Shoulder Dystocia Prediction and Management Outline IntroductionDefinition Incidence














- Slides: 41
Shoulder Dystocia Prediction and Management
Outline • • Introduction/Definition Incidence Aetiology / Risk Factors Prediction Management/ Prevention Complications / Litigation Controversies
Introduction • A serious frightening and threatening obstetric emergency. • It’s a situation where if undue haste is not balanced with delay, a delivery which would have been a normal happy event becomes catastrophic.
Definition • Shoulder dystocia has no universally accepted definition. • It occurs when the shoulders fail to traverse the pelvis after delivery of the head (Smeltzer 1986). • Resnik defined “True Shoulder Dystocia as deliveries requiring in addition to the usual downward traction and episiotomy, manouvres to deliver the Shoulders”.

• Sponge et al found a mean head-to-body delivery time of 24 seconds in normal babies compared with 79 seconds in those with shoulder dystocia and therefore proposed that any head-to-body delivery time greater than 60 seconds should be regarded as shoulder dystocia
INCIDENCE • Incidence figures varies according to the definition used. • It varies between 0. 37%-1. 1% of all deliveries • With the definition of true shoulder dystocia it can be as low as 0. 23%. (Beneditti et al). - Incidence is generally on the increase due to increasing birthweight, improved perinatal care, better reporting and documentation • Experience of the accoucher and position assumed by the patient during delivery also affects the incidence
AETIOLOGY /RISK FACTORS • Basically the aetiology of shoulder dystocia are-: • A disproportion between the fetal chest and maternal pelvis. Kwawukwame 2000 • Malrotation of the fetal shoulder at the pelvic inlet • A maternal pelvis flattened anteroposteriorly or a platypelloid pelvis

• In normal delivery the movement of the shoulders aids its passage through the birth canal since the bisacromial diameter is wider than the biparietal diameter • Big fetuses require an initial further rotation towards the transverse direction for the shoulders to enter the pelvis • Failure of this rotation leads to persistence of the antero-posterior position of the shoulders at the brim • Hence impaction of the shoulders

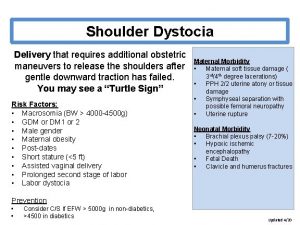
RISK FACTORS MATERNAL FACTORS • Obesity: Macrosomia is common among obese women by its effect on fetal weight and increased incidence of gestational diabetes. Mothers weighing >81 kg experienced 30% of all S. D (Seigworth 1966)
• Diabetes mellitus: The macrosomia of IDDM is characterised by selective organomegaly. Greater Shoulder/Head 1, Chest/Head 2, Abdomen/Head 3 ratios cf babies of similar weight of non-diabetic mothers. (Mondalou et al 1, Delpapa et al 2, Cohen et al 3 ).
• Prolonged pregnancy-: Eden et al found incidence of S. D at 40 weeks to be 0. 7% rising to 1. 3% at >/= 42 weeks. A no of fetuses particularly males have been known to continue growing exceeding 4 kg after 42 weeks gestation.
• Previous shoulder dystocia-: recurrent risk of 9. 8 -13. 8% • Short maternal stature-(less than 1. 5 m), • Advanced maternal age and Multiparity.

FETAL FACTORS • Weight-: incidence of S. D is proportional to the birth weight • S. D is 11 and 22 times more common in babies weighing more than 4000 g and 4500 g respectively (Acker et al 1985) • Incidence of 5. 2% in 4000 g-4250 g and 21% for 4750 g-5000 g in non-diabetics, • 8. 4%and 23. 5% for similar weight in diabetic women was found by Nesbitt et al (1998)
• INTRAPARTUM RISK FACTORS • Vacuum extraction and forceps delivery especially in the midcavity for prolonged second stage (Sokol et al 2002) • Arrest disorders • Primary dysfunctional labour • Epidural anaesthesia- controversial.

PREDICTION • Most risk factors are poor predictors of S. D and only about 25% of cases exhibit at least one significant risk factor (Gherman et al) • Fifty to sixty percent of S. D occurred in infants who weighed less than 4000 g. • Gonen et al(1996), using a combination of clinical(sensitivity-20%) and sonographic(error-+/-12%) data found poor correlation between prenatal estimation of birth weight and actual birth weight.
• However, a rate of fetal abdominal growth >1. 2 cm/wk between 32 -39 wks is predictive. • Macrosomia index: chest/biparietal diameter of 1. 4 or more.
MANAGEMENT • “Turtle neck sign” where there is failure of restitution and the neck is not visible and baby’s face appears fat may be the first warning sign of impending danger. • Decreasing the time interval between delivery of the fetal head to body is of great importance to baby’s survival. • Resist pulling on baby’s head • Don’t apply fundal pressure
• Don’t cause excessive rotation of the fetal head • Left lateral positioning may overcome mild S. D. This may be difficult for the patient. • “Shoulder dystocia drill” sequence depends on the experience of the operator and the help available.

HELPER mnemonic • H-: call for help (senior obstetrician, midwife, paediatrician, anaesthetist) • E-: episiotomy protects the pelvis, creates access to pelvis and increases chances of shoulder delivery. • L -: legs. Here maternal hips are abducted flexed and rotated, straightening the sacrum, and reducing the angle of pelvic inclination (Mc Roberts manoeuvre)

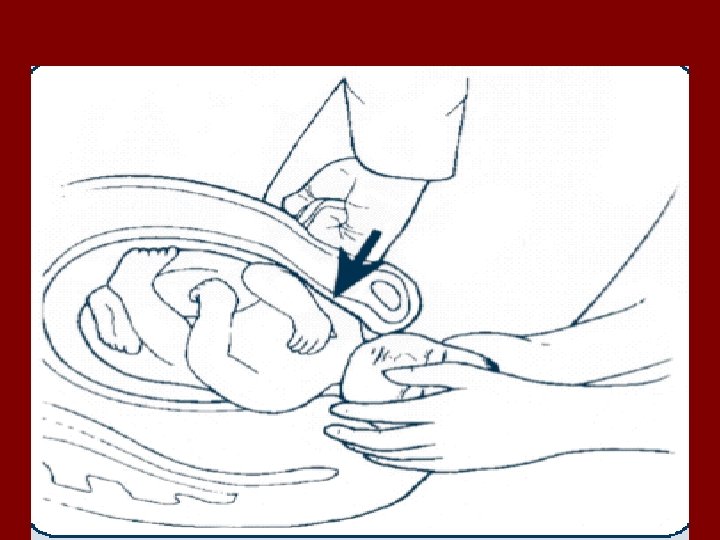
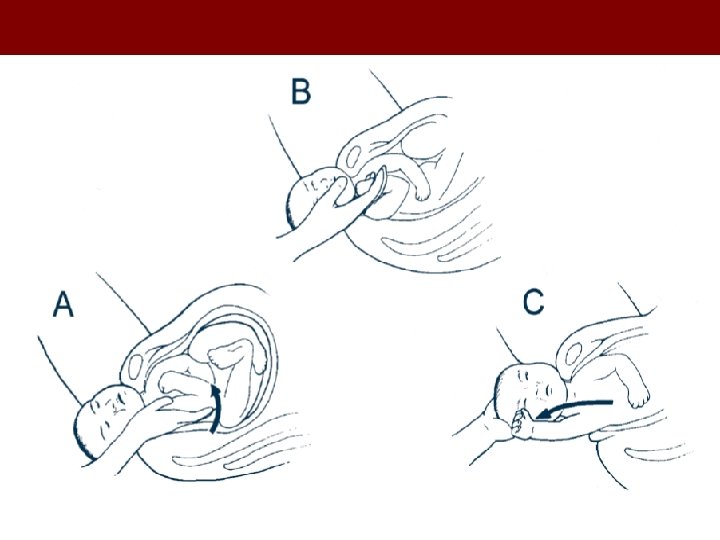
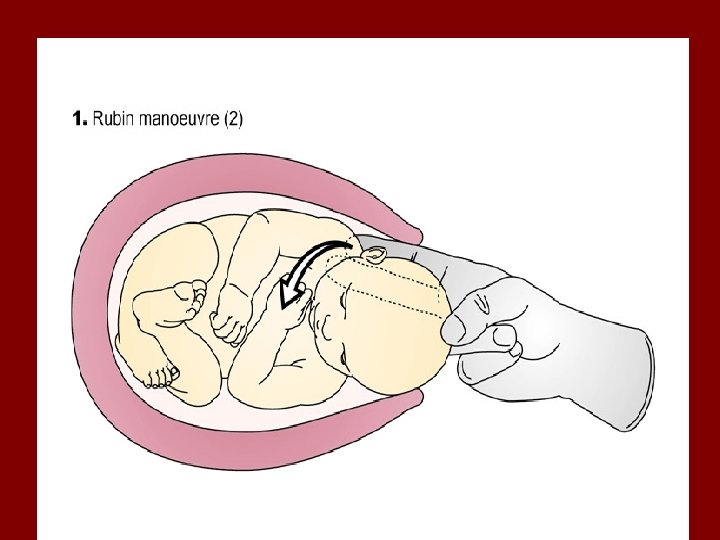
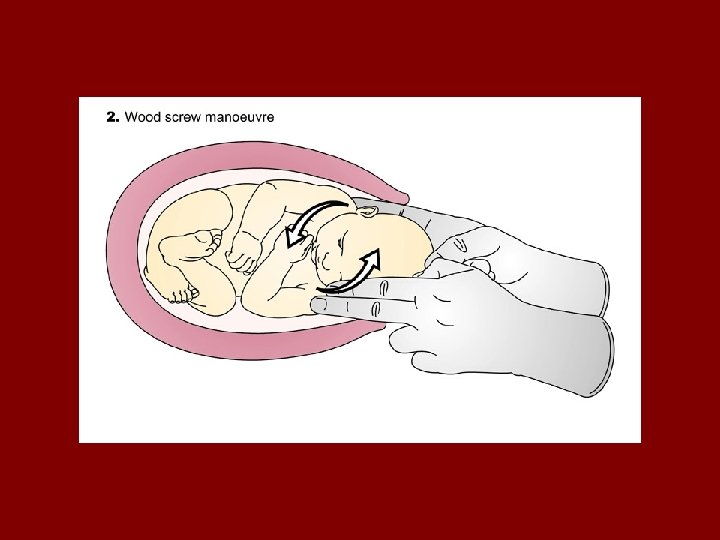
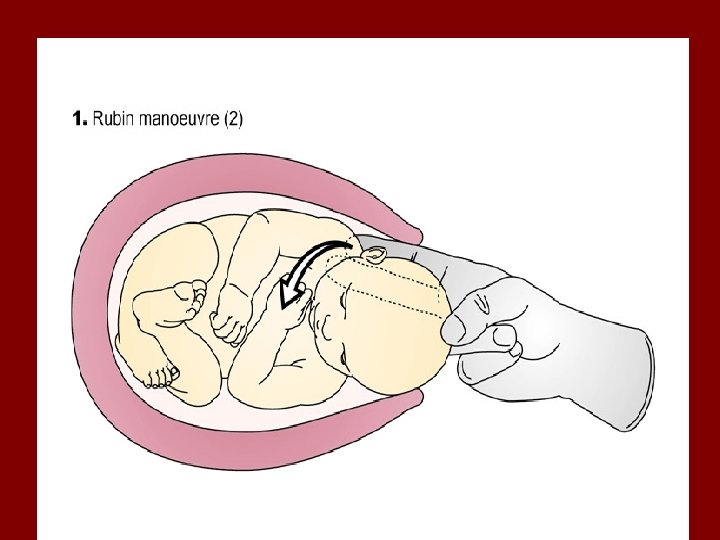
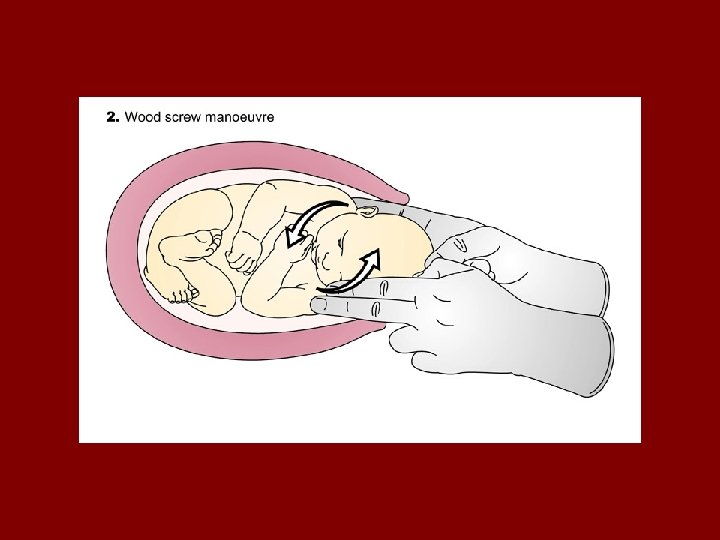
• P-: pressure, lateral suprapubic pressure should be applied by an assistant to dislodge the shoulders from the symphysis and adducts the shoulders causing reduction in bisacromial diameter. • E-: enter manoeuvres. a. wood’s cockscrew b. rubin manoeuvre.
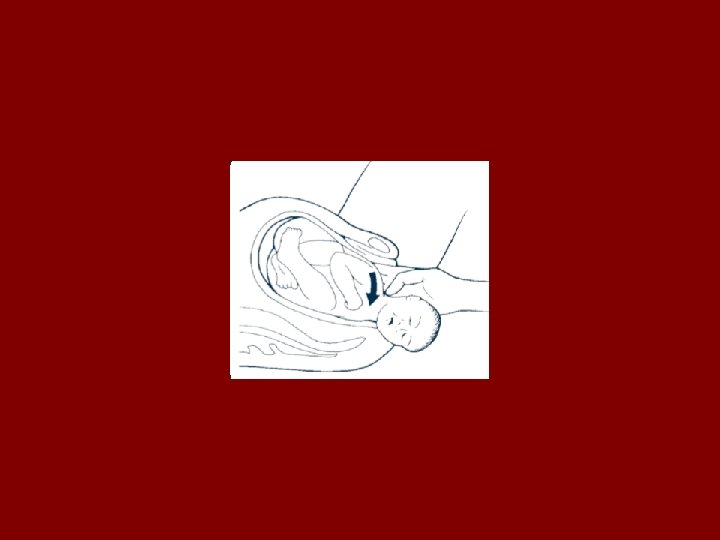
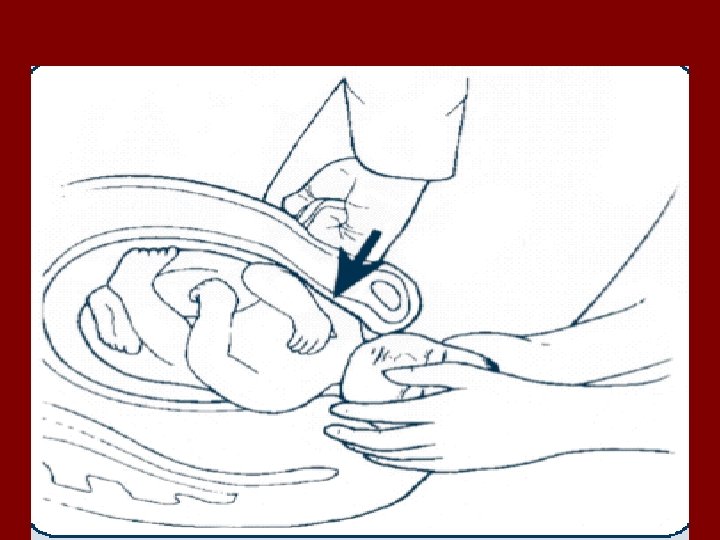
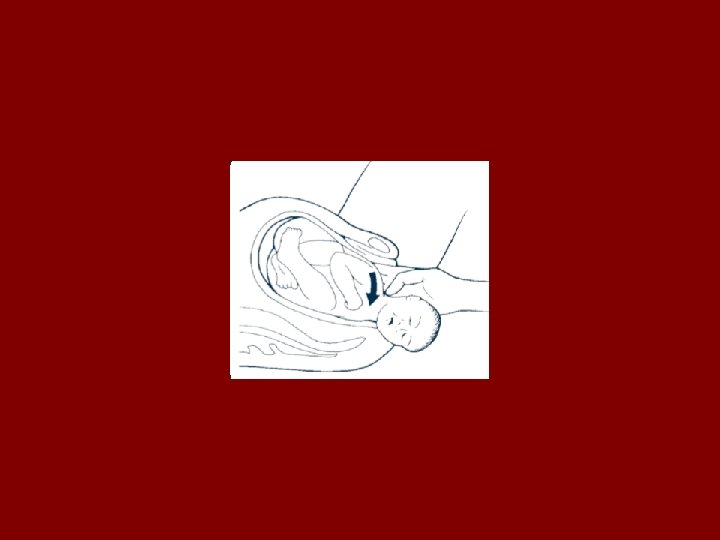
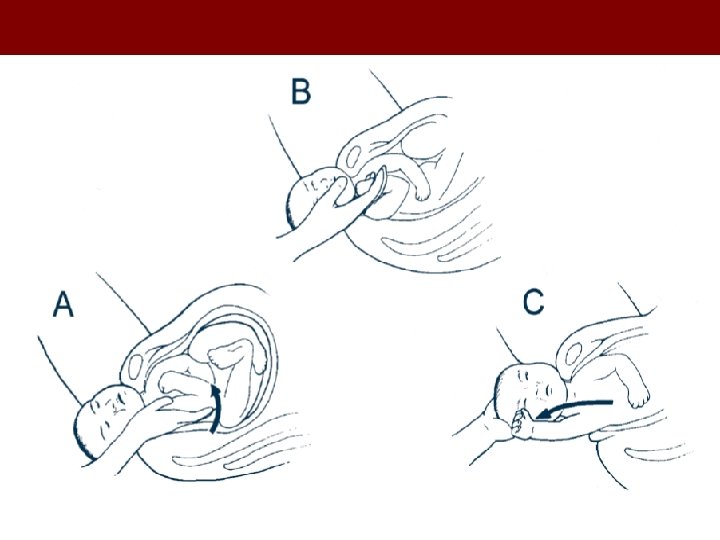
c. delivery of the posterior shoulder. R-: removal of the posterior arm by inserting operator’s hand in the vagina to cause flexion of the posterior arm at the shoulder and the elbow to retrieve the hand or forehand. This may result in fracture of clavicle or humerus.
• Cephalic replacement (Zavannelli manoeuvre): A desperate measure to replace the fetal head for abdominal delivery with the use of tocolytics, correction of restitution, flexion of head and gradual return into the vagina-followed by caesarean section -usually associated with maternal morbidity e. g ruptured uterus, PPH, endometritis
Other alternative measures • Deliberate fracture of the clavicles • Symphysiotomy • Cleidotomy





COMPLICATIONS • MATERNAL -Genital lacerations -Postpartum hemorrhage: atonic/traumatic -Bladder injury -Fistulae: VVF, RVF -wound sepsis and dehiscence -Symphyseal separation/ neuropathy
COMPLICATIONS contd • NEONATAL -Mortality: 2 - 29% -Morbidity: 20 -25% -Asphyxia: as evidenced by early neonatal seizures and permanent central neurological deficits. -Brachial plexus injury: In 11. 6 -16. 5%, most common is Erb’s palsy due to avulsion injury to C 5 & 6 nerve roots (95% usually resolve within neonatal period). Klumpke’s paralysis due to injury to C 7, C 8 nerve roots.

-phrenic nerve palsy leading to paralysis of the hemidiaphragm -thoracic spinal cord injury will cause overflow and rectal incontinence -sympathetic outflow tract from T 1 injury causes diminished pigmentation of the iris Bachial plexus injury have better prognosis than lower root traumas
Skeletal injuries-: fracture of the clavicle and humerus may occur but both have excellent prognosis.
PREVENTION • Pre-conceptional maternal weight reduction/ diabetic control: Coustan et al observed a decrease rate of S. D from 20. 4% to 13. 4% in those on dietary regimen and to 4. 8% in those on insulin regimen. • Avoidance of mid-cavity instrumental delivery for macrosomic infants following a delayed second stage.
-Elective caesarean section- controversies -Training and teaching of birth attendants with regular rehearsals of methods of dealing with S. D.
RISK OF LITIGATION S. D poses tremendous risk of litigation to the physician. Appropriate documentation of -decisions taken -procedures employed -outcome of procedures -effective communication with the baby’s mother will go a long way in reducing such risks. .

CONTROVERSIES • Elective caesarean section of macrosomia • Accuracies of clinical and sonographic estimates of fetal weight in management’s decision-making
CONCLUSION • • A life threatening obstetric emergency High index of suspicion Call for help Above there should be a team leader
 Helper mnemonic for shoulder dystocia
Helper mnemonic for shoulder dystocia Definition of shoulder dystocia
Definition of shoulder dystocia Dr reza nasr gynecologist
Dr reza nasr gynecologist Shoulder dystocia helper
Shoulder dystocia helper Waiter's tip hand
Waiter's tip hand Mcroberts maneuver
Mcroberts maneuver Attack rate epidemiology formula
Attack rate epidemiology formula Incidence vs incidence rate
Incidence vs incidence rate Introductiondefinition
Introductiondefinition Introductiondefinition
Introductiondefinition Types of style
Types of style Stages of normal labour
Stages of normal labour Vermont sheep and goat
Vermont sheep and goat Tmu crazy colors
Tmu crazy colors What is a quote sandwich examples
What is a quote sandwich examples How to calculate incidence rate example
How to calculate incidence rate example Incidence geometry proofs
Incidence geometry proofs Owasp cloud top 10
Owasp cloud top 10 Perpendicular incidence
Perpendicular incidence Contoh soal cumulative incidence
Contoh soal cumulative incidence Contoh soal attack rate dalam epidemiologi
Contoh soal attack rate dalam epidemiologi Tiroir ant cheville
Tiroir ant cheville Oriented incidence matrix
Oriented incidence matrix At what angle of incidence is the angle of refraction 90
At what angle of incidence is the angle of refraction 90 Walk dengan semua ruas dalam barisan berbeda
Walk dengan semua ruas dalam barisan berbeda How to calculate cumulative incidence example
How to calculate cumulative incidence example Prevented fraction
Prevented fraction Incidence matrix
Incidence matrix Rx cheville face
Rx cheville face Incidence de bernageau
Incidence de bernageau Oriented graph example
Oriented graph example Incidence matrix in discrete mathematics
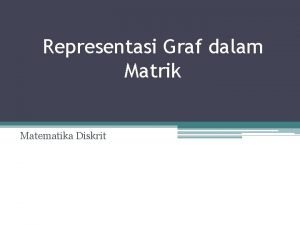
Incidence matrix in discrete mathematics Consumer incidence
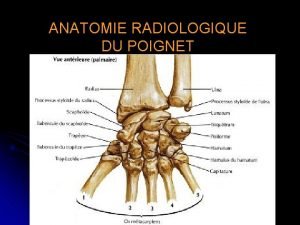
Consumer incidence Radio poignet normal profil
Radio poignet normal profil Incidence de railhac épaule
Incidence de railhac épaule Incidence de garth
Incidence de garth Government transfer payments examples
Government transfer payments examples Contoh soal representasi graf dalam matriks
Contoh soal representasi graf dalam matriks Epaule de face
Epaule de face Ukuran frekuensi penyakit adalah
Ukuran frekuensi penyakit adalah Incidence matrix
Incidence matrix Incidence de guntz definition
Incidence de guntz definition