SHYMA P V 11 DO 93 CONTENTS Introduction







- Slides: 49
SHYMA. P. V 11 DO 93
CONTENTS Introduction Definition Classification Pathogenesis Histopathology Clinical features Periodontal pocket examination Treatment plan
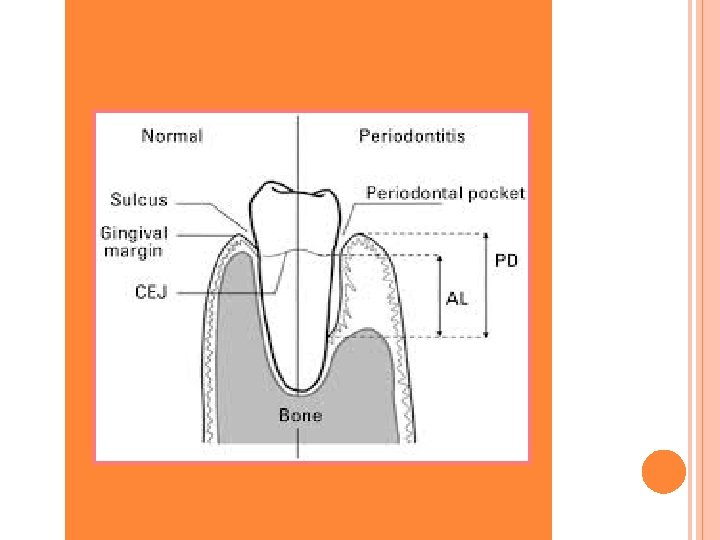
INTRODUCTION Periodontal pocket is one of the most important clinical feature of periodontal disease It may occur by coronal movement of gingival margin, apical displacement of the gingival attachment or a combination of above two process
DEFINITION PERIODONTAL POCKET is defined as the pathological deepening gingival sulcus.
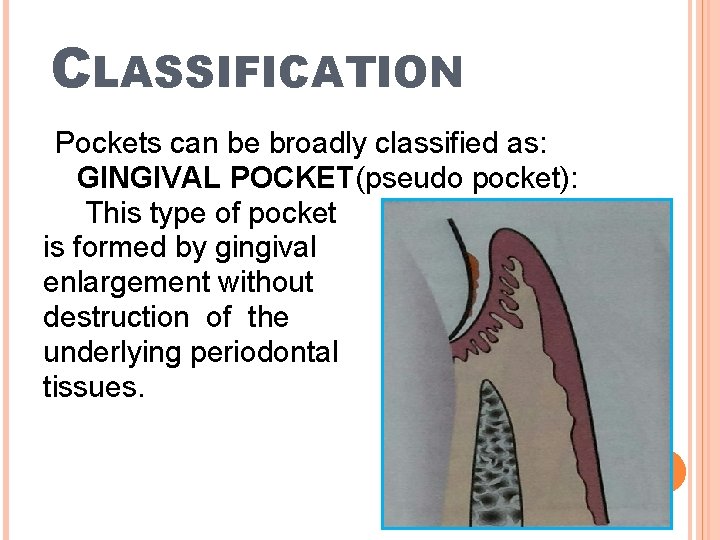
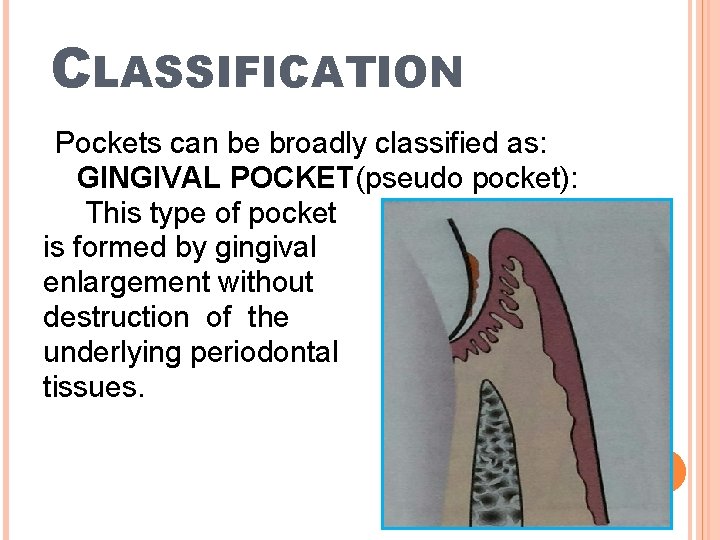
CLASSIFICATION Pockets can be broadly classified as: GINGIVAL POCKET(pseudo pocket): This type of pocket is formed by gingival enlargement without destruction of the underlying periodontal tissues.
PERIODONTAL POCKET: This type of pocket occurs with the destruction of the supporting periodontal structure. Progressive pocket deepening leads to destruction of supporting periodontal tissues and loosening & exfoliation of the teeth.
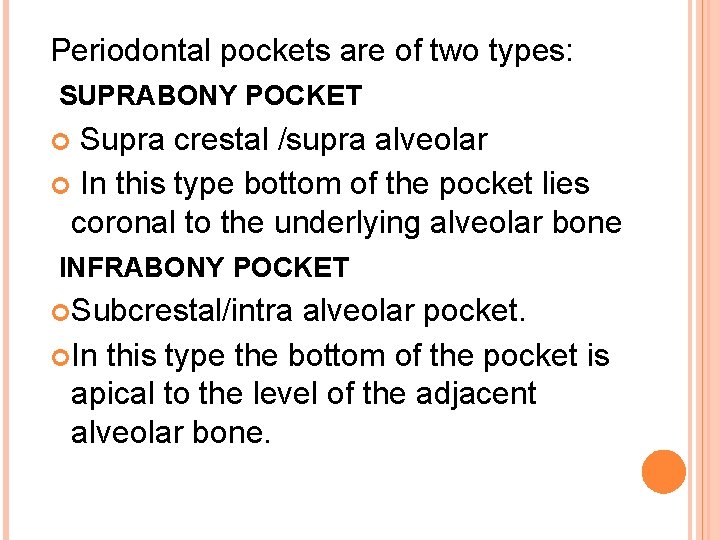
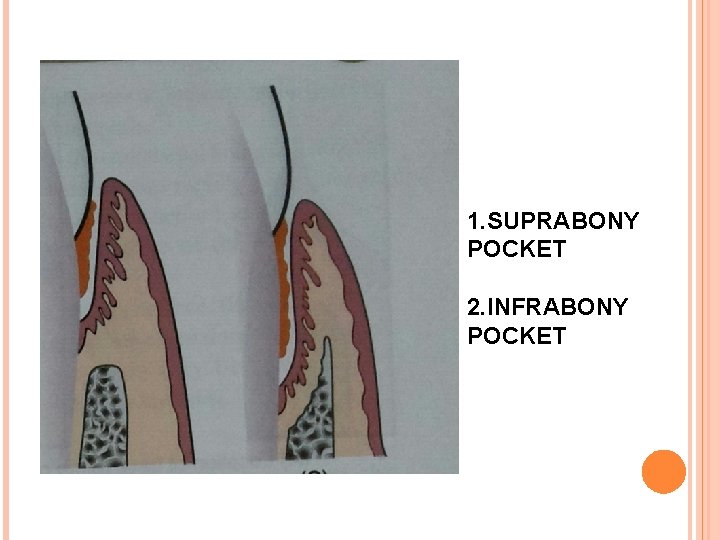
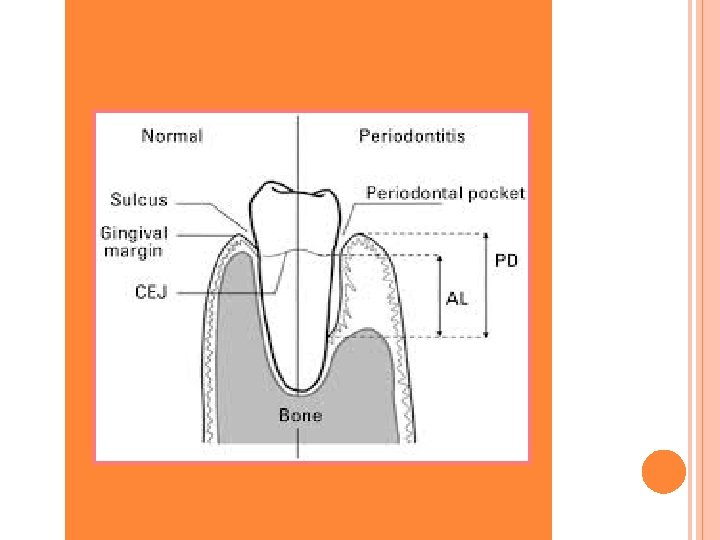
Periodontal pockets are of two types: SUPRABONY POCKET Supra crestal /supra alveolar In this type bottom of the pocket lies coronal to the underlying alveolar bone INFRABONY POCKET Subcrestal/intra alveolar pocket. In this type the bottom of the pocket is apical to the level of the adjacent alveolar bone.
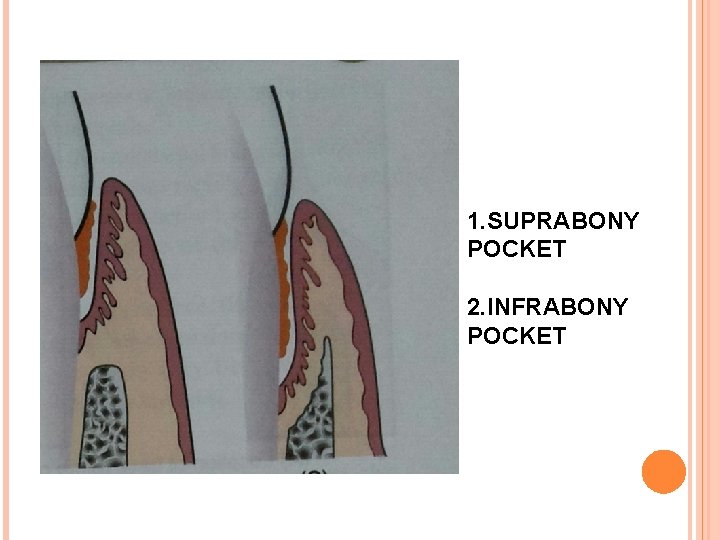
1. SUPRABONY POCKET 2. INFRABONY POCKET
CLASSIFICATION OF POCKET ACCORDING TO THE INVOLVED TOOTH SURFACE: Simple pocket. Compound pocket. Complex pocket.

A)SIMPLE B)COMPOUND C)COMPLEX POCKET.
DEPENDING ON THE NATURE OF THE SOFT TISSUE WALL OF THE POCKET: EDEMATOUS POCKET: Inflammatory fluid and cellular exudate predominates , pocket wall is bluishred , soft , spongy and friable , with a smooth shiny surface. FIBROTIC POCKET: Relative predominance of newly formed connective tissue cells and fibers. Pocket wall is more firm and pink.
CLINICAL FEATURES Clinical signs , suggestive of the presence of periodontal pocket are; Bluish-red thickened marginal gingiva. A bluish- red vertical zone, from the gingival margin to alveolar bone Gingival bleeding , suppuration or both. Tooth mobility , extrusion. Diastema formation. Rolled edge separating the gingival margin from the tooth surface. Enlarged edematous gingiva.


Periodontal Pocket is generally painless, but may give raise to symptoms such as; localized /radiating pain/ sensation of pressure after eating , which gradually diminishes Foul taste in localized area. Sensitivity to hot and cold. Toothache in the absence of caries
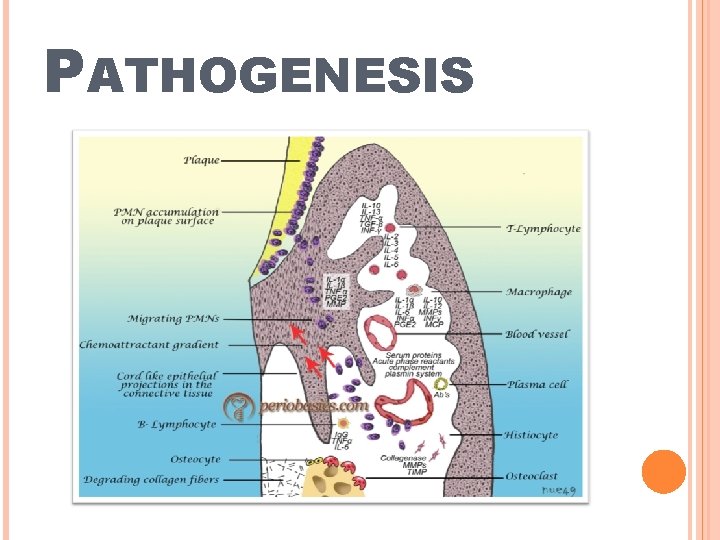
PATHOGENESIS
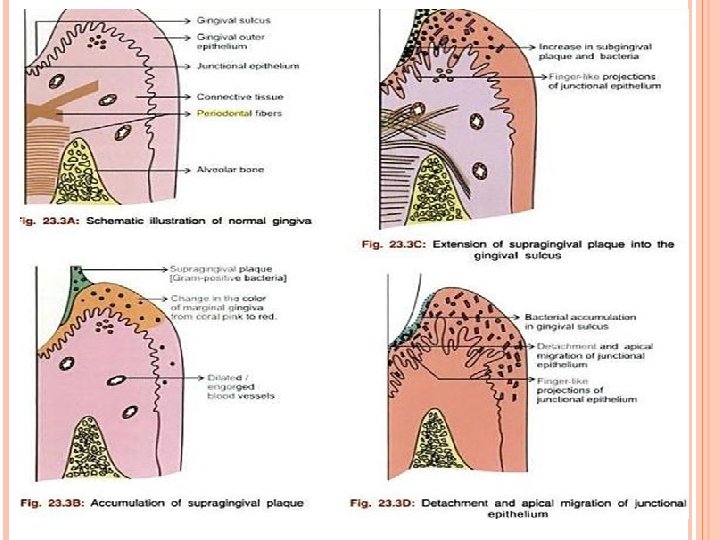
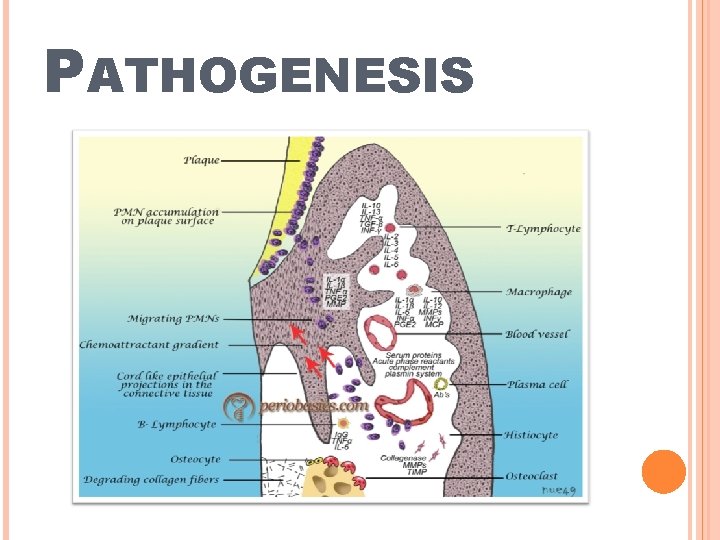
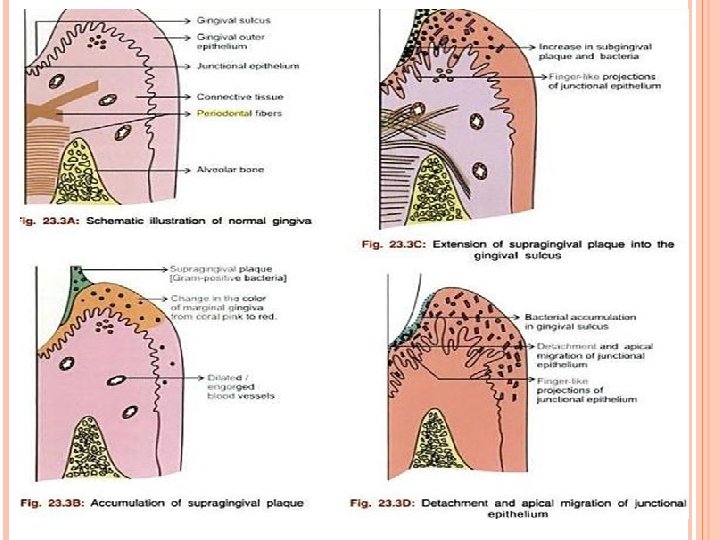
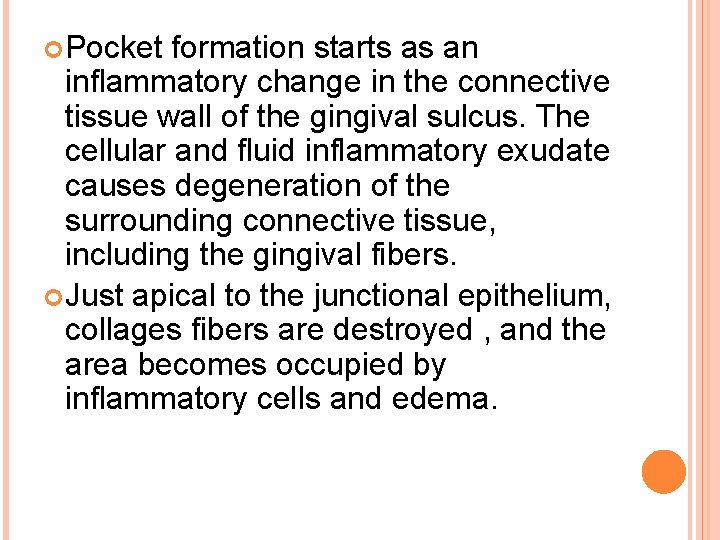
Pocket formation starts as an inflammatory change in the connective tissue wall of the gingival sulcus. The cellular and fluid inflammatory exudate causes degeneration of the surrounding connective tissue, including the gingival fibers. Just apical to the junctional epithelium, collages fibers are destroyed , and the area becomes occupied by inflammatory cells and edema.
MECHANISM OF COLLAGEN LOSS There are two mechanisms involved: FIRST MECHANISM: Collagenases and other enzymes secreted by fibroblasts, polymorphonuclear leukocytes , and macrophages. These enzymes degrade the collagen and other matrix macromolecules into small peptides which are called as matrix metalloprotinases.
SECOND MECHANISM : Fibroblasts phagocytize collagen fibers by extending cytoplasmic processes to the ligament -cementum interface and degrade the inserted collagen fibrils and the fibrils of the cementum matrix.
As a consequence of the loss of collagen , the apical cells of the junctional epithelium proliferate along the root, extending fingerlike projections two or three cells in thickness. The coronal portion of the junctional epithelium detaches from the root as the apical portion migrates. As result of inflammation , PMNs invade the coronal end of the junctional epithelium in increasing numbers.
When the relative volume of PMNs reaches approximately 60% / more of the junctional epithelium , the tissue looses cohesiveness and detaches from the tooth surface. The degree of leukocytes infiltration of the junctional epithelium is independent of the volume of inflamed connective tissue. Thus a periodontal pocket is established
HISTOPATHOLOGY SOFT TISSUE WALL: Ø Connective tissue: Edematous , densely infiltrated with plasma cells, lymphocytes &PMNs. Blood vessels are increased in number , dilated & engorged, particularly in the sub epithelial connective tissue layer. varying degree of degeneration , single or multiple necrotic foci. also shows the proliferation of endothelial cells , newly formed capillaries , fibroblast & collagen fibers.
Ø Junctional Epithelium: At the base of the pocket junctional epithelium is much shorter than that of a normal sulcus , may show degeneration. Ø Lateral Wall of the Periodontal Pocket: It is the place where most severe degeneration change takes place. Epithelium shows both proliferation & degenerative changes.

Epithelial buds /interlacing cords of epithelial cells project from the lateral wall into the adjacent inflamed connective tissue. These epithelial projections are densely infiltrated with leukocytes & other inflammatory cells Progressive degeneration & necrosis of epithelium leading to ulceration of the lateral wall & exposure of underlying connective tissue
BACTERIAL INVASION Bacterial invasion along the lateral and apical areas of the pocket Some bacteria transverse the basal lamina and invade the subepithelial connective tissue Bacteria found in intercellular spaces of the epithelium , -Filamentous rods & coccoid organisms with the predominant Gram negative cell walls.
MICRO TOPOGRAPHY OF GINGIVAL WALL OF THE POCKET: Under scanning electron microscope following areas have been noted : 1. Areas of relative Quiescence Flat surface, minor depression & occational shedding of cells. 2. Areas of Bacterial Accumulation: Bacteria are mainly cocci , rods , filaments and few spirochetes. 3. Areas of Emergence of Leukocyte: Leukocyte appear in the pocket wall through holes located in the intercellular spaces.
4. Areas of leukocyte -Bacteria Interaction phagocytosis. 5. Areas of Intense Epithelial Desquamation. Semi- attached & folded epithelial squames , sometimes partially covered with bacteria. 6. Areas of Ulceration with Exposed connective tissue 7. Areas of Hemorrhage. Numerous erythrocytes.
ROOT SURFACE WALL Changes seen in the root surface wall of the periodontal pocket are significant bcz they may perpetuate the periodontal infection, cause pain & complicate periodontal treatment. Deepening of periodontal pocket Degeneration of Sharpey’s fibers in the cementum Exposure of cementum to oral environment.
the Penetration and growth of bacteria into cementum(pathological granules) Fragmentation and breakdown of cementum surface. Areas of necrotic cementum. In addition , bacterial product such as endotoxins have also been detected in the cementum wall of periodontal pocket.
These changes are manifested clinically by, softening of the cementum surface , usually asymptomatic , painful when a probe or a explorer penetrate the area. Necrotic area on the root surface act as a reservoir for reinfection.
POCKET Debris CONTENTS ( microorganisms , enzymes, endotoxins & other metabolic product). Gingival crevicular fluid. Food remnants. Salivary mucin. Desquamated epithelial cell and leukocyte. Purulent exudate(living , degenerated & necrotic leukocytes, bacteria, serum , scanty fibrin).
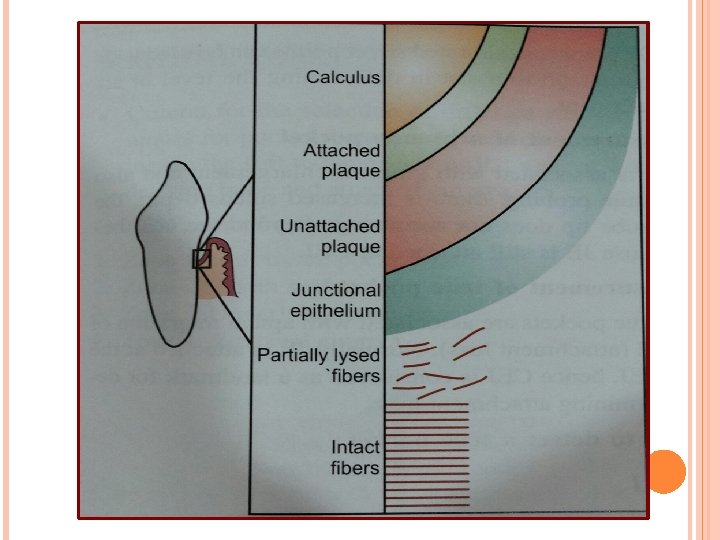
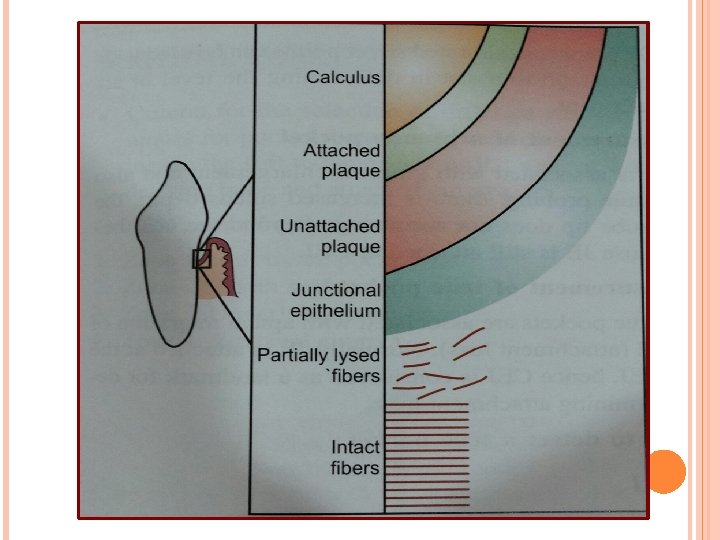
SURFACE MORPHOLOGY OF THE TOOTH WALL OF PERIODONTAL POCKET: Following zones can be found in the bottom of a periodontal pocket: 1. Cementum covered by calculus 2. Attached plaque Covers calculus & extends apically from it to a variable degree, probably 100 -500 micro m
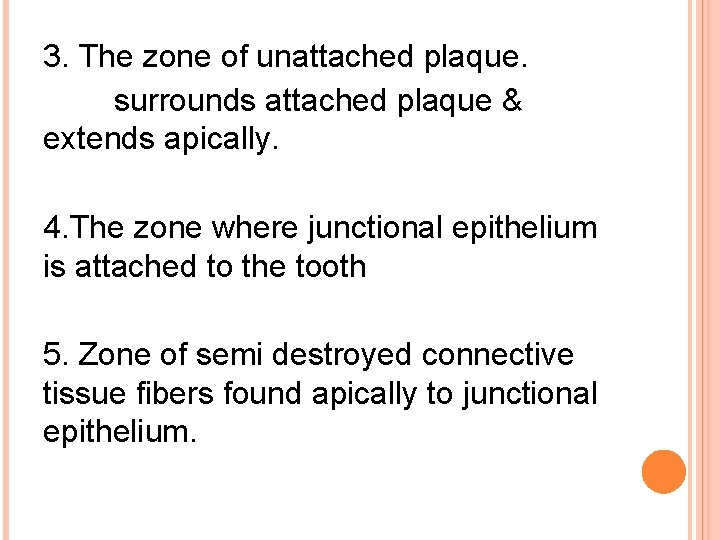
3. The zone of unattached plaque. surrounds attached plaque & extends apically. 4. The zone where junctional epithelium is attached to the tooth 5. Zone of semi destroyed connective tissue fibers found apically to junctional epithelium.
DETECTION OF POCKET: Only method of detecting and measuring periodontal pockets is careful explotation with a periodontal probe. Gutta percha points or calibrated silver points can be used with the radiography to assist in determining the level of attachment of periodontal pocket.

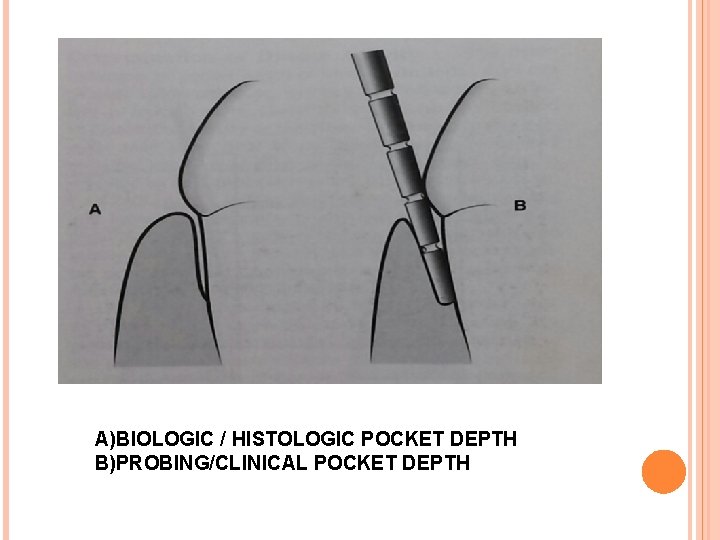
POCKET PROBING: Two different pocket depths are, 1)Biological / Historical depth 2)Clinical / Probing depth. The Biological depth is the distance between the gingival margin and the base of the pocket (the coronal end of the junctional epithelium.
The Probing depth is the distance to which an instrument(probe) penetrates into the pocket depends on factors such as, size of probe , Force with which it is introduced. (0. 75 N) Direction of penetration Resistance of the tissues.
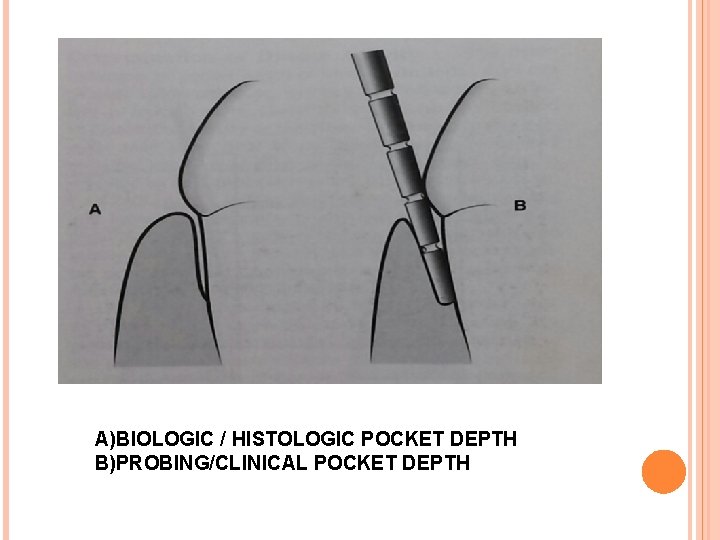
A)BIOLOGIC / HISTOLOGIC POCKET DEPTH B)PROBING/CLINICAL POCKET DEPTH
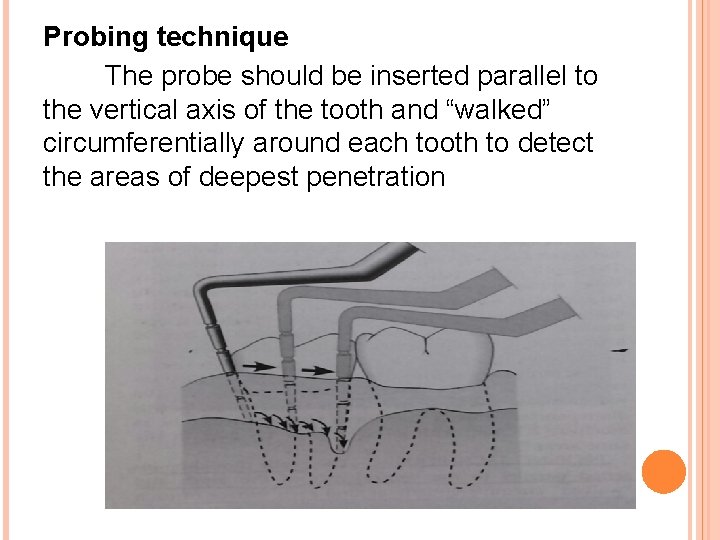
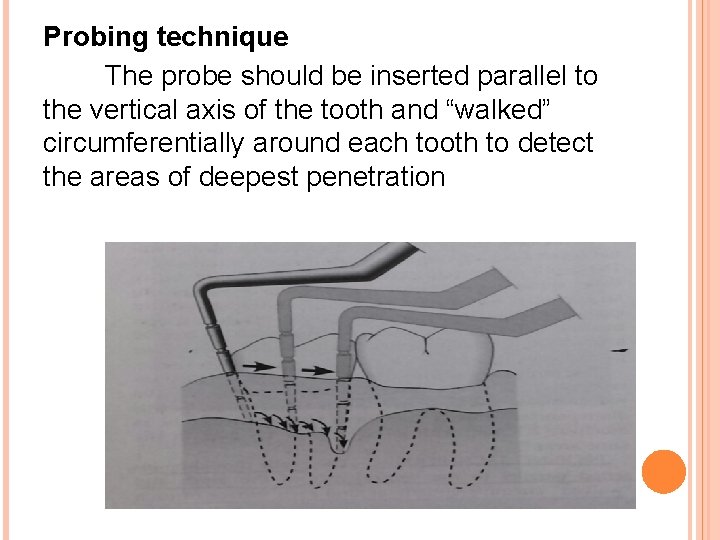
Probing technique The probe should be inserted parallel to the vertical axis of the tooth and “walked” circumferentially around each tooth to detect the areas of deepest penetration
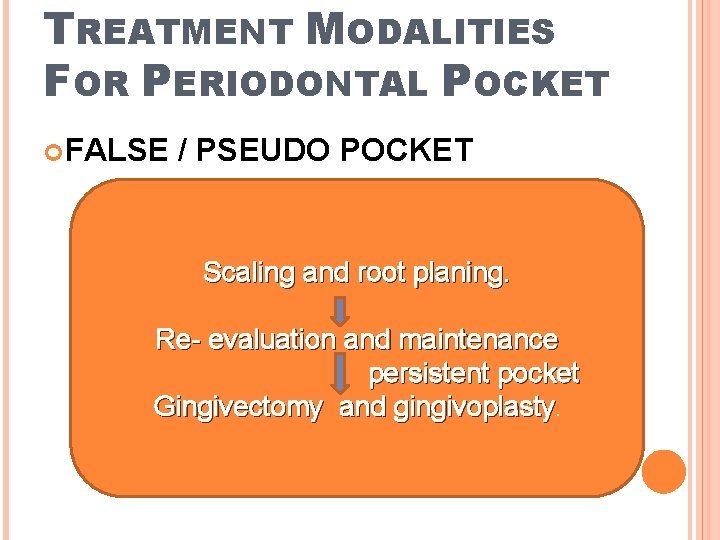
TREATMENT MODALITIES FOR PERIODONTAL POCKET FALSE / PSEUDO POCKET Scaling and root planing. Re- evaluation and maintenance persistent pocket Gingivectomy and gingivoplasty.

PERIODONTAL POCKET TRUE PERIODONTAL POCKET Scaling and root planing. Revaluation and maintenance Removal of pocket wall and removal of tooth side of the pocket.
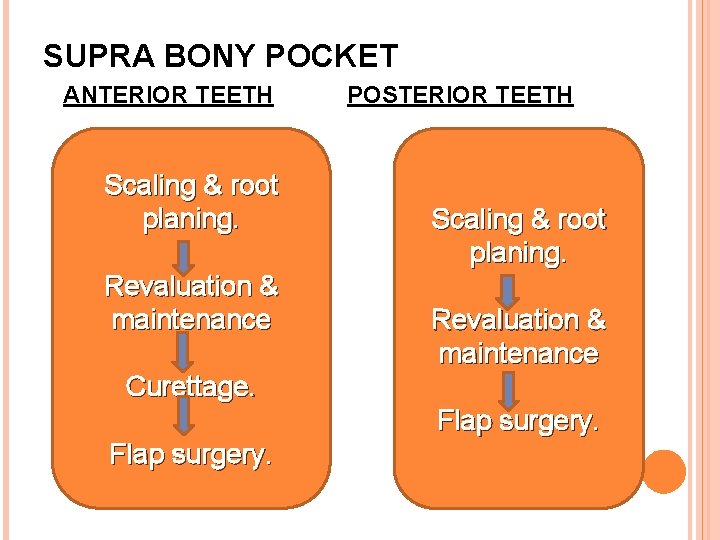
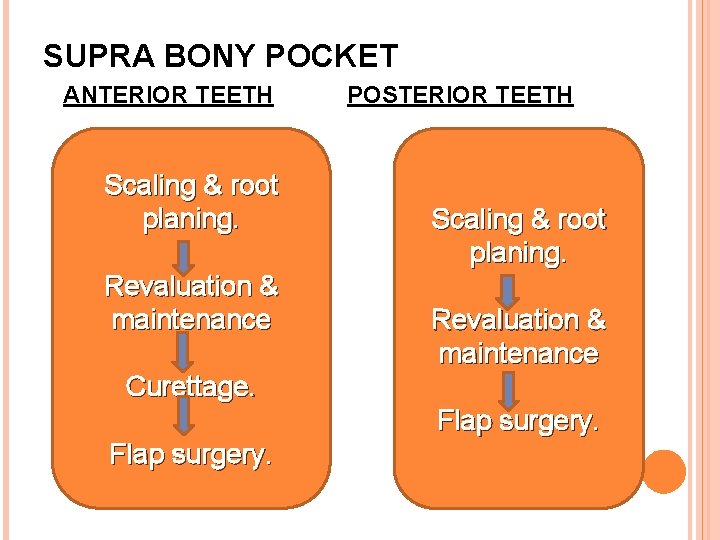
SUPRA BONY POCKET ANTERIOR TEETH Scaling & root planing. Revaluation & maintenance POSTERIOR TEETH Scaling & root planing. Revaluation & maintenance Curettage. Flap surgery.
INFRABONY POCKETS Infrabony pockets New attatchment procedures
CONCLUSION Periodontal disease can be irreversed if it is diagnosed at its early stage. If it is left undiagnosed, untreated can progress leading to destruction of periodontal tissue , ultimately resulting in loss of teeth which in turn will affect the general health of an individual. Periodontal health is closely related to oral hygiene, so maintenance of oral hygiene is of prime importance.
REFERENCE Text book of Carranza’s clinical periodontology Text book of periodontics by Sahithya reddy.

THANK YOU