Shock By DR Ahmad Gaber Mahmoud Introduction n

Shock By DR. Ahmad Gaber Mahmoud
Introduction n n Definition of shock Types or causes of shock Pathophysiology of shock Diagnosis of shock 1. Clinical stages of shock 2. Causes of shock Treatment of shock
A more recent definition calls shock “the collapse and progressive failure of the cardiovascular system. ” I. e. Acute circulatory failure. n Shock left untreated may be fatal. It must be recognized and treated immediately, or the patient may die. n
Shock The definition of shock does not involve low blood pressure, rapid pulse or cool clammy skin - these are merely the signs. Simply stated shock results from Inadequate perfusion leading to failure of tissue oxygenation with Generalized cellular hypoxia.
Maintaining perfusion requires: Volume n Pump n Vessels n Failure of one or more of these causes shock n
Types of Shock
Types or causes of shock: S: Septic shock n H: Hypovolemic shock n O: Obstructive shock n C: Cardiogenic shock n K: Kinetic or Distributive shock n
Shock n Septic Shock – Mixed Shock • Overwhelming infection • Caused by gram negative bacteria that release endotoxins (endotoxemic shock). • Peritonitis, cholangitis, genitourinary infection & infected CV catheter • Predisposed by immunosuppression – Diabetes, corticosteroids, chemotherapy – Malignancy & HIV/ AIDS
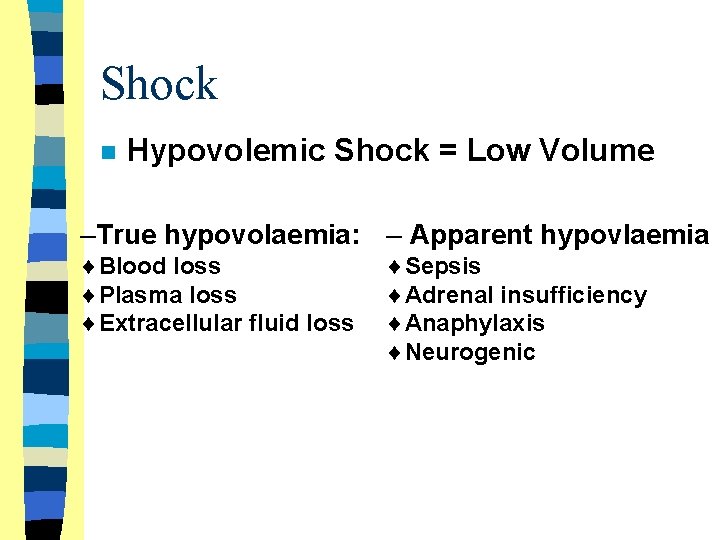
Shock n Hypovolemic Shock = Low Volume –True hypovolaemia: – Apparent hypovlaemia ¨Blood loss ¨Plasma loss ¨Extracellular fluid loss ¨Sepsis ¨Adrenal insufficiency ¨Anaphylaxis ¨Neurogenic

Shock n Obstructive Shock = Obstruction to blood flow – Tension pneumothorax or haemothorax – Cardiac tamponade (due to pericardial effusion or hemopericardium) – Aortic stenosis or critical coarctation – Pulmonary embolism
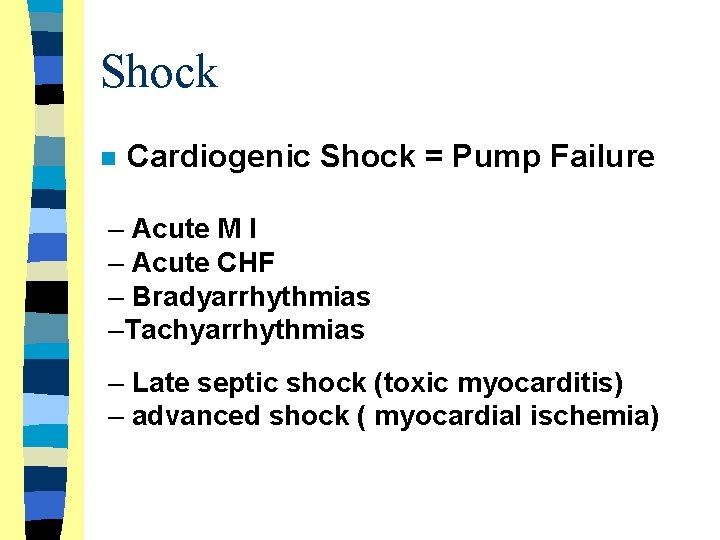
Shock n Cardiogenic Shock = Pump Failure – Acute M I – Acute CHF – Bradyarrhythmias –Tachyarrhythmias – Late septic shock (toxic myocarditis) – advanced shock ( myocardial ischemia)
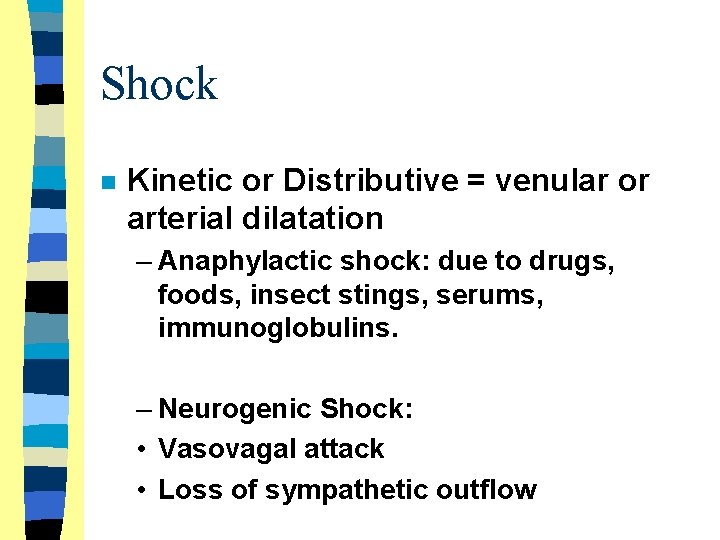
Shock n Kinetic or Distributive = venular or arterial dilatation – Anaphylactic shock: due to drugs, foods, insect stings, serums, immunoglobulins. – Neurogenic Shock: • Vasovagal attack • Loss of sympathetic outflow
Pathophysiology of Shock
Shock Pathophysiology of shock n Hypoperfusion of tissues is serious as it lead to tissue iscaemia ( hypoxia & substrate deficiency) and tissue damage
Shock Inadequate oxygenation or perfusion causes: u. Inadequate cellular oxygenation u. Shift from aerobic to anaerobic metabolism
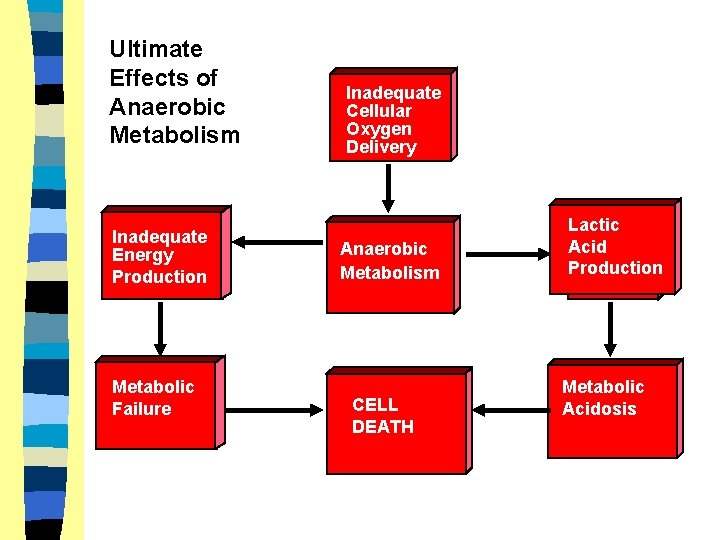
Ultimate Effects of Anaerobic Metabolism Inadequate Energy Production Metabolic Failure Inadequate Cellular Oxygen Delivery Anaerobic Metabolism CELL DEATH Lactic Acid Production Metabolic Acidosis
Shock Pathophysiological stages of shock: n Three phases – Compensated stage – Decompensated stage – Irreversible stage
Compensated Shock n During this early stage there is Sympathoadrenal response with excess catecholamine release to prevent the fall in blood pressure.
Compensated Shock n Cardiac effects • Increased force of contractions • Increased rate • Increased cardiac output
Compensated Shock n Peripheral effects • Arteriolar constriction • Pre-/post-capillary sphincter contraction • Increased peripheral resistance • Shunting of blood to core organs
Compensated Shock n Decreased renal blood flow – Renin released from kidney arteriole – Renin & Angiotensinogen combine – Converts to Angiotensin I – Angiotensin I converts to Angiotensin II • Peripheral vasoconstriction • Increased aldosterone release (adrenal cortex) – promotes reabsorption of sodium & water
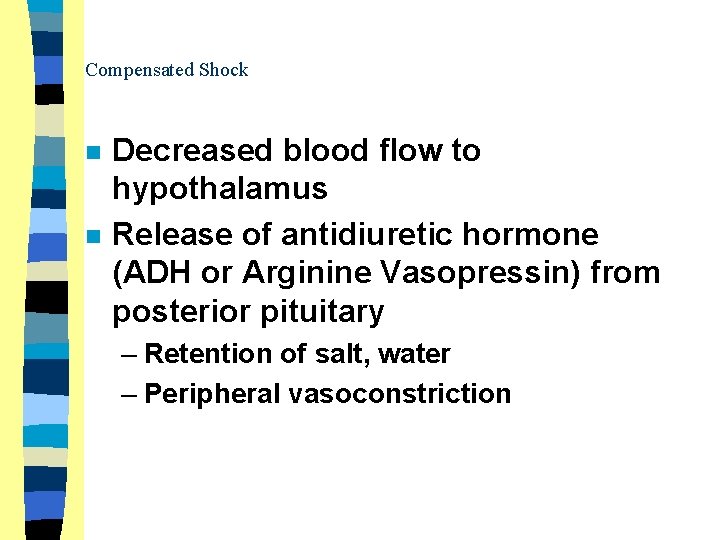
Compensated Shock n n Decreased blood flow to hypothalamus Release of antidiuretic hormone (ADH or Arginine Vasopressin) from posterior pituitary – Retention of salt, water – Peripheral vasoconstriction
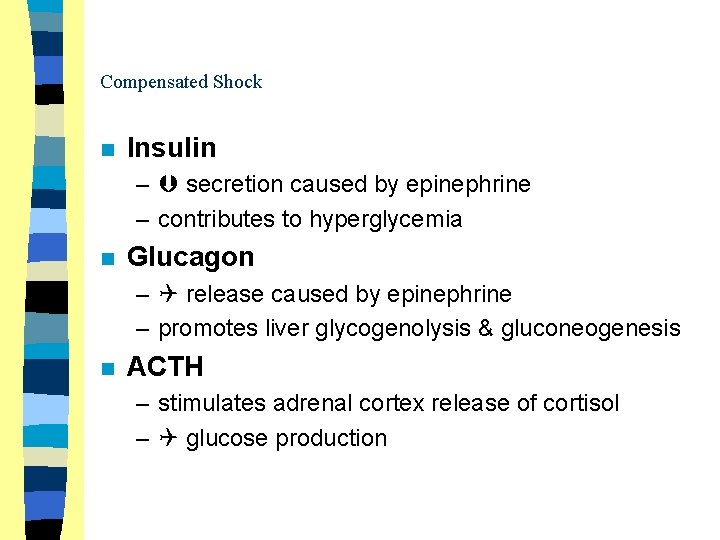
Compensated Shock n Insulin – secretion caused by epinephrine – contributes to hyperglycemia n Glucagon – release caused by epinephrine – promotes liver glycogenolysis & gluconeogenesis n ACTH – stimulates adrenal cortex release of cortisol – glucose production
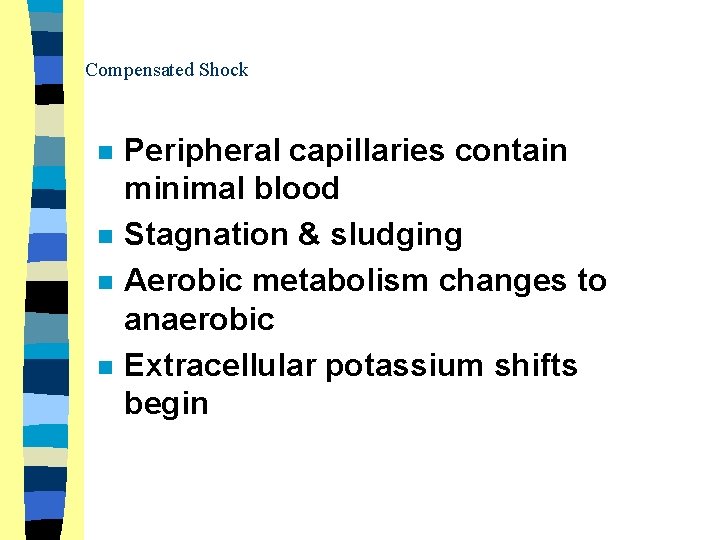
Compensated Shock n n Peripheral capillaries contain minimal blood Stagnation & sludging Aerobic metabolism changes to anaerobic Extracellular potassium shifts begin
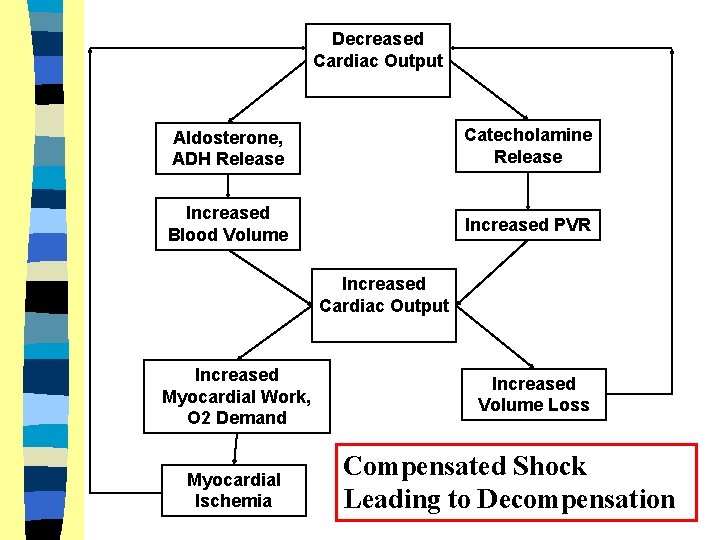
Decreased Cardiac Output Aldosterone, ADH Release Catecholamine Release Increased Blood Volume Increased PVR Increased Cardiac Output Increased Myocardial Work, O 2 Demand Myocardial Ischemia Increased Volume Loss Compensated Shock Leading to Decompensation
Decompensated Shock n Compensatory mechanisms fail and hypotension occurs – Cardiac Effects • Decreased RBC oxygenation • Decreased coronary blood flow • Myocardial ischemia • Decreased force of contraction
Decompensated Shock n Presentation – Peripheral effects • Relaxation of precapillary sphincters • Continued contraction of postcapillary sphincters • Peripheral pooling of blood • D. I. C. • Plasma leakage into interstitial spaces
Decompensated Shock n Presentation – Peripheral effects • Continued anaerobic metabolism • Continued increase in extra cellular potassium
Irreversible Shock Post-capillary sphincter relaxation n Loss of peripheral vascular resistance n
Irreversible Shock n Washout of accumulated products • Hydrogen ion • Potassium • Carbon dioxide n n Systemic metabolic acidosis occurs Cardiac Output decreases further
Irreversible Shock Permanent cellular damage. n Death occurs due to refractory acidosis, myocardial & brain ischemia. n
Diagnosis of Shock
Diagnosis of Shock n Should includes: 1 - Clinical stages of shock 2 - Cause of shock
Clinical stages of Shock n n Grade I (Early shock= peripheral hypoperfusion) Grade II (Established shock = Arterial hypotension) Grade III (Advanced shock = Vital organ hypoperfusion) Grade IV (Irreversible shock = irreversible cellular damage)
1 - Early Shock n Clinical manifestations: – Restlessness, anxiety • Earliest sign of shock – Tachycardia • ? Bradycardia in cardiogenic, neurogenic – Peripheral hypoperfusion: • Cold extremities • Slow capillary refill over fingernails • Skin mottling & peripheral cyanosis • In septic shock, peripheral vasoconstriction is absent (Warm shock)
2 - Established Shock n n The clinical triad of tachycardia, hypotension & poor peripheral perfusion becomes evident. Early manifestations of vital organ hypoperfusion start to appear: – Deep rapid respiration ( metabolic acidosis) – Oliguria (renal hypoperfusion) – Irritability followed by drowsiness & confusion
3 - Advanced Shock n n n Multiple organ system failure (MOSF). Reperfusion injury due to release of harmful mediators from endothelium, endotoxins & different cells Manifestations of MOSF: – Kidneys: Acute renal failure – Lungs: ARDS – GIT: stress ulcers, bacterial translocation – Liver: Acute hepatic failure – Metabolic: acidosis & electrolyte disturbance – Blood: DIC, thrmbocytopenia – Brain: Hypoxic ischemic encephalopathy – Heart: myocardial ischaemia
4 - Irreversible (refractory) Shock n Terminal stage with irreversible cellular damage: – Serious arrhythmias (myocardial ischemia) – Deep coma (brain ischemia) – Metabolic acidosis refractory to therapy (p. H is below 7. 0 in spite of vigorous correction with sodium bicarbonate) – Other MOSF becomes evident
Detection of the cause of Shock Etiologically shock is classified into the known 5 types n It is important to realize the following: n § Mixed shock § Changing shock
Detection of Cause of Shock n 1 - Septic Shock: clinical manifestations of sepsis & shock can be divided into 5 stages with increasing severity: I. III. IV. V. Sepsis and systemic inflammatory response syndrome (SIRS). Sever sepsis. Early septic shock. Late or refractory septic shock. Multiple organ system failure (MOSF)
I. Sepsis &SIRS Clinical manifestation of infection n Fever or Hypothermia n Tachycardia and tachypnea n Bandemia( above 10%), leukocytosis or leukopenia, elevated ESR &CRP n
II. Severe Sepsis n Clinical manifestation of sepsis plus one or more of the following: - acute mental changes. - oliguria. - lactic acidosis. - hypoxaemia
III. Early septic shock Clinical manifestation of sever sepsis. n Hypotension or poor peripheral perfusion that respond to I. V. fluids. n Peripheral hypoperfusion is usually absent during this stage (warm shock). n
IV. Late or refractory septic shock Clinical manifestation of sever sepsis. n Hypotension or poor peripheral perfusion refractory to I. V. fluids. n Peripheral hypoperfusion is marked during this stage (cold shock). n Inotropic drug support is necessary to improve myocardial contractility. n
V. Multiple organ system failure n More than one of the following 5: • • • n DIC ARDS ARF AHF Acute CNS dysfunction Mortality rate is very high during this stage ( 50 %).
Detection of Cause of Shock 2 - Hypovolemic Shock: n • • Clinical diagnosis is not difficult as the manifestation of causative disease are well evident ( hemorrhage, burn, dehydration). It usually respond dramatically to volume expansion and specific replacement therapy.
Detection of Cause of Shock 3 - Obstructive Shock: n • • • Occurs due to either obstruction of venous return or obstruction to arterial out flow. The condition suspected in any shock state not responding to volume expansion. Chest x- ray (pneumothorax) and echocardiography ( cardiac tamponade) are essential for diagnosis.
Detection of Cause of Shock 4 - Cardiogenic Shock: n Clinical situations suggesting cardiogenic shock: • • Shock following cardiopulmonary resuscitation (due to myocardial ischemia). Shock in patients with known congenital or acquired heart disease. Shock in patients without history of cardiac disease but with cardiomegally. Septic shock not responding to I. V. fluid expansion (for more than 1 hour)
Detection of Cause of Shock 5 - Distributive Shock: n • • • It occurs due to vascular dilatation which leads to relative hypovolaemia & decreased venous retune. Early septic shock, anaphylactic shock and neurogenic shock are classical examples. All these types respond to volume expansion and specific therapy (antibiotic in septic shock and antihistaminic & steroids in anaphylactic shock).
Shock n Mixed Shock – Anaphylactic Shock • Severe allergic reaction • Histamine is released • Blood vessels – Dilate (loss of resistance) – Leak (loss of volume)
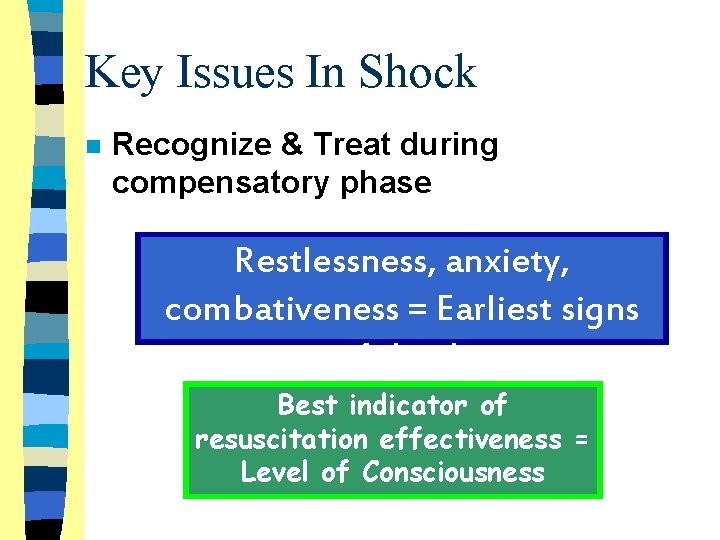
Key Issues In Shock n Recognize & Treat during compensatory phase Restlessness, anxiety, combativeness = Earliest signs of shock Best indicator of resuscitation effectiveness = Level of Consciousness
Key Issues In Shock Falling BP = LATE sign of shock n BP is NOT same thing as perfusion n Pallor, tachycardia, slow capillary refill = Shock, until proven otherwise n
Key Issues In Shock Isolated head trauma does NOT cause shock (“possible” in peds)
General Shock Management n n 1. Monitoring: 2. Cardiovascular support 3. Multisystem support. 4. specific treatment.
General Shock Management n • Monitoring: Clinical monitoring – Heart rate and respiratory rate – Peripheral perfusion ( skin temperature, capillary refill time & core-toe temperature difference). – Arterial blood pressure. – Urine output. – Level of consciousness. – Arterial oxygen saturation by pulse oximetre
General Shock Management n • Monitoring: Laboratory monitoring – – – Arterial blood gases ( hypoxemia &acidosis). Serum electrolyte. Blood sugar. Hemoglobin and coagulation profile. Sepsis screen. Renal function tests.
General Shock Management n • Monitoring: Radiological & imaging monitoring – Chest x- ray ( pneumothorax, cardiomegaly). – Echocardiography. • Invasive hemodynamic monitoring: - Central venous pressure (CVP). - Pulmonary artery pressure (PAP) and pulmonary capillary wedge pressure (PCWP). - Cardiac output (CO).
General Shock Management n Cardiovascular support: 1 - Oxygen therapy: . Give oxygen( 100%) with oxygen mask. . Reduce concentration over the next few hours. . Consider Intubation. 2 - Preload augmentation ( volume expansion) : . Give ringer lactate or saline. . Consider albumin or plasma transfusion. . Chest x- ray & Echo if no response.
General Shock Management n Cardiovascular support: 3 - contractility augmentation (inotropic drug): . Indicated in poor response to volume expansion. . Give dopamine IV infusion. . Add dobutamine when the response is inadequate. . Consider adrenaline in extremely severe cases. . Consider invasive hemodynamic monitoring.
General Shock Management n Cardiovascular support: 4 - After load reduction ( vasodilator drugs): . Indicated in poor response to inotropic drugs ( i. e. cardiogenic). . Give sodium nitroprusside I. V. infusion. . Consider pulmonary vasodilator. 5 - Treatment of arrhythmias: . Correct hypoxia, acidosis, and electrolyte disturbances. . Give the appropriate antiarrhythmic drug.
General Shock Management n Multisystem support: 1 - Respiratory Support: . Early oxygen therapy in all cases to prevent or delay respiratory fatigue. . Endotracheal intubation & CPAP for pulmonary edema. . Hyper oxygenation & Hyperventilation for acute pulmonary hypertension. 2 - Renal support : . Keep urine output above 1 ml/kg/hour. . . Give volume expanders, diuretics & low dose dopamine in oliguria. . Peritoneal dialysis in sever cases.
General Shock Management n Multisystem support: 3 - Metabolic Support: . Correct hypothermia and hyperthermia. . Correct metabolic acidosis. . Correct electrolyte disturbances. . Correct hypoglycemia or hyperglycemia 2 - Gastrointestinal support : . Antacids, & cold saline wash for stress ulcers. . Intestinal decontamination to prevent bacterial translocation. . Rest GIT in ileus. 3 - Hematological support: . Correct coagulopathies with vitamin K, fresh frozen plasma and platelets. . Consider heparinization if peripheral gangrene occurs.
General Shock Management n Specific treatment Early specific management of the underlying cause of shock will often delay further progression or deterioration requiring more aggressive therapy.
Hypovolemic Shock n n n Control severe external bleeding Elevate lower extremities Pneumatic anti-shock garment
Hypovolemic Shock n Two large bore IV lines – Infuse Lactated Ringer’s solution – Titrate BP to 90 -100 mm Hg
Hypovolemic Shock n n Do NOT delay transport Start IVs enroute to hospital
Cardiogenic Shock n n Supine, or head and shoulders slightly elevated Do NOT elevate lower extremities
Cardiogenic Shock n n Keep open line, micro-drip set Fluid challenge based on cardiovascular mechanism and history – Titrate to BP ~ 90 mm Hg
Cardiogenic Shock n n Treat the underlying cause if possible Treat rate, then rhythm, then BP u. Correct bradycardia or tachycardia v. Correct irregular rhythms w Treat BP • Cardiac contractility – Dobutamine, Dopamine • Peripheral resistance – Dopamine, Norepinephrine
Cardiogenic Shock n Obstructive Shock – Treat the underlying cause • Tension Pneumothorax • Pericardial Tamponade – Isotonic fluids titrated to BP w/o pulmonary edema – Control airway • Intubation
Shock Management Avoid vasopressors until hypovolemia ruled out, or corrected
Shock Management Squeezing partially empty tank can cause ischemia, necrosis of kidney and bowel
Vasogenic Shock n n n Consider need to assist ventilations Patient supine; lower extremities elevated Avoid Trendelenburg
Vasogenic Shock n n Infuse isotonic crystalloid – “Top off tank” Consider PASG Consider possible hypovolemia Consider vasopressors
Vasogenic Shock n n Maintain body temperature Hypothermia may occur
Vasogenic Shock n Anaphylaxis – Suppress inflammatory response • Antihistamines • Corticosteroids – Oppose histamine response • Epinephrine – bronchospasm & vasodilation – Replace intravascular fluid • Isotonic fluid titrated to BP ~ 90 mm
Shock in Children Small blood volume – Increased hypovolemia risk n Very efficient compensatory mechanisms – Failure may cause “sudden” shock n
Shock in Children n n Avoid massive fluid infusion – Use 20 cc/kg boluses High surface to volume ratio – Increased hypothermia risk
Shock in the Elderly n Poor cardiovascular condition – Rapid decompensation n n Sepsis more likely Hypoperfusion cause: – CVA – AMI – Seizures – Bowel Infarctions – Renal failure
Shock in the Elderly n Assessment more difficult – Peripheral vascular disease – Weak pulses – Altered sensorium – Hypertension masking hypoperfusion – Beta-blockers masking hypoperfusion n Fluid infusion may produce volume overload/CHF
Shock in OB Patients n n Pulse increases 10 to 15 bpm BP lower than in non-pregnant patient Blood volume increased by 45% – Slower onset of shock signs/ symptoms Fluid resuscitation requires greater volume
Shock in OB Patients n n Oxygen requirement increased 10 to 20% Pregnant uterus may compress vena cava, decreasing venous return to heart – Place women in late-term pregnancy on left-side n Fetus can be in trouble even though mother looks well-perfused

- Slides: 84