SIGNS 1EXAMINATION OF THE NOSE INSPECTION EPISTAXIS bleeding
SIGNS

(1)EXAMINATION OF THE NOSE INSPECTION Ø EPISTAXIS( bleeding from the nose), Ø CHEEK SWELLING Ø PARAESTHESIA OF THE CHEEK Ø PROPTOSIS OF THE ORBIT Ø RHINORRHOEA( persistent discharge of watery mucus) Ø RHYNOPHYMA( swelling of the nose due to enormous enlargement of the sebaceous gland) Ø ANOSMIA( complete loss of sense of smell) Ø HYPOSMIA( decrease sense of smell) The anterior part of the nose can be examined using a nasal speculum and light source. Endoscopes are required to examine the nasal cavity and postnasal space.
(2) EXAMINATION OF THE CHEST INSPECTION Look for mental alertness, cyanosis, breathlessness at rest, respiratory rate, use of accessory muscles, any deformity or scars on the chest and movement on both sides. A coarse tremor or flap of the outstretched hands indicates CO 2 intoxication. Prominent veins on the chest may imply obstruction of the superior vena cava.
CYANOSIS: is a bluish colour of the skin and mucous membranes, due to the presence of more than 5 g/d. L of desaturated haemoglobin. When due to central causes, cyanosis is visible on the tongue (especially the underside) and lips, and indicates a Pa. O 2 below 6 k. Patients with central cyanosis will also be cyanosed peripherally. Peripheral cyanosis without central cyanosis is caused by a reduced peripheral circulation and is noted on the fingernails and skin of the extremities with associated coolness of the skin.
RESPIRATORY RATE: The normal rate of respiration in a relaxed adult is about 14 -16 breaths per minute. Trachypnoea is an increased respiratory rate observed by the doctor, whilst apnoea means ceasation of respiration. Cheyne-stokes breathing or periodic respiration is the name given to a disturbance of respiratory rhythm, in which there is a cyclical deepening and quickening of respiration followed by diminishing respiratory effort and rate. It occurs with periods of apnoea between episodes of tachypnoea
FINGER CLUBBING: is present when the normal angle between the base of the nail and the nail fold is lost. The base of the nail is fluctuant owing to increased vascularity, and there is an increased curvature of the nail in all directions, with expansion of the end of the digit. of tac Some causes of finger clubbing Respiratory ØBronchial carcinoma, especially epidermoid (squamous cell) type (major cause) ØChronic suppurative lung disease: ØBronchiectasis ØLung abscess ØEmpyema ØPulmonary fibrosis (e. g. cryptogenic fibrosing alveolitis) ØPleural and mediastinal tumours (e. g. mesothelioma) ØCryptogenic organizing pneumonia

PALPATION Check the position of the trachea ( at the suprasternal notch) and apex beat. Examine the supraclavicular fossa for enlarged lymph nodes. The distance between the sternal notch and the cricoid cartilage (three to four finger breadths in full expiration) is reduced in patients with severe airflow limitation. Check chest expansion. Spread your hands around the chest so that the thumbs just meet in the mid-line. Ask the patient to take a deep breath. Your thumbs will be dragged apart to a distance roughly equivalent to half the chest expansion. If expansion is asymmetrical it will be felt and seen. Chest expansion is the difference between the circumference of the chest at full inspiration and after a full expiration, measured at the level of the nipples
PERCUSSION The whole surface of the lungs must be percussed. Place one hand flat on chest, keeping the finger you intend to strike straight and firmly applied to the underlying skin. Tap the centre of the middle phalanx of this finger with the tip of the middle finger of the other hand. Listen carefully to the sound and compare it to the sound produced by percussing the same area on the other side of the chest. The two areas most often forgotten when percussing the chest are the lateral zones high in the axillae, and the anterior aspect of the apices behind the clavicles. Percuss this latter area by striking the clavicle directly with the percussing finger
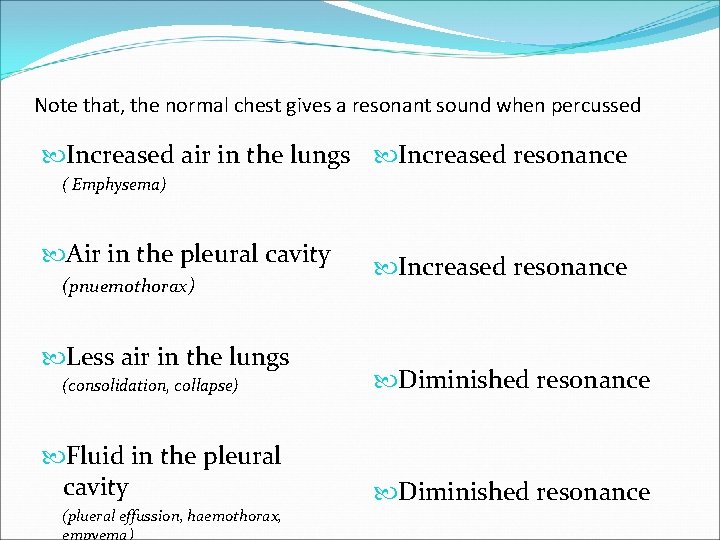
Note that, the normal chest gives a resonant sound when percussed Increased air in the lungs Increased resonance ( Emphysema) Air in the pleural cavity (pnuemothorax) Less air in the lungs (consolidation, collapse) Fluid in the pleural cavity (plueral effussion, haemothorax, empyema) Increased resonance Diminished resonance
AUSCULTATION The patient is asked to take deep breaths through the mouth. Inspiration sounds are more prolonged than expiration. Healthy lungs filter off most of the high-frequency component, which is mainly due to turbulent flow in the larynx. Normal breath sounds are harsher anteriorly over the upper lobes (particularly on the right) and described as vesicular. ØBRONCHIAL BREATHING: is heard best over consolidated or collapsed lung and sometimes over areas of localized fibrosis or bronchiectasis. Such areas conduct the high-frequency hissing component of breath sounds well. Characteristically, the noise heard during inspiration and expiration is equally long but separated by a short silent phase. Whispering pectoriloquy (whispered, higher-pitched, sounds heard distinctly through a stethoscope) invariably accompanies bronchial breathing.
ADDED SOUNDS WHEEZE ( rhonci) Wheeze is usually heard during expiration and results from vibrations in the collapsible part of the airways when apposition occurs as a result of the flowlimiting mechanisms. Wheezes are heard in asthma and in chronic obstructive pulmonary disease, but are not invariably present. In the most severe cases of asthma a wheeze may not be heard, as airflow may be insufficient to generate the sound. Wheezes may be monophonic (single large airway obstruction) or polyphonic (narrowing of many small airways). An end-inspiratory (as opposed to expiratory) 'squeak' may be heard in obliterative bronchiolitis. CRACKLES These brief crackling sounds are probably produced by opening of previously closed bronchioles, and their timing during breathing is of significance - early inspiratory crackles are associated with diffuse airflow limitation, whereas late inspiratory crackles are characteristically heard in pulmonary oedema, fibrosis of the lung and bronchiectasis.
PLEURAL RUB. This is a creaking or groaning sound that is usually well localized. It is indicative of inflammation and roughening of the pleural surfaces, which normally glide silently over one another. VOCAL RESONANCE When listening to the breaths sounds with your stethoscope you will detect vibrations which have been made in the large airways. Vocal resonance is the resonance of sounds in the chest made by the voice. When testing it, you are detecting vibrations transmitted to the chest from the vocal cords as the patient reapeats a phrase, usually the words ¨ninety nine ¨ Healthy lung attenuates high-frequency notes, leaving the booming low-pitched components of speech. Consolidated lung has the reverse effect, transmitting the high frequencies; the spoken word then takes on a bleating quality. Whispered (and therefore high-pitched) speech can barely be heard over healthy lung, whereas consolidation allows its clear transmission.
BIBLIOGRAPHY �KUMAR AND CLARK CLINICAL MEDICINE 6 E �DAVIDSON´S INTERNAL MEDICINE 19 TH EDITION �HARRISSON´S PRINCIPLES OF INTERNAL MEDICINE 17 TH EDITION �WIKIPEDIA �WWW. EMEDICINE. COM
ØTHANK YOU!! ØGRACIAS!! ØMERCI!! ØJEREH NGEN JEF!! ØALA BARAKA!! ØJARAMA!!
- Slides: 14