Should the Guidelines for Unprotected LM PCI Change


- Slides: 18
Should the Guidelines for Unprotected LM PCI Change? Yes… No… Maybe… Gregg W. Stone MD Columbia University Medical Center The Cardiovascular Research Foundation
DISCLOSURES Gregg W. Stone, MD Honoraria – Boston Scientific Corporation, Abbott Vascular
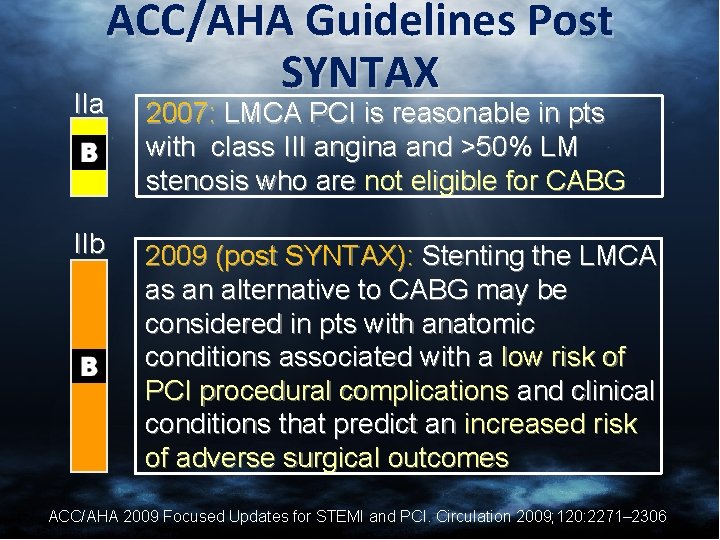
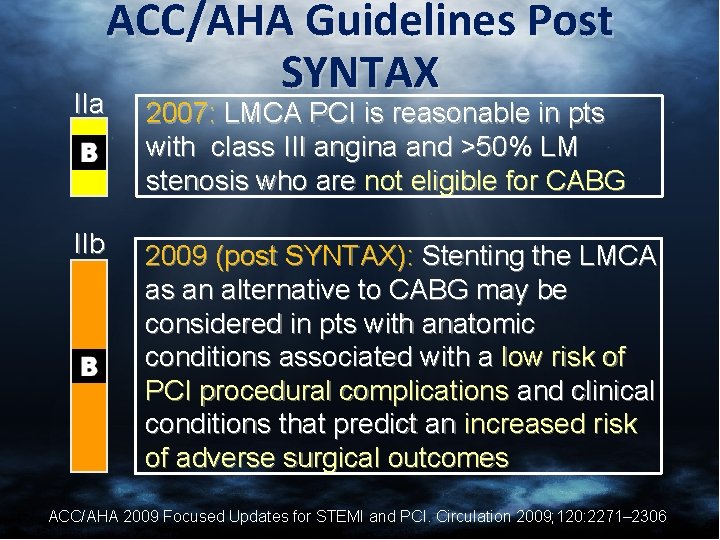
ACC/AHA Guidelines Post SYNTAX IIa 2007: LMCA PCI is reasonable in pts with class III angina and >50% LM stenosis who are not eligible for CABG IIb 2009 (post SYNTAX): Stenting the LMCA as an alternative to CABG may be considered in pts with anatomic conditions associated with a low risk of PCI procedural complications and clinical conditions that predict an increased risk of adverse surgical outcomes ACC/AHA 2009 Focused Updates for STEMI and PCI. Circulation 2009; 120: 2271– 2306
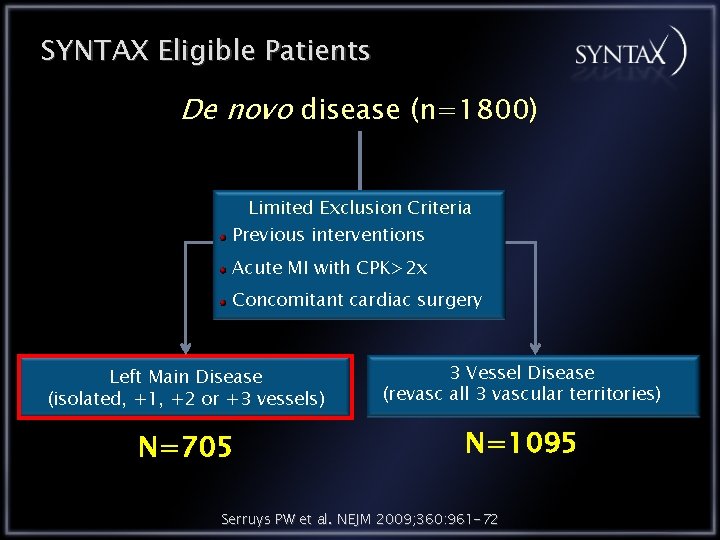
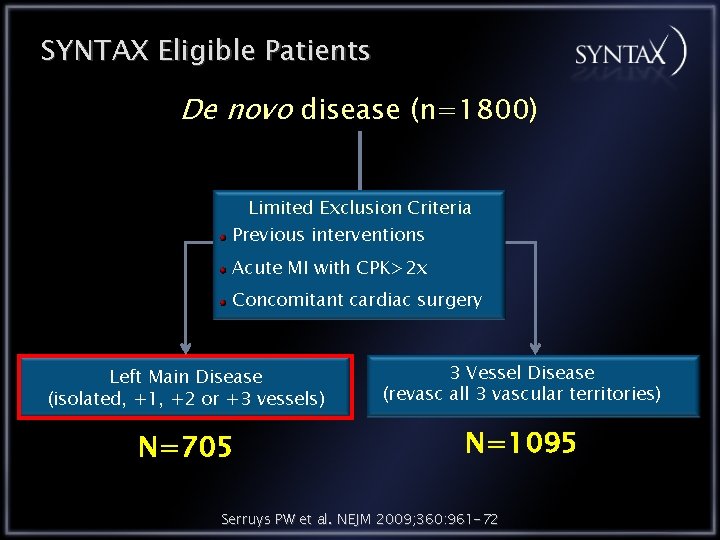
SYNTAX Eligible Patients De novo disease (n=1800) Limited Exclusion Criteria Previous interventions Acute MI with CPK>2 x Concomitant cardiac surgery Left Main Disease (isolated, +1, +2 or +3 vessels) 3 Vessel Disease (revasc all 3 vascular territories) N=705 N=1095 Serruys PW et al. NEJM 2009; 360: 961 -72
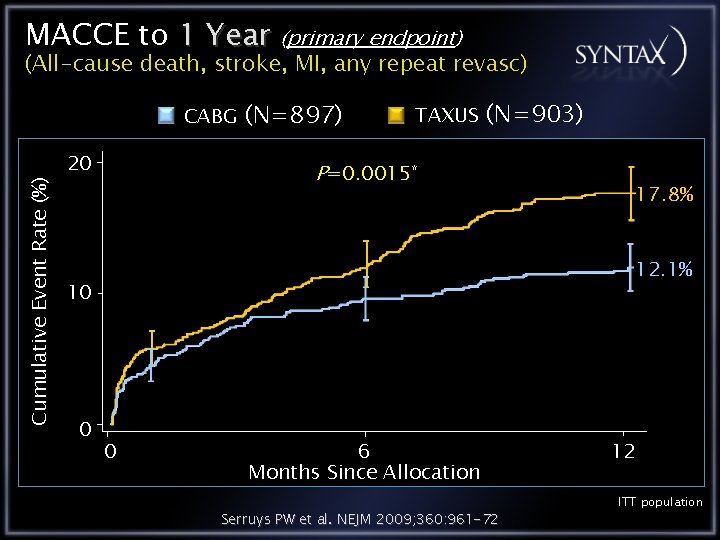
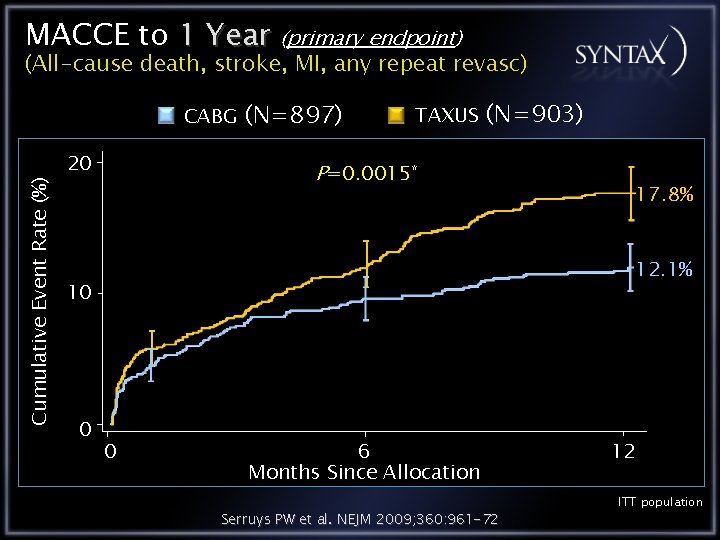
MACCE to 1 Year (primary endpoint) (All-cause death, stroke, MI, any repeat revasc) Cumulative Event Rate (%) CABG 20 (N=897) TAXUS (N=903) P=0. 0015* 12. 1% 10 0 17. 8% 0 6 Months Since Allocation Serruys PW et al. NEJM 2009; 360: 961 -72 12 ITT population
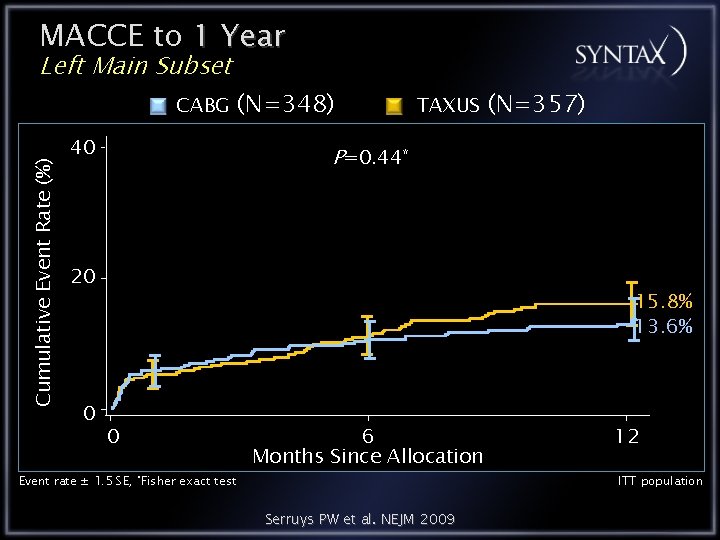
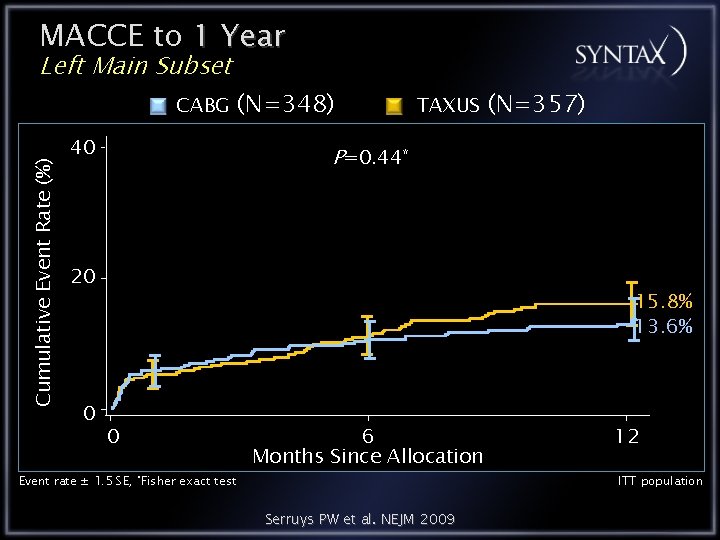
MACCE to 1 Year Left Main Subset Cumulative Event Rate (%) CABG 40 (N=348) TAXUS P=0. 44* 20 0 (N=357) 15. 8% 13. 6% 0 Event rate ± 1. 5 SE, *Fisher exact test 6 Months Since Allocation Serruys PW et al. NEJM 2009 12 ITT population
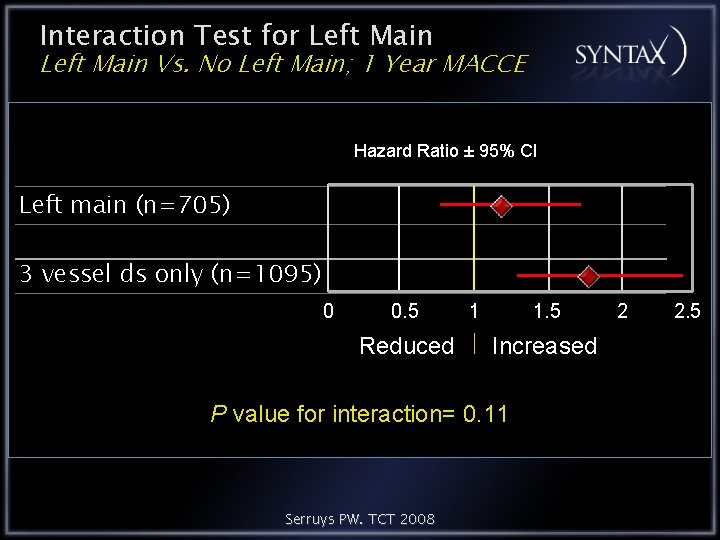
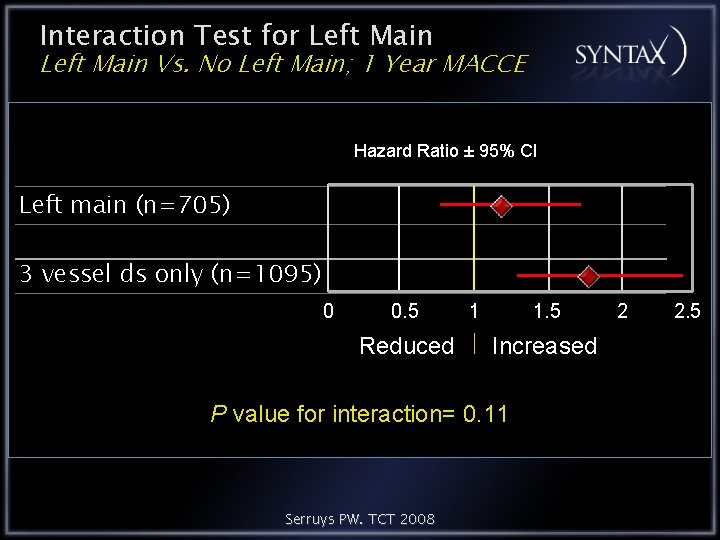
Interaction Test for Left Main Vs. No Left Main; 1 Year MACCE Hazard Ratio ± 95% CI Left main (n=705) 3 vessel ds only (n=1095) 0 0. 5 Reduced 1 1. 5 Increased P value for interaction= 0. 11 Serruys PW. TCT 2008 2 2. 5
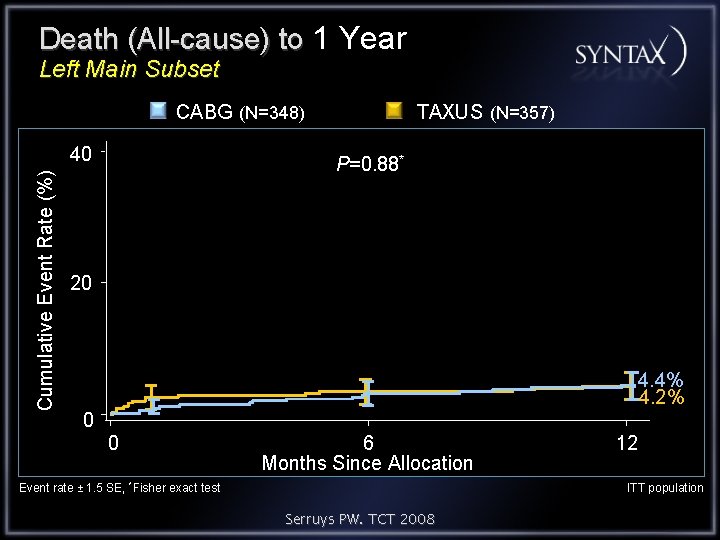
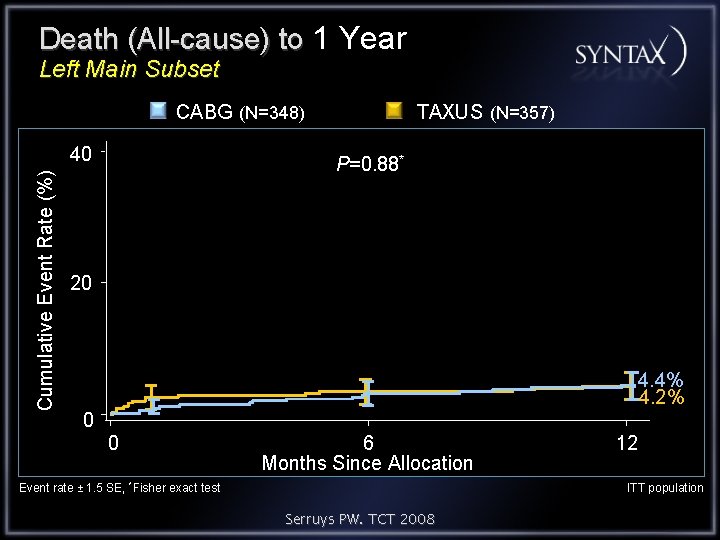
Death (All-cause) to 1 Year Left Main Subset CABG (N=348) Cumulative Event Rate (%) 40 TAXUS (N=357) P=0. 88* 20 4. 4% 4. 2% 0 0 6 Months Since Allocation Event rate ± 1. 5 SE, *Fisher exact test 12 ITT population Serruys PW. TCT 2008
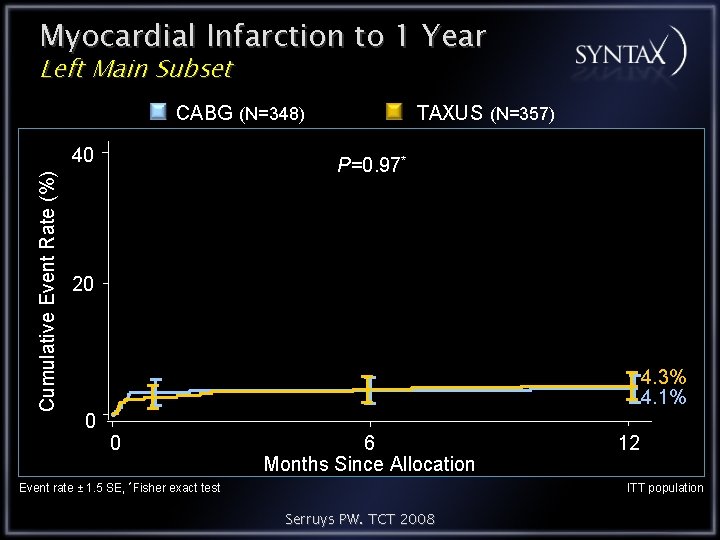
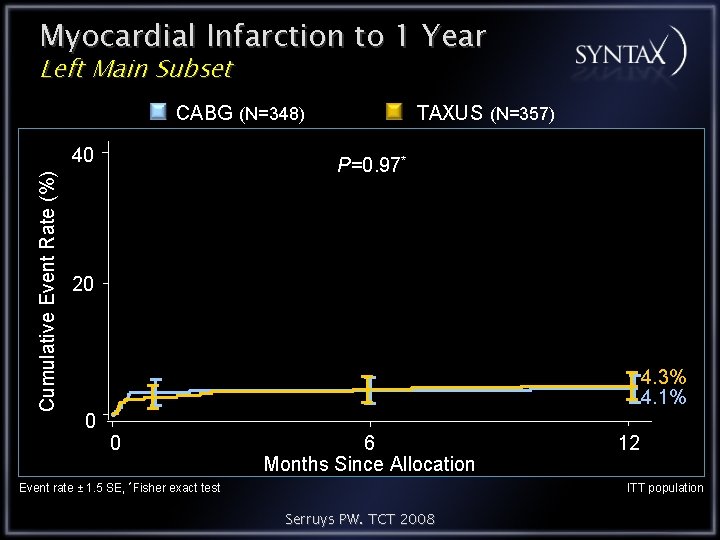
Myocardial Infarction to 1 Year Left Main Subset CABG (N=348) Cumulative Event Rate (%) 40 TAXUS (N=357) P=0. 97* 20 4. 3% 4. 1% 0 0 6 Months Since Allocation Event rate ± 1. 5 SE, *Fisher exact test 12 ITT population Serruys PW. TCT 2008

CVA (Stroke) to 1 Year Left Main Subset CABG (N=348) Cumulative Event Rate (%) 40 TAXUS (N=357) P=0. 009* 20 0 2. 7% 0. 3% 0 6 Months Since Allocation Event rate ± 1. 5 SE, *Fisher exact test 12 ITT population Serruys PW. TCT 2008
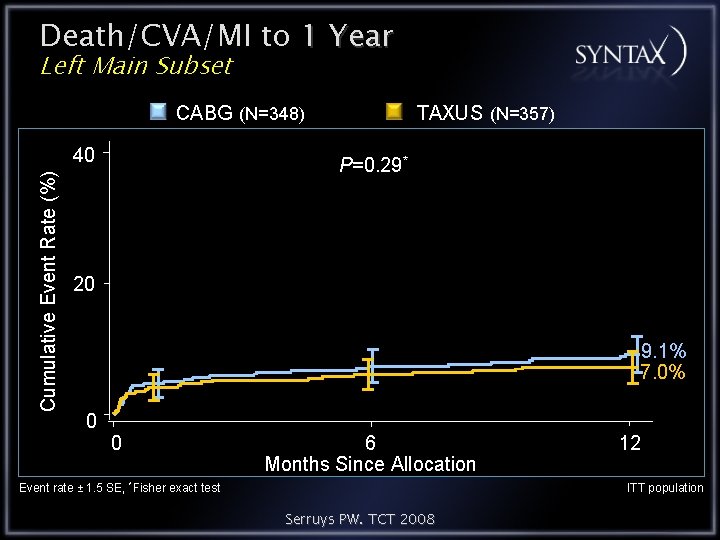
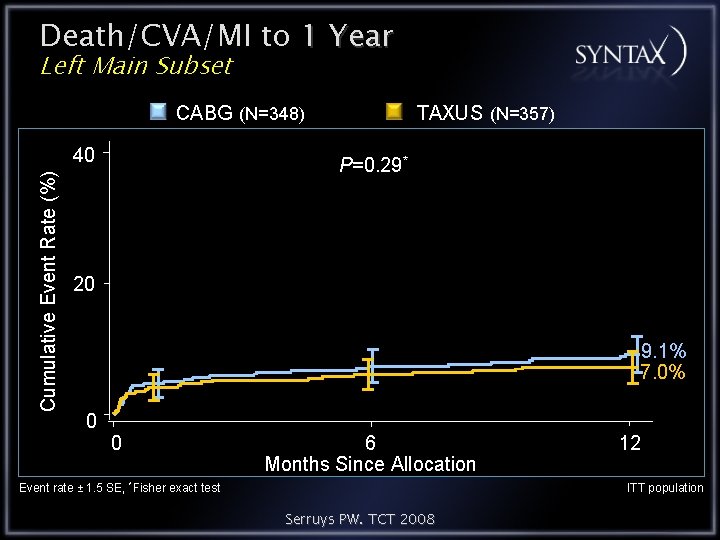
Death/CVA/MI to 1 Year Left Main Subset CABG (N=348) Cumulative Event Rate (%) 40 TAXUS (N=357) P=0. 29* 20 9. 1% 7. 0% 0 0 6 Months Since Allocation Event rate ± 1. 5 SE, *Fisher exact test 12 ITT population Serruys PW. TCT 2008
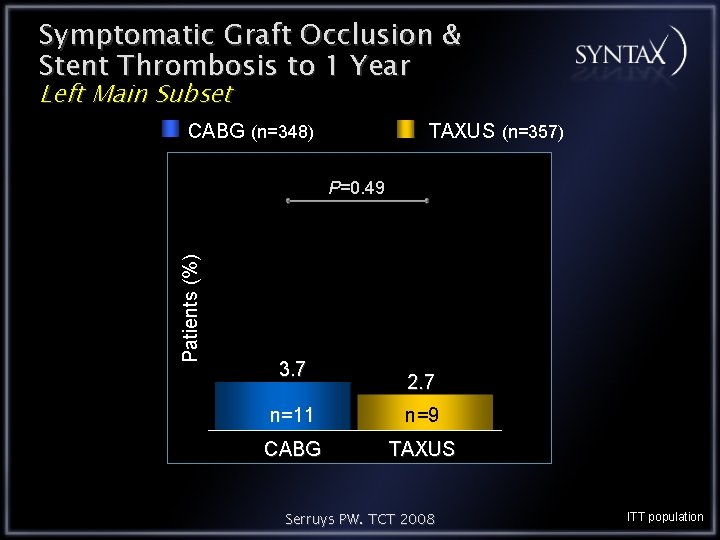
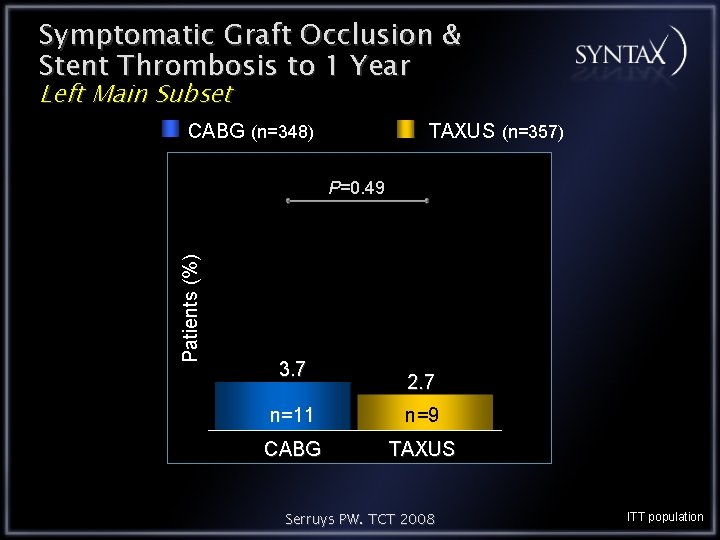
Symptomatic Graft Occlusion & Stent Thrombosis to 1 Year Left Main Subset CABG (n=348) TAXUS (n=357) Patients (%) P=0. 49 3. 7 2. 7 n=11 n=9 CABG TAXUS Serruys PW. TCT 2008 ITT population

Revascularization* to 1 Year Left Main Subset CABG (N=348) Cumulative Event Rate (%) 40 TAXUS (N=357) P=0. 02* 20 12. 0% 6. 7% 0 0 Event rate ± 1. 5 SE, *Fisher exact test 6 Months Since Allocation *Any Serruys PW. TCT 2008 12 revascularization (PCI or CABG); ITT population
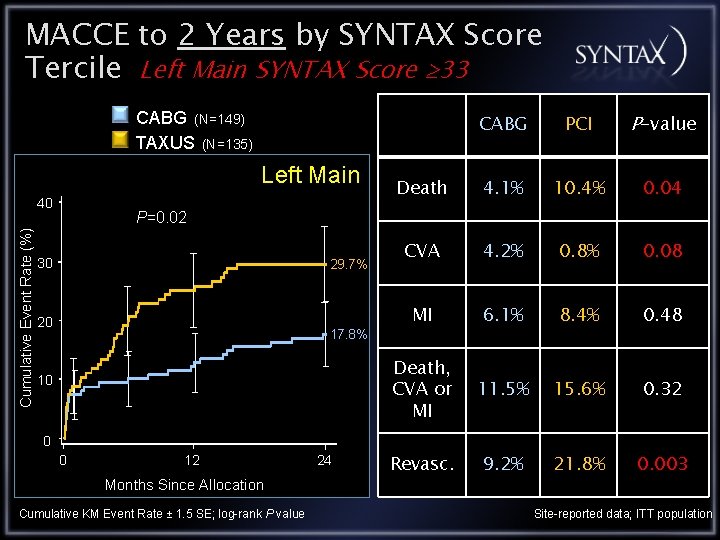
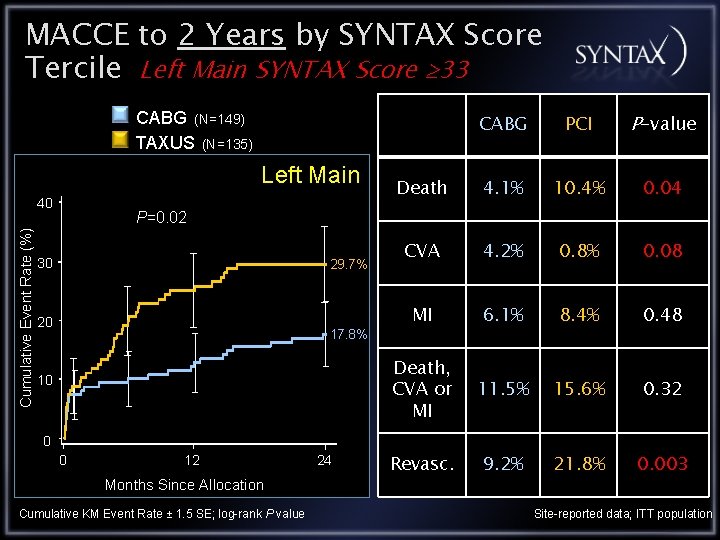
MACCE to 2 Years by SYNTAX Score Tercile Left Main SYNTAX Score 33 CABG (N=149) TAXUS (N=135) Left Main Cumulative Event Rate (%) 40 CABG PCI P-value Death 4. 1% 10. 4% 0. 04 CVA 4. 2% 0. 8% 0. 08 MI 6. 1% 8. 4% 0. 48 Death, CVA or MI 11. 5% 15. 6% 0. 32 Revasc. 9. 2% 21. 8% 0. 003 P=0. 02 30 29. 7% 20 17. 8% 10 0 0 12 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value 24 Site-reported data; ITT population
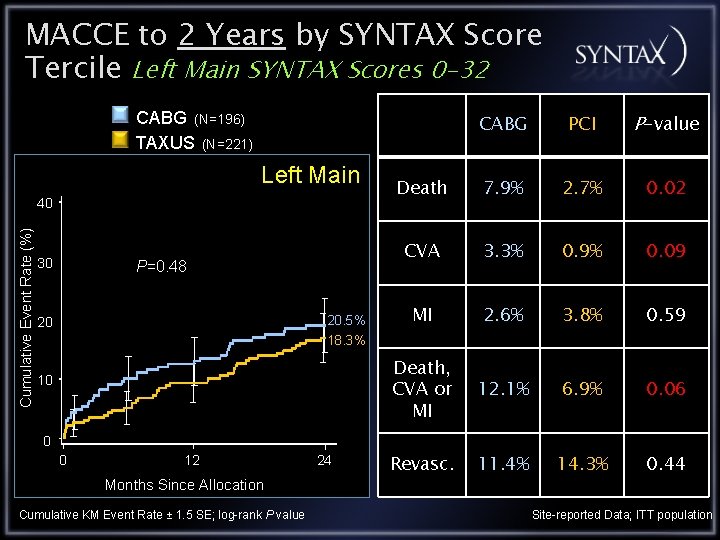
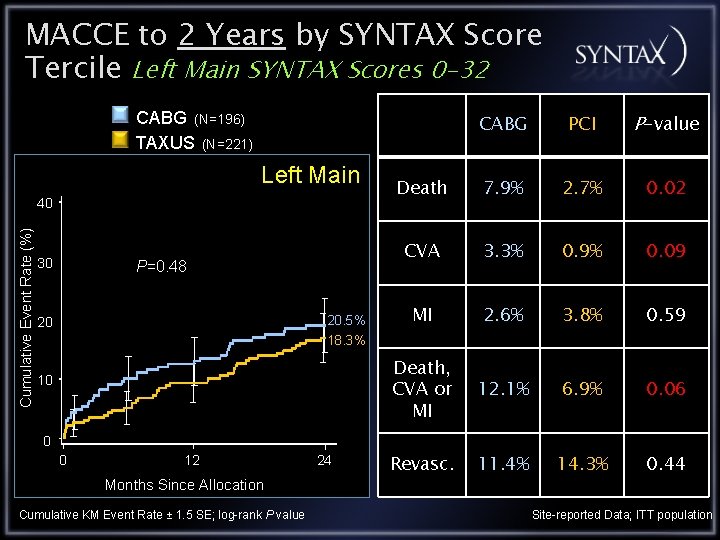
MACCE to 2 Years by SYNTAX Score Tercile Left Main SYNTAX Scores 0 -32 CABG (N=196) TAXUS (N=221) Left Main Cumulative Event Rate (%) 40 30 P=0. 48 20. 5% 20 CABG PCI P-value Death 7. 9% 2. 7% 0. 02 CVA 3. 3% 0. 9% 0. 09 MI 2. 6% 3. 8% 0. 59 Death, CVA or MI 12. 1% 6. 9% 0. 06 Revasc. 11. 4% 14. 3% 0. 44 18. 3% 10 0 0 12 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value 24 Site-reported Data; ITT population
Conclusions Are the current guidelines for elective LM PCI (class IIb) appropriate? YES But, is LM PCI for selected lesions (e. g. SYNTAX score ≤ 32) preferred? I believe so, but…. . A large-scale, randomized trial of LM PCI vs. DES is required before the guidelines should change!
Do we really need another randomized trial of PCI vs. CABG for LM disease? • YES: SYNTAX leaves many questions unanswered 1) SYNTAX suggests (but doesn’t prove) that: - PCI and CABG for LM ds. have similar rates of death/MI/stroke - PCI may be acceptable or superior for certain LM subsets 2) Could the results be further improved with a better DES? 3) What is the optimal approach to the distal bifurcation? 4) Could IVUS and/or FFR improve outcomes?
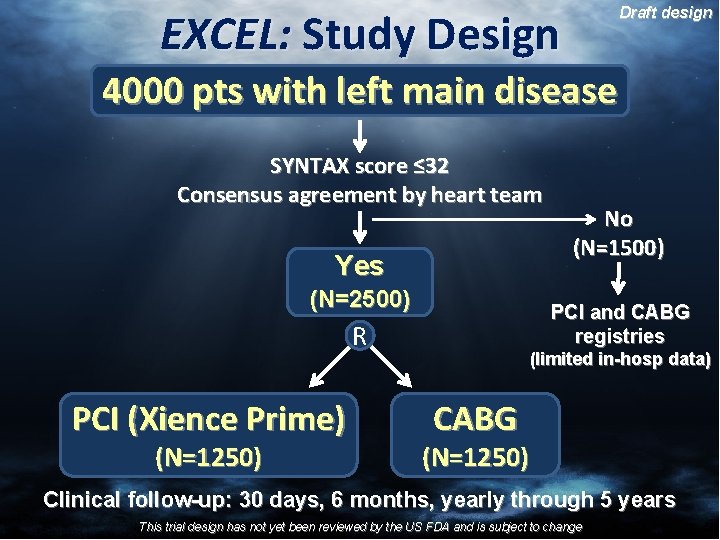
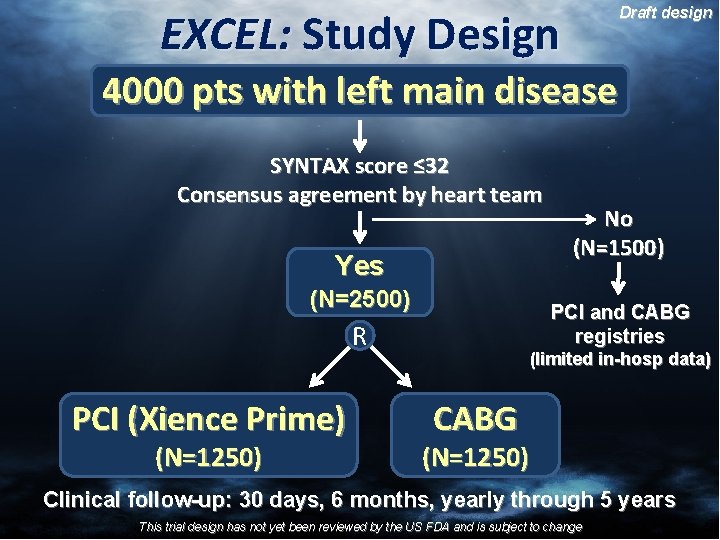
EXCEL: Study Design Draft design 4000 pts with left main disease SYNTAX score ≤ 32 Consensus agreement by heart team Yes (N=2500) PCI and CABG registries R PCI (Xience Prime) (N=1250) No (N=1500) (limited in-hosp data) CABG (N=1250) Clinical follow-up: 30 days, 6 months, yearly through 5 years This trial design has not yet been reviewed by the US FDA and is subject to change