Should we routinely perform prophylactic central neck dissection


- Slides: 59
Should we routinely perform prophylactic central neck dissection for patients with Papillary Carcinoma of the Thyroid? Clarence Mak NDH/AHNH
n n 30 year old Female No FHx of Thyroid Ca USG -Single 2 cm right lobe thyroid nodule -LN -ve
Questions to ask 1. What is the rationale supporting routine prophylactic central neck dissection? 2. What are the arguments against prophylactic central neck dissection? 3. Current evidence ?
What is the rationale supporting routine central neck dissection?
1. High incidence of microscopic disease n Incidence of clinically non-palpable (microscopic) disease more common than expected, 40 -70% n Pre-op imaging not sensitive enough USG high specificity & PPV low sensitivity in detecting cervical LN metastasis only 40 -83%* low negative predictive value (~60%) for central neck LN Role of central compartment neck dissection for adequate assessment of nodal involvement/ guide staging Stulak JM et. al Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 2006: 141: 5: 489 -494
2. LN metastasis and recurrence mainly in central neck n Central compartment is the most common site for LN metastases and recurrence n Recurrence is common -up to 30% of patients -up to 20 years after initial diagnosis n Mayo clinic 60 -year observation for 900 patients 80% of recurrence located in central compartment ~1/4 will have recurrence, in central neck compartment Roh JL et. al Total thyroidectomy plus neck dissection in differentiated thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007 245: 604 -610 Hay ID et. al Papillary Thyroid microcarcionoma: a study of 900 cases observed in a 60 -year period. Surgery 2009. 144: 980 -987
3. A guide for adjuvant radioactive iodine treatment n T 1 tumours Post surgical administriation of 131 I depends on LN status n T 1 tumour < 1 cm, unifocal, N 0 131 I not indicated n T 1 PTC patients Routine neck dissection identified a 30% increase in patients indicated for 131 I ablation preoperatively considered to be N 0, found to have unexpected nodal metastases Barczyński M, Konturek A, Stopa M, Nowak W: Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg 2013, 100: 410– 418 Shindo M, Wu JC, Park EE, Tanzella F: The importance of central compartment elective lymph node excision in the staging and treatment of papillary thyroid cancer. Arch Otolaryngol Head Neck Surg 2006, 132: 650 – 654
What are the arguments against prophylactic central neck dissection ?
Arguments AGAINST p. CND n Most micrometastatic central LN are subclinical recurrences clinically significant? n Good prognosis of papillary Ca thyroid 10 -year survival 95%, 15 -year survival 90% significant survival benefit? n Possibility of nerve injury and hypoparathyroidism n Very experienced surgeons re-exploration of central compartment is still feasible, even if recurrence
What is the current evidence available?
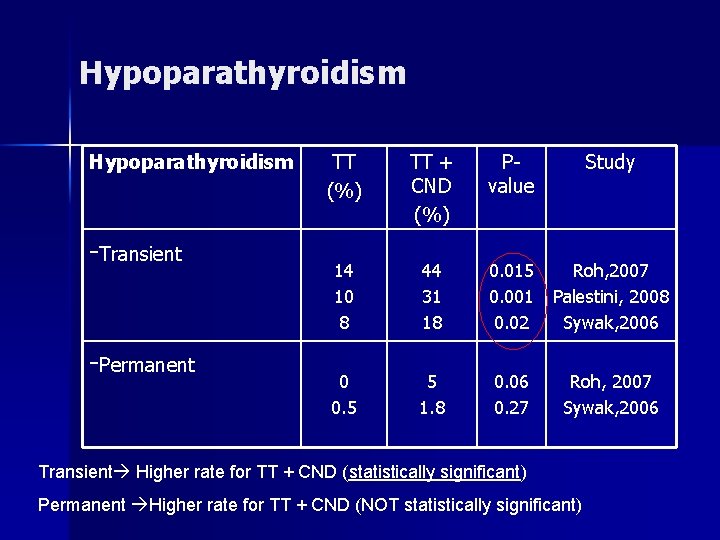
Does it have increased risks? Recurrent laryngeal nerve (RLN) injury n Hypoparathyroidism n
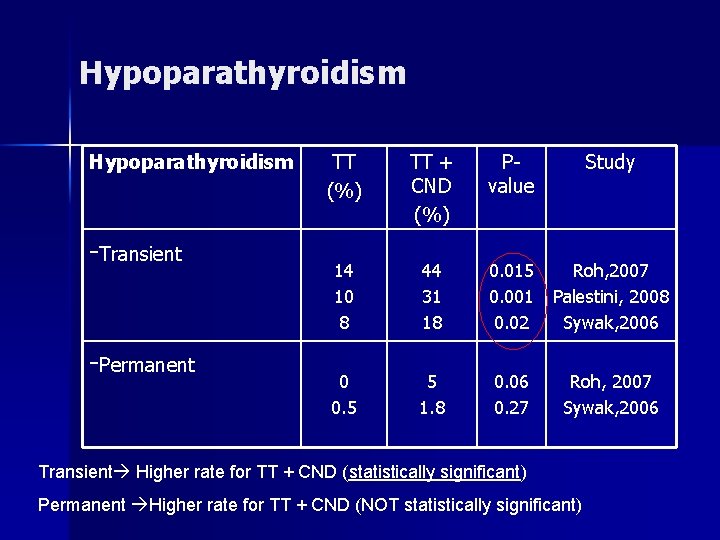
Hypoparathyroidism -Transient -Permanent TT (%) TT + CND (%) Pvalue Study 14 10 8 44 31 18 0. 015 0. 001 0. 02 Roh, 2007 Palestini, 2008 Sywak, 2006 0 0. 5 5 1. 8 0. 06 0. 27 Roh, 2007 Sywak, 2006 Transient Higher rate for TT + CND (statistically significant) Permanent Higher rate for TT + CND (NOT statistically significant)
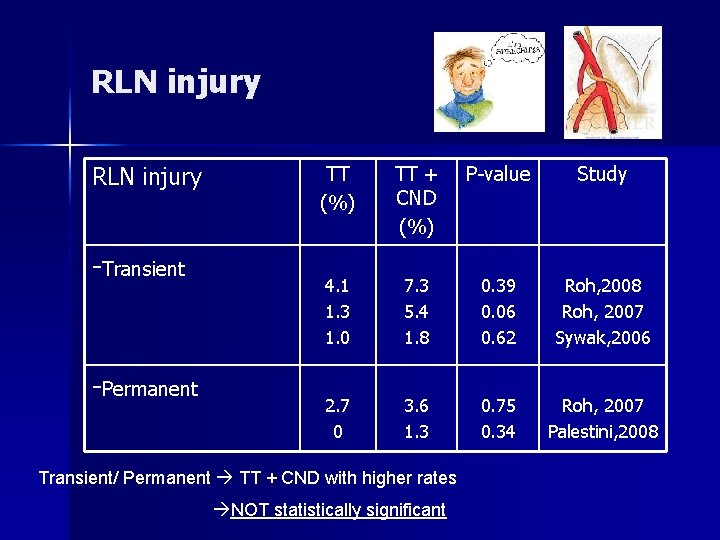
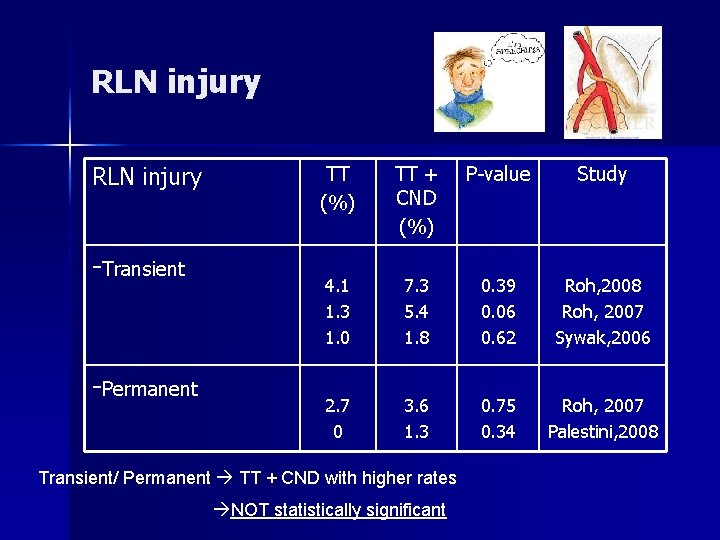
RLN injury -Transient -Permanent TT (%) TT + CND (%) P-value Study 4. 1 1. 3 1. 0 7. 3 5. 4 1. 8 0. 39 0. 06 0. 62 Roh, 2008 Roh, 2007 Sywak, 2006 2. 7 0 3. 6 1. 3 0. 75 0. 34 Roh, 2007 Palestini, 2008 Transient/ Permanent TT + CND with higher rates NOT statistically significant
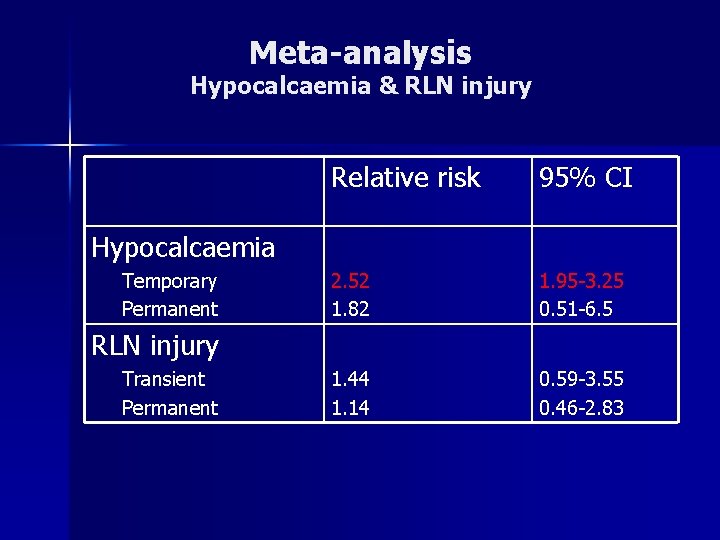
Meta-analysis Hypocalcaemia & RLN injury
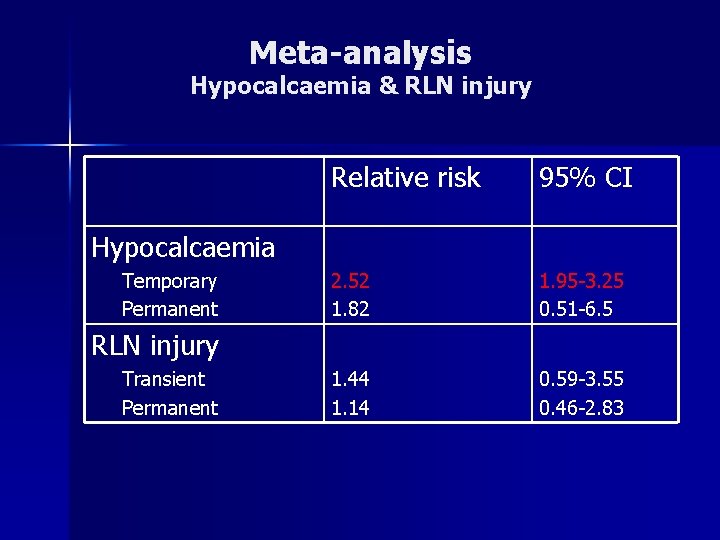
Meta-analysis Hypocalcaemia & RLN injury Relative risk 95% CI 2. 52 1. 82 1. 95 -3. 25 0. 51 -6. 5 1. 44 1. 14 0. 59 -3. 55 0. 46 -2. 83 Hypocalcaemia Temporary Permanent RLN injury Transient Permanent
Locoregional Control Survival
n Previous evidence -retrospective studies -short FU n Meta-analyses -heterogenous studies -heterogenous results n PTC carries a good prognosis Most studies with short FU unable to demonstrate a difference between TT/p. CND vs TT
n n Retrospective cohort study, 10 years , 640 patients 282 TT (1993 -1997) vs 358 TT/p. CND (1998 -2002)
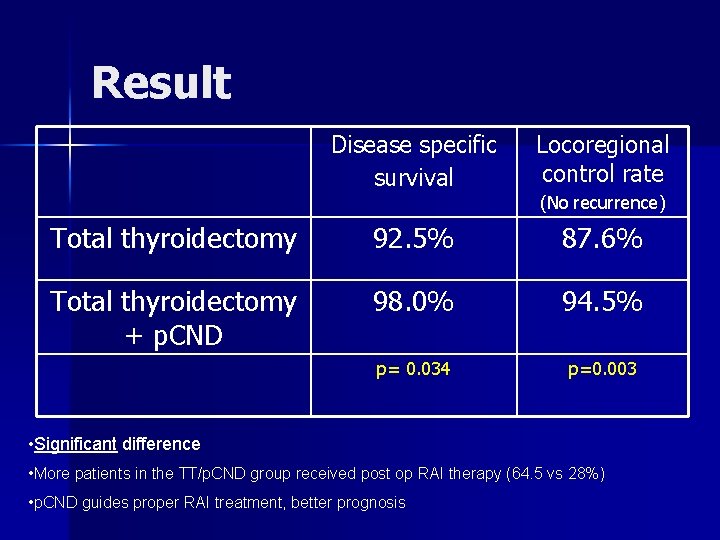
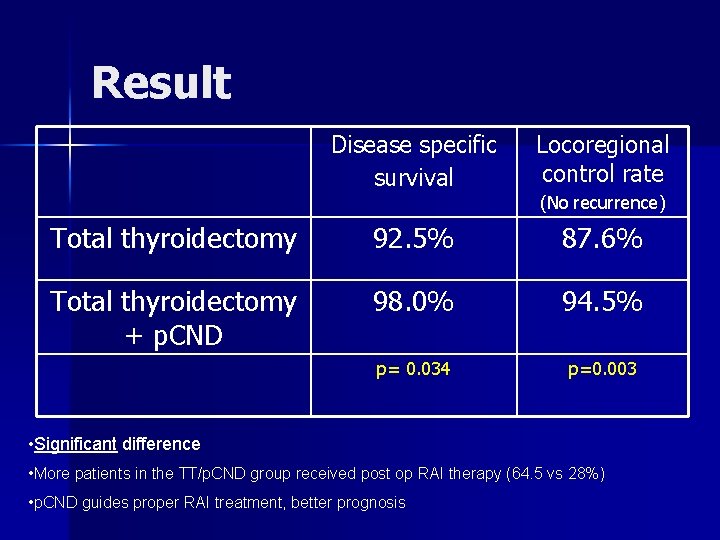
Result Disease specific survival Locoregional control rate Total thyroidectomy 92. 5% 87. 6% Total thyroidectomy + p. CND 98. 0% 94. 5% p= 0. 034 p=0. 003 (No recurrence) • Significant difference • More patients in the TT/p. CND group received post op RAI therapy (64. 5 vs 28%) • p. CND guides proper RAI treatment, better prognosis
n 11 studies with 2, 318 patients n Included a more homogenous study population, (c. N 0 PTC)
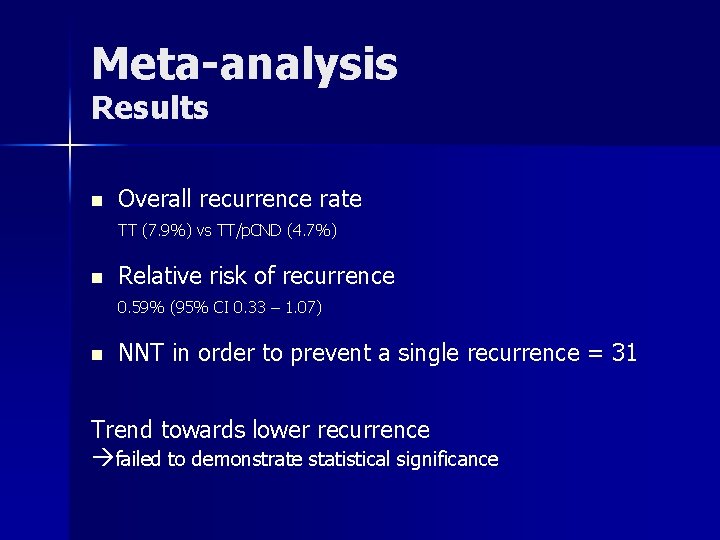
Meta-analysis Results n Overall recurrence rate TT (7. 9%) vs TT/p. CND (4. 7%) n Relative risk of recurrence 0. 59% (95% CI 0. 33 – 1. 07) n NNT in order to prevent a single recurrence = 31 Trend towards lower recurrence failed to demonstrate statistical significance
Current evidence n Risk Temporary hypoparathyroidism RLN injury risk same n Benefit Trend of better survival and locoregional control Not statistically significant in meta-analysis
Recommendations/ Guidelines
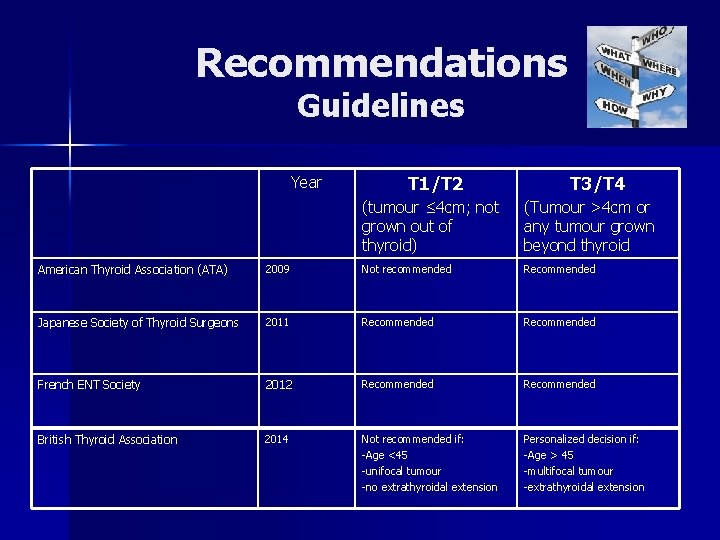
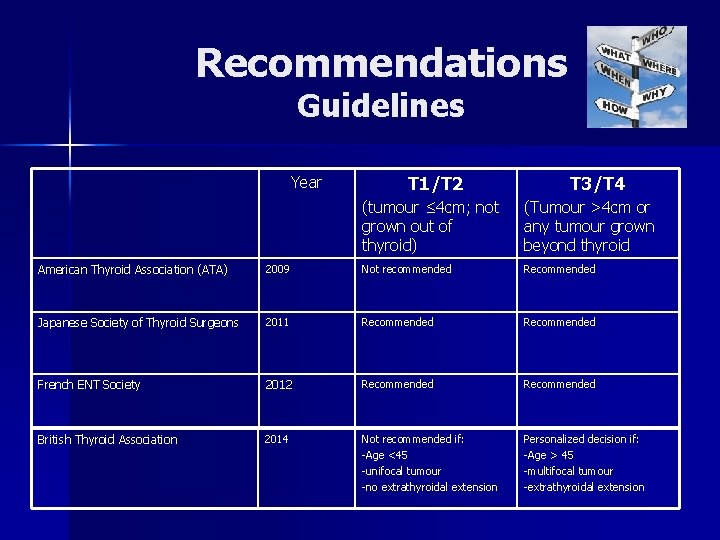
Recommendations Guidelines Year T 1/T 2 T 3/T 4 (tumour ≤ 4 cm; not grown out of thyroid) (Tumour >4 cm or any tumour grown beyond thyroid American Thyroid Association (ATA) 2009 Not recommended Recommended Japanese Society of Thyroid Surgeons 2011 Recommended French ENT Society 2012 Recommended British Thyroid Association 2014 Not recommended if: -Age <45 -unifocal tumour -no extrathyroidal extension Personalized decision if: -Age > 45 -multifocal tumour -extrathyroidal extension
30 year old, 2 cm papillary carcinoma, LN –ve…. . . Risk Survival Burden from recurrence

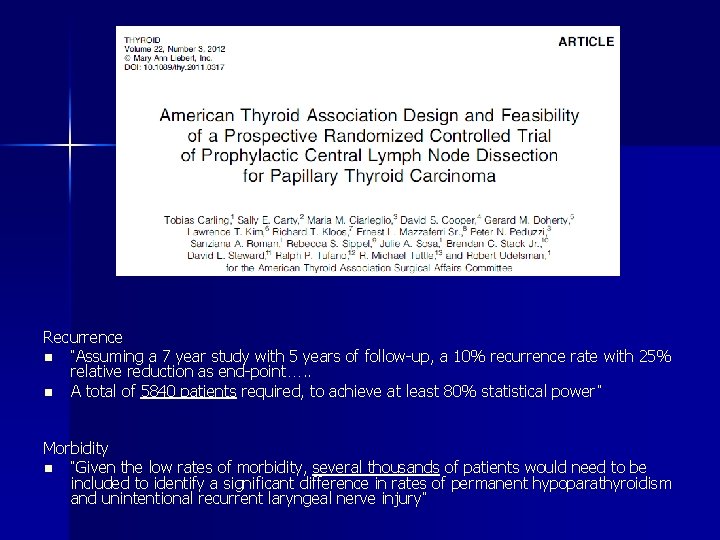
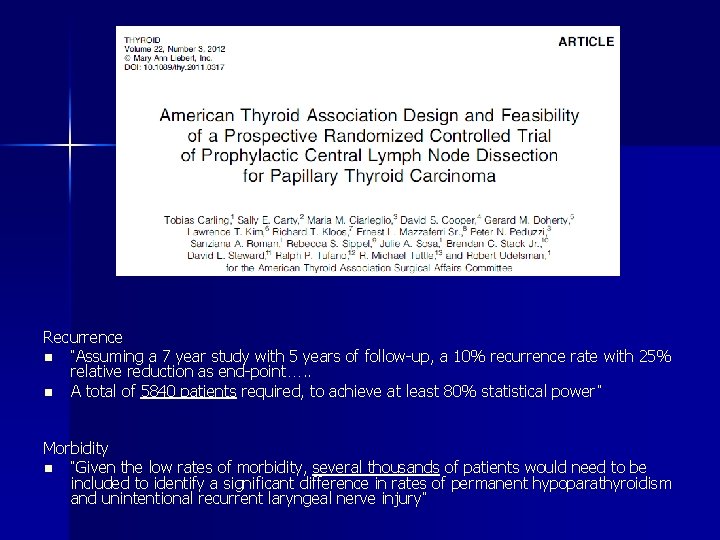
Recurrence n “Assuming a 7 year study with 5 years of follow-up, a 10% recurrence rate with 25% relative reduction as end-point…. . n A total of 5840 patients required, to achieve at least 80% statistical power” Morbidity n “Given the low rates of morbidity, several thousands of patients would need to be included to identify a significant difference in rates of permanent hypoparathyroidism and unintentional recurrent laryngeal nerve injury”
Sentinel LN Biopsy
114 patients with clinically node –ve PTC, peri-tumoral injection of methylene blue intraop n All patients underwent TT + CND n SLN identified in 73. 7% of patients n Results -High specificity (100%) and PPV (100%) -Sensitivity only 64. 9% & false –ve rate 35. 1% suggesting that SLNB is not adequate as screening tool n
Predictors of LN metastases
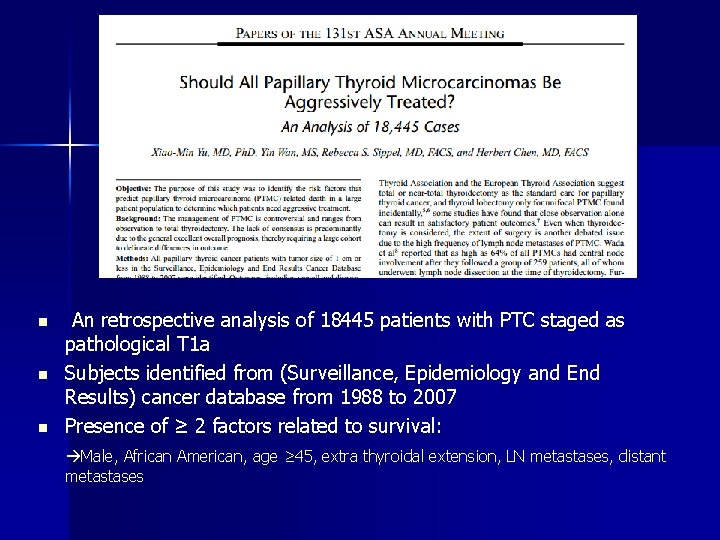
n n n An retrospective analysis of 18445 patients with PTC staged as pathological T 1 a Subjects identified from (Surveillance, Epidemiology and End Results) cancer database from 1988 to 2007 Presence of ≥ 2 factors related to survival: Male, African American, age ≥ 45, extra thyroidal extension, LN metastases, distant metastases
n Other risk factors favoring recurrence: -History of familial thyroid cancer -Tumour factors primary tumour > 2 cm multifocal bilateral presence of disease in thyroid

BRAF mutation
BRAF mutation BRAF = B-type Raf kinase, located in chromosome 7 n Most common mutation conversion of valine to glutamate of amino acid, causing a constitutively active BRAF kinase n Active BRAF kinase being an oncogene in human cancer n
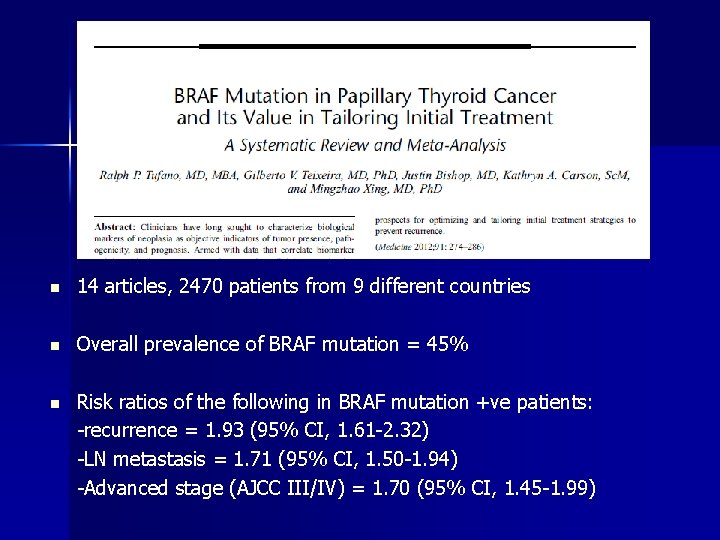
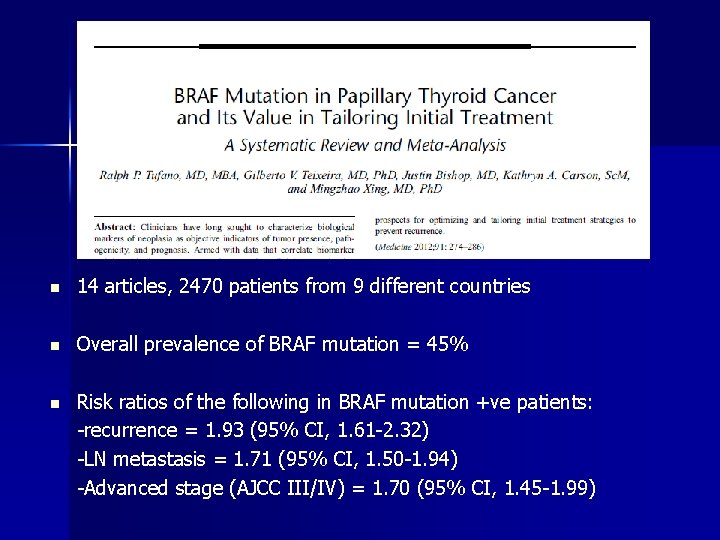
n 14 articles, 2470 patients from 9 different countries n Overall prevalence of BRAF mutation = 45% n Risk ratios of the following in BRAF mutation +ve patients: -recurrence = 1. 93 (95% CI, 1. 61 -2. 32) -LN metastasis = 1. 71 (95% CI, 1. 50 -1. 94) -Advanced stage (AJCC III/IV) = 1. 70 (95% CI, 1. 45 -1. 99)
Unilateral vs Bilateral neck dissection
Unilateral vs Bilateral n Unilateral p. CND -serves as an indicator of regional spread -tool for selecting patients for further treatment -lower morbidity rates than bilateral p. CND Giordano D, Valcavi R, Thompson GB et al (2012) Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 22: 911– 917
Unilateral vs Bilateral n However, central lymph node metastases (CLNM) can be found in 25% of contralateral level VI Thus, unilateral PND may not be considered as a therapeutic step in patients with CLNM Raffaelli M, De Crea C, Sessa L et al (2012) Prospective evaluation of total thyroidectomy versus ipsilateral versus bilateral central neck dissection in patients with clinically node-negative papillary thyroid carcinoma. Surgery 152: 957– 964
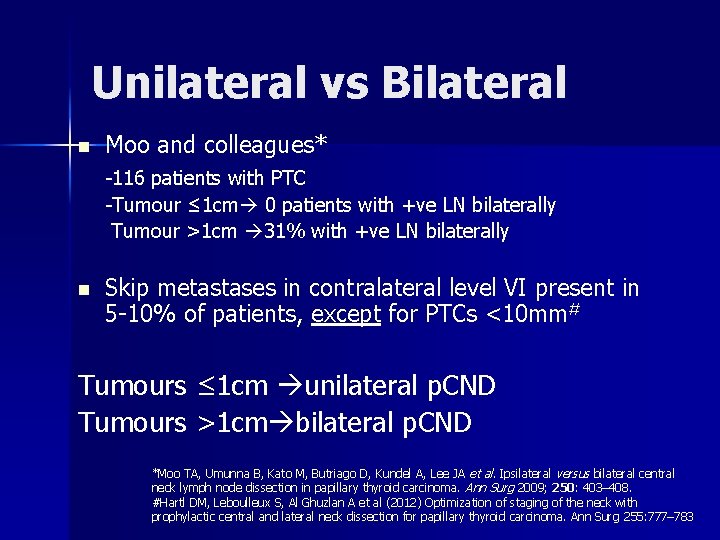
Unilateral vs Bilateral n Moo and colleagues* -116 patients with PTC -Tumour ≤ 1 cm 0 patients with +ve LN bilaterally Tumour >1 cm 31% with +ve LN bilaterally n Skip metastases in contralateral level VI present in 5 -10% of patients, except for PTCs <10 mm# Tumours ≤ 1 cm unilateral p. CND Tumours >1 cm bilateral p. CND *Moo TA, Umunna B, Kato M, Butriago D, Kundel A, Lee JA et al. Ipsilateral versus bilateral central neck lymph node dissection in papillary thyroid carcinoma. Ann Surg 2009; 250: 403– 408. #Hartl DM, Leboulleux S, Al Ghuzlan A et al (2012) Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg 255: 777– 783
Post operative radioactive iodine ablation
Post-operative radioiodine ablation therapy n Radioactive iodine -aims to destroy any possible occult residual microscopic thyroid carcinoma to reduce future disease recurrence n Side effects -Salivary dysfunction, nasolacrimal duct obstruction -small risk of 2 o primary malignancies
Post-op ablative radioiodine Recent consensus: Post surgical administriation of 131 I classified as T 1 (diameter < 2 cm) depends on LN status
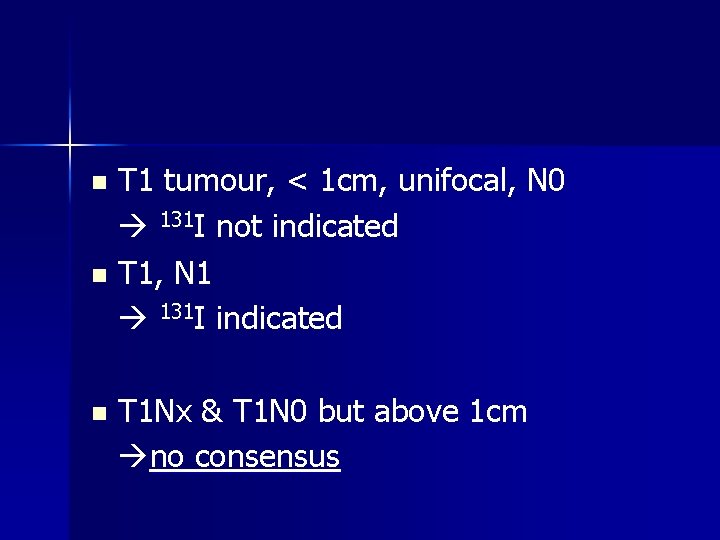
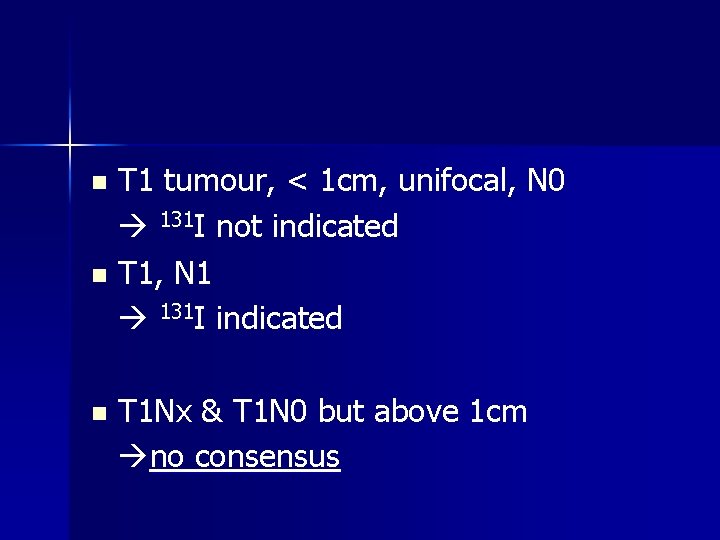
T 1 tumour, < 1 cm, unifocal, N 0 131 I not indicated n T 1, N 1 131 I indicated n n T 1 Nx & T 1 N 0 but above 1 cm no consensus
Is prophylactic CND useful in finding the patients with T 1 N 1, who were initially thought to be T 1 N 0, in which 131 I would now be indicated?
n Literature reports a 30% increase in the number of patients with T 1 PTC (preoperatively considered to be N 0), for whom 131 I ablation was indicated following routine neck dissection demonstrating unexpected nodal metastases. Barczyński M, Konturek A, Stopa M, Nowak W: Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg 2013, 100: 410– 418 Shindo M, Wu JC, Park EE, Tanzella F: The importance of central compartment elective lymph node excision in the staging and treatment of papillary thyroid cancer. Arch Otolaryngol Head Neck Surg 2006, 132: 650– 654
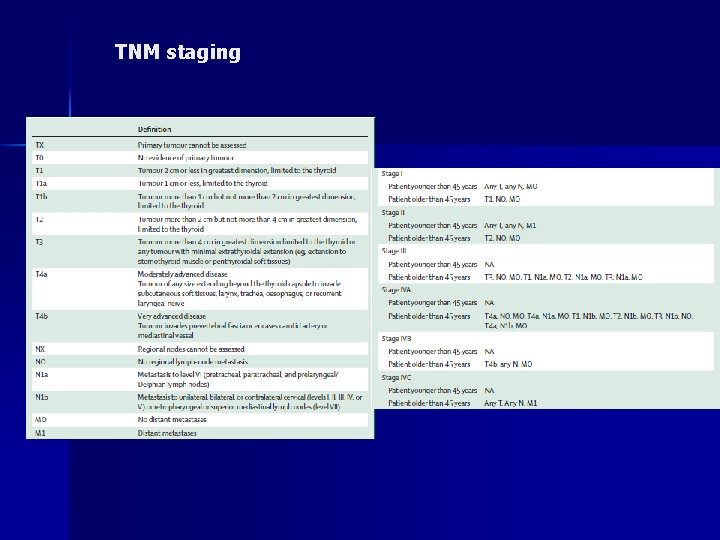
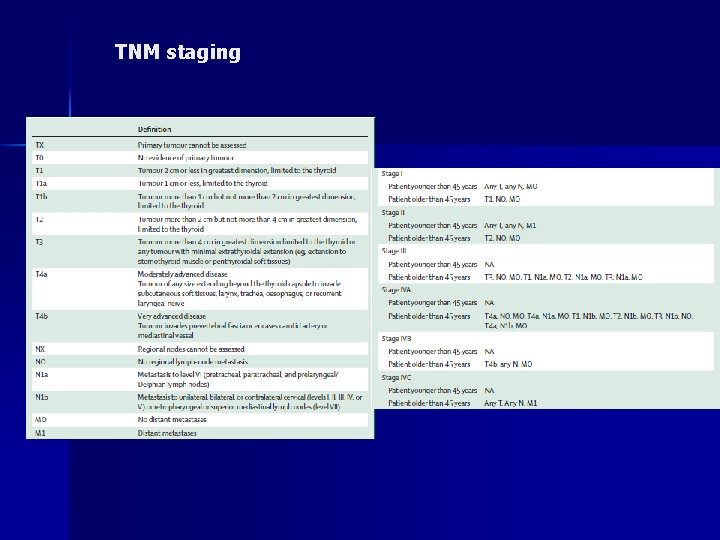
TNM staging
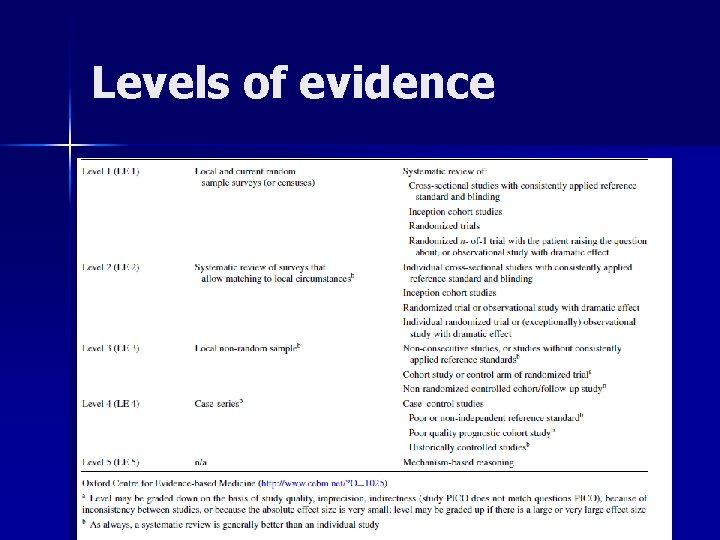
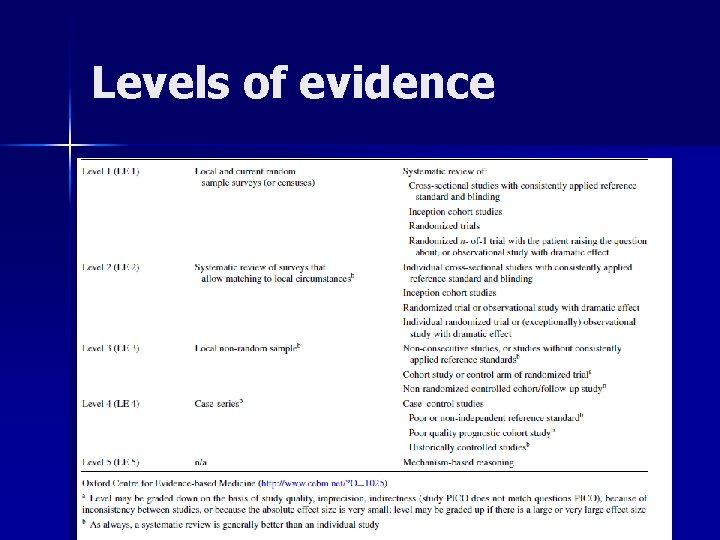
Levels of evidence
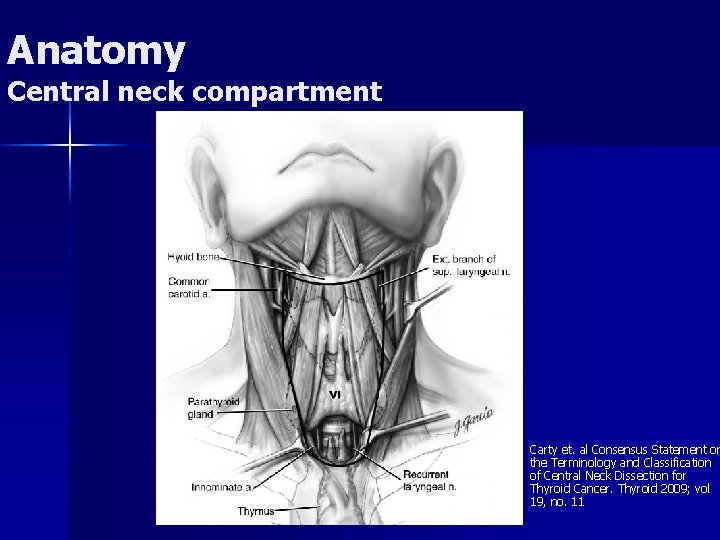
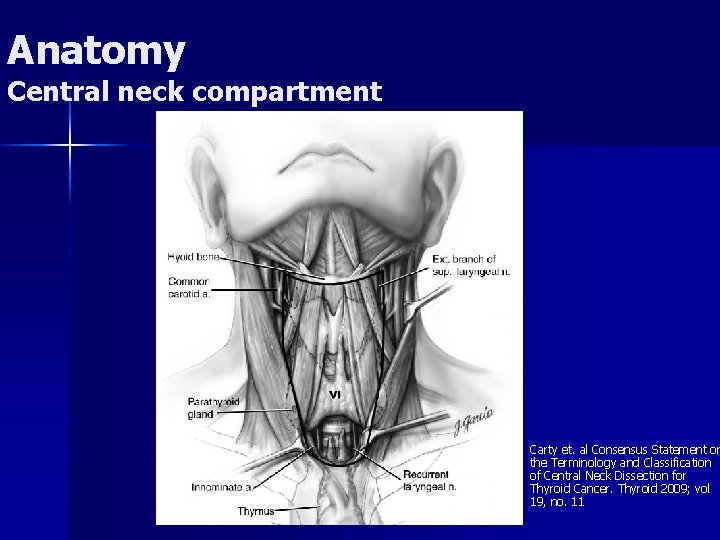
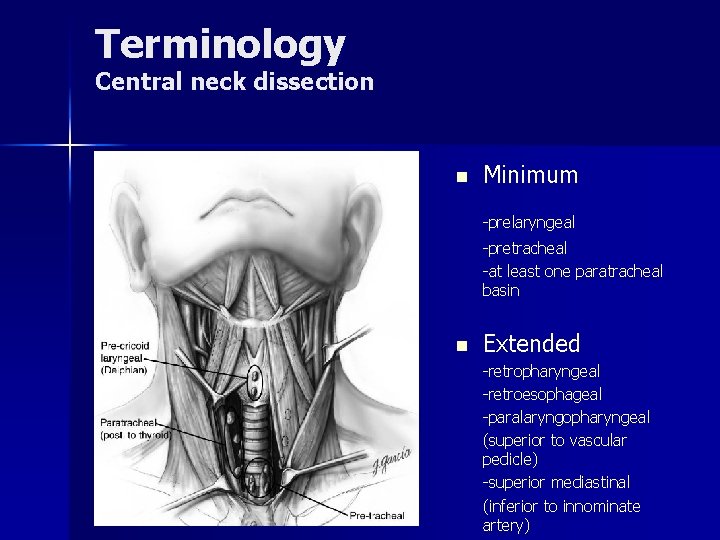
Anatomy Central neck compartment n Carty et. al Consensus Statement on the Terminology and Classification of Central Neck Dissection for Thyroid Cancer. Thyroid 2009; vol 19, no. 11
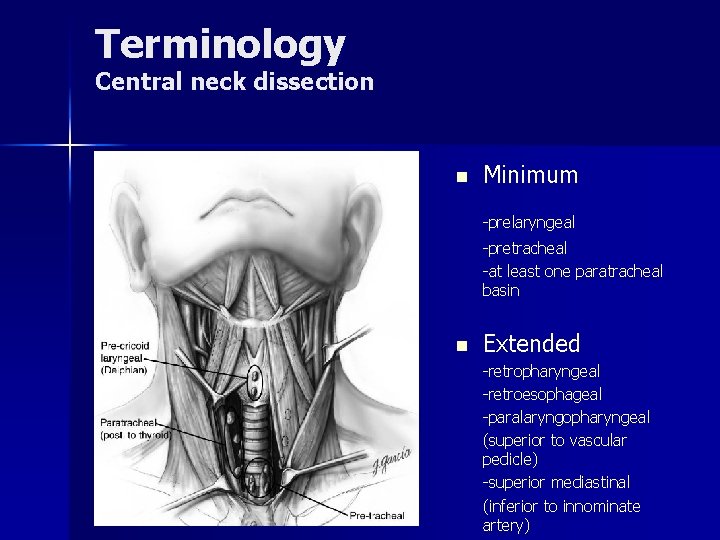
Terminology Central neck dissection n Minimum -prelaryngeal -pretracheal -at least one paratracheal basin n Extended -retropharyngeal -retroesophageal -paralaryngopharyngeal (superior to vascular pedicle) -superior mediastinal (inferior to innominate artery)
Possibility of high level evidence?
Terminology n Therapeutic neck dissection nodal metastasis apparent clinically (preoperatively/ intraoperatively) or by imaging (clinically N 1 a) n Prophylactic (elective) neck dissection nodal metastasis was not detected clinically or by imaging (clinically N 0)
Lateral neck LN dissection
Prophylactic Lateral Neck Dissection n Supporters -Prophylactic lateral neck dissection can identify and better stage the >50% of patients with +ve central nodes who will have metastatic nodes in levels III/ IV n Against -No evidence that prophylactic neck dissection improves survival or loco-regional control -overtreats 75% of patients BTA guidelines, 2014 n No evidence of central compartment LN prophylactic lateral neck dissection not recommended n Central compartment LN +ve Personalized decision making
Therapeutic Lateral Neck Dissection n Patients with overt metastatic disease in lateral neck will have clinical/ radiological evidence of central neck LN metastases in more than 80% of cases n Suspicious/ clinically involved nodes in lateral neck therapeutic central and selective lateral neck dissection (levels IIa. Vb) recommended accessory nerve, SCM, and interal jugular vein preserved
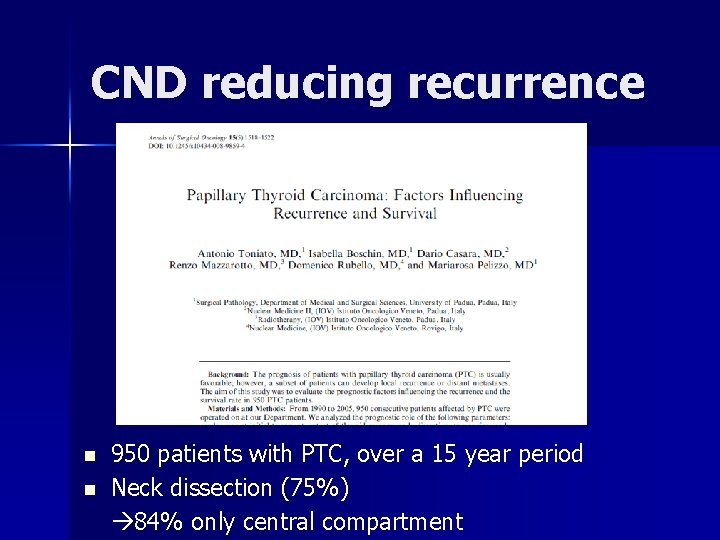
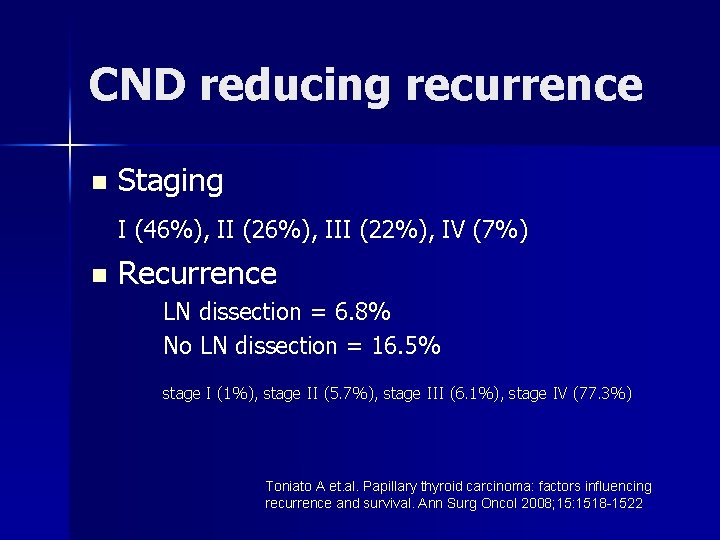
CND reducing recurrence n n 950 patients with PTC, over a 15 year period Neck dissection (75%) 84% only central compartment
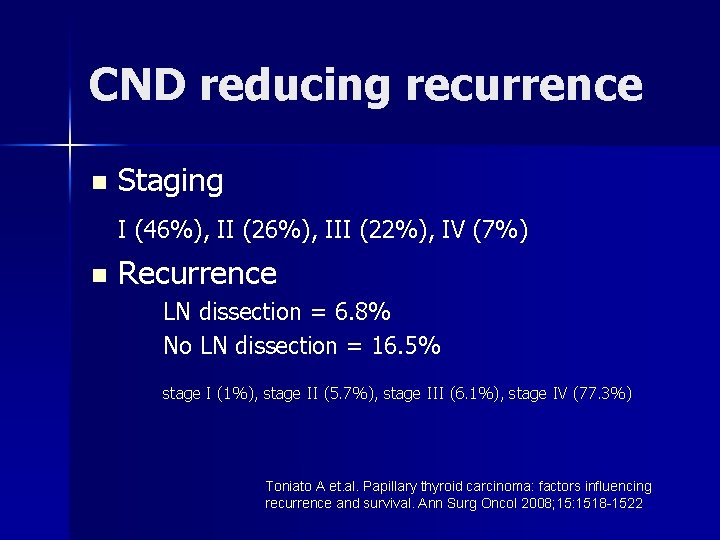
CND reducing recurrence n Staging I (46%), II (26%), III (22%), IV (7%) n Recurrence LN dissection = 6. 8% No LN dissection = 16. 5% stage I (1%), stage II (5. 7%), stage III (6. 1%), stage IV (77. 3%) Toniato A et. al. Papillary thyroid carcinoma: factors influencing recurrence and survival. Ann Surg Oncol 2008; 15: 1518 -1522
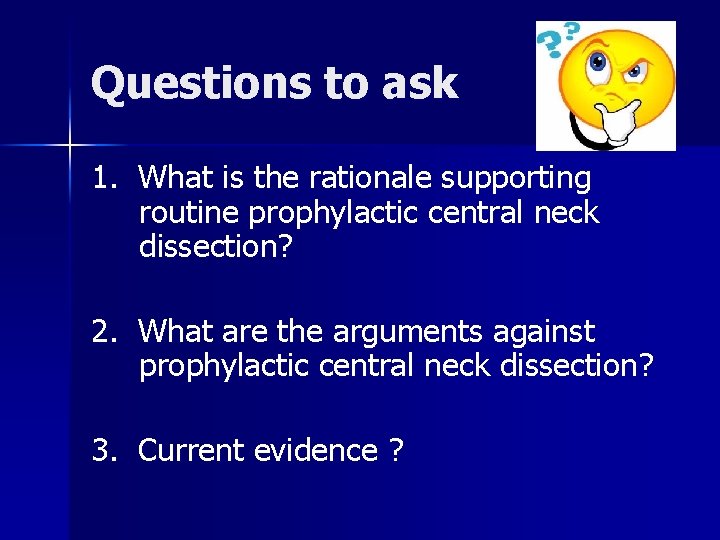
4. Lowers Tg level n. Lowers postoperative thyroglobulin levels n. Undetectable thyroglobulin level TT + CND (72%) vs TT (43%) n. More effective detection of persistent/ recurrent disease Sywak M, Cornford L, Roach P, et al. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery 2006; 140: 1000 -5; discussion 1005 -7.