Single donor vs pooled random donor platelet concentrates


- Slides: 35
Single donor vs pooled random donor platelet concentrates: A review of literature S. H. Arif Rehman S, Ahmad SS, Khan AI, Nasreen T. Department of Pathology, JN Medical College, AMU, Aligarh, India
Objective To understand the advantages of BCPP its comparison with SDP and RDP
Platelet products available RDP – Random donor platelet – Separated by single unit of WB after 6 – 8 hrs collection BCPP – Buffy coat pooled platelet – prepared after pooling 5 – 6 units of buffy coat SDP – Single donor platelet – collected from single donor by apharesis
Random donor platelet (RDP) When platelet is separated from single WB unit Contain around 4 – 5 x 1010/L Platelet Sufficient to raise the platelet count by 5000 in 70 kg adult. Therefore in case of thrombocytopenia when platelet count is up to 10000/μl or below 5 6 units of PC require to raise the count by 30 to 40, 000
Apharesis unit (SDP) Apheresis is a Greek word which means to separate or remove. In plateletpheresis, blood is withdrawn from a donor in anticoagulant solution and separated into components. Platelets are retained and the remaining components are returned to the individual.
Plateletpheresis product (SDP) an average of the equivalent of 6 -10 units (3 -5 x 1011 platelets) of RDP. An increment 30, 000 to 40, 000 / unit jumbo pack is expected from SDP same as from 5 – 6 units of RDP Problems with RDP – multi donor exposure and alloimmunization
Buffy coat pooled platelet (BCPP) Certain studies suggest that buffy coat pooled platelet (BCPP) showed a similar result of platelet increment as with SDP after 1 hour and 24 hrs in Dengue patients with thrombocytopenia. (Chatterji et al, 2014) Singh et al (2009) reported that quality of SDP is definitely superior than RDP, but when BCPP is compared with SDP it gives almost similar results in term of platelet increment
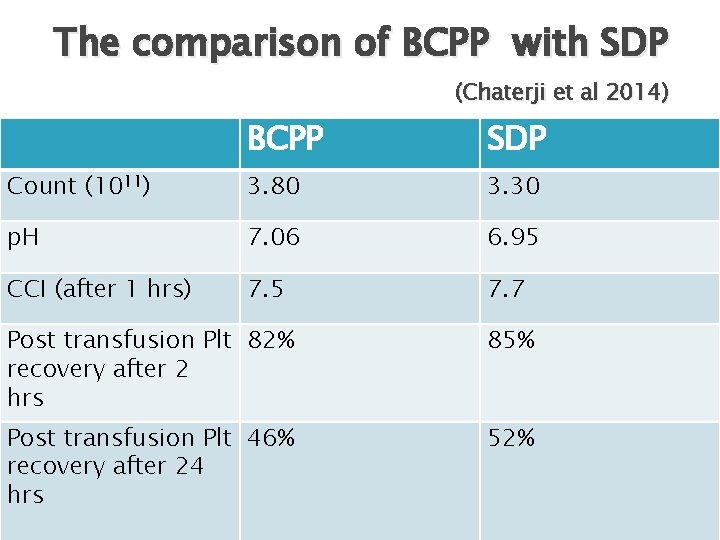
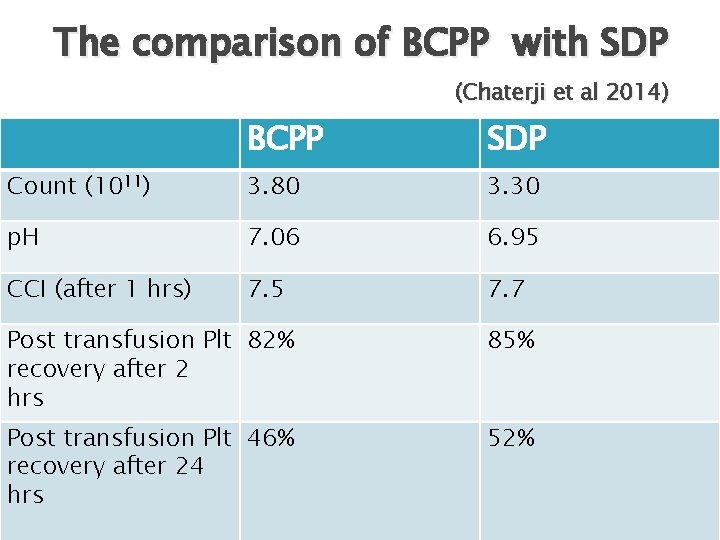
The comparison of BCPP with SDP (Chaterji et al 2014) BCPP SDP Count (1011) 3. 80 3. 30 p. H 7. 06 6. 95 CCI (after 1 hrs) 7. 5 7. 7 Post transfusion Plt 82% recovery after 2 hrs 85% Post transfusion Plt 46% recovery after 24 hrs 52%
• • So BCPP may be used as replacement of SDP in developing countries due to – Higher cost Trained personal Specialized costly machines Separate licensing is required for platelet aphaeresis. But issue of multi donor exposure and more chances of alloimmunization can not be avoided

Indications of platelet transfussion To treat haemorrhage secondary to thrombocytopenia: • • • Dengue These are important indications in developing countries and other endemic areas Malaria ITP In emergency with severe bleeding only TTP Although different opinions are available in literatures about these indications, but DIC with personal experience use of FFP and Septicaemia PC, dramatic responses are noted in these patients
Prophylaxis from haemorrhage in patients with bone marrow suppression with oncologic diseases. § Prophylaxis with platelet count < 10, 000 cells/mm 3 §
BCPP, RDP vs SDP There is lot of literatures available for the discussion of which product is better Many transfusion medicine services favour the primary use of BCPP whereas others favour SDP due to one or the other reasons. But main consideration of debate is these 5 areas –
1. Infectious complications. 2. Transfusion reaction rate. 3. Leukodepletion. 4. Reduction of transfusion frequency. 5. Alloimmunization associated with their use and prevention.
Infectious complications As the platelet are stored at RT, the chances of bacterial contamination or septic platelet transfusion reaction (SPTR) are more common as compared to the other components. Due to multiple donors with RDP and BCPP the chances of bacterial contamination is more as compared to SDP.
Which is attributed to contamination of the platelet product from donor skin flora or inadvertent selection of donors with asymptomatic bacteraemia. SDP has advantage over RDP in this aspect
Transfusion Reaction rate For transfusion reaction in recipients: § Febrile non hemolytic transfusion reactions (FNHTR): m/c type associated with platelet products. § Cause: contaminating WBCs or by cytokines in the plasma produced by the WBCs during storage. Allergic reaction, anaphylactic reactions: A/b to donor plasma proteins.
§ § § Hypocalcaemia: large volume of platelets transfused rapidly especially in liver disease. Transfusion associated acute lung injury (TRALI): Antibodies against Neutrophils. Alloimmunization to HLA antigen: due to Immune response to foreign Ags on platelets (HLA). Most commonly seen in multiple transfusions

Ø SDP contains no plasma proteins, reduced or no WBCs and WBC antibodies. Hence, reduction of FNHTR, allergic reaction, anaphylaxis & TRALI. Alloimmunization will also be reduced. Ø However, SDP. Hypocalcemia is more common with Ø FNHTR in PCs can be reduced by leukodepletion. Ø Allergic reactions and anaphylaxis can be reduced to some extend by washing the platelets.
Overall, SDP has advantage of reducing the transfusion reaction, over RDP. But, RDP are easy to be made, less expensive and some of the transfusion reactions can be controlled by leukodepletion and washing. Transfusion reactions related to plasma, Ab and leukocytes may also be minimize in BCPP also as in BCPP there are less plasma protein and further it is leukodepleted also.
Donors reaction More with Apharesis because – Ø Longer time taken as compared to whole blood donation Ø Citrate toxicity as there is circulation of citrated blood in the body during the process Ø • Citrates chelates Ca 2+ leading to reduced free or ionised calcium (Free Ca 2+ involved in coagulation & cellular calcium channels)
Vasovagal complications are more common with WB donation while citrate toxicity is commonly noted with apharesis donation Ø Hypovolemia and Vascular access related adverse effects are similar in both type of donation Ø However giving calcium supplement, hot beverage during process and engaging the donor towards other activity such as TV and music reduces these type of complication in apharesis donors Ø
Leukodepletion Leukoreduced blood components have proven benefit for: Prevention of FNHTR Reduction of infectious risks from cellassociated viruses such as CMV. Reduction of alloimmunization in transfusion recipients. Reduction in TRALI.
Current apheresis equipment can provide leukoreduced products at the time of collection. Hence, SDP having advantage over PCs in this aspect also.
Reduction of transfusion frequency with SDP The kinetics of transfused platelets have been carefully studied by Hanson and Slichter. There is direct relation between platelet dose and its effect on post-transfusion platelet count. higher post-transfusion platelet counts would result in a longer period of time for the platelet count to return to baseline. Hence, larger doses of platelets would reduce the required transfusion frequency.
This practice has important implications for patient care: Many patients with hematologic or oncologic diseases will move to outpatient therapies. Prolonged transfusion-free intervals can substantially improve the quality of life. Bleeding is controlled rapidly especially in ITP and more time is available for recovery of the patient, before a 2 nd transfusion is needed.
Alloimmunization Platelet alloimmunization remains the most important long-term complication of platelet transfusion therapy Refractoriness is most commonly associated with antibodies against alloantigen on platelets. These antibodies are produced as an immune response to HLA class I antigens on leukocytes and platelets.
Leukodepletion is a practical method to reduce alloimmunization. Leukodepletion is more easily available in case of SDP. Once a patient becomes alloimmunized, platelet transfusions with SDP that are either HLA-matched or crossmatched are the standard of care.
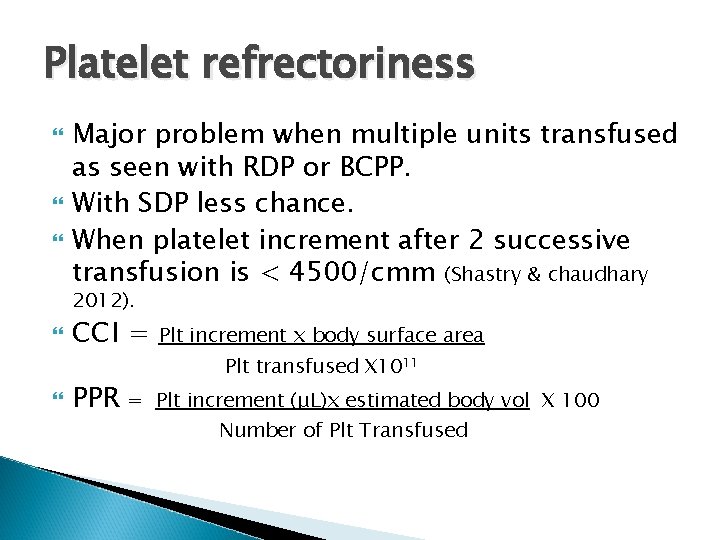
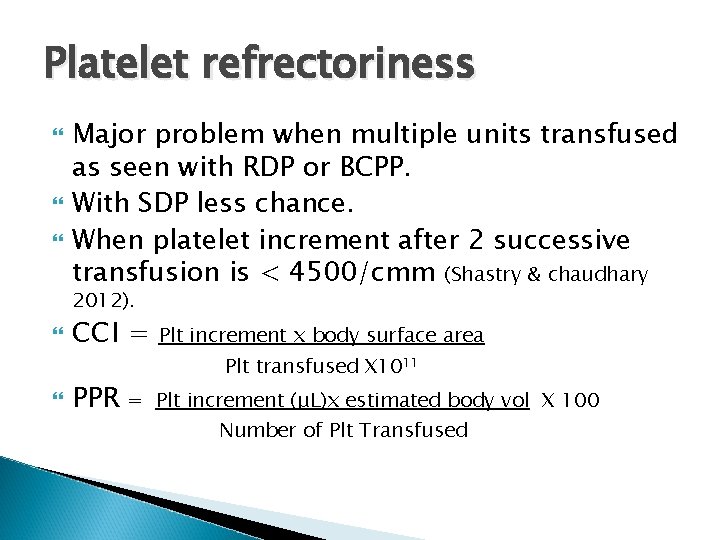
Platelet refrectoriness Major problem when multiple units transfused as seen with RDP or BCPP. With SDP less chance. When platelet increment after 2 successive transfusion is < 4500/cmm (Shastry & chaudhary 2012). CCI = PPR Plt increment x body surface area Plt transfused X 1011 = Plt increment (μL)x estimated body vol X 100 Number of Plt Transfused
BCPP also gives leukoreduced platelets Pietersz et al (1999) reported that with 97. 5% confidence that 100% of the LD-PC contain <5 x 106 leukocytes, and with 95% confidence that more than 99% of the LD-PC contain fewer than 1 x 106 leukocytes Singh et al (2009) and in other studies showed that platelet obtained from buffy coat are better leukocyte reduced than PRP – PC similar to apharesis platelet
Conclusion Single-donor platelets have major advantages over RDP when considering: § Risk of SPTR. § Platelet transfusion management of the alloimmunized or refractory patient. § Ease of leukoreduction. § Ability to reduce transfusion frequency and donor exposure.
RDP advantages over SDP: § Cost effective, especially to the patients of developing and underdeveloped nations. § Easy to prepare, need less trained staff. § SDP has more chances of donor reactions.
Further BCPP can be tried as compared to SDP as many comparative studies concluded that BCPP product can replace SDP due to – cost effectiveness, specialized machine, trained staff and separate licensing process
Take home message Depends upon the situation we can decide the product for platelet considering – Risk benefit ratio, cost effective ratio
References Saran RK. Transfusion Medicine Technical Manual. 2 nd ed. Directorate General of Health Services, Ministry of Health &Family Welfare, Government of India New Delhi 2003 : 229 -43. Rock G. Apheresis : Four Decades of Practice. 2002 ; 83 (Suppl 1): 45 -7. Blajchman MA: Transfusion-associated immunomodulation and universal white cell reduction: are we putting the cart before the horse? Transfusion 1999, 39: 665– 670. Simon TL, Dzik WH, Snyder EL, Christopher PS, Ronald GS, editors. Principles of Transfusion Medicine. 3 ed. Lippincott Williams & Wilkins 2002; 648 -58. Ness PM, Campbell-Lee SA. Single donor versus pooled random donor platelet concentrates. Curr Opin Hematol. 2001 Nov; 8(6): 3926. Hanson SR, Slichter SJ: Platelet kinetics in patients with bone marrow hypoplasia: evidence for a fixed platelet requirement. Blood 1985, 66: 1105– 1109.
Chatterjee K, Coshic P, Borgohain M, Agarwal N. Experience of buffy coat pooling of platelets as a supportive care in thrombocytopenic dengue patients: A prospective study. Asian Journal of Transfusion Science. 2014; 8(2): 89 -91. doi: 10. 4103/0973 -6247. 137439. Singh RP, Marwaha N, Malhotra P, Dash S. Quality assessment of platelet concentrates prepared by platelet rich plasma-platelet concentrate, buffy coat poor-platelet concentrate (BC-PC) and apheresis-PC methods. Asian Journal of Transfusion Science. 2009; 3(2): 86 -94. doi: 10. 4103/0973 -6247. 53882. Crocco I, Franchini M, Garozzo G, et al. Adverse reactions in blood and apheresis donors: experience from two Italian transfusion centres. Blood Transfusion. 2009; 7(1): 35 -38. doi: 10. 2450/2008. 0018 -08. Shastry S, Chaudhary R. Clinical factors influencing corrected count increment. Tr & apharesis Sci. 2012; 47(3), 327– 330