Single Ventricle Palliation Stage One Reconstruction Louise Callow
- Slides: 19
Single Ventricle Palliation: Stage One Reconstruction Louise Callow, CPNP, MSN Pediatric Cardiac Surgery University of Michigan Congenital Heart Center I have no disclosures
What We Know, Why We Care, How We Learn • What: – 1 in 5000 live births – Goals S 1 P consistent • Why: – Resource utilization – Morbidity significant, mortality high – Belief that MBTS and associated low DBP created tenuous hemodynamics • How: – Single Ventricle Reconstruction Trial (SVR Trial) – The Tale of Two Shunts www. wikipedia. org Rosenthal D. Single Ventricle Reconstruction Trial. A work in Progress. Circulation, 2014; 129: 200 -2001.
SVR Trial: Searching for Answers • NHLBI in association with PHN • 15 clinical centers from May 2005 to July 2008 • 549 neonates randomized to RVPAS (N=274) or MBTS (275) • Primary outcome transplant free survival at 12 months Ohye RG et al. Cause, timing, and location of death in the Single Ventricle Reconstruction Trial. J Thorac Cardiovasc Surg 2012; 1 -8.
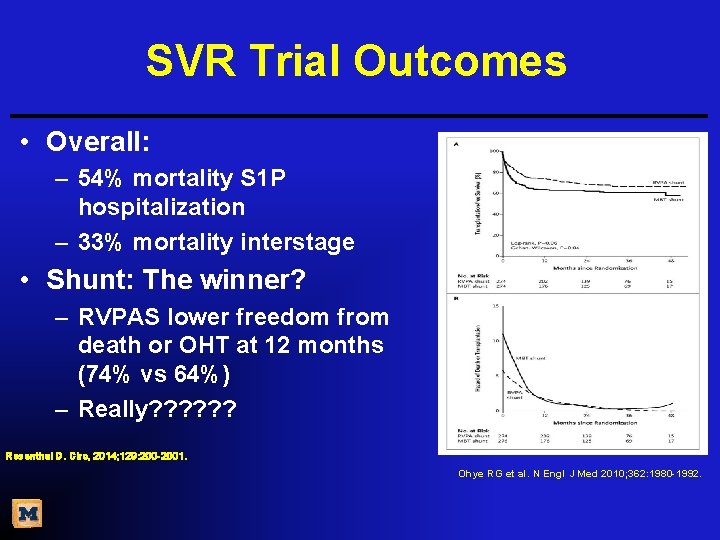
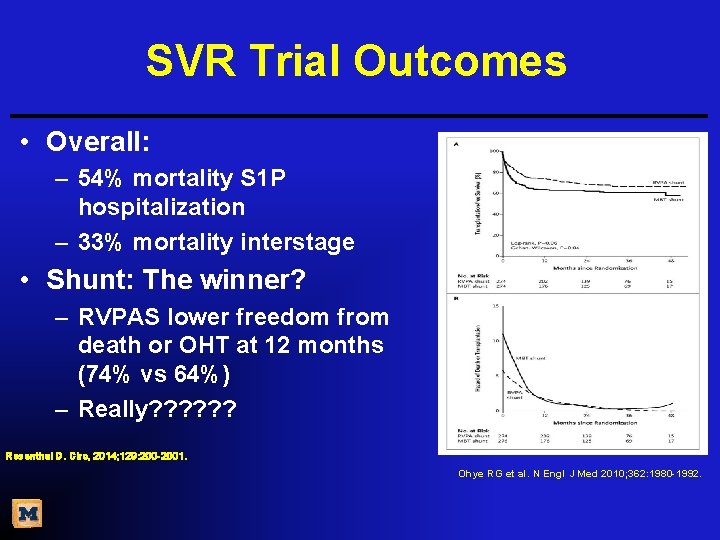
SVR Trial Outcomes • Overall: – 54% mortality S 1 P hospitalization – 33% mortality interstage • Shunt: The winner? – RVPAS lower freedom from death or OHT at 12 months (74% vs 64%) – Really? ? ? Rosenthal D. Circ, 2014; 129: 200 -2001. Ohye RG et al. N Engl J Med 2010; 362: 1980 -1992.
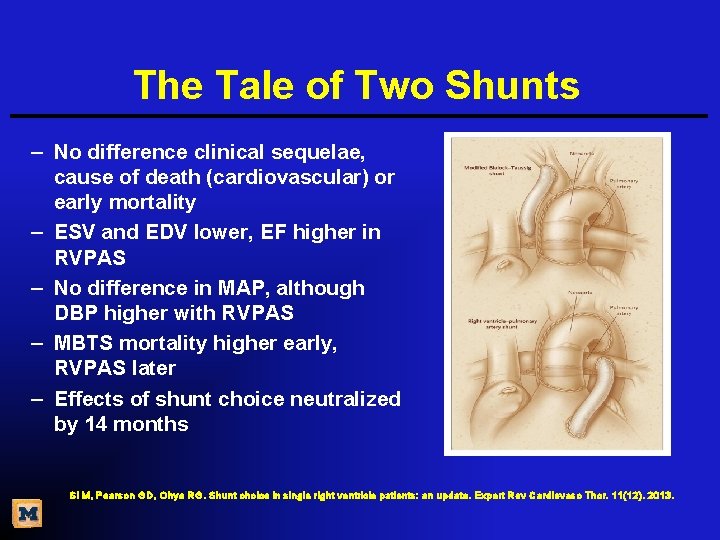
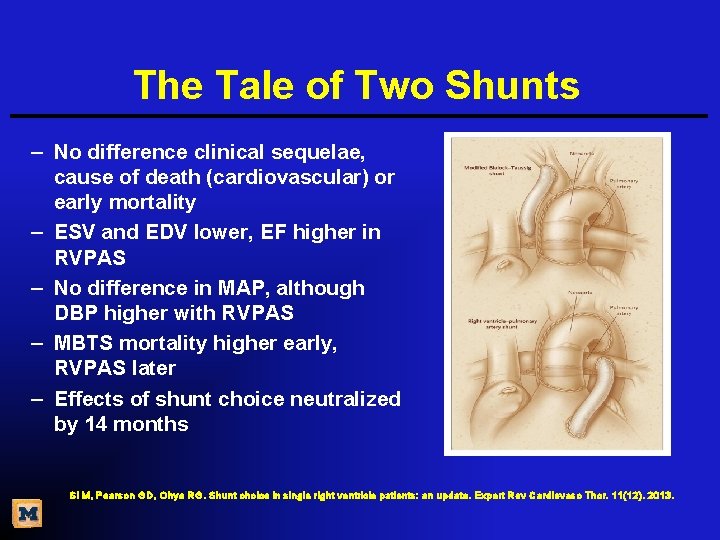
The Tale of Two Shunts – No difference clinical sequelae, cause of death (cardiovascular) or early mortality – ESV and EDV lower, EF higher in RVPAS – No difference in MAP, although DBP higher with RVPAS – MBTS mortality higher early, RVPAS later – Effects of shunt choice neutralized by 14 months Si M, Pearson GD, Ohye RG. Shunt choice in single right ventricle patients: an update. Expert Rev Cardiovasc Thor. 11(12). 2013.
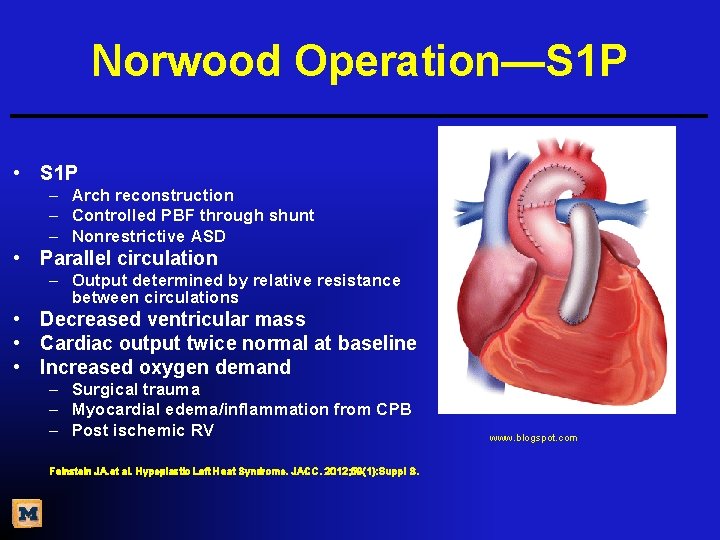
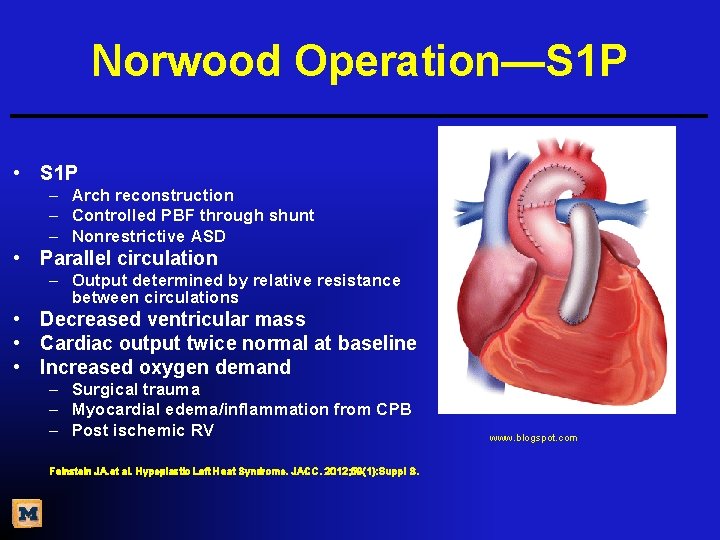
Norwood Operation—S 1 P • S 1 P – Arch reconstruction – Controlled PBF through shunt – Nonrestrictive ASD • Parallel circulation – Output determined by relative resistance between circulations • Decreased ventricular mass • Cardiac output twice normal at baseline • Increased oxygen demand – Surgical trauma – Myocardial edema/inflammation from CPB – Post ischemic RV Feinstein JA. et al. Hypoplastic Left Heat Syndrome. JACC. 2012; 59(1): Suppl S. www. blogspot. com
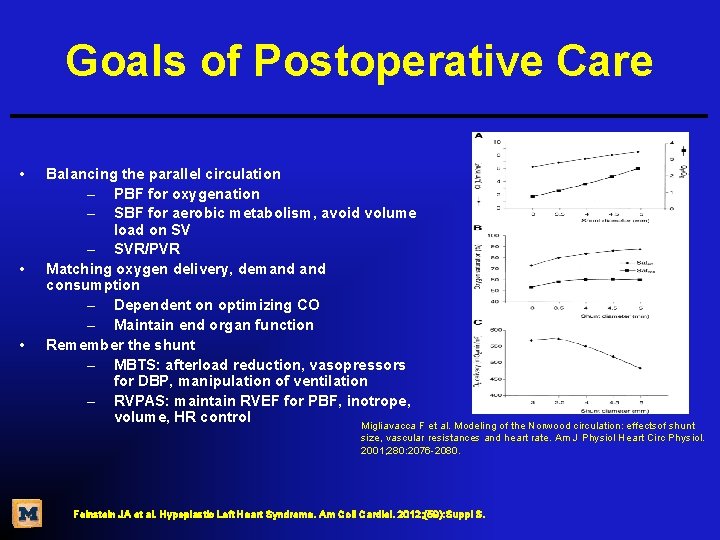
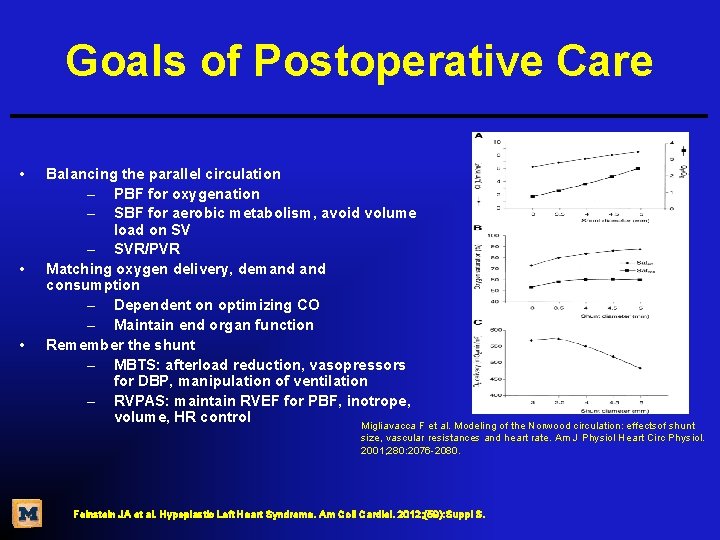
Goals of Postoperative Care • • • Balancing the parallel circulation – PBF for oxygenation – SBF for aerobic metabolism, avoid volume load on SV – SVR/PVR Matching oxygen delivery, demand consumption – Dependent on optimizing CO – Maintain end organ function Remember the shunt – MBTS: afterload reduction, vasopressors for DBP, manipulation of ventilation – RVPAS: maintain RVEF for PBF, inotrope, volume, HR control Migliavacca F et al. Modeling of the Norwood circulation: effectsof shunt size, vascular resistances and heart rate. Am J Physiol Heart Circ Physiol. 2001; 280: 2076 -2080. Feinstein JA et al. Hypoplastic Left Heart Syndrome. Am Coll Cardiol. 2012; (59): Suppl S.
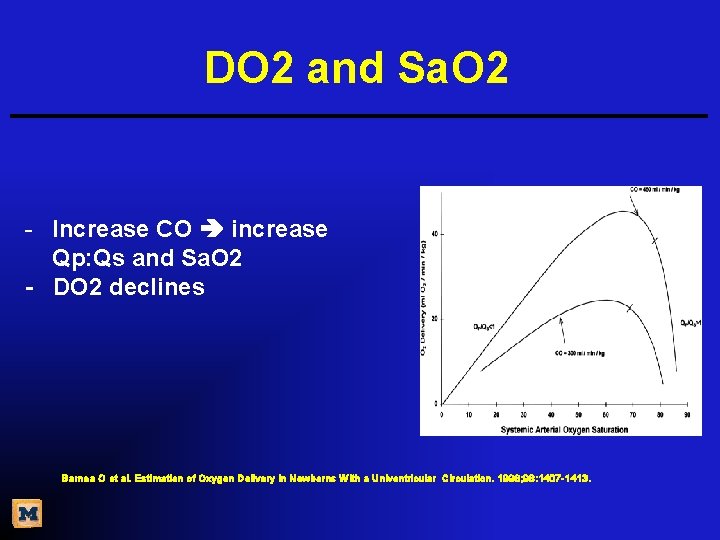
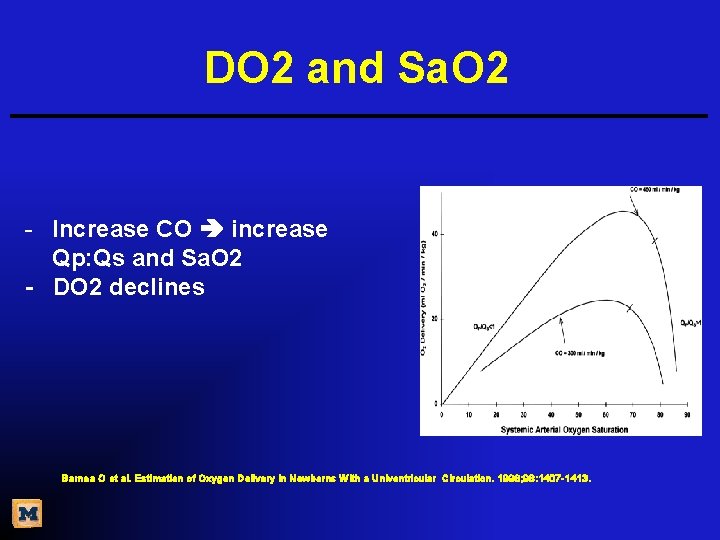
DO 2 and Sa. O 2 - Increase CO increase Qp: Qs and Sa. O 2 - DO 2 declines Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
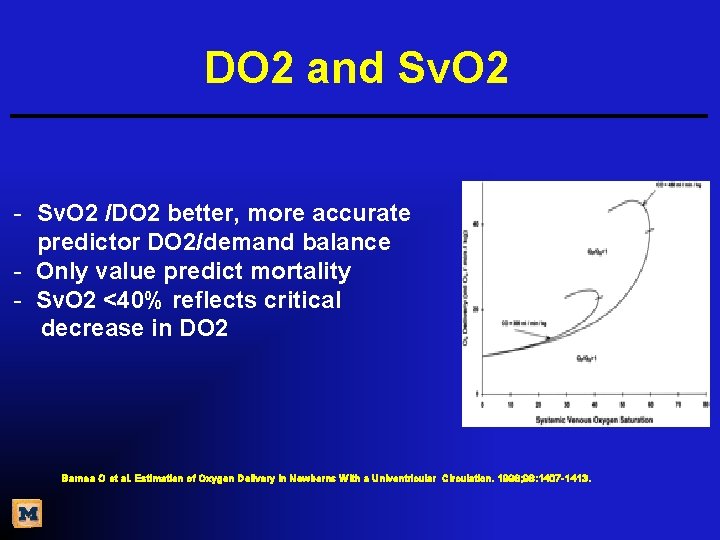
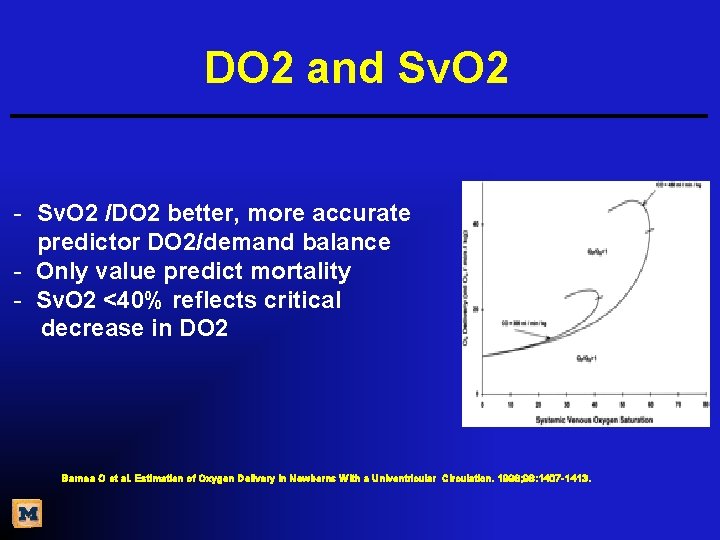
DO 2 and Sv. O 2 - Sv. O 2 /DO 2 better, more accurate predictor DO 2/demand balance - Only value predict mortality - Sv. O 2 <40% reflects critical decrease in DO 2 Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
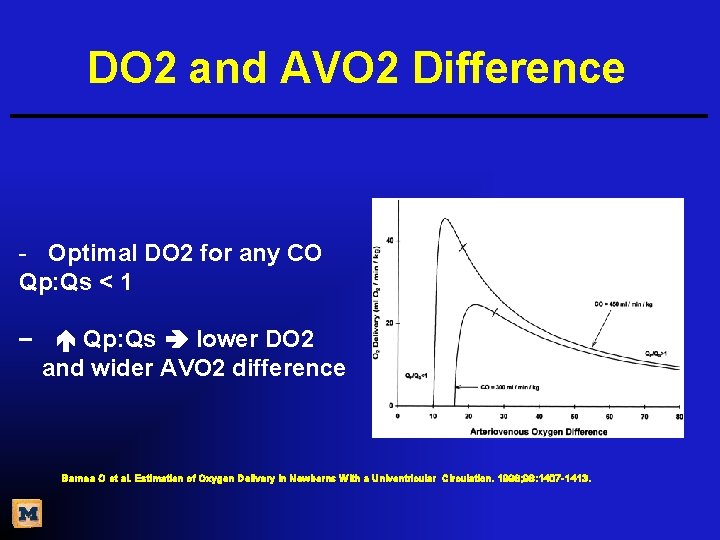
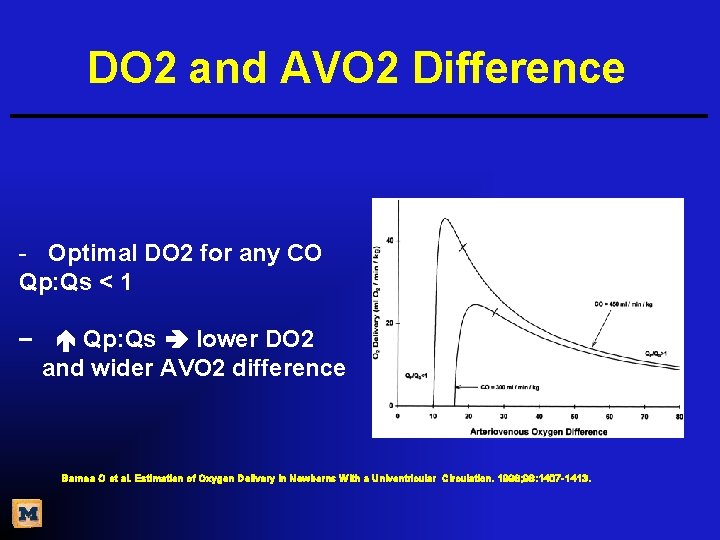
DO 2 and AVO 2 Difference - Optimal DO 2 for any CO Qp: Qs < 1 − Qp: Qs lower DO 2 and wider AVO 2 difference Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
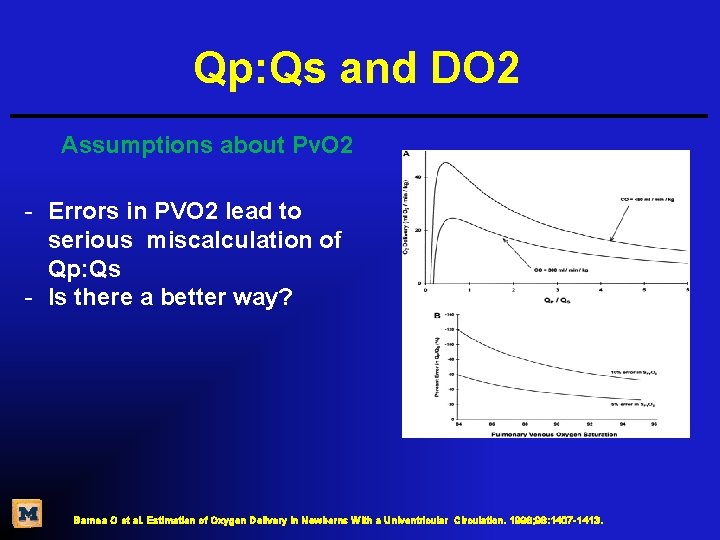
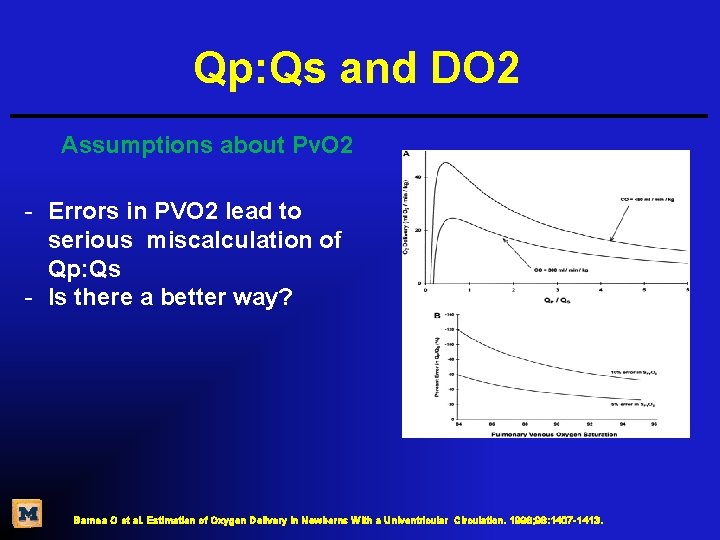
Qp: Qs and DO 2 Assumptions about Pv. O 2 - Errors in PVO 2 lead to serious miscalculation of Qp: Qs - Is there a better way? Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
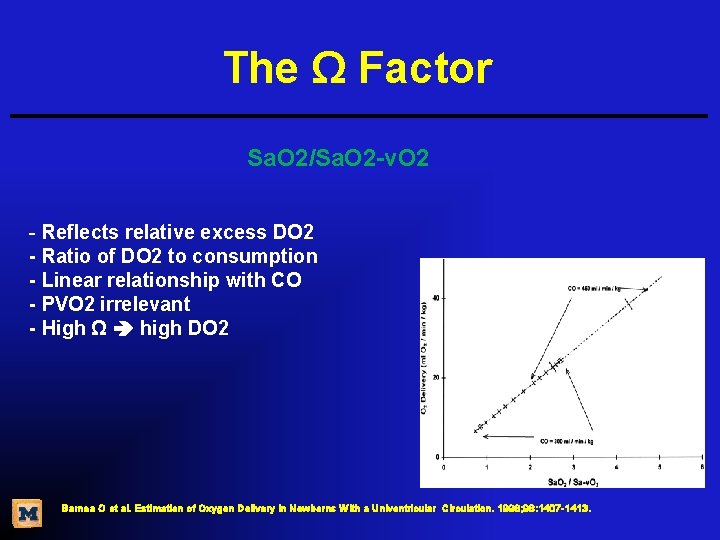
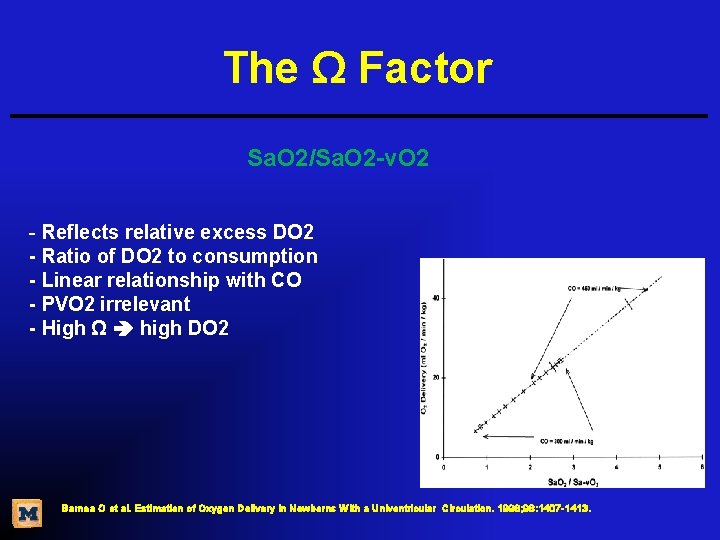
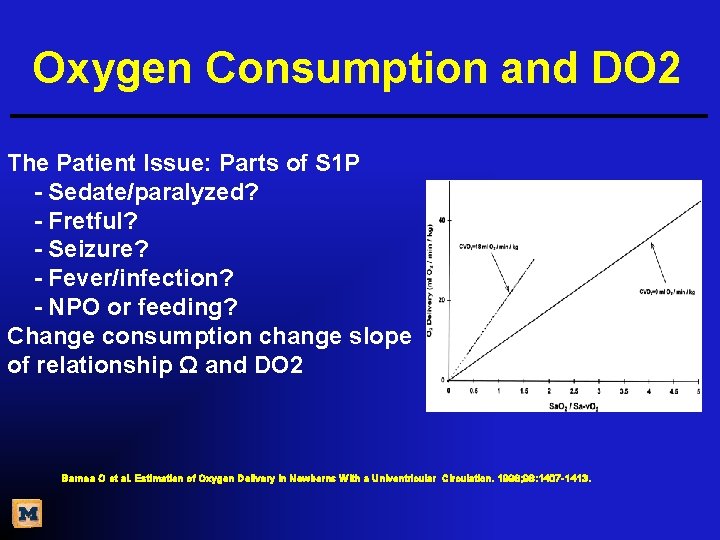
The Ω Factor Sa. O 2/Sa. O 2 -v. O 2 - Reflects relative excess DO 2 - Ratio of DO 2 to consumption - Linear relationship with CO - PVO 2 irrelevant - High Ω high DO 2 Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
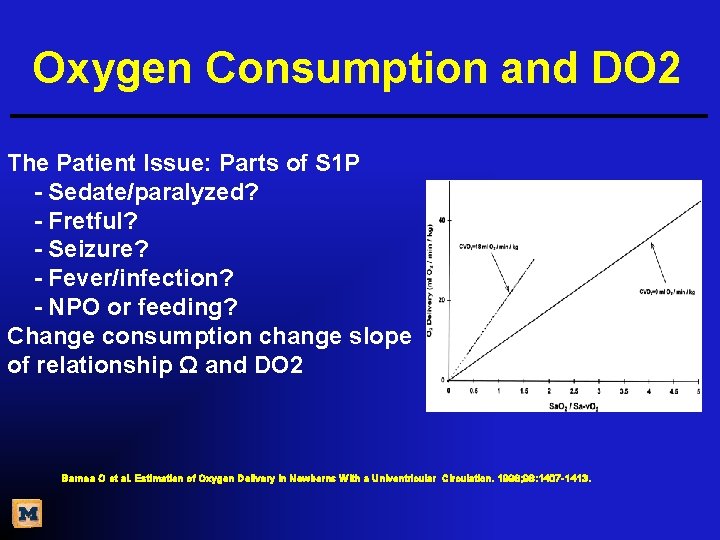
Oxygen Consumption and DO 2 The Patient Issue: Parts of S 1 P - Sedate/paralyzed? - Fretful? - Seizure? - Fever/infection? - NPO or feeding? Change consumption change slope of relationship Ω and DO 2 Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
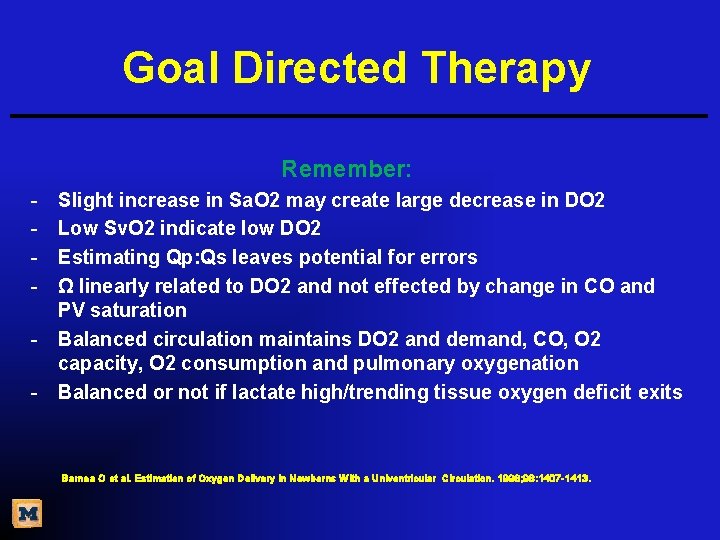
Goal Directed Therapy Remember: - Slight increase in Sa. O 2 may create large decrease in DO 2 Low Sv. O 2 indicate low DO 2 Estimating Qp: Qs leaves potential for errors Ω linearly related to DO 2 and not effected by change in CO and PV saturation Balanced circulation maintains DO 2 and demand, CO, O 2 capacity, O 2 consumption and pulmonary oxygenation Balanced or not if lactate high/trending tissue oxygen deficit exits Barnea O et al. Estimation of Oxygen Delivery in Newborns With a Univentricular Circulation. 1998; 98: 1407 -1413.
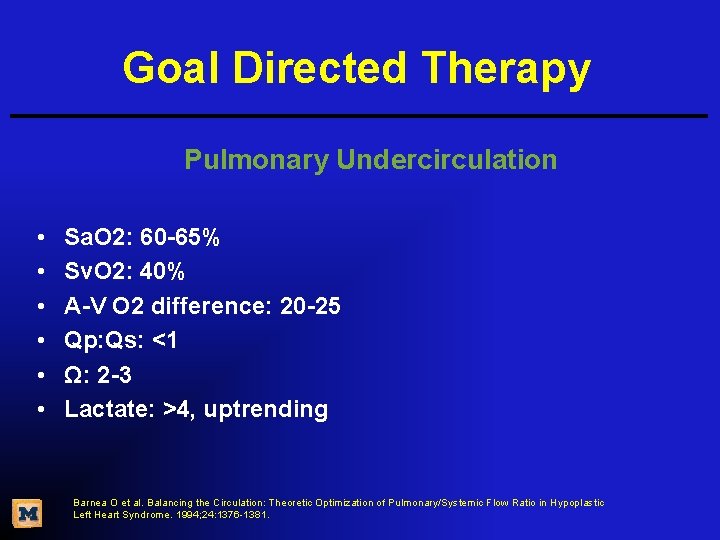
Goal Directed Therapy Pulmonary Undercirculation • • • Sa. O 2: 60 -65% Sv. O 2: 40% A-V O 2 difference: 20 -25 Qp: Qs: <1 Ω: 2 -3 Lactate: >4, uptrending Barnea O et al. Balancing the Circulation: Theoretic Optimization of Pulmonary/Systemic Flow Ratio in Hypoplastic Left Heart Syndrome. 1994; 24: 1376 -1381.
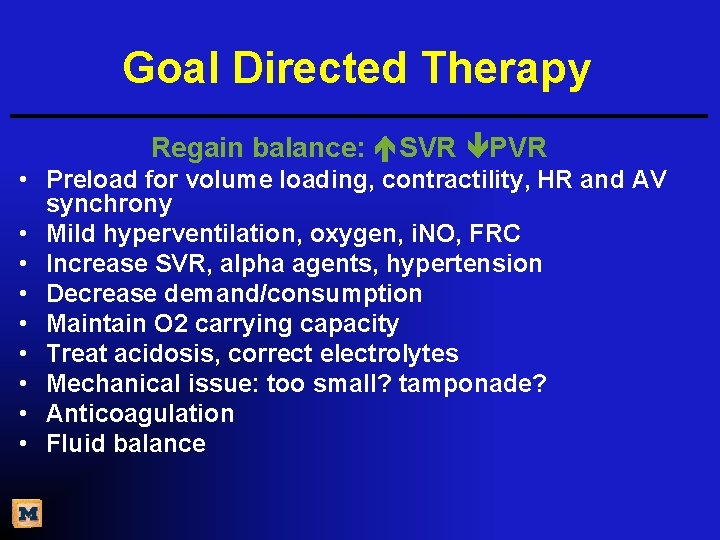
Goal Directed Therapy Regain balance: SVR PVR • Preload for volume loading, contractility, HR and AV synchrony • Mild hyperventilation, oxygen, i. NO, FRC • Increase SVR, alpha agents, hypertension • Decrease demand/consumption • Maintain O 2 carrying capacity • Treat acidosis, correct electrolytes • Mechanical issue: too small? tamponade? • Anticoagulation • Fluid balance
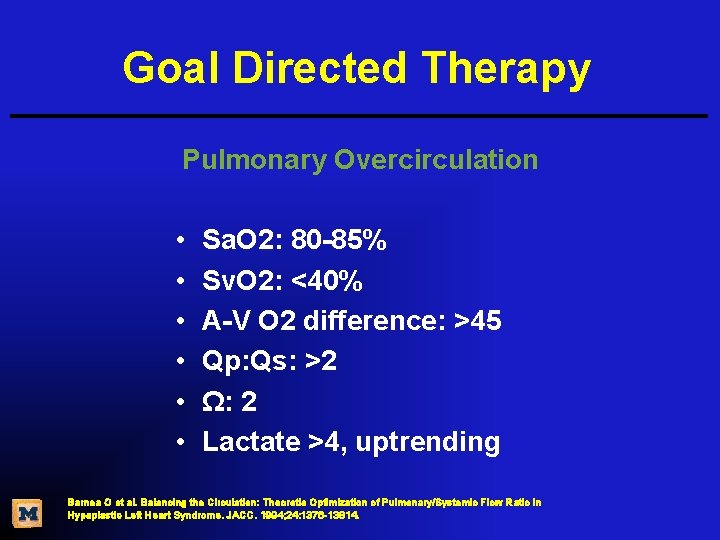
Goal Directed Therapy Pulmonary Overcirculation • • • Sa. O 2: 80 -85% Sv. O 2: <40% A-V O 2 difference: >45 Qp: Qs: >2 Ω: 2 Lactate >4, uptrending Barnea O et al. Balancing the Circulation: Theoretic Optimization of Pulmonary/Systemic Flow Ratio in Hypoplastic Left Heart Syndrome. JACC. 1994; 24: 1376 -13814.
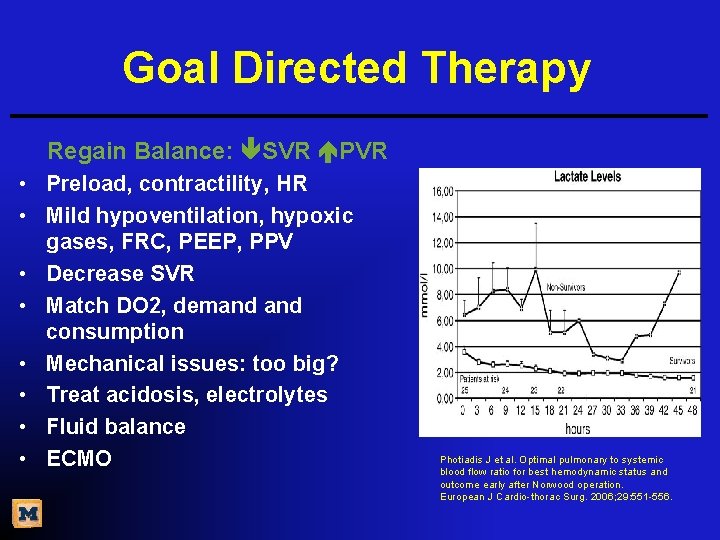
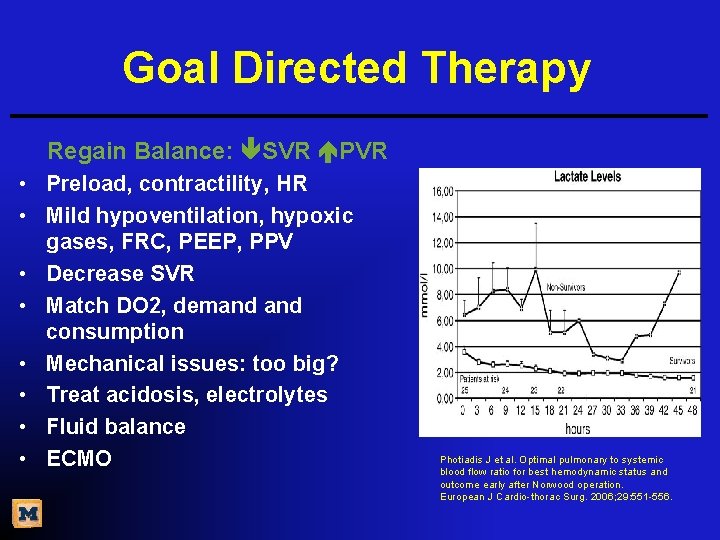
Goal Directed Therapy Regain Balance: SVR PVR • Preload, contractility, HR • Mild hypoventilation, hypoxic gases, FRC, PEEP, PPV • Decrease SVR • Match DO 2, demand consumption • Mechanical issues: too big? • Treat acidosis, electrolytes • Fluid balance • ECMO Photiadis J et al. Optimal pulmonary to systemic blood flow ratio for best hemodynamic status and outcome early after Norwood operation. European J Cardio-thorac Surg. 2006; 29: 551 -556.
S 1 P • It’s hard work • Lots of unknowns • Need for improvement in all areas • Quest for knowledge never ending • Nursing SVR trial? ? ? ? www. 123 rf. com