Shock Inadequate oxygenation or perfusion causes u Inadequate







- Slides: 45
Shock Inadequate oxygenation or perfusion causes: u. Inadequate cellular oxygenation u. Shift from aerobic to anaerobic metabolism
Objectives • • Understand what shock is Define types of shock Understand Pathophysiology of shock Understand how to treat shock
WHAT IS SHOCK? Inadequate Tissue Perfusion
Circulatory Homeostasis Tissue perfusion is driven by blood pressure BP = CO X PVR CO – Cardiac Output PVR – Peripheral Vascular resistance
Cardiac Output CO = SV X HR This means that BP= SV X HR X PVR Blood Pressure = Stroke Volume X Heart Rate X Peripheral Vascular Resistance
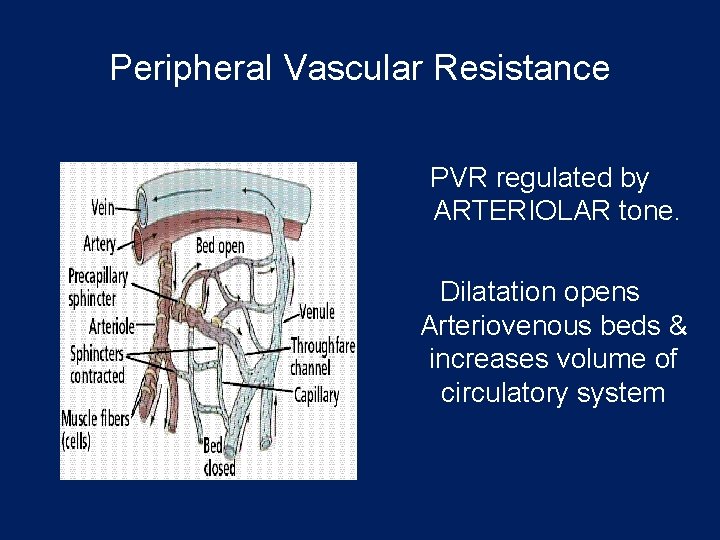
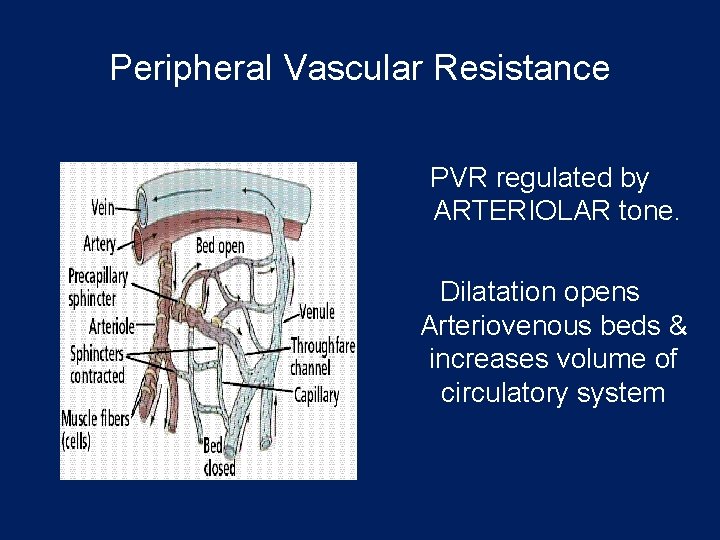
Peripheral Vascular Resistance PVR regulated by ARTERIOLAR tone. Dilatation opens Arteriovenous beds & increases volume of circulatory system
Pathophysiological Response • “Flight or fight response” • • Increased Catecholamine release Activation of Renin-Angiotensin system Increase glucocorticoid and mineralcorticoid release Activation of Sympathetic nervous system
Shock The pathway to shock follows a common metabolic pattern.
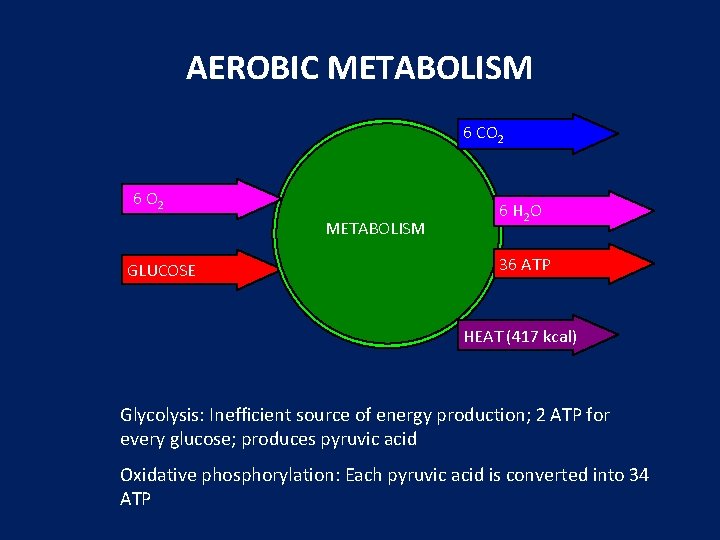
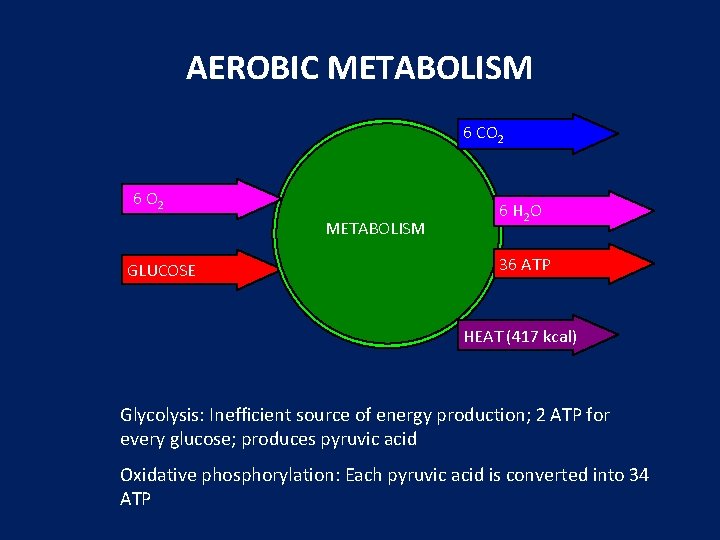
AEROBIC METABOLISM 6 CO 2 6 O 2 METABOLISM GLUCOSE 6 H 2 O 36 ATP HEAT (417 kcal) Glycolysis: Inefficient source of energy production; 2 ATP for every glucose; produces pyruvic acid Oxidative phosphorylation: Each pyruvic acid is converted into 34 ATP
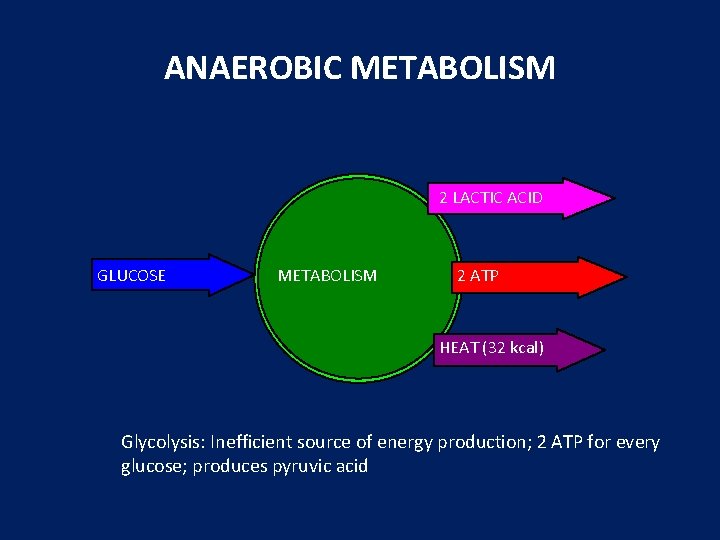
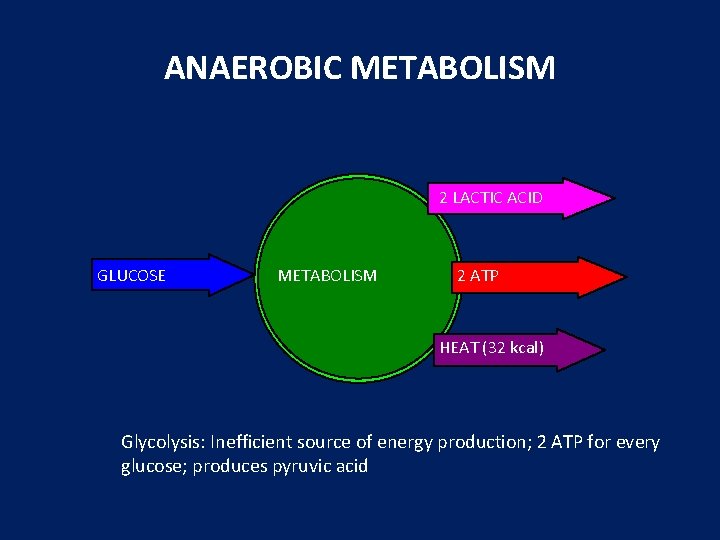
ANAEROBIC METABOLISM 2 LACTIC ACID GLUCOSE METABOLISM 2 ATP HEAT (32 kcal) Glycolysis: Inefficient source of energy production; 2 ATP for every glucose; produces pyruvic acid
Anaerobic Metabolism • Occurs without oxygen – oxydative phosphorylation can’t occur without oxygen – glycolysis can occur without oxygen – cellular death leads to tissue and organ death – can occur even after return of perfusion • organ or organism death

Ultimate Effects of Anaerobic Metabolism Inadequate Energy Production Metabolic Failure Inadequate Cellular Oxygen Delivery Anaerobic Metabolism CELL DEATH Lactic Acid Production Metabolic Acidosis
Maintaining perfusion requires: • • Volume Pump Vessels Failure of one or more of these causes shock
Stages of Shock • Compensated – The body’s compensatory mechanisms are able to maintain some degree of tissue perfusion. • Decompensated – The body’s compensatory mechanisms fail to maintain tissue perfusion (blood pressure falls). • Irreversible – Tissue and cellular damage is so massive that the organism dies even if perfusion is restored.

Shock • Do you remember how to quickly estimate blood pressure by pulse? • If you palpate a pulse, you know SBP is at least this number 60 70 80 90
Shock • Shock is inadequate tissue perfusion.
Shock (Classifications) • Physiological classifications better describe underlying problem: – Cardiogenic Shock – Hypovolemic Shock – Distributive Shock • Spinal Shock • Septic Shock • Anaphylactic
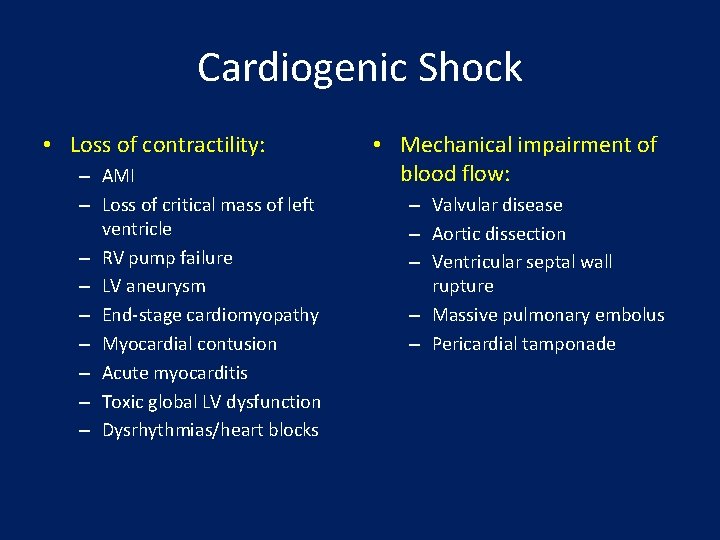
Cardiogenic Shock • The heart cannot pump enough blood to meet the metabolic demands of the body.
Cardiogenic Shock • Loss of contractility: – AMI – Loss of critical mass of left ventricle – RV pump failure – LV aneurysm – End-stage cardiomyopathy – Myocardial contusion – Acute myocarditis – Toxic global LV dysfunction – Dysrhythmias/heart blocks • Mechanical impairment of blood flow: – Valvular disease – Aortic dissection – Ventricular septal wall rupture – Massive pulmonary embolus – Pericardial tamponade
Hypovolemic Shock • Fluid (blood or plasma) is lost from the intravascular space.

Hypovolemic Shock • Trauma: – Solid organ injury – Pulmonary parenchymal injury – Myocardial laceration/rupture – Vascular injury – Retroperitoneal hemorrhage – Fractures – Lacerations – Epistaxis – Burns • GI Tract: – – – – – Esophageal varices Ulcer disease Gastritis/esophagitis Mallory-Weiss tear Malignancies Vascular lesions Inflammatory bowel disease Ischemic bowel disease Infectious GI disease Pancreatitis
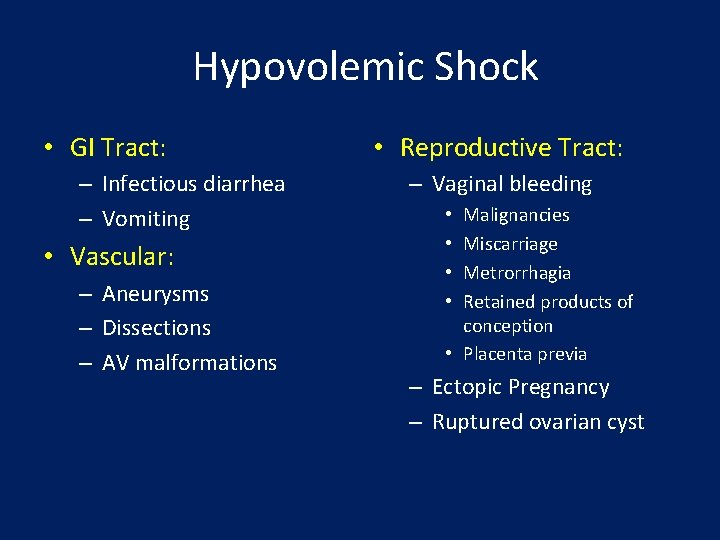
Hypovolemic Shock • GI Tract: – Infectious diarrhea – Vomiting • Vascular: – Aneurysms – Dissections – AV malformations • Reproductive Tract: – Vaginal bleeding Malignancies Miscarriage Metrorrhagia Retained products of conception • Placenta previa • • – Ectopic Pregnancy – Ruptured ovarian cyst
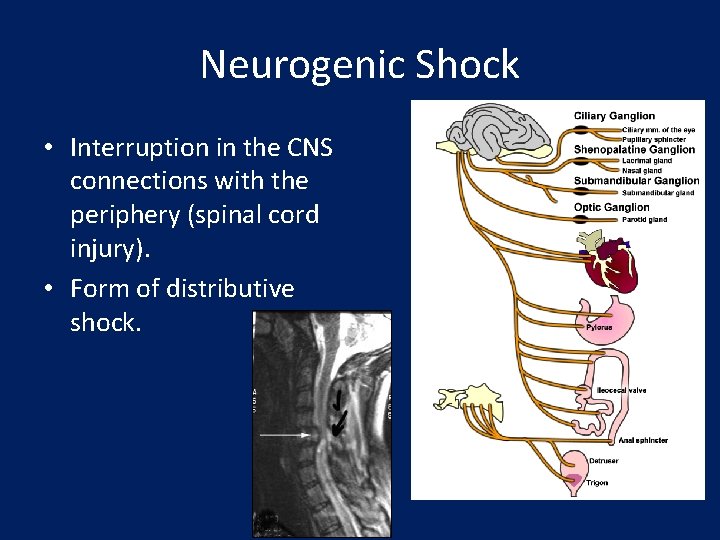
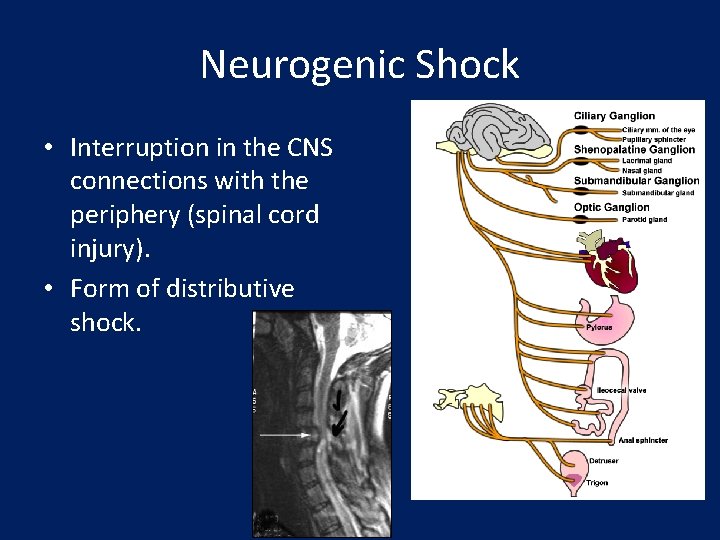
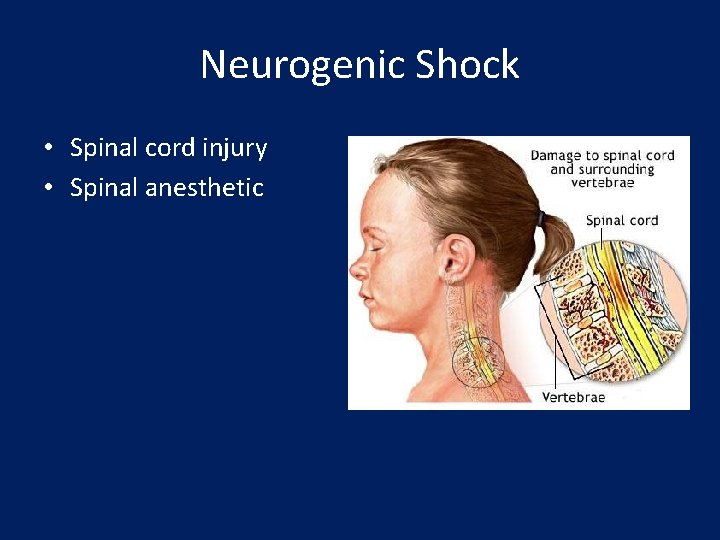
Neurogenic Shock • Interruption in the CNS connections with the periphery (spinal cord injury). • Form of distributive shock.
Neurogenic Shock • Spinal cord injury • Spinal anesthetic

Anaphylactic Shock • Shock resulting from widespread hypersensitivity. • Form of distributive shock. Killer Bee
Anaphylactic Shock • Drugs: – Penicillin and related antibiotics – Aspirin – Trimethoprimsulfamethoxazole (Bactrim, Septra) – Vancomycin – NSAIDs • Other: – Hymenoptera stings – Insect parts and molds – X-Ray contrast media (ionic) • Foods and Additives: – – – – – Shellfish Soy beans Nuts Wheat Milk Eggs Monosodium glutamate Nitrates and nitrites Tartrazine dyes (food colors)
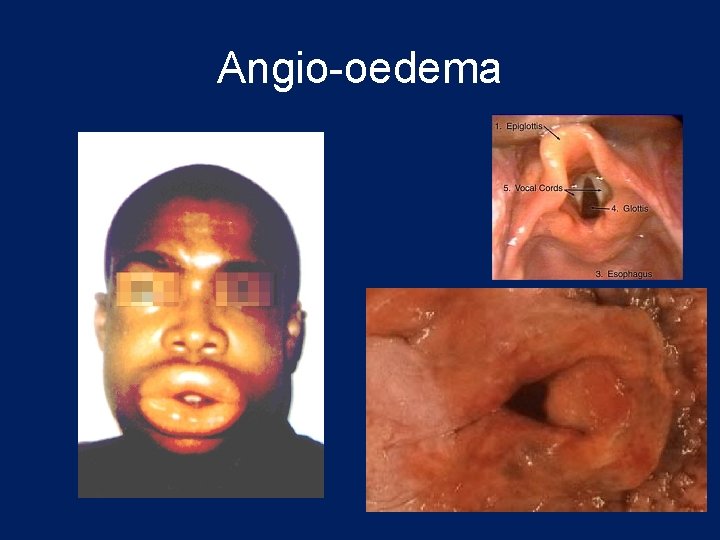
Anaphylactic Shock Common Features • • Angio-oedema Bronchoconstriction Vasodilatation and hypotension Urticareal rash
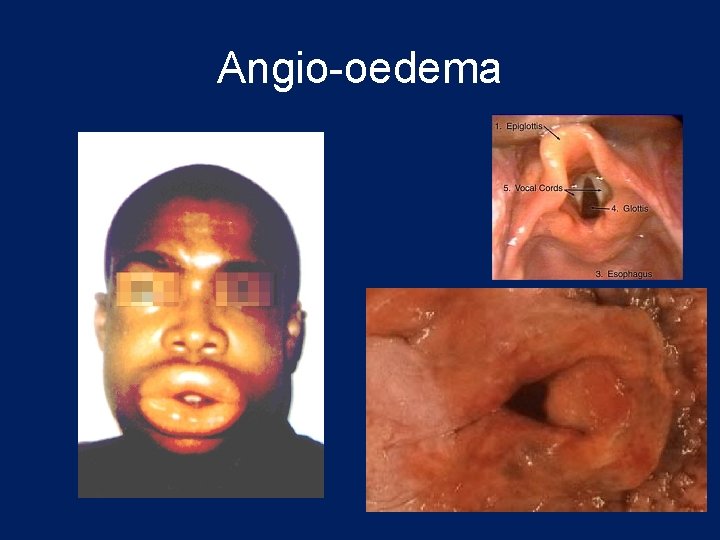
Angio-oedema
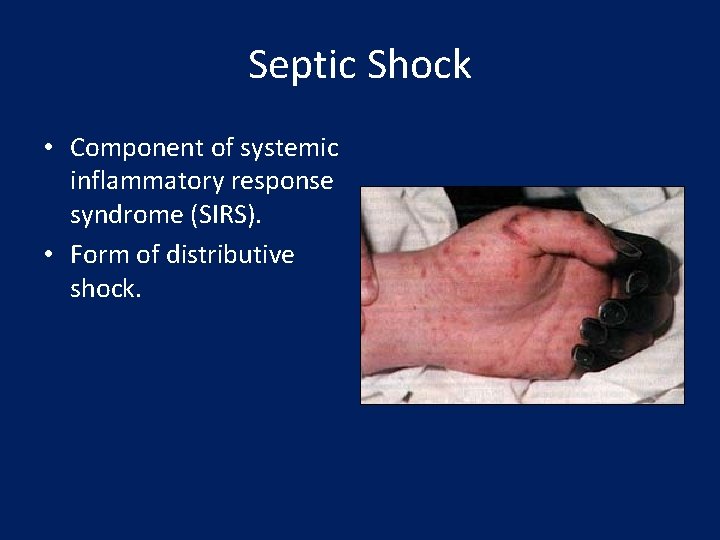
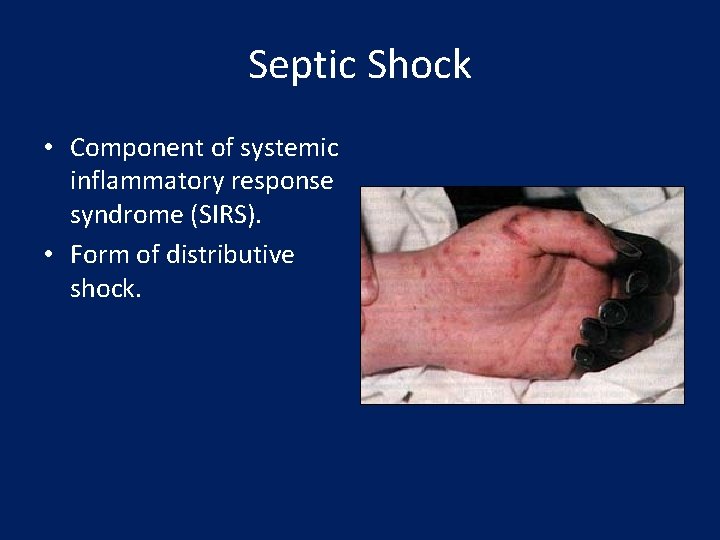
Septic Shock • Component of systemic inflammatory response syndrome (SIRS). • Form of distributive shock.
Septic Shock • Patient has nidus of infection. • Causative organism releases: – Endotoxin • Toxic shock syndrome toxin-1 • Toxin A (Pseudomonas aeruginosa) – Structure Components • Teichoic acid antigen • Endotoxin – Activates immune system cascade

Treatment of Shock • Ensure Adequate Intravascular Volume • Support Pump
Goals of Treatment • ABCDE • Airway • control work of Breathing • optimize Circulation • assure adequate oxygen Delivery • achieve End points of resuscitation
Airway • Determine need for intubation but remember: intubation can worsen hypotension • Sedatives can lower blood pressure • Positive pressure ventilation decreases preload • May need volume resuscitation prior to intubation to avoid hemodynamic collapse
Control Work of Breathing • Respiratory muscles consume a significant amount of oxygen • Tachypnea can contribute to lactic acidosis • Mechanical ventilation and sedation decrease WOB and improves survival
Optimizing Circulation • Isotonic crystalloids • Titrated to: • CVP 8 -12 mm Hg • Urine output 0. 5 ml/kg/hr (30 ml/hr) • Improving heart rate • May require 4 -6 L of fluids • No outcome benefit from colloids
Maintaining Oxygen Delivery • Decrease oxygen demands • Provide analgesia and anxiolytics to relax muscles and avoid shivering • Maintain arterial oxygen saturation/content • Give supplemental oxygen • Maintain Hemoglobin > 10 g/d. L • Serial lactate levels or central venous oxygen saturations to assess tissue oxygen extraction
End Points of Resuscitation • Goal of resuscitation is to maximize survival and minimize morbidity • Use objective hemodynamic and physiologic values to guide therapy • Goal directed approach • • Urine output > 0. 5 m. L/kg/hr CVP 8 -12 mm. Hg MAP 65 to 90 mm. Hg Central venous oxygen concentration > 70%

Cardiogenic Shock • Treatment: – – – – Oxygen Monitors Nitrates (if possible) Morphine or fentanyl Pressor support (dopamine or dobutamine) If no pulmonary edema, consider small fluid boluses IABP Definitive therapy (fibrinolytic therapy, PTCA, CABG, ventricular assist device, cardiac transplant)
Hypovolemic Shock • Treatment: – Oxygen – Supine position – Monitors – IV access – Fluid replacement – Pressor support (rarely needed) – Correct underlying cause
Hypovolemic Shock • Fluid replacement: – Hypovolemia: • Crystalloids • Colloids – Hemorrhage: • Whole blood • Packed RBCs • Crystalloids
Neurogenic Shock • Treatment: – ABCDE – Fluid resuscitation with crystalloid – PA catheter helpful in preventing overhydration. – Look for other causes of hypotension – Consider vasopressor support with dopamine or dobutamine – Transfer patient to regional spine center
Anaphylactic Shock • Treatment: – – – Airway (have low threshold for early intubation) Oxygenation and ventilation Epinephrine (IV, IM, Subcutaneously) IV Fluids (crystalloids) Antihistamines • Benadryl • Zantac – – Steroids Beta agonists Aminophylline Pressor support (dopamine, dobutamine or epinephrine)

Septic Shock • Treatment: – – – – – Airway and ventilatory management Oxygenation IV fluids (crystalloids) Pressor support (dopamine, norepinephrine) Empiric antibiotics Removal of source of infection Adrenaline, Bronco dilators Na. HCO 3? Steroids? Anti-endotoxin antibodies
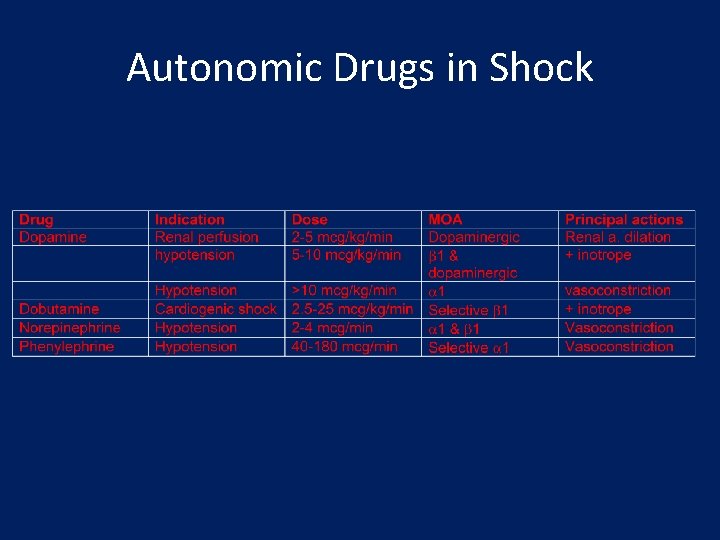
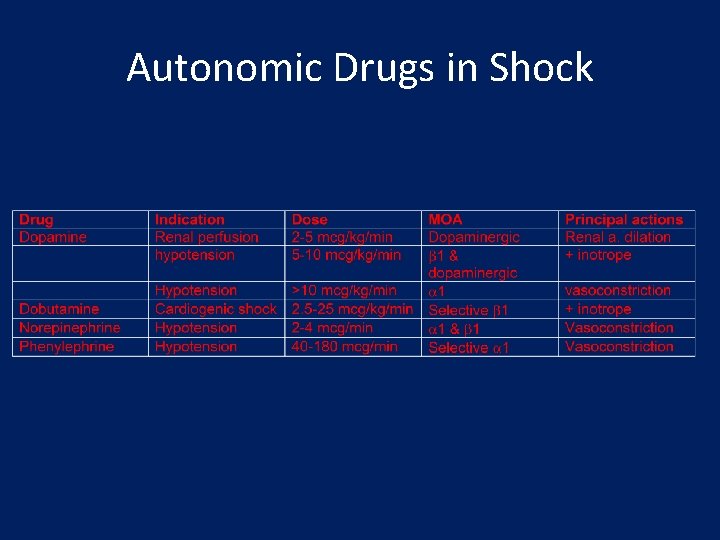
Autonomic Drugs in Shock
Summary • To understand the shock, you must first understand the pathophysiology. • Once you understand the pathophysiology, then recognition of the signs and symptoms and treatment becomes intuitive.