed & inicision closed
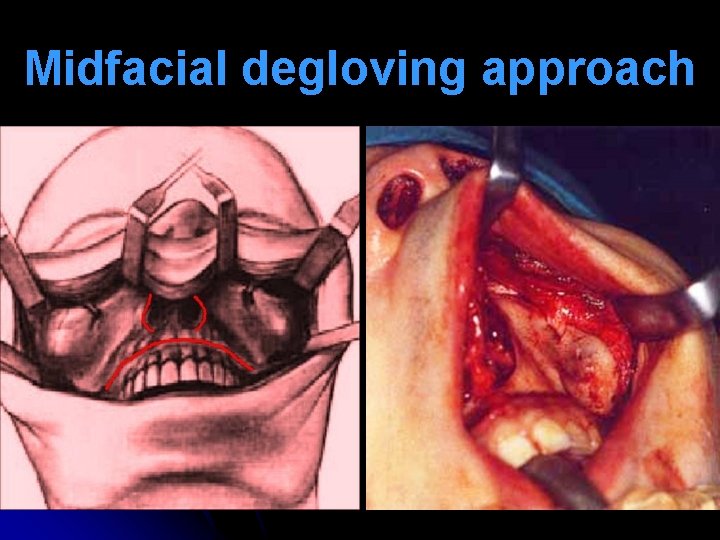
Midfacial degloving approach

Sino-nasal Malignancy
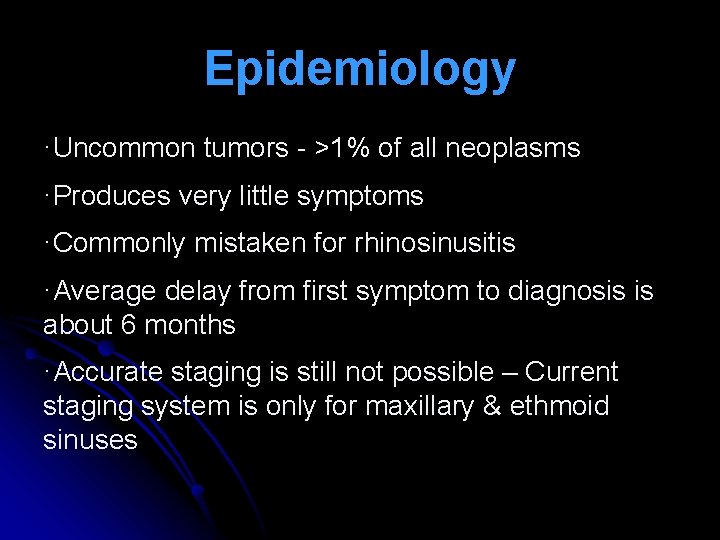
Epidemiology ·Uncommon tumors - >1% of all neoplasms ·Produces very little symptoms ·Commonly mistaken for rhinosinusitis ·Average delay from first symptom to diagnosis is about 6 months ·Accurate staging is still not possible – Current staging system is only for maxillary & ethmoid sinuses
Epidemiology ·Incidence – 1% per 100, 000 / year ·Commonly develop during 5 th – 6 th decades of life ·Twice as common in men than women ·Common sino-nasal malignancy – Primary epithelial tumors followed by non-epithelial malignant tumors ·Tumors arising from nose 25% and tumors arising from sinuses 75% · 60% of squamous carcinomas arise from maxillary sinus, 20% from nasal cavity rest from ethmoids. 1% arise from sphenoid
Common sinonasal malignancy ·Squamous cell carcinoma – commonest ·Adenocarcinomas ·Adenocystic carcinomas ·Undifferentiated carcinomas ·Non Hodgkin's lymphoma ·Melanomas
Adenocarcinoma

Risk factors l Hardwood dust (adenocarcinoma) l Softwood dust (squamous carcinoma) l Nickel refining; chromium workers l Boot, shoe and textile workers l Mustard gas exposure l Human papilloma virus
Maxillary sinus malignancy
Early Clinical features Mimic maxillary sinusitis l Nasal stuffiness l Blood-stained nasal discharge l Facial paraesthesias or pain l Epiphora
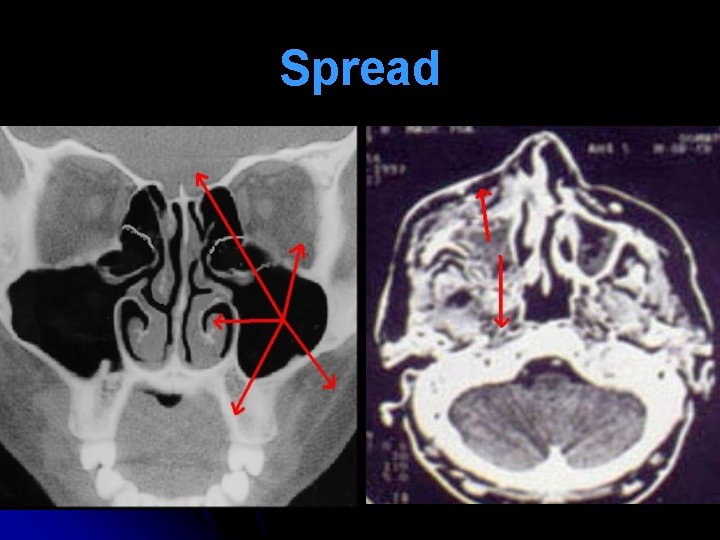
Spread
Late Clinical features Medial spread: l Unilateral nasal obstruction l Unilateral purulent nasal discharge l Epistaxis l Unilateral, friable, nasal mass Anterior spread: l Cheek swelling l Invasion of facial skin
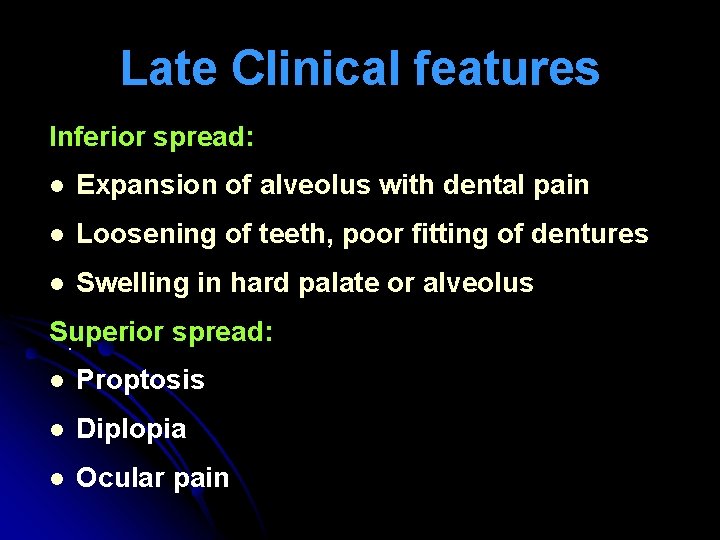
Late Clinical features Inferior spread: l Expansion of alveolus with dental pain l Loosening of teeth, poor fitting of dentures l Swelling in hard palate or alveolus Superior spread: . l Proptosis l Diplopia l Ocular pain
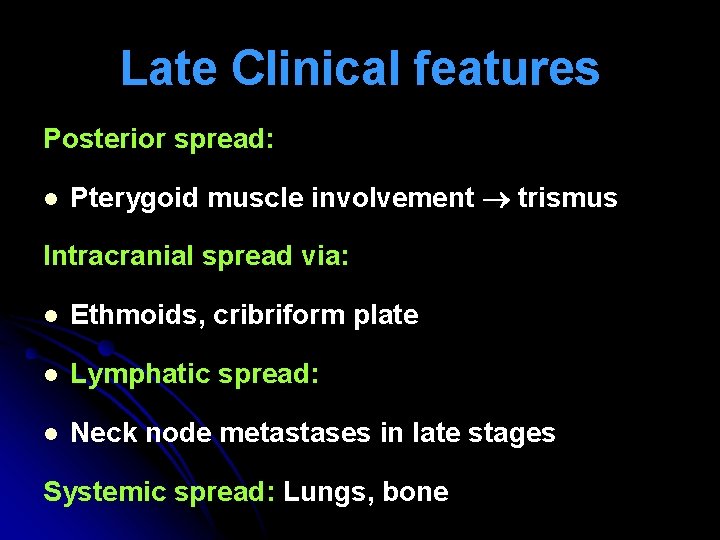
Late Clinical features Posterior spread: l Pterygoid muscle involvement trismus Intracranial spread via: l Ethmoids, cribriform plate l Lymphatic spread: l Neck node metastases in late stages Systemic spread: Lungs, bone

Cheek swelling

Cheek skin involvement

Alveolar & Palatal swelling
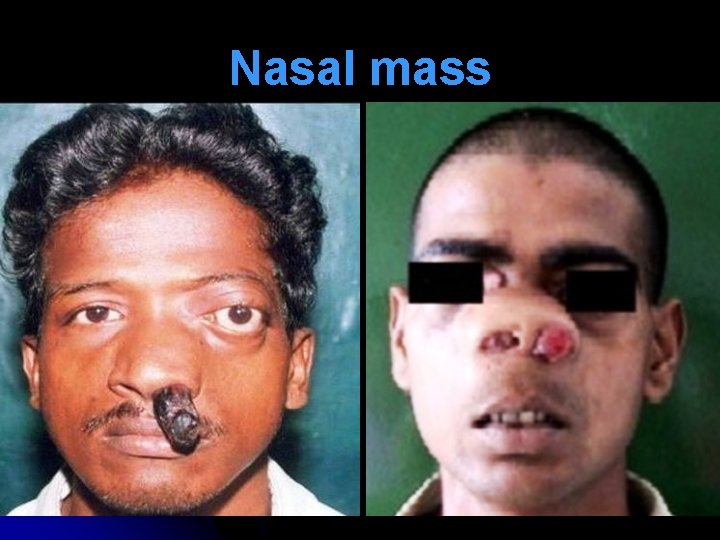
Nasal mass
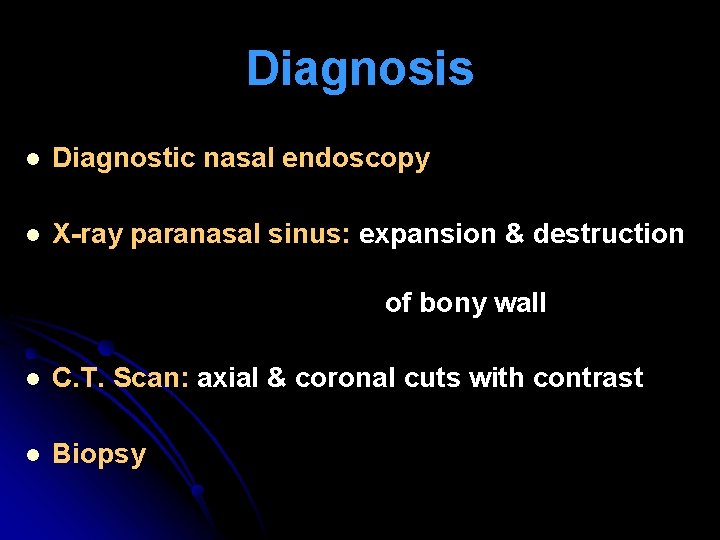
Diagnosis l Diagnostic nasal endoscopy l X-ray paranasal sinus: expansion & destruction of bony wall l C. T. Scan: axial & coronal cuts with contrast l Biopsy
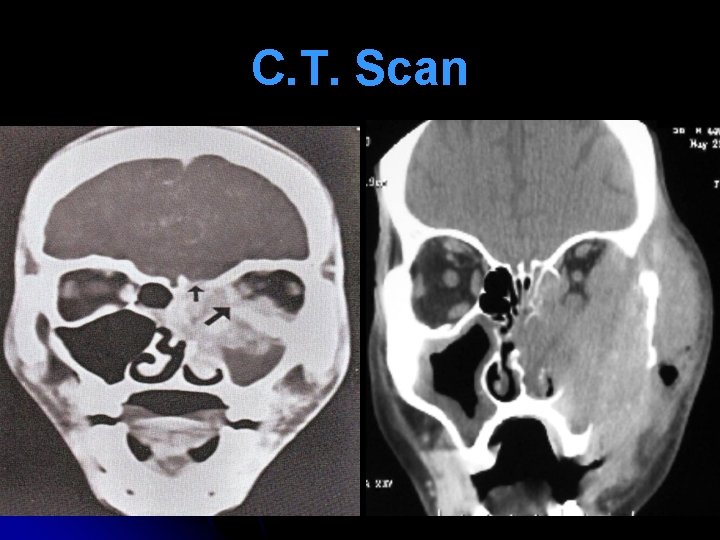
C. T. Scan
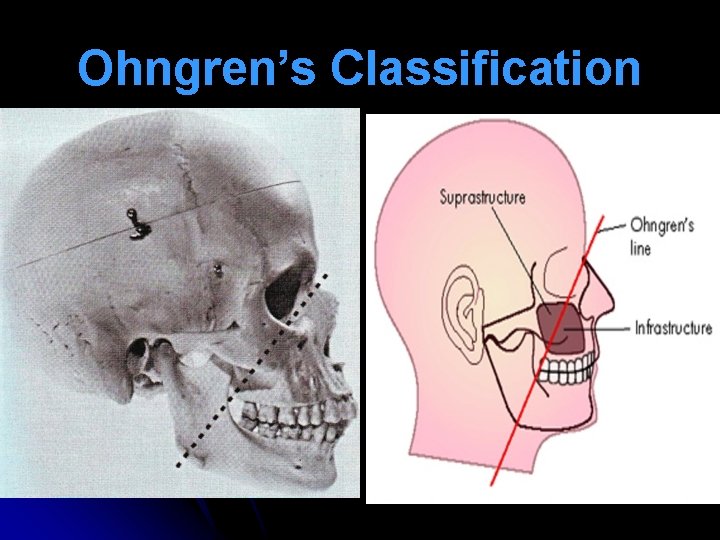
Ohngren’s Classification
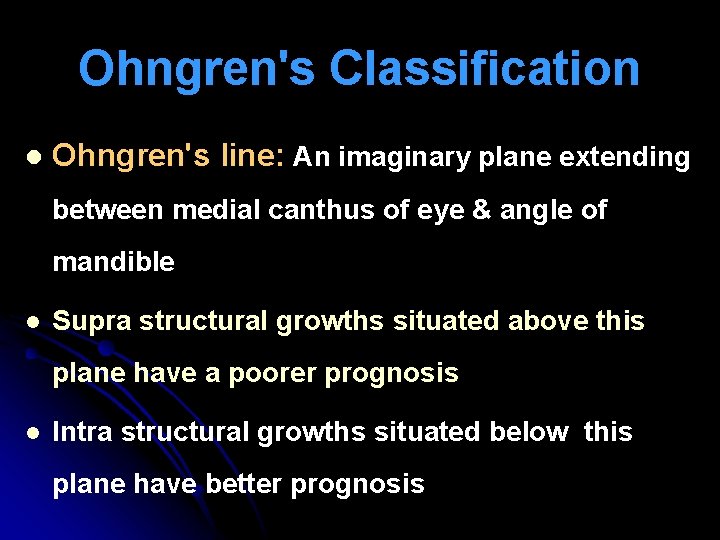
Ohngren's Classification l Ohngren's line: An imaginary plane extending between medial canthus of eye & angle of mandible l Supra structural growths situated above this plane have a poorer prognosis l Intra structural growths situated below this plane have better prognosis
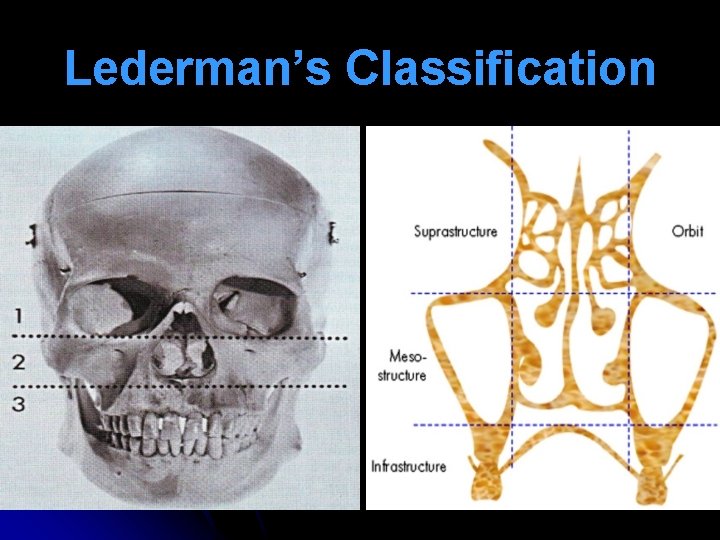
Lederman’s Classification
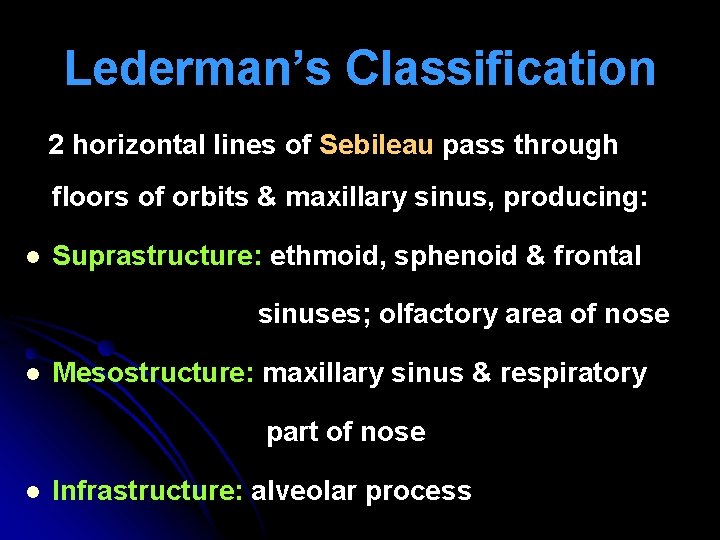
Lederman’s Classification 2 horizontal lines of Sebileau pass through floors of orbits & maxillary sinus, producing: l Suprastructure: ethmoid, sphenoid & frontal sinuses; olfactory area of nose l Mesostructure: maxillary sinus & respiratory part of nose l Infrastructure: alveolar process
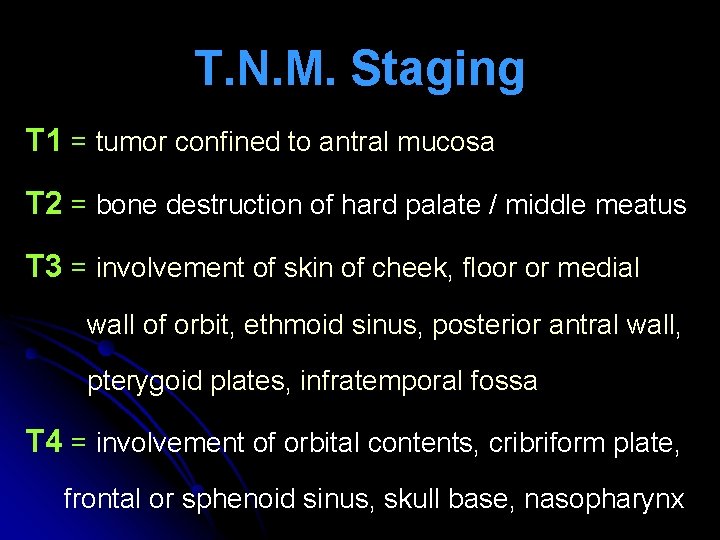
T. N. M. Staging T 1 = tumor confined to antral mucosa T 2 = bone destruction of hard palate / middle meatus T 3 = involvement of skin of cheek, floor or medial wall of orbit, ethmoid sinus, posterior antral wall, pterygoid plates, infratemporal fossa T 4 = involvement of orbital contents, cribriform plate, frontal or sphenoid sinus, skull base, nasopharynx

Treatment l T 1 & T 2 = Surgery or Radiotherapy l T 3 = Surgery + Radiotherapy l T 4 = Surgery + Radiotherapy + Chemotherapy l Europeans: pre-operative Radiotherapy (50006500 c. Gy) surgery after 4 -6 weeks l Americans: Surgery post-operative Radiotherapy after 4 -6 weeks
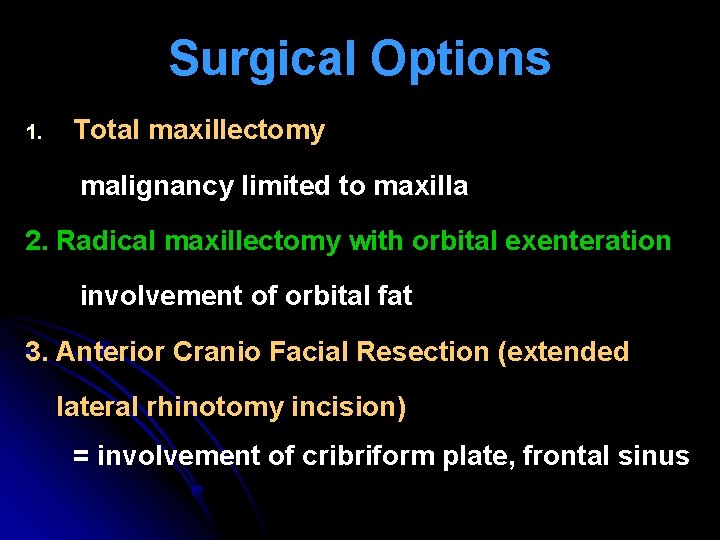
Surgical Options 1. Total maxillectomy malignancy limited to maxilla 2. Radical maxillectomy with orbital exenteration involvement of orbital fat 3. Anterior Cranio Facial Resection (extended lateral rhinotomy incision) = involvement of cribriform plate, frontal sinus

Palatal defect & prosthesis
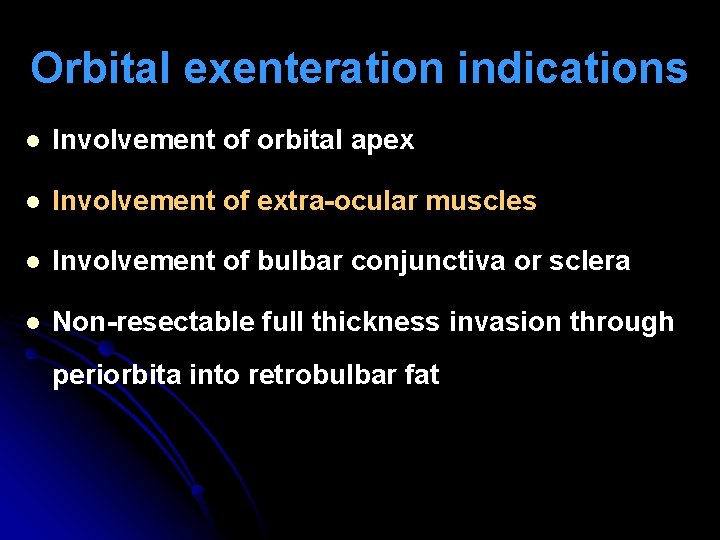
Orbital exenteration indications l Involvement of orbital apex l Involvement of extra-ocular muscles l Involvement of bulbar conjunctiva or sclera l Non-resectable full thickness invasion through periorbita into retrobulbar fat

Thank You
- Slides: 48